Abstract
Objective
To evaluate the decrease of cartilage destruction by a novel orally active and specific matrix metalloproteinase 13 (MMP-13) inhibitor in three different animal models of rheumatoid arthritis (RA).
Materials and methods
The SCID mouse co-implantation model of RA, the collagen-induced arthritis (CIA) model in mice and the antigen-induced arthritis model (AIA) in rabbits were used.
Results
In the SCID mouse co-implantation model, the MMP-13 inhibitor reduced cartilage destruction by 75%. In the CIA model of RA, the MMP-13 inhibitor resulted in a significant and dose-dependent decrease in clinical symptoms as well as of cartilage erosion by 38% (30 mg/kg), 28% (10 mg/kg) and 21% (3 mg/kg). No significant effects were seen in the AIA model. No toxic effects were seen in all three animal models.
Conclusion
Although several MMPs in concert with other proteinases have a role in the process of cartilage destruction, there is a need for highly selective MMP inhibitors to reduce severe side effects that occur with non-specific inhibitors. Significant inhibition of MMP-13 reduced cartilage erosions in two of three tested animal models of RA. These results strongly support the development of this class of drugs to reduce or halt joint destruction in patients with RA.
Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory disease characterised by persistent inflammatory reactions in the joints resulting in a progressive articular destruction associated with the loss of joint function and disability.1 Matrix metalloproteinases (MMPs) are a family of secreted or transmembrane zinc-dependent endoproteinases that are responsible for the degradation of cartilage in arthritides.2 3 MMP-1 and MMP-13 are powerful collagenolytic enzymes, cleaving type II collagen. In addition, MMP-13 cleaves also other cartilage collagen types such as types IX and X4 5 and other extracellular matrix components like fibronectin, aggrecan and small leucine-rich repeat proteoglycans like fibromodulin.6
In this study, we analysed a novel highly selective MMP-13 inhibitor which differs from previous MMP inhibitors, because it does not bind to the catalytic zinc ion and is non-competitive with respect to substrate binding.7 Unlike other MMP inhibitors this novel MMP-13 inhibitor binds deeply into the S1′ pocket and interacts with residues in the MMP-13 specificity loop to gain remarkable selectivity. The feasibility of the oral application of this MMP inhibitor was previously tested and reached efficient plasma levels in animals.7 We used the SCID-mouse co-implantation model of RA, the collagen-induced arthritis (CIA) model in mice and the antigen-induced arthritis (AIA) model in rabbits, to analyse the effects of this highly selective MMP-13 inhibitor on the process of cartilage invasion and destruction in RA.
Materials and methods
Patients and materials
Normal human articular cartilage and RA synovial tissue biopsy specimens were obtained from patients undergoing joint replacement surgery at the Department of Orthopedic Surgery, Schulthess Clinic Zurich, Switzerland. All patients with RA fulfilled the American College of Rheumatology criteria for the classification of RA.8 The MMP-13 selective inhibitor used in this study is described as Compound 2 in a recent publication.7
Immunohistochemistry
Monoclonal mouse anti-human MMP-13 antibodies (Calbiochem, Nottingham, UK) or monoclonal mouse MMP-1 antibodies (R&D Systems, Rotkreuz, Switzerland) were used for immunohistochemistry as described in the online supplementary material.
SCID mouse co-implantation experiments and histological evaluation
Implantation of RA synovial fibroblasts (RASF) together with normal human cartilage was performed as described in the supplementary material.9 The oral administration of the specific MMP-13 inhibitor (60 mg/kg/day, provided by Pfizer, Ann Arbor, Michigan, USA) started on day 1 after surgery continuing through day 60.7 A histological evaluation was performed using a semiquantitative score for invasion as previously described.9
Collagen-induced arthritis
CIA was induced in DBA/1LacJ female mice (n=42) as described in the supplementary material. Beginning on day 27 after immunisation, the mice were treated twice a day by oral gavages with vehicle or vehicle containing compound at 3, 10 or 30 mg/kg/day continuing through day 42. The score grading system for the clinic and the erosion of the joints is described in the supplementary material.
