Abstract
Objective
To investigate the prevalence of arthritis and associations with arthritis in American Indian and Alaska Native populations.
Methods
Data on self-reported, doctor-diagnosed arthritis from the baseline visit of 9,968 American Indian and Alaska Native adults from Alaska and the Southwest US were included. The prevalence of arthritis and univariate and multivariate associations between arthritis and demographic characteristics, health-related factors, and treatment are described.
Results
The prevalence of self-reported arthritis increased with age. The age-sex adjusted prevalence was high in Alaska (26.1%) and low in the Southwest US (16.5%) as compared with the US population (21.5%). In both centers, arthritis was associated with age, lack of employment, chronic medical conditions, and poorer self-reported overall health. Arthritis was associated with female sex in Alaska only, whereas education, marital status, and urban residency were associated with arthritis in the Southwest US. In both centers, self-reported physical health measured by the Short Form 12 Health Survey was lower in people with arthritis, and mental health was not associated with arthritis. More frequent use of antiinflammatory medications was reported with arthritis in both centers, but increased use of traditional medicine and healers were associated with arthritis only in Alaska.
Conclusion
Compared with US rates, the prevalence of self-reported arthritis was higher among Alaska Native people and lower in a Southwest American Indian population. Some factors associated with arthritis differ between the 2 populations.
INTRODUCTION
The burden of arthritis in the US is periodically estimated by surveillance studies. The National Health Interview Survey (NHIS), a household interview survey, found the age-adjusted prevalence of self-reported, doctor-diagnosed arthritis in the US between 2003 and 2005 to be 21.5% (1). The Behavioral Risk Factor Surveillance System (BRFSS), a telephone survey, provides annual state-based estimates of the prevalence of arthritis using a case definition of arthritis that includes both self-reported, doctor-diagnosed arthritis and chronic joint symptoms (2,3). The 2005 BRFSS found the unadjusted prevalence of arthritis to range from 22.1% to 34.9% in the US (4). The NHIS has found an increased prevalence of self-reported arthritis among older people, women, people with lower levels of education or physical activity, and those with a higher body mass index (BMI) (1). In Australia, the Victorian Population Health Survey recently found an arthritis prevalence of 23% overall, and confirmed an association of arthritis with age, sex, education, and BMI. In addition, the Victorian Population Health Survey found that self-reported arthritis was more common in people of lower socioeconomic status and that people with arthritis had a poorer self-reported health status (5).
Increased prevalence of specific types of arthritis has been reported in some American Indian and Alaska Native populations. These include rheumatoid arthritis (6,7), spondylarthropathy (7,8), and systemic lupus erythematosus (7,9). Although American Indian and Alaska Native people are included in the US national and state-based surveillance studies, they represent a small proportion of the overall population. Furthermore, most analyses report prevalence of self-reported arthritis by racial/ethnic categories including only white, African American, Hispanic, and other, making it difficult to draw any conclusions about American Indian and Alaska Native people. In the 2002 NHIS, arthritis was reported with a similar prevalence in white and African American respondents, while Hispanics and “other/multiple race” people reported arthritis less frequently (10). Recent analysis of the NHIS data from 2002–2003 separated American Indian and Alaska Native people from other races and found a higher prevalence of arthritis in this population, with an odds ratio (OR) of 1.58 compared with the white population (11). Differences between American Indian and Alaska Native tribes or regions, and associations between self-reported arthritis and demographic or health-related factors, have not been explored in these populations.
The Education and Research Towards Health (EARTH) study was designed as the baseline enrollment phase of a prospective cohort study to evaluate the risk and protective factors for chronic diseases among American Indian and Alaska Native adults. Participants provided information on self-reported medical conditions in addition to multiple demographic, lifestyle, cultural, and health-related factors. The aim of this analysis was to determine the prevalence of self-reported, doctor-diagnosed arthritis and associated demographic and health-related factors in the EARTH study population.
PARTICIPANTS AND METHODS
Study population
Participants were recruited in Alaska and the Southwest US. In Alaska, participants were recruited from 26 communities in 3 distinct regions of the state. In the Southwest US, participants were recruited on the Navajo Nation from 2 stationary locations and in a mobile van that traveled throughout the same area. In each community, attempts were made to enroll all residents of the community who met the following inclusion criteria: American Indian or Alaska Native eligible for Indian Health Service health care, age ≥18 years, not pregnant, not actively undergoing chemotherapy, and physically and mentally able to understand the consent form and to complete survey instruments. Recruitment began in March 2004; data are included from participants enrolled prior to March 1, 2007.
This study was approved by the Alaska Area Institutional Review Board, the Navajo Nation Human Research Review Board, the Indian Health Service National Institutional Review Board, and the University of Utah Institutional Review Board. Regional, local, and village tribal health boards and chapters within local health boards approved and supported the study. A Tribal Advisory Board and a Scientific Advisory Board provided oversight for the study.
Data collection
Detailed methods have been described previously (12). Briefly, at the study visit participants completed questionnaires administered by audio computer-assisted self-interview (ACASI) using a touch-screen computer. These included a detailed health, lifestyle, and physical activity (HLPA) questionnaire and a diet history questionnaire. The HLPA questionnaire contained questions on self-reported medical conditions, physical and mental health status (Short Form 12 Health Survey [SF-12]) (13), physical activity, lifestyle, cultural factors (including language spoken at home and degree of identification with tribal traditions), use of nonsteroidal antiinflammatory drugs (NSAIDs) and aspirin, and use of traditional medicines or traditional healers. Demographic data were collected, including age, sex, level of education, employment, marital status, household income, and location of residence. Questionnaires were designed in collaboration between the EARTH coordinating center and field offices with tribal input. The questionnaires were translated into Yup’ik and Navajo audio files by fluent speakers trained in the study methodology, with consultation or adjudication by at least 1 other native speaker to ensure consistency. Participants could choose to hear the questionnaire read in English, Yup’ik, or Navajo, and could switch between languages at any time (14). In a usability study of participants in the Southwest US, 97.2% of participants reported that the ACASI questionnaires were easy to use, and the mean combined completion time for the HLPA and diet history questionnaires was 65 minutes (14). Medical measurements were performed, including height, weight, waist and hip circumference, blood pressure, and fasting glucose and lipid panel. Quality control procedures were in place to ensure standardized data collection across centers.
