SUMMARY
Desmoid tumor is a rare, benign fibroblastic tumor that is characterized by highly aggressive local invasiveness.
The authors report the case of a 35 year old male who presented with a 20 cm para-umbilical tumor invading the right rectus abdominis muscle. This required a wide excision of the abdominal wall. The resulting defect was closed with a single-stage latissimus dorsi myocutaneous free flap in combination with a prosthetic mesh reconstruction.
The authors discuss the therapeutic options for management of these rare tumors and the variety of available techniques for coverage and reconstruction after extensive parietal loss of substance.
Keywords: Abdominal wall, Loss of substance, Reconstruction of the abdominal wall, Latissimus dorsi free flap, Desmoid tumor, Fibromatosis
Desmoid tumors are histologically benign but agressive non-encapsulated tumors consisting of well-differentiated fibroblastic cells in a collagen matrix ; they arise from the surface of a fascial or musculo-aponeurotic structure.
CASE REPORT
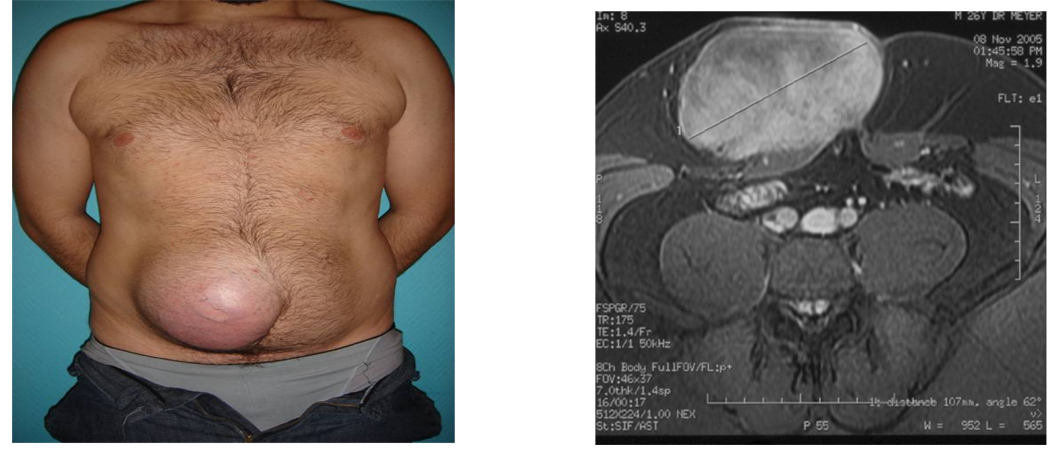
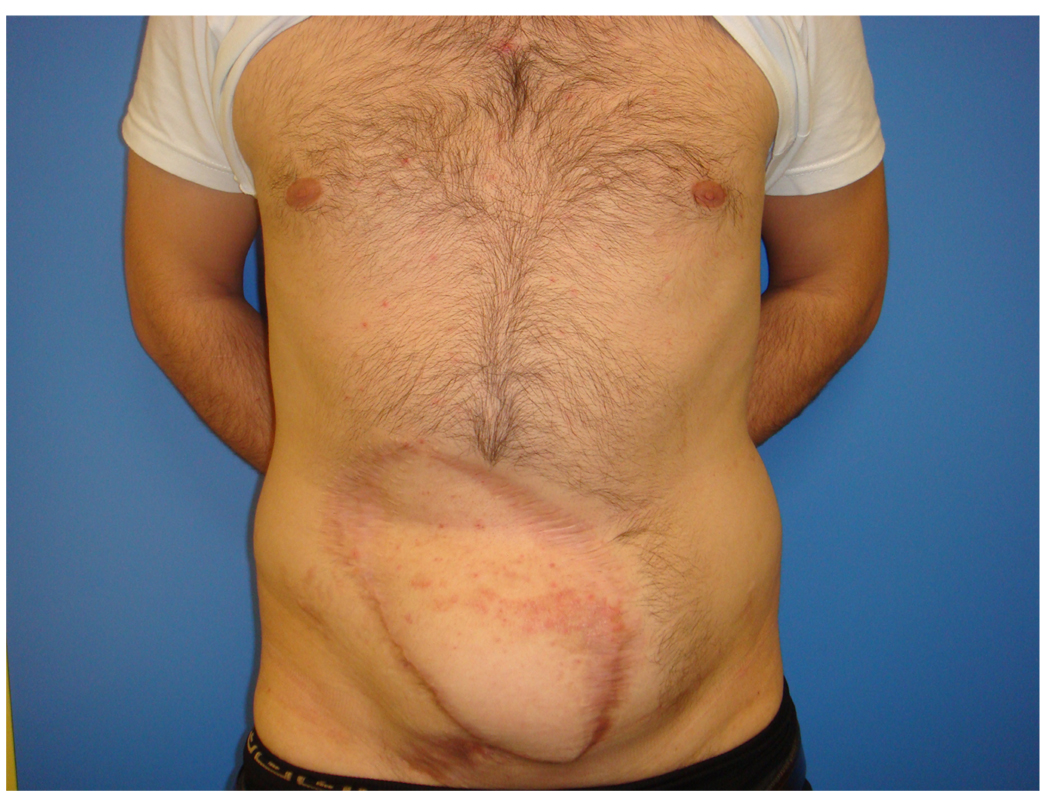
A 35 year old male presented with a 20 cm diameter tumor which was noticed after a recent traumatic episode. Family history was non-contributory. The patient described steady growth of the mass over a four month period. It was located in the right para-umbilical region [fig.1]. There was no palpable lymphadenopathy. The patient had noted no signs of obstruction or problems with intestinal transit.
Figure 1.
Pre-operative appearance : 35 year old male patient with a20 cm. periumbilical mass.
MRI showing infiltration of the rectus aponeurosis
Fine-needle aspiration cytology revealed fusiform cells suggestive of two possible diagnoses, sarcoma or desmoid tumor. Ultrasound showed the tumor to be heterogeneous and hypervascular on doppler exam. MRI was a critical study for the pre-operative assessment of tumor extension ; it showed invasion of the right rectus muscle and anterior rectus sheath including the linea alba and extending to the left anterior rectus sheath