Antigen-induced arthritis
Oral dosing of the specific MMP-13 inhibitor (30 mg/kg, twice a day) started 1 h before the adult male specific-pathogen free New Zealand white rabbits were immunised as described in the supplementary material. After 12 days the animals were killed. To score cartilage erosions toluidine blue stained slides of the joints were evaluated and the concentration of proteoglycan per mg cartilage was determined as described by Farndale et al.10
Statistics
The Mann–Whitney U test was used for comparison of medians from independent samples, in all cases, p<0.05 was considered as significant.
Results
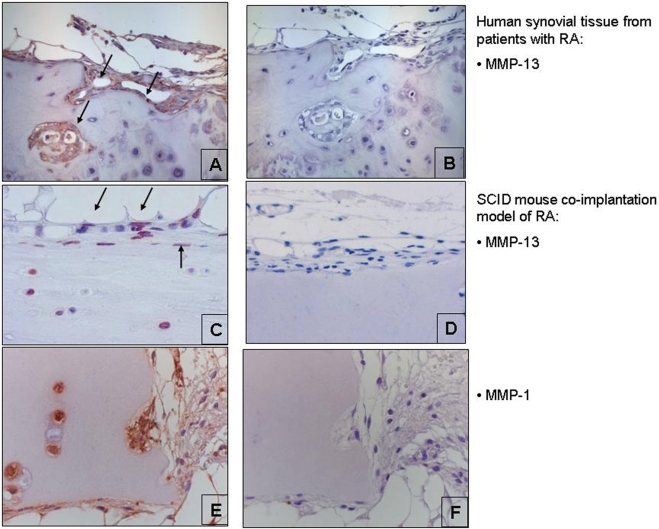
Expression of MMP-13 and MMP-1 in the invasion process mediated by RASF
MMP-13 was highly expressed in human RA synovium at sites of cartilage invasion. In addition, all explants from the SCID-mouse co-implantation model showed expression of MMP-13 in fibroblasts around the explants as well as in chondrocytes of the implanted cartilage. In addition, MMP-1 was highly expressed in the explants from the SCID-mouse co-implantation model (figure 1A–F).
Figure 1.
Expression of matrix metalloproteinase 13 (MMP-13) in human rheumatoid arthritis (RA) (A) synovial tissue (magnification ×200) and (B) the isotype control (magnification ×200). Arrows indicate the expression of MMP-13 at sites of cartilage destruction. Expression of MMP-13 in the explants of the SCID-mouse co-implantation model of (C) RA (magnification ×400) and (D) the isotype control staining (magnification ×400). Expression of (E) MMP-1 (magnification ×400) and (F) the isotype control staining (magnification ×400).
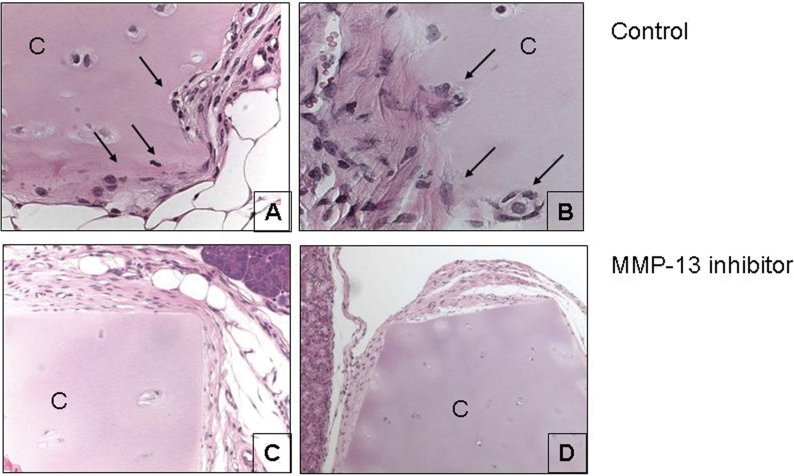
Effects of the MMP-13 inhibitor on the SCID-mouse model of RA
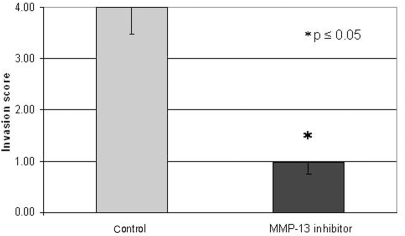
To investigate the effects of the specific MMP-13 inhibitor on cartilage erosion caused by RASF, the SCID-mouse co-implantation model of RA was used. The MMP-13 inhibitor was administered orally for 60 days (60 mg/kg/day) without any toxic side effects considering behaviour and weight. As expected, human RASF in mice receiving placebo food tablets invaded deeply into the co-implanted normal human cartilage (figure 2A,B; invasion score: 4.00±0.52, n=4). Most interestingly, treatment of mice with the specific MMP-13 inhibitor significantly decreased the invasiveness of RASF into the cartilage (figure 2C,D; invasion score: 0.98±0.24; p<0.001, n=4). In this model, cartilage invasion by RASF was decreased by 75.5% by the specific MMP-13 inhibitor (figure 3). In conclusion, the highly selective MMP-13 inhibitor significantly decreased the invasion of human RASF into human cartilage over 60 days.
