Abstract
Background
Mixed-states of bipolar disorders (BPD) may predict worse future illness and more depressive than manic morbidity, challenging a tendency to conflate mixed-states and mania.
Methods
Patients (N=247) were followed-up systematically for 24 months following hospitalization for initial major episodes of DSM-IV type I BPD and scored for weekly interval morbidity-types.
Results
Overall morbidity during follow-up was 1.6-times greater following mixed (n=97) versus manic (n=150) first-episodes of BPD (60.0 vs. 37.8 %-of-weeks; p<0.0001). Patients with initial mixed-states had a nearly 12-fold later excess of mixed-states, 6.5-times more major depression, and 69% more dysthymia during follow-up than those presenting in mania. In contrast, manic first-episodes were followed by over 10-times more mania, 6-times more hypomania, and 35% more psychotic illness.
Limitations
Estimates of longitudinal morbidity may be inaccurate, and ongoing treatment may distort them.
Conclusions
Based on detailed, prospective assessments among first-episode BPD patients, those presenting in mixed-states were more ill, and much more likely to experience mixed, depressive and dysthymic morbidity during follow-up, versus much more mania, hypomania, and perhaps more psychosis following mania. The findings support two markedly dissimilar subtypes of BPD, and call for more explicit therapeutic studies of mixed-states.
Keywords: Bipolar disorder, mania, mixed-states, morbidity, onset, prediction
Bipolar disorder (BPD) is characterized by episodic major recurrences of mania, hypomania, major-depression, or mixed-states, less severe intermittent or sustained morbidity, and variable intervals of approximate euthymia, with substantial risks of disability and mortality, even following an initial episode (Turvey et al., 1999; Perugi et al., 2000; Tohen et al., 2000, 2003; Paykel et al., 2006; Huxley and Baldessarini, 2007; Forty et al., 2009; Baldessarini et al., 2010a). Mixed-states involve complex admixtures or rapidly alternations of mainly excited or mainly depressive states (Salvatore et al. 2002). There is growing evidence that early BPD mixed-states may be followed by particularly severe later morbidity that includes a great deal of dysphoria, depression and suicide-risk; moreover, their optimal treatment remains much less studied than mania or bipolar depression (Berk et al., 2005; Vieta et al., 2005; González-Pinto et al., 2007). There is some evidence that the nature of initial episodes, including mixed-states versus mania, can predict similar and greater morbidity during later follow-up (Azorin et al., 2009; Forty et al., 2009; Swan et al., 2009), usually based on retrospective or mid-course studies, rather than with systematic, prospective assessment of psychopathology in detail from onset (Baldessarini et al., 2010a).
Despite the emerging impression that the course of BPD illness differs substantially following initial manic, mixed, or depressive presentations, there appears to be a tendency to consider manic and mixed episodes, in particular, as both closely related and to be contrasted to bipolar depressive episodes. Evidence for this tendency can be found in many contemporary therapeutic trials, in which type-I BPD patients in manic and mixed-states are both enrolled, often without separate analysis of their responses (e.g., Del Bello et al., 2006; Keck et al., 2006; Perlis et al., 2006; Strakowski et al., 2007; Niufan et al., 2008; Vieta et al., 2008; McIntyre et al., 2009; Young et al., 2009; Ketter et al., 2010).
Given the importance of testing the potential predictive value of mania and mixed-states, based on early and prospective assessment of details of morbid-states, we now report on analyses of estimated proportions of time spent in specific morbid states following first-lifetime manic or mixed first major episodes in 247 DSM-IV type-I BPD patients followed-up prospectively and systematically for two years from onset based on first-lifetime hospitalization.
