SYNOPSIS
Objectives
Water fluoridation is one of the most effective public health programs of the past century. However, efforts to extend water fluoridation into currently non-fluoridated areas are often thwarted. Despite considerable evidence regarding the effectiveness of water fluoridation at an individual level, published national community-based studies are rare. This study compared children's decay experience and prevalence between areas with and without water fluoridation in Australia.
Methods
Oral health data were obtained from clinical examinations of 128,990 5- to 15-year-old children attending for a regular visit with their respective Australian state or territory School Dental Service in 2002. Water fluoridation status, residence remoteness, and socioeconomic status (SES) were obtained for each child's recorded residential postcode area.
Results
Children from every age group had greater caries prevalence and more caries experience in areas with negligible fluoride concentrations in the water (<0.3 parts per million [ppm]) than in optimally fluoridated areas (≥0.7 ppm). Controlling for child age, residential location, and SES, deciduous and permanent caries experience was 28.7% and 31.6% higher, respectively, in low-fluoride areas compared with optimally fluoridated areas. The odds ratios for higher caries prevalence in areas with negligible fluoride compared with optimal fluoride were 1.34 (95% confidence interval [CI] 1.29, 1.39) and 1.24 (95% CI 1.21, 1.28) in the deciduous and permanent dentitions, respectively.
Conclusions
This study demonstrates the continued community effectiveness of water fluoridation and provides support for the extension of this important oral health intervention to populations currently without access to fluoridated water.
Dental disease in the form of dental caries is associated with a range of adverse outcomes including substantial pain, reduced sleep capacity, decreased ability to eat some foods, social embarrassment, and lowered self-esteem.1–3 While individual treatment for dental caries is effective, such treatment may be delayed because of financial or other reasons until people are experiencing significant levels of pain and functional impairment. Dental caries is one of the most common diseases in modern societies and carries with it a considerable financial burden.4
The most widely implemented public health intervention for the prevention of dental caries is water fluoridation, a practice that involves the deliberate addition of fluoride to the public water supply. Fluoride improves dental health by being incorporated into the crystalline structure of the tooth to form fluorapatite, which is less soluble than hydroxyapatite, and thereby inhibits the process of demineralization or decay. It also enhances remineralization of the tooth surface, inhibits bacterial metabolism, and inhibits plaque formation.5 Numerous studies have indicated that water fluoridation is effective in reducing dental caries.6 In recognition of this outcome, the Centers for Disease Control and Prevention (CDC) proclaimed water fluoridation as one of the 10 major public health achievements of the 20th century, alongside vaccinations and the control of infectious diseases.7 However, water fluoridation remains relevant in the 21st century, and the U.S. Surgeon General has argued that it “continues to be a vital, cost-effective method of preventing dental caries.”8
Despite the established effectiveness of water fluoridation, many countries have not adopted this public health practice. Indeed, even in those countries with the highest population coverage of fluoridated water, a substantial percentage of people still do not have access to its benefits. In Australia, for example, it was estimated that only 69% of the Australian population in 2006 had access to optimally fluoridated water, with this figure varying across states and territories from 4.7% in Queensland to 100.0% in the Australian Capital Territory.9 The percentage of the population with access to fluoridated water in Australia was similar to that in the U.S. and higher than that of most other countries with water fluoridation.
One reason that some countries have been reluctant to implement water fluoridation is because some decision makers in those countries regard fluoride as an environmental pollutant, a view that has been fostered by lobby groups opposed to water fluoridation.10 However, the argument that water fluoridation is hazardous ignores the importance of fluoride concentration to toxicity. In Australia, for example, although fluoride is officially listed as being both harmful to health and pervasive in the environment, this declaration is qualified by the acknowledgement that it is present “at very low levels that are not believed to be harmful.”11
Water fluoridation is one of numerous public health practices that have generated a degree of controversy at the hands of often small but mobilized groups capable of swaying the views of both politicians and the public. For example, the implementation of water chlorination, compulsory child immunizations, mandatory seatbelt use, free distribution of condoms, and bans on smoking in public places have been criticized as being attacks on personal freedom or downright harmful. Interestingly, other public health policies using fluoride, such as salt or milk fluoridation, have generated less controversy than water fluoridation. Perhaps this dichotomy reflects the fact that salt fluoridation and other such practices are employed much less frequently, and that organized opposition to water fluoridation predominantly stems from the U.S., where water fluoridation is widely implemented but salt fluoridation is not. The continued opposition to water fluoridation can also be attributed to the widespread devolution of political decision-making to local political regions, which are more reactive to outspoken minority and special-interest groups.
