Summary
HIV-infected prisoners face an inordinate number of community re-entry challenges. In 2007, 102 HIV-infected prisoners in Malaysia were surveyed anonymously within six months prior to release to assess the prevalence and correlates of community re-entry challenges. Staying out of prison (60.8%), remaining off drugs (39.2%), finding employment (35.3%) and obtaining HIV care (32.4%) were the re-entry challenges reported most frequently. Global stigma, negative self-image and public attitudes-related stigma were independently associated with challenges to obtaining HIV care. In multivariate analyses, those with previous incarcerations (adjusted odds ratio [AOR], 3.2; 95% confidence interval [CI], 1.4–7.6), higher HIV-related symptoms (AOR, 2.0; 95% CI, 1.0–4.1) and higher public attitudes-related stigma (AOR, 2.5; 95% CI, 1.2–5.1) had a significantly higher likelihood of identifying more re-entry challenges. Targeted interventions, such as effective drug treatment, HIV care and public awareness campaigns, are crucial for stemming the HIV epidemic and improving health outcomes among HIV-infected prisoners in Malaysia.
Keywords: Malaysia, prisoners, HIV, AIDS, substance abuse, re-entry, HIV stigma
BACKGROUND
The global magnitude of incarceration is staggering. During the past two decades, prison populations around the world have steadily increased, and by the end of 2008, nearly 10 million people were incarcerated worldwide.1,2 Malaysia's imprisonment rate, which is one of the highest in southeast Asia,2 is inextricably linked to its war on drugs. From 2001 to 2007, drug-related arrests increased from 21,000 to 54,000. This, coupled with the recent introduction of mandatory sentences of two to five years for those who failed government-sponsored drug treatment at compulsory drug treatment centres or had been convicted of drug use more than twice, contributed to 16,237 prisoners or 38% of the total prison population by the end of 2007.3
Nearly all prisoners return to local communities, and therefore face a cascade of interrelated challenges during their transition back into the community.4–6 Numerous factors, including problems associated with obtaining employment,7 financial and poverty-related burdens,8,9 stable housing and transitional support,10–12 and reuniting with family and other support networks,13 are just a few of the cited issues that contribute to re-incarceration. Re-entry challenges are magnified for those who have significant medical co-morbidity; a disproportionate number of prisoners are affected with a myriad of illnesses, including mental illness, substance use disorders and infectious diseases such as HIV/AIDS, viral hepatitis and tuberculosis.5,14–18 Disruptions in continuity of care, lack of health-care coverage and resources, and high rates of drug and alcohol relapse thwart positive health and social outcomes for both HIV-infected and non-infected prisoners.4,15,19–21
Infectious diseases such as HIV/AIDS pose special community re-entry issues globally.5 Not only are there considerable challenges in the continuity of HIV care,22 which when discontinued leads to significant co-morbidity and mortality, but also results in heightened risks for infection of others when risk reduction interventions are not provided.23 In particular, the most common mode of transmission of HIV among prisoners is injection drug use and there is scant evidence of effective treatments that successfully transitions HIV-infected prisoners with substance use disorders back to the community.
In Malaysia, criminalization of drug use and a delayed public health response exacerbated the growing HIV epidemic, particularly among injection drug users (IDUs).24 As a result, 75% of cumulative HIV/AIDS cases occurred among IDUs.25 In 2005, the government recognized that it had not achieved a reduction in HIV/AIDS cases and rapidly implemented syringe exchange26 and methadone maintenance programmes.27 Nevertheless, the prevalence of HIV among 50,000 Malaysian prisoners, where HIV testing is mandatory, is approximately 6%;16 this is 15 times greater than that found in the general adult population where it is 0.4%.25 As a consequence, HIV-infected prisoners in Malaysia represent a critical group for targeted intervention, yet their community re-entry challenges have not been assessed. Therefore, the objective of this study was to identify the prevalence and correlates of community re-entry challenges faced by HIV-infected male prisoners prior to transition from prison back into the community.
METHODS
Study setting
This study was conducted in June 2007 at Pengkalan Chepa Prison, a male correctional facility in Kota Bharu, Malaysia. Kota Bharu, situated near the Thailand–Malaysia border, is the capital of Kelantan, one of the poorest states in Malaysia.28 As is the case throughout Malaysia, all prison inmates at the prison undergo mandatory HIV testing and HIV-infected prisoners are segregated in dormitory settings.
Study subjects
Study eligibility included being HIV-infected and being within six months of community release. Prison officials queried the prison database and provided a list of 102 individuals who met eligibility criteria to a medical practitioner. The practitioner subsequently asked each eligible inmate if he was interested in participating in an anonymous survey about making plans for transition back to the community. Interested inmates were referred to a member of the study team who described in private the nature of the study, obtained written consent and conducted the 30-minute interview. All 102 referred inmates agreed to participate. No names or unique identifiers were collected, nor were coercive incentives or disincentives provided. All interviews were conducted in Bahasa Malaysia by trained, bilingual interviewers from the University of Malaya. All procedures and data collection forms for this study were reviewed and approved by the Medical Ethics Committee at the University of Malaya Medical Centre.
