Abstract
Employers may be loath to fund vaccination programs without understanding the economic consequences. We developed a decision analytic computational simulation model including dynamic transmission elements that determined the cost-benefit of employer-sponsored workplace vaccination from the employer's perspective. Implementing such programs was relatively inexpensive (<$35/vaccinated employee) and, in many cases, cost saving across diverse occupational groups in all seasonal influenza scenarios. Such programs were cost-saving for a 20% serologic attack rate pandemic scenario (−$15 to −$995) per vaccinated employee) and a 30% serologic attack rate pandemic scenario (range −$39 to −$1,494 per vaccinated employee) across all age and major occupational groups.
Keywords: Influenza, Workplace, Vaccination
Introduction
In 2009 an estimated 60% of U.S. adults over the age of 18 were employed, with approximately 16% remaining in the workforce beyond their 65th year of life.[1] Consequently, working adults comprise a large population segment which can be affected by influenza.[2] Employees spend a substantial amount of time at their place of work—on average 38.9 hours per week—with 26.5% of the workforce exceeding 40 hours per week.[3] Studies have documented contact patterns at workplace conducive to influenza's spread.[4-6] Vaccinating employees against seasonal and, in years such as 2009, pandemic influenza can help employers prevent influenza-induced absenteeism that leads to lost workplace productivity.[7-8]
Recognizing the central role businesses and employers play in protecting the health and safety of their employees, the Centers for Disease Control and Prevention (CDC) and the Occupational Safety and Health Administration (OSHA) have produced materials intended to guide employers in their planning and preparedness for seasonal and pandemic influenza. The guidance is intended to help employers take actions to decrease influenza spread, maintain business continuity, and secure critical infrastructure.[9-10] OSHA recommends that employers prioritize vaccination—an engineering work practice control—because it is a long-term and effective intervention that reduces reliance on employee behavioral changes such as hand hygiene and respiratory etiquette.[9] The CDC also recommends that employers: encourage employees to seek vaccination against both seasonal and pandemic influenza, offer influenza vaccination opportunities at their worksite or consider allowing employees time off from work to seek vaccination, and negotiate with insurers for coverage of influenza vaccination.[10] In February of 2010 the Advisory Committee for Immunization Practices (ACIP) released the provisional recommendation that all people 6 months of age or older receive annual influenza vaccination, unless contraindicated.[11-12]
Despite the potential benefits of vaccination, self-reports as part of the National Health Interview Survey suggest that vaccine coverage among healthy adults 18 to 49 years is only approximately 20%.[13] Offering vaccination in the workplace could increase coverage by making vaccination more convenient and reducing or eliminating the associated cost may further improve influenza vaccine uptake. Studies have shown that individuals who received influenza vaccine at work cited convenience as an important factor in the decision to be vaccinated.[14-16] Following physicians' offices, workplaces are the most common location to receive an influenza vaccination, with one-third of 18-49 year old vaccine recipients and one-fifth of 50-64 year old vaccine recipients receiving the vaccine at work.[17] The addition of workplace education programs can provide information and allay employees' concerns about influenza vaccination.
Workplace vaccination programs can be costly, requiring health worker time and diverting employees' time from work; individual employers may be loath to provide such a service without understanding its economic potential benefits. Although studies have demonstrated the cost-effectiveness of vaccinating healthy adults, few have looked specifically at employer-sponsored vaccination programs—along with associated administration and education costs—and how their economic value may vary by type of workplace.[18-21] Bridges et al and Nichol et al concluded that vaccination of working adults is cost-effective when the vaccine is well-matched to the predominant circulating strain of influenza, but may not provide an economic benefit in all years.[20-21]
Several cost-effectiveness analyses have assumed the societal and third party payor perspectives, but these approaches may not yield results directly relevant to employers who are more concerned about how such interventions will affect the budgets of their specific organizations or companies.[19, 22-24] A few studies have looked at specific vaccination programs at particular work sites (including chemical plants in Brazil and Malaysia, a bank in Columbia, and textile plants in North Carolina), but the value of such interventions may vary depending on an employer's industry and firm size.[18, 25-27]
We developed a computational simulation model to estimate the economic value of employer-sponsored workplace influenza vaccination across each of the top 22 major occupational groups in the United States, as defined by the Bureau of Labor Statistics. Sensitivity analyses varied key model parameters and allowed us to delineate how the cost-benefit of such strategies may vary by occupational group, effective or net reproductive number (R) of influenza (the average number of secondary cases generated per primary case during the infectious period[28-29]), vaccine cost, vaccine type [live attenuated influenza vaccine (LAIV) versus trivalent inactivated vaccine (TIV)], incentive to individual employees for vaccination, influenza scenario (pandemic vs. seasonal) and age-stratified risk of influenza. The results of our model, particularly those from the sensitivity analyses, may help guide individual employers in their decision making.