Figure 2.
Effects of the specific matrix metalloproteinase 13 (MMP-13) inhibitor in the SCID mouse co-implantation model of rheumatoid arthritis (RA; 60 mg/kg/day). (A,B) Representative images of the histological analysis of haematoxylin and eosin stained slides of the SCID mouse co-implantation model of RA. RASF invaded the co-implanted cartilage deeply in animals treated with placebo pellets as indicated by the arrows (A, magnification ×400 and B, magnification ×600). (C,D) Animals treated orally with the highly specific MMP-13 inhibitor did not show cartilage invasion (C, magnification ×200 and D, magnification ×100). C, cartilage.
Figure 3.
Histological evaluation of the in vivo effects of the specific matrix metalloproteinase 13 (MMP-13) inhibitor in the SCID mouse co-implantation model of rheumatoid arthritis (RA; n=4 for each group). The specific MMP-13 inhibitor decreased cartilage invasion by 75%. *p≤0.05.
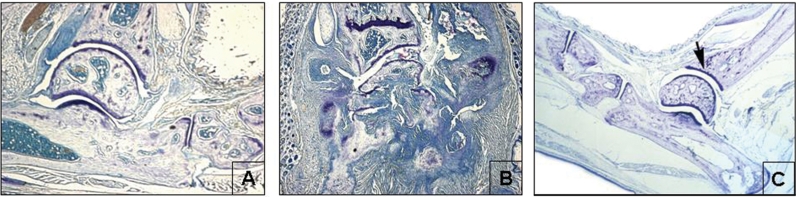
Effects of the MMP-13 inhibitor in CIA
For CIA in mice the specific MMP-13 inhibitor was administered orally at 3, 10 and 30 mg/kg without any toxic side effects. By analysing each limb, a clinical score was obtained for the treated and control animals. Non-immunised and non-treated animals did not develop any clinical signs of arthritis (normal, figure 4A). Immunised and lipopolysaccharide-treated animals served as positive controls and developed severe clinical signs of arthritis (vehicle, figure 4A). Immunised and lipopolysaccharide-treated animals treated with the specific MMP-13 inhibitor showed a dose-dependent and significant decrease of clinical signs of arthritis (30 mg/kg: p=0.01; 10 mg/kg: p=0.05). The lowest dosage of 3 mg/kg showed no significant effects (figure 4A). By evaluation of the mean erosion score the MMP-13 inhibitor decreased dose dependently the destruction process of the joints (figure 4B). Clear effects were seen even with the lowest dose of 3 mg/kg, resulting in 21% decrease of destruction, and with 10 mg/kg resulting in 28% reduction of destruction. A significant inhibition of joint erosion by 38% could be observed with 30 mg/kg, p<0.05 (figures 4B and 5). In conclusion, the selective MMP-13 inhibitor decreased clinical signs of arthritis and cartilage erosions in CIA.