Study measures
Structured interviews included demographic information, drug use and re-entry challenges, as well as standardized and validated scales measuring HIV stigma29 and HIV symptoms.30 Opioid dependence was defined if the subject reported the persistent use of heroin or any other known opioid during the 12 months prior to the current incarceration and met at least three of seven standardized criteria for opioid dependence. A list of re-entry challenges was created from a review of the existing literature and discussion with local experts; those included in this study were staying out of prison, remaining off drugs, finding employment, obtaining HIV care, getting financial support from family, finding adequate housing and reuniting with family or friends. For each re-entry task, a 5-point Likert scale was used to determine the level of difficulty; a re-entry challenge was identified if the task was perceived as `hard' or `very hard'. The questionnaire was created in English and translated and back-translated into Bahasa Malaysia by trained English/Bahasa Malaysia bilingual interviewers.31
DATA ANALYSIS
Data analysis was done using SAS, version 9.1.3 (SAS Institute Inc, Cary, NC, USA). Descriptive statistics were generated by conducting frequencies on all predictor variables and re-entry challenges. Demographic and social circumstances were measured as categorical variables, but were further collapsed into fewer levels because of small frequencies in some categories. All items from the Berger HIV Stigma Scale were measured using the original 4-point Likert scale. All 20 items from the HIV Symptom Index were measured according to whether or not a subject indicated having the symptom. Stigma, HIV-related symptoms and age were dichotomized as being high or low relative to the median. Previous incarcerations and previous detentions in rehabilitation centres were dichotomized into `none' and `any' since a large percentage of the sample reported never having had both (24.5% and 46.1%, respectively). Responses to the remaining variables were measured dichotomously.
Bivariate associations between the predictor variables and the outcome variables were conducted using the Pearson's chi-square test or Fisher's exact test as appropriate. For multivariate analyses, an ordinal outcome variable representing the total number of re-entry challenges reported was created and proportional odds logistic regression was used. The odds ratios (OR) and 95% confidence intervals (CI) presented are estimates of the likelihood of reporting a greater number of re-entry challenges. A P value of 0.10 was used to enter the multivariate model, and variables significant at the 0.05 level were retained. A backward elimination strategy was used to determine the most parsimonious set of predictors. The proportional odds assumption for the final multivariate model was met.
RESULTS
Table 1 describes the baseline characteristics of the subjects. The mean age was 33.0 years with the majority reporting being Malay (96.1%), not married (81.4%), opioid-dependent (81.4%), living with family prior to the present incarceration (87.3%), having had a family visit while currently incarcerated (75.0%) and having been previously incarcerated (75.5%; mean = 2.5±2.3, range = 0–10 times). Approximately half the sample had previous detentions in a rehabilitation centre (53.9%; mean = 1.1±1.4, range = 0–6 times) and reported ≥7 HIV-related symptoms (52.0%; mean = 7.1±3.7, range = 0–17). Nearly two-thirds reported having known someone close who died of AIDS (65.7%), while less than half had provided care for someone with HIV/AIDS (42.2%). While the entire sample was HIV-infected, only two subjects reported having ever been prescribed antiretroviral medications.
Table 1.
Characteristics of subjects (n = 102)
| Characteristic | n | % |
|---|---|---|
| Age (years) | ||
| <33 | 51 | 50.0 |
| ≥33 | 51 | 50.0 |
| Ethnicity | ||
| Malay | 98 | 96.1 |
| Other* | 4 | 3.9 |
| Education † | ||
| Primary | 21 | 20.6 |
| Lower secondary | 46 | 45.1 |
| Higher secondary or higher | 35 | 34.3 |
| Marital status | ||
| Not married‡ | 83 | 81.4 |
| Married | 19 | 18.6 |
| Living arrangement prior to incarceration | ||
| With family | 89 | 87.3 |
| Other§ | 13 | 12.7 |
| Previous incarcerations | ||
| None | 25 | 24.5 |
| Any | 77 | 75.5 |
| Previous detentions in rehabilitation centre | ||
| None | 47 | 46.1 |
| Any | 55 | 53.9 |
| Family visits during incarceration | ||
| No | 25 | 24.5 |
| Yes | 77 | 75.5 |
| Provided care for someone living with HIV/AIDS | ||
| No | 59 | 57.8 |
| Yes | 43 | 42.2 |
| Knew someone close who died of AIDS | ||
| No | 35 | 34.3 |
| Yes | 67 | 65.7 |
| Ever prescribed antiretroviral medications | ||
| No | 100 | 98.0 |
| Yes | 2 | 2.0 |
| Number of HIV-related symptoms (median = 7)** | ||
| Low | 50 | 49.0 |
| High | 52 | 51.0 |
| Opioid-dependent | ||
| No | 19 | 18.6 |
| Yes | 83 | 81.4 |
| Total stigma score (median = 97) †† | ||
| Low | 48 | 47.1 |
| High | 54 | 52.9 |
| Personalized stigma subscale score (median = 42) †† | ||
| Low | 41 | 40.2 |
| High | 61 | 59.8 |
| Disclosure stigma subscale score (median = 26) †† | ||
| Low | 43 | 42.2 |
| High | 59 | 57.8 |
| Negative self-image stigma subscale score (median = 32) †† | ||
| Low | 45 | 44.1 |
| High | 57 | 55.9 |
| Public attitudes stigma subscale score (median = 48) †† | ||
| Low | 50 | 49.0 |
| High | 52 | 51.0 |
Other = Indian, Chinese, mixed or other
Indicates highest level of education attained. Primary is up to Grade 6, lower secondary is up to Grade 9, higher secondary or higher is up to Grade 12 or university
Not married = single, separated or widowed
Other = reported living alone, with friends, in a hostel or homeless/on the streets
Derived from the HIV Symptom Index
Derived from the Berger HIV Stigma Scale
In this sample: total stigma scores ranged from 69 to 125 (mean = 99.1±9.7); personalized stigma subscale scores ranged from 31 to 55 (mean = 43.9±5.2); disclosure stigma subscale scores ranged from 16 to 34 (mean = 26.1±2.9); negative self-image stigma subscale scores ranged from 21 to 44 (mean = 32.4±3.5); and public attitudes stigma subscale scores ranged from 37 to 65 (mean = 49.0±5.6).