Definition of variables
In this study, arthritis is defined as an answer of yes to the question: “Did a doctor or other health care provider ever tell you that you had some form of arthritis including osteoarthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?” Based on tribal input during questionnaire development, this is a slight modification of the question currently asked in the NHIS and BRFSS: “Have you ever been told by a doctor or other health care professional that you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?”
The demographic and socioeconomic variables analyzed included age at study visit, sex, education, employment, urban or rural residence, marital status, and household income. Education was defined as less than high school (did not complete high school) versus high school or greater (completed high school, General Educational Development certification, or a higher level of education). Employment status was defined as currently employed (employed for wages, self-employed, between seasonal jobs, or out of work for less than 1 year) or not employed (out of work for more than 1 year, homemaker, student, retired, or disabled). Location of residence was defined as urban or rural based on zip code using the 2000 US Census definition of urban areas (a population of 50,000 or greater). Based on this definition, the only urban recruitment site was in Southcentral Alaska (Anchorage). Marital status was defined as married (married or living as married) or not married (divorced, separated, widowed, or never married). Household income was dichotomized as ≥$15,000/year versus <$15,000/year, because this approximately represented the median household income of the study population. The analysis was stratified by study center (Alaska or Southwest US). Regional differences between the 3 recruitment sites in Alaska were also analyzed (Southcentral, Southeastern, and Southwestern Alaska). Language spoken at home was categorized as American Indian/Alaska Native language only, American Indian/Alaska Native language and English, English only, or other. Participants reporting other were excluded from analyses with arthritis due to the small sample size. Degree of identification with tribal traditions was categorized as a lot/some versus a little/not at all.
A count of chronic medical conditions was created by summing self-reported medical conditions from the HLPA questionnaire, excluding arthritis. The conditions included were high blood pressure, heart disease, high cholesterol, stroke, gallbladder disease, kidney failure, liver disease, thyroid disease, asthma, chronic obstructive pulmonary disease, glaucoma, cataract, depression, diabetes, and cancer. Physical activity was classified as vigorous based on activities scored as requiring ≥6.0 metabolic equivalents (15), and hours per week of vigorous activity were calculated. Three categories of vigorous activity were included: no vigorous activity, >0 to <2.5 hours per week, and ≥2.5 hours per week. Only vigorous activity was included based on physical activity validation data from this study showing that vigorous activity was better recalled than moderate activity (Murtaugh M, et al: unpublished observations).
BMI was calculated based on the standard formula (kg/m2) using height and weight measured at the baseline study visit, and was categorized as normal (18.5–24.9), overweight (25.0 –29.9), or obese (≥30). Participants who were underweight (BMI <18.5) were excluded from the analysis (270 [2.7%] study participants), as has been done in other studies due to concerns of higher rates of arthritis in this category (5), as well as the small sample size in this cohort.
Self-reported health status was defined by participants’ answer to the question: “In general, would you say your health is excellent, very good, good, fair, or poor?” on the SF-12 questionnaire. For data analysis, responses were dichotomized into the categories excellent/very good/good or fair/poor. The SF-12 physical component summary (PCS) and mental component summary (MCS) scores were calculated using the standard algorithms for the 1998 US population reference group. Pain was categorized as interfering with work in the last 4 weeks either “quite a bit/a lot/moderately” (yes) or “a little bit/not at all” (no). Use of NSAIDs and aspirin were considered positive if participants reported current use for ≥1 month. Traditional medicine and traditional healer use were considered positive if they had been used anytime during the past year.
Statistical analysis
Data were analyzed using SAS software, version 9.1 (SAS Institute, Cary, NC). The unadjusted prevalence of arthritis was calculated for the entire cohort, by study site, and by the characteristics of interest. For comparison with other published studies, the estimates of prevalence were age adjusted and age-sex adjusted to the 2000 US population standard distribution of age and sex. Because the prevalence of arthritis differed substantially between Alaska and the Southwest US, prevalence estimates were calculated separately for each center. Multivariate logistic regression analysis was performed to calculate adjusted prevalence ORs and 95% confidence intervals for the characteristics of interest with all variables included in the model, with separate models for Alaska and the Southwest US. Analyses of health-related factors were also stratified by center and multivariate logistic regression was used to calculate adjusted ORs. The characteristics found to be associated with arthritis in the previous models for each center were included as covariates in the logistic regression analyses of health-related factors. Multiple linear regression was used to determine the effect of arthritis on PCS and MCS scores, adjusting for the same covariates. For all variables, participants with missing data were excluded from the analysis. P values less than 0.05 were considered significant.
RESULTS
A total of 10,371 participants enrolled in the study prior to March 1, 2007. Data from 403 participants who answered “don’t know” or “refused” to the arthritis question, or who had a missing value on the arthritis question, were excluded from the analysis. When compared with those who were included, excluded participants were older (P < 0.0001) and less likely to have a high school education or greater (P = 0.004), but did not differ by sex distribution, rural versus urban residency, study center, language spoken at home, or degree of identification with tribal traditions. We report on the 9,968 participants with data on arthritis (Table 1). The distribution of all characteristics other than marital status was significantly different between the 2 study centers.
Table 1.