Ideally, studies of water fluoridation measure exposure at the individual level, as there may be considerable variation in exposure within a fluoridated or non-fluoridated area as a result of residential mobility (i.e., people moving in and out of fluoridated areas) as well as differences in consumption of public water and fluoride-containing beverages and foods. Studies at the individual level are preferred over studies at the community or population level, which do not take into account individual fluoride exposure or other individual risk factors. However, while community-level studies do not provide good evidence of the efficacy or “actual” effectiveness of fluoridated water consumption, they provide valuable information concerning the effectiveness of water fluoridation in practice, as it is mitigated by a number of other factors. For instance, if very few children are actually consuming adequate quantities of fluoridated public water, the community-level or “practical” effectiveness of water fluoridation may be low, regardless of its efficacy. A pattern of lower decay experience in fluoridated areas compared with non-fluoridated areas would, therefore, be consistent with the argument that a practical benefit is obtained by the addition of fluoride to water supplies.
While a small number of community-level studies have shown water fluoridation to be effective,12–15 some individuals point to studies that show, or allege, either the opposite effect or no effect and have used these studies to dismiss the effectiveness of water fluoridation generally.16 For instance, a study by Yiamouyiannis17 found no caries preventive effect for water fluoridation among U.S. children, although a subsequent study using the same database found significant associations.18 Opponents of water fluoridation make a continued case for the abolition of water fluoridation based on a series of articles from Australia, New Zealand, and elsewhere that argue that water fluoridation is not effective.19–26
Diesendorf has argued that for researchers to either confirm or refute the hypothesis that declines in caries experience are attributable to factors other than water fluoridation, “it is necessary (but not ‘sufficient’) to examine the absolute values of caries prevalence in fluoridated and unfluoridated areas.” He goes on to argue that even if only a small number of non-fluoridated areas have comparable caries experience to that seen in some fluoridated areas, this would provide a strong case for reexamining studies showing the effectiveness of water fluoridation.22 Although such an extreme position is most likely an exercise in sophistry and ignores crucial and obvious variations in dental caries experience resulting from other causes, it is the case that if water fluoridation is effective, we would expect a pattern of results showing reduced caries experience in fluoridated areas after controlling for basic possible confounding factors.
Given the ubiquity of fluoride in the environment where water fluoridation is practiced, it is imperative that we ask whether or not children's caries experience is actually lower in areas with a higher concentration of fluoride in the water. In Australia, descriptive and anecdotal evidence suggests that children's oral health is poor in those areas that have had the least water fluoridation. For example, Queensland, which for many decades remained the only Australian state or territory to have not implemented wide-scale water fluoridation, has consistently ranked among the poorest child oral health in the country.27 In countries such as the U.S., where there are no established school dental programs to provide preventive and restorative treatment to school-aged children, water fluoridation is perhaps even more important and is likely to be even more effective as a population preventive oral health practice.
A report released by the Australian Institute of Health and Welfare in 2007 documented consistently better oral health for children living in fluoridated areas than for children living in non-fluoridated areas.28 However, these differences were not quantified and the socioeconomic circumstances and regional location of the children—factors that have previously been found to be associated with both water fluoridation and children's oral health—were not taken into account in the comparisons. The aim of this study, therefore, was to evaluate whether children living in areas with higher concentrations of fluoride in the public water supply have significantly reduced dental caries compared with children residing in non-fluoridated or low-fluoride areas, after controlling for the possible confounding effects of age, regional location, and area-based socioeconomic status (SES).
METHODS
This study used data from a national surveillance survey of children's dental health conducted in Australia in 2002. Oral health data were obtained on a random sample of children attending routine visits with their respective state or territory School Dental Service (SDS), a free or subsidized oral health program offering preventive and restorative treatments to school-aged children. Enrollment in SDS is voluntary, and the percentage of children enrolled varies across and within Australia's states and territories, as well as between primary and secondary levels of schooling. Generally, enrollment for younger children is higher than for older children, with the percentages of children being seen by SDS substantially diminished by the late teen years. At younger ages, more than 80% of children may be regularly seen within SDS.