Materials and methods
Model Structure
Using TreeAge Pro 2009 (TreeAge Software, Williamstown, MA), we constructed a stochastic decision analytic computational model that included dynamic transmission elements to simulate the decision of whether to implement a workplace-based influenza vaccination program from the employer's perspective. This model accounted for the costs of workplace-based vaccination, including lost productivity from employees' participation in the vaccination queue, and productivity losses from influenza-induced absenteeism. It was assumed that the employer bore all costs associated with vaccine education and administration, including paying for a healthcare professional to administer vaccine, vaccine costs, and an educational initiative that would divert time from work productivity. Previously developed materials, including videos, online content and printable handouts freely available from the U.S. Department of Health and Human Services flu.gov website and the U.S. Centers for Disease Control and Prevention Seasonal Influenza website were the materials selected for the employee educational intervention in this analysis.[12, 30]
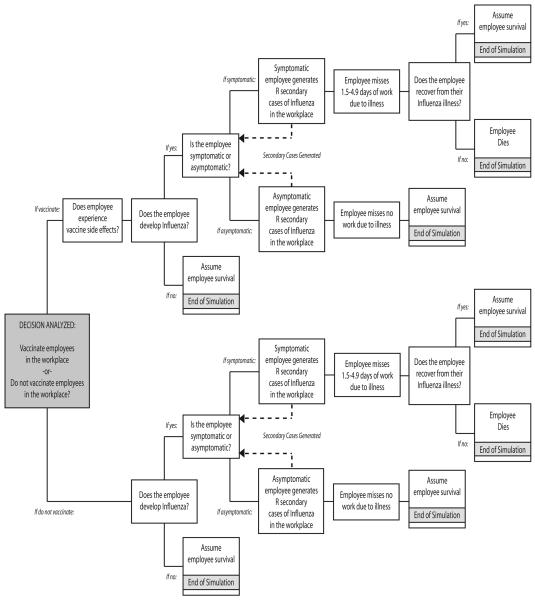
Figure 1 is a graphic representation of the decision and subsequent outcomes analyzedby our cost-benefit economic model. The grey box to the left represents the decision (whether or not employees should be vaccinated against influenza in the workplace) and the subsequent boxes represent possible outcomes; the probability of each event and its attendant costs are drawn from a set of model input parameters and probability distributions, as defined in Table 1. Each new case generated via workplace contact cycles into the model and progresses through until a terminus is reached. An employee's risk of contracting influenza depended on whether he or she received an influenza vaccine and the efficacy of that vaccine. Baseline analyses focused on the impact on the vaccine recipient and did not consider indirect protection conferred to non-vaccinated employees. Additional scenarios incorporated transmission into the model whereby an infected individual generated a number of additional cases at work, based on the value of R input into the model.
Figure 1.
Schematic of the decision (whether to implement a workplace-based influenza vaccination program from the employer's perspective) and subsequent outcomes analyzed by our stochastic decision analytic computational model
TABLE 1.