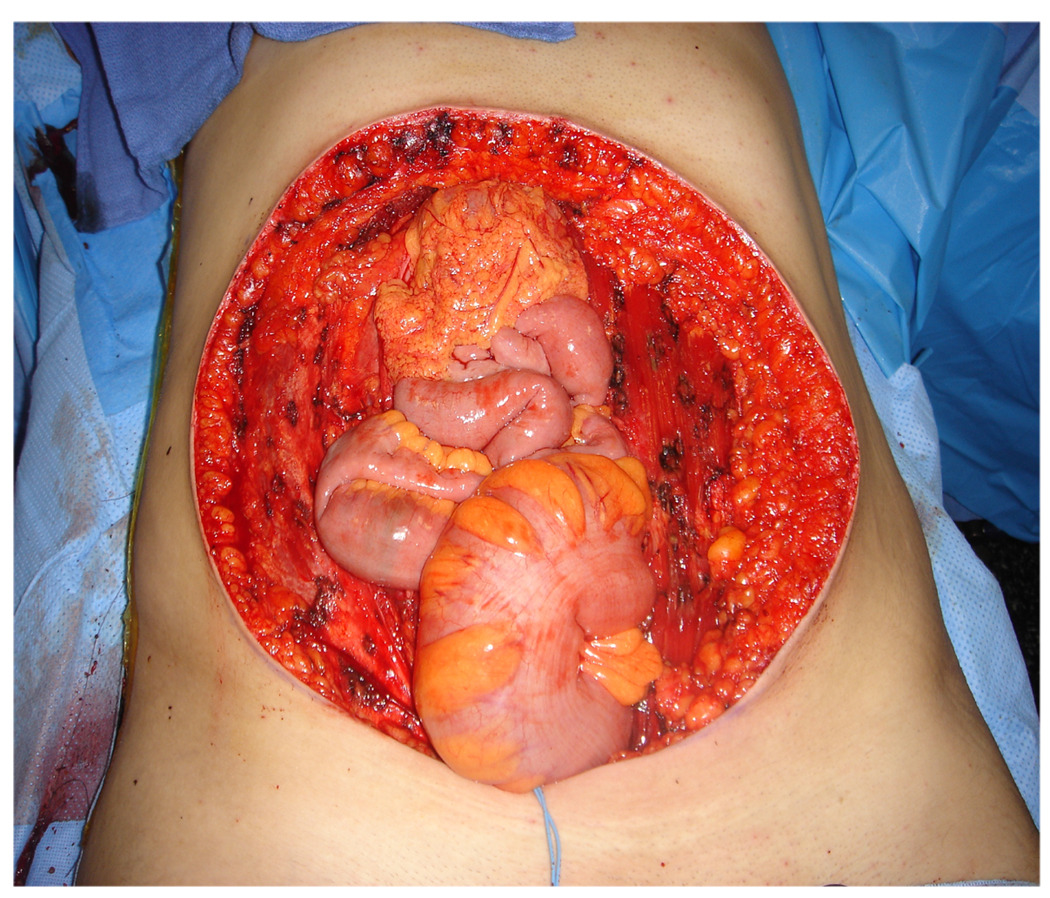
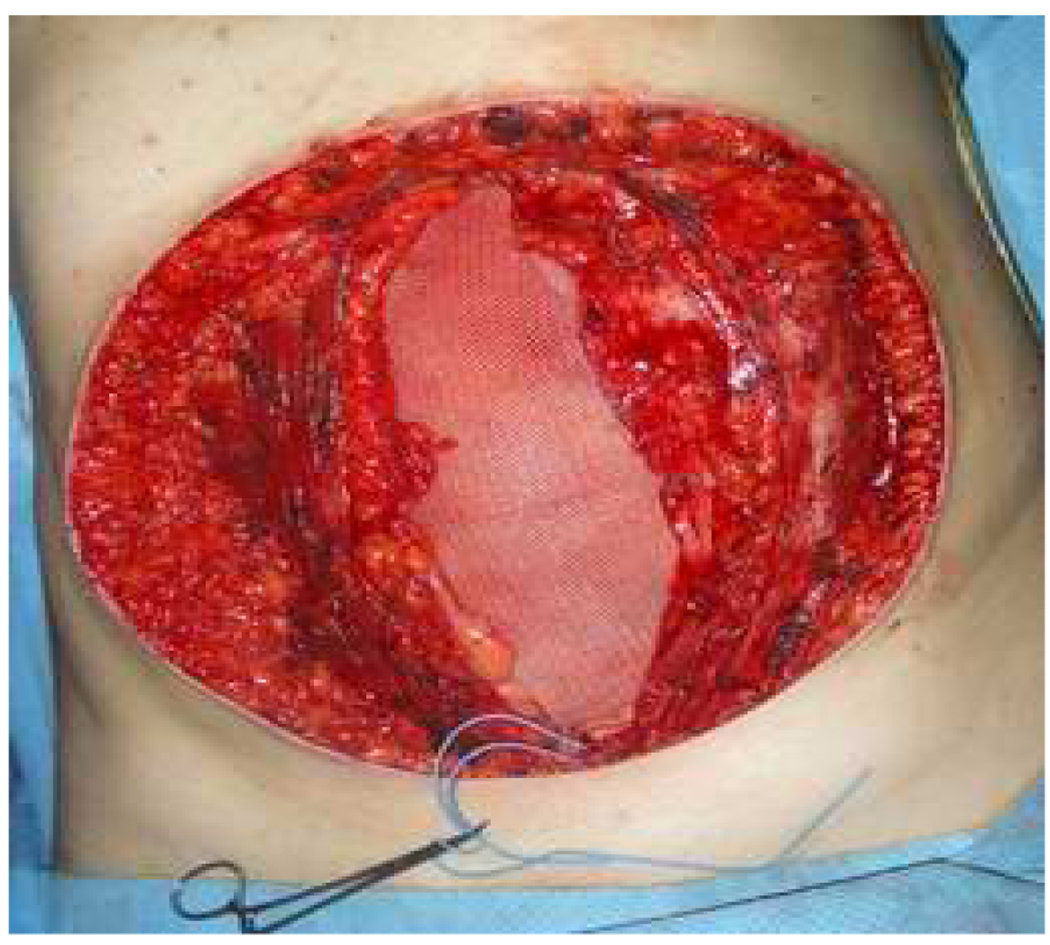
The surgical procedure was performed with a double team of digestive and plastic surgeons. The tumor was resected en bloc with lateral margins of 5 cm ; the excised specimen measured 25 × 25 cm. It included the right rectus muscle with its anterior and posterior aponeuroses, the midline linea alba, and left anterior rectus sheath. Tumor-free resection margins were confirmed by frozen section pathology examination (fig.2). Abdominal exploration revealed no colonic polyps. Abdominal wall reconstruction was performed at the same operative session. A bi-layer synthetic prosthesis was sutured to the fascial edges of thedefect with the smooth inert layer facing inward toward the intestinal viscera (fig.3). This was then covered by a latissimus dorsi myocutaneous free flap.
