Abstract
Purpose
This paper 1) provides the calibration procedures and methods for metabolic and activity monitor data collection, 2) compares measured MET values to the MET values from the Compendium of Physical Activities, and 3) examines the relationship between accelerometer output and METs for a range of physical activities
Methods
Participants (n=277) completed 11 activities for seven minutes each from a menu of 23 physical activities. Oxygen consumption (VO2) was measured using a portable metabolic system and an accelerometer was worn. MET values were defined as follows; measuredMETs (VO2/measured RMR) and standardMETs (VO2/3.5ml·kg·min−1). For the total sample and by sub-group (age [young <40y], sex and BMI [normal-weight <25 kg·m2]), measuredMETs and standardMETs were compared to the Compendium, using 95% confidence intervals to determine statistical significance (α=0.05). Average count·min−1 for each activity and the linear association between count·min−1 and METs are presented.
Results
Compendium METs were different than measured METs for 17/21 activities (81%). The number of activities different than the Compendium were similar between sub-groups or when standard METs were used. The average counts for the activities ranged from 11 counts·min−1(dishes) to 7490 counts·min−1 (2.23m·s−1, 3%) The r2 between counts and METs was 0.65.
Conclusions
This study provides valuable information about data collection, metabolic responses, and accelerometer output for common physical activities in a diverse participant sample. The Compendium should be updated with additional empirical data and linear regression models are inappropriate for accurately predicting METs from accelerometer output.
Keywords: Energy expenditure, Activity monitors, Compendium of Physical Activities, calibration
Introduction
There is a clear association between physical activity (PA) and numerous health benefits. However, as outlined in the recent Physical Activity Guidelines Advisory Committee Report (PAGAC), there is a gap in our understanding of the dose-response relationship between PA and health outcomes that is due, in part, to poor and inconsistent measures of PA exposure (24). Traditionally, researchers have relied on subjective self-report techniques such as questionnaires, interviews, and recall diaries (32). Although these techniques are susceptible to researcher and subject bias, the validity of self-report measures was enhanced by the development of the Compendium of Physical Activities (2–3). The Compendium standardizes subjective measurements by assigning MET values for over 600 activities, which allows researchers to compare data across studies (3). However, not all of the activity MET values in the Compendium were empirically derived and if criterion metabolic measurements are available, the studies included a narrow range of activities and small homogenous samples (18).
Due to recall bias associated with subjective techniques, objective measurement of PA has emerged as a valid alternative (11). Recent advances in motion sensor technology and data processing have made accelerometer based physical activity monitors (accelerometers) the device of choice for measuring frequency, duration and intensity of PA (36). Although there is no recall bias associated with objective monitoring, accelerometers have yet to realize their promise to provide accurate estimates of energy expenditure (EE) (26). The most common approach to process accelerometer output is to "calibrate" the device in a laboratory by simultaneously recording accelerometer output (e.g., counts) and some physiological variable (e.g., METs) (12, 14, 34). The relationship between these variables is then determined using regression equations. These equations are used to predict point estimates of EE or to determine duration and intensity of an activity using “cut-points”. The cut-points define the range of accelerometer output corresponding to light, moderate, vigorous and very vigorous intensity (<3 METs, 3–5.99 METs, ≥6 METs, ≥9 METs, respectively). However, there are over 30 published prediction techniques to estimate EE from accelerometer output that often produce widely different estimates of EE (12, 31). Differences in these EE estimates are partially a result of current data processing techniques used to translate accelerometer output into METs. The most commonly used technique, the linear regression model, was developed based on the premise EE increases linearly with vertical acceleration in locomotion activities (14). Researchers have suggested this method may be inappropriate for non-locomotive activities, such as activities of daily living in a free-living environment (26). However, linear regression models are still commonly used (36) and more research is needed to understand the magnitude and source of error when linear processing techniques are developed on a diverse sample of activities. In addition, differences in EE estimates from accelerometer output arise from inconsistencies in the calibration process, which make comparing results among studies difficult (13–14, 18). Researchers rarely provide detailed information regarding calibration methods, further contributing to confusion in the literature.
In summary, there is no uniform standard of practice for the calibration of objective measurements, thereby, limiting the comparison of results among studies. Enhanced transparency and emphasis on calibration methodology would make such comparisons possible. In addition, more research is needed to understand the efficacy of a linear regression model to translate accelerometer output into estimates of EE across a range of activities and intensities. Furthermore, it is important to continuously provide empirical data to upgrade the quality of the Compendium by measuring metabolic responses for a range of activities from diverse participant groups. Therefore, the objective of this study is to advance the field of PA measurement by: 1) providing detailed information on the calibration procedures and methods for metabolic and activity monitor data collection in a large, diverse sample, 2) examining the accelerometer output and EE relationship in this large sample spanning several activity types and intensities, 3) comparing the metabolic data collected on a wide range of physical activities to the MET values from the Compendium of Physical Activities, by sex, age and body mass index (BMI) groups.
Methods
Eligibility and Recruitment
Participants were recruited from the University of Massachusetts, Amherst and surrounding areas. Eligible participants were between the ages 20–60 yrs, were not taking medications that altered metabolism, and were free of any musculoskeletal, metabolic, cardiovascular, or pulmonary diseases. No exclusions were placed on fitness level or other health habits. Recruitment was blocked to ensure uniform age and sex distributions among the study sample (approximately 35 males and 35 females in each of the four decades). Complete descriptive characteristics for the sample are reported in Table 1. The total number of participants was 277; 50.2% female and 17% minorities. The average age was (mean ± SD) 38 ± 12.4 years, and average BMI 24.6 ± 4.01 kg·m−2.
Table 1.
Descriptive characteristics [Mean (SD)] for all particpants and by sub-groups.
|
Age (y) |
BMI (m/kg2) |
PAS (0–7 scale) |
Height (cm) |
Body Mass (kg) |
RMR (ml/kg/min) |
|
|---|---|---|---|---|---|---|
|
All Subjects |
38.0 | 24.63 | 5.29 | 170.95 | 72.26 | 3.30 |
| (N=277) | (12.4) | (4.01) | (1.95) | (9.59) | (14.53) | (0.49) |
| Female | 38.3 | 24.22 | 4.93 | 164.34 | 65.45 | 3.21 |
| (n = 139) | (12.1) | (4.28) | (2.10) | (7.17) | (12.56) | (0.46) |
| Male | 37.8 | 25.03 | 5.66 | 177.52 | 79.03 | 3.39 |
| (n = 138) | (12.7) | (3.68) | (1.71) | (6.75) | (13.13) | (0.49) |
| OW | 39.8 | 28.65 | 4.96 | 172.04 | 84.94 | 3.01 |
| (n = 107) | (12.3) | (3.55) | (2.00) | (9.29) | (13.05) | (0.41) |
| NW | 37.0 | 22.25 | 5.49 | 170.31 | 64.77 | 3.47 |
| (n = 170) | (12.4) | (1.70) | (1.89) | (9.71) | (9.18) | (0.45) |
| Young | 27.9 | 23.91 | 5.14 | 171.16 | 70.28 | 3.42 |
| (n = 145) | (6.2) | (3.54) | (2.06) | (9.40) | (12.97) | (0.48) |
| Old | 49.8 | 25.47 | 5.47 | 170.71 | 74.57 | 3.16 |
| (n = 132) | (5.46) | (4.35) | (1.79) | (9.80) | (15.86) | (0.46) |
BMI = body mass index; SD = standard deviation; PAS = physical activity status (a self-report of activity that ranged from 0–7); RMR = resting metabolic rate; OW = overweight defined as a BMI ≥ 25 m/kg2; NW = normal weight (BMI < 25 m/kg2); Young = age 20–39 years; Old = 40–60 years.
