Abstract
OBJECTIVES
To examine the relationship between functional limitations and pain across a spectrum of age, ranging from mid life to advanced old age.
DESIGN
Cross-sectional study.
SETTING
The 2004 Health and Retirement Study (HRS), a nationally representative study of community-living persons aged 50 and older.
PARTICIPANTS
Eighteen thousand five hundred thirty-one participants in the 2004 HRS.
MEASUREMENTS
Participants who reported that they were often troubled by pain that was moderate or severe most of the time were defined as having significant pain. For each of four functional domains, subjects were classified according to their degree of functional limitation: mobility (able to jog 1 mile, able to walk several blocks, able to walk one block, unable to walk one block), stair climbing (able to climb several flights, able to climb one flight, not able to climb a flight), upper extremity tasks (able to do 3, 2, 1, or 0), and activity of daily living (ADL) function (able to do without difficulty, had difficulty but able to do without help, need help).
RESULTS
Twenty-four percent of participants had significant pain. Across all four domains, participants with pain had much higher rates of functional limitations than subjects without pain. Participants with pain were similar in terms of their degree of functional limitation to participants 2 to 3 decades older. For example, for mobility, of subjects aged 50 to 59 without pain, 37% were able to jog 1 mile, 91% were able to walk several blocks, and 96% were able to walk one block without difficulty. In contrast, of subjects aged 50 to 59 with pain, 9% were able to jog 1 mile, 50% were able to walk several blocks, and 69% were able to walk one block without difficulty. Subjects aged 50 to 59 with pain were similar in terms of mobility limitations to subjects aged 80 to 89 without pain, of whom 4% were able to jog 1 mile, 55% were able to walk several blocks, and 72% were able to walk one block without difficulty. After adjustment for demographic characteristics, socioeconomic status, comorbid conditions, depression, obesity, and health habits, across all four measures, participants with significant pain were at much higher risk for having functional limitations (adjusted odds ratio (AOR) = 2.85, 95% confidence interval (CI) = 2.20–3.69, for mobility; AOR = 2.84, 95% CI = 2.48–3.26, for stair climbing; AOR = 3.96, 95% CI = 3.43–4.58, for upper extremity tasks; and AOR = 4.33; 95% CI = 3.71–5.06, for ADL function).
CONCLUSION
Subjects with pain develop the functional limitations classically associated with aging at much earlier ages.
Keywords: pain, functional limitations, activities of daily living, quality of life, disability
Functional limitations that impair the ability to live independently increase markedly with age.1–10 These functional limitations often develop insidiously as the end result of chronic health conditions.11 Because these functional limitations are so strongly associated with aging, they are often thought of as a core part of the phenotype of aging,7 but there is great variability between people of similar age in the degree of functional limitation. Some are free of functional limitations even into their 90s, whereas others develop significant functional limitations well before ages that would be considered old.12
Pain is known to be common in people with disability, and pain is a well-known risk factor for the development of disability.13–23 Thus, it is logical that pain may be an important factor that distinguishes those who experience functional limitations earlier in life from those who do not experience major functional limitations until late in life, but the authors are aware of no population-based studies that describe the relationships between disability and pain across the age span.
To address this, data were analyzed from the 2004 Health and Retirement Study (HRS), a population-based study of community-living persons in the United States aged 50 and older. Limitations in four domains that threaten the ability of people to live independently as they age were considered: mobility, stair climbing, upper extremity tasks, and activities of daily living (ADLs). The prevalence of functional limitations in people with and without significant pain in each domain were compared across a wide spectrum of ages ranging from middle age to advanced old age.
METHODS
Subjects
This was a cross-sectional study of subjects in the 2004 HRS.24 The goal of the HRS is to examine changes in health and wealth as people transition from work to retirement to old age. The 2004 wave of the HRS was designed to be representative of community-living people in the United States aged 50 and older. Of the 18,585 subjects in HRS, 54 were excluded, because they did not provide data on pain, leaving a final sample size of 18,531 subjects.