Figure 2.
Intra-operative view : after tumor résection : 25 × 25 cm. loss of substance.
Figure 3.
Double-faced prosthetic patch placed intra-peritoneally.
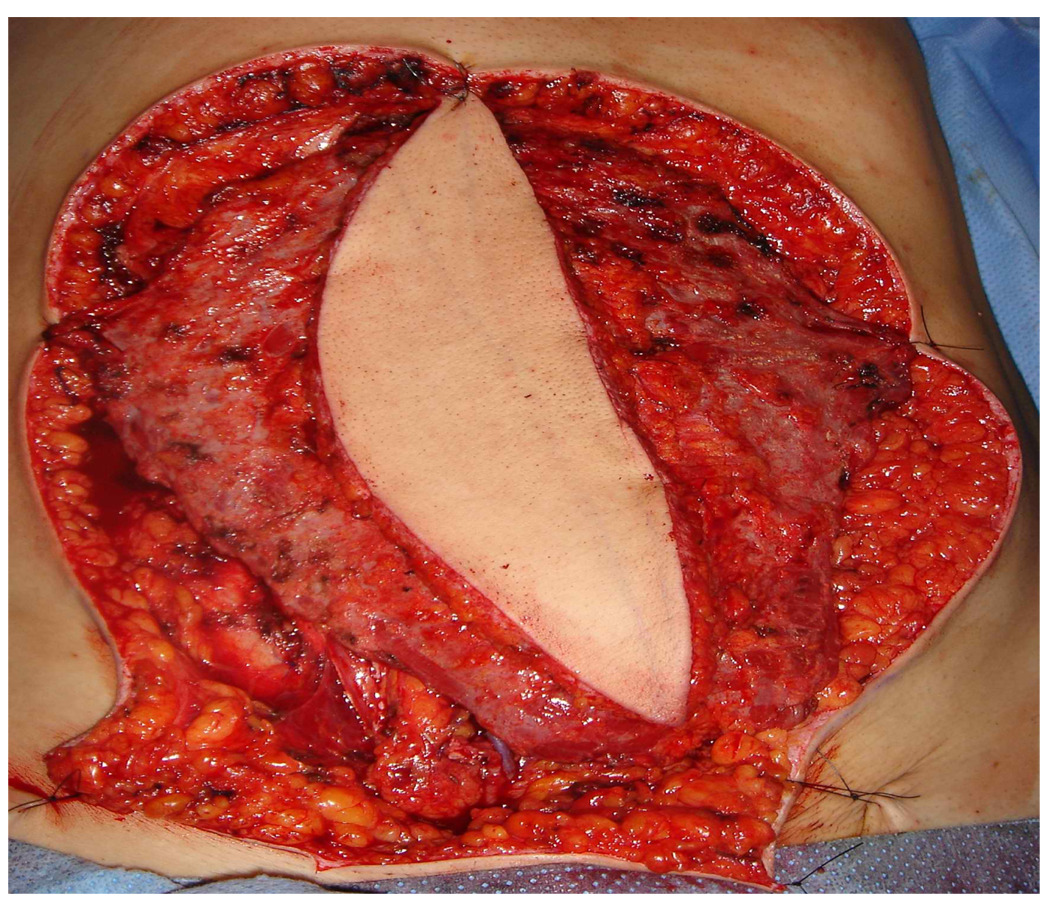
Microsurgical end-to-end anastomosis of the thoracodorsal vessels to the inferior epigastric vessels was performed (fig.4). The 10 × 20 cm cutaneous pallet did not provide complete coverage of the muscle ; delayed split thickness skin grafts were applied to complete the coverage on the 10th post-operative day. There were no post-operative complications and the length of hospitalization was 15 days. Pathologic examination revealed a fibroblastic spindle-cell proliferation confirming the diagnosis of desmoid tumor. The en bloc resection included 5 cm tumor-free margins. At 24 months of follow-up, the patient has has no evidence of recurrence and has a solid parietal reconstruction (fig.5).
