SYNOPSIS
Objectives
This study examined whether the association between obesity and 12-month prevalence of major depressive disorder (MDD) varied according to racial/ethnic status and nativity in representative national samples of black, Latino, Asian, and non-Hispanic white people.
Methods
We used data from the Comprehensive Psychiatric Epidemiology Surveys.
Results
In analyses by gender, obesity was associated with an elevated risk of MDD among non-Hispanic white women (adjusted odds ratio [AOR] =1.73; 95% confidence interval [CI] 1.27, 2.35; p=0.001). Formal test for interaction revealed significant variation by race present between non-Hispanic white women and black, Latin, and Asian women. No significant differences were evident among men. In analyses by nativity, the association between obesity and MDD was significant among U.S.-born non-Hispanic white women (AOR=1.62; 95% CI 1.16, 2.27; p=0.001) and U.S.-born black women (AOR=1.29; 95% CI 1.01, 1.66; p=0.041). Significant interactions were present among U.S.-born white and black women, Latin women, and Asian women. No significant interactions were evident among foreign-born women. Similarly, no significant differences were present among native-born or foreign-born men.
Conclusions
The findings suggest that the association between obesity and MDD varies according to racial/ethnic status and nativity. Understanding the link between obesity and depression may be imperative to designing interventions to address body weight maintenance and reduction strategies among women.
Obesity is a major public health concern in the United States, with its overall prevalence in the adult population increasing during the past decade.1 While obesity is a serious health issue by itself, it is also associated with other health problems, including psychiatric illnesses. Previous studies suggest that obesity may be significantly associated with major depressive disorder (MDD).2–10 A unique set of paradoxical findings arises when we examine how obesity and depression are associated with each other among different racial/ethnic groups.
The prevalence of obesity varies by race/ethnicity as well as gender. Specifically, the prevalence of obesity is highest (in order of prevalence) among black, Latino, white, and Asian populations.11 Because some racial/ethnic groups have higher rates of obesity than white people and obesity may be a risk factor for psychiatric illnesses, we might expect that obese individuals within these groups, especially black and Latino minority groups, would have higher rates of depression than white people. However, this may not be the case. Research findings suggest that compared with non-Hispanic white people, black, Latino, and Asian minority groups have lower 12-month rates of MDD.11–15 Despite the lower prevalence, black, Latino, and Asian minority populations affected by MDD are less likely to receive treatment and are more likely to be severely and chronically impaired by MDD than non-Hispanic white people.13,15,16
While obesity is a serious health issue by itself, it is also associated with other health problems, including psychiatric illnesses. The literature on the association between obesity and depression has been inconsistent, with most, but not all,17,18 studies suggesting a positive association.2–10,19,20
Despite the higher prevalence of obesity among some racial/ethnic groups, our understanding of the obesity-depression association among these groups is limited in the following ways. First, previous studies often have not specifically examined the association between obesity and depression among racial/ethnic groups.2,3,5,8,9,19 This is largely a function of insufficient numbers of racial/ethnic group members in survey data that result in pooled sample methods by which all racial groups are examined together. Although pooled sample analyses estimate outcomes fairly well, they may not flesh out subtle and significant differences between racial/ethnic groups. This limits the conclusions that may be drawn based on race/ethnicity.21
Second, in studies that have examined whether the association between obesity and MDD varies by racial/ethnic status, the association remains inconclusive. Carpenter et al.10 reported on data from a national survey of black and white adults and found that obesity was significantly associated with past-year Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) major depression among women. The association between body weight and major depression was comparable for black and white women. Heo and colleagues6 used data from a nationally representative sample of white, black, and Hispanic adults, and reported that among women, the prevalence of past month depressed mood increased in obese people regardless of race. However, using data from the National Comorbidity Survey Replication (NCS-R), Simon and colleagues7 found the association between obesity and lifetime mood disorder was significant among non-Hispanic white compared with nonwhite people. Specifically, in a formal test for interaction, there was a borderline significant difference in the odds ratios between non-Hispanic white and nonwhite people. A possible explanation for the contradictory results could be that racial differences were difficult to detect because of insufficient numbers of racial/ethnic minorities compared with non-Hispanic white people. For example, non-Hispanic white people comprised between 73% and 88% of the sample in previously noted studies. Although studies were able to conduct analyses separately for African Americans and Hispanic people,6,7,10 racial/ethnic groups that were included in these studies were underrepresented compared with their numbers in the U.S. population.22
Third, there is increasing recognition that nativity status is an important indicator of variation in body mass index (BMI) and mental health outcomes among racial/ethnic groups. Findings from the National Health Interview Surveys (NHISs) suggest that U.S.-born adults have a greater prevalence of obesity than foreign-born adults.23,24 Furthermore, U.S.-born black women were twice as likely to be obese compared with U.S.-born white women.23 Studies have also shown that among foreign-born samples of Asian and Latino populations, the number of years spent in the U.S. was directly related to an increased risk of being overweight or obese.16,25 In addition, previous mental health research on black, Latino, and Asian populations suggests that aspects of nativity and the immigrant experience are associated with MDD.26–31 For example, various aspects of nativity, such as family burden, cultural conflict, and perceived neighborhood safety, have been shown to be associated with 12-month MDD.29 To our knowledge, there are no previous studies that have examined the role of nativity in the association between obesity and MDD.
In the present study, we used data from the Collaborative Psychiatric Epidemiology Studies (CPES) to investigate whether the association between obesity and 12-month prevalence of MDD varies according to racial/ethnic status or nativity in nationally representative samples of black, Latino, Asian, and non-Hispanic white people.
METHODS
Sampling design
A detailed description of the CPES protocol and sampling design has been previously documented.32 Briefly, three national surveys of Americans' mental health comprise the CPES: the NCS-R,33 the National Study of American Life (NSAL),34 and the National Latino and Asian American Study of Mental Health (NLAAS).35 Participants were recruited using two sampling methods: (1) core sampling based on multistage stratified area probability designs, resulting in nationally representative household samples; and (2) high-density supplemental sampling to oversample Census block groups for target ancestry groups (Afro-Caribbean, Chinese, Filipino, Vietnamese, and Puerto Rican).