Measures
Pain
First, subjects were asked, “Are you often troubled with pain?” Subjects who answered yes were then asked, “How bad is the pain most of the time: mild, moderate, or severe?” Subjects who answered yes to the first question and rated the pain as moderate or severe were classified as having significant pain.
Functional Limitations
Four measures of functional limitation were considered, and for each measure, subjects’ functional ability was classified based on their responses to a series of questions examining varying degrees of functional impairment. For mobility, subjects were asked if they had any difficulty running or jogging 1 mile, walking several blocks, or walking one block. For stair climbing, subjects were asked if they had any difficulty climbing several flights of stairs without resting. Those who reported difficulty with several flights were then asked if they had difficulty with one flight of stairs. For upper extremity tasks, subjects were asked whether they had any difficulty extending their arms above their shoulders, pulling or pushing large objects like a living room chair, or lifting or carrying weights heavier than 10 pounds like a heavy bag of groceries. Subjects were classified as able to do all three, able to do two, able to do one, or unable to do any of these tasks. For ADL function, subjects were asked whether they had difficulty with five ADL: bathing, dressing, transferring, toileting, and eating. If subjects had difficulty with an ADL, they were asked if they needed help with the activity. Subjects were classified as able to do all of the ADLs without difficulty, having difficulty with at least one ADL but not needing help, or needing help with at least one ADL.
Potential Confounders
Several measures that could potentially confound the relationship between pain and functional limitations were considered. Demographic characteristics such as age, race, and sex were measured according to self-report. Measures of socioeconomic status included years of education, income, and total net worth. Comorbid conditions, including arthritis, hypertension, diabetes mellitus, cancer, chronic lung disease, myocardial infarction, congestive heart failure, and stroke, were obtained by asking subjects if a physician had ever told them that they had the condition. Depression was measured using the eight-item Center for Epidemiologic Studies Depression Scale.25 Subjects were classified as depressed if they reported three or more symptoms. Obesity was defined as a body mass index greater than 30. Subjects were also asked whether they were current smokers, whether they consumed alcohol, and whether they engaged in physical activity two or more times a week.
Analyses
The analyses used the sampling and design weights provided by the HRS to account for the probability of selection and clustering in the HRS sample. The characteristics of subjects reporting significant pain were compared using chi-square tests for categorical variables and t-tests for continuous variables. For each measure of functional limitation, subjects were stratified according to decade of age, and the extent of functional limitation in subjects with and without significant pain was graphically compared.
To examine the effect of potential confounding factors on the relationship between pain and functional limitations, a series of logistic regression analyses were conducted. First, only demographic characteristics were adjusted for. Next, a series of domains of potential confounders were also adjusted for. These domains included socioeconomic status (education, income, and net worth), arthritis, comorbid conditions other than arthritis (as listed in Table 1), depression, obesity, and health habits (smoking, alcohol, and exercise). Finally, all of these domains were adjusted for simultaneously. To simplify the presentation of the results, each of the functional limitation measures was dichotomized for these analyses. Because the rates of arthritis were high in subjects reporting pain, each of these analyses was repeated in subjects with and without arthritis.
Table 1.