Written informed consent approved by the institution human subjects review committee was obtained for all participants. During the consenting visit, blood pressure was measured following five minutes of quiet sitting and volunteers with systolic blood pressure > 140 mmHg and/or diastolic blood pressure > 90 mmHg were excluded. All participants completed a health history questionnaire, a PA readiness questionnaire (35) and a PA status questionnaire during the informed consent visit (30).
Following the consenting visit, males ≥ 40 yrs and females ≥50 yrs completed a graded exercise stress test (to 90% of age predicted maximum heart rate) supervised by a physician. Potential test subjects exhibiting ST segment depression, irregular heart rates during exercise or other signs or symptoms of cardiovascular disease were excluded from participation and were referred to their personal physician for further evaluation. Twenty subjects had a positive stress test and did not complete the study. The maximum heart rate achieved during this screening test was used as an upper heart rate limit during participation in subsequent activities.
Testing Procedure
Participants reported to the exercise physiology laboratory at the University of Massachusetts, Amherst, following a four hour restriction of food, caffeine and exercise. Height was measured to the nearest 0.5cm and weight was measured to the nearest 0.1kg using a floor scale/stadiometer (Detecto; Webb City, MO) while participants wore a thin layer of clothing and no shoes. Participants then rested for 15 minutes in a supine position on a bed in a private section of the climate-controlled laboratory with dim lighting. Participants were instructed to remain still and awake throughout the rest period. Following the rest period, resting metabolic rate (RMR) was measured using the MedGem (Microlife USA, Dunedin, FL), a handheld indirect calorimeter. Participants were supine during the measurement period, which lasted between 5–10 minutes. The protocol used for measurement of RMR is consistent with published recommendations (10). The MedGem calculates oxygen consumption (VO2) based on a modified Weir equation and uses a fixed respiratory exchange ratio of 0.85. Details of the MedGem are published elsewhere (17). The MedGem has been shown to be valid for measuring RMR compared to the gold-standard Douglas bag method (22).
Study Protocol
Participants completed 11 activities for seven minutes each, with a four minute rest period between activities. In order to clearly mark the beginning and end of an activity in the accelerometer data, the subjects were asked to stand completely still for the 30 seconds immediately prior to and immediately following each activity. The protocol was separated into two sections 1) treadmill activities and 2) activities of daily living (ADL’s). The order of the protocol sections was randomized across subjects (e.g. the first subject completed the treadmill then ADLs, the second completed ADL’s the treadmill etc.). Participants were given a 10–15 minute break between sections and the metabolic unit was re-calibrated in this time.
1. Treadmill
All participants completed the same six treadmill activities at three speeds (1.34, 1.56, 2.23 m·sec−1) each at 0% and 3% grade. The order of treadmill conditions was balanced across participants. An activity was discontinued or not attempted if heart rate exceeded the peak heart rate achieved during the graded exercise test (for older subjects) or if the participant could not safely complete the activity. Prior to data collection, the treadmill was calibrated for each individual, at all speeds, using a tachometer (Checkline, Cedarhurst, NY). If the treadmill speed was not within 0.01 mph of the assigned speed, the treadmill was adjusted.
2. Activities of Daily Living
All participants completed a total of five self-paced ADL’s. Three activities were completed by all participants: ascending the stairs, descending the stairs, and moving a box. The remaining two ADL’s were selected from a list of 14 activities based on a blocked randomized design by sex and age groups. These activities are listed below and covered a broad range of behaviors in the sport, leisure, recreation, occupation, and household domains and are based on the study by Bassett et al. (5). Participants were instructed to complete an activity “as they would in their own home” activity to ensure individual variability.
Ascend the stairs: Participants began in the basement of a 16 story building and were instructed to walk up the stairs as they would in everyday life, including the use of a handrail if they typically used one. They were instructed to continue walking until any one of the following termination criteria were met: 1) Seven minutes elapsed, 2) they reached the top of the building,3) volitional fatigue, or 4) heart rate exceeded the physician set limit based on stress test screening for older participants.
Descend the stairs: Participants began at the top of the 16 story building and were given the same instructions and termination criteria as ascending the stairs.
Moving the Box: Participants moved a 6 kg box back and forth from 0.84 m high shelf to a designated spot on the floor 8 m away.
Basketball: A series of poly-spot targets were distributed around a basketball net in a gymnasium. Participants were instructed to start by shooting from one of the poly-spot targets and then continue to dribble between and shoot from any of the targets. If they made the basket, they picked up the target and dribbled the ball to half court, placed the target at half-court and dribbled back to another target.
Tennis: Participants were given a standard racquet and a package of tennis balls. A court was outlined on the gymnasium floor and participants were instructed to continue to rally against the wall as if playing with a partner.
Gardening: Participants were given a shovel and trowel and instructed to plant ten artificial plants in an 11.5 m2 dirt patch.
Mowing: Participants mowed a 152 m2 lawn using a standard electric lawn mower.
Raking: Participants raked a152 m2 lawn outdoors.
Trimming: Participants used an electric trimmer to trim the grass surrounding the building and trees in the area.
Dishes: Participants were instructed to wash and dry a set of dishes in a sink. A variety of rags and scrub brushes were available for use.
Dusting: Participants were given a dusting cloth and instructed to dust small objects on a table, a bookshelf, and a television stand within the laboratory.
Laundry: A large box of clothes was placed on a table and participants were instructed to fold and then place clothes in a box. If the item was something they would typically hang in a closet, they were to hang the item and place it on a rack approximately 1 m away.
Mopping: Participants were instructed to mop a 4.8 m×1.1 m tile floor with a bucket filled with water and cleaning solution and a standard sponge mop.