The combined analysis weights were created from the analysis weights for each study. First, population-specific weights from each study were adjusted to the 2002 Current Population Survey (CPS) totals. Second, each study was partitioned into subgroups by race and geographic region within the U.S. To create the combined analysis weights, the adjusted study-specific weights were scaled by relative size of the study subgroup to the combined subgroup across all three studies.36
Procedures
The NCS-R, NSAL, and NLAAS interviews were conducted in English and administered face-to-face using a computer-assisted instrument and by telephone.19,20,28 When requested, NLAAS interviews were conducted in the respondents' native language (e.g., Spanish, Chinese, Tagalog, or Vietnamese).28,37 CPES surveys were conducted between February 2001 and December 2003. Written informed consent was obtained for all participants in their preferred languages, and study procedures and protocols were approved by the Internal Review Boards of Cambridge Health Alliance, the University of Washington, the University of Michigan, and Harvard Medical School.27,28,33,37
Sample
The full CPES sample included data from 20,013 adults aged 18 and older who resided in any of the 50 contiguous states and Washington, D.C. The NCS-R sample consisted of 6,696 non-Hispanic white, 1,230 black, 883 Latino, and 189 Asian people. The NSAL sample consisted of 3,570 African American, 1,621 black of Caribbean ancestry, and 891 non-Hispanic white people.27 The NLAAS Latino sample consisted of 868 Mexican, 495 Puerto Rican, 577 Cuban, and 614 “other” Latino people.37 The NLAAS Asian sample comprised 2,095 individuals including 600 Chinese, 508 Filipino, 520 Vietnamese, and 467 “other” Asian people.28 The final response rates for the surveys were as follows: 70.9% (NCS-R), 72.3% (NSAL), and 73.2% (NLAAS).
The final sample included 16,450 respondents (with complete information on all variables in the analyses) who self-identified as non-Hispanic white (n=5,691), black (n=5,434), Latino (n=3,268), and Asian (n=2,057).
Measures
The outcome of interest in our study was the 12-month prevalence (the occurrence of the depressive event within 12 months of the interview) of MDD as measured by the diagnostic interview of the World Mental Health Initiative version of the Composite International Diagnostic Interview,38 a fully structured diagnostic instrument based on criteria of the DSM-IV.39 Previous studies have shown that there are consistent similarities in the core features of MDD across racial/ethnic groups.40,41 To date, clinical reappraisal interviews have been conducted in conjunction with the NCS-R and the NSAL. The Structured Clinical Interview of DSM-IV (SCID),42 a diagnostic interview that requires clinical expertise to administer, was used in the reappraisal studies. Because the SCID does not contain a diagnosis for mania, it cannot be used to generate diagnoses for MDD. However, it can be used to diagnose major depressive episode (MDE). For example, in the NSAL, a comparison of the Composite International Diagnostic Interview and the SCID for 12-month prevalence of MDE revealed fair concordance for African Americans and lower concordance for Caribbean black people.15 The clinical reappraisal study for the NCS-R also indicated fair concordance for 12-month MDE.12
Obesity
Obesity was determined from self-reports of height and weight. Respondents were classified as either obese (BMI ≥30 kilograms/meter squared [kg/m2]) or non-obese (BMI 18.5–29.9 kg/m2) both for consistency with previous research2,7,20 and a lack of evidence suggesting that overweight status is statistically associated with depression.4,5,9,17,18 In addition, the goal of this study was to examine the relationship between 12-month MDD and obesity, and the low prevalence of 12-month MDD among racial/ethnic groups precludes further subdivision of the non-obese group. Earlier research suggests that self-reported height and weight are highly correlated with direct physical measurements, but self-reported data result in underestimation of weight and overestimation of height,43 leading to low estimates of overweight and obesity.7 Individuals with BMI <18.5 kg/m2 (n=477) were excluded from the analyses because research has shown a U-shaped relationship between BMI and the prevalence of mood disorders.10
Covariates
In the present study, we adjusted for age, marital status, educational attainment, employment status, and current smoking status. Although aging is correlated with both MDD and BMI, all age groups were included in the analysis because evidence suggests that age moderates the association between obesity and depression, such that there is a stronger association between obesity and depression among those younger than 65 years of age.6 Age (measured in years) was assessed as a continuous variable based on the date of the interview and self-reported date of birth.
Married individuals have consistently been shown to have a lower prevalence of MDD than those who are unmarried.44,45 Marital status was dichotomized: married or cohabitating vs. not married (widowed/separated/divorced/never married). Given the gender differences in the obesity-depression relationship and increased risk of 12-month MDD among women with ≥16 years of education,46 educational attainment (measured in years) was treated as a dichotomized variable based on self-reported number of years of education (≥16 years vs.<16 years).
With few exceptions, being unemployed and out of the labor force, compared with being employed, is consistently associated with a higher risk of 12-month MDD.46 Employment status was dichotomized: being employed vs. being unemployed (includes being out of the labor force). In line with previous findings that current smoking is associated with MDD47,48 and smoking initiation,49 current smoking was dichotomized: current smoker vs. nonsmoker (never smoked, previously smoked).
Analysis
All analyses used SVY LOGISTIC procedure of STATA® version 10.0, which provides estimates that account for the incorporation of complex survey sampling methods, including multistage and cluster study designs.50 Weighted cross-tabulations were used to describe characteristics of the CPES data. Prior to conducting the multivariate analysis, we assessed the variation in 12-month MDD prevalence by obesity status for a variety of sociodemographic characteristics, as well as the bivariate association between obesity and the 12-month MDD. Next, a series of logistic regression analyses were conducted to assess the unadjusted and adjusted association between obesity and 12-month MDD stratified by gender. Interaction terms between obesity and race were created, and included obesity and black, obesity and Latino, obesity and Asian, and obesity and non-Hispanic white. These interaction terms were included in the unadjusted and adjusted models to determine whether the obesity-depression association varied according to racial/ethnic status. Wald tests were conducted to determine whether there were statistically significant differences in the association between obesity and MDD by race.