Characteristics of Subjects
| Characteristic | No Pain (n = 14,124) | Pain (n = 4,407) | P-Value |
|---|---|---|---|
| Age, mean ± standard deviation | 65.0 ± 10.7 | 65.1 ± 10.6 | .53 |
| Age, % | |||
| 50–59 | 40 | 38 | .39 |
| 60–69 | 28 | 30 | |
| 70–79 | 20 | 20 | |
| 80–89 | 11 | 11 | |
| ≥90 | 2 | 2 | |
| Female, % | 52 | 61 | < .001 |
| Ethnicity, % | |||
| White | 82 | 79 | .01 |
| Black | 9 | 10 | |
| Hispanic | 7 | 8 | |
| Other | 3 | 3 | |
| < 12 years education, % | 17 | 24 | < .001 |
| Income, $1,000, median (IQR) | 46 (22–86) | 32 (15–59) | < .001 |
| Net worth, $1,000, median (IQR) | 203 (53–510) | 108 (21–328) | < .001 |
| Employed ≥20 h/wk, % | 46 | 29 | < .001 |
| Comorbid conditions, % | |||
| Arthritis | 47 | 81 | < .001 |
| Hypertension | 48 | 59 | < .001 |
| Diabetes mellitus | 15 | 23 | < .001 |
| Cancer | 12 | 14 | .001 |
| Chronic lung disease | 7 | 16 | < .001 |
| Myocardial infarction | 2 | 4 | < .001 |
| Congestive heart failure | 2 | 6 | < .001 |
| Stroke | 6 | 10 | < .001 |
| Depression, %* | 21 | 48 | < .001 |
| Body mass index ≥30.0 | 25 | 36 | < .001 |
| Current smoker, % | 23 | 28 | < .001 |
| Drinks alcohol, % | 57 | 45 | < .001 |
| Exercises ≥2 times per week, % | 63 | 44 | < .001 |
Eight-item Center for Epidemiologic Studies Depression Scale score ≥3.
IQR = interquartile range
RESULTS
Twenty-four percent of the subjects reported that they were often troubled by pain of moderate to severe intensity. The age distribution was virtually identical in subjects with and without pain, with a mean age of 65 in both groups. The prevalence of pain was 24% in subjects aged 50 to 59, 24% in those aged 60 to 69, 23% in those aged 70 to 79, 24% in those aged 80 to 89, and 26% in those aged 90 and older, but subjects with pain differed from subjects without pain on every other measure (Table 1). Subjects with pain were more likely to be female (61% vs 52%, P < .001) and slightly more likely to be nonwhite (21% vs 18%, P = .01). Subjects with pain were worse off on each measure of socioeconomic status, including being more likely to have less than 12 years of education (24% vs 17%, P < .001), and were less likely to be working (29% vs 46%, P < .001). Subjects with pain were more likely to have each comorbid condition. This was particularly true for arthritis (81% vs 47%, P < .001). Subjects with pain also had more depression and were more likely to be obese, more likely to smoke, less likely to drink alcohol, and less likely to exercise.
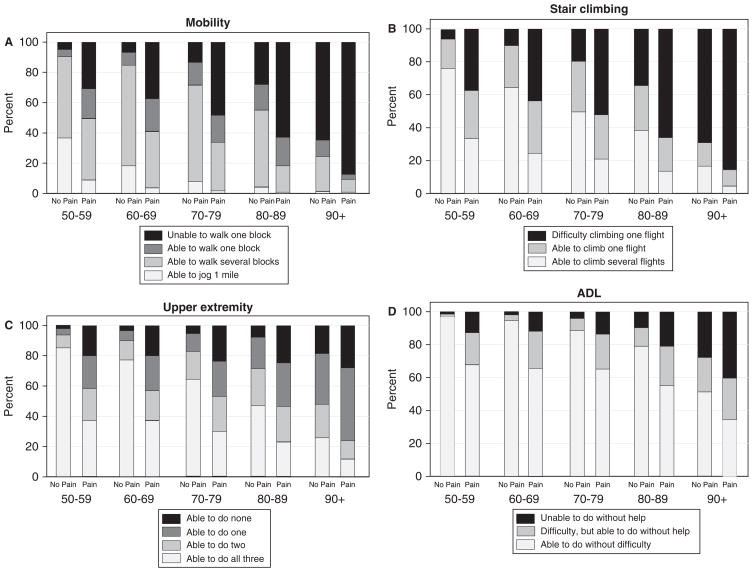
Across all four functional status measures, subjects with pain were strikingly more likely to have limitations than subjects without pain (Figure 1). Although rates of functional limitation rose markedly with age, subjects with pain were similar in terms of the degree of functional limitation to subjects 2 to 3 decades older without pain. For example, for mobility (Figure 1A), of subjects aged 50 to 59 without pain, 37% were able to jog 1 mile, 91% were able to walk several blocks, and 96% were able to walk one block without difficulty. In contrast, of subjects aged 50 to 59 with pain, 9% were able to jog 1 mile, 50% were able to walk several blocks, and 69% were able to walk one block without difficulty. Subjects aged 50 to 59 with pain were similar in terms of mobility limitations to subjects aged 80 to 89 without pain, of whom 4% were able to jog 1 mile, 55% were able to walk several blocks, and 72% were able to walk one block without difficulty.