Organizing the room: a series of objects were scattered around the room (approximately 9 m2) including children’s toys, books, DVD’s, bottles, sporting equipment. Participants were instructed to pick up items as if cleaning up at home.
Painting: Participants were given a roller and paint in a tray. They were instructed to paint two wooden boards (1.3×2.4 m2 each).
Sweeping: Participants were given a broom, dustpan, and a trash bin and instructed to sweep a 4.8 m×1.1 m tile floor.
Vacuuming: Small papers were placed around the exercise physiology laboratory and participants were instructed to vacuum a carpeted room (approximately 9 m2)
Instrumentation
Portable metabolic system: Oxygen consumption during activities was measured using a portable metabolic system (Oxycon mobile, Cardinal Health, Yorba Linda, CA). This device is a battery-operated, portable and wireless unit that measures breath-by-breath gas exchange. It was secured to the body using a vest similar to a backpack and weighs 950 grams (23). A face mask (Hans Rudolf, Inc., Kansas City, MO) was connected to the flow sensor unit and detected the air flow by the rotation of a low-resistance, bidirectional turbine to measure ventilation. The expired air was analyzed for O2 and CO2 concentrations using a microfuel O2 sensor and a thermal conductivity CO2 sensor. Immediately prior to data collection, a two-point (0.2 and 2.0 L·s−1) air flow calibration was performed using the automatic flow calibrator, and the gas analyzers were calibrated using a certified gas mixture of 16 % O2, 4.01% CO2 and a measurement delay time was determined (18). This metabolic measurement system has been shown to be a valid device to measure VO2 (24, 28). Across the range of approximately 1.0 to 5.0 L·min−1 the mean difference between the Oxycon Mobile and Douglas Bag measures of VO2 ranged from 0.00 to 0.07 L·min−1 (28). These differences are comparable with other portable measurement systems (4).
Accelerometer
The ActiGraph GT1M (ActiGraph, Pensacola, FL) is a small (3.8×3.7×1.8 cm) lightweight (27grams) uniaxial accelerometer. Detailed specifications of the monitor are published elsewhere (1). Each participant wore an ActiGraph GT1M initialized to collect data in 1 second epochs and was placed on the anterior superior iliac spine along the anterior axillary line on the non-dominant hip.
Heart rate
A polar heart rate monitor (S610i, Polar USA) was worn around the chest at the level of the xyphoid process. Heart rate was recorded every five seconds. The polar watch was synchronized with the accelerometer using the same lap top computer prior to each testing session. The polar watch time was then used to synchronize the metabolic data to the accelerometer data.
Data Cleaning and Analysis procedures
A total of 277 participants were asked to complete 11 activities each (3047 activities). After data cleaning and elimination of invalid and incomplete activities, the data set consisted of 2745 activities. The reasons for invalid data and the methods for determining the VO2 and accelerometer count value for each activity are described below.
One hundred and twenty-seven activities were not attempted due to participants’ discomfort with the treadmill speed, or if heart rate exceeded the prescribed maximum on a previous, less intense activity (e.g. if heart rate >90% max at 2.23 m·s−1 at 0% grade, the same speed at 3% grade was not attempted). In total, an average of ten activities was completed by each participant, resulting in a total of 2920 activities.
Oxygen consumption
In order to be included in the analysis, an activity needed to be performed for at least 160 seconds. The first two minutes (to allow for steady state to be attained) and the last ten seconds were eliminated, with a minimum of 30 seconds of data for the activity included in the analysis. Ninety-five activities were eliminated because the subject stopped the activity due to volitional fatigue or if heart rate exceeded the exercise test peak before 160 seconds of data were collected. After elimination of incomplete activities, the data set consisted of 2825 activities. An additional 50 activities were eliminated due to technical problems with the metabolic measurement system including sample tube occlusion and mouthpiece malfunction. After cleaning the VO2 data, the data set consisted of 2775 activities.
The MET value for the activity was defined as the steady-state VO2. For an activity that was performed for seven minutes, VO2 for minutes two through six minutes and 50 seconds were averaged to represent the activity oxygen cost. For comparison with the Compendium of Physical Activities, the VO2 was converted into METs. Due to recent evidence suggesting the standard 3.5 ml·kg−1·min−1 does not represent the RMR of the general population (9, 19), we present the oxygen cost of activities in two formats: The standard MET (measured VO2/ 3.5 ml·kg−1·min−1) and measured MET (measured VO2/measured RMR).
Accelerometers
The accelerometer data were recorded for all activities. Thirty activities (1.1%) were eliminated due to errors in data collection leaving a sample of 2745 activities with valid monitor data. Errors in initialization and device malfunction were the most common sources of monitor data error. The accelerometer output in counts per minute for each activity was determined by first multiplying the count per second by sixty to get (counts·min−1) and then averaging the counts per minute to obtain one counts·min−1 value for each activity. This method for establishing counts·min−1 ensured the activity monitor and metabolic measurements were synchronized for each second of data collection. For example, if an activity was completed for 5 minutes by the participant, the minute 2 through four minutes and 50 seconds time period was defined the metabolic and accelerometer output time period for that activity.
Statistical Analysis
For each activity, the average MET value measured in the laboratory was compared to the corresponding value in the Compendium of Physical Activities. To select the Compendium codes to be included in our comparison, two researchers reviewed the Compendium to select the description that best matched the activities in the present study. If there were discrepancies, they were discussed with all the authors until a consensus was reached. Two activities completed in the present investigation were not found in the Compendium: walking 1.34 m·s−1 at 3% grade and running 2.23 m·s−1 at 3% grade, thus the results are presented for the 21 activities with direct comparisons. Table 2 presents the activities with the Compendium code that was used and the corresponding MET value. If the Compendium value did not fall within the 95% confidence interval of the measured MET value, the value was considered significantly different from the measured value (α=0.05). Additional analyses were performed for sex, BMI, and age groups. The counts·min−1 and MET relationship was determined using the line of best fit (linear regression model). All statistical analyses were done using the computer language and statistics package R (http://www.R-project.org) (27).
Table 2.
