Abstract
Background
In 2004, the German federal state of Baden-Württemberg implemented a quality management system for pre-hospital emergency care. Since then, there has been a semi-annual assessment of the frequency of different types of emergency medical interventions and the quality of care.
Methods
The frequencies of different types of intervention were determined and reported both in absolute numbers and as incidence figures, i.e., interventions per 1000 inhabitants per year. The quality of care was rated with the Mainz Emergency Evaluation Score (MEES), and analyses of resuscitation outcomes and guideline implementation were performed.
Results
From 2004 to 2008, there were a total of 524 833 pre-hospital emergency medical interventions in Baden-Württemberg. The annual incidence of emergency interventions rose by 22% over this period (from 16.2 to 19.9 interventions per 1000 inhabitants per year), and the percentage of patients who were severely ill or severely injured rose as well, from 47.3% to 51.1%. The percentage of patients over age 75 rose from 29.1% to 31.3%. 11 858 patients with myocardial infarction (MI) were treated in 2008; the incidence of treatment for MI rose by 60% from 2004 to 2008, from 0.907 to 1.448 interventions per 1000 inhabitants per year. A major improvement in the diagnostic evaluation of MI came about through the purchase of more 12-channel ECG machines. In 2008, the emergency medical teams succeeded in improving the patient’s condition in 69.07% of all cases (77.9% for MI, 63.2% for stroke, 74.4% for multiple trauma). 21 patients per 100 000 inhabitants per year arrived in the hospital alive after out-of-hospital cardiac arrest and pre-hospital resuscitation.
Conclusions
Even in the face of increasing utilization, the quality of emergency medical care in Baden-Württemberg has remained high. Since a quality management system was introduced in 2004, the physicians in charge of emergency medical teams have had access to the data that they need in order to evaluate and further develop the services that they provide.
Emergency medical services provide essential care and are no longer viewed as just a means of transport. The most important duty of these services is qualified emergency medical care and management of acutely ill or severely injured persons on scene and during transport to the nearest suitably equipped hospital. In the Federal Republic of Germany the emergency medical service has become an independent medical entity, as expressed in 1994 by the German Medical Association’s recommendation that the post of “Medical Director, Emergency Services” be created.
In 2004 the Ministry for Work and Social Affairs of the German federal state of Baden-Württemberg set up a quality assurance project for the emergency medical service in order to evaluate the impact of this system and the potential for further development, in cooperation with the cost bearers and service providers (self-governing bodies) and with expert support from the Southwest German Emergency Physicians’ Working Group (Arbeitsgemeinschaft Südwestdeutscher Notärzte, agwsn).
Following an official recommendation, by the year 2008 some 106 of the 130 local emergency medical services in the state of Baden-Württemberg had joined this project. The operational organization of the quality assurance system has been described elsewhere and is not discussed in full here (1).
The present investigation took advantage of the state-wide data of the NADOK project in Baden-Württemberg to analyze the spectrum and frequency of interventions by the emergency medical services, together with the quality of care provided, over a period of four years. The results of this analysis can be used to aid decisions on the future development of the emergency medical service.
Materials and methods
Every intervention by an emergency physician is documented in writing and recorded electronically in the framework of the NADOKTM or NADOKliveTM system. Each of the 106 participating local services exported the relevant data in a defined format (2) at six-monthly intervals (3). These intervention data were analyzed by an independent body via the fiduciary agency of the State Medical Association (Landesärztekammer) of Baden-Württemberg. The populations of the areas covered by the individual emergency medical services were derived from the records of the State Statistics Office of Baden-Württemberg for inhabitants registered in the year 2007.
An intervention by an emergency physician was deemed “evaluable” when logical and formal checks of the data fields revealed no violation of plausibility. Age and the durations of all stages of the intervention had to be recorded; interventions simply involving patient transfer from one institution to another were excluded, as were those in which death was merely confirmed.
The quality of emergency medical care was ascertained and analyzed by means of established scores such as the Mainz Emergency Evaluation Score (MEES), the Delta-MEES, and the National Advisory Committee for Aeronautics (NACA) Score (4, 5).