Characteristics of EARTH study participants from Alaska and the Southwest US*
| Characteristic | Alaska (n = 3,695) | Southwest US (n = 6,273) | P† |
|---|---|---|---|
| Age, mean ± SD years | 40.3 ± 14.8 | 39.4 ± 14.0 | 0.0013 |
| Age, years | |||
| 18–24 | 661 (17.9) | 1,194 (19.0) | < 0.0001 |
| 25–34 | 727 (19.7) | 1,302 (20.8) | |
| 35–44 | 915 (24.8) | 1,524 (24.3) | |
| 45–54 | 764 (20.7) | 1,253 (20.0) | |
| 55–64 | 371 (10.0) | 736 (11.7) | |
| ≥65 | 257 (7.0) | 264 (4.2) | |
| Sex | |||
| Male | 1,453 (39.3) | 2,287 (36.5) | 0.0043 |
| Female | 2,242 (60.7) | 3,986 (63.5) | |
| Education, total | n = 3,659‡ | n = 6,221‡ | |
| Less than high school | 811 (22.2) | 1,635 (26.3) | < 0.0001 |
| High school/GED or greater | 2,848 (77.8) | 4,586 (73.7) | |
| Employment, total | n = 3,683 | n = 6,271 | |
| Employed | 2,464 (66.9) | 3,769 (60.1) | < 0.0001 |
| Not employed | 1,219 (33.1) | 2,502 (39.9) | |
| Marital status, total | n = 3,680 | n = 6,264 | |
| Married | 1,574 (42.8) | 2,738 (43.7) | 0.36 |
| Not married | 2,106 (57.2) | 3,526 (56.3) | |
| Residency, total | n = 3,695 | n = 6,252 | |
| Urban | 1,355 (36.7) | 284 (4.5) | < 0.0001 |
| Rural | 2,340 (63.3) | 5,968 (95.5) | |
| Alaska region, total | n = 3,695 | ||
| Southcentral | 1,355 (36.7) | NA | |
| Southeast | 863 (23.3) | ||
| Southwest | 1,477 (40.0) | ||
| Language spoken at home, total | n = 3,695 | n = 6,262 | |
| AI/AN only | 297 (8.0) | 706 (11.3) | < 0.0001 |
| AI/AN and English | 916 (24.8) | 3,691 (58.9) | |
| English only | 2,468 (66.8) | 1,834 (29.3) | |
| Other | 14 (0.4) | 31 (0.5) | |
| Identification with tribal traditions, total | n = 3,691 | n = 6,262 | |
| A lot/some | 2,567 (69.6) | 4,750 (75.8) | < 0.0001 |
| A little/not at all | 1,124 (30.4) | 1,512 (24.2) | |
| Income, total | n = 3,167 | n = 5,397 | |
| <$15,000 | 1,294 (40.9) | 2,896 (53.7) | < 0.0001 |
| ≥$15,000 | 1,873 (59.1) | 2,501 (46.3) | |
| BMI kg/m2, total§ | n = 3,695 | n = 6,273 | |
| 18.5–24.9 | 933 (25.2) | 1,009 (16.1) | < 0.0001 |
| 25.0–29.9 | 1,178 (31.9) | 1,997 (31.8) | |
| ≥30 | 1,559 (42.2) | 3,022 (48.2) | |
| Vigorous physical activity, hours/week, total | n = 3,530 | n = 6,020 | |
| None | 1,283 (36.4) | 1,689 (28.1) | < 0.0001 |
| >0 to <2.5 | 1,293 (36.6) | 2,497 (41.5) | |
| ≥2.5 | 954 (27.0) | 1,834 (30.5) | |
| Chronic medical conditions, total | n = 3,695 | n = 6,273 | |
| None | 1,420 (38.4) | 2,983 (47.6) | < 0.0001 |
| 1–2 | 1,594 (43.1) | 2,391 (38.1) | |
| >2 | 681 (18.4) | 899 (14.3) | |
| General health, total | n = 3,695 | n = 6,253 | |
| Excellent/very good/good | 2,777 (75.2) | 4,552 (72.8) | 0.0099 |
| Fair/poor | 918 (24.8) | 1,701 (27.2) |
Values are the number (percentage) unless otherwise indicated. EARTH = Education and Research Towards Health; GED = General Educational Development certification; NA = not applicable; AI = American Indian; AN = Alaska Native; BMI = body mass index.
Calculated by Student’s t-test for continuous variables and by chi-square test for categorical variables.
Sample size varies by category because missing values are excluded.
Total includes those who are underweight, not presented separately here (n = 25 in Alaska and n = 245 in the Southwest US). Total percentages do not add up to 100%.