Compendium code and MET value description used for comparison to the study activities
| Compendium | ||||
|---|---|---|---|---|
| Study Activity | MET value |
Code | Heading | Description |
| Ascend stairs | 5 | 17026 | walking | Carrying 1–15lb load upstairs |
| Shooting baskets | 4.5 | 15050 | sports | Basketball, non-game, general |
| Box | 4 | 11800 | occupation | walking, 3.0 mph, moderately and carrying light objects less than 25 lbs |
| Descending stairs | 3 | 17070 | walking | downstairs |
| Washing dishes | 2.3 | 05041 | home activities | wash dishes - standing or in general (not broken into stand/walk components |
| Dusting | 2.5 | 05040 | home activities | cleaning, light (dusting, straightening up, changing linen, carrying out trash |
| Gardening | 4.5 | 08140 | lawn and garden | planting seedlings, shrubs |
| 2.23 m/s, 3% grade | NA | NA | NA | NA |
| 1.56 m/s, 3% grade | 6.0 | 17210 | walking | walking, 3.5 mph, uphill |
| 1.34 m/s, 3% grade | NA | NA | NA | NA |
| Folding laundry | 2 | 05090 | home activities | implied standing - laundry, fold or hang clothes, put clothes in washer or dryer, packing suitcase |
| 2.23 m/s, 0% grade | 8 | 17231 | walking | walking, 5.0 mph |
| 1.56m/s, 0% grade | 3.8 | 17200 | walking | walking, 3.5 mph, level, brisk, firm surface, walking for exercise |
| 1.34 m/s, 0% grade | 3.3 | 17190 | walking | walking, 3.0 mph, level, moderate pace, firm surface |
| Mopping | 3.5 | 05021 | home activities | mopping |
| Mowing | 5.5 | 08095 | lawn and garden | mowing lawn, general |
| Painting | 4.5 | 06165 | home repair | painting, |
| Raking | 4 | 08165 | lawn and garden | raking lawn |
| Organizing a room | 3 | 05147 | home activities | implied walking - putting away household items - moderate effort |
| Sweeping | 3.3 | 05010 | home activities | carpet sweeping, sweeping floors |
| Tennis | 7 | 15675 | sports | tennis, general |
| Trimming lawn | 3.5 | 08215 | lawn and garden | trimming shrubs or trees, power cutter, using leaf blower, edger |
| Vacuuming | 3.5 | 05043 | home activities | vacuuming |
Results
The measured METs and standard METs are presented in Tables 3 and 4, respectively. For the total sample, the measured METs for four activities (mowing, vacuuming, sweeping and trimming) were not significantly different than the Compendium values. The Compendium values were significantly higher than the measured MET for three activities and the measured MET values were higher than the Compendium for 14 activities. A summary of the significant differences in measured MET values within each sub-group compared to the Compendium values are in Table 5. Across all sub-groups, ascending the stairs, playing basketball, tennis, cleaning a room, moving a box, and the level treadmill speeds were significantly different than the Compendium values. There were no clear differences in the accuracy of the Compendium values among sub-groups. The differences between measured and Compendium METs were greater for higher intensity activities. For example, the measured MET value for ascending the stairs was 5.3 METs higher than the Compendium MET value. For other activities the differences ranged from 0.2 METs to 2.8 METs.
Table 3.
Measured MET values for study activities compared to the MET values from the Compendium of Physical Activities
| Measured METs |
Compendium MET value |
||||
|---|---|---|---|---|---|
| N | Mean | SD | 95% CI | ||
| Ascend stairs | 215 | 10.3* | 1.89 | 10.00, 10.51 | 5 |
| Shooting baskets | 39 | 9.3* | 1.96 | 8.70, 9.93 | 4.5 |
| Moving a box | 271 | 5.0* | 1.05 | 4.88, 5.13 | 4 |
| Descending stairs | 231 | 4.4* | 1.03 | 4.28, 4.54 | 3 |
| Washing dishes | 42 | 2.1 | 0.40 | 2.01, 2.26 | 2.3 |
| Dusting | 39 | 2.8* | 0.66 | 2.62, 3.04 | 2.5 |
| Gardening | 38 | 4.0* | 1.25 | 3.59, 4.39 | 4.5 |
| 2.23 m/s, 3% grade | 189 | 10.4 | 1.49 | 10.14, 10.56 | N/A |
| 1.56 m/s, 3% grade | 266 | 6.2* | 0.94 | 6.07, 6.29 | 6 |
| 1.34 m/s, 3% grade | 268 | 5.2 | 0.79 | 5.11, 5.30 | N/A |
| Folding laundry | 39 | 2.4* | 0.30 | 2.32, 2.51 | 2 |
| 2.23 m/s, 0% grade | 227 | 9.2* | 1.36 | 9.03, 9.38 | 8 |
| 1.56 m/s, 0% grade | 267 | 5.0* | 0.83 | 4.92, 5.12 | 3.8 |
| 1.34 m/s, 0% grade | 270 | 4.2* | 0.69 | 4.13, 4.30 | 3.3 |
| Mopping | 38 | 3.9* | 0.77 | 3.67, 4.16 | 3.5 |
| Mowing | 37 | 5.9 | 1.36 | 5.42, 6.29 | 5.5 |
| Painting | 38 | 3.3* | 0.85 | 3.03, 3.58 | 4.5 |
| Raking | 39 | 4.7* | 1.35 | 4.26, 5.11 | 4 |
| Organizing a room | 37 | 5.2* | 1.11 | 4.87, 5.58 | 3 |
| Sweeping | 40 | 3.4 | 0.71 | 3.17, 3.61 | 3.3 |
| Tennis | 39 | 9.5* | 1.61 | 9.04, 10.06 | 7 |
| Trimming lawn | 38 | 3.6 | 0.78 | 3.34, 3.83 | 3.5 |
| Vacuuming | 38 | 3.5 | 0.66 | 3.28, 3.70 | 3.5 |
Measured METs (measured VO2/measured resting metabolic rate).
If the Compendium MET value is outside the 95 % Confidence interval (CI) for the measured MET the values are considered statistically different at α = 0.05, indicated with *
N= number of participants that completed that activity.
Table 4.