The MEES measures the vital functions of an emergency patient. The status of each of seven vital parameters is classified into four categories: normal (4 points), slightly abnormal (3 points), severely abnormal (2 points), and life-threatening (1 point). The total score on initial assessment is termed MEES1; the total score at handover, MEES2. The difference between MEES2 and MEES1, known as Delta-MEES, represents the quality of care. A positive difference of 2 points or more is counted as improvement in the patient’s condition, a negative difference of 2 points or more as worsening. A difference of only 1 point is classified as no change. The vital functions measured are heart rate, systolic blood pressure, respiratory rate, and oxygen saturation, together with ECG rhythm, Glasgow Coma Score, and degree of pain.
The NACA scoring system is employed internationally to describe the severity of injury and illness in emergency medicine. NACA I and NACA II stand for mild to moderate deviation from normal, NACA III indicates a severe but not life-threatening condition, NACA IV does not exclude short-term progression to a life-threatening state, NACA V means acute danger to life, NACA VI stands for successful resuscitation, and NACA VII represents death. The worst status during the period of emergency medical care is recorded.
The majority of analyses were descriptive. The frequency of emergency physician deployments was expressed in absolute terms and as an annual rate per 1000 inhabitants. Relative frequencies (percentages) were calculated throughout, mean values and confidence intervals where appropriate. The t-test and the chi-square test were used to calculate significance. A probability of error of <5% was considered to show a statistically significant difference. The statistical software SPSS 14.0 was used for analysis.
Results
Baden-Württemberg, with a population of 10.74 million, has emergency medical teams based at 130 locations. Of these 130 teams, 106 participated in our study. In 2008 they provided a total of 162 724 data sets, 43 605 more than in 2005.
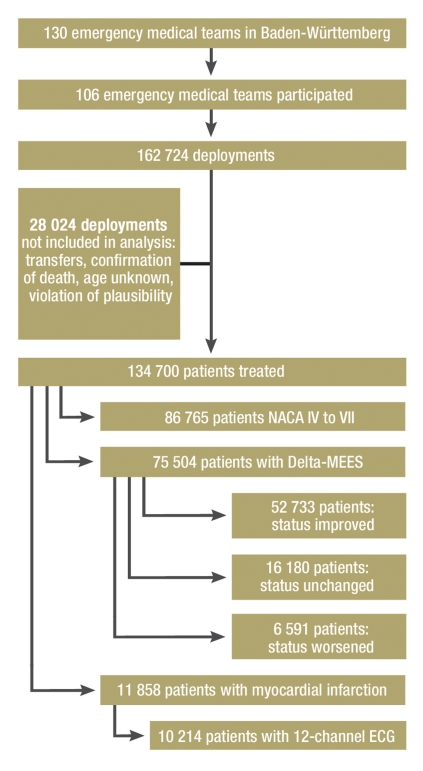
The 144 069 evaluable emergency physician deployments in the year 2008 contributed data on 134 700 patients, a significant increase of 27 525 (25.7%) compared with 2005 (Figure 1, Table 1).
Figure 1.
Case numbers in 2008: classification of 134 700 treated patients with regard to NACA category (severity), Delta-MEES (treatment success), and diagnosis of myocardial infarction
Table 1.