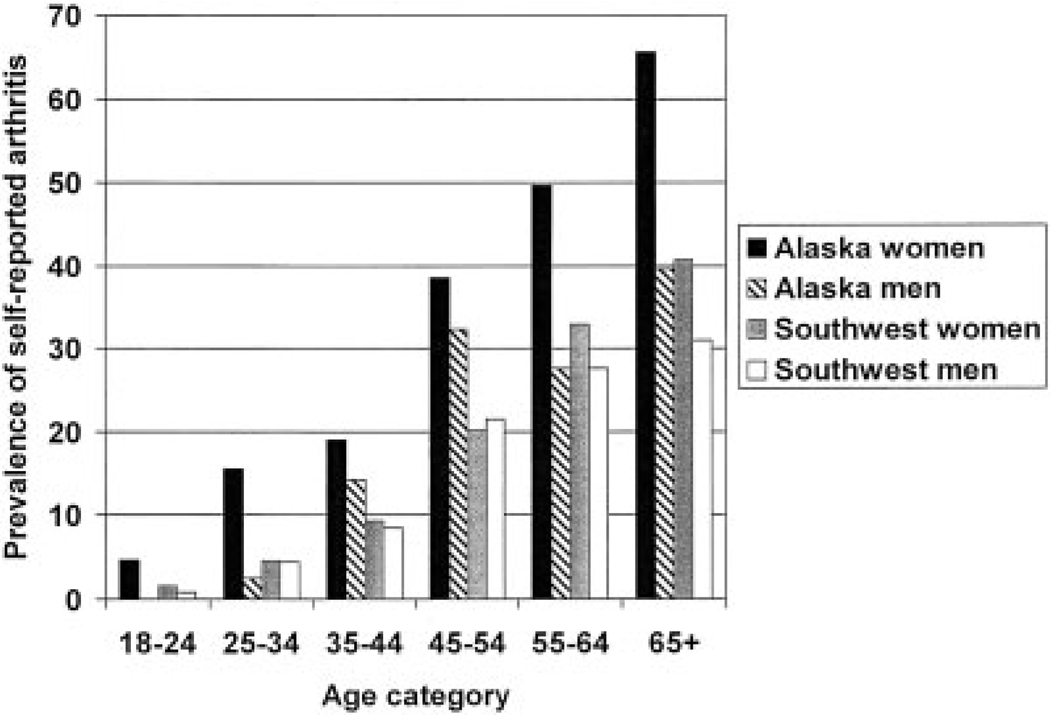
As shown in Figure 1, the prevalence of arthritis increased with age in both Alaska and the Southwest US. The prevalence of arthritis was consistently lower in the Southwest US than Alaska for all age categories. In Alaska, arthritis was more commonly reported by women in all age groups. In the Southwest US, the age-specific prevalence of arthritis was similar in both sexes until age 55 years and over, at which point arthritis was reported more commonly by women. The overall prevalence of arthritis in participants age 55 years and over was 48.4% in Alaska and 32.8% in the Southwest US.
Figure 1.
Prevalence of self-reported arthritis by age and sex for Education and Research Towards Health study participants from Alaska and the Southwest US.
Table 2 shows the prevalence of self-reported arthritis, including unadjusted, age-adjusted, and age-sex adjusted prevalences, by center. The age-sex adjusted prevalence of self-reported arthritis was 26.1% in the Alaska Native cohort and 16.5% in the Southwest American Indian cohort, as compared with 21.5% in the 2003–2005 NHIS (1). In both centers, self-reported arthritis was more common in women, but the differences by sex were more pronounced in the Alaska cohort than in the Southwest US cohort. In both centers, there was a trend toward higher age-sex adjusted prevalence of self-reported arthritis in those not currently employed, residing in urban locations, and with higher BMI, more chronic medical conditions, and poorer self-reported health status. In the Southwest US, people with higher levels of education had a higher prevalence of self-reported arthritis, but there was no clear trend in Alaska. The trends in self-reported arthritis prevalence by language spoken and identification with tribal traditions varied by center. There was no association of self-reported arthritis with income in either center, and this remained true when income was analyzed in smaller categories or with different cut points (data not shown).
Table 2.
Age-adjusted and age-sex adjusted prevalence of self-reported arthritis and associations in EARTH study participants*
| Alaska | Southwest US | |||||
|---|---|---|---|---|---|---|
| Characteristic | Unadjusted | Age adjusted† |
Age-sex adjusted‡ |
Unadjusted | Age adjusted† |
Age-sex adjusted‡ |
| Total | 22.2 | 26.9 | 26.1 | 12.7 | 16.7 | 16.5 |
| Sex | ||||||
| Male | 17.5 | 20.9 | NA | 11.3 | 15.2 | NA |
| Female | 25.2 | 30.4 | NA | 13.5 | 17.5 | NA |
| Education | ||||||
| Less than high school | 25.5 | 26.6 | 26.0 | 13.3 | 15.7 | 15.3 |
| High school/GED or greater | 21.2 | 27.0 | 26.3 | 12.4 | 17.6 | 17.5 |
| Employment | ||||||
| Employed | 17.3 | 24.4 | 24.0 | 9.9 | 14.4 | 14.2 |
| Not employed | 32.3 | 31.5 | 30.2 | 16.9 | 19.6 | 19.7 |
| Marital status | ||||||
| Married | 25.0 | 26.0 | 25.4 | 15.3 | 17.3 | 17.5 |
| Not married | 20.2 | 27.7 | 26.8 | 10.7 | 16.2 | 16.0 |
| Residency | ||||||
| Rural | 21.1 | 25.3 | 24.8 | 12.6 | 16.5 | 16.3 |
| Urban | 24.1 | 29.9 | 28.6 | 15.5 | 22.4 | 21.2 |
| Alaska region | ||||||
| Southcentral | 24.1 | 29.9 | 28.6 | |||
| Southeast | 27.6 | 29.2 | 28.6 | |||
| Southwest | 17.3 | 22.9 | 22.5 | |||
| Language | ||||||
| AI/AN only | 24.6 | 23.7 | 24.0 | 17.3 | 17.7 | 17.3 |
| AI/AN and English | 24.1 | 25.5 | 24.8 | 13.3 | 16.2 | 16.9 |
| English only | 21.2 | 28.2 | 27.3 | 9.8 | 17.4 | 16.1 |
| Identification with tribal traditions |
||||||
| A lot/some | 23.8 | 27.0 | 26.4 | 13.1 | 16.5 | 16.4 |
| A little/not at all | 18.6 | 26.3 | 24.5 | 11.2 | 17.2 | 16.4 |
| Income | ||||||
| <$15,000 | 22.9 | 26.0 | 25.8 | 12.9 | 17.5 | 17.1 |
| ≥$15,000 | 22.1 | 27.1 | 26.1 | 12.8 | 16.6 | 16.6 |
| BMI, kg/m2 | ||||||
| 18.5–24.9 | 14.9 | 21.8 | 21.8 | 8.1 | 13.6 | 13.4 |
| 25.0–29.9 | 20.7 | 25.5 | 25.2 | 11.5 | 14.0 | 14.1 |
| ≥30 | 27.6 | 30.3 | 29.5 | 15.0 | 19.4 | 18.8 |
| Vigorous physical activity, hours/week |
||||||
| None (reference) | 30.5 | 28.3 | 26.0 | 19.8 | 18.7 | 19.0 |
| >0 to <2.5 | 20.4 | 28.4 | 28.1 | 11.0 | 16.5 | 16.6 |
| ≥2.5 | 13.5 | 23.2 | 23.9 | 8.1 | 16.2 | 16.4 |
| Chronic medical conditions | ||||||
| None | 8.8 | 14.0 | 14.2 | 5.1 | 9.6 | 9.6 |
| 1–2 | 22.2 | 26.1 | 25.6 | 14.3 | 15.9 | 15.9 |
| >2 | 50.4 | 41.1 | 38.8 | 33.7 | 27.6 | 27.5 |
| General health | ||||||
| Excellent/very good/good | 18.4 | 23.9 | 23.3 | 10.1 | 13.5 | 13.1 |
| Fair/poor | 33.9 | 35.0 | 33.5 | 19.3 | 24.8 | 25.1 |
Values are the percentage. EARTH = Education and Research Towards Health; NA = not applicable; GED = General Educational Development certification; AI = American Indian; AN = Alaska Native; BMI = body mass index.