Methods
Subjects and treatments
Patients were initially evaluated at first-lifetime hospitalizations for an episode of major affective or psychotic illness, and followed prospectively and systematically at intervals ranging from a week to six months for several years, with SCID-based assessments at intake and at 24 months supporting final consensus diagnoses of DSM-IV type I BPD. Two-year consensus diagnoses were employed to minimize risk of instability of some initial DSM-IV diagnoses over time (Salvatore et al., 2009). At follow-up assessments, interval weekly morbid status was reconstructed in life-charts, based on both in-person and by-telephone, semi-structured interviews of patients, supplemented by interviews with relatives and treating physicians, and from medical records. Patients were evaluated over the past decade at McLean Hospital in Boston, Massachusetts, following methods detailed previously (Tohen et al., 2000, 2003; Baldessarini et al., 2010a). Protocols were approved by the McLean Institutional Review Board and subjects provided written, informed consent for study-participation and for anonymous and aggregate reporting of study-information. In this naturalistic, follow-up study, treatments were not controlled by experimental protocols nor was conformity to therapeutic standards required; instead, patients were monitored and treated by their individual clinicians based on prevailing community standards.
Morbidity assessments
Initial illnesses were categorized by consensus as relatively pure DSM-IV mania versus mixed-states that met full diagnostic criteria for mania and major depression or showed rapid or polyphasic alternation between such polarities. Morbidity during follow-up included DSM-IV manic, hypomanic, mixed, or major depressive states, as well as less severe dysthymic or dysphoric states that did not meet DSM-IV criteria but appeared to be clinically significant. Estimated times in both full and subsyndromal, specific morbid states were recorded as the primary outcome measure.
To evaluate the potential impact of current mood-states as well as the accuracy of reported morbidity during intervals between follow-up assessments, in a sub-sample of 81 patients, we repeatedly rated current morbid states with standardized clinical scales, including a 36-item Expanded Brief Psychiatric Rating Scale (BPRS-E) that includes symptoms typical of BPD patients, the 24-item Hamilton Depression Rating Scale (HDRS-24) for depressive symptoms, and Young Mania Rating Scale (YMRS) for manic features with scoring modified by recent recommendations (Tohen et al., 2003; Baldessarini et al., 2010a). We also compared 24-month episodic morbidity in a sub-sample of 50 patients followed unusually closely (examined every 1–2 weeks) compared to 100 other randomly selected patients matched 2:1 for age and sex.
Data analyses
Estimated times (percentage of weeks) in specific morbid states were analyzed by ANOVA methods (F; degrees-of-freedom [df] = 1; 245) for continuous variables, or contingency tables (χ2; df=1) for categorical measures. Statistical significance required two-sided p ≤ 0.05. Data are means ± standard deviations (SD).
Results
Of the 247 first-episode type I BPD patients, 150 presented in mania and 97 in DSM-IV mixed episodes (39.3%). Both groups were very similar in sex-distribution: 54.0% men with initial mania vs. 54.6% with mixed-states. However, manic first-episodes requiring hospitalization occurred at significantly younger ages than did mixed-states (28.6±11.2 vs. 33.1±12.3 years; F=49.4, p<0.0001).
In preliminary analyses, we found no significant relationships of current morbidity at follow-up assessments and reported interval morbidity; in addition, patients observed directly every 1–2 weeks during follow-up did not yield different outcomes from the overall samples (not shown). Two-year follow-up morbidities of manic versus mixed-state first-episodes differed greatly (Table). Overall morbidity during follow-up was 1.59-times greater for patients with mixed first-episodes (60.0% vs. 37.8% weeks of follow-up; p<0.0001; Table).
Table.
Morbidity as %-of-weeks during first two years in 247 cases of first-episode DSM-IV type I bipolar disorder
| Morbidity | Onset Types | Relative Risk | F-value | p-value | |
|---|---|---|---|---|---|
| Mixed (n=97) | Mania (n=150) | ||||
| Mixed-states | 30.8 ± 37.6 | 2.58 ± 12.1 | 11.9 | 73.0 | <0.0001 |
| Dysthymia | 15.3 ± 23.5 | 9.03 ± 20.7 | 1.69 | 4.86 | 0.03 |
| Major Depression | 10.2 ± 18.9 | 1.56 ± 6.16 | 6.54 | 26.8 | <0.0001 |
| Mania | 1.75 ± 2.95 | 18.0 ± 28.5 | 0.10 | 31.0 | <0.0001 |
| Hypomania | 0.91 ± 4.01 | 5.50 ± 18.7 | 0.17 | 5.66 | 0.02 |
| Psychosis | 0.77 ± 5.29 | 1.04 ± 7.06 | 0.40 | 0.10 | 0.75 |
| All morbidity | 60.0 ± 36.9 | 37.8 ± 35.5 | 1.59 | 22.3 | <0.0001 |
DSM-IV bipolar I disorder patients (N=247) were followed prospectively for 2 years from first-lifetime major episodes of mania or mixed-states, with the percent of weeks in specific morbid-states indicated, with differences between the sub-groups.