| 2005 | 2006 | 2007 | 2008 | Total | Mean | SD | |
| Number of teams participating | 98 | 103 | 105 | 106 | |||
| Population represented (%) | 7350 360 (70.2) | 7 752 623 (74.0) | 8 138 60 (77.7) | 8 186 430 (78.2) | |||
| Data sets = deployments | 119 119 | 133 133 | 147 220 | 162 724 | 562 196 | 140 549 | 18 712 |
| Evaluable deployments (%) | 114 725 (96.31) | 126 106 (94.72) | 139 933 (95.04) | 144 069 (88.54) | 410 108 | 131 208 | 13 407 |
| Patients treated | 107 175 | 117 598 | 130.270 | 134 700 | 489 743 | 122 436 | 12 491 |
| NACA IV to VII (%) | 50 728 (47.34) | 58 184 (49.48) | 65284 (47.97) | 68 765 (51.05) | 242 961 | ||
| Deployments/1000 inhabitants/year | 16.2 | 17.2 | 18.1 | 19.9 | |||
| p-Value | |||||||
| Delta-MEES present (%) | 63 988 (75.3) | 68 617 (72.89) | 71 860 (68.54) | 75 504 (69.07) | <0.001 | ||
| Arrival time ≥ 15 minutes (%) | 98 418 (91.83) | 107 978 (91.82) | 119 396 (91.65) | 123 989 (92.05) | 0.8625 | ||
| Children under 7 years (%) | 3901 (3.6) | 4164 (3.5) | 4611 (5.5) | 4697 (3.5) | |||
| Children under 7/1000 inhabitants/year | 0.531 | 0.537 | 0.567 | 0.574 | <0.001 | ||
| Patients >75 years (%) | 31 238 (29.1) | 34 836 (29.6) | 39 565 (30.4) | 42 137 (31.3) | |||
| Patients >75 years/1000 inhabitants/year | 4.25 | 4.493 | 4.862 | 5.147 | <0.001 | ||
| Diagnosis: myocardial infarction (%) | 6666 (6.2) | 8970 (7.6) | 10 762 (8.3) | 11 858 (8.8) | |||
| Proportion thereof with 12-channel ECG (%) | 3468 (52) | 6182 (68.9) | 8554 (79.5) | 10 214 (86.1) | <0.001 | ||
| Diagnosis: myocardial infarction/1000 inhabitants/year | 0.907 | 1.157 | 1.322 | 1.448 | <0.001 | ||
| Resuscitations | 5188 | 5798 | 5802 | 5008 | |||
| Successful resuscitation (%) | 1461 (28.16) | 1687 (29.1) | 1696 (29.23) | 1705 (34.05) | |||
| Unsuccessful resuscitation | 3727 | 4111 | 4106 | 3303 | |||
| Resuscitations/100000 inhabitants/year | 71 | 75 | 71 | 61 | <0.001 | ||
| Successful resuscitations/100000 inhabitants/year | 19.88 | 21.76 | 20.84 | 20.83 | 0.0957 | ||
| Medications per patient | 1.16 | 1.2 | 1.18 | 1.19 | <0.001 | ||
| Total medications given | 124 657 | 140 913 | 153 247 | 160 688 | |||
| Analgesics (%) | 25 600 (23.89) | 28 070 (23.87) | 30 357 (23.3) | 32 138 (23.86) | |||
| Sedatives (%) | 18 345 (17.12) | 19. 78 (16.73) | 20 928 (16.07) | 21 351 (15.85) | |||
| Heparin or ASA (%) | 16 324 (15.23) | 17 506 (14.89) | 18 492 (14.2) | 19 100 (14.1) | |||
| Antiarrhythmic agents (%) | 8348 (7.79) | 8037 (6.83) | 8088 (6.21) | 10 955 (8.16) | |||
| Peripheral vein cannulation (%) | 87 724 (81.85) | 97 227 (82.68) | 107 474 (82.5) | 110 986 (82.39) |
SD, standard deviation
The populations covered by the participating emergency medical services represented 78.2% of the total inhabitants of Baden-Württemberg in 2008. The emergency medical utilization rate was equivalent to 19.9 deployments per 1000 inhabitants per year.
In more than two thirds of cases a consultant was deployed. The figure was 60.8% in 2005 and 68.1% in 2008. In the year 2008 anesthetists were involved in 51.7% of cases, internists in 28.4%, and surgeons in 10.8%.
As a criterion of complete documentation we checked for the presence of Delta-MEES data on the seven vital parameters measured by MEES. Rates of 75.3% to 69.07% were recorded.
The time that elapsed between alerting the emergency service and arrival of the team on scene was less than 15 minutes in 91.65% to 92.05% of cases.
