SYNOPSIS
Objective
We conducted an evaluation to determine if the number of claims reimbursed for caries-related procedures for children in the New York State Medicaid program varied by county fluoridation coverage.
Methods
We calculated the mean number of claims per recipient for children in each county separately for the treatment of caries and all other procedures not related to caries using the 2006 Medicaid claims data.
Results
Compared with the predominantly fluoridated counties, the mean number of restorative, endodontic, and extraction procedures per recipient was 33.4% higher in less fluoridated counties. The mean number of claims per child for caries-related services was inversely correlated with the extent of fluoridation in a county (Spearman's correlation coefficient = −0.54, p<0.0001), but claims for non-caries related services were not.
Conclusions
These findings, when added to the already existing weight of evidence, have implications for promoting policies at the federal and state levels to strengthen the fluoridation program.
Community water fluoridation (CWF) is a classic example of a population-based strategy for controlling dental caries (tooth decay), a common chronic disease.1 It focuses on environmental and policy changes instead of relying on changes in individual behavior, and reaches large segments of the population at a low cost. CWF not only incorporates fluoride into developing teeth, but it also frequently delivers low levels of fluoride to saliva. Furthermore, salivary and plaque fluoride concentrations are likely to be directly related to water fluoride concentrations among children.2 The Centers for Disease Control and Prevention (CDC) estimates that for every dollar spent, CWF saves $38 in treatment costs.3 In Colorado, fluoridation was associated with annual savings of $148.9 million in 2003, or a mean of $61 per person.4
Despite these obvious advantages, only 69.2% of the U.S. population served by community water systems received optimally fluoridated water in 2006. Only 25 states and the District of Columbia have met the U.S. Public Health Service Healthy People 2010 goal of reaching 75% of the population on public water supplies.5 There are many reasons why other states have not met the objective. Laws for implementing CWF vary widely, with only 12 states and the District of Columbia mandating CWF on a statewide basis.6 In most states, CWF is enacted by a local body, either by ordinance or by a referendum. The concerns that are often raised during the discussions about fluoridation cover a broad range of issues including perceived risk and harm of adding fluoride to the water supply; lack of resources to purchase equipment and chemicals, which has substantially increased in recent years; quality and quantity of studies to demonstrate benefits and absence of risks; technical feasibility; the notion that caries is not a problem in the community; ideas speculating that fluoride's main mode of action is topical (hence, no need for systemic ingestion) or that alternative caries prevention programs are just as effective; and debate about individual freedom and community benefit.7–9
The Guide to Community Preventive Services found strong evidence for promoting and continuing community water fluoridation.10 However, some communities have not considered it or have questioned its continuation because the benefits are not easily discernable, and doubts about fluoride's safety, though unfounded, can easily be misleading when raised by opponents.11–13 The finding that dental caries in children has declined in fluoridated and non-fluoridated areas makes it more challenging to argue for the continuation of fluoridation. Fluoride is now available from other sources such as toothpaste, tablets, and rinses, thus making it appear that fluoridation is unnecessary.14–16 Despite the availability of these other sources of fluoride, two large national studies conducted during the 1980s in the U.S. reaffirmed the benefits of CWF.17,18 The National Children's Caries Survey showed that children living in fluoridated areas had 18% to 25% fewer carious lesions compared with those living in non-fluoridated areas.14 The National Preventive Dentistry Demonstration Program (NPDDP) also showed that CWF was the most cost-effective of various types of combinations of school-based preventive dental care procedures.14,17 However, such studies are unlikely to be repeated because it would be difficult to justify their cost given the already available weight of evidence regarding the safety, effectiveness, and cost savings of fluoridation. Therefore, researchers have used other resources, such as Medicaid claims data and economic models, to assess the impact of CWF on the cost of providing dental treatment.4,19,20
Although numerous epidemiologic studies in New York State (NYS) have shown the safety and effectiveness of fluoridation in reducing caries, data on the impact of the fluoridation program on Medicaid claims could be more convincing to policy makers at the local level.15, 21–25 Therefore, an evaluation was undertaken to determine if the number of claims reimbursed for specific caries-related services for children in the Medicaid program varied by county fluoridation coverage. The analysis assessed if the extent of fluoridation is correlated with the mean number of claims reimbursed for restorative, extraction, and endodontic procedures (caries-related services) performed under the Medicaid program to treat dental caries in the Early Periodic Screening, Diagnosis, and Treatment (EPSDT) program age range.