Adjusted to the standard 2000 US population distribution of age.
Adjusted to the standard 2000 US population distribution of age and sex (except for category of sex).
In Table 3, the results of multivariate analysis of self-reported arthritis and the characteristics evaluated in Table 2 are presented using adjusted prevalence ORs. After adjustment for all variables in the Alaska cohort (except rural/urban, because the Alaska region captures this variable), reports of arthritis were significantly associated with increasing age, female sex, lack of current employment, obesity, higher number of chronic medical conditions, and fair or poor general health status. In the Southwest US cohort, reports of arthritis were associated with increasing age, higher education level, lack of current employment, marital status (not currently married), urban residency, higher number of chronic medical conditions, and fair or poor general health status. In both models, increasing age remained significant when age was entered as a continuous variable (data not shown).
Table 3.
Multivariate associations with reporting of arthritis in EARTH study participants*
| Characteristic | Alaska | Southwest US |
|---|---|---|
| Age, years | ||
| 18–24† | 1.0 | 1.0 |
| 25–34 | 4.1 (2.2–7.8) | 3.1 (1.6–5.8) |
| 35–44 | 7.6 (4.1–14.2) | 5.4 (2.9–9.9) |
| 45–54 | 13.7 (7.4–25.4) | 12.5 (6.8–23.0) |
| 55–64 | 17.8 (9.4–34.0) | 20.4 (11.0–37.8) |
| ≥65 | 19.8 (9.8–39.6) | 25.5 (13.0–49.8) |
| Sex | ||
| Male† | 1.0 | 1.0 |
| Female | 1.3 (1.1–1.6) | 1.0 (0.8–1.2) |
| Education | ||
| Less than high school† | 1.0 | 1.0 |
| High school/GED or greater | 1.1 (0.8–1.4) | 1.3 (1.0–1.6) |
| Employment | ||
| Employed† | 1.0 | 1.0 |
| Not employed | 1.5 (1.2–1.8) | 1.3 (1.1–1.6) |
| Marital Status | ||
| Married† | 1.0 | 1.0 |
| Not married | 1.1 (0.9–1.4) | 0.8 (0.6–0.9) |
| Residency | ||
| Rural† | NA | 1.0 |
| Urban | NA | 1.6 (1.1–2.3) |
| Alaska region | ||
| Southcentral† | 1.0 | NA |
| Southeast | 1.1 (0.9–1.4) | NA |
| Southwest | 0.8 (0.6–1.0) | NA |
| Language spoken at home | ||
| AI/AN only | 1.0 (0.7–1.4) | 1.0 (0.8–1.2) |
| AI/AN and English | 1.2 (0.9–1.5) | 0.8 (0.7–1.0) |
| English only† | 1.0 | 1.0 |
| Identification with tribal traditions | ||
| A lot/some | 1.0 (0.8–1.2) | 1.0 (0.8–1.2) |
| A little/not at all† | 1.0 | 1.0 |
| Income | ||
| <$15,000 | 0.9 (0.8–1.2) | 1.1 (0.9–1.3) |
| ≥$15,000† | 1.0 | 1.0 |
| BMI, kg/m2 | ||
| 18.5–24.9† | 1.0 | 1.0 |
| 25.0–29.9 | 1.1 (0.8–1.5) | 0.9 (0.7–1.2) |
| ≥30 | 1.3 (1.0–1.7) | 1.2 (0.9–1.5) |
| Vigorous physical activity, hours/week | ||
| None† | 1.0 | 1.0 |
| >0 to <2.5 | 1.2 (0.9–1.4) | 0.8 (0.7–1.0) |
| ≥2.5 | 1.2 (1.0–1.6) | 0.9 (0.7–1.1) |
| Chronic medical conditions | ||
| None | 1.0 | 1.0 |
| 1–2 | 1.9 (1.5–2.4) | 1.8 (1.4–2.3) |
| >2 | 3.8 (2.8–5.1) | 3.2 (2.5–4.1) |
| General health | ||
| Excellent/very good/good | 1.0 | 1.0 |
| Fair/poor | 1.6 (1.3–2.0) | 1.6 (1.4–2.0) |
Values are the adjusted OR (95% confidence interval). ORs are from multivariate models regressing the outcome of arthritis on all listed variables. The Alaska and Southwest US samples were fit separately. The Alaska model excludes the urban/rural covariate and Southwest US model excludes Alaska region covariate. EARTH = Education and Research Towards Health; GED = General Educational Development certification; NA = not applicable; AI = American Indian; AN = Alaska Native; BMI = body mass index; ORs = odds ratios.