Figure 1.
Limitations in four domains of functioning across age in subjects with and without pain. (A) Subjects were classified according the highest mobility level they could perform without difficulty: able to jog 1 mile, walk several blocks, walk one block, or unable to walk one block. (B) Subjects were classified according to the highest level of stair climbing ability they could perform without difficulty: able to climb several flights, able to climb one flight, or not able to climb one flight. (C) Subjects were classified according to how many of three upper extremity tasks they could perform without difficulty: extending their arms above their shoulders, pulling or pushing large objects like a living room chair, or lifting or carrying weights over 10 pounds like a heavy bag of groceries. (D) Subjects were classified according to their ability to perform basic activities of daily living (ADLs): able to do all without difficulty, having difficulty with at least one but still able to do without help, or needing help.
Although the strength of the association between pain and mobility limitation decreased somewhat with increasing age, a strong association between pain and mobility limitations persisted through the 10th decade of life.
For stair climbing, 76% of subjects aged 50 to 59 who did not have pain had no difficulty climbing several flights of stairs, compared with 33% of subjects with pain. Subjects aged 50 to 59 with pain were more limited in terms of stair climbing than subjects aged 80 to 89 without pain, of whom 39% had no difficulty climbing several flights of stairs.
For upper extremity tasks, for subjects without pain, task difficulty was generally uncommon in those aged 50 to 59, with a steady increase in the number of difficult tasks with increasing age. For subjects with pain, although rates of difficulty increased with age, the effect of age was less because of high rates of task difficulty in even the youngest subjects. Similarly, ADL difficulty and dependence were relatively rare in younger subjects without pain, with the prevalence rates becoming high only after the age of 80. In contrast, for subjects with pain, rates of difficulty and dependence were high at younger ages. For example, subjects with pain aged 50 to 59 had rates of ADL difficulty and dependence that exceeded those of subjects aged 80 to 89 without pain.
A strong association between pain and functional limitations persisted after adjustment for potentially confounding factors (Table 2). Although adjustment for each group of potential confounders decreased the association between pain and each functional limitation measure, the effect of most of these factors was relatively modest, with arthritis and health habits generally having the largest effect, although even after adjusting for all potential confounding factors, strong associations persisted between each functional limitation measure and pain.
Table 2.
Adjusted Association Between Pain and Functional Limitations
| Odds Ratio (95% Confidence Interval) for Relationship Between Pain and Disability | ||||||||
|---|---|---|---|---|---|---|---|---|
| Functional Limitation Measure |
Demographic Characteristics Only* |
Socioeconomic Status |
Arthritis | Other Comorbid Conditions† |
Depression | Obesity | Health Habits | All |
| Mobility† | 5.80 (4.77–7.05) | 4.93 (3.97–6.12) | 4.38 (3.62–5.29) | 4.97 (4.03–6.14) | 5.12 (4.21–6.22) | 5.55 (4.55–6.77) | 4.55 (3.61–5.73) | 2.85 (2.20–3.69) |
| Stair climbing§ | 5.27 (4.76–5.84) | 4.62 (4.19–5.11) | 4.12 (3.74–4.55) | 4.56 (4.09–5.08) | 4.43 (4.01–4.88) | 5.07 (4.58–5.62) | 4.66 (4.11–5.29) | 2.84 (2.48–3.26) |
| Upper extremity tasks¶ | 6.37 (5.80–6.99) | 5.60 (5.08–6.18) | 5.10 (4.61–5.65) | 5.56 (5.05–6.13) | 5.29 (4.81–5.82) | 6.22 (5.66–6.82) | 6.24 (5.55–7.02) | 3.96 (3.43–4.58) |
| Activities of daily living|| | 6.92 (6.25–7.67) | 6.24 (5.60–6.96) | 5.57 (4.98–6.23) | 6.04 (5.45–6.68) | 5.50 (4.93–6.13) | 6.62 (5.96–7.35) | 6.67 (5.97–7.46) | 4.33 (3.71–5.06) |
Demographic characteristics include age, ethnicity, and sex. All subsequent models adjusted for demographic characteristics in addition to the variables specified.