Model Inputs
| Description (Units) | Mean | 95% Range |
Source | |
|---|---|---|---|---|
| Lower Limit |
Upper Limit |
|||
| COSTS (US$) | ||||
|
| ||||
| Nurse Hourly Salary | 27.20 | 13.85 | 56.57 | [36] |
| Inactivated Influenza Vaccine (TIV) | 11.63 | 8.12 | 15.14 | [44] |
| Live Attenuated Influenza Vaccine (LAIV) | 19.70 | --- | --- | [44] |
|
| ||||
| DURATIONS | ||||
|
| ||||
| Nurse Time Per Vaccination (minutes) | 5 | --- | --- | [19] |
| Employee Time for Education (minutes) | 30 | --- | --- | Assumption |
| Employee Time Per Vaccination (minutes) | 30 | --- | --- | [19] |
| Vaccine Side Effects (days) | 0.75 | 0.5 | 1 | [45] |
| Influenza-related absenteeism (days) | 2.7 | 1.5 | 4.9 | [2] |
| Work Hours per Day | 8 | --- | --- | Assumption |
|
| ||||
| PROBABILITIES (%) | ||||
|
| ||||
| Influenza for Unvaccinated Employee (18-49 yrs) | 6.6 | 3.2 | 10.0 | [46] |
| Influenza for Unvaccinated Employee (50-64 yrs) | 6.6 | 3.2 | 10.0 | [46] |
| Influenza for Unvaccinated Employee (65+ yrs) | 9.0 | 4.2 | 13.8 | [46] |
| Death given Influenza Infection (18-49 yrs) | 0.009 | 0.003 | 0.015 | [46] |
| Death given Influenza Infection (50-64 yrs) | 0.134 | 0.044 | 0.224 | [46] |
| Death given Influenza Infection (65+ yrs) | 1.17 | 0.390 | 1.95 | [46] |
| Vaccine Efficacy | 80 | 56 | 91 | [47] |
|
| ||||
| SENSITIVITY ANALYSES | Values | Source | ||
|
| ||||
| Effective Reproductive Number (R) | 0.0, 1.2, 1.6 | Assumption | ||
| Employee Age (years) | 18-49, 50-64, 65+ | Assumption | ||
| Probability of Influenza (pandemic setting) | Baseline (as above), 20%, 30% | Assumption | ||
| Percentage of Illness that is Symptomatic | 50%, 65%, 80% | [19, 31-34, 48-49] |
||
Each employee who developed influenza had a probability of developing symptomatic or asymptomatic disease. It was assumed that asymptomatic individuals (whether infectious or not) missed no work, while those with true symptomatic influenza or influenza-like-illness (ILI) stayed home from work (the duration of this absenteeism determined by a probability draw from a uniform distribution ranging from 1.5 to 4.9 days), resulting in a productivity loss to the employer equivalent to that employee's salary through the duration of absenteeism. Our model did not differentiate between ILI and true influenza disease for symptomatic individuals, as this distinction cannot truly be made without clinical laboratory testing. The percent of individuals with influenza disease who are symptomatic has been reported to range widely, from 40%-50% for 2009 H1N1 and 67-86% for seasonal influenza.[31-34] For the purpose of these analyses, the cost of interim replacement labor was not considered.
A small percentage of employees did not survive influenza (the baseline scenario usedthe seasonal influenza case fatality rate for healthy median working-age adults) and accrued a productivity loss equivalent to the median tenure of employment, defined as the point at which half of all workers had more tenure and half had less tenure at the same firm.[35] The model assumed that employees were otherwise healthy individuals.
For each simulation run, the following formula determined the incremental cost-benefit of vaccination:
| (1) |
Data Inputs
Table 1 lists various probability and cost data inputs for our model and the corresponding data sources used. All probability variables drew from beta distributions; all other variables drew from gamma distributions, except for the duration of absenteeism which drew from a uniform distribution ranging from 1.5 to 4.9 days, based on data from a literature review on influenza and work absenteeism.[2] All costs were converted into 2009 U.S. dollars using a 3% discount rate. Our model assumed 8 hours in a workday, 5 workdays in a week, 30 minutes of employee time for vaccine education prior to the vaccination session, 30 minutes of employee time lost for wait in the queue and vaccine administration, and 5 minutes of nurse time for brief questions and administration per employee receiving an influenza vaccination.[19]
Sensitivity Analyses
Sensitivity analyses systematically varied key model variables including the probability of symptomatic influenza or influenza-like-illness (50% to 80%), the duration of absenteeism (1.5 to 4.9 days), vaccine cost (TIV: $11.63 [95% CI: $8.12-$15.14] and LAIV: $19.70 per dose, respectively), and influenza risk or serologic attack rate among employees (3.2% to 30%).[9] Varying the last parameter simulated pandemic influenza scenarios. Additional scenarios examined trivalent inactivated (TIV) versus live attenuated influenza vaccine (LAIV) use.
The base case scenario (where R=0) only focused on vaccine benefits for the individual and did not account for secondary cases that an infected employee might generate in the workplace during the infectious period. Another set of scenarios accounted for potential transmission of influenza in the workplace by varying the R of influenza from 1.2 to 1.6. Finally, a set of scenarios examined the cost-benefit of offering each employee a financial incentive to get vaccinated. For each simulation run, probabilistic sensitivity analyses evaluated the effects of simultaneously varying all input parameters over the ranges listed in Table 1.