Standard MET values for study activities compared to the MET values from the Compendium of Physical Activities
| Standard METs | Compendium MET value |
||||
|---|---|---|---|---|---|
| N | Mean | SD | 95% CI | ||
| Ascending stairs | 215 | 9.6* | 1.85 | 9.34, 9.83 | 5 |
| Basketball | 39 | 8.3* | 2.32 | 7.61, 9.07 | 4.5 |
| Moving a box | 271 | 4.5* | 0.93 | 4.42, 4.64 | 4 |
| Descending stairs | 231 | 4.0* | 0.85 | 3.87, 4.09 | 3 |
| Washing dishes | 42 | 1.9* | 0.36 | 1.77, 1.98 | 2.3 |
| Dusting | 39 | 2.6 | 0.50 | 2.41, 2.73 | 2.5 |
| Gardening | 38 | 3.6* | 1.09 | 3.29, 3.98 | 4.5 |
| 2.23 m/s, 3% grade | 189 | 9.7 | 0.97 | 9.61, 9.88 | NA |
| 1.56m/s, 3% grade | 266 | 5.6* | 0.58 | 5.51, 5.65 | 6 |
| 1.34 m/s, 3% grade | 268 | 4.7 | 0.51 | 4.64, 4.76 | NA |
| Folding laundry | 39 | 2.3* | 0.36 | 2.16, 2.39 | 2 |
| 2.23 m/s, 0% grade | 227 | 8.5* | 0.94 | 8.35, 8.60 | 8 |
| 1.56m/s, 0% grade | 267 | 4.5* | 0.55 | 4.46, 4.59 | 3.8 |
| 1.34 m/s, 0% grade | 270 | 3.8* | 0.46 | 3.75, 3.86 | 3.3 |
| Mopping | 38 | 3.5 | 0.76 | 3.29, 3.77 | 3.5 |
| Mowing | 37 | 5.3 | 1.02 | 5.00, 5.66 | 5.5 |
| Painting | 38 | 3.0* | 0.91 | 2.74, 3.32 | 4.5 |
| Raking | 39 | 4.1 | 1.08 | 3.76, 4.43 | 4 |
| Organizing a room | 37 | 4.8* | 1.10 | 4.44, 5.15 | 3 |
| Sweeping | 40 | 3.1 | 0.62 | 2.92, 3.31 | 3.3 |
| Tennis | 39 | 9.0* | 1.82 | 8.39, 9.54 | 7 |
| Trimming lawn | 38 | 3.2* | 0.63 | 2.96, 3.36 | 3.5 |
| Vacuuming | 38 | 3.3* | 0.58 | 3.07, 3.43 | 3.5 |
Standard MET (measured VO2/3.5 ml·kg−1·min−1)
If the Compendium MET value is outside the 95 % Confidence interval for the standard MET the values are considered statistically different at α = 0.05, indicated with *
N= number of participants that completed that activity.
Table 5.
Summary of differences between standard METs and Compendium METs and measured METs and Compendium METs by sub-group
| a. | Not significantly different | Compendium is higher | Standard MET is higher |
|---|---|---|---|
|
All subjects |
5 | 6 | 10 |
| Female | 6 | 6 | 9 |
| Male | 6 | 5 | 10 |
| OW | 4 | 8 | 9 |
| NW | 6 | 4 | 11 |
| Young | 6 | 5 | 10 |
| Old | 5 | 6 | 10 |
| b. | Not significantly different | Compendium is higher | Measured MET is higher |
|
All subjects |
4 | 3 | 14 |
| Female | 6 | 2 | 13 |
| Male | 8 | 2 | 11 |
| OW | 9 | 1 | 11 |
| NW | 5 | 3 | 13 |
| Young | 7 | 3 | 11 |
| Old | 6 | 1 | 14 |
OW = overweight defined as a body mass index BMI ≥ 25 m/kg2; NW = normal weight (BMI < 25 m/kg2); Young = age 20–39 years, Old = 40–60 years;
Standard MET (measured VO2/3.5 ml·kg−1·min−1);
Measured MET (measured VO2/resting metabolic rate).
The MET value is considered significantly different if the Compendium MET value is outside the 95% Confidence Intervals.
For the total sample using standard METs (3.5ml·kg−1·min−1) as the RMR, the MET values for five activities were not significantly different than the Compendium MET values (sweeping, dusting, mopping, mowing, and raking). The Compendium MET values were higher than the standard METs for six activities and the standard MET values were higher than the Compendium MET values for ten activities. Similar to measured METs, the greatest difference was for ascending the stairs (4.6 METs) and other differences ranged from 0.2 METs to 3.8 METs. A summary of the significant differences within each sub-group in standard MET values compared to the Compendium is presented in Table 5. There were no clear differences in the accuracy of the Compendium among the sub-groups.
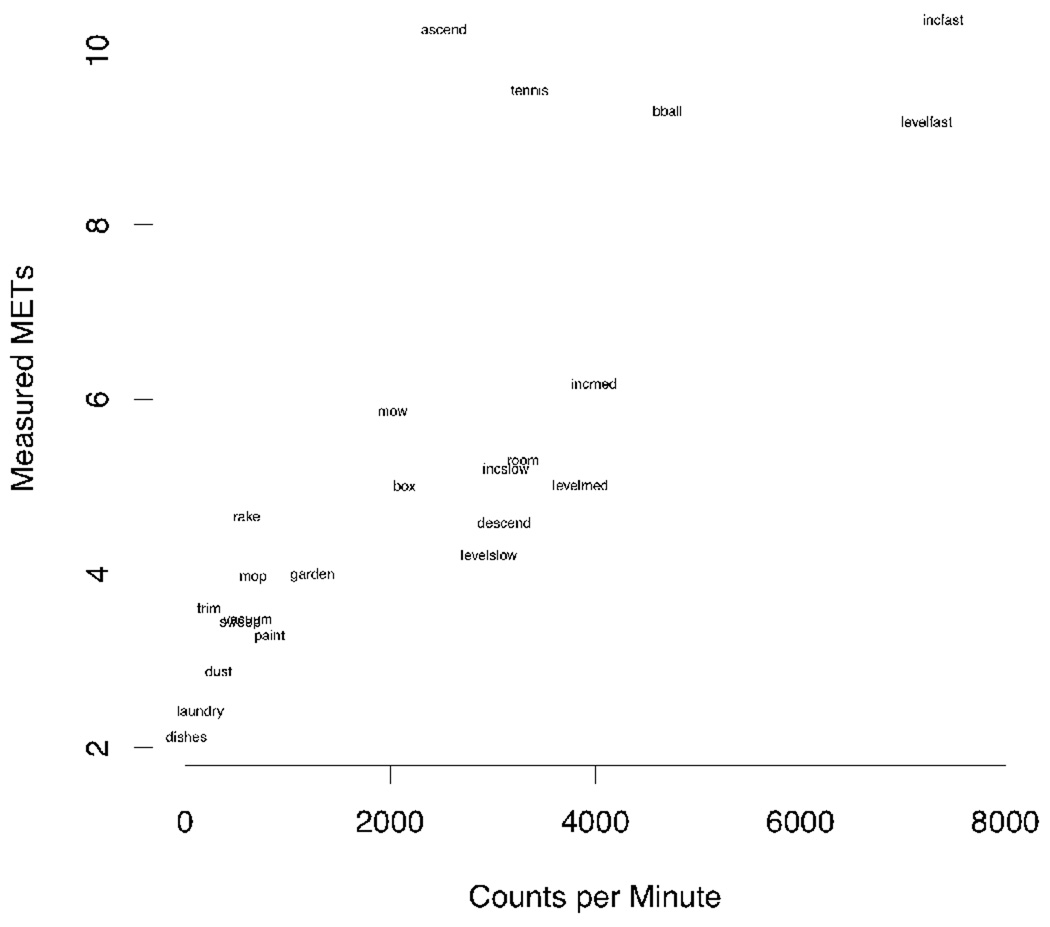
The average accelerometer output for each activity is shown in Table 6. Average accelerometer output ranged from 11 counts·min−1 (washing dishes) to 7490 counts·min−1 (2.23 m·s−1 at 3% grade). The relationship between average count and measured MET values for each activity is presented in Figure 1. The r2 value for a line of best fit is 0.65.