Reference group.
Health-related factors and treatments demonstrating the impact of arthritis in these American Indian and Alaska Native populations are presented in Table 4. For categorical variables, the ORs for the Alaska cohort were adjusted for age, sex, Alaska region, employment, chronic medical conditions, and general health. The ORs for the Southwest US cohort were adjusted for age, rural/urban residency, employment, chronic medical conditions, education, general health, and marital status. Arthritis was significantly associated with lower SF-12 PCS scores in both Alaska and the Southwest US as compared with those reporting no arthritis, after adjusting for all covariates using multiple linear regression, but there was no significant association with the MCS score. Current NSAID use, aspirin use, and pain interfering with work were significantly more common in both centers in people who reported arthritis. Use of traditional medicines and traditional healers were associated with arthritis in Alaska, but not in the Southwest US. The overall prevalence of use of traditional healers was higher in the Southwest US than Alaska, but use of traditional medicines was similar in both centers.
Table 4.
Health status and treatment in EARTH study participants reporting arthritis*
| Alaska† | Southwest US‡ | |||||||
|---|---|---|---|---|---|---|---|---|
| Arthritis | No arthritis |
Adjusted OR (95% CI) |
P | Arthritis | No arthritis |
Adjusted OR (95% CI) |
P | |
| Health status | ||||||||
| SF-12 PCS score, mean | 43.9 | 52.6 | < 0.0001 | 42.7 | 49.7 | < 0.0001 | ||
| SF-12 MCS score, mean | 46.2 | 46.7 | 0.84 | 44.0 | 45.9 | 0.11 | ||
| Pain interfering with work, % | 48.8 | 15.3 | 3.4 (2.8–4.2) | 52.7 | 19.5 | 3.1 (2.6–3.7) | ||
| Treatment, % | ||||||||
| NSAIDs | 33.5 | 13.8 | 2.5 (2.0–3.0) | 36.3 | 16.6 | 2.2 (1.8–2.6) | ||
| Aspirin | 27.1 | 11.6 | 1.3 (1.1–1.7) | 35.1 | 17.2 | 1.4 (1.2–1.7) | ||
| Traditional medicine | 32.4 | 24.8 | 1.3 (1.1–1.6) | 28.7 | 28.2 | 1.1 (0.9–1.3) | ||
| Traditional healer | 12.2 | 6.4 | 1.4 (1.0–1.9) | 34.2 | 32.4 | 1.2 (1.0–1.4) | ||
EARTH = Education and Research Towards Health; OR = odds ratio; 95% CI = 95% confidence interval; SF-12 = Short Form 12 Health Survey; PCS = physical component summary; MCS = mental component summary; NSAIDs = nonsteroidal antiinflammatory drugs.
ORs are from a logistic regression model including age, sex, Alaska region, employment, chronic medical conditions, and general health. P values are from linear regression, including the same variables, of PCS and MCS.
ORs are from a logistic regression model including age, rural/urban residency, employment, chronic medical conditions, education, general health, and marital status. P values are from linear regression, including the same variables, of PCS and MCS.
DISCUSSION
The prevalence of self-reported, doctor-diagnosed arthritis was high in Alaska Native people and low in a Southwest American Indian population compared with the 2003–2005 US population as measured by the NHIS (1). Self-reported arthritis prevalence increases with age in both the Alaska Native and the American Indian cohorts, although prevalence is lower in each age group among the Southwest American Indian population. In both Alaska and the Southwest US, self-reported arthritis was associated with lack of current employment, number of chronic medical conditions, and fair or poor general health status. Arthritis was also associated with female sex in Alaska; in the Southwest, higher education, not being currently married, and residing in urban areas were associated with arthritis. Poorer physical but not mental health status was associated with arthritis in both Alaska and the Southwest. Use of traditional medicines and healers were associated with arthritis only in Alaska.
Few published data exist on the prevalence of self-reported arthritis in American Indian and Alaska Native populations. A survey of 8,305 American Indian and Alaska Native elders from 94 sites found the prevalence of arthritis in people age 55 years and over to be 43.5%, which is slightly higher than the 40% prevalence in the general US population in this age group (16). In our study, we found a higher prevalence in people age 55 years and over in Alaska (48.4%), but a lower prevalence in the Southwest US (32.8%). Another survey of American Indian elders from 1 tribe age 60 years and over found that 49.6% reported a diagnosis of arthritis, and that arthritis was commonly associated with other comorbid conditions (17). In Canada, the 2001 Aboriginal Peoples Survey found the prevalence of self-reported arthritis to be 19.3% in nonreserve Aboriginal adults, which is nearly twice the prevalence found in the general Canadian population (18).
There are several possible explanations for the regional differences we found in the burden of self-reported arthritis. The first is that the prevalence of arthritis may be truly high in Alaska Native people and low in Southwest American Indian people. Population differences in the prevalence of specific types of arthritis have been previously described, e.g., a high prevalence of rheumatoid arthritis in the Alaska Native people of Southeast Alaska (6,7) and a high prevalence of spondylarthropathy in Northern and Western Alaska (7,8) as well as in the Navajo population (originally described as “Navajo arthritis”) (19,20). However, the prevalence of these disorders is low compared with the total proportion of self-reported arthritis in American Indian and Alaska Native populations (6,8,21). Therefore, it is likely that more common disorders such as osteoarthritis and other noninflammatory musculoskeletal conditions account for the majority of self-reported arthritis in both American Indian and Alaska Native populations. Regional variations in the prevalence of noninflammatory conditions could partially explain the differences found, but other explanations should be considered.