Figure 4.
Placement of the latissimus dorsi free flap.
Figure 5.
Post-operative result at 24 months.
DISCUSSION
Despite the invasive potential of desmoid tumors and their high rate of local recurrence, wide surgical excision remains the management of choice ; the recurrence rate depends on the completeness of initial resection. Three studies have confirmed the relationship between the size of the lateral margins and the rate of local recurrence ; they all insist on the importance of complete « R0 » resection [1–3]. Yet none of these studies has established an unequivocal consensus on optimal margin width.
Adequate surgery is the cornerstone of treatment, particularly since the results of radiotherapy and chemotherapy have been either disappointing or uncertain [3]. But adequate radical resection may result in a huge loss of substance as was seen in this case; the entire thickness of the abdominal wall extending far beyond the periumbilical tumor was removed. The latissimus dorsi free flap is an ideal choice for reconstruction of such a wide full-thickness defect [4,5]. With more limited loss of substance, primary coverage can be achieved by mobilization of adjacent skin, muscle, and aponeurotic layers with the help of relaxing incisions. Resultant lateral skin defects can be covered with split-thickness skin grafts and subsequently corrected with tissue expansion techniques. But the reconstruction of full-thickness abdominal wall defects is precarious, often performed under tension ; risks of dehiscence or necrosis contraindicate the use of any bridging prosthesis other than absorbable patches.
For larger defects, myocutaneous pedicle flaps offer solid well-vascularized coverage. Depending on defect size, any one of several pedicle flaps may be suitable [6,7] : flaps based on the rectus abdominis or the latissimus dorsi work well for upper abdominal defects. Flaps based on the rectus femoris, the vastus lateralis–anterolateral thigh flap[8], the sartorius[9], and the tensor fascia lata (10) have all been used for coverage of lower abdominal wall defects.
The rectus femoris flap is a Type II in the classification of Mathes and Nahai (one dominant vascular pedicle with several accessory pedicles which are incapable of nourishing the flap). The dominant pedicle is the descending branch of the lateral circumflex femoral artery originating off the deep femoral artery. It yields a muscular plaque of 20 × 12 cm and can support a paddle of harvestable skin up to 20 × 12 cm. It is a reliably vascularized flap but its surface coverage is somewhat limited and donor site sequelae are fairly significant. Sacrifice of the rectus femoris muscle results in a 20% decrease in extensor strength of the knee compared with the contralateral side.
The anterolateral thigh flap is a septocutaneous flap whose vascularization is based on the perforating branches of the descending branch of the lateral circumflex artery. It offers a maximum flap size of 18 × 24 cm when used as a pedicle flap and up to 25 × 35 cm when used as a free flap. The reliable vascularity of this flap allows its use in combination with a non-resorbable prosthetic patch.
The tensor fascia lata flap offers the particular advantage of a solid layer for parietal repair, thereby avoiding the need for prosthetic repair.
Only free flaps offer freedom from spatial constraints. The latissimus dorsi free flap is an ideal transfer. It offers maximal surface coverage. Donor site sequelae are minimal. Vascular pedicles are of good caliber and can be microsurgically anastomosed to either the superior or inferior epigastric vessels depending on the location requiring reconstruction. The excellent trophic quality of the latissimus dorsi muscle and the reliability of the flap allow effective coverage over sizeable prosthetic reconstructions.