RESULTS
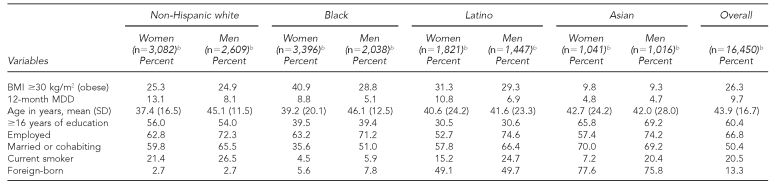
Table 1 shows the sociodemographic characteristics of the sample stratified by gender and race. As expected, women reported a higher prevalence of 12-month MDD than men, except among Asian populations. Among racial/ethnic groups, both men and women reported a similar prevalence of obesity, except among black people; black women were more likely to report BMIs ≥30 kg/m2.
Table 1.
Descriptive statisticsa for study variables stratified by race/ethnicity, Comprehensive Psychiatric Epidemiology Surveys
aData are presented as percentage of respondents unless otherwise indicated.
bSample size numbers reflect actual number of respondents; all percentages are weighted and incorporate sampling weights.
BMI = body mass index
kg/m2 = kilograms per meter squared
MDD = major depressive disorder
SD = standard deviation
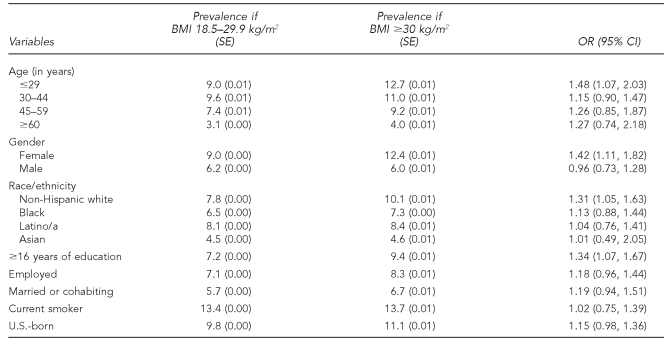
Table 2 shows the variation in the 12-month prevalence of MDD with obesity by a range of sociodemographic characteristics. Column 3 of Table 2 gives the unadjusted odds ratios comparing the prevalence of 12-month MDD among the BMI ≥30 kg/m2 group relative to the non-obese group (BMI 18.5–29.9 kg/m2). Obesity was significantly associated with higher odds of 12-month MDD among respondents ≤29 years of age (odds ratio [OR] = 1.48; 95% confidence interval [CI] 1.07, 2.03) and among women (OR=1.42; 95% CI 1.11, 1.82). Other subgroups where obesity was significantly associated with increased MDD were non-Hispanic white people (OR=1.31; 95% CI 1.05, 1.63) and those with ≥16 years of education (OR=1.34; 95% CI 1.07, 1.67).
Table 2.
Twelve-month prevalencea of MDD by obesity status stratified by sociodemographic characteristics, Comprehensive Psychiatric Epidemiology Surveys
aAll proportions are weighted and incorporate sampling weights.
MDD = major depressive disorder
BMI = body mass index
kg/m2 = kilograms per meter squared
SE = standard error
OR = odds ratio
CI = confidence interval
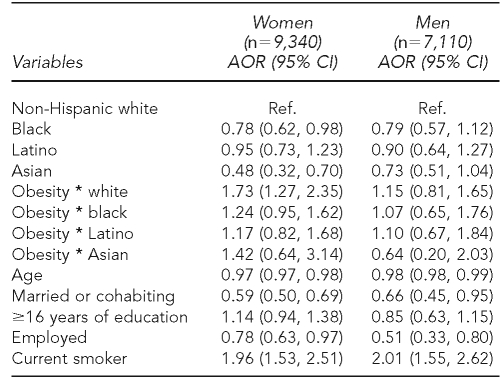
In Table 3, we examined whether race moderated the association between obesity and 12-month MDD among black, Latino, and Asian populations compared with the non-Hispanic white group. In the fully adjusted models, the association between obesity and 12-month MDD was significant only among white women (adjusted odds ratio [AOR] = 1.73; 95% CI 1.27, 2.35). A formal test for an interaction effect found significant variation by race between non-Hispanic white and black women (p=0.004), white women and Latinas (p=0.004), and white and Asian women (p=0.03). No statistically significant associations were evident between obesity and 12-month MDD by race among men.
Table 3.
Results from logistic regression of obesity on 12-month MDD by race/ethnicity among women and men in the Comprehensive Psychiatric Epidemiology Surveys
MDD = major depressive disorder
AOR = adjusted odds ratio
CI = confidence interval
Ref. = referent group
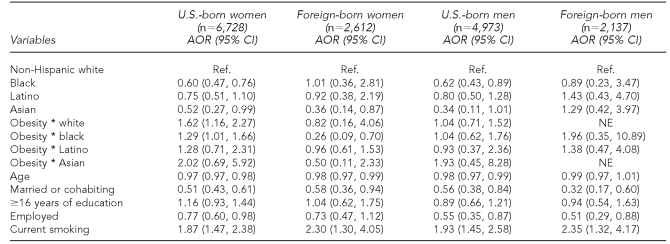
In Table 4, we examined the association between obesity and 12-month MDD among U.S.-born and foreign-born women and men. In the adjusted models, among U.S.-born women, the association between obesity and 12-month MDD was significant among U.S.-born non-Hispanic white women compared with U.S.-born nonwhite women (AOR=1.62; 95% CI 1.16, 2.27). In addition, U.S.-born black women had higher odds of experiencing 12-month MDD compared with U.S.-born nonblack women (AOR=1.29; 95% CI 1.01, 1.66). A formal test for interaction showed significant variation by race between U.S.-born non-Hispanic white and U.S.-born black women (p<0.001), U.S.-born white women and U.S.-born Latinas (p=0.03), and U.S.-born white and U.S.-born Asian women (p=0.03). Foreign-born women with BMIs ≥30 kg/m2 reported being at lower risk of 12-month MDD and, in the case of foreign-born black women, the odds of 12-month MDD were significantly lower than among foreign-born nonblack women (AOR=0.26; 95% CI 0.09, 0.70). Although the association between obesity and 12-month MDD appeared stronger among foreign-born black women, a formal test for interaction showed no significant variation (p=0.12). Again, no statistically significant associations were evident between obesity and 12-month MDD by nativity among men.