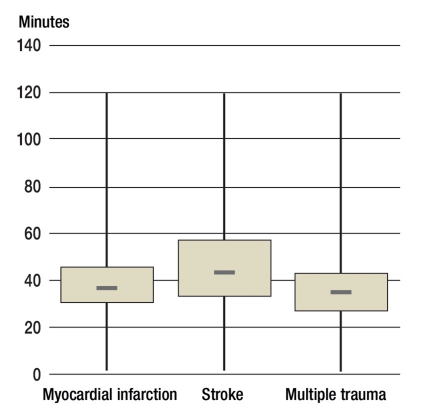
The period between arrival on scene and handover to hospital staff is used for diagnosis and treatment as well as transport. This time remained more or less constant over the study period for the tracer diagnoses myocardial infarction, multiple trauma, and stroke. However, the care and transport of multiple trauma victims took less time than that of stroke patients (median 43 minutes in 2008) (figure 2).
Figure 2.
Box plot (median and interquartile range) showing the duration of pre-hospital care from arrival on scene to hospital handover for the tracer diagnoses myocardial infarction, stroke, and multiple trauma. The shortest times were attained in patients with multiple trauma.
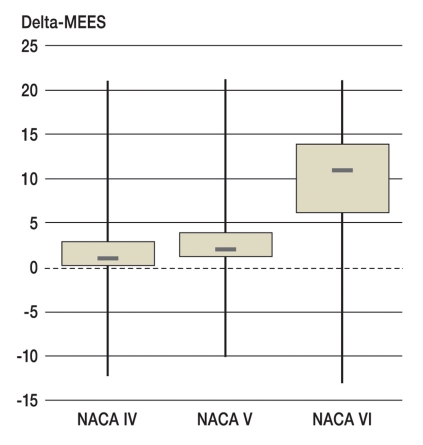
An improvement in status as assessed by Delta-MEES was attained in more than two thirds of patients. As can be seen from Figure 3, emergency medical intervention achieves the greatest improvement in patients with severely compromised vital functions: those classified as NACA VI showed a median Delta-MEES of +11. All vital functions in this group of patients exhibit pathological disruption but can improve markedly in response to appropriate treatments.
Figure 3.
Box plot (median and interquartile range) showing the improvement in Delta-MEES, corresponding to improvement in vital functions, in patients assigned to NACA classes IV, V, and VI. Severely ill and severely injured patients benefit most from emergency medical care.
While the proportion and absolute number of patients over 75 years of age increased significantly year by year, the proportion of emergencies involving young children remained static (table 1).
The most frequent diagnosis was myocardial infarction, which rose from 0.907 to 1.448 cases per 1000 inhabitants per year. It should be underlined that the diagnosis was increasingly confirmed by the use of 12-channel ECG before arrival at the hospital.
The Delta-MEES data revealed that patients with a myocardial infarction improved the most after emergency medical intervention, stroke patients the least. However, the role of the emergency medical team in the latter group is essentially restricted to stabilization of vital functions and optimization of the logistics of care. Multiple trauma victims respond well to treatment overall, but deterioration cannot always be prevented (table 2).
Table 2. Change in status of patients with tracer diagnoses according to Delta-MEES.
| Diagnosis | Myocardial infarction | ||||
| Year | 2005 | 2006 | 2007 | 2008 | p |
| n | 5596 | 7538 | 8241 | 9318 | |
| Improved (%) | 4472 (79.91) | 5862 (77.77) | 6472 (78.53) | 7259 (77.9) | 0.001 |
| Unchanged (%) | 721 (12.88) | 1040 (13.8) | 1165 (14.14) | 1331 (14.28) | 0.003 |
| Worse (%) | 403 (7.2) | 636 (8.44) | 604 (7.33) | 728 (7.81) | 0.003 |
| Diagnosis | Stroke | ||||
| Year | 2005 | 2006 | 2007 | 2008 | |
| n | 6909 | 7269 | 7806 | 8224 | |
| Improved (%) | 4577 (66.25) | 4719 (64.92) | 5064 (64.87) | 5196 (63.18) | <0.001 |
| Unchanged (%) | 1706 (24.69) | 1875 (25.79) | 2008 (25.27) | 2262 (27.5) | 0.012 |
| Worse (%) | 626 (9.06) | 675 (9.29) | 734 (9.4) | 766 (9.31) | <0.001 |
| Diagnosis | Multiple trauma | ||||
| Year | 2005 | 2006 | 2007 | 2008 | |
| n | 431 | 516 | 587 | 630 | |
| Improved (%) | 319 (74.01) | 390 (75.58) | 442 (75.3) | 469 (74.44) | 0.001 |
| Unchanged (%) | 50 (11.6) | 60 (11.63) | 71 (12.1) | 77 (12.22) | 0.001 |
| Worse (%) | 62 (14.39) | 66 (12.79) | 74 (12.61) | 84 (13.33) | <0.001 |
The number of resuscitations rose in 2006 and again in 2007, but in 2008 it fell to below the figure for 2005. The selection implied in the lower number of attempted resuscitations led to an improvement in the resuscitation success rate. The recorded incidence of 71 to 61 resuscitation attempts per 100 000 inhabitants corresponds to the reference data of the American Heart Association (AHA) (6).