Table 6.
Mean and standard deviation (SD) for accelerometer output (cnts˙min−1) for each activity
| Activity | N | Mean | SD |
|---|---|---|---|
| Ascending stairs | 215 | 2770 | 819 |
| Basketball | 39 | 4703 | 1675 |
| Moving a box | 271 | 2156 | 571 |
| Descending stairs | 231 | 3157 | 892 |
| Washing dishes | 42 | 11 | 28 |
| Dusting | 39 | 360 | 257 |
| Gardening | 38 | 1243 | 745 |
| 2.23 m/s, 3% grade | 189 | 7490 | 1787 |
| 1.56 m/s, 3% grade | 266 | 3998 | 826 |
| 1.34 m/s, 3% grade | 268 | 3137 | 657 |
| Folding laundry | 39 | 148 | 170 |
| 2.23 m/s, 0% grade | 227 | 7411 | 1822 |
| 1.56 m/s, 0% grade | 267 | 3866 | 817 |
| 1.34 m/s, 0% grade | 270 | 2970 | 573 |
| Mopping | 38 | 680 | 576 |
| Mowing | 37 | 2050 | 723 |
| Painting | 38 | 838 | 870 |
| Raking | 39 | 615 | 490 |
| Organizing a room | 37 | 3384 | 1255 |
| Sweeping | 40 | 575 | 461 |
| Tennis | 39 | 3343 | 1022 |
| Trimming lawn | 38 | 268 | 270 |
| Vacuuming | 38 | 613 | 325 |
Note: N is number of participants who completed the activity.
Figure 1.
Relationship between average accelerometer output (counts·min−1) and measured METs for each activity
Note: Measured METs: measured oxygen consumption/ measured resting metabolic rate.
Discussion
This study provides a framework for researchers to design future activity monitor calibration studies by providing detailed procedures and methods for metabolic and activity monitor data collection on a large and diverse population. Previously, PA measurement research lacked uniform standards of practice for studies designed to evaluate objective monitors and metabolic responses. Thus, these procedures for calibration of activity monitors will facilitate comparisons across studies and improve the transparency in the PA measurement literature.
A description of the accelerometer output across the range of activities was provided, however counts·min−1 has little practical meaning for PA researchers. Therefore, we examined the relationship between accelerometer output (counts·min−1) and METs to examine the efficacy of a linear prediction model developed on a diverse set of activities. We found that a linear regression model to predict METs from accelerometer output accounted for 65% of the variability in our sample, which is considered a moderate to high association. However, Figure 1 clearly illustrates three intrinsic errors when a linear regression model is used to estimate METs based on accelerometer output. Specifically, the first error is that linear regression model cannot accurately predict MET values for activities that require upper body effort (such as carrying a load). For example, the MET value for moving a box is 0.8 METs higher than walking 1.34 m·s−1 however, the accelerometer output is 800 counts·min−1 lower for moving the box. Secondly, the linear regression model cannot distinguish walking on a grade from walking on level ground. Specifically, the mean accelerometer output for level walking at 1.56 m·s−1 is 3886 counts·min−1 and the average MET value is 5.0 METs, which is moderate intensity. Walking 1.56 m·s−1 with a 3% grade is only 133 counts·min−1 greater than walking without the grade; however the MET value is 6.2, which is vigorous intensity. Third, the linear regression model does not accurately predict the MET values for ascending stairs or other intermittent high intensity activities. For example, the mean measured METS for walking up stairs was 10.3, which is considered very vigorous activity. However, based on the accelerometer value of 2770 counts·min−1 for ascending the stairs, the Freedson MET equation would predict 3.6 METs, which is moderate intensity (14). These errors are evident when accelerometers are used to assess free-living PA behavior. A recent review comparing accelerometer predicted of EE to doubly labeled water found the ActiGraph to be valid however, the r2 values ranged from 0.1 to 0.6 (25). The large range of error is likely due to differences between the activities used in calibration and the activities the participants perform in their free-living environment and in the techniques used to calibrate monitors.
In order for accelerometers to achieve their potential for accurate prediction of free-living EE, new methods for processing accelerometer output are needed. For example, Pober et al. showed that free-living activities with the same MET value can have different average count values (e.g. walking and vacuuming), while other features of the acceleration signal are different between activities (26). Our lab and others have recently explored sophisticated techniques including artificial neural networking and Hidden Markov Modeling, which use multiple features of the acceleration signal rather than average monitor output (e.g. counts·min−1) over time (6–7, 26, 33) . These methods improve MET estimates compared to simple regression, however more data are needed to “train” and refine the models to accurately predict METs across a range of participants and activities (33).
This study also provides researchers the average and range of MET values for a variety of common physical activities. In addition, we compared our measured MET values to the MET values from the Compendium of Physical Activities. We report that measured METs in our diverse sample were significantly different from Compendium METs for 17/21 activities (81%). The number of activities that were not different than the Compendium was similar if measured RMR or the standard 3.5 ml·kg·min−1 was used to determine METs. Some of the significant differences between the Compendium METs and the measured METs were small. For example, the measured METs for gardening, dusting, 1.56 m·s−1, folding laundry and mopping were all different than the Compendium MET value, but the difference was less than 0.5 METs. However, there were a number of other activities that had > 1 MET absolute differences, which could result in significant errors when the Compendium MET values are used to estimate total daily PA. Although the large number of activities that were different than the Compendium may be surprising, our results are consistent with Bassett et al, who found 15 of 25 measured MET values (60%) were significantly different than the Compendium value in a smaller, more homogenous sample (5). The majority of the MET values in this study were higher than the Compendium values. One possible explanation for these differences is that subjects were not in steady-state. To investigate this, we compared the mean METs in the third minute to the mean METs in the last minute for each activity. For two activities (gardening and hedge trimming), METs decreased about 8% (about 0.3 METs). For the rest of the activities, the differences were all less than 5%. Therefore, the differences in MET values were not a result of a drift in MET values throughout the seven minutes. It is unrealistic to expect all individuals will perform self-paced activity at a constant work rate and thus some MET differences are expected.
It is important that changes to the Compendium be considered for those activities where the reported MET values are substantially different from measured MET values. The Compendium is an invaluable research tool, but should be updated with additional empirical data and perhaps more specific activities (e.g., moving a 6 kg box). When measured RMR was used, over 60% of Compendium MET values were lower than the measured MET values. Thus, to avoid underestimating the energy cost of activities, additional changes to the Compendium should include a correction for differences in measured RMR compared to the standard 3.5 ml·kg·min−1 (19) or the Compendium should be revised to include measured METs.