Table 4.
Results from logistic regression of obesity on 12-month MDD by race/ethnicity among U.S.-born and foreign-born women and men in the Comprehensive Psychiatric Epidemiology Surveys
MDD = major depressive disorder
AOR = adjusted odds ratio
CI = confidence interval
Ref. = referent group
NE = not estimable
DISCUSSION
In this study, we examined whether the association between obesity and the 12-month prevalence of MDD varied according to racial/ethnic status and nativity in nationally representative samples of black, Latino, Asian, and non-Hispanic white populations. Our findings suggest that racial/ethnic status moderated the association between obesity and 12-month MDD. The results indicated that non-Hispanic white women who were obese had significantly higher odds of experiencing 12-month MDD compared with black, Latina, and Asian women. We also observed an interesting variation in the relationship between obesity and depression across racial/ethnic groups. The association was stronger among non-Hispanic white women, such that significant interactions were present among non-Hispanic white and black, Latina, and Asian women. Our finding, in part, is consistent with another U.S. survey that suggested a borderline significant difference in the obesity-depression relationship between non-Hispanic white and nonwhite populations. However, unlike Simon and colleagues,7 we were able to show a significant positive association between obesity and a specific mood disorder, and that the obesity-depression relationship significantly varied across racial/ethnic groups.
Although previous studies have documented a positive association between obesity and MDD among women regardless of race,6,10 it is clear from our study that race moderates the association between obesity and MDD. Potential explanations for the divergent results may include differences in study design. The CPES is the first psychiatric epidemiologic survey that includes nationally representative samples of black Caribbean, English- and Spanish-speaking Latino, and Asian American populations.27,28,37 The inherent racial/ethnic diversity present in the CPES may have allowed us to detect subtle and significant differences in the obesity-depression relationship among racial/ethnic groups.
In this study, it is not possible to determine the mechanisms that explain the elevated risk of 12-month MDD among non-Hispanic white women relative to nonwhite women. However, previous research has proposed various underlying pathways that link obesity to depression among women. Body dissatisfaction among obese people (especially among white women) may contribute to depression.51–60 Alternatively, weight-based stigma or discrimination has been proposed as a mechanism that may result in an adverse mental health outcome.61–65 Specifically, perceived weight discrimination has been found to be significantly associated with 12-month MDD.63 Finally, obesity and depression may be linked through early-life adversity, such as childhood abuse, which is a causal factor in both obesity and depression among women.66,67
Among men, obesity was associated with an increased risk of 12-month MDD. However, the higher odds were not statistically significant. This result supports findings from another U.S. psychiatric epidemiology study that investigated the obesity-depression relationship.9 Despite our findings, other studies suggest a significant positive association between obesity and 12-month MDD among obese men.5,7 Considering that there were no statistically significant effects of the interaction between gender and obesity in the studies that found a positive significant obesity-depression relationship among men, we posit that the divergent results may be a function of differences in statistical power (due to the relatively low prevalence of depression among men across studies) rather than differences in the magnitude of the obesity-depression relationship.
We also found evidence that the obesity-depression association varied according to nativity. Our findings add to the literature and suggest that obesity is a significant risk factor for MDD only among native-born, non-Hispanic white women. This finding is interesting because there were no racial differences in the association between obesity and MDD among foreign-born women. A potential explanation as to why foreign-born individuals who are obese may not be at risk for MDD has been suggested by previous studies. A recent review article showed that foreign-born individuals in the U.S. have better health outcomes, over a range of physical conditions, than native-born Americans.68
Empirical evidence from previous studies supports this pattern. In the case of MDD, foreign-born black, Latina, and Asian women reported a lower prevalence of MDD compared with their native-born counterparts.27,28,37 Upon arrival to the U.S., female immigrants were less likely to be obese (15%) than U.S.-born females (19%). These percentages, however, are marked by group differences. Specifically, foreign-born Latinas were four percentage points less likely to be obese than their native-born counterparts, and foreign-born black women were 10 percentage points less likely to be obese than their native-born counterparts.69 Our findings provide evidence in support of the “healthy immigrant effect.” This phenomenon is generally supported in the literature and suggests that upon arrival to the U.S., immigrants are healthier than their native-born counterparts but that over time, this health advantage disappears.70
The cross-sectional nature of our data precludes us from fully examining the healthy immigrant effect. However, there is ample evidence that shows selective immigration processes may explain why immigrants, upon arrival to the U.S., are in better health than their native-born counterparts. First, healthier immigrants are more likely to enter the country either by choice or due to the U.S. immigration screening process (Unpublished report. Jasso G, Massey DS, Rosenzweig MR, Smith JP. Immigrant health—selectivity and acculturation. Santa Monica (CA): RAND Corp.; 2004). Second, unhealthy immigrants may be more likely to return to their country of origin.71 Finally, immigrants of higher socioeconomic status may be healthier, and may be more likely to remain in the U.S., while immigrants who are less healthy may be more likely to die prematurely.69
Limitations
The findings from this study should be interpreted in light of the following limitations. First, the use of cross-sectional data limited our ability to establish causal associations between obesity and MDD. Second, our analyses relied upon the World Mental Health Composite International Diagnostic Instrument to diagnose MDD. Although this diagnostic instrument has been validated in diverse community settings, we cannot rule out the possibility that the prevalence of MDD among nonwhite people may have been underestimated, especially if respondents expressed their problems in unique ways that were not identified by DSM-IV. This may be a particular issue, as culture can affect both the clinical presentation of specific psychiatric disorders and the ability to recall or report symptoms.15,35
Third, height and weight were assessed by self-report. Past methodological research suggests that self-reported height and weight are highly correlated with direct physical measurement,72–74 but self-reported measurements tend to consistently underestimate weight and overestimate height.73 We know of no evidence to suggest that underestimation of weight would affect the association between obesity and depression. Previous studies that suggest an association between obesity and depression have included self-report3–7,9,10 and actual measurements of height and weight.9,75,76
Fourth, our analyses did not consider the potential influence of previous depressive episodes on weight. Depression can be a chronic disease with remission, relapse, and recurrence.77,78 However, misclassification of depression would be expected to lessen or obscure the association between obesity and depression.19 Fifth, our analysis did not include assessments of psychotropic medication use. Medication used to manage depressive or anxiety disorders may result in weight gain.79 However, the prevalence of psychotropic medication use is more prevalent among non-Hispanic white people than among black and Latino populations.80 This suggests that psychotropic medication use would be expected to blunt the obesity-depression relationship among non-Hispanic white people.