Because of changes in service delivery occurring in the most populous Australian state, New South Wales, no data were available from this jurisdiction in 2002. Children were sampled from most states and territories based on their date of birth, although one state (South Australia) provided a complete enumeration of all children attending SDS. Where children received more than one examination during the 2002 calendar year, the information derived from examinations other than the first was excluded. More specific details regarding the survey and state-level sampling procedures are available elsewhere.28
Oral health examinations within SDS are made by dentists or dental therapists operating using standard epidemiologic criteria, as outlined by the World Health Organization.29 Data were made available as a by-product of standard service delivery with examinations conducted by a large number of dentists, hygienists, and therapists across Australia. Disease prevalence was defined as the presence of one or more teeth with decay into the dentine, that were filled as a result of decay, or that had been extracted because of decay. Disease experience was recorded as a count of the total number of decayed, missing, or filled teeth, designated as “dmft” in the deciduous dentition (baby teeth) and “DMFT” in the permanent dentition. Because of the many dental staff operating in SDSs around Australia, it is not possible to calibrate examiners; however, dental staff generally receive similar training and operate under similar conditions that would lead to a reduction in any possible systematic bias.
The level of fluoride in the water was obtained from a database maintained at the Australian Research Centre for Population Oral Health and kept updated by regular communication with relevant authorities and organizations in Australia's states and territories. The optimum concentration of fluoride in the water is considered to be approximately one part per million (ppm), although this varies slightly according to mean daily temperatures within a region. Fluoride concentrations for this study were categorized as negligible (0.0–0.29 ppm), suboptimal (0.3–0.69 ppm), or optimal (≥0.7 ppm). In Australia some remote areas have higher levels of naturally occurring fluoride in the water (>1.5 ppm) and these were included in the optimal category. Only a small percentage of children in Australia do not have access to tap water.
Remoteness and SES were assessed using national area-based indices. The rural, remote, and metropolitan areas (RRMA) classification was used to determine the remoteness of the location in which a child lived.30 For this analysis, possible classifications of residence were metropolitan, rural, or remote. Area-based SES was assigned using the socioeconomic indices for areas (SEIFA) index of relative socioeconomic disadvantage (IRSD), which is computed from a selection of 20 indicators of SES obtained from the Australian Census of Population and Housing.31 High values on the SEIFA IRSD occur when an area has few families of low income and few people with little training and in unskilled occupations; low values on the index occur when the area has many low-income families and people with little training and who are in unskilled occupations. All indices were matched on the postcode of residence of each child sampled or, if this information was not available, the postcode of the dental clinic to which the child attended. IRSD values were categorized as low SES (<955.0), low–mid SES (955.01–995.0), mid–high SES (995.01–1,030.0), and high SES (≥1,030.01).
Analytic plan
Data were weighted both within each state and territory by probability of selection and by time since last visit, and across each state and territory by the 5- to 14-year-old resident estimated population obtained from the Australian Bureau of Statistics (ABS). Weighting by time since last visit was used so that children on longer recall intervals for a dental examination, who generally have less dental disease, were not underrepresented in the analysis. Many SDSs in Australia have shorter recall intervals for children considered to be at risk or who have more extensive disease experiences, and longer recall intervals for children considered to be not at risk. Recall intervals can vary from a few months to two or more years. Therefore, in any one year, there is an overrepresentation of dental visits from high-risk compared with low-risk children. Overall, the weighting procedure was designed to produce representative estimates on children enrolled (but not necessarily receiving examinations) in SDSs across Australia in 2002.
The significance of differences in caries experience (dmft and DMFT) between optimally fluoridated and non-fluoridated areas was tested for each age year using analysis of variance and F tests, while differences in caries prevalence were tested using Pearson Chi-square tests. Because of the non-normal distribution of dmft and DMFT scores, Poisson log-linear regression modeling was used to test for the significance of the effect of water fluoridation on caries experience after controlling for child age, socioeconomic disadvantage, and residential remoteness. Modeling used a hybrid Fisher/Newton-Raphson parameter estimation method and Huber (sandwich) covariance matrices to compute standard errors, p-values, and 95% confidence intervals (CIs). Estimated marginal means were calculated for water fluoridation categories after adjusting for other variables in the model. Finally, logistic regression models were fitted for caries prevalence in both the deciduous and permanent dentition, also controlling for child age, socioeconomic disadvantage, and residential remoteness. Wald F scores were used to determine statistical significance, and odds ratios (ORs) and 95% CIs were also computed. All analyses were conducted using SPSS® version 17.32
RESULTS
Oral health data were available on 128,990 children aged 5 to 15 years. There was missing information on the water fluoridation status of 3,000 children (2.3%). Because only a small percentage of the weighted number of children (3,069; 2.4%) were categorized as residing in areas with suboptimal water fluoride concentrations (0.3–0.69 ppm), these children were excluded from the analyses, leaving an unweighted total of 111,576 children.