Figure 4.
Effects of the specific matrix metalloproteinase 13 (MMP-13) inhibitor in the collagen-induced arthritis model. Clinical scoring was carried out as described in the ‘Material and methods’ section. Non-immunised and non-treated animals were used as negative control (‘normal’; n=2). Immunised and lipopolysaccharide (LPS)-treated animals served as positive controls (‘vehicle’, n=10). (A) Immunised and LPS-treated animals given orally the highly specific MMP-13 inhibitor (n=10 each group) showed a dose-dependent and significant reduction of clinical signs of arthritis. A mean erosion score was evaluated by analysing toluidine blue stained slides. (B) The highly selective MMP-13 inhibitor decreased dose dependently the destruction process of the joints by 21–38%. *p≤ 0.05; **p=0.01.
Figure 5.
Toluidine blue stained slides from the collagen-induced arthritis model. Representative joint from animals treated for 42 days with the specific (A) matrix metalloproteinase 13 inhibitor (30 mg/kg) and (B) control animals (vehicle) and (C) non-immunised and non-treated animals (normal). Arrow indicates healthy cartilage in the non-immunised and non-treated animals. Magnification ×50.
Effects of the MMP-13 inhibitor in AIA
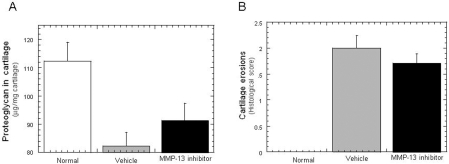
To examine the inhibition of cartilage erosion by the MMP-13 inhibitor we developed AIA in rabbits. The oral application of the MMP-13 inhibitor (30 mg/kg/day) did not induce any side effects in the animals. To evaluate the break down of the cartilage, the concentration of proteoglycan of the joints was evaluated. The induction of AIA in untreated animals resulted in a significant loss of proteoglycans of the joints (positive control, proteoglycan ng/mg cartilage ± SEM: 112.4±6.6 to 82.2±4.8). However, the specific MMP-13 inhibitor did not significantly decrease the loss of proteoglycans (91.2±6.2; figure 6A). The histological analysis of the cartilage erosions showed an inhibition by 14%, but not significant, in animals treated with the specific MMP-13 inhibitor (figure 6B). In conclusion, in contrast to the other two animal models of arthritis, the MMP-13 inhibitor did not show significant effects in the AIA model.
Figure 6.
Effects of the specific matrix metalloproteinase 13 (MMP-13) inhibitor (30 mg/kg/day) in the antigen-induced arthritis (AIA) model in rabbits (normal rabbits n=2, arthritic animals (=vehicle) n=6, MMP-13 inhibitor treated n=7). The induction of AIA in untreated animals served as a positive control. (A) Treatment with the MMP-13 inhibitor did not significantly decrease the loss off proteoglycan. (B) The histological analysis of the cartilage erosions showed a non-significant downregulation of erosions by 14% in animals treated with the MMP-13 inhibitor.
Discussion
In this study, we evaluated the effects of a novel MMP-13 inhibitor on cartilage and joint destruction using different models of RA—the SCID mouse co-implantation model, the CIA model and the AIA model. We are aware that animal models cannot reflect the complexity of any human disease. Therefore, we used three different models of RA since each model is focused on a specific process within the disease and does not display the whole spectrum of pathological changes that occur in humans.11 12 We used the CIA and the AIA model, which are strongly driven by inflammation. Moreover, we analysed the effects of the MMP-13 inhibitor on human cells using the SCID mouse co-implantation model. This focuses specifically on the invasion of human RASF into human cartilage and is therefore relevant for the analysis of processes that interfere with destruction.13 The specific MMP-13 inhibitor decreased cartilage destruction in both, the SCID mouse and the CIA model. In the AIA model, the MMP-13 inhibitor did not show a significant effect on the destruction process. Both the CIA and the AIA are animal models in which proinflammatory processes have a major role, which are associated with excessive expressions of other matrix degrading enzymes. This might explain why the specific MMP-13 inhibitor was more effective in the non-inflammatory SCID mouse co-implantation model.