CONCLUSIONS
Our findings complement findings from other U.S.-based psychiatric epidemiology studies that indicate that obesity is a significant risk factor for 12-month MDD among women.9 We add to this literature by suggesting that both race and nativity status moderate the obesity-depression relationship. Given the dramatic increase in obesity among the general population, and the high prevalence of obesity among certain racial/ethnic groups, our study's findings highlight the importance of interventions that not only address weight maintenance and reduction strategies, but also address the effects of MDD among obese women.
Acknowledgments
The authors thank the National Latino and Asian American Study writing group for helpful comments on earlier drafts of this article.
Footnotes
This research was supported by National Institute of Mental Health (NIMH) research grants #MH06220, #MH62207, #MH62209, #HD049142, and Robert Wood Johnson Foundation grant #DA18715, with generous support from the Substance Abuse and Mental Health Services Administration and the Office of Behavioral and Social Sciences Research (OBSSR). The National Survey of American Life was supported by NIMH #U01-MH57716 with supplemental support from the National Institutes of Health (NIH) OBSSR, the National Institute on Aging (#5R01 AG02020282), the National Institute on Drug Abuse, and the University of Michigan. Preparation of this article was also aided by grants from NIMH (#1P01 MH58565, #1T32 MH67555, and #5TMH16806). This article was also made possible by grant #1KL2RR025015-01 from the National Center for Research Resources, a component of NIH, and NIH Roadmap for Medical Research.
REFERENCES
- 1.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 2.Mather AA, Cox BJ, Enns MW, Sareen J. Associations of obesity with psychiatric disorders and suicidal behaviors in a nationally representative sample. J Psychosom Res. 2009;66:277–85. doi: 10.1016/j.jpsychores.2008.09.008. [DOI] [PubMed] [Google Scholar]
- 3.Scott KM, Bruffaerts R, Simon GE, Alonso J, Angermeyer M, de Girolamo G, et al. Obesity and mental disorders in the general population: results from the world mental health surveys. Int J Obes (Lond) 2008;32:192–200. doi: 10.1038/sj.ijo.0803701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Petry NM, Barry D, Pietrzak RH, Wagner JA. Overweight and obesity are associated with psychiatric disorders: results from the National Epidemologic Survey on Alcohol and Related Conditions. Psychosom Med. 2008;70:288–97. doi: 10.1097/PSY.0b013e3181651651. [DOI] [PubMed] [Google Scholar]
- 5.Barry D, Pietrzak RH, Petry NM. Gender differences in associations between body mass index and DSM-IV mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Ann Epidemiol. 2008;18:458–66. doi: 10.1016/j.annepidem.2007.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heo M, Peitrobelli A, Fontaine KR, Sirey JA, Faith MS. Depressive mood and obesity in US adults: comparison and moderation by sex, age, and race. Int J Obes (Lond) 2006;30:513–9. doi: 10.1038/sj.ijo.0803122. [DOI] [PubMed] [Google Scholar]
- 7.Simon GE, Von Korff M, Saunders K, Miglioretti DL, Crane PK, van Belle G, et al. Association between obesity and psychiatric disorders in the US adult population. Arch Gen Psychiatry. 2006;63:824–30. doi: 10.1001/archpsyc.63.7.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McIntyre RS, Konarski JZ, Wilkins K, Soczynska JK, Kennedy SH. Obesity in bipolar disorder and major depressive disorder: results from a national community health survey on mental health and well-being. Can J Psychiatry. 2006;51:274–80. doi: 10.1177/070674370605100502. [DOI] [PubMed] [Google Scholar]
- 9.Onyike CU, Crum RM, Lee HB, Lyketsos CG, Eaton WW. Is obesity associated with major depression? Results from the Third National Health and Nutrition Examination Survey. Am J Epidemiol. 2003;158:1139–47. doi: 10.1093/aje/kwg275. [DOI] [PubMed] [Google Scholar]
- 10.Carpenter KM, Hasin DS, Allison DB, Faith MS. Relationships between obesity and DSM-IV major depressive disorder, suicide ideation, and suicide attempts: results from a general population study. Am J Public Health. 2000;90:251–7. doi: 10.2105/ajph.90.2.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang Y, Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 12.Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 13.Breslau J, Kendler KS, Su M, Gaxiola-Aguilar S, Kessler RC. Lifetime risk and persistence of psychiatric disorder across ethnic groups in the United States. Psychol Med. 2005;35:317–27. doi: 10.1017/s0033291704003514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62:1097–106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 15.Williams DR, Gonzalez HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Arch Gen Psychiatry. 2007;64:305–15. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- 16.Alegria M, Chatterji P, Wells K, Cao Z, Chen CN, Takeuchi D, et al. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatr Serv. 2008;59:1264–72. doi: 10.1176/appi.ps.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.John U, Meyer C, Rumpf HJ, Hapke U. Relationships of psychiatric disorders with overweight and obesity in an adult general population. Obes Res. 2005;13:101–9. doi: 10.1038/oby.2005.13. [DOI] [PubMed] [Google Scholar]