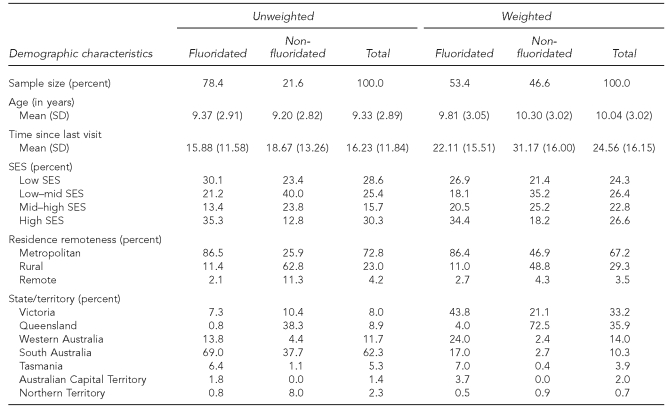
In all, 46.6% of children in the study resided in areas with negligible fluoride in the water, while 53.4% of children resided in optimally fluoridated areas (Table 1). Differences between fluoridated and non-fluoridated areas in the age of children, time since last visit, distribution of SES, residence remoteness, and state/territory of residence are shown for both the unweighted and weighted sample. Weighting the sample resulted in an overall change to the distribution of the various variables as well as changes in the distribution across fluoridated and non-fluoridated areas.
Table 1.
Weighted and unweighted sample descriptive statistics for fluoridated and non-fluoridated areas in Australia, 2002
SD = standard deviation
SES = socioeconomic status
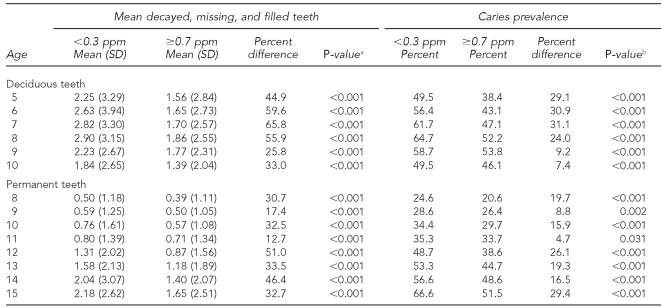
Dental caries prevalence and experience by water fluoridation status for all age groups is shown in Table 2. In both the deciduous and permanent dentition, and for all age groups, children who lived in areas with negligible fluoride concentrations (<0.3 ppm) had more decayed, missing, and filled teeth than did children who lived in areas with optimal fluoride concentrations (≥0.7 ppm). Differences for all age groups were statistically significant and ranged from 25.8% to 65.8% in the deciduous dentition, and from 12.7% to 51.0% in the permanent dentition. Caries prevalence was greater for children living in non-fluoridated areas for all age groups in both the deciduous and permanent dentitions. In the deciduous dentition, the caries prevalence for children living in non-fluoridated areas was between 7.4% and 31.1% higher than that of children living in optimally fluoridated areas. In the permanent dentition, the differences ranged from 4.7% to 29.4% higher.
Table 2.