METHODS
Medicaid utilization and expenditure data
We obtained all of the reimbursed claims for dental procedures performed under the Medicaid program for 57 counties and New York City during the 2006 calendar year from the NYS Department of Health's Office of Health Insurance Programs. The analysis was limited to 606,125 children (unduplicated) younger than age 21 who had at least one claim for a dental procedure. For calculating the number of claims per child as an indicator, we selected the number of recipients as the denominator because it reflects the actual number of services delivered per child. Adults were excluded because of their uncertain residential history and the possibility of claims submitted for them for replacement of old fillings and for extractions due to conditions not related to caries. Children's current residential history is more likely to reflect exposure to fluoridation. They are less likely to get replacement fillings, and tooth extractions in children are mainly to treat caries. Dental procedures were grouped by Current Dental Terminology (CDT) procedure codes, and categorized broadly into caries-related (e.g., extraction, endodontic, and restorative) and non-caries-related services (e.g., all other services).
County water fluoridation coverage
We determined fluoridation coverage for each county using the CDC-based Water Fluoridation Reporting System (WFRS), which provides information concerning the population receiving fluoridated water for each county.26 The percentage of people receiving fluoridated water in each county was determined by dividing the number of residents on fluoridated water by the total population from the 2007 U.S. Census data.27 Next, we categorized counties according to the percentage of the population on fluoridated water into three strata: less fluoridated (≤30%), partially fluoridated (31%–69%), and predominantly fluoridated (≥70%) to obtain two groups of counties with the least and greatest penetration of water fluoridation. We considered the NYS mean of 70% of the population on public water supplies receiving fluoridated water as predominantly fluoridated because we estimated that this is likely to be the maximum extent of fluoridation in most counties. Similarly, the opportunities for increasing the percentage covered by fluoridation are greatest in counties with fluoridation levels below 30%, which closely approximates to a tertile.
Demographic information
We obtained demographic information from the 2006 U.S. Census data, the 2006 KIDS COUNT Data Book, and the Kids' Well-being Indicators Clearinghouse (KWIC) to compare the characteristics of fluoridated and non-fluoridated counties.28–30 We merged these datasets and conducted analyses using SAS® version 9.1.31
Claims for dental procedures
We based the analysis on 787,067 claims for the treatment of caries (i.e., restorative, extraction, and endodontic procedures) and 1,094,332 claims for all other procedures not related to the treatment of caries. We excluded claims related to diagnostic and oral prophylactic services for calculating non-caries-related procedures, as these are also related to the treatment of caries. We calculated the mean number of claims per recipient in each county separately for the treatment of caries and all other procedures using the total number of children who received a dental service as the denominator. We developed scatter plots to visualize the mean number of claims per recipient according to the fluoridation status of the county. Spearman's correlation coefficients were calculated to assess the relationship between the extent of fluoridation in a county and the mean number of claims. We also calculated the mean number of claims for the less fluoridated, partial, and predominantly fluoridated counties for three age groups.
We used a linear regression model to assess the effect of county fluoridation coverage on mean number of claims after controlling for county-level characteristics shown in Table 1. The model included county-level characteristics such as the percentage nonwhite, the percentage of children participating in the free or reduced school-lunch program, the percentage urban, and the number of dentists who submitted at least one claim per 100,000 Medicaid-eligible clients.
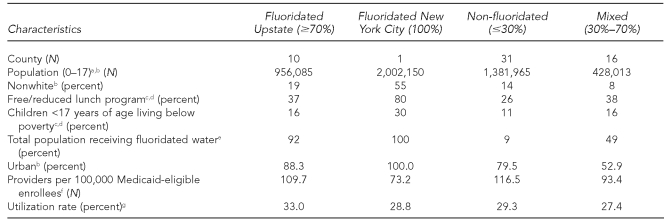
Table 1.