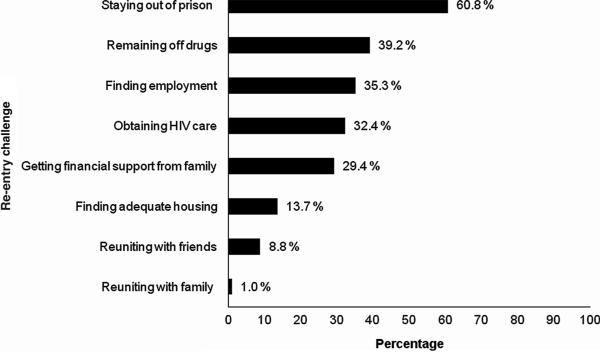
Figure 1 depicts the proportion of the sample that identified re-entry challenges. Staying out of prison was the most prevalent challenge (60.8%) facing this sample, followed by remaining off drugs (39.2%). Roughly one-third of the sample reported difficulty finding employment (35.3%), obtaining HIV care (32.4%) and getting financial support from family (29.4%). A smaller proportion, 13.7% and 8.8%, respectively, identified difficulty finding adequate housing and reuniting with friends.
Figure 1.
Proportion of subjects identifying community re-entry challenges
Bivariate associations between predictor variables and re-entry challenges are represented in Table 2. Lower education level was associated with difficulty obtaining financial support from family (P = 0.004) and reuniting with friends (P = 0.008). Previous incarceration was associated with difficulty staying out of prison (P = 0.004). High numbers of HIV-related symptoms were associated with difficulty finding employment (P = 0.006) and getting financial support from family (P = 0.04). High levels of stigma, including negative self-image and public attitudes stigma, were associated with difficulty obtaining HIV care (P = 0.05, P = 0.02 and P = 0.0005, respectively). A low disclosure stigma subscale score was associated with difficulty staying out of prison (P = 0.05). Although these did not quite approach significance, those who were not married, were previously incarcerated, had a higher number of HIV-related symptoms, and had higher total stigma and public attitudes stigma scores expressed difficulty with achieving at least six out of the seven re-entry tasks.
Table 2.
Bivariate associations between predictor variables and re-entry challenges
| % of those reporting difficulty |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Staying out of prison |
P value | Remaining off drugs |
P value | Finding employment |
P value | Obtaining HIV care |
P value | Getting financial support from family |
P value | Finding adequate housing |
P value | Reuniting with friends |
P value |
| Age | ||||||||||||||
| < 33 | 66.7 | 0.22 | 45.1 | 0.22 | 31.4 | 0.41 | 39.2 | 0.14 | 29.4 | 1.00 | 11.8 | 0.57 | 7.8 | 1.00 |
| ≥ 33 | 54.9 | 33.3 | 39.2 | 25.5 | 29.4 | 15.7 | 9.8 | |||||||
| Education | ||||||||||||||
| Primary | 57.1 | 0.89 | 33.3 | 0.78 | 33.3 | 0.76 | 28.6 | 0.91 | 52.4 | 0.004 | 14.3 | 0.75 | 23.8 | 0.008 |
| Lower secondary | 63.0 | 39.1 | 39.1 | 32.6 | 32.6 | 10.9 | 8.7 | |||||||
| Higher secondary or higher | 60.0 | 42.9 | 31.4 | 34.3 | 11.4 | 17.1 | 0.0 | |||||||
| Marital status | ||||||||||||||
| Not married | 63.9 | 0.18 | 41.0 | 0.45 | 37.4 | 0.36 | 33.7 | 0.53 | 27.7 | 0.43 | 14.5 | 1.00 | 9.6 | 1.00 |
| Married | 47.4 | 31.6 | 26.3 | 26.3 | 36.8 | 10.5 | 5.3 | |||||||
| Living arrangement prior to incarceration | ||||||||||||||
| With family | 60.7 | 0.95 | 39.3 | 0.95 | 37.1 | 0.37 | 32.6 | 1.00 | 27.0 | 0.19 | 13.5 | 1.00 | 9.0 | 1.00 |
| Other | 61.5 | 38.5 | 23.1 | 30.8 | 46.2 | 15.4 | 7.7 | |||||||
| Previous incarcerations | ||||||||||||||
| None | 36.0 | 0.004 | 24.0 | 0.07 | 32.0 | 0.69 | 24.0 | 0.30 | 24.0 | 0.49 | 12.0 | 1.00 | 12.0 | 0.69 |
| Any | 68.8 | 44.2 | 36.4 | 35.1 | 31.2 | 14.3 | 7.8 | |||||||
| Previous detentions in rehabilitation centre | ||||||||||||||
| None | 53.2 | 0.15 | 29.8 | 0.07 | 36.2 | 0.86 | 25.5 | 0.17 | 31.9 | 0.61 | 14.9 | 0.75 | 8.5 | 1.00 |
| Any | 67.3 | 47.3 | 34.6 | 38.2 | 27.3 | 12.7 | 9.1 | |||||||
| Family visits during incarceration | ||||||||||||||
| No | 60.0 | 0.93 | 32.0 | 0.40 | 44.0 | 0.29 | 28.0 | 0.59 | 24.0 | 0.49 | 16.0 | 0.74 | 16.0 | 0.22 |
| Yes | 61.0 | 41.6 | 32.5 | 33.8 | 31.2 | 13.0 | 6.5 | |||||||
| Provided care for someone living with HIV/AIDS | ||||||||||||||
| No | 64.4 | 0.38 | 39.0 | 0.96 | 35.6 | 0.94 | 32.2 | 0.97 | 28.8 | 0.88 | 13.6 | 0.95 | 10.2 | 0.73 |