Caries prevalence and mean number of decayed, missing, and filled teeth of 5- to 15-year-old children in Australia, by water fluoridation status, age, and dentition, 2002
aAnalysis of variance F test
bPearson Chi-square test
PPM = parts per million
SD = standard deviation
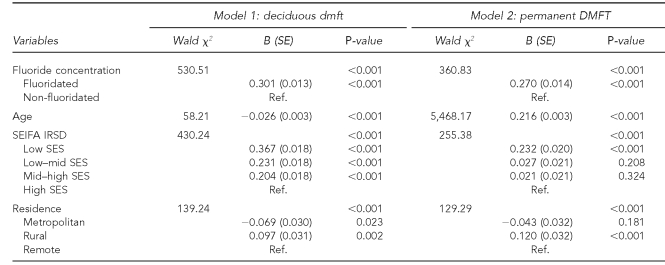
Poisson log-linear regression modeling was used to test for the significance of the association between water fluoride concentration and dental disease after controlling for child age, residential location, and area SES (Table 3). Despite age, SES, and remoteness all having statistically significant associations with child caries experience, fluoride concentration in the water remained a statistically significant predictor of child dental disease. Adjusted (estimated marginal) mean caries experience was computed for both fluoride concentration groups for deciduous and permanent dentition. The mean dmft of 5- to 10-year-old children residing in optimally fluoridated areas (mean = 1.81, 95% CI 1.77, 1.86) was significantly lower than the mean dmft of comparably aged children residing in areas with negligible fluoride in the public water (mean 5 2.33, 95% CI 2.28, 2.38). The absolute magnitude of difference was 0.52 dmft, while the relative difference was 28.7%. In the permanent dentition, the absolute magnitude of difference between the DMFT of 8- to 15-year-old children residing in areas with negligible fluoride (mean 5 1.04, 95% CI 1.01, 1.06) and those residing in optimally fluoridated areas (mean = 0.79, 95% CI 0.77, 0.82) was 0.25, and this represented a relative difference of 31.6%.
Table 3.
Poisson log-linear regression models of water fluoridation status, age, SES, and residential location on deciduous dmft and permanent DMFT in a study of 5- to 15-year-old children in Australia, 2002
SES = socioeconomic status
dmft = decayed, missing, or filled teeth (deciduous teeth)
DMFT = decayed, missing, or filled teeth (permanent teeth)
SE = standard error
Ref. = referent group
SEIFA = socioeconomic indices for areas
IRSD = index of relative socioeconomic disadvantage
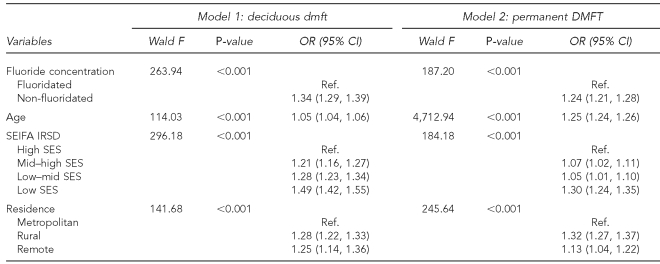
Prevalence of caries experience was modeled for each dentition using binary logistic regression analysis (Table 4). In both multivariate models, water fluoridation status was statistically significant after controlling for the other independent variables. Children living in areas with a negligible fluoride concentration in the public water supply had 1.34 times the odds of having at least one decayed, missing, or filled deciduous tooth compared with children living in optimally fluoridated areas. In the permanent dentition, children living in non-fluoridated or low-fluoride areas had 1.24 times the odds of having at least one DMFT compared with children in optimally fluoridated areas.
Table 4.
Logistic regression models of water fluoridation status, age, SES, and residential location on deciduous and permanent caries prevalence
SES = socioeconomic status
dmft = decayed, missing, or filled teeth (deciduous teeth)
DMFT = decayed, missing, or filled teeth (permanent teeth)
OR = odds ratio
CI = confidence interval
Ref. = referent group
SEIFA = socioeconomic indices for areas
IRSD = index of relative socioeconomic disadvantage
DISCUSSION
This study found a strong and consistent pattern of results indicating that children residing in areas with ≥0.7 ppm fluoride in the water supplies had both lower caries prevalence and lower caries experience. These associations were statistically significant after controlling for the child's age, the SES of the area in which the child lived, and the remoteness of the child's residential location.
Although water fluoridation was associated with a substantial 29% reduction in deciduous caries experience and a 32% reduction in permanent caries experience across all age groups, these differences are somewhat lower than the 40% to 60% reductions sometimes cited in relation to water fluoridation.33 Certainly, some studies have found for specific age groups up to a 55% reduction in deciduous surface-level caries and a 65% reduction in permanent surface-level caries.34 In a recent study conducted in a smaller population group in South Australia, >50% lifetime exposure to fluoridated water in children between birth and age 3 years was associated with 0.4 times the odds of having caries compared with children with no exposure to fluoridated water.35
One explanation for the discrepancy of the results of this study with those of some other studies is that this study did not ascertain individual-level exposure to fluoridated water. It is quite likely that many children residing in fluoridated areas have lived part of their lives in non-fluoridated areas, and vice versa. Residential mobility in Australia, as in many countries, is increasingly common. Indeed, lacking individual exposure data, the results of ecological or community-level data, such as those conducted in this study, are always more likely to be attenuated. Some of the children assumed to have lived all their lives in a non-fluoridated area will have spent time in—and therefore obtained the benefits from—a fluoridated area, while some children assumed to have spent all their lives in a fluoridated area may have spent part of their childhood in a non-fluoridated area, where no benefit from fluoridation would be obtained. Another explanation for the lower effect sizes in this study is that in contrast to earlier studies from the 1950s and 1960s, other fluoride vehicles (e.g., fluoridated toothpaste) are now widespread, and caries experience is much lower, so the benefits of water fluoridation are somewhat muted compared with the era of low fluoride exposure and very high disease prevalence.