Between 81% and 83% of emergency patients had a peripheral venous access created and therefore received an infusion. An average of 1.2 medications were administered per patient. Analgesics and sedatives were used most frequently, but anticoagulants and antiarrhythmic agents were also commonly given.
Discussion
The general population expects and demands high-quality emergency medical care by emergency physicians. According to Section V of the German Social Code (Sozialgesetzbuch), however, cost effectiveness of the services provided has priority. Utilization of the pre-hospital emergency services is increasing by 3% to 5% yearly; the rate of deployment of emergency physicians depends on the population density. A sample survey (7) indicated a rate of 24.1 emergency physician call-outs per 1000 inhabitants per year in 2004/2005.
In contrast, we present routine data from a continuous survey of a large region that also yield information on the medical quality of emergency care provision in a densely populated German federal state. Emergency physicians attended 119 119 incidents in 2005 and 162 724 incidents in 2008, an increase from 16.2 to 19.9 per 1000 inhabitants per year over a four-year period.
The emergency medicine services have responded to this increase in demand by improving the content and structure of provision. Scientifically based guidelines and care strategies are reflected in the treatment given at the site of the incident (8).
This achieves comparability of results despite the wide heterogeneity of structural conditions (9, 10).
In Baden-Württemberg, characteristic of the general lack of established quality assurance structures, there is no post of “Medical Director, Emergency Services” whose holder is responsible for quality management (QM) in emergency service provision. This function is partially assigned to the Senior Emergency Physician on the District Committee (Leitender Notarzt im Bereichsauschuss). Thus the NADOK analysis assumes special importance as the sole QM instrument.
Robust data resulting from complete, valid documentation of all emergency service interventions are necessary for analysis. Documentation during an intervention is still predominantly manual. On subsequent computer input, high data quality can be enforced by stringent plausibility checks. In contrast to other publications, the documentation system we used for this study (NADOKTM) is characterized by a high proportion of evaluable cases (11).
Baden-Württemberg’s decision to adopt semi-annual central evaluation of uniformly documented routine data from individual local emergency physicians has therefore led to the availability of structure and process data that permit longitudinal analysis. The quality of medical care and other aspects of pre-hospital emergency medicine thus becomes transparent (3).
The limitations of our study result from the fact that the data are recorded without uniform training. Rather than compulsory site-specific quality criteria, adherence to generally accessible guidelines was required.
Some of our findings suggest that action needs to be taken. First of all, the structure quality in terms of time from alert to arrival and availability of technical resources in the form of 12-channel ECG and capnometry devices failed by far to satisfy the requirements of DIN 75079 and the current state of knowledge in emergency medicine. This represents a structural deficit.
Genzwürker et al. established that 12-channel ECG was available to 52.6% of emergency medical teams in 2001 (12), but to 89.7% in 2005 (13). Our findings confirm this trend. Longitudinal data on the rate of myocardial infarctions diagnosed by means of 12-channel ECG show clearly how this deficit too was favorably influenced by the then newly initiated quality assurance procedures, thus improving process quality. Most recently, a 12-channel ECG examination was carried out in 86.1% (n = 10 214) of patients suspected to have suffered a myocardial infarction.