All comorbid conditions in Table 1 except arthritis.
Dichotomized as difficulty versus no difficulty walking one block.
Dichotomized as difficulty versus no difficulty climbing one flight of stairs.
Dichotomized as able to do ≥2 without difficulty versus able to do 1 or 0.
Dichotomized as difficulty (difficulty or dependence) versus no difficulty.
Pain was strongly associated with all measures of functional limitation regardless of whether subjects had arthritis, although the relationship between pain and functional limitation was stronger for subjects without arthritis, particularly for ADL difficulty (Table 3).
Table 3.
Adjusted Association Between Pain and Functional Limitations in Subjects with and without Arthritis
| Functional Limitation Measure | Adjusted for Demographic Characteristics | Interaction P-Value | Adjusted for All Characteristics* | Interaction P-Value | ||
|---|---|---|---|---|---|---|
| No Arthritis | Arthritis | No Arthritis | Arthritis | |||
| OR (95% CI) | OR (95% CI) | |||||
| Mobility | 4.61 (3.53–6.02) | 4.19 (3.20–5.48) | .64 | 3.24 (2.24–4.67) | 2.53 (1.82–3.51) | .34 |
| Stair climbing‡ | 4.88 (3.86–6.18) | 3.82 (3.45–4.24) | .12 | 3.78 (2.83–5.04) | 2.48 (2.14–2.88) | .02 |
| Upper extremity tasks§ | 6.49 (5.14–8.19) | 4.65 (4.17–5.19) | .05 | 5.66 (4.23–7.58) | 3.43 (2.96–3.99) | .02 |
| Activities of daily living¶ | 10.77 (8.07–14.35) | 4.74 (4.18–5.39) | < .001 | 9.18 (6.19–13.61) | 3.54 (3.02–4.14) | < .001 |
Demographics, socioeconomic status, comorbid conditions, depression, obesity, and health habits.
Dichotomized as difficulty versus no difficulty walking one block.
Dichotomized as difficulty versus no difficulty climbing one flight of stairs.
Dichotomized as able to do 2 or more without difficulty versus able to do 1 or 0.
Dichotomized as difficulty (difficulty or dependence) versus no difficulty.
OR = odds ratio; CI = confidence interval.
DISCUSSION
The relationship between pain and functional limitations was examined in a nationally representative sample of persons aged 50 and older. Four functional limitations that are strongly associated with aging and are part of the spectrum of late-life disability were considered.6,7 Declines in the ability to complete these and other similar functional tasks important for independent living are viewed by many patients and clinicians as the most important clinical manifestation of aging. This study found that subjects with significant pain develop the functional limitations classically associated with aging at markedly earlier ages. Across each functional limitation, the degree of limitation in subjects with pain appears similar to that of subjects without pain who are 2 to 3 decades older.
Because this was a cross-sectional study, it is not known whether pain is causing functional limitations or whether functional limitations are causing pain, but it seems likely that the relationship is bidirectional. The magnitude of this association strongly suggests mutual feedback loops in which pain and functional limitations are mutually reinforcing, with pain exacerbating functional limitations and functional limitations exacerbating pain. Although testing this hypothesis will require observational and interventional studies, the phenomenon of multiple conditions reinforcing each other in ways that cause downward health spirals is well described.26 Additional analyses that take advantage of the longitudinal follow-up in the HRS may be able to partially address some of these issues.