Occupational Groups
Every workplace consists of a mixture of individuals serving various roles. To help employers understand how their specific mixture of employees may affect the economic impact of vaccination, sensitivity analyses explored the economic effects of vaccinating individuals from each of the top 22 major occupational groups in the United States as defined by the Bureau of Labor Statistics and listed in Table 2.[36]
Table 2.
Characteristics of the 22 Major Occupational Groups in the United States—May 2008[24]
| Occupational Group Ranked By Median Hourly Wage (Low to High) |
Number Employed | Median Wage (80% Range) in US$ |
Median Length of Tenure in Years |
|---|---|---|---|
|
All Occupations (Based on the median wage & tenure of working adults) |
135,185,230 | 15.57 (8.02, 37.99) | 4.1 |
| Food Preparation and Serving Related | 11,438,550 | 8.59 (6.89, 14.41) | 2 |
| Farming, Fishing, and Forestry | 438,490 | 9.34 (7.71, 18.27) | 3.1 |
| Personal Care and Service | 3,437,520 | 9.82 (7.19, 18.64) | 2.6 |
| Building and Grounds Cleaning and Maintenance | 4,429,870 | 10.52 (7.48, 18.07) | 3.6 |
| Sales and Related | 14,336,430 | 11.69 (7.43, 34.23) | 2.9 |
| Healthcare Support | 3,779,280 | 11.80 (8.25, 18.48) | 3.1 |
| Transportation and Material Moving | 9,508,750 | 13.14 (7.89, 24.63) | 3.8 |
| Production | 9,919,120 | 13.99 (8.53, 25.11) | 5 |
| Office and Administrative Support | 23,231,750 | 14.32 (8.63, 24.30) | 4.2 |
| Protective Service | 3,128,960 | 16.65 (8.73, 34.05) | 5.9 |
| Construction and Extraction | 6,548,760 | 18.24 (10.69, 33.81) | 3.5 |
| Community and Social Services | 1,861,750 | 18.38 (10.62, 32.03) | 4.8 |
| Installation, Maintenance, and Repair | 5,374,850 | 18.60 (10.46, 30.99) | 5 |
| Arts, Design, Entertainment, Sports, and Media | 1,804,940 | 19.99 (9.33, 43.18) | 3.4 |
| Education, Training, and Library | 8,451,250 | 21.26 (9.58, 38.84) | 5.4 |
| Healthcare Practitioner and Technical | 7,076,800 | 27.20 (13.85, 56.57) | 4.9 |
| Life, Physical, and Social Science | 1,296,840 | 27.51 (14.56, 52.07) | 4 |
| Business and Financial Operations | 6,135,520 | 27.89 (15.88, 49.59) | 4.6 |
| Architecture and Engineering | 2,521,630 | 32.09 (17.31, 54.65) | 6.4 |
| Computer and Mathematical Science | 3,308,260 | 34.26 (18.04, 56.69) | 4.5 |
| Legal | 1,003,270 | 34.49 (16.04, **) | 4.3 |
| Management | 6,152,650 | 42.15 (20.40, **) | 6 |
NOTE:
This wage is equal to or greater than $80.00 per hour and not reported by the U.S. Bureau of Labor Statistics.
Results
Each simulation run was comprised of 1,000 trials of 1,000 simulated employees, resulting in 1,000,000 hypothetical vaccination decisions. From here on, all reported positive dollar value results represent a net cost to the employer while all negative dollar values indicate net cost savings to the employer.
Our initial set of seasonal influenza simulation runs used a seasonal influenza attack rate stratified by age (6.6% ± 1.7% for employees age 18-64 and 9.0% ± 2.4% for employees over the age of 65) and only considered the effects of vaccination on the vaccine recipient and not on other unvaccinated employees (R=0). Additional scenarios explored the impact of varying R (R=0, 1.2 and 1.6), vaccine type (TIV or LAIV) and the percentage of influenza cases that were symptomatic (50%, 65%, and 80%). Results for all 22 major occupational groups and the median wage American worker (denoted "all occupations"), presented as median incremental cost (US$) per employee vaccinated are presented in Table 3 (TIV) and Table 4 (LAIV). In Table 3 the range of values in each cell reflects the range of 3 median costs—for adults aged 18-49, 50-64, and over 65—in each scenario.