Characteristics of New York State counties by fluoridation status, 2006
aCensus Bureau (US). Table 1: annual estimates of the population for counties of New York: April 1, 2000, to July 1, 2007 (CO-EST2007-01-36) [cited 2008 Apr 20]. Available from: URL: http://www.census.gov/popest/counties/tables/CO-EST2007-01-36.xls
bAuthors' calculation based on: Table 1, U.S. Census 2000 summary file 1, matrices P1, P2, P3, PCT12, and P13, Census 2000, U.S. Census Bureau [cited 2008 Apr 26]. Available from: URL: http://factfinder.census.gov/servlet/DatasetMainPageServlet?_ds_name=DEC_2000_SF1_U&_program=DEC&_lang=en
cNew York State Council on Children and Families. Kids' Well-being Indicators Clearinghouse (KWIC) [cited 2008 Apr 30]. Available from: URL: http://www.nyskwic.org
dAuthors' calculation based on: New York State Council on Children and Families. NYS KIDS COUNT 2006 data book [cited 2006 Sep 21]. Available from: URL: http://www.ccf.state.ny.us.initiatives/archive/kc/2006databookPDFs/complete2006databook.pdf
eAuthors' calculation based on: Centers for Disease Control and Prevention (US). My water's fluoride [cited 2008 Apr 18]. Available from: URL: http://apps.nccd.cdc.gov/MWF/Index.asp
fNumerator is the number of dentists who billed ≥$1,000 in 2006.
gReflects the percent of Medicaid enrollees with at least one claim
RESULTS
Table 1 shows the characteristics of the counties by fluoridation status, including selected demographic characteristics, the percentage of population groups receiving fluoridated water, Medicaid enrollees per provider, and the utilization rate of the counties by assigned fluoridation coverage status. We assigned New York City to a separate group because its demographic characteristics are different from the other counties. Demographic characteristics for the predominantly fluoridated counties and less fluoridated counties were comparable.
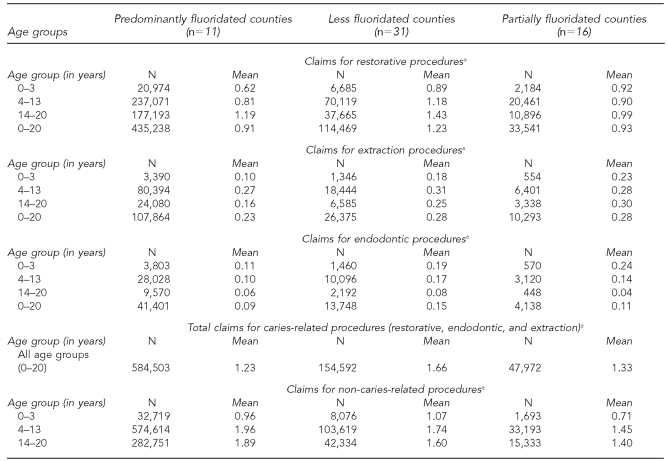
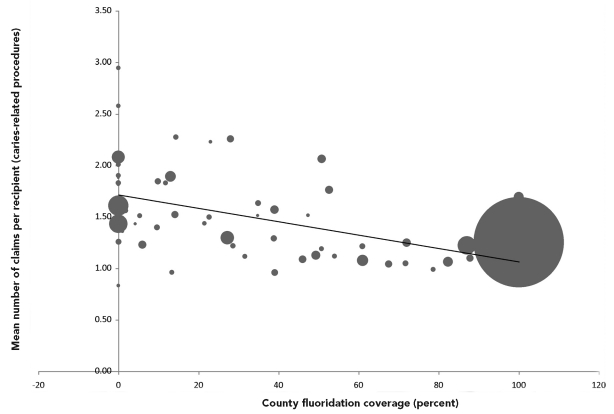
The mean numbers of claims for restorative, endodontic, and extraction procedures per recipient for less fluoridated, partially fluoridated, and predominantly fluoridated counties were 1.66, 1.33, and 1.23, respectively (Table 2). Compared with the predominantly fluoridated counties, the mean number of restorative, endodontic, and extraction procedures per recipient was 33.4% and 8.1% higher in less fluoridated and partially fluoridated counties, respectively. We consistently observed this difference in every age group. The Figure shows a scatter plot of claims for the mean number of restorative, endodontic, and extraction procedures per recipient. The results show that as the county fluoridation coverage increased, the mean number of claims per recipient decreased (Spearman's correlation coefficient =−0.54, p<0.0001). The dispersion of the data expressed as a coefficient of variation around the mean number of claims was larger in less fluoridated counties when compared with that in more fluoridated counties.
Table 2.
Claims for restorative, endodontic, extraction, and other non-caries-related procedures by fluoridation status and age groups in counties in New York State: New York State Medicaid claims data, 2006
aN represents the number of claims and mean represents the average number of claims per recipient.