Possible factors contributing to reporting of arthritis include cultural beliefs about arthritis, awareness of arthritis among both participants and their health care providers, and access to health care. A study of arthritis beliefs in urban American Indian people found that people with joint pain did not initially assume it was due to arthritis, and that they were likely to minimize the description of pain to their doctor because of cultural practices (22). We did not find any association between 2 crude measures of cultural identification and the reporting of arthritis, but it is possible that other cultural factors play a role, including the relationship between patients and providers in addition to cultural beliefs about arthritis. Our finding that education level was associated with self-reported arthritis in the Southwest US suggests that education could increase awareness of arthritis. Regional differences in providers’ understanding of arthritis or availability of rheumatology services could also impact awareness of arthritis. The finding that people with more chronic medical conditions were more likely to report arthritis suggests that contact with the health care system can increase the likelihood of reporting a diagnosis of arthritis, and regional differences in health care utilization could partially account for these findings.
In addition, although the case definition of arthritis has been validated for population surveillance and in senior centers (2,3), it has not been validated in Alaska Native or American Indian populations as compared with the gold standard of clinical history and examination or medical record review. Clearly the measure of self-reported, doctor-diagnosed arthritis provides strikingly different results in these 2 populations, and future studies should investigate its validity in these populations relative to clinical examination or medical record review.
The variations in prevalence of self-reported, doctor-diagnosed arthritis by study center could partially be attributed to the regions of Alaska and the Southwest US included in this study. Although the results may not be generalizable to all American Indian and Alaska Native populations, in the study sites where enrollment took place in both Alaska and the Southwest US, characteristics of the study participants (other than sex, which was accounted for in adjustments) were similar to US census data for the total population in each area (12).
We found differences not only in prevalence of arthritis, but also in associated factors in Alaska and the Southwest US. Notable differences from the national and international data are the lack of a consistent association of sex with arthritis in the Southwest US, the association of higher levels of education with arthritis in the Southwest US, and the lack of significant association of BMI or physical activity with arthritis in either center (1,5,23). In the US population, the age-adjusted prevalence of arthritis was 18.1% in men and 24.4% in women (1). The absolute difference between rates by sex is higher in Alaska and lower in the Southwest US, and in the Southwest, differences by sex occurred only after age 55 years. In addition, we found no association between household income and arthritis in either cohort, though employment status was associated. It is possible that risk factors for the development of arthritis vary between populations. It is also possible that some of these differences are related to the performance of the surveillance question in these populations. Finally, the range of characteristics, such as BMI and income, differ from the general US population, which could have impacted the observed associations.
Because this is a cross-sectional report, we can assess associations with arthritis but cannot determine causality. From these data, is impossible to know whether arthritis causes people to move to urban regions for care or services, or if people living in urban regions are more likely to develop arthritis. It is likely that the differences in employment are attributable to arthritis, but the association between arthritis and lack of employment included a heterogeneous group of people in the nonemployed group; although the association remained after adjusting for age, other factors might be contributing to this finding. Continuing these studies prospectively would allow detection of incident cases of arthritis and possible identification of health and lifestyle factors associated with the onset of arthritis in American Indian and Alaska Native people.
Previous population-based studies have determined the prevalence of arthritis-attributable work limitation to be significant at ~30% of people reporting arthritis (24). We did not specifically ask about arthritis-attributable work limitation, but we found that approximately half of the people reporting arthritis in both Alaska and the Southwest US also reported pain interfering with work. In both study centers, self-reported physical health status as determined by the SF-12 was significantly worse in people with arthritis, further supporting the frequency of physical limitations due to arthritis. The findings related to traditional medicine and traditional healers suggest that Alaska Native people might be more likely to seek out these services for arthritis; Southwest American Indian people both with and without arthritis reported frequent use of traditional healers.
In summary, we found from the baseline visit in a prospective study of American Indian and Alaska Native populations that the prevalence of self-reported, doctor-diagnosed arthritis is high in Alaska Native people and low in a Southwest American Indian population as compared with the US population. Arthritis burden increases with age in both populations, but factors associated with arthritis differ between the Alaska Native and Southwest American Indian populations. Further study is needed to validate the measure of self-reported, doctor-diagnosed arthritis in American Indian and Alaska Native populations and to prospectively evaluate risk and protective factors for incident arthritis.
ACKNOWLEDGMENTS
We would like to acknowledge the contributions and support of the Navajo Nation, the Indian Health Service, the Alaska Native Tribal Health Consortium Board of Directors, Southcentral Foundation, Southeast Alaska Regional Health Consortium, the Yukon-Kuskokwim Health Corporation, Fort Defiance and Shiprock Health Boards, Tribal Advisory Board Members, the staff on the Navajo Nation, the staff in Alaska, and the University of Utah Coordinating Center staff.
Supported by grants from the National Cancer Institute (CA88958, CA96095).
Footnotes
The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official view of the National Cancer Institute.
Dr. Tom-Orme has received consultant fees (less than $10,000) from the National Coalition of Ethnic Minority Nurses Association.
AUTHOR CONTRIBUTIONS
Dr. Ferucci had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study design. Schumacher, Lanier, Edwards, Tom-Orme, Slattery.
Acquisition of data. Schumacher, Lanier, Murtaugh, Edwards, Tom-Orme, Slattery.
Analysis and interpretation of data. Ferucci, Schumacher, Lanier, Murtaugh, Helzer, Slattery.
Manuscript preparation. Ferucci, Schumacher, Lanier, Murtaugh, Edwards, Helzer, Slattery.
Statistical analysis. Ferucci, Schumacher, Lanier.
Community and tribal institutional review board approval. Tom-Orme.