| Yes | 55.8 | 39.5 | 34.9 | 32.6 | 30.2 | 14.0 | 7.0 | |||||||
| Knew someone close who died of AIDS | ||||||||||||||
| No | 60.0 | 0.91 | 28.6 | 0.11 | 31.4 | 0.55 | 34.3 | 0.76 | 37.1 | 0.22 | 14.3 | 1.00 | 2.9 | 0.16 |
| Yes | 61.2 | 44.8 | 37.3 | 31.3 | 25.4 | 13.4 | 11.9 | |||||||
| Number of HIV-related symptoms | ||||||||||||||
| Low | 56.0 | 0.33 | 36.0 | 0.51 | 22.0 | 0.006 | 38.0 | 0.23 | 20.0 | 0.04 | 10.0 | 0.28 | 6.0 | 0.49 |
| High | 65.4 | 42.3 | 48.1 | 26.9 | 38.5 | 17.3 | 11.5 | |||||||
| Opioid-dependent | ||||||||||||||
| No | 42.1 | 0.06 | 26.3 | 0.20 | 31.6 | 0.71 | 31.6 | 0.94 | 47.4 | 0.06 | 10.5> | 1.00 | 10.5 | 0.67 |
| Yes | 65.1 | 42.2 | 36.1 | 32.5 | 25.3 | 14.5 | 8.4 | |||||||
| Total stigma score | ||||||||||||||
| Low | 60.4 | 0.94 | 35.4 | 0.46 | 31.2 | 0.42 | 22.9 | 0.05 | 29.2 | 0.96 | 12.5 | 0.73 | 6.3 | 0.49 |
| High | 61.1 | 42.6 | 38.9 | 40.7 | 29.6 | 14.8 | 11.1 | |||||||
| Personalized stigma subscale score | ||||||||||||||
| Low | 63.4 | 0.66 | 31.7 | 0.20 | 29.3 | 0.30 | 24.4 | 0.16 | 31.7 | 0.68 | 17.1 | 0.42 | 7.3 | 0.74 |
| High | 59.0 | 44.3 | 39.3 | 37.7 | 27.9 | 11.5 | 9.8 | |||||||
| Disclosure stigma subscale score | ||||||||||||||
| Low | 72.1 | 0.05 | 39.5 | 0.96 | 34.9 | 0.94 | 30.2 | 0.70 | 20.9 | 0.11 | 9.3 | 0.27 | 4.7 | 0.21 |
| High | 52.5 | 39.0 | 35.6 | 33.9 | 35.6 | 17.0 | 11.9 | |||||||
| Negative self-image stigma subscale score | ||||||||||||||
| Low | 62.2 | 0.79 | 31.1 | 0.14 | 35.6 | 0.96 | 20.0 | 0.02 | 24.4 | 0.33 | 11.1 | 0.50 | 6.7 | 0.73 |
| High | 59.7 | 45.6 | 35.1 | 42.1 | 33.3 | 15.8 | 10.5 | |||||||
| Public attitudes stigma subscale score | ||||||||||||||
| Low | 64.0 | 0.51 | 30.0 | 0.06 | 26.0 | 0.05 | 16.0 | 0.0005 | 28.0 | 0.76 | 10.0 | 0.28 | 6.0 | 0.49 |
| High | 57.7 | 48.1 | 44.2 | 48.1 | 30.8 | 17.3 | 11.5 | |||||||
Bivariate and multiple ordinal logistic regression results are depicted in Table 3. In the bivariate analysis, those who had previous incarcerations, high number of HIV-related symptoms, high negative self-image stigma subscale scores and high public attitudes stigma scores had a significantly higher likelihood of identifying a greater number of re-entry challenges. In the multiple logistic regression analysis, the outcomes were similar to the bivariate findings except that levels of negative self-image stigma no longer remained significant.
Table 3.
Bivariate and adjusted ordinal logistic regression results
| Odds ratio (95% CI) |
||
|---|---|---|
| Characteristic | Bivariate | Adjusted |
| Age ≥33 | 0.8 (0.4–1.6) | - |
| Education | ||
| Lower secondary | 0.9 (0.4–2.3) | - |
| Higher secondary or higher | 0.7 (0.3–1.7) | - |
| Married | 0.6 (0.3–1.5) | - |
| Lived with family prior to incarceration | 1.3 (0.5–3.7) | - |
| Previous incarcerations | 3.3 (1.4–7.7)* | 3.2 (1.4–7.6)* |
| Previous detentions in a rehabilitation centre | 1.8 (0.9–3.6) | - |
| Family visits during incarceration | 0.8 (0.4–1.9) | - |
| Provided care for someone living with HIV/AIDS | 1.0 (0.5–2.1) | - |
| Knew someone close who died of AIDS | 1.3 (0.6–2.6) | - |
| Number of HIV-related symptoms ≥7 | 2.1 (1.0–4.2)* | 2.0 (1.0–4.1)* |
| Opioid-dependent | 1.3 (0.5–3.1) | - |
| Total stigma score ≥97 | 1.8 (0.9–3.6) | - |
| Personalized stigma subscale score ≥42 | 1.6 (0.8–3.2) | - |
| Disclosure stigma subscale score ≥26 | 1.2 (0.6–2.4) | - |
| Negative self-image stigma subscale score ≥32 | 2.2 (1.1–4.5)* | - |
| Public attitudes stigma subscale score ≥48 | 3.0 (1.4–6.1)* | 2.5 (1.2–5.1)* |
P< 0.05
DISCUSSION
To our knowledge, this is the first investigation assessing the community re-entry challenges faced by HIV-infected male prisoners in Malaysia. Remaining out of prison, staying off drugs, finding employment and obtaining HIV care emerged as the most prevalent re-entry challenges.