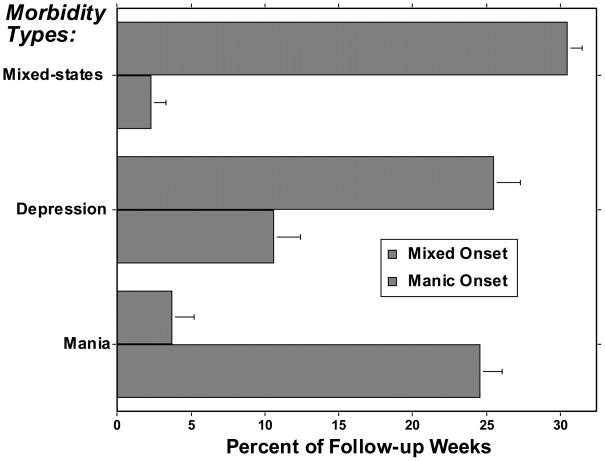
Regarding specific types of morbidity, BPD patients presenting initially in mixed-states had nearly 12-fold later excess of mixed states (p<0.0001), 6.5-times more major depressive episodes (p<0.0001), and 69% more dysthymia than patients presenting in mania (p=0.03). In contrast, manic first-episodes were followed by over 10-times more mania (p<0.0001), 6-times more hypomania (p=0.02), and 35%, but nonsignificantly, more psychotic illness than after mixed-state first episodes (Table). Pooled analysis of: [a] major or minor mixed-states, [b] major depression or dysthymia, and [c] mania, hypomania or psychosis, as proposed morbidity-clusters, yielded highly significant differences between patients presenting in mixed-states versus mania (all p<0.0001; Fig.).
Figure.
Distribution of morbidity (%-of-weeks-ill) during 2-year follow-up following first-lifetime mixed (striped bars) versus manic (gray bars) episodes, comparing time in major or minor mixed-states, major depression or dysthymia, and mania-hypomania-psychosis. All differences between patients starting in mixed-states versus mania are highly significant (all F ≥ 20, all p<0.0001).
Discussion
The present findings indicate strongly that initial mixed-states of DSM-IV type-I BPD were not only followed by more weeks of illness during two-years of follow-up, but also much more mixed, depressive, and dysthymic illness, and much less mania, hypomania, or psychotic illness compared to patients presenting initially in relatively pure mania (Table and Fig.). The findings accord with suggestions in reports cited above that mixed-states are followed by more severe illnesses and more depressive morbidity than following initial mania. Moreover, the findings are based on systematic, prospective and detailed assessments from first-episodes. They strongly support the conclusion that the dissimilar presentations predicted markedly dissimilar future illness-courses, do not support the equivalence of mania and mixed-states, and indicate distinct clinical subtypes.
This study is limited by uncertainties involved in defining morbidity during follow-up with intermittent assessments, possibly biased by current mood or by characteristics of the private, university-affiliated, psychiatric hospital in which the study was conducted. Nevertheless, we made efforts to support the estimates of percent-of-weeks-ill by comparisons to results with frequently evaluated patients and by use of standard depression and mania symptom rating scales to verify current states: neither method of verification showed differences in morbidity estimates from the overall sample. It is also possible that illnesses, including depressive episodes, occurred in some cases prior to the index hospitalization, complicating estimates of onset-age, for example (Baldessarini et al., 2010). Another potential confound is that patients were treated clinically by community standards during follow-up, and with lack of control over treatment. However, if treatment is a relevant factor, such a circumstance might suggest that patients presenting in mixed-states were less treatment-responsive. Indeed, this possibility is not ruled out and requires further testing (Berk et al., 2005; Vieta et al., 2005; González-Pinto et al., 2007). It is also important to consider specifically the depressive component of long-term morbidity of patients presenting initially in mixed-states. This component of BPD is especially difficult to treat successfully without inducing destabilizing effects, such as with antidepressants (Ghaemi et al., 2008; Tondo et al., 2009; Baldessarini et al. 2010c).