Figure.
Mean number of claims per recipient for restorative, endodontic, and extraction procedures in 0- to 20-year-olds by county and fluoridation status: New York State Medicaid claims data, 2006
Note: Each data point reflects the relative size of the eligible population. The coefficient of variation was 27.2%, 23.4%, and 18.3%, respectively, for ≤30%, 30%–69%, and ≥70% county fluoridation coverage.
The mean number of claims per recipient for non-caries-related claims did not follow the same pattern as that for procedures performed for the treatment of caries. There was no correlation between county fluoridation coverage and mean claims per recipient for non-caries-related procedures (Spearman's correlation coefficient =−0.06909, p=0.6063).
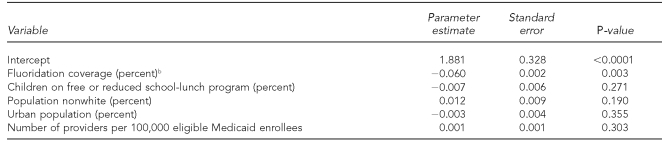
The regression analysis showed that for every 10% increase in the fluoridation status of a county, the number of claims per child for caries-related services declined by 0.06 (p<0.01) (Table 3). This equates to a difference of 60 claims per 100 children when the county's fluoridation status changes from zero to 100%.
Table 3.
Regression analysis of claims for restorative, extraction, and endodontic procedures per child: New York State Medicaid claims data, 2006a
aUnit of analysis is county (n=58); r2=0.2817.
bEstimated decrease in the mean number of claims per child is based on a 10% increase in fluoridation coverage of a county. An increase from 0% to 100% in fluoridation equates to a decline of 0.6 claims per child.
DISCUSSION
The analysis of the data showed fewer claims per recipient for procedures related to caries in predominantly fluoridated counties compared with less fluoridated counties. The finding that claims for caries-related procedures, but not other dental procedures, were correlated with the fluoridation status of the county strengthens the contribution of fluoridation in explaining this geographic variation. It is highly unlikely that a systematic error favoring fluoridation has occurred with respect to only caries-related procedures but not non-caries-related procedures. Furthermore, a finding of greater variation among less fluoridated areas is consistent with the effect of fluoridation in that while fluoridation reaches all segments of the population, other alternatives can have varying effects.
Based on the NYS Medicaid Fee Schedule, a single claim for a simple restoration on a permanent tooth costs $55. It can range from $43 to $580, depending upon the procedure performed. Therefore, the mean cost of a simple restorative service per Medicaid recipient is estimated to be $91.30 (1.66 × 3 $55) and $67.65 (1.23 × 3 $55) in less fluoridated and predominantly fluoridated counties in NYS, respectively. The difference between these two groups in treatment costs per recipient (younger than 21 years of age) averaged $23.63, assuming that all of them received a simple restoration. This is a conservative estimate, as claims for adjunctive services such as examinations; radiographs and complex treatments; and costs related to transportation, emergency room visits, and lost productivity are not included. Such annual decreases in claims per recipient when applied to lifetime exposure of the whole population have large societal benefits. This assumes greater importance for counties in NYS, as their share of Medicaid contribution is significantly reduced. These results are consistent with the studies conducted in Louisiana and Texas, which found that substantial savings in public programs were associated with CWF programs. In Louisiana, the difference in treatment costs per Medicaid-eligible child residing in fluoridated parishes compared with those residing in non-fluoridated parishes ranged from $14.68 for one-year-olds to $58.91 for 3-year-olds. The mean difference in treatment costs per eligible preschooler was $36.28.19 In the Texas Health Steps (EPSDT-Medicaid) program, the mean dental treatment cost per child decreased by $24 for a unit increase in fluoridation level (0.0 milligrams/liter fluoride (mg/L F) to 1.0 mg/L F).20
Implications
These findings have implications for promoting policies at the federal and state levels to strengthen the fluoridation program. Recently, many communities have considered discontinuation of water fluoridation due to the increased cost of chemicals. Basically, the savings associated with fluoridation are not linked to the costs carried by the community water supplier. Therefore, policy initiatives that provide more direct links between fluoridation costs and benefits may be attractive. Such initiatives may include subsidies for water system infrastructure and chemical costs. Initiatives that involve disincentives and incentives for communities and insurance programs could be explored.32
Limitations and considerations of alternative explanations
This study was subject to several limitations. An evaluation study such as this could be undertaken only in states where there is wide geographic variation in population coverage by fluoridation. Although approximately 12 million NYS residents receive fluoridated water, only about 40% of residents outside New York City live in fluoridated communities. Therefore, populations were available to assess the impact. However, measuring the impact of fluoridation to control dental caries is difficult because it is characterized by a complex interaction of multiple risk factors. Epidemiologic studies require follow-up of individuals for a long period of time and careful documentation of exposure to fluoridation, and other sources of fluoride, at the individual level. Furthermore, the diffusion of fluoride-added drinking water to non-fluoridated areas via processed beverages dilutes the effects.33 The cost of undertaking an evaluation of such a proven population-based intervention can be enormous and, thus, difficult to justify. It is even more challenging to design such evaluation studies because fluoridated and non-fluoridated communities may be inherently different with respect to known and unknown variables. Communities decide to adopt fluoridation because of high levels of dental caries. However, an indirect assessment by limiting the analysis to the Medicaid population may be more valid because to some extent, the eligibility for Medicaid is based on uniform criteria and, therefore, this population is more homogeneous than the general population.