The findings from this prison-derived sample have important implications broadly for the HIV epidemic in Malaysia, as these prisoners are highly representative of the group most predominantly affected by the epidemic in this country – young, injection drug-using ethnic Malay males.25 The stated re-entry challenges themselves were not too dissimilar from those generally reported by prisoners, and the magnitude of individuals identifying these challenges was often lower than expected, consistent with the unrealistic optimism of prisoners towards their post-release success that has been reported elsewere.32–34 For instance, 61% stated that staying out of prison would be a challenge, yet an even higher percentage of the sample had been incarcerated many times previously. Although it is well-established that prior incarceration is a risk factor for re-incarceration,8,35 including among HIV-infected individuals,36 the cognitive dissonance in recognizing this association was striking.
As further evidence of this dissonance, one-third of the subjects expressed concern for obtaining HIV care upon release. This finding is surprising, especially among a sample that reported a significant burden of HIV-related symptoms, presumably because of more advanced HIV disease, and for whom only 2% had ever been prescribed antiretroviral therapy successfully. These results, however, are consistent with previously documented inequities in HIV care for drug users in Malaysia, where only 2% of 315 patients receiving antiretroviral treatment in a publicly funded hospital were IDUs.37 The reality facing the vast majority of IDUs in Malaysia and in other parts of the world is that while they are among the most at risk and affected by HIV/AIDS, they are also among the least likely to receive antiretroviral medications.38,39
The results from this study offer several insights into why disparities in access to care may exist for this population. First, stigma, especially negative self-image and public disclosure, plays an important role among IDUs in Malaysia obtaining HIV care or perceiving it to be a re-entry challenge. Mounting research confirms the widespread, persistent and debilitating nature of HIV-related stigma, including in southeast Asia.40,41 Several practices in Malaysia may contribute to the persistence of high public attitudes stigma. For instance, Muslim burial rites require that the body be thoroughly cleansed, and according to public health laws, this must be supervised by police or local health officials. Cleansing is done with bleach for people who are known to be infected with HIV; in rural areas, particularly, this practice threatens to single out families for having had an HIV-infected relative.42 Additionally, HIV contact tracing traditionally involved public health officers making home visits to inform families that they had been exposed to an HIV-infected individual, again reinforcing the societal and individual anxiety and stigma towards HIV/AIDS. In this sample, high public attitudes stigma was significantly associated with identifying difficulty with finding employment and obtaining HIV care. After adjusting for any previous incarcerations and the high number of HIV-related symptoms reported, those reporting high levels of public attitudes stigma were about three times more likely to identify a greater number of re-entry challenges compared with those with low scores. An element of the perception of high public attitudes stigma related to HIV may also be the stigma of being an ex-prisoner.43,44 As a result, HIV-infected prisoners may be disadvantaged in their ability to overcome their re-entry challenges due to the compound stigma they perceive. For instance, stigma in health-care settings can be expressed through breaches of confidentiality, substandard levels of care, refusal to offer services and other forms of discriminatory care.40,41,45 Stigma that is internalized, regardless of the source, can lead to perceptions of unworthiness, shame, guilt and other forms of negative self-image that can complicate efforts towards HIV-treatment-seeking behaviors.29,46,47
Malaysia is now experiencing the kind of stigmatization of HIV-infected marginalized groups that first unfolded three decades ago in the USA.48 Apart from moral judgement, HIV stigma within Malaysian society is largely rooted in the fear of transmission and infection, which has persisted despite past awareness campaigns that HIV cannot be spread by casual and household contact.49 Therefore, novel interventions are needed within the Malaysian context at both the individual and the societal levels to mitigate HIV-related stigma. Guidelines and examples of successful programmes have already been established, including public awareness campaigns of transformation of HIV/AIDS into a chronic but treatable condition.50
Paradoxically, high levels of disclosure stigma did not emerge as a significant correlate of more re-entry challenges. This is surprising, given what is known about the perceived risks and benefits of the decision to disclose one's HIV status in other settings.41,51,52 On the other hand, a greater proportion of those with low levels of disclosure stigma identified difficulty with staying out of prison. Since HIV testing is mandatory upon entry into Malaysian prisons and the majority of subjects in this study had been incarcerated multiple times, these individuals may have perceived less stigma in disclosing their HIV status; however, due to their history of prior incarceration, they may have also been more aware of the difficulties they were likely to face in avoiding future incarceration. It is also surprising that social support indicators, such as having lived with family prior to incarceration or family visits during incarceration, were not significantly associated with identifying fewer re-entry challenges.