The results of the study have varying relevance to individual Australian states and territories. In states such as New South Wales, Western Australia, and Tasmania as well as the Australian Capital Territory, community water fluoridation is already widespread and benefiting more than 90% of the population.8 However, there are still many rural areas in states such as South Australia and Victoria that have not received water fluoridation, and the recent introduction of water fluoridation into Queensland is only aimed at communities of a certain population size. Given the considerable benefit of water fluoridation still found to occur, it might be time to reassess the financial and health benefits that might be achieved by extending water fluoridation coverage in those states and territories where a large number of adults and children still do not have access to fluoridated water.
Researchers typically avoid the community-level approach adopted in this study because it fails to control for a number of individual-level factors that may also be related to caries experience. In addition, and as mentioned previously, individual exposure to fluoride in water cannot be determined. If children's consumption of fluoridated water is low or other mitigating circumstances are present, then the actual benefit or efficacy of water fluoridation might not translate into any practical benefit. Therefore, it is telling that despite variations in residential mobility, the distribution of fluoride-containing foods and beverages into non-fluoridated areas (termed the “halo effect”), and reduced exposure to fluoridated water in fluoridated areas caused by the inevitable consumption of non-fluoridated beverages, the community or practical effectiveness of water fluoridation found in this study remains high.
The lack of individual-level information on other fluoride exposures might seem to pose a question regarding the validity of this study's results because it is possible that there are other differences between the two populations that might explain the differences in caries experience between children in fluoridated and non-fluoridated areas. However, there is no reason to believe that children living in fluoridated areas have a greater use of other fluoride products than do children living in non-fluoridated areas. Indeed, analyses conducted in Australia have found very little difference in exposure to discretionary fluorides such as toothpaste and mouthwash between children from fluoridated and non-fluoridated areas.36,37 There are also few differences in terms of treatment experience, as all children in this study were treated by the SDSs that cover Australia's states and territories.
Opponents of water fluoridation regularly make ecological or community-level comparisons in an attempt to portray water fluoridation as being ineffective. This portrayal may take the form of comparing caries experience in a single selected non-fluoridated area to the caries prevalence in another purposefully selected fluoridated area. Whereas this strategy is self-serving and lacks scientific merit, the approach adopted in this study was to examine differences in child oral health across the totality of fluoridated and non-fluoridated areas in Australia where information was available. However, there is a considerable double standard when it comes to the evaluation of data on the effectiveness of water fluoridation by some water fluoridation opponents. Colquhoun,38 for example, dismisses a study by Brunelle and Carlos18 as being seriously flawed because no statistical analyses were performed. Yet, an article by Diesendorf22 that relies on an “eyeball” comparison of fluoridated and non-fluoridated areas is promoted as a legitimate study showing no relation between water fluoridation and tooth decay.38 Such tactics exemplify the numerous misleading and manipulative arguments put forward by some opponents of water fluoridation.39 However, this study represents one of the largest and most comprehensive community-level studies of the effectiveness of water fluoridation ever conducted and should help to refute claims that there is no difference in children's dental disease between fluoridated and non-fluoridated areas.
CONCLUSIONS
This study documents that Australian children living in areas with ≥0.7 ppm fluoride in the water have significantly lower caries experience and caries prevalence than their same-aged counterparts residing in areas with no or minimal concentrations of fluoride in the water. Effects were observed for every age group in both the deciduous and permanent dentition. Associations between fluoride concentration in the water supply and dental disease were significant after controlling for child age, residential location, and the socioeconomic characteristics of the area in which the children resided.