- 18.Jorm AF, Korten AE, Christensen H, Jacomb PA, Rodgers B, Parslow RA. Association of obesity with anxiety, depression, and emotional well-being: a community survey. Aust N Z J Public Health. 2003;7:434–40. doi: 10.1111/j.1467-842x.2003.tb00423.x. [DOI] [PubMed] [Google Scholar]
- 19.Simon GE, Ludman EJ, Linde JA, Operskalski BH, Ichikawa L, Rohde P, et al. Association between obesity and depression in middle-aged women. Gen Hosp Psychiatry. 2008;30:32–9. doi: 10.1016/j.genhosppsych.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Scott KM, McGee MA, Wells JE, Oakley Browne MA. Obesity and mental disorders in the adult general population. J Psychosom Res. 2008;64:97–105. doi: 10.1016/j.jpsychores.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 21.Mizell CA. Life course influences on African American men's depression: adolescent parental composition, self-concept, and adult earnings. J Black Stud. 1999;29:467–90. [Google Scholar]
- 22.Census Bureau (US) State and county quickfacts. [cited 2007 Jun 4]. Available from: URL: http://quickfacts.census.gov/qfd/states/00000.html.
- 23.Barrington DS, Baquero MC, Borrell LN, Crawford ND. Racial/ethnic disparities in obesity among US-born and foreign-born adults by sex and education. Obesity (Silver Spring) 2010;18:422–4. doi: 10.1038/oby.2009.212. [DOI] [PubMed] [Google Scholar]
- 24.Goel MS, McCarthy EP, Phillips RS, Wee CC. Obesity among US immigrant subgroups by duration of residence. JAMA. 2004;292:2860–7. doi: 10.1001/jama.292.23.2860. [DOI] [PubMed] [Google Scholar]
- 25.Barcenas CG, Wilkinson AV, Strom SS, Cao Y, Saunders KC, Mahabir S, et al. Birthplace, years of residence in the United States, and obesity among Mexican-American adults. Obesity (Silver Spring) 2007;15:1043–52. doi: 10.1038/oby.2007.537. [DOI] [PubMed] [Google Scholar]
- 26.Lauderdale DS, Rathouz PJ. Body mass index in a US national sample of Asian Americans: effects of nativity, years since immigration and socioeconomic status. Int J Obes Relat Metab Disord. 2000;24:1188–94. doi: 10.1038/sj.ijo.0801365. [DOI] [PubMed] [Google Scholar]
- 27.Williams DR, Haile R, Gonzalez HM, Neighbors H, Baser R, Jackson JS. The mental health of black Caribbean immigrants: results from the National Survey of American Life. Am J Public Health. 2007;97:52–9. doi: 10.2105/AJPH.2006.088211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Takeuchi DT, Zane N, Hong S, Chae DH, Gong F, Gee GC, et al. Immigration-related factors and mental disorders among Asian Americans. Am J Public Health. 2007;97:84–90. doi: 10.2105/AJPH.2006.088401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alegria M, Shrout PE, Woo M, Guarnaccia P, Sribney W, Vila D, et al. Understanding differences in past year psychiatric disorders for Latinos living in the US. Soc Sci Med. 2007;65:214–30. doi: 10.1016/j.socscimed.2007.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grant BF, Stinson FS, Hasin DS, Dawson DA, Chou SP, Anderson K. Immigration and lifetime prevalence of DSM-IV psychiatric disorders among Mexican Americans and non-Hispanic whites in the United States. Arch Gen Psychiatry. 2004;61:1226–33. doi: 10.1001/archpsyc.61.12.1226. [DOI] [PubMed] [Google Scholar]
- 31.Ortega AN, Rosenheck R, Alegria M, Desai RA. Acculturation and lifetime risk of psychiatric and substance use disorders among Hispanics. J Nerv Ment Dis. 2000;11:728–35. doi: 10.1097/00005053-200011000-00002. [DOI] [PubMed] [Google Scholar]
- 32.Heeringa SG, Wagner J, Torres M, Duan N, Adams T, Berglund P. Sample designs and sampling methods for the Collaborative Psychiatric Epidemiology Studies (CPES) Int J Methods Psychiatr Res. 2004;13:221–40. doi: 10.1002/mpr.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kessler RC, Berglund P, Chiu WT, Demler O, Heeringa S, Hiripi E, et al. The US National Comorbidity Survey Replication (NCS-R): design and field procedures. Int J Methods Psychiatr Res. 2004;13:69–92. doi: 10.1002/mpr.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jackson JS, Torres M, Caldwell CH, Neighbors HW, Nesse RM, Taylor RJ, et al. The National Survey of American Life: a study of racial, ethnic and cultural influences on mental disorders and mental health. Int J Methods Psychiatr Res. 2004;13:196–207. doi: 10.1002/mpr.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alegria M, Takeuchi D, Canino G, Duan N, Shrout P, Meng XL, et al. Considering context, place and culture: the National Latino and Asian American Study. Int J Methods Psychiatr Res. 2004;13:208–20. doi: 10.1002/mpr.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Heeringa SG, Berglund P. National Institutes of Mental Health (NIMH) Collaborative Psychiatric Epidemiology Survey Program (CPES) data set: integrated weights and sampling error codes for design-based analysis. 2007. [cited 2007 Jun 4]. Available from: URL: http://www.icpsr.umich.edu/cocoon/cpes/using.xml?section=Weighting.