The powerful and robust association between pain and functional limitations suggests that pain and functional limitations may often be part of the same underlying pathophysiological process. This may sometimes make a more-unified clinical approach to these syndromes appropriate. Although routine evaluation for functional limitations is often only performed in geriatrics settings, a high prevalence of difficulty with activities important to daily functioning was found in subjects with pain many years before they reach ages viewed as “geriatric.” Because nearly one-quarter of subjects across the age range reported significant pain, the public health burden of these limitations is large. Although the prevalence of functional limitations increases markedly with age, the prevalence of significant pain was similar across the age ranges. This suggests that, in persons of similar age, pain may be a crucial clinical marker for being at high risk for functional limitations. This strongly implies that an evaluation for functional limitations should be part of the routine evaluation of all patients with significant pain. Furthermore, treatment strategies may need to focus on both pain management and functional rehabilitation. Similarly, evaluation and treatment of pain is an essential component of the evaluation of functional limitation. A recent meta-analysis supports the belief that self-management strategies focused on both pain and functional limitations may result in improvement of both syndromes.27
Most of the subjects with pain also had arthritis, and it is likely that arthritis contributes to functional limitation through its effects on joint morphology and through pain. For ADL tasks and upper extremity difficulty, pain had less effect on functional limitation in subjects with arthritis than those without arthritis. This is probably because arthritis, even in the absence of pain, has a substantial effect on functional ability, resulting in a lower marginal effect of pain. Nonetheless, the added effect of pain on all measures of functional limitation was high in subjects with arthritis.
The prevalence of pain was similar across age groups. This is in contrast to some studies finding a higher prevalence of pain with increasing age.19 In addition, other studies have reported higher pain prevalence than the current study.19,22 Although the reasons for these differences are not fully clear, subtle variations in how pain is assessed can affect its prevalence. For example, the requirement that pain be of at least moderate severity probably resulted in a lower prevalence estimate. Also, it was not required that pain be present daily, and daily persistent pain has a stronger association with age than more-sporadic pain.22
Strong associations between pain and functional limitations has been described extensively in the literature. For example, it has been shown that elderly people with back pain are more likely to develop ADL disability,17 and strong associations between musculoskeletal pain and functional limitations have been described.15 The current study extends this existing literature in several ways. First, because this was a population-based sample, it was possible to precisely quantify the association between multiple functional measures, providing nationally representative data. Second, because considerable data about other causes of functional limitations were available, it was possible to demonstrate that the association between pain and functional limitations is independent of many potential confounders. Finally, this was one of the first studies to examine the association between pain and functional limitations in the context of aging, leading to the novel finding that subjects with pain have functional status profiles similar to pain-free subjects 2 to 3 decades older.
The most important limitation of this study relates to the measurement of pain. Although the measure of pain that was used has face validity, capturing a measure of symptomatic distress that would be relevant to most subjects, assessment of pain was nonspecific. It was not known how long subjects had pain, its location, or cause. It was also not known whether subjects were receiving treatment for pain, although this probably biased the results toward more-conservative findings, because it would have resulted in the misclassification of subjects with treated pain as not having pain. Furthermore, although the assessment of pain is appropriately subjective, it is possible that pain and disability may affect the subjective interpretation of each condition. For example, it is possible that subjects with functional limitations felt a given level of pain to be more severe and that subjects with pain perceive a given level of functional limitation to be more severe. However, it is unlikely this potential measurement bias could fully explain the strength of association between pain and functional limitations.
In summary, this population-based study of the epidemiology of pain and functional limitations across middle and late life found strong associations between pain and functional limitations across many decades of life. In terms of their degree of limitation, subjects with pain are similar to subjects without pain who are 2 to 3 decades older. Evaluation and management strategies for pain and functional limitation should consider the strong co-occurrence of these conditions.