In conclusion, this study adds strong support to the hypothesis that DSM-IV type-I BPD patients with mixed-state first major episodes have a poorer prognosis than those presenting in mania, and that the type of illness involved includes much more recurrence of mixed-states as well as depression and dysthymia. In contrast, patients presenting in mania had less illness overall, and much more mania and hypomania, and tended to have more psychosis during follow-up. These findings encourage considering the two sub-groups separately in therapeutic trials and other studies, and underscore the challenge of treating the depressive components of BPD.
Acknowledgments
Supported in part by NIH grant MH-073049 (to RJB & MT), a grant from the Bruce J. Anderson Foundation and by the McLean Private Donors Research Fund for Bipolar Disorder research (to RJB), a grant from NARSAD (to PS), by the Atlas Foundation (to MT). The funding sources had no influence on the conduct, analysis, or reporting of this study.
Footnotes
Disclosures: Dr. Baldessarini has recently been a consultant or investigator-initiated research collaborator with: AstraZeneca, Auritec, Biotrofix, Janssen, JDS-Noven, Lilly, Luitpold, NeuroHealing, Novartis, Pfizer, and SK-BioPharmaceutical Corporation; he is not a member of pharmaceutical speakers’ bureaus, nor does he or any family member hold equity positions in biomedical or pharmaceutical corporations. Dr. Tohen was formerly an employee of Eli Lilly & Co (to 2008), and has consulted to, or received speaker’s honoraria from Astra-Zeneca, Bristol Myers-Squibb, Eli Lilly, Glaxo-SmithKline, Johnson & Johnson, and Wyeth Corporations; his spouse is an Eli Lilly employee and stockholder. Other authors have no relevant disclosures of potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Azorin JM, Aubrun E, Bertsch J, Reed C, Gerard S, Lukasiewicz M. Mixed states vs. pure mania in the French sample of the EMBLEM study: results at baseline and 24 months (European Mania in Bipolar Longitudinal Evaluation of Medication study) BMC Psychiatry. 2009;9:33–41. doi: 10.1186/1471-244X-9-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldessarini RJ, Bolzani L, Cruz N, Jones PB, Lai M, Lepri B, Perez J, Salvatore P, Tohen M, Tondo L, Vieta E. Onset-age of bipolar disorders at six international sites. J Affect Disord. 2010a;121:143–146. doi: 10.1016/j.jad.2009.05.030. [DOI] [PubMed] [Google Scholar]
- Baldessarini RJ, Salvatore P, Tohen M, Khalsa H-MK, Gebre-Medhin P, Imaz H, Gonzalez-Pinto A, Perez Sanchez-Toledo J, Beathge C, Cruz N, Maggini C. Morbidity in 303 bipolar I disorder patients from first major episodes. Bipolar Disord. 2010b doi: 10.1111/j.1399-5618.2010.00812.x. in press. [DOI] [PubMed] [Google Scholar]
- Baldessarini RJ, Vieta E, Calabrese JR, Tohen M, Bowden C. Bipolar depression: overview and commentary. Harv Rev Psychiatry. 2010c doi: 10.3109/10673221003747955. in press. [DOI] [PubMed] [Google Scholar]
- Berk M, Dodd S, Malhi GS. Bipolar missed states’: the diagnosis and clinical salience of bipolar mixed states. Aust NZ J Psychiatry. 2005;39:215–221. doi: 10.1080/j.1440-1614.2004.01557.x. [DOI] [PubMed] [Google Scholar]