Table 3.
Median Incremental Cost per Employee (US$) for Employer-Sponsored Seasonal Influenza Vaccination—TIV
| Occupational Group Ranked By Median Hourly Wage (Low to High) |
50% Symptomatic | 65% Symptomatic | 80% Symptomatic | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Workplace Ra | Workplace Ra | Workplace Ra | |||||||
| 0 | 1.2 | 1.6 | 0 | 1.2 | 1.6 | 0 | 1.2 | 1.6 | |
|
All Occupations (based on median wage & tenure) |
18 to 20 | −17 to −9 | −28 to −10 | 14 to 15 | −21 to −20 | −31 to −27 | 8 to 9 | −28 to −26 | −38 to −36 |
| Food Preparation & Serving Related | 16 to 17 | −2 to 2 | −8 to 5 | 14 to 15 | −4 to −2 | −10 to −9 | 12 to 12 | −6 to −6 | −13 to −11 |
| Farming, Fishing, & Forestry | 17 to 17 | −4 to 1 | −11 to 3 | 14 to 14 | −7 to −4 | −13 to −12 | 10 to 11 | −10 to −7 | −18 to −14 |
| Personal Care & Service | 17 to 17 | −4 to −2 | −3 to 0 | 14 to 14 | −8 to −5 | −14 to −9 | 11 to 12 | −11 to −11 | −19 to −16 |
| Building and Grounds Cleaning & Maintenance | 17 to 18 | −4 to 0 | −12 to 2 | 14 to 14 | −8 to −4 | −14 to −12 | 11 to 12 | −10 to −7 | −18 to −16 |
| Sales & Related | 18 to 19 | −12 to −7 | −16 to −6 | 14 to 14 | −19 to −12 | −28 to −25 | 9 to 10 | −20 to −19 | −32 to −30 |
| Healthcare Support | 17 to 18 | −7 to 0 | −14 to 1 | 14 to 15 | −9 to −4 | −17 to −14 | 11 to 11 | −12 to −12 | −20 to −17 |
| Transportation & Material Moving | 17 to 19 | −9 to −2 | −9 to −5 | 14 to 14 | −12 to −10 | −22 to −18 | 10 to 10 | −18 to −14 | −27 to −26 |
| Production | 18 to 19 | −10 to −5 | −12 to −3 | 14 to 15 | −16 to −11 | −24 to −18 | 10 to 10 | −19 to −18 | −29 to −25 |
| Office and Administrative Support | 18 to 19 | −10 to −4 | −19 to −4 | 14 to 14 | −15 to −13 | −22 to −20 | 9 to 10 | −19 to −18 | −28 to −27 |
| Protective Service | 18 to 20 | −16 to −8 | −20 to −10 | 14 to 15 | −20 to −19 | −32 to −30 | 9 to 10 | −28 to −27 | −40 to −36 |
| Construction & Extraction | 19 to 21 | −19 to −8 | −31 to −12 | 14 to 14 | −24 to −19 | −35 to −33 | 8 to 9 | −28 to −28 | −42 to −38 |
| Community & Social Services | 19 to 20 | −18 to −11 | −29 to −13 | 14 to 14 | −22 to −14 | −37 to −30 | 9 to 10 | −28 to −28 | −40 to −37 |
| Installation, Maintenance, & Repair | 19 to 21 | −15 to −10 | −29 to −11 | 14 to 16 | −23 to −21 | −34 to −30 | 7 to 9 | −28 to −27 | −41 to −40 |
| Arts, Design, Entertainment, Sports, & Media | 19 to 22 | −22 to −14 | −34 to −20 | 14 to 14 | −27 to −22 | −44 to −36 | 9 to 9 | −36 to −36 | −55 to −49 |
| Education, Training, & Library | 20 to 22 | −21 to −13 | −34 to −18 | 14 to 15 | −27 to −22 | −41 to −35 | 6 to 10 | −34 to −32 | −51 to −47 |
| Healthcare Practitioner & Technical | 21 to 24 | −36 to −23 | −54 to −35 | 14 to 15 | −42 to −36 | −59 to −55 | 5 to 6 | −58 to −51 | −73 to −69 |
| Life, Physical, & Social Science | 21 to 23 | −36 to −28 | −52 to −26 | 14 to 17 | −44 to −30 | −61 to −56 | 4 to 6 | −51 to −44 | −70 to −63 |
| Business & Financial Operations | 22 to 24 | −35 to −26 | −52 to −33 | 13 to 14 | −40 to −38 | −59 to −57 | 5 to 6 | −51 to −48 | −67 to −62 |
| Architecture & Engineering | 23 to 26 | −40 to −26 | −60 to −36 | 13 to 17 | −48 to −39 | −66 to −50 | 4 to 5 | −58 to −57 | −74 to −73 |
| Computer & Mathematical Science | 19 to 25 | −39 to −29 | −64 to −38 | 14 to 16 | −50 to −45 | −75 to −70 | 3 to 5 | −60 to −59 | −86 to −84 |
| Legal | 24 to 28 | −50 to −38 | −74 to −53 | 12 to 15 | −61 to −51 | −86 to −75 | 2 to 4 | −72 to −69 | −98 to −93 |
| Management | 25 to 30 | −62 to −41 | −89 to −58 | 12 to 14 | −68 to −66 | −95 to −91 | 1 to 2 | −83 to −75 | −115 to −103 |
NOTE: Negative values (shaded in grey) indicate cost savings.