Acknowledgments
Supported by a Multidisciplinary Clinical Research Center Grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (5P60AR053308-020). The Health and Retirement Study, the data source for this study, is funded by the National Institute on Aging (U01AG009740). Dr. Covinsky is supported in part by a midcareer investigator award from the National Institute on Aging (5K24AG029812-02).
Sponsor’s Role: The study sponsor had no role in the design, methods, subject recruitment, data collection, analysis, or preparation of the paper.
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Author Contributions: Covinsky, Dunlop, and Yelin: study concept and design, acquisition of data, analysis and interpretation of data, and preparation of manuscript. Lindquist: acquisition of data, analysis and interpretation of data, and preparation of manuscript.
References
- 1.Covinsky KE, Palmer RM, Fortinsky RH, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses. Increased vulnerability with age. J Am Geriatr Soc. 2003;51:451–458. doi: 10.1046/j.1532-5415.2003.51152.x. [DOI] [PubMed] [Google Scholar]
- 2.Guralnik JM, Land KC, Blazer D, et al. Educational status and active life expectancy among older blacks and whites. N Engl J Med. 1993;329:110–116. doi: 10.1056/NEJM199307083290208. [DOI] [PubMed] [Google Scholar]
- 3.Guralnik JM, LaCroix AZ, Branch LG, et al. Morbidity and disability in older persons in the years prior to death. Am J Public Health. 1991;81:443–447. doi: 10.2105/ajph.81.4.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guralnik JM, LaCroix AZ, Abbott RD, et al. Maintaining mobility in late life. I. Demographic characteristics and chronic conditions. Am J Epidemiol. 1993;137:845–857. doi: 10.1093/oxfordjournals.aje.a116746. [DOI] [PubMed] [Google Scholar]
- 5.Guralnik JM, Fried LP, Salive ME. Disability as a public health outcome in the aging population. Annu Rev Public Health. 1996;17:25–46. doi: 10.1146/annurev.pu.17.050196.000325. [DOI] [PubMed] [Google Scholar]
- 6.Fried LP, Guralnik JM. Disability in older adults: Evidence regarding significance, etiology, and risk. J Am Geriatr Soc. 1997;45:92–100. doi: 10.1111/j.1532-5415.1997.tb00986.x. [DOI] [PubMed] [Google Scholar]
- 7.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: Evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56A:M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 8.Gill TM, Robison JT, Tinetti ME. Difficulty and dependence: Two components of the disability continuum among community-living older persons. Ann Intern Med. 1998;128:96–101. doi: 10.7326/0003-4819-128-2-199801150-00004. [DOI] [PubMed] [Google Scholar]
- 9.Gill TM, Robison JT, Tinetti ME. Predictors of recovery in activities of daily living among disabled older persons living in the community. J Gen Intern Med. 1997;12:757–762. doi: 10.1046/j.1525-1497.1997.07161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mor V, Wilcox V, Rakowski W, et al. Functional transitions among the elderly: Patterns, predictors, and related hospital use. Am J Public Health. 1994;84:1274–1280. doi: 10.2105/ajph.84.8.1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gill TM, Allore H, Holford TR, et al. The development of insidious disability in activities of daily living among community-living older persons. Am J Med. 2004;117:484–491. doi: 10.1016/j.amjmed.2004.05.018. [DOI] [PubMed] [Google Scholar]