This study adds to an ever-growing evidence base on the effectiveness of water fluoridation. Ultimately, it is necessary that public health officials, researchers, and those in the medical profession can point to lower disease rates in communities with water fluoridation than in those communities without water fluoridation, despite various attenuating factors that may be in operation. It is anticipated that those areas that have yet to implement water fluoridation because of the belief that it is no longer effective will face mounting pressure to change their position in the years to come as scientific evidence of effectiveness continues to be demonstrated.
REFERENCES
- 1.Pahel BT, Rozier RG, Slade GD. Parental perceptions of children's oral health: the Early Childhood Oral Health Impact Scale (ECOHIS) Health Qual Life Outcomes. 2007;5:6. doi: 10.1186/1477-7525-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Slade GD, Spencer AJ. Development and evaluation of the Oral Health Impact Profile. Community Dent Health. 1994;11:3–11. [PubMed] [Google Scholar]
- 3.Slade GD, Nuttall N, Sanders AE, Steele JG, Allen PF, Lahti S. Impacts of oral disorders in the United Kingdom and Australia. Br Dent J. 2005;198:489–93. doi: 10.1038/sj.bdj.4812252. [DOI] [PubMed] [Google Scholar]
- 4.Australian Institute of Health and Welfare. Health expenditure Australia 2005–06. Canberra: Australian Institute of Health and Welfare; 2007. [Google Scholar]
- 5.Mount GJ, Hume WR. Preservation and restoration of tooth structure. 2nd ed. Brighton (Australia): Knowledge Books and Software; 2005. [Google Scholar]
- 6.McDonagh M, Whiting P, Bradley E, Cooper C, Sutton A, Chestnutt I, et al. A systematic review of public water fluoridation. University of York Centre for Reviews and Dissemination. York (England): York Publishing Services; 2000. [Google Scholar]
- 7.Ten great public health achievements—United States, 1900–1999. MMWR Morb Mortal Wkly Rep. 1999;48(12):241–3. [PubMed] [Google Scholar]
- 8.Armfield JM. The extent of water fluoridation coverage in Australia. Aust N Z J Public Health. 2006;30:581–2. doi: 10.1111/j.1467-842x.2006.tb00794.x. [DOI] [PubMed] [Google Scholar]
- 9.Benjamin RM. Oral health: the silent epidemic. Public Health Rep. 2010;125:158–9. doi: 10.1177/003335491012500202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Farkas EJ. Water fluoridation in eleven countries. Soc Sci Med. 1982;16:2155–8. [Google Scholar]
- 11.Australian Government Department of the Environment, Water, Heritage and the Arts. Fluoride compounds: health effects. [cited 2010 Apr 29]. Available from: URL: http://www.npi.gov.au/substances/fluoride-compounds/health.html.
- 12.Armfield JM. Public water fluoridation and dental health in New South Wales. Aust N Z J Public Health. 2005;29:477–83. doi: 10.1111/j.1467-842x.2005.tb00230.x. [DOI] [PubMed] [Google Scholar]
- 13.Lee M, Dennison PJ. Water fluoridation and dental caries in 5- and 12-year-old children from Canterbury and Wellington. N Z Dent J. 2004;100:10–5. [PubMed] [Google Scholar]
- 14.Jones C, Taylor G, Woods K, Whittle G, Evans D, Young P. Jarman underprivileged area scores, tooth decay and the effect of water fluoridation. Community Dent Health. 1997;14:156–60. [PubMed] [Google Scholar]
- 15.Riley JC, Lennon MA, Ellwood RP. The effect of water fluoridation and social inequalities on dental caries in 5-year-old children. Int J Epidemiol. 1999;28:300–5. doi: 10.1093/ije/28.2.300. [DOI] [PubMed] [Google Scholar]
- 16.Diesendorf M, Colquhoun J, Spittle B. Fluoridation and bones: authors' response to critics. Aust N Z J Public Health. 1998;22:165–7. [PubMed] [Google Scholar]
- 17.Yiamouyiannis JA. Water fluoridation and tooth decay: results from the 1986-1987 national survey of U.S. schoolchildren. Fluoride. 1990;23:55–67. [Google Scholar]