- DelBello MP, Kowatch RA, Adler CM, Stanford KE, Welge JA, Barzman DH, Nelson E, Strakowski SM. Double-blind randomized pilot study comparing quetiapine and divalproex for adolescent mania. J Am Acad Child Adolesc Psychiatry. 2006;45:305–313. doi: 10.1097/01.chi.0000194567.63289.97. [DOI] [PubMed] [Google Scholar]
- Forty L, Jones L, Jones I, Smith DJ, Caesar S, Fraser C, Gordon-Smith K, Hyde S, Craddock N. Polarity at illness onset in bipolar I disorder and clinical course of illness. Bipolar Disord. 2009;11:82–88. doi: 10.1111/j.1399-5618.2008.00654.x. [DOI] [PubMed] [Google Scholar]
- Ghaemi SN, Wingo AP, Filkowski MA, Baldessarini RJ. Long-term antidepressant treatment in bipolar disorder: meta-analyses of benefits and risks. Acta Psychiatr Scand. 2008;118:347–356. doi: 10.1111/j.1600-0447.2008.01257.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Pinto A, Aldama A, Mosquera F, González-Gómez C. Epidemiology, diagnosis and management of mixed mania. CNS Drugs. 2007;21:611–626. doi: 10.2165/00023210-200721080-00001. [DOI] [PubMed] [Google Scholar]
- Huxley N, Baldessarini RJ. Disability and its treatment in bipolar disorder patients. Bipolar Disord. 2007;9:183–196. doi: 10.1111/j.1399-5618.2007.00430.x. [DOI] [PubMed] [Google Scholar]
- Keck PE, Jr, Calabrese JR, McQuade RD, Carson WH, Carlson BX, Rollin LM, Marcus RN, Sanchez R. Randomized, double-blind, placebo-controlled 26-week trial of aripiprazole in recently manic patients with bipolar I disorder. J Clin Psychiatry. 2006;67:626–637. doi: 10.4088/jcp.v67n0414. [DOI] [PubMed] [Google Scholar]
- Ketter TA, Agid O, Kapur S, Loebel A, Siu CO, Romano SJ. Rapid antipsychotic response with ziprasidone predicts subsequent acute manic/mixed episode remission. J Psychiatr Res. 2010;44:8–14. doi: 10.1016/j.jpsychires.2009.07.006. [DOI] [PubMed] [Google Scholar]
- McIntyre RS, Cohen M, Zhao J, Alphs L, Macek TA, Panagides J. Three-week, randomized, placebo-controlled trial of asenapine in the treatment of acute mania in bipolar mania and mixed states. Bipolar Disord. 2009;11:673–686. doi: 10.1111/j.1399-5618.2009.00748.x. [DOI] [PubMed] [Google Scholar]
- Niufan G, Tohen M, Qiuqing A, Fude Y, Pope E, McElroy H, Ming L, Gaohua W, Xinbao Z, Huichun L, Liang S. Olanzapine versus lithium in the acute treatment of bipolar mania: a double-blind, randomized, controlled trial. J Affect Disord. 2008;105:101–108. doi: 10.1016/j.jad.2007.04.020. [DOI] [PubMed] [Google Scholar]
- Paykel ES, Abbott R, Morriss R, Hayhurst H, Scott J. Subsyndromal and syndromal symptoms in the longitudinal course of bipolar disorder. Br J Psychiatry. 2006;189:118–123. doi: 10.1192/bjp.bp.105.013870. [DOI] [PubMed] [Google Scholar]
- Perlis RH, Baker RW, Zarate CA, Jr, Brown EB, Schuh LM, Jamal HH, Tohen M. Olanzapine versus risperidone in the treatment of manic or mixed States in bipolar I disorder: a randomized, double-blind trial. J Clin Psychiatry. 2006;67:1747–1753. doi: 10.4088/jcp.v67n1112. [DOI] [PubMed] [Google Scholar]
- Perugi G, Micheli C, Akiskal HS, Madaro D, Socci C, Quilici C, Musetti L. Polarity of the first episode, clinical characteristics, and course of manic-depressive illness: systematic retrospective investigation of 320 bipolar I patients. Comprehen Psychiatry. 2000;41:13–18. doi: 10.1016/s0010-440x(00)90125-1. [DOI] [PubMed] [Google Scholar]