Although our data suggest that revisions should be made to the Compendium of Physical Activities, it is important to point out that the observed errors were not differentially distributed across sub-groups. These results support the use of one Compendium of Physical Activities for all adults age 20–60 yrs regardless of sex or BMI. A Compendium for children has been published recently (29) and additional empirical data should be collected in participants > 60 yrs to ensure self-report data are based on accurate estimations of EE in this population.
There are some study limitations to be noted. All activities were performed in the laboratory and not in a natural environment, which may have altered how the participant completed the activity. To minimize this effect, participants were instructed to perform the activity as they would in a free-living environment and given minimal additional instruction. Additionally, previous research suggests that the MET values of activities performed in the lab and at home are similar (8, 15–16, 37). A second limitation is that the sample is a convenience sample and it is likely our study sample was healthier than the general population. Inclusion criteria included being free of disorders that impair mobility or medication that affect metabolism; thus our results cannot be generalized to clinical populations. On average, participants reported a five on a self report PA scale that ranged from zero to seven, which is equivalent to running one to five miles per week or spending 30–60 minutes in similar physical activities. Although this amount of PA is less than the current PA guidelines (24), it is still higher than the general population (36). In addition, while our total sample varied in age and BMI, some individuals could not complete all the activities, such as jogging and ascending 16 flights of stairs. Thus, the MET values for those specific activities may only be generalizable to a more active population. Finally, RMR was measured using the MedGem, which is not a gold-standard measurement tool for RMR. However, a review comparing the MedGem to criterion measures concluded the device was valid, with an average difference between MedGem and Douglas bag in adults of less than 1% and the intra-class reliability coefficient was r = 0.98 (20–21). In addition, the MedGem self-calibrates, is inexpensive and easy to use compared to the Douglas Bag, thus reducing the burden on participants who completed a lengthy protocol.
This study has a number of important strengths. The study sample was very large for this type of investigation and included a wide age range of participants. An equal number of men and women and a representative sample of ethnic minorities were recruited (17%). Although our sample was more active than the general population (36), we attempted to recruit a wide range of fitness levels and were successful in recruiting a wide range of BMI’s (17.6 to 42.4 kg·m−2) and a range of PA levels. In addition to the diverse study sample, the participants completed a broad range of activities including common household, sporting and locomotion activities.
This study provides valuable information about the specific details of data collection, metabolic responses, and accelerometer output for common physical activities that were completed by a diverse participant sample. Due to the considerable variation between measured MET values and the corresponding MET values reported in the Compendium of Physical Activities, these data should be used to update the Compendium. Our results support that the Compendium is valid for a wide age range (20–60y) and that average MET values are similar across sex and BMI groups. Finally, we showed a linear regression model is an inappropriate approach when using accelerometer output (counts·min−1) to predict corresponding MET values in a range of activities. Future research should consider non-linear and advanced processing methods to accurately predict EE from accelerometer output.
Acknowledgements
Funded by NIH RO1 CA121005
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Our appreciation is extended to all the participants who volunteered and the graduate and undergraduate students who assisted with data collection.
The results of the present study do not constitute endorsement by ACSM.
References
- 1.ActiGraph. Actisoft Analysis Software 3.2 User's Manual. Fort Walton Beach, FL: MTI Health Services; 2005. p. 17. [Google Scholar]
- 2.Ainsworth BE, Haskell WL, Leon AS, Jacobs DR, Jr, Montoye HJ, Sallis JF, Paffenbarger RS., Jr Compendium of physical activities: classification of energy costs of human physical activities. Medicine and science in sports and exercise. 1993;25(1):71–80. doi: 10.1249/00005768-199301000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, O'Brien WL, Bassett DR, Jr, Schmitz KH, Emplaincourt PO, Jacobs DR, Jr, Leon AS. Compendium of physical activities: an update of activity codes and MET intensities. Medicine and science in sports and exercise. 2000;32 9 Suppl:S498–S504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 4.Atkinson G, Davison RC, Nevill AM. Performance characteristics of gas analysis systems: what we know and what we need to know. International journal of sports medicine. 2005;26 Suppl 1:S2–S10. doi: 10.1055/s-2004-830505. [DOI] [PubMed] [Google Scholar]
- 5.Bassett DR, Jr, Ainsworth BE, Swartz AM, Strath SJ, O'Brien WL, King GA. Validity of four motion sensors in measuring moderate intensity physical activity. Med Sci Sports Exerc. 2000;32 9 Suppl:S471–S480. doi: 10.1097/00005768-200009001-00006. [DOI] [PubMed] [Google Scholar]
- 6.Bonomi AG, Goris AH, Yin B, Westerterp KR. Detection of type, duration, and intensity of physical activity using an accelerometer. Medicine and science in sports and exercise. 2009;41(9):1770–1777. doi: 10.1249/MSS.0b013e3181a24536. [DOI] [PubMed] [Google Scholar]
- 7.Bonomi AG, Plasqui G, Goris AH, Westerterp KR. Improving assessment of daily energy expenditure by identifying types of physical activity with a single accelerometer. J Appl Physiol. 2009;107(3):655–661. doi: 10.1152/japplphysiol.00150.2009. [DOI] [PubMed] [Google Scholar]
- 8.Brooks AG, Withers RT, Gore CJ, Vogler AJ, Plummer J, Cormack J. Measurement and prediction of METs during household activities in 35- to 45-year-old females. Eur J Appl Physiol. 2004;91(5–6):638–648. doi: 10.1007/s00421-003-1018-9. [DOI] [PubMed] [Google Scholar]
- 9.Byrne NM, Hills AP, Hunter GR, Weinsier RL, Schutz Y. Metabolic equivalent: one size does not fit all. J Appl Physiol. 2005;99(3):1112–1119. doi: 10.1152/japplphysiol.00023.2004. [DOI] [PubMed] [Google Scholar]