Many factors influence geographic variation in the mean number of claims for caries-related procedures, such as enrollment rates in Medicaid, disease occurrence, availability of dentists, and subsequent treatment. Therefore, one should be cautious in attributing this geographic variation solely to water fluoridation. Furthermore, the availability of fluoride in beverages and fluoride provided through organized programs, which distribute tablets and rinses in non-fluoridated communities, may underestimate the effect of fluoridation. A survey of third-grade children in less fluoridated communities in NYS showed that reportedly 20% to 80% of children had received fluoride tablets on a regular basis.34 About 100,000 school-aged children in non-fluoridated areas are targeted for participation in a weekly fluoride rinse program. In addition, toothpaste and processed beverages are the other sources of fluoride. Programs such as school-based sealant programs are also available in these areas. Therefore, the observation of an effect in fluoridated counties is impressive.
A limitation of this study was the use of Medicaid administrative data, for which the accuracy of reporting of claims is unknown. There are three different reimbursement methods in the NYS Medicaid program, which could have led to under- or overreporting of claims. However, there is no reason to believe that the reporting is associated with the fluoridation status of a county. We measured the exposure to fluoridation at the ecologic level, and covariates at the individual level were not available to control for confounding.
The length or magnitude of the children's exposure to fluoridation and other sources of fluoride were not available and, therefore, a comparison made between more and less fluoridated counties could lead to misclassification of children with respect to exposure. Also, we did not have data to verify that the water systems maintained fluoride concentrations at the optimal level. In addition, the extent of the use of other preventive measures is unknown. Furthermore, only aggregate-level claims at the county level were available. Nevertheless, one can examine alternative explanations for the geographic variation. First, utilization of services can vary depending upon the availability of dentists. However, the overall utilization among these predominantly fluoridated and less fluoridated counties was largely similar (33% vs. 29%). Second, dental caries is cumulative and, therefore, age of children can affect service utilization and the mix of services (Table 2). In this study, there were consistently fewer claims for caries-related procedures in every age group. Finally, dental sealants are also effective in preventing dental caries, but fewer than 8% of all children in the Medicaid program receive sealants. Furthermore, the difference in claims was observed even in the youngest age group who do not receive sealants.
In general, ecologic studies only provide weak evidence for establishing causal relationships. Therefore, to establish causality, these types of studies must be followed by more rigorous, analytical approaches. We justify the use of an ecologic design for this analysis because it is used as an evaluation method to monitor the benefits of a proven population-based intervention. The effectiveness, safety, and cost savings of fluoridation have been demonstrated, and the biological mechanism of fluoride action is established. Furthermore, we explored alternative explanations, such as the availability of dentists, age distribution, service mix, urban-rural nature, and poverty level of the county.
Although the use of Medicaid administrative data is a limitation of this study, there are several advantages: these data are readily available, this study is based on the whole population rather than a sample, and the number of children receiving the benefits is large. As it stands, this analysis of children enrolled in the Medicaid program serves as a surveillance study of the fluoridation program.
CONCLUSIONS
We found that the mean number of claims for caries-related services for children in the NYS Medicaid program was correlated with the extent of fluoridation in a county. These annual decreases in claims per recipient, when applied to lifetime exposure of the whole population, have large societal benefits. These findings, added to the already existing weight of evidence, have implications for promoting policies at the federal and state levels to strengthen the fluoridation program.