Outcome quality is depicted by the recognized MEES system. Determination of the Delta-MEES requires complex calculations involving two values of each of seven vital parameters. Good documentation quality can thus be assumed if a Delta-MEES is recorded. Rates exceeding 80% are achieved by one third of local emergency services. However, the quality of documentation could not be maintained and improved with an increasing number of participants. This effect can be attributed to the fact that the QM system is not yet fully developed.
We considered myocardial infarction, stroke, and multiple trauma as tracer diagnoses. They count among the “first hour” emergencies, i.e., those in which the patient’s fate is determined in the first 60 minutes.
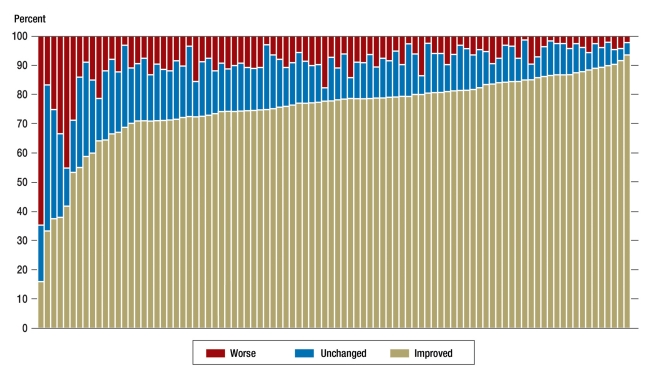
Both in emergencies as a whole and in the patients with tracer diagnoses, the action taken by the emergency physician achieves a significant improvement in status in two thirds of cases. Only in a small proportion of patients can worsening not be prevented. A glance at the individual results (figure 4), however, reveals differences that clearly underline the importance of QM. This benchmark graph shows the potential for improvement on the part of emergency service teams at some locations.
Figure 4.
Benchmark graph showing the outcome quality of each individual emergency services team for the care of patients with myocardial infarction in 2008. The distribution of Delta-MEES values into better, unchanged, or worse varies among the locations
With regard to the NACA classification, the indications for the utilization of emergency physicians’ services have shifted little over time. Thus, almost half of the deployments are for significant emergency medical indications (patients with manifest or threatened compromise of vital functions). According to Bernhard et al., these deployments are associated with higher patient numbers and more problems (14). Emergency physicians are therefore confronted significantly more often with critical situations and patients: resuscitations and children under 7 years of age.
Corresponding to the demographic development of the general population, case numbers have naturally increased particularly sharply in the over-75s. This age group, with its typical morbidity patterns, makes up almost one third of the total number of emergency patients.
On the one hand the proportion of emergencies in which a consultant is deployed arouses expectations with regard to adequate quality of care, but on the other hand the “consultant standard” is already satisfied in two-thirds of cases even before the patient reaches the hospital.
Treatment with effective medications is a unique feature of (emergency) physicians’ activity. In comparison with systems in which emergency physicians are not active, the efficacy of the substances used has been shown to be relevant to the outcome (15). Medicinal treatment plans are usually defined in standard operating procedures, and these are employed particularly in the tracer diagnoses (16).
Central aspects such as the proportion of interventions within the legally prescribed response time (arrival within 15 minutes in 95% of cases in a given year) came to public attention through the acquisition and comparison of data from the whole federal state. Only recently have they resulted in a series of long overdue structural changes. The responsible authorities in Baden-Württemberg, working together with the emergency medical dispatch centers, developed means of determining the legal response time. As expected, the results were under the times reported here. As a consequence, enduringly effective quality assurance procedures had to be set up.
In 2008, based on a broad consensus and scientific evidence from experts, key points were formulated for the emergency medical management of the time-critical emergencies myocardial infarction, stroke, multiple trauma, and severe head injury (17). It would seem reasonable for these key points to be reflected in the quality assurance system. Owing to sector- and system-overlapping data interfaces between outpatient and inpatient treatment, the times specified in the key points cannot be derived from routine data, but have to be gathered—if at all—from study or registry data (18). However, this is urgently necessary in order to permit rapid ascertainment of the consequences of changes in allocation strategies or patient behavior (19). Direct delivery to a cardiac catheterization unit is already the norm in many centers, but there is no central collection of data to prove the effect of this practice on outcome quality (20). However, the pre-hospital times revealed by our study confirm the target times laid down in the key points (21).