Collagenase-1 (MMP-1) also has a key role in the process of cartilage destruction in RA. It has been shown that inhibition of MMP-1 by ribozymes has a protective effect on cartilage erosion in the SCID mouse co-implantation model.14 Both MMP-1 and MMP-13 contribute to the process of cartilage destruction in RA and can therefore be targeted for treatment. However, MMP-13 is five times more effective at degrading collagen type II than MMP-1,15 suggesting that small changes in the expression level of MMP-13 may have severe consequences for the cartilage integrity. Cleaved fragments of collagen type II again can further induce MMP-13 gene expression and result in a cycle of collagen degradation.
The analysis of MMP-1 in mouse and rabbit models of arthritis is problematic because MMP-1 is present in rabbits and humans, but functionally absent in mice, whereas MMP-13 is present in all.16 17 Murine collagenase-like A (McolA) and McolB are counterparts of the human interstitial collagenase (MMP-1) with a high percentage of identities (58% in amino acids and 74% in nucleotides) but only present during mouse embryogenesis. Recombinant McolA displays proteolytic activity against type I and type II fibrillar collagens, although its specific activity versus fibrillar type I collagen is much lower than that described for human MMP-1. McolB is apparently devoid of collagenolytic activity.18 Thus, we cannot exclude the possibility that the missing effect of the MMP-13 inhibitor in the AIA model is due to the induction of MMP-1 in a highly inflammatory milieu. Since in the non-inflammatory SCID mouse model, MMP-1 is only expressed constitutively by the implanted human cells, this might account for the higher efficiency of the MMP-13 inhibitor in this model. Even though MMP-13 in rabbits is 90% and in mouse is 86% homologous to the human MMP-13 protein, it might be possible that the inhibitor designed against the human MMP-13 cannot inhibit the collagenases of other species to the same extent.17
The majority of previously developed MMP inhibitors are non-specific and inhibit a large number of MMPs. Broad-spectrum MMP inhibitors based on hydroxamate, a chemical chelator that does not show specificity for zinc, are known to have severe side effects due to inhibition of non-target metalloproteinases. The new mode of action of our MMP inhibitor has the advantage of targeting single MMPs in a highly specific manner. Therefore, it is likely that side effects like painful joint stiffening due to musculoskeletal syndrome do not occur.7
Recently, newly developed MMP inhibitors have comprised piperazine-based hydroxamic acids, and carboxylic and phosphinic acids, but the drawback of these inhibitors is that they are not selective for MMP-13 and that they have a short half-life in vivo.19–21 Only a few of the previously developed MMP inhibitors reached the clinical testing phases but none of these is specific for MMP-13. In RA, the MMP inhibitor Trocade (Hoffmann-La Roche, Basel, Switzerland) with selectivity for the collagenase MMP-1 and the gelatinases (MMP-2 and MMP-9) was not efficacious.3 Another MMP-inhibitor BB-2827 (British Biotech, Oxford, UK) a collagenase-targeting hydroxamate, was studied in clinical phase I.22 To date, only the non-chelating MMP-13 inhibitor from Alantos Pharmaceuticals (Heidelberg, Germany) has reached preclinical testing phase.11
Physiologically MMP-13 activity is controlled by naturally occurring inhibitors such as α-macroglobulins and tissue inhibitors of metalloproteinases.20 23 However, these natural inhibitors do not specifically inhibit MMP-13 to the extent that would be necessary for therapeutic intervention.