Acknowledgments
The authors thank Guthrie Burkhead, MD, MPH, and Mark Moss, DDS, MS, PhD, for their helpful comments.
REFERENCES
- 1.Ten great public health achievements—United States, 1900–1999. MMWR Morb Mortal Wkly Rep. 1999;48(50):1141. [PubMed] [Google Scholar]
- 2.Pessan JP, Silva SM, Lauris JR, Sampaio FC, Whitford GM, Buzalaf MA. Fluoride uptake by plaque from water and from dentifrice. J Dent Res. 2008;87:461–5. doi: 10.1177/154405910808700501. [DOI] [PubMed] [Google Scholar]
- 3.Griffin SO, Jones K, Tomar SL. An economic evaluation of community water fluoridation. J Public Health Dent. 2001;61:78–86. doi: 10.1111/j.1752-7325.2001.tb03370.x. [DOI] [PubMed] [Google Scholar]
- 4.O'Connell JM, Brunson D, Anselmo T, Sullivan PW. Costs and savings associated with community water fluoridation programs in Colorado. Prev Chronic Dis. 2005;2 Spec No:A06. [PMC free article] [PubMed] [Google Scholar]
- 5.Populations receiving optimally fluoridated public drinking water—United States, 1992–2006. MMWR Morb Mortal Wkly Rep. 2008;57(27):737–41. [PubMed] [Google Scholar]
- 6.The Pew Center on the States. The cost of delay: state dental policies fail one in five children. Washington: The Pew Charitables Trusts; 2010. Feb, [cited 2010 May 12]. Also available from: URL: http://www.pewcenteronthestates.org/uploadedFiles/Cost_of_Delay_web.pdf. [Google Scholar]
- 7.Analyzing selected criticisms of water fluoridation. J Can Dent Assoc. 1981;47:1–12. [PubMed] [Google Scholar]
- 8.Neenan ME. Obstacles to extending fluoridation in the United States. Community Dent Health. 1996;13(Suppl 2):10–20. [PubMed] [Google Scholar]
- 9.Newbrun E. The fluoridation war: a scientific dispute or a religious argument? J Public Health Dent. 1996;56(5 Spec No):246–52. doi: 10.1111/j.1752-7325.1996.tb02447.x. [DOI] [PubMed] [Google Scholar]
- 10.Truman BI, Gooch BF, Evans CA Jr, editors. The guide to community preventive services: interventions to prevent dental caries, oral and pharyngeal cancers, and sports-related craniofacial injuries. Am J Prev Med. 2002;23(Suppl 1) doi: 10.1016/s0749-3797(02)00449-x. [DOI] [PubMed] [Google Scholar]
- 9.Moore K. Officials considering removal of fluoride from Schenectady water. Daily Gazette. 2008. Feb 8, [cited 2008 Feb 8]. Available from: URL: http://www.dailygazette.com/news/2008/feb/08/0208_fluoride.