- 12.Fries JF. Measuring and monitoring success in compressing morbidity. Ann Intern Med. 2003;139(5 Pt 2):455–459. doi: 10.7326/0003-4819-139-5_part_2-200309021-00015. [DOI] [PubMed] [Google Scholar]
- 13.Edmond SL, Felson DT. Function and back symptoms in older adults. J Am Geriatr Soc. 2003;51:1702–1709. doi: 10.1046/j.1532-5415.2003.51553.x. [DOI] [PubMed] [Google Scholar]
- 14.Ensrud KE, Nevitt MC, Yunis C, et al. Correlates of impaired function in older women. J Am Geriatr Soc. 1994;42:481–489. doi: 10.1111/j.1532-5415.1994.tb04968.x. [DOI] [PubMed] [Google Scholar]
- 15.Leveille SG, Ling S, Hochberg MC, et al. Widespread musculoskeletal pain and the progression of disability in older disabled women. Ann Intern Med. 2001;135:1038–1046. doi: 10.7326/0003-4819-135-12-200112180-00007. [DOI] [PubMed] [Google Scholar]
- 16.Reid MC, Guo Z, Towle VR, et al. Pain-related disability among older male veterans receiving primary care. J Gerontol A Biol Sci Med Sci. 2002;57A:M727–M732. doi: 10.1093/gerona/57.11.m727. [DOI] [PubMed] [Google Scholar]
- 17.Reid MC, Williams CS, Gill TM. Back pain and decline in lower extremity physical function among community-dwelling older persons. J Gerontol A Biol Sci Med Sci. 2005;60A:793–797. doi: 10.1093/gerona/60.6.793. [DOI] [PubMed] [Google Scholar]
- 18.Weiner DK, Haggerty CL, Kritchevsky SB, et al. How does low back pain impact physical function in independent, well-functioning older adults? Evidence from the Health ABC Cohort and implications for the future. Pain Med. 2003;4:311–320. doi: 10.1111/j.1526-4637.2003.03042.x. [DOI] [PubMed] [Google Scholar]
- 19.AGS Panel on Persistent Pain in Older Persons. The management of persistent pain in older persons. J Am Geriatr Soc. 2002;50(6 Suppl):S205–S224. doi: 10.1046/j.1532-5415.50.6s.1.x. [DOI] [PubMed] [Google Scholar]
- 20.Ettinger WH, Jr, Fried LP, Harris T, et al. Self-reported causes of physical disability in older people: The Cardiovascular Health Study. CHS Collaborative Research Group. J Am Geriatr Soc. 1994;42:1035–1044. doi: 10.1111/j.1532-5415.1994.tb06206.x. [DOI] [PubMed] [Google Scholar]
- 21.Helme RD, Gibson SJ. The epidemiology of pain in elderly people. Clin Geriatr Med. 2001;17:417–431. doi: 10.1016/s0749-0690(05)70078-1. [DOI] [PubMed] [Google Scholar]
- 22.Mantyselka PT, Turunen JH, Ahonen RS, et al. Chronic pain and poor self-rated health. JAMA. 2003;290:2435–2442. doi: 10.1001/jama.290.18.2435. [DOI] [PubMed] [Google Scholar]
- 23.Scudds RJ, Ostbye T. Pain and pain-related interference with function in older Canadians: The Canadian Study of Health and Aging. Disabil Rehabil. 2001;23:654–664. doi: 10.1080/09638280110043942. [DOI] [PubMed] [Google Scholar]
- 24.Juster F, Suzman R. An overview of the health and retirement study. J Hum Resour. 1995;30:S7–S56. [Google Scholar]
- 25.Wallace RB, Herzog AR, Ofstedal MB, et al. HRS/AHEAD Documentation Report: Documentation of affective functioning measures in the Health and Retirement Study. Ann Arbor, MI: Survey Research Center; University of Michigan; 2000. [Google Scholar]
- 26.Tinetti ME, Inouye SK, Gill TM, et al. Shared risk factors for falls, incontinence, and functional dependence. Unifying the approach to geriatric syndromes. JAMA. 1995;273:1348–1353. [PubMed] [Google Scholar]
- 27.Reid MC, Papaleontiou M, Ong A, et al. Self-management strategies to reduce pain and improve function among older adults in community settings: A review of the evidence. Pain Med. 2008;9:409–424. doi: 10.1111/j.1526-4637.2008.00428.x. [DOI] [PMC free article] [PubMed] [Google Scholar]