In principle, all hospitals that care for trauma patients and serve as base for an emergency medical service can participate in the trauma register of the German Society for Trauma Surgery (Deutsche Gesellschaft für Unfallchirurgie) (22). The trauma register’s site-specific quality report contains cross-system outcome-relevant data, including pre-hospital times. The same is true for the resuscitation register of the German Society for Anesthesiology and Intensive Care Medicine (Deutsche Gesellschaft für Anästhesiologie und Intensivmedizin), where the outcome quality is also presented in cross-sector fashion (23).
The procedures introduced here present data on emergency medical care that were previously not available in this form of continuous evaluation. In light of the significant improvement in patient status that has been achieved, we believe our conclusions are confirmed by those recently drawn by a panel of experts in the federal state of Hesse (24) and assume that the associated decrease of 200 euros per case in subsequent inpatient treatment costs found in Hesse also applies to Baden-Württemberg. Thus, independent of the health benefit for the individual, the increasing quality of emergency medical care relieves the burden on the healthcare system as a whole.
Key Messages.
Eighty percent of emergency physicians in Baden-Württemberg participate in a statewide quality project that was set up in 2004.
The incidence of emergency physician deployments rose by 22% (from 16.2 to 19.9 per 1000 inhabitants per year) and the proportion of severely ill or injured patients increased from 47.3% to 51.1%.
In two thirds of all patients emergency medical treatment by physicians achieved a discernible improvement in general status and in vital functions.
Quality indicators confirm the persisting effect of pre-hospital emergency medical care.
The interpretation of local results assists the physicians in charge of emergency medical teams in their quality management.
Acknowledgments
Translated from the original German by David Roseveare.
Footnotes
Conflict of interest statement
Dr. Messelken is a consultant for Datapec (Pliezhausen, Germany), the developer and distributor of NADOK and NADOKlive. The remaining authors declare that no conflict of interest exists according to the guidelines of the International Committee of Medical Journal Editors.
References
- 1.Messelken M, et al. Externe Qualitätssicherung im Rettungsdienst. Notfall & Rettungsmedizin. 2005;8:476–483. [Google Scholar]
- 2.Messelken M, Schlechtriemen T. Der minimale Notarztdatensatz MIND2. Notfall & Rettungsmedizin. 2003;6:189–192. [Google Scholar]
- 3.Messelken M, Dirks B. Zentrale Auswertung von Notarzteinsätzen im Rahmen externer Qualitätssicherung. Notfall & Rettungsmedizin. 2001;4:408–415. [Google Scholar]
- 4.Hennes HJ, Reinhardt T, Dick W. Beurteilung des Notfallpatienten mit dem Mainz Emergency Evaluation Score MEES. Notfallmedizin. 1992;18:130–136. [Google Scholar]
- 5.Tryba M, Brüggemann H, Echtermeyer V. Klassifizerung von Erkrankungen und Verletzungen in Notarztrettungssystemen. Notfallmedizin. 1980;6:725–727. [Google Scholar]
- 6.Sayre MR, Cantrell S, White LJ, Hiestand BC, Keseg DP, Koser S. Impact of the 2005 American Heart Association cardiopulmonary resuscitation and emergency cardiovascular care guidelines on out-of-hospital cardiac arrest survival Prehosp. Emerg Care2. 009;13:469–477. doi: 10.1080/10903120903144965. [DOI] [PubMed] [Google Scholar]
- 7.Schmiedel R, Behrendt H. Leistungen des Rettungsdienstes 2004/05. Berichte der Bundesanstalt für Straßenwesen - Mensch und Sicherheit. 2007;M 188 [Google Scholar]