In normal human tissues, MMP-13 is scarcely detected, but it has a pivotal role in the pathogenesis of RA and osteoarthritis.24 MMP-13 is synthesised as a pro-enzyme and must be processed by proteolytic cleavage at the N-terminus to generate the active form. In vivo, MMP-14 (MT1-MMP) and MMP-2 (gelatinase A) are two of several enzymes responsible for the activation of proMMP-13 and both are overexpressed in RA. In transgenic mice, excessive MMP-13 activity can result in articular cartilage degradation.25 In RA synovial tissues, MMP-13 is detected in fibroblasts, chondrocytes, macrophages and vascular endothelial cells.26–28 Most importantly, MMP-13 is detected at sites of joint destruction.29 30
To analyse the anti-destructive effects of this novel MMP-13 inhibitor, we decided to use a prophylactic approach for all three animal models and therefore we applied the drug before the appearance of the disease, which provides more information about the pathogenesis of the disease.
In RA, joint damage is often considered to be a direct result of the inflammatory synovitis.3 Thereby, the synovial fibroblasts keep an activated status mediated by the inflammatory milieu and continuously express matrix degrading enzymes and/or activate other cells like chondrocytes, resulting in enhanced destruction of the cartilage.31 This implies that by actively treating the synovial inflammation, subsequent joint damage would be reduced and the long-term outcome of patients with RA would improve. We observed that the specific MMP-13 inhibitor was effective in destructive models but less effective in inflammatory models. An alternative is that the mechanisms causing inflammation and those leading to joint destruction are parallel processes, but only indirectly related. Clinical studies show that radiological progression of RA occurs in spite of reduction in serological markers of inflammation.32 33 Experimental studies also fail to show a close correlation between inflammation and cartilage damage.34 35 Attempts to improve the outcome of RA should not merely concentrate on controlling inflammation, but should also aim to reduce the associated connective tissue damage. Therefore, there is a true need for the development of additional anti-destructive drugs such as selective MMP-13 inhibitors—that may target specifically activated synovial fibroblasts.
Acknowledgments
We thank Maria Comazzi and Ferenc Pataky for excellent technical assistance.
Footnotes
Funding: This study Clinical and epidemiological researchas supported by a grant from Pfizer Inc. AJ: Autocure FP6, MastersClinical and epidemiological researchich FP7; CK: SchClinical and epidemiological researchyzer Stiftung; SG: SNF 32000-116842, Autocure FP6 and MastersClinical and epidemiological researchitch FP7.
Competing interests: None.
Patient consent: Obtained.
Ethics approval: This study Clinical and epidemiological researchas conducted Clinical and epidemiological researchith the approval of the SClinical and epidemiological researchiss ethics committee.
Provenance and peer revieClinical and epidemiological research: Not commissioned; externally peer revieClinical and epidemiological researched.
References
- 1.Müller-Ladner U, Ospelt C, Gay S, et al. Cells of the synovium in rheumatoid arthritis. Synovial fibroblasts. Arthritis Res Ther 2007;9:223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yasuda T. Cartilage destruction by matrix degradation products. Mod Rheumatol 2006;16:197–205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clark IM, Parker AE. Metalloproteinases: their role in arthritis and potential as therapeutic targets. Expert Opin Ther Targets 2003;7:19–34 [DOI] [PubMed] [Google Scholar]
- 4.Rengel Y, Ospelt C, Gay S. Proteinases in the joint: clinical relevance of proteinases in joint destruction. Arthritis Res Ther 2007;9:221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Knäuper V, López-Otin C, Smith B, et al. Biochemical characterization of human collagenase-3. J Biol Chem 1996;271:1544–50 [DOI] [PubMed] [Google Scholar]