REFERENCES
- 1.Centers for Disease Control and Prevention (CDC) Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation: United States, 2003–2005. MMWR Morb Mortal Wkly Rep. 2006;55:1089–1092. [published errata appear in MMWR Morb Mortal Wkly Rep 2006;55:1129 and MMWR Morb Mortal Wkly Rep 2007;56:55] [PubMed] [Google Scholar]
- 2.Sacks JJ, Harrold LR, Helmick CG, Gurwitz JH, Emani S, Yood RA. Validation of a surveillance case definition for arthritis. J Rheumatol. 2005;32:340–347. [PubMed] [Google Scholar]
- 3.Bombard JM, Powell KE, Martin LM, Helmick CG, Wilson WH. Validity and reliability of self-reported arthritis: Georgia senior centers, 2000–2001. Am J Prev Med. 2005;28:251–258. doi: 10.1016/j.amepre.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC) Behavioral risk factor surveillance system survey data. Atlanta: US Department of Health and Human Services, CDC; 2005. [Google Scholar]
- 5.Busija L, Hollingsworth B, Buchbinder R, Osborne RH. Role of age, sex, and obesity in the higher prevalence of arthritis among lower socioeconomic groups: a population-based survey. Arthritis Rheum. 2007;57:553–561. doi: 10.1002/art.22686. [DOI] [PubMed] [Google Scholar]
- 6.Ferucci ED, Templin DW, Lanier AP. Rheumatoid arthritis in American Indians and Alaska Natives: a review of the literature. Semin Arthritis Rheum. 2005;34:662–667. doi: 10.1016/j.semarthrit.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 7.Peschken CA, Esdaile JM. Rheumatic diseases in North America’s indigenous peoples. Semin Arthritis Rheum. 1999;28:368–391. doi: 10.1016/s0049-0172(99)80003-1. [DOI] [PubMed] [Google Scholar]
- 8.Boyer GS, Templin DW, Cornoni-Huntley JC, Everett DF, Lawrence RC, Heyse SF, et al. Prevalence of spondyloarthropathies in Alaskan Eskimos. J Rheumatol. 1994;21:2292–2297. [PubMed] [Google Scholar]
- 9.Peschken CA, Esdaile JM. Systemic lupus erythematosus in North American Indians: a population based study. J Rheumatol. 2000;27:1884–1891. [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention (CDC) Racial/ethnic differences in the prevalence and impact of doctor-diagnosed arthritis: United States, 2002. MMWR Morb Mortal Wkly Rep. 2005;54:119–123. [PubMed] [Google Scholar]
- 11.Hootman JM, Schieb L, Helmick CG. Race/ethnic disparities in arthritis prevalence and impact, United States, 2002–03 [abstract] Arthritis Rheum. 2006;54 Suppl 9:S825. [Google Scholar]
- 12.Slattery ML, Schumacher MC, Lanier AP, Edwards S, Edwards R, Murtaugh MA, et al. A prospective cohort of American Indian and Alaska Native people: study design, methods, and implementation. Am J Epidemiol. 2007;166:606–615. doi: 10.1093/aje/kwm109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1995;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Edwards SL, Slattery ML, Murtaugh MA, Edwards RL, Bryner J, Pearson M, et al. Development and use of touch-screen audio computer-assisted self-interviewing in a study of American Indians. Am J Epidemiol. 2007;165:1336–1342. doi: 10.1093/aje/kwm019. [DOI] [PubMed] [Google Scholar]
- 15.Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32 Suppl 9:S498–S504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 16.Muus KJ, McDonald LR, Ludtke RL, Allery AJ, Knudson A, Moulton P. Arthritis among American Indian and Alaska Native elders: prevalence, demographic patterns, and comorbidities. J Native Aging Health. 2007;2:5–13. [Google Scholar]
- 17.John R, Kerby DS, Hennessy CH. Patterns and impact of comorbidity and multimorbidity among community-resident American Indian elders. Gerontologist. 2003;43:649–660. doi: 10.1093/geront/43.5.649. [DOI] [PubMed] [Google Scholar]
- 18.Statistics Canada. Aboriginal Peoples Survey 2001: initial findings. Well-being of the nonreserve Aboriginal population. 2003 URL: http://www.statcan.ca/english/freepub/89-589-XIE/index.htm.
- 19.Muggia AL, Bennahum DA, Williams RC., Jr Navajo arthritis: an unusual, acute, self-limited disease. Arthritis Rheum. 1971;14:348–355. doi: 10.1002/art.1780140305. [DOI] [PubMed] [Google Scholar]
- 20.Rate RG, Morse HG, Bonnell MD, Kuberski TT. “Navajo arthritis” reconsidered: relationship to HLA–B27. Arthritis Rheum. 1980;23:1299–1302. doi: 10.1002/art.1780231112. [DOI] [PubMed] [Google Scholar]
- 21.Lawrence RC, Helmick CG, Arnett FC, Deyo RA, Felson DT, Giannini EH, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41:778–799. doi: 10.1002/1529-0131(199805)41:5<778::AID-ART4>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 22.Kramer BJ, Harker JO, Wong AL. Arthritis beliefs and self-care in an urban American Indian population. Arthritis Rheum. 2002;47:588–594. doi: 10.1002/art.10795. [DOI] [PubMed] [Google Scholar]
- 23.Hootman JM, Macera CA, Ham SA, Helmick CG, Sniezek JE. Physical activity levels among the general US adult population and in adults with and without arthritis. Arthritis Rheum. 2003;49:129–135. doi: 10.1002/art.10911. [DOI] [PubMed] [Google Scholar]
- 24.Theis KA, Murphy L, Hootman JM, Helmick CG, Yelin E. Prevalence and correlates of arthritis-attributable work limitation in the US population among persons ages 18–64: 2002 National Health Interview Survey data. Arthritis Rheum. 2007;57:355–363. doi: 10.1002/art.22622. [DOI] [PMC free article] [PubMed] [Google Scholar]