- 10.Compher C, Frankenfield D, Keim N, Roth-Yousey L. Best practice methods to apply to measurement of resting metabolic rate in adults: a systematic review. J Am Diet Assoc. 2006;106(6):881–903. doi: 10.1016/j.jada.2006.02.009. [DOI] [PubMed] [Google Scholar]
- 11.Corder K, Brage S, Ekelund U. Accelerometers and pedometers: methodology and clinical application. Curr Opin Clin Nutr Metab Care. 2007;10(5):597–603. doi: 10.1097/MCO.0b013e328285d883. [DOI] [PubMed] [Google Scholar]
- 12.Crouter SE, Churilla JR, Bassett DR., Jr Estimating energy expenditure using accelerometers. Eur J Appl Physiol. 2006;98(6):601–612. doi: 10.1007/s00421-006-0307-5. [DOI] [PubMed] [Google Scholar]
- 13.Crouter SE, Clowers KG, Bassett DR., Jr A novel method for using accelerometer data to predict energy expenditure. J Appl Physiol. 2006;100(4):1324–1331. doi: 10.1152/japplphysiol.00818.2005. [DOI] [PubMed] [Google Scholar]
- 14.Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc. 1998;30(5):777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 15.Gunn SM, Brooks AG, Withers RT, Gore CJ, Owen N, Booth ML, Bauman AE. Determining energy expenditure during some household and garden tasks. Med Sci Sports Exerc. 2002;34(5):895–902. doi: 10.1097/00005768-200205000-00026. [DOI] [PubMed] [Google Scholar]
- 16.Gunn SM, Brooks AG, Withers RT, Gore CJ, Plummer JL, Cormack J. The energy cost of household and garden activities in 55- to 65-year-old males. Eur J Appl Physiol. 2005;94(4):476–486. doi: 10.1007/s00421-004-1302-3. [DOI] [PubMed] [Google Scholar]
- 17.MedGem website [Internet] Golden (CO): [cited 2009 Jan1]. Available from: http://www.mimhs.com/watchwt/solutions/medgem/overview/ [Google Scholar]
- 18.Hendelman D, Miller K, Baggett C, Debold E, Freedson P. Validity of accelerometry for the assessment of moderate intensity physical activity in the field. Medicine and science in sports and exercise. 2000;32 9 Suppl:S442–S449. doi: 10.1097/00005768-200009001-00002. [DOI] [PubMed] [Google Scholar]
- 19.Kozey S, Lyden K, Staudenmayer J, Freedson PS. Errors in MET estimates of physical activities using 3.5ml.kg-1.min-1 as the baseline oxygen consumption. J Phys Activ Health. doi: 10.1123/jpah.7.4.508. in press. [DOI] [PubMed] [Google Scholar]
- 20.McDoniel SO. Systematic review on use of a handheld indirect calorimeter to assess energy needs in adults and children. Int J Sport Nutr Exerc Metab. 2007;17(5):491–500. doi: 10.1123/ijsnem.17.5.491. [DOI] [PubMed] [Google Scholar]
- 21.Nieman DC, Austin MD, Chilcote SM, Benezra L. Validation of a new handheld device for measuring resting metabolic rate and oxygen consumption in children. Int J Sport Nutr Exerc Metab. 2005;15(2):186–194. doi: 10.1123/ijsnem.15.2.186. [DOI] [PubMed] [Google Scholar]
- 22.Nieman DC, Trone GA, Austin MD. A new handheld device for measuring resting metabolic rate and oxygen consumption. J Am Diet Assoc. 2003;103(5):588–592. doi: 10.1053/jada.2003.50116. [DOI] [PubMed] [Google Scholar]
- 23.Perret C, Mueller G. Validation of a new portable ergospirometric device (Oxycon Mobile) during exercise. Int J Sports Med. 2006;27(5):363–367. doi: 10.1055/s-2005-865666. [DOI] [PubMed] [Google Scholar]
- 24.Physical Activity Guidelines Advisory Committee report. To the Secretary of Health and Human Services. Part A: executive summary. Nutr Rev. 2009;67(2):114–120. doi: 10.1111/j.1753-4887.2008.00136.x. [DOI] [PubMed] [Google Scholar]
- 25.Plasqui G, Westerterp KR. Physical activity assessment with accelerometers: an evaluation against doubly labeled water. Obesity (Silver Spring, Md. 2007;15(10):2371–2379. doi: 10.1038/oby.2007.281. [DOI] [PubMed] [Google Scholar]
- 26.Pober DM, Staudenmayer J, Raphael C, Freedson PS. Development of novel techniques to classify physical activity mode using accelerometers. Med Sci Sports Exerc. 2006;38(9):1626–1634. doi: 10.1249/01.mss.0000227542.43669.45. [DOI] [PubMed] [Google Scholar]
- 27.R Core Development Team. R Foundation for Statistical Computing version 2.7.2. Vienna, Austria: R: A Language and Environment for Statistical Computing; 2009. Jul 1, [cited 2009 Available from: http://www.R-project.org. [Google Scholar]
- 28.Rosdahl H, Gullstrand L, Salier-Eriksson J, Johansson P, Schantz P. Evaluation of the Oxycon Mobile metabolic system against the Douglas bag method. Eur J Appl Physiol. [Internet] 2009 doi: 10.1007/s00421-009-1326-9. [cited]; Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=20043228. [DOI] [PubMed]
- 29.Ridley K, Ainsworth BE, Olds TS. Development of a compendium of energy expenditures for youth. The International Journal of Behavioral Nutrition and Physical Activity [Internet] 2008 doi: 10.1186/1479-5868-5-45. [cited];5. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=18782458. [DOI] [PMC free article] [PubMed]
- 30.Ross RM, Jackson AS. Exercise Concepts, Calculations, and Computer Applications. Brown and Benchmark publishers; 1990. pp. 95–103. [Google Scholar]
- 31.Rothney MP, Schaefer EV, Neumann MM, Choi L, Chen KY. Validity of physical activity intensity predictions by ActiGraph, Actical, and RT3 accelerometers. Obesity (Silver Spring, Md. 2008;16(8):1946–1952. doi: 10.1038/oby.2008.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sallis JF, Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Research quarterly for exercise and sport. 2000;71 2 Suppl:S1–S14. [PubMed] [Google Scholar]
- 33.Staudenmayer J, Pober D, Crouter SE, Bassett DR, Freedson P. An artificial neural network to estimate physical activity energy expenditure and identify physical activity type from an accelerometer. J Appl Physiol. 2009;107(4):1300–1307. doi: 10.1152/japplphysiol.00465.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Swartz AM, Strath SJ, Bassett DR, Jr, O'Brien WL, King GA, Ainsworth BE. Estimation of energy expenditure using CSA accelerometers at hip and wrist sites. Med Sci Sports Exerc. 2000;32 9 Suppl:S450–s456. doi: 10.1097/00005768-200009001-00003. [DOI] [PubMed] [Google Scholar]
- 35.Thomas S, Reading J, Shephard RJ. Revision of the Physical Activity Readiness Questionnaire (PAR-Q) Can J Sport Sci. 1992;17(4):338–345. [PubMed] [Google Scholar]
- 36.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Medicine and science in sports and exercise. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 37.Withers RT, Brooks AG, Gunn SM, Plummer JL, Gore CJ, Cormack J. Self-selected exercise intensity during household/garden activities and walking in 55 to 65-year-old females. Eur J Appl Physiol. 2006;97(4):494–504. doi: 10.1007/s00421-006-0177-x. [DOI] [PubMed] [Google Scholar]