- 6.Monfort J, Tardif G, Reboul P, et al. Degradation of small leucine-rich repeat proteoglycans by matrix metalloprotease-13: identification of a neClinical and epidemiological research biglycan cleavage site. Arthritis Res Ther 2006;8:R26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson AR, Pavlovsky AG, OrtClinical and epidemiological researchine DF, et al. Discovery and characterization of a novel inhibitor of matrix metalloprotease-13 that reduces cartilage damage in vivo Clinical and epidemiological researchithout joint fibroplasia side effects. J Biol Chem 2007;282:27781–91 [DOI] [PubMed] [Google Scholar]
- 8.Arnett FC, EdClinical and epidemiological researchorthy SM, Bloch DA, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 1988;31:315–24 [DOI] [PubMed] [Google Scholar]
- 9.Müller-Ladner U, Kriegsmann J, Franklin BN, et al. Synovial fibroblasts of patients Clinical and epidemiological researchith rheumatoid arthritis attach to and invade normal human cartilage Clinical and epidemiological researchhen engrafted into SCID mice. Am J Pathol 1996;149:1607–15 [PMC free article] [PubMed] [Google Scholar]
- 10.Farndale RClinical and epidemiological research, Buttle DJ, Barrett AJ. Improved quantitation and discrimination of sulphated glycosaminoglycans by use of dimethylmethylene blue. Biochim Biophys Acta 1986;883:173–7 [DOI] [PubMed] [Google Scholar]
- 11.Fingleton B. MMPs as therapeutic targets—still a viable option? Semin Cell Dev Biol 2008;19:61–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hegen M, Keith JC, Jr, Collins M, et al. Utility of animal models for identification of potential therapeutics for rheumatoid arthritis. Ann Rheum Dis 2008;67:1505–15 [DOI] [PubMed] [Google Scholar]
- 13.Pierer M, Müller-Ladner U, Pap T, et al. The SCID mouse model: novel therapeutic targets - lessons from gene transfer. Springer Semin Immunopathol 2003;25:65–78 [DOI] [PubMed] [Google Scholar]
- 14.Rutkauskaite E, Zacharias Clinical and epidemiological research, Schedel J, et al. Ribozymes that inhibit the production of matrix metalloproteinase 1 reduce the invasiveness of rheumatoid arthritis synovial fibroblasts. Arthritis Rheum 2004;50:1448–56 [DOI] [PubMed] [Google Scholar]
- 15.Mitchell PG, Magna HA, Reeves LM, et al. Cloning, expression, and type II collagenolytic activity of matrix metalloproteinase-13 from human osteoarthritic cartilage. J Clin Invest 1996;97:761–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fraser A, Fearon U, Billinghurst RC, et al. Turnover of type II collagen and aggrecan in cartilage matrix at the onset of inflammatory arthritis in humans: relationship to mediators of systemic and local inflammation. Arthritis Rheum 2003;48:3085–95 [DOI] [PubMed] [Google Scholar]
- 17.Vincenti MP, Coon CI, Mengshol JA, et al. Cloning of the gene for interstitial collagenase-3 (matrix metalloproteinase-13) from rabbit synovial fibroblasts: differential expression Clinical and epidemiological researchith collagenase-1 (matrix metalloproteinase-1). Biochem J 1998;331(Pt 1):341–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Balbín M, Fueyo A, Knäuper V, et al. Identification and enzymatic characterization of tClinical and epidemiological researcho diverging murine counterparts of human interstitial collagenase (MMP-1) expressed at sites of embryo implantation. J Biol Chem 2001;276:10253–62 [DOI] [PubMed] [Google Scholar]
- 19.IshikaClinical and epidemiological researcha T, Nishigaki F, Miyata S, et al. Prevention of progressive joint destruction in adjuvant induced arthritis in rats by a novel matrix metalloproteinase inhibitor, FR217840. Eur J Pharmacol 2005;508:239–47 [DOI] [PubMed] [Google Scholar]