- 37.Alegria M, Mulvaney-Day N, Torres M, Polo A, Cao Z, Canino G. Prevalence of psychiatric disorders across Latino subgroups in the United States. Am J Public Health. 2007;97:68–75. doi: 10.2105/AJPH.2006.087205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kessler RC, Ustun TB. The World Mental Health (WMH) survey initiative version of the World Health Organization Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.American Psychological Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington: American Psychiatric Association; 1994. [Google Scholar]
- 40.Ballenger JC, Davidson JR, Lecrubier Y, Nutt DJ, Kirmayer LJ, Lepine JP, et al. Consensus statement on transcultural issues in depression and anxiety from the international consensus group on depression and anxiety. J Clin Psychiatry. 2001;62(Suppl 13):47–55. [PubMed] [Google Scholar]
- 41.Simon GE, VonKorff M, Piccinelli M, Fullerton C, Ormel J. An international study of the relation between somatic symptoms and depression. N Engl J Med. 1999;341:1329–35. doi: 10.1056/NEJM199910283411801. [DOI] [PubMed] [Google Scholar]
- 42.First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV axis I disorders, research version, non-patient edition (SCID-1/NP) New York: Biometrics Research, New York State Psychiatric Institute; 2002. Nov, [Google Scholar]
- 43.Taylor AW, Dal Grande E, Gill TK, Chittleborough CR, Wilson DH, Adams RJ, et al. How valid are self-reported height and weight? A comparison between CATI self-report and clinic measurements using a large cohort study. Aust N Z J Public Health. 2006;30:238–46. doi: 10.1111/j.1467-842x.2006.tb00864.x. [DOI] [PubMed] [Google Scholar]
- 44.Bulloch AG, Williams JV, Lavorato DH, Patten SB. The relationship between major depression and marital disruption is bidirectional. Depress Anxiety. 2009;26:1172–7. doi: 10.1002/da.20618. [DOI] [PubMed] [Google Scholar]
- 45.Aseltine RH, Jr, Kessler RC. Marital disruption in a community sample. J Health Soc Behav. 1993;34:237–51. [PubMed] [Google Scholar]
- 46.Gavin AR, Walton E, Chae DH, Alegria M, Jackson JS, Takeuchi D. The associations between socioeconomic status and major depressive disorder among blacks, Latinos, Asians, and non-Hispanic whites: findings from the Collaborative Psychiatric Epidemiology Studies. Psychol Med. 2010;40:51–61. doi: 10.1017/S0033291709006023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Widome R, Linde JA, Rohde P, Ludman EJ, Jeffery RW, Simon GE. Does the association between depression and smoking vary by body mass index (BMI) category? Prev Med. 2009;49:380–3. doi: 10.1016/j.ypmed.2009.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schwartz MB, Brownell KD. Obesity and body image. Body Image. 2004;1:43–56. doi: 10.1016/S1740-1445(03)00007-X. [DOI] [PubMed] [Google Scholar]
- 49.Rohde P, Lewinsohn PM, Brown RA, Gau JM, Kahler CW. Psychiatric disorders, familial factors and cigarette smoking: I. Associations with smoking initiation. Nicotine Tob Res. 2003;5:85–98. doi: 10.1080/1462220031000070507. [DOI] [PubMed] [Google Scholar]
- 50.StataCorp. STATA: Release 10.0. College Station (TX): StataCorp; 2007. [Google Scholar]
- 51.Smith DE, Thompson JK, Raczynski JM, Hilner JE. Body image among men and women in a biracial cohort: the CARDIA study. Int J Eat Disord. 1999;25:71–82. doi: 10.1002/(sici)1098-108x(199901)25:1<71::aid-eat9>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 52.Cash TF, Roy RE. Pounds of flesh: weight, gender, and body images. In: Sobal J, Maurer D, editors. Interpreting weight: the social management of fatness and thinness. Hawthorne (NY): Aldine de Gruyter; 1999. pp. 209–28. [Google Scholar]
- 53.Davison TE, McCabe MP. Relationship between men's and women's body image and their psychological, social, and sexual functioning. Sex Roles. 2005;2:463–75. [Google Scholar]
- 54.Breitkopf CR, Littleton H, Berenson A. Body image: a study in a tri-ethnic sample of low income women. Sex Roles. 2007;56:373–80. [Google Scholar]
- 55.Lynch E, Liu K, Spring B, Hankinson A, Wei GS, Greenland P. Association of ethnicity and socioeconomic status with judgments of body size: the Coronary Artery Risk Development in Young Adults (CARDIA) study. Am J Epidemiol. 2007;165:1055–62. doi: 10.1093/aje/kwk114. [DOI] [PubMed] [Google Scholar]
- 56.Grabe S, Hyde JS. Ethnicity and body dissatisfaction among women in the United States: a meta-analysis. Psychol Bull. 2006;132:622–40. doi: 10.1037/0033-2909.132.4.622. [DOI] [PubMed] [Google Scholar]
- 57.Anderson LA, Eyler AA, Galuska DA, Brown DR, Brownson RC. Relationship of satisfaction with body size and trying to lose weight in a national survey of overweight and obese women aged 40 and older, United States. Prev Med. 2002;35:390–6. doi: 10.1006/pmed.2002.1079. [DOI] [PubMed] [Google Scholar]
- 58.Celio AA, Zabinski MF, Wilfley DE. African American body images. In: Cash TR, Pruzinsky T, editors. Body image: a handbook of theory, research, and clinical practice. New York: Guilford Press; 2002. pp. 234–42. [Google Scholar]