- 12.Armfield JM. When public action undermines public health: a critical examination of antifluoridationist literature. Aust New Zealand Health Policy. 2007;4:25. doi: 10.1186/1743-8462-4-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hazard vs. outrage: public perception of fluoridation risks. J Public Health Dent. 1990;50:285–7. doi: 10.1111/j.1752-7325.1990.tb02137.x. [DOI] [PubMed] [Google Scholar]
- 14.Brunelle JA, Carlos JP. Recent trends in dental caries in U.S. children and the effect of water fluoridation. J Dent Res. 1990;69(Spec No):723–7. doi: 10.1177/00220345900690S141. [DOI] [PubMed] [Google Scholar]
- 15.Kumar JV, Swango PA, Lininger LL, Leske GS, Green EL, Haley VB. Changes in dental fluorosis and dental caries in Newburgh and Kingston, New York. Am J Public Health. 1998;88:1866–70. doi: 10.2105/ajph.88.12.1866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leverett DH. Fluorides and the changing prevalence of dental caries. Science. 1982;217:26–30. doi: 10.1126/science.7089534. [DOI] [PubMed] [Google Scholar]
- 17.Klein SP, Bohannan HM, Bell RM, Disney JA, Foch CB, Graves RC. The cost and effectiveness of school-based preventive dental care. Am J Public Health. 1985;75:382–91. doi: 10.2105/ajph.75.4.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heller KE, Eklund SA, Burt BA. Dental caries and dental fluorosis at varying water fluoride concentrations. J Public Health Dent. 1997;57:136–43. doi: 10.1111/j.1752-7325.1997.tb02964.x. [DOI] [PubMed] [Google Scholar]
- 19.Water fluoridation and costs of medicaid treatment for dental decay—Louisiana, 1995–1996. MMWR Morb Mortal Wkly Rep. 1999;48(34):753–7. [PubMed] [Google Scholar]
- 20.Texas Department of Health. Water fluoridation costs in Texas: Texas Health Steps (EPSDT-MEDICAID) 2000. May,
- 21.Ast DB, Fitzgerald B. Effectiveness of water fluoridation. J Am Dent Assoc. 1962;65:581–7. doi: 10.14219/jada.archive.1962.0311. [DOI] [PubMed] [Google Scholar]
- 22.Ast DB, Smith DJ, Wachs B, Cantwell KT. Newburgh-Kingston caries-fluorine study. XIV. Combined clinical and roentgenographic dental findings after ten years of fluoride experience. J Am Dent Assoc. 1956;52:314–25. doi: 10.14219/jada.archive.1956.0042. [DOI] [PubMed] [Google Scholar]
- 23.Gelberg KH, Fitzgerald EF, Hwang SA, Dubrow R. Fluoride exposure and childhood osteosarcoma: a case-control study. Am J Public Health. 1995;85:1678–83. doi: 10.2105/ajph.85.12.1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kumar JV, Green EL, Wallace W, Carnahan T. Trends in dental fluorosis and dental caries prevalences in Newburgh and Kingston, NY. Am J Public Health. 1989;79:565–9. doi: 10.2105/ajph.79.5.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mahoney MC, Nasca PC, Burnett WS, Melius JM. Bone cancer incidence rates in New York State: time trends and fluoridated drinking water. Am J Public Health. 1991;81:475–9. doi: 10.2105/ajph.81.4.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention (US) My water's fluoride. [cited 2008 Apr 18]. Available from: URL: http://apps.nccd.cdc.gov/MWF/Index.asp.
- 27.Census Bureau (US) Table 1: annual estimates of the population for counties of New York: April 1, 2000, to July 1, 2007 (CO-EST2007-01-36) [cited 2008 Apr 20]. Available from: URL: http://www.census.gov/popest/counties/tables/CO-EST2007-01-36.xls.
- 28.Census Bureau (US) U.S. Census 2000 summary file 1, matrices P1, P2, P3, PCT12, and P13. [cited 2008 Apr 26]. Available from: URL: http://factfinder.census.gov/servlet/DatasetMainPageServlet?_ds_name=DEC_2000_SF1_U&_program=DEC&_lang=en.
- 29.New York State Council on Children and Families. NYS KIDS COUNT 2006 data book. [cited 2006 Sep 21]. Available from: URL: http://www.ccf.state.ny.us.initiatives/archive/kc/2006databookPDFs/complete2006databook.pdf.
- 30.New York State Council on Children and Families. Kids' Well-being Indicators Clearinghouse (KWIC) [cited 2008 Apr 30]. Available from: URL: http://www.nyskwic.org.
- 31.SAS Institute, Inc. SAS: Version 9.1 for Windows. Cary (NC): SAS Institute, Inc.; 2002–2003. [Google Scholar]
- 32.Brownell KD, Frieden TR. Ounces of prevention—the public policy case for taxes on sugared beverages. N Engl J Med. 2009;360:1805–8. doi: 10.1056/NEJMp0902392. [DOI] [PubMed] [Google Scholar]
- 33.Griffin SO, Gooch BF, Lockwood SA, Tomar SL. Quantifying the diffused benefit from water fluoridation in the United States. Community Dent Oral Epidemiol. 2001;29:120–9. doi: 10.1034/j.1600-0528.2001.290206.x. [DOI] [PubMed] [Google Scholar]
- 34.Kumar JV, Altshul DL, Cooke TL, Green EL. Oral health status of third grade children: New York State oral health surveillance system. Albany (NY): New York State Department of Health; 2005. Dec 15, Also available from: URL: http://www.health.state.ny.us/prevention/dental/docs/child_oral_health_surveillance.pdf. [Google Scholar]