- 18.Brunelle JA, Carlos JP. Recent trends in dental caries in U.S. children and the effect of water fluoridation. J Dent Res. 1990;69 doi: 10.1177/00220345900690S141. Spec No:723-7. [DOI] [PubMed] [Google Scholar]
- 19.Colquhoun J. New evidence on fluoridation. Soc Sci Med. 1984;19:1239–46. doi: 10.1016/0277-9536(84)90377-0. [DOI] [PubMed] [Google Scholar]
- 20.Colquhoun J. Fluorides and the decline of tooth decay in New Zealand. Fluoride. 1993;26:125–34. [Google Scholar]
- 21.Diesendorf M. A re-examination of Australian fluoridation trials. Search. 1986;17:256–62. [Google Scholar]
- 22.Diesendorf M. The mystery of declining tooth decay. Nature. 1986;322:125–9. doi: 10.1038/322125a0. [DOI] [PubMed] [Google Scholar]
- 23.Diesendorf M. Have the benefits of water fluoridation been overestimated? Int Clin Nutr Rev. 1990;10:292–303. [Google Scholar]
- 24.Gray AS. Fluoridation. Time for a new base line? J Can Dent Assoc. 1987;53:763–5. [PubMed] [Google Scholar]
- 25.Teotia SPS, Teotia M. Dental caries: a disorder of high fluoride and low dietary calcium interactions (30 years of personal research) Fluoride. 1994;27:59–66. [Google Scholar]
- 26.Ziegelbecker RC, Ziegelbecker R. WHO data on dental caries and natural water fluoride levels. Fluoride. 1993;26:263–6. [Google Scholar]
- 27.Armfield JM, Roberts-Thomson KF, Spencer AJ. The Child Dental Health Survey, Australia 1999: trends across the 1990s. Canberra: Australian Institute of Health and Welfare; 2003. [Google Scholar]
- 28.Armfield JM, Slade GD, Spencer AJ. Water fluoridation and children's dental health: the Child Dental Health Survey, Australia 2002. Canberra: Australian Institute of Health and Welfare; 2007. [Google Scholar]
- 29.World Health Organization. Oral health surveys—basic methods. 4th ed. Geneva: WHO; 1997. [Google Scholar]
- 30.Department of Primary Industries and Energy, Department of Human Services and Health. Rural, remote and metropolitan areas classification 1991 Census edition. Canberra: Australian Government Publishing Service; 1994. [Google Scholar]
- 31.Australian Bureau of Statistics. Information paper—an introduction to socio-economic indexes for areas (SEIFA), 2006. ABS catalogue no. 2039.0. Canberra: ABS; 2008. [Google Scholar]
- 32.SPSS, Inc. SPSS® Version 17.0 for Windows. Chicago: SPSS, Inc; 2008. [Google Scholar]
- 33.Horowitz HS. The effectiveness of community water fluoridation in the United States. J Public Health Dent. 1996;56(5 Spec No):253–8. doi: 10.1111/j.1752-7325.1996.tb02448.x. [DOI] [PubMed] [Google Scholar]
- 34.Slade GD, Spencer AJ, Davies MJ, Stewart JF. Caries experience among children in fluoridated Townsville and unfluoridated Brisbane. Aust N Z J Public Health. 1996;20:623–9. doi: 10.1111/j.1467-842x.1996.tb01077.x. [DOI] [PubMed] [Google Scholar]
- 35.Do LG, Spencer AJ. Risk-benefit balance in the use of fluoride among young children. J Dent Res. 2007;86:723–8. doi: 10.1177/154405910708600807. [DOI] [PubMed] [Google Scholar]
- 36.Armfield JM, Spencer AJ, Slade GD. Consumption of non-fluoridated water and compensatory use of discretionary fluorides. Paper presented at the 38th Annual Scientific Meeting of the International Association of Dental Research (Australian – New Zealand Division); 1998 Sep 27–29; Brisbane, Australia. [Google Scholar]
- 37.Armfield JM, Spencer AJ, Roberts-Thomson KF. Compensatory discretionary fluoride use among children not consuming fluoridated water. Paper presented at the Ninth World Congress on Preventive Dentistry; 2009 Sep 7-10; Phuket, Thailand. [Google Scholar]
- 38.Colquhoun J. Why I changed my mind about water fluoridation. Fluoride. 1998;31:103–18. doi: 10.1353/pbm.1997.0017. [DOI] [PubMed] [Google Scholar]
- 39.Armfield JM. When public action undermines public health: a critical examination of antifluoridationist literature. Aust New Zealand Health Policy. 2007;4:25. doi: 10.1186/1743-8462-4-25. [DOI] [PMC free article] [PubMed] [Google Scholar]