- 59.Johnson F, Wardle J. Dietary restraint, body dissatisfaction, and psychological distress: a prospective analysis. J Abnorm Psychol. 2005;114:119–25. doi: 10.1037/0021-843X.114.1.119. [DOI] [PubMed] [Google Scholar]
- 60.Bay-Cheng LY, Zucker AN, Stewart AJ, Pomerleau CS. Linking femininity, weight concern, and mental health among Latina, black, and white women. Psychol Women Q. 2002;26:36–45. [Google Scholar]
- 61.Carr D, Friedman MA. Is obesity stigmatizing? Body weight, perceived discrimination, and psychological well-being in the United States. J Health Soc Behav. 2005;46:244–59. doi: 10.1177/002214650504600303. [DOI] [PubMed] [Google Scholar]
- 62.Friedman KE, Reichmann SK, Costanzo PR, Zelli A, Ashmore JA, Musante GJ. Weight stigmatization and ideological beliefs: relation to psychological functioning in obese adults. Obes Res. 2005;13:907–16. doi: 10.1038/oby.2005.105. [DOI] [PubMed] [Google Scholar]
- 63.Hatzenbuehler ML, Keyes KM, Hasin DS. Associations between perceived weight discrimination and the prevalence of psychiatric disorders in the general population. Obesity (Silver Spring) 2009;17:2033–9. doi: 10.1038/oby.2009.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Carr D, Friedman MA, Jaffe K. Understanding the relationship between obesity and positive and negative affect: the role of psychosocial mechanisms. Body Image. 2007;4:165–77. doi: 10.1016/j.bodyim.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 65.Annis NM, Cash TF, Hrabosky JI. Body image and psychosocial differences among stable average weight, currently overweight, and formerly overweight women: the role of stigmatizing experiences. Body Image. 2004;1:155–67. doi: 10.1016/j.bodyim.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 66.Noll JG, Zeller MH, Trickett PKL, Putnam FW. Obesity risk for female victims of childhood sexual abuse: a prospective study. Pediatrics. 2007;120:e61–7. doi: 10.1542/peds.2006-3058. [DOI] [PubMed] [Google Scholar]
- 67.Kendler KS, Bulik CM, Silberg J, Hettema JM, Myers J, Prescott CA. Childhood sexual abuse and adult psychiatric and substance use disorders in women: an epidemiological and Cotwin control analysis. Arch Gen Psychiatry. 2000;57:953–9. doi: 10.1001/archpsyc.57.10.953. [DOI] [PubMed] [Google Scholar]
- 68.Argeseaunu Cunningham S, Ruben JD, Narayan KM. Health of foreign-born people in the United States: a review. Health Place. 2008;14:623–35. doi: 10.1016/j.healthplace.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 69.Antecol H, Bedard K. Unhealthy assimilation: why do immigrants converge to American health status levels? Demography. 2006;43:337–60. doi: 10.1353/dem.2006.0011. [DOI] [PubMed] [Google Scholar]
- 70.House JS, Kessler RC, Herzog AR. Age, socioeconomic status, and health. Milbank Q. 1990;68:383–411. [PubMed] [Google Scholar]
- 71.Palloni A, Arias E. Paradox lost: explaining the Hispanic adult mortality advantage. Demography. 2004;41:385–415. doi: 10.1353/dem.2004.0024. [DOI] [PubMed] [Google Scholar]
- 72.Stevens J, Keil JE, Wald LR, Gazes PC. Accuracy of current, 4-year, and 28-year self-reported body weight in an elderly population. Am J Epidemiol. 1990;132:1156–63. doi: 10.1093/oxfordjournals.aje.a115758. [DOI] [PubMed] [Google Scholar]
- 73.Kuczmarski MF, Kuczmarski RJ, Najjar M. Effects of age on validity of self-reported height, weight, and body mass index: findings from the Third National Health and Nutrition Examination Survey, 1988–1994. J Am Diet Assoc. 2001;101:28–34. doi: 10.1016/S0002-8223(01)00008-6. [DOI] [PubMed] [Google Scholar]
- 74.Niedhammer I, Bugel I, Bonenfant S, Goldberg M, Leclerc A. Validity of self-reported weight and height in the French GAZEL cohort. Int J Obes Relat Metab Disord. 2000;24:1111–8. doi: 10.1038/sj.ijo.0801375. [DOI] [PubMed] [Google Scholar]
- 75.Istvan J, Zavela K, Weidner G. Body weight and psychological distress in NHANES I. Int J Obes Relat Disord. 1992;16:999–1003. [PubMed] [Google Scholar]
- 76.Johnston E, Johnson S, McLeod P, Johnston M. The relation of body mass index to depressive symptoms. Can J Public Health. 2004;95:179–83. doi: 10.1007/BF03403643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lin EH, Katon WJ, VonKorff M, Russo JE, Simon GE, Bush TM, et al. Relapse of depression in primary care: rate and clinical predictors. Arch Fam Med. 1998;7:443–9. doi: 10.1001/archfami.7.5.443. [DOI] [PubMed] [Google Scholar]
- 78.Nierenberg AA, Petersen TJ, Alpert JE. Prevention of relapse and recurrence in depression: the role of long-term pharmacotherapy and psychotherapy. J Clin Psychiatry. 2003;64(Suppl 15):13–7. [PubMed] [Google Scholar]
- 79.Schwartz TL, Nihalani N, Jindal S, Virk S, Jones N. Psychiatric medication-induced obesity: a review. Obes Rev. 2004;5:115–21. doi: 10.1111/j.1467-789X.2004.00139.x. [DOI] [PubMed] [Google Scholar]
- 80.Paulose-Ram R, Jonas BS, Orwig D, Safran MA. Prescription psychotropic medication use among the U.S. adult population: results from the third National Health and Nutrition Examination Survey, 1988–1994. J Clin Epidemiol. 2004;57:309–17. doi: 10.1016/j.jclinepi.2003.05.001. [DOI] [PubMed] [Google Scholar]