In addition to stigma, limited interaction between HIV-infected prisoners and HIV care providers further contributes to inequities in access to care for this population. The lack of interface with appropriate HIV care likely contributed to the low prevalence of identifying difficulty obtaining HIV care in this sample, precisely because these individuals may not be aware of the HIV treatment options available to them or because of the well-known difficulties in obtaining care. Given that high-risk drug and sexual behaviours often continue during53 and after38 incarceration, placing HIV-infected prisoners and their partners54,55 at continued risk for negative health outcomes, it is critical to link HIV-infected prisoners to comprehensive transitional or case management programmes that include HIV and drug treatment services.22
In this study sample, the magnitude of individuals identifying drug treatment as a re-entry challenge also seemed disproportionately low compared with those meeting criteria for opioid dependence. Specifically, 81% met criteria for opioid dependence, a chronic and relapsing disease, yet only 39% reported remaining drug-free as a challenge. It is unclear whether the disconnect between the perceived versus the real need arose from the lack of knowledge concerning effective and newly available pharmacotherapy for the treatment of opioid dependence or the false perception that forced abstinence in prison was effective treatment. Either way, these individuals are at high risk for relapse. Public awareness efforts are urgently needed to facilitate knowledge about opioid dependence as a treatable medical condition, potentially by using methadone or buprenorphine. Such evidence-based treatment modalities have the added benefit of reducing recidivism, the highest ranking re-entry challenge, as well as reducing high-risk HIV behaviours, and improving adherence to HIV and antiretroviral therapy outcomes.5,56–60
At the multivariate level, previous incarcerations, high levels of HIV symptoms and high levels of public attitudes stigma were independently associated with identifying more re-entry challenges. Interventions that reduce the risk of incarceration, perhaps through provision of employment and assistance with drug relapse-prevention (e.g. methadone maintenance), may be especially helpful for this population. HIV treatment, particularly given the high degree of HIV symptoms found in this sample, is profoundly deficient for transitioning prisoners. Unmanaged HIV-related symptoms can reduce prisoners' capacity to engage in the routine tasks that are critical to the success of their long-term reintegration into the community. In this sample, for example, a high number of HIV-related symptoms were found to be associated with difficulty finding employment and getting financial support from family at the bivariate level. Thus, finding ways to effectively link these individuals to effective HIV care is urgently needed to reduce their symptoms and get them back into the workforce.
This study had several limitations. The small sample size and single study site may have reduced the power to detect a greater number of significant associations and the generalisability of the results to all HIV-infected prisoners, respectively. It is also unclear to what extent the perceived difficulties associated with specific re-entry tasks translated into actual difficulties after the subject was released since follow-up analyses were not conducted. Moreover, the cross-sectional nature of the study does not determine causality and confers only an association that must be addressed in prospective, longitudinal studies. Nevertheless, this study provides important insight into community re-entry challenges that HIV-infected male prisoners in Malaysia face upon release, and offers critical insight into potential areas of need for future intervention.
The findings from this study demonstrate that the most prevalent re-entry challenges identified by this sample of HIV-infected, opioid-dependent male prisoners in Malaysia are consistent with the challenges faced by their counterparts around the globe: remaining out of prison, staying off drugs, finding employment and obtaining HIV care. At the same time, however, many of the individuals in this study who met criteria for opioid dependence, frequent recidivism and high HIV symptom indices did not identify these issues as re-entry challenges. It is therefore critical that future evidence-based interventions focus on both treatment and education in order to properly address the re-entry challenges faced by this population.
ACKNOWLEDGEMENTS
The authors would like to thank the University of Malaya Research University Grant 2007 for their funding for these clinical and research efforts as well as the National Institute on Drug Abuse for research (R01 DA025943, Altice) and career development support (K24 DA017072, Altice).
REFERENCES
- 1.Walmsley R. Global Incarceration and Prison Trends. Forum on Crime and Society. UNODC; Vienna: 2003. pp. 65–78. [Google Scholar]
- 2.Walmsley R. World Prison Population List. 8th edn. International Centre for Prison Studies; King's College London: 2009. [Google Scholar]
- 3.National Anti-Drug Agency . Drug Report 2007. Ministry of Home Affairs; Malaysia: 2007. [Google Scholar]
- 4.Seal D, Eldrige G, Kacanek D, Binson D, Macgowan R. A longitudinal, qualitative analysis of the context of substance use and sexual behavior among 18- to 29-year-old men after their release from prison. Soc Sci Med. 2007;65:2394–406. doi: 10.1016/j.socscimed.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 5.UNODC/WHO/UNAIDS . HIV/AIDS Prevention, Care, Treatment and Support in Prison Settings. UNODC; Vienna: 2006. [Google Scholar]