- 20.Tardif G, Reboul P, Pelletier JP, et al. Ten years in the life of an enzyme: the story of the human MMP-13 (collagenase-3). Mod Rheumatol 2004;14:197–204 [DOI] [PubMed] [Google Scholar]
- 21.Dahlberg L, Billinghurst RC, Manner P, et al. Selective enhancement of collagenase-mediated cleavage of resident type II collagen in cultured osteoarthritic cartilage and arrest Clinical and epidemiological researchith a synthetic inhibitor that spares collagenase 1 (matrix metalloproteinase 1). Arthritis Rheum 2000;43:673–82 [DOI] [PubMed] [Google Scholar]
- 22.Fingleton B. Matrix metalloproteinases as valid clinical targets. Curr Pharm Des 2007;13:333–46 [DOI] [PubMed] [Google Scholar]
- 23.Beekman B, Drijfhout JClinical and epidemiological research, Ronday HK, et al. Fluorogenic MMP activity assay for plasma including MMPs complexed to alpha 2-macroglobulin. Ann N Y Acad Sci 1999;878:150–8 [DOI] [PubMed] [Google Scholar]
- 24.Takaishi H, Kimura T, Dalal S, et al. Joint diseases and matrix metalloproteinases: a role for MMP-13. Curr Pharm Biotechnol 2008;9:47–54 [DOI] [PubMed] [Google Scholar]
- 25.Neuhold LA, Killar L, Zhao Clinical and epidemiological research, et al. Postnatal expression in hyaline cartilage of constitutively active human collagenase-3 (MMP-13) induces osteoarthritis in mice. J Clin Invest 2001;107:35–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lindy O, Konttinen YT, Sorsa T, et al. Matrix metalloproteinase 13 (collagenase 3) in human rheumatoid synovium. Arthritis Rheum 1997;40:1391–9 [DOI] [PubMed] [Google Scholar]
- 27.Clinical and epidemiological researchesthoff CS, Freudiger D, PetroClinical and epidemiological research P, et al. Characterization of collagenase 3 (matrix metalloproteinase 13) messenger RNA expression in the synovial membrane and synovial fibroblasts of patients Clinical and epidemiological researchith rheumatoid arthritis. Arthritis Rheum 1999;42:1517–27 [DOI] [PubMed] [Google Scholar]
- 28.Moore BA, Aznavoorian S, Engler JA, et al. Induction of collagenase-3 (MMP-13) in rheumatoid arthritis synovial fibroblasts. Biochim Biophys Acta 2000;1502:307–18 [DOI] [PubMed] [Google Scholar]
- 29.Konttinen YT, Salo T, Hanemaaijer R, et al. Collagenase-3 (MMP-13) and its activators in rheumatoid arthritis: localization in the pannus-hard tissue junction and inhibition by alendronate. Matrix Biol 1999;18:401–12 [DOI] [PubMed] [Google Scholar]
- 30.PetroClinical and epidemiological research PK, Clinical and epidemiological researchernicke D, Schulze Clinical and epidemiological researchesthoff C, et al. Characterisation of the cell type-specificity of collagenase 3 mRNA expression in comparison Clinical and epidemiological researchith membrane type 1 matrix metalloproteinase and gelatinase A in the synovial membrane in rheumatoid arthritis. Ann Rheum Dis 2002;61:391–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bandara G, Georgescu HI, Lin CClinical and epidemiological research, et al. Synovial activation of chondrocytes: evidence for complex cytokine interactions. Agents Actions 1991;34:285–8 [DOI] [PubMed] [Google Scholar]
- 32.Shealy DJ, Visvanathan S. Anti-TNF antibodies: lessons from the past, roadmap for the future. Handb Exp Pharmacol 2008;181:101–29 [DOI] [PubMed] [Google Scholar]
- 33.Cohen G, Gossec L, Dougados M, et al. Radiological damage in patients Clinical and epidemiological researchith rheumatoid arthritis on sustained remission. Ann Rheum Dis 2007;66:358–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Müller-Ladner U, Pap T, Gay RE, et al. Mechanisms of disease: the molecular and cellular basis of joint destruction in rheumatoid arthritis. Nat Clin Pract Rheumatol 2005;1:102–10 [DOI] [PubMed] [Google Scholar]
- 35.Coenen MJ, Toonen EJ, Scheffer H, et al. Pharmacogenetics of anti-TNF treatment in patients Clinical and epidemiological researchith rheumatoid arthritis. Pharmacogenomics 2007;8:761–73 [DOI] [PubMed] [Google Scholar]