- Salvatore P, Baldessarini RJ, Centorrino F, Egli S, Albert M, Gerhard A, Maggini C. Weygandt’s, The Manic-Depressive Mixed States: Translation and commentary on its significance in the evolution of the concept of bipolar manic-depressive disorder. Harv Rev Psychiatry. 2002;10:255–275. doi: 10.1080/10673220216283. [DOI] [PubMed] [Google Scholar]
- Salvatore P, Baldessarini RJ, Tohen M, Khalsa HMK, Perez Sanchez-Toledo J, Zarate CA, Jr, Vieta E, Maggini C. McLean-Harvard International First-Episode Project: two-year stability of DSM-IV diagnoses in 500 first-episode psychotic disorder patients. J Clin Psychiatry. 2009;70:458–466. doi: 10.4088/jcp.08m04227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strakowski SM, Tsai SY, Delbello MP, Chen CC, Fleck DE, Adler CM, Arndt S, Amicone J. Outcome following a first manic episode: cross-national US and Taiwan comparison. Bipolar Disord. 2007;9:820–827. doi: 10.1111/j.1399-5618.2007.00411.x. [DOI] [PubMed] [Google Scholar]
- Swann AC, Steinberg JL, Lijffijt M, Moeller GF. Continuum of depressive and manic mixed states in patients with bipolar disorder: quantitative measurement and clinical features. World Psychiatry. 2009;8:166–172. doi: 10.1002/j.2051-5545.2009.tb00245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tohen M, Hennen J, Zarate CM, Jr, Baldessarini RJ, Strakowski SM, Stoll AL, Faedda GL, Suppes T, Gebre-Medhin P, Cohen BM. Two-year syndromal and functional recovery in 219 cases of first-episode major affective disorder with psychotic features. Am J Psychiatry. 2000;157:220–228. doi: 10.1176/appi.ajp.157.2.220. [DOI] [PubMed] [Google Scholar]
- Tohen M, Zarate CA, Jr, Hennen J, Khalsa HMK, Strakowski SM, Gebre-Medhin P, Salvatore P, Baldessarini RJ. The McLean-Harvard First-Episode Mania Study: prediction of recovery and first recurrence. Am J Psychiatry. 2003;160:2099–2107. doi: 10.1176/appi.ajp.160.12.2099. [DOI] [PubMed] [Google Scholar]
- Tondo L, Vázquez G, Baldessarini RJ. Mania associated with antidepressant-treatment: comprehensive meta-analysis. Acta Psychiatr Scand. 2009 Dec 2; doi: 10.1111/j.1600-0447.2009.01514.x. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- Turvey CL, Coryell WH, Solomon DA, Leon AC, Endicott J, Keller MB, Keller MB, Akiskal HS. Long-term prognosis of bipolar I disorder. Acta Psychiatr Scand. 1999;99:110–119. doi: 10.1111/j.1600-0447.1999.tb07208.x. [DOI] [PubMed] [Google Scholar]
- Vieta E, Panicali F, Goetz I, Reed C, Comes M, Tohen M. Olanzapine monotherapy and olanzapine combination therapy in the treatment of mania: 12-week results from the European Mania in Bipolar Longitudinal Evaluation of Medication (EMBLEM) observational study. J Affect Disord. 2008;106:63–72. doi: 10.1016/j.jad.2007.05.009. [DOI] [PubMed] [Google Scholar]
- Vieta E. Bipolar mixed states and their treatment. Expert Rev Neurother. 2005;5:63–68. doi: 10.1586/14737175.5.1.63. [DOI] [PubMed] [Google Scholar]
- Young AH, Oren DA, Lowy A, McQuade RD, Marcus RN, Carson WH, Spiller NH, Torbeyns AF, Sanchez R. Aripiprazole monotherapy in acute mania: 12-week randomised placebo- and haloperidol-controlled study. Br J Psychiatry. 2009;194:40–48. doi: 10.1192/bjp.bp.108.049965. [DOI] [PubMed] [Google Scholar]