- 6.Springer S, Altice F. Managing HIV/AIDS in correctional settings. Curr HIV/AIDS Rep. 2005;2:165–70. doi: 10.1007/s11904-005-0011-9. [DOI] [PubMed] [Google Scholar]
- 7.Uggen C, Staff J. Work as a turning point for criminal offenders. Corrections Manage Q. 2001;5:1–16. [Google Scholar]
- 8.Freudenberg N, Daniels J, Crum M, Perkins T, Richie B. Coming home from jail: the social and health consequences of community reentry for women, male adolescents, and their families and communities. Am J Public Health. 2008;98:S191–202. doi: 10.2105/ajph.98.supplement_1.s191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Needels KE. Go directly to jail and do not collect? A long-term study of recidivism, employment, and earnings among prison releasees. J Res Crime Delinquency. 1996;33:471–96. [Google Scholar]
- 10.Lanier M, Paoline EA., 3rd Expressed needs and behavioral risk factors of HIV-positive inmates. Int J Offender Ther Comp Criminol. 2005;49:561–73. doi: 10.1177/0306624X04272981. [DOI] [PubMed] [Google Scholar]
- 11.Roman CG. A roof is not enough: successful prisoner reintegration requires experimentation and collaboration. Criminol Public Policy. 2006;3:161–8. [Google Scholar]
- 12.LaVigne NG, Wolf SJ, Jannetta J. Voices of Experience: Focus Group Findings on Prisoner Reentry in the State of Rhode Island. Urban Institute Justice Policy Center; Washington, DC: 2004. [Google Scholar]
- 13.LaVigne NG, Visher C, Castro J. Chicago Prisoners' Experiences Returning Home. Urban Institute Justice Policy Center; Washington, DC: 2004. [Google Scholar]
- 14.Galea S, Vlahov D. Social determinants and the health of drug users: socioeconomic status, homelessness, and incarceration. Public Health Rep. 2002;117:S135–45. [PMC free article] [PubMed] [Google Scholar]
- 15.Belenko S. Assessing released inmates for substance-abuse-related service needs. Crime Delinquency. 2006;52:94–113. [Google Scholar]
- 16.Dolan K, Kite B, Black E, Aceijas C, Stimson G. HIV in prison in low-income and middle-income countries. Lancet Infect Dis. 2007;7:32–41. doi: 10.1016/S1473-3099(06)70685-5. [DOI] [PubMed] [Google Scholar]
- 17.Pearson F, Cleland C, Chaple M, Hamilton Z, Prendergast M, Rich J. Substance use, mental health problems, and behavior at risk for HIV: evidence from CJDATS. J Psychoactive Drugs. 2008;40:459–69. doi: 10.1080/02791072.2008.10400652. [DOI] [PubMed] [Google Scholar]
- 18.Wilper AP, Woolhandler S, Boyd JW, et al. The health and health care of US prisoners: results of a nationwide survey. Am J Public Health. 2009;99:666–72. doi: 10.2105/AJPH.2008.144279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cooke C. Joblessness and homelessness as precursors of health problems in formerly incarcerated African American men. J Nurs Scholarsh. 2004;36:155–60. doi: 10.1111/j.1547-5069.2004.04013.x. [DOI] [PubMed] [Google Scholar]
- 20.Jarrett N, Adeyemi S, Huggins T. Bridging the gap: providing health care to newly released men. J Health Care Poor Underserved. 2006;17:70–80. doi: 10.1353/hpu.2006.0008. [DOI] [PubMed] [Google Scholar]
- 21.van Olphen J, Freudenberg N, Fortin P, Galea S. Community reentry: perceptions of people with substance use problems returning home from New York City jails. J Urban Health. 2006;83:372–81. doi: 10.1007/s11524-006-9047-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Springer S, Pesanti E, Hodges J, Macura T, Doros G, Altice F. Effectiveness of antiretroviral therapy among HIV-infected prisoners: reincarceration and the lack of sustained benefit after release to the community. Clin Infect Dis. 2004;38:1754–60. doi: 10.1086/421392. [DOI] [PubMed] [Google Scholar]
- 23.Glaser J, Greifinger R. Correctional health care: a public health opportunity. Ann Intern Med. 1993;118:139–45. doi: 10.7326/0003-4819-118-2-199301150-00010. [DOI] [PubMed] [Google Scholar]
- 24.Mazlan M, Schottenfeld RS, Chawarski MC. New challenges and opportunities in managing substance abuse in Malaysia. Drug Alcohol Rev. 2006;25:473–8. doi: 10.1080/09595230600883354. [DOI] [PubMed] [Google Scholar]
- 25.UNGASS . UNGASS Country Progress Report. Malaysia: 2008. [Google Scholar]
- 26.Reid G, Kamarulzaman A, Sran SK. Malaysia and harm reduction: the challenges and responses. Int J Drug Policy. 2007;18:136–40. doi: 10.1016/j.drugpo.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 27.Noordin N, Merican M, Rahman H, Lee S, Ramly R. Substitution treatment in Malaysia. Lancet. 2008;372:1149–50. doi: 10.1016/S0140-6736(08)61479-8. [DOI] [PubMed] [Google Scholar]
- 28.Leete R. Kelantan's Human Development Progress and Challenges. UNDP; Kuala Lumpur: 2004. [Google Scholar]
- 29.Berger B, Ferrans C, Lashley F. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001;24:518–29. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- 30.Justice A, Holmes W, Gifford A, et al. Development and validation of a self-completed HIV symptom index. J Clin Epidemiol. 2001;54:S77–90. doi: 10.1016/s0895-4356(01)00449-8. [DOI] [PubMed] [Google Scholar]
- 31.Glaser BG, Strauss A. The Discovery of Grounded Theory: Strategies for Qualitative Research. Aldine Transaction; Chicago: 1967. [Google Scholar]
- 32.Burnett R, Maruna S. So `prison works', does it? The criminal careers of 130 men released from prison under Home Secretary, Michael Howard. Howard J Crim Justice. 2004;43:390–404. [Google Scholar]
- 33.Dhami M, Mandel D, Loewenstein G, Ayton P. Prisoners' positive illusions of their post-release success. Law Human Behav. 2006;30:631–47. doi: 10.1007/s10979-006-9040-1. [DOI] [PubMed] [Google Scholar]