Some authors propose the use of an innervated musculocutaneous flap. According to Ninkovic et al [11], grafting of the thoracodorsal nerve to an intercostal nerve branch results in re-innervation of the latissimus dorsi muscle with satisfactory muscle contraction to reinforce the parietal repair. Electromyographic studies on 4 patients after 2 years showed active muscular contraction and complete reinnervation of the latissimus dorsi muscle flap. The innervated latissimus dorsi free flap may represent an alternative allowing a dynamic reconstruction of the abdominal wall with long-term stability.
CONCLUSION
The latissimus dorsi free flap is an ideal solution for reconstruction of extensive defects of the abdominal or chest wall. This flap has numerous advantages : good perfusion based on microsurgical anastomosis of good caliber vessels, unconstrained freedom of placement, a large surface coverage, and a well-vascularized muscular coverage which is resistant to infection and can tolerate radiation therapy if necessary. When used in conjunction with a double faced prosthetic patch, it results in a complete and effective parietal reconstruction.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Sutton RJ, Thomas JM. Desmoid tumours of the anterior abdominal wall. Eur J Surg Oncol. 1999;25:398–400. doi: 10.1053/ejso.1999.0664. [DOI] [PubMed] [Google Scholar]
- 2.Ballo MT, Zagars GK, Pollack A, Pisters PWT, Pollock A. Desmoid tumor: prognostic factors and outcome after surgery, radiation therapy, or combined surgery and radiation therapy. J Clin Oncol. 1999;17:158–167. doi: 10.1200/JCO.1999.17.1.158. [DOI] [PubMed] [Google Scholar]
- 3.Couturaud B, Arnaud E, Revol M, Servant JM. Tumeurs malignes de la paroi abdominale. Dix ans d’expérience à l’Hôpital Saint-Louis. Ann Chir Plast Esthet. 1999;44:373–383. [PubMed] [Google Scholar]
- 4.Le Fourn B, Lejeune F, Sartre JY, Loirat Y, Pannier M. Large abdominal wall reconstruction by free flap after recurrence of a dermatofibrosarcoma protuberans. Ann Chir Plast Esthet. 1996;41:660–665. [PubMed] [Google Scholar]
- 5.Brenner P, Rammelt S. Abdominal wall and foot reconstruction after extensive desmoid tumor resection with free tissue transfer. Lagenbecks Arch Surg. 2002;386:592–597. doi: 10.1007/s00423-002-0277-y. [DOI] [PubMed] [Google Scholar]
- 6.Mathes SJ, Steinwald PM, Foster RD, Hoffman WY, Anthony JP. Complex abdominal wall reconstruction. A comparison of flap and mesh closure. Ann Surg. 2000;232:586–596. doi: 10.1097/00000658-200010000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rohrich RJ, Lowe JB, Hackney FL, Hobar PC. An algorithm for abdominal wall reconstruction. Plast Reconstr Surg. 2000;105:202–216. doi: 10.1097/00006534-200001000-00036. [DOI] [PubMed] [Google Scholar]
- 8.Kimata Y, Uchiyama K, Ebihara S. Anterolateral thigh flap donor-site complications and morbidity. Plast Reconstr Surg. 2000;106:584–589. doi: 10.1097/00006534-200009030-00009. [DOI] [PubMed] [Google Scholar]
- 9.Sensöz O, Ustüner TE, Taner OF. Use of a sartorius myofasciocutaneous flap for reconstruction of a large, full-thickness abdominal wall defect. Ann Plast Surg. 1990;25:193–196. doi: 10.1097/00000637-199009000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Williams JK, Carlson GW, Dechalain T, Howell R, Coleman J. Role of tensor fasciae latae in abdominal wall reconstruction. Plast Reconstr Surg. 1998;101:713–718. doi: 10.1097/00006534-199803000-00020. [DOI] [PubMed] [Google Scholar]
- 11.Ninkovic M, Kronberger P, Harpf C, Rumer A, Anderl H. Free innervated latissimus dorsi muscle flap reconstruction of full-thickness abdominal wall defects. 1998;101:971–978. doi: 10.1097/00006534-199804040-00013. [DOI] [PubMed] [Google Scholar]