- 8.Arntz H-R, Tebbe U, Schuster HP, Sauer G, Meyer J. Leitlinien zur Diagnostik und Therapie des akuten Herzinfarktes in der Prähospitalphase. Notfall & Rettungsmedizin. 2000;3:347–554. [Google Scholar]
- 9.Gottwik MG, Senges J. Kommentar zum 22. Bericht über die Leistungszahlen der Herzkatheterlabors in der Bundesrepublik Deutschland. Kardiologe. 2008;2:325–326. [Google Scholar]
- 10.DGU, D.G.f.U. Weißbuch Schwerverletzten-Versorgung. 2006 [Google Scholar]
- 11.Sefrin P, Brandt M. Das DIVI - Notarztprotokoll als Basis für ein Qualitätsmanagement im Rettungsdienst. Der Notarzt. 2001;17(Sonderheft 1):68–70. [Google Scholar]
- 12.Genzwürker H, et al. Ausstattung von Notarztbesetzten Rettungsmitteln in Baden-Württemberg. Anaesthesist. 2002;51:367–373. doi: 10.1007/s00101-002-0303-z. [DOI] [PubMed] [Google Scholar]
- 13.Genzwürker H, et al. Strukturqualitat im Notarztdienst. Vergleich der Ausstattung arztbesetzter Rettungsmittel in Baden-Wurttemberg in den Jahren 2001 und 2005. Anaesthesist. 2007;56:665–672. doi: 10.1007/s00101-007-1194-9. [DOI] [PubMed] [Google Scholar]
- 14.Bernhard M, et al. Patientenspektrum im Notarztdienst. Was hat sich in den letzten 20 Jahren geändert? Anaesthesist. 2006;55:1157–1165. doi: 10.1007/s00101-006-1106-4. [DOI] [PubMed] [Google Scholar]
- 15.Fischer M, et al. Effektivitats- und Effizienzvergleich der Rettungsdienstsysteme in Birmingham (UK) und Bonn (D) Anasthesiol Intensivmed Notfallmed Schmerzther. 2003;38:630–642. doi: 10.1055/s-2003-42507. [DOI] [PubMed] [Google Scholar]
- 16.Ohmann C, Jonas M, Röhrborn A. Madler C, editor. Algorithmen, Expertensysteme und Pathways Akutmedizin - Die ersten 24 Stunden.München, Jena. Urban & Fischer. 2009:169–184. [Google Scholar]
- 17.Altemeyer KH, Dirks B, Lackner CK, Schindler KH. Notfallmedizinische Versorgung der Bevölkerung - Eckpunkte aus akutmedizinischer Sicht. Anästhesiologie und Intensivmedizin. 2009;1:60–62. [Google Scholar]
- 18.Zeymer U, et al. Reperfusion rate and inhospital mortality of patients with ST segment elevation myocardial infarction diagnosed already in the prehospital phase: results of the German Prehospital Myocardial Infarction Registry (PREMIR) Resuscitation. 2009;80:402–406. doi: 10.1016/j.resuscitation.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 19.Gärtner C, Walz L, Bauernschmitt E, Ladwig KH. Patientenbezogene Determinanten der prähospitalen Verzögerung beim akuten Myokardinfarkt. Dtsch Arztebl Int. 2008;105(15):286–291. doi: 10.3238/arztebl.2008.0286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Scholz KH, Knobelsdorf G, et al. Prozessentwicklung in der Herzinfarktversorgung. Herz. 2008;33:102–109. doi: 10.1007/s00059-008-3120-6. [DOI] [PubMed] [Google Scholar]
- 21.Werf v.d. F. Management of acute myocardial infarction in patients presenting with persisting ST-Segment elevation. European Heart Journal. 2008;29:2909–2945. doi: 10.1093/eurheartj/ehn416. [DOI] [PubMed] [Google Scholar]
- 22.Leidel BA, Kanz K. Die interdisziplinäre Notfallaufnahme aus chirurgisch-traumatologischer Sicht. Notfall Rettungsmed. 2009;12:267–276. [Google Scholar]
- 23.Gräsner JT, et al. A national resuscitation registry of out-of-hospital cardiac arrest in Germany—a pilot study. Resuscitation. 2009;80:199–203. doi: 10.1016/j.resuscitation.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 24.Herdt J, Karbstein M Report Nr 761 HA Hessen Agentur GmbH Wiesbaden. Effektivität und Effizienz des Rettungsdienstes in Hessen. 2009 [Google Scholar]