- 34.Visher C, LaVigne N, Farrell J. Illinois Prisoners' Reflections on Returning Home. The Urban Institute; Washington, DC: 2003. [Google Scholar]
- 35.Rich J, Holmes L, Salas C, et al. Successful linkage of medical care and community services for HIV-positive offenders being released from prison. J Urban Health. 2001;78:279–89. doi: 10.1093/jurban/78.2.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marlow E, White M, Tulsky J, Estes M, Menendez E. Recidivism in HIV-infected incarcerated adults: influence of the lack of a high school education. J Urban Health. 2008;85:585–95. doi: 10.1007/s11524-008-9272-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kamarulzaman A. Antiretroviral therapy in HIV-infected patients in Kuala Lumpur, Malaysia. 15th Annual Conference of the Australasian Society for HIV Medicine: Global Crisis, Global Action; Cairns, Australia. 2003. [Google Scholar]
- 38.Aceijas C, Oppenheimer E, Stimson G, Ashcroft R, Matic S, Hickman M. Antiretroviral treatment for injecting drug users in developing and transitional countries 1 year before the end of the `Treating 3 million by 2005. Making it happen. The WHO strategy' (`3 by 5') Addiction. 2006;101:1246–53. doi: 10.1111/j.1360-0443.2006.01509.x. [DOI] [PubMed] [Google Scholar]
- 39.Celentano D, Vlahov D, Cohn S, Shadle V, Obasanjo O, Moore R. Self-reported antiretroviral therapy in injection drug users. JAMA. 1998;280:544–6. doi: 10.1001/jama.280.6.544. [DOI] [PubMed] [Google Scholar]
- 40.Busza J. Promoting the positive: responses to stigma and discrimination in Southeast Asia. AIDS Care. 2001;13:441–56. doi: 10.1080/09540120120057978. [DOI] [PubMed] [Google Scholar]
- 41.Paxton S. The paradox of public HIV disclosure. AIDS Care. 2002;14:559–67. doi: 10.1080/09540120208629674. [DOI] [PubMed] [Google Scholar]
- 42.AIDS/STI Unit . Guidelines for Muslim Burial Rites from a Health Perspective. 2nd edn. Ministry of Health Malaysia; Petaling: 2002. [Google Scholar]
- 43.Pager D. The mark of a criminal record. Am J Sociol. 2003;108:937–75. [Google Scholar]
- 44.Uggen C, Manza J, Behrens A. Less than the Average Citizen: Stigma, Role Transition, and the Civic Reintegration of Convicted Felons. Willan Publishing; Cullompton, Devon: 2004. [Google Scholar]
- 45.Ogden J, Nyblade L. Common at its Core: HIV-related Stigma Across Contexts. International Center for Research on Women; Washington, DC: 2005. [Google Scholar]
- 46.Lee RS, Kochman A, Sikkema KJ. Internalized stigma among people living with HIV-AIDS. AIDS Behav. 2002;6:309–19. [Google Scholar]
- 47.Vanable P, Carey M, Blair D, Littlewood R. Impact of HIV-related stigma on health behaviors and psychological adjustment among HIV-positive men and women. AIDS Behav. 2006;10:473–82. doi: 10.1007/s10461-006-9099-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Novick A. Stigma and AIDS: three layers of damage. J Gay Lesbian Med Assoc. 1998;1:53–60. [Google Scholar]
- 49.Zulkifli SN, Huang SL, Low W, Wong YL. Study on the Impact of HIV on People Living with HIV, their Families and Community in Malaysia Project Report. United Nations Country Team on HIV/AIDS; Malaysia: 2006. [Google Scholar]
- 50.UNAIDS . Reducing HIV Stigma and Discrimination: A Critical Part of National AIDS Programmes. Joint United Nations Programme on HIV/AIDS; Geneva: 2007. [Google Scholar]
- 51.Parson JT, Vanora J, Missildine W, Purcell DW, Gomez CA. Positive and negative consequences of HIV disclosure among seropositive injection drug users. AIDS Educ Prev. 2004;16:459–75. doi: 10.1521/aeap.16.5.459.48741. [DOI] [PubMed] [Google Scholar]
- 52.Chesney MA, Smith AW. Critical delays in HIV testing and care: the potential role of stigma. Am Behav Sci. 1999;42:1162–7. [Google Scholar]
- 53.Dolan K, Wodak A, Hall W. A bleach program for inmates in NSW: an HIV prevention strategy. Aust N Z J Public Health. 1998;22:838–40. doi: 10.1111/j.1467-842x.1998.tb01506.x. [DOI] [PubMed] [Google Scholar]
- 54.Stephenson B, Wohl D, McKaig R, et al. Sexual behaviours of HIV-seropositive men and women following release from prison. Int J STD AIDS. 2006;17:103–8. doi: 10.1258/095646206775455775. [DOI] [PubMed] [Google Scholar]
- 55.Spaulding A, Stephenson B, Macalino G, Ruby W, Clarke J, Flanigan T. Human immunodeficiency virus in correctional facilities: a review. Clin Infect Dis. 2002;35:305–12. doi: 10.1086/341418. [DOI] [PubMed] [Google Scholar]
- 56.Stallwitz A, Stöver H. The impact of substitution treatment in prisons – a literature review. Int J Drug Policy. 2007;18:464–74. doi: 10.1016/j.drugpo.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 57.Lawrinson P, Ali R, Buavirat A, et al. Key findings from the WHO collaborative study on substitution therapy for opioid dependence and HIV/AIDS. Addiction. 2008;103:1484–92. doi: 10.1111/j.1360-0443.2008.02249.x. [DOI] [PubMed] [Google Scholar]
- 58.Larney S, Dolan K. A literature review of international implementation of opioid substitution treatment in prisons: equivalence of care? Eur Addict Res. 2009;15:107–12. doi: 10.1159/000199046. [DOI] [PubMed] [Google Scholar]
- 59.Smith-Rohrberg D, Bruce RD, Altice F. Review of corrections-based therapy for opiate-dependent patients: implications for buprenorphine treatment among correctional populations. J Drug Issues. 2004;34:451–80. [Google Scholar]
- 60.Keen J, Rowse G, Mathers N, Campbell M, Seivewright N. Can methadone maintenance for heroin-dependent patients retained in general practice reduce criminal conviction rates and time spent in prison? Br J Gen Pract. 2000;50:48–9. [PMC free article] [PubMed] [Google Scholar]