R represents the effective reproductive number (R) of influenza within a workplace. This is the average number of secondary cases generated per primary case during the infectious period. The age-stratified serologically confirmed influenza attack rates assumed for the above scenarios are: 6.6% (95% CI: 3.2%-10.0%) for employees age 18-64 and 9.0% (95% CI: 4.2%-13.8%) for employees over the age of 65.
Table 4.
Median Incremental Cost per Employee (US$) for Employer-Sponsored Seasonal Influenza Vaccination—LAIV
| Occupational Group Ranked By Median Hourly Wage (Low to High) |
50% Symptomatic | 65% Symptomatic | 80% Symptomatic | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Workplace Ra | Workplace Ra | Workplace Ra | |||||||
| 0 | 1.2 | 1.6 | 0 | 1.2 | 1.6 | 0 | 1.2 | 1.6 | |
|
All Occupations (based on median wage & tenure) |
29 | 1 | −8 | 23 | −10 | −21 | 17 | −16 | −29 |
| Food Preparation & Serving Related | 25 | 9 | 6 | 23 | 6 | 1 | 20 | 2 | −4 |
| Farming, Fishing, & Forestry | 26 | 8 | 2 | 22 | 3 | −5 | 19 | −2 | −9 |
| Personal Care & Service | 26 | 8 | 2 | 22 | 2 | −2 | 20 | −3 | −9 |
| Building and Grounds Cleaning & Maintenance | 27 | 8 | 3 | 23 | 5 | −4 | 19 | −2 | −9 |
| Sales & Related | 28 | 0 | −10 | 22 | −7 | −13 | 19 | −9 | −21 |
| Healthcare Support | 26 | 7 | 1 | 22 | 4 | −6 | 19 | −1 | −12 |
| Transportation & Material Moving | 26 | 5 | −6 | 23 | −3 | −11 | 18 | −8 | −16 |
| Production | 27 | 3 | −5 | 23 | 0 | −9 | 19 | −9 | −15 |
| Office and Administrative Support | 27 | 3 | −3 | 23 | −1 | −12 | 18 | −9 | −18 |
| Protective Service | 28 | −1 | −11 | 23 | −11 | −21 | 18 | −17 | −28 |
| Construction & Extraction | 28 | −1 | −12 | 22 | −9 | −24 | 17 | −18 | −28 |
| Community & Social Services | 28 | −1 | −11 | 23 | −6 | −19 | 17 | −19 | −32 |
| Installation, Maintenance, & Repair | 29 | −1 | −14 | 23 | −9 | −21 | 17 | −19 | −32 |
| Arts, Design, Entertainment, Sports, & Media | 30 | −6 | −18 | 22 | −16 | −21 | 17 | −25 | −41 |
| Education, Training, & Library | 29 | −2 | −19 | 23 | −14 | −25 | 17 | −24 | −34 |
| Healthcare Practitioner & Technical | 32 | −16 | −26 | 22 | −32 | −48 | 15 | −42 | −63 |
| Life, Physical, & Social Science | 32 | −14 | −30 | 23 | −23 | −42 | 14 | −37 | −62 |
| Business & Financial Operations | 32 | −11 | −28 | 22 | −25 | −43 | 17 | −36 | −60 |
| Architecture & Engineering | 33 | −13 | −39 | 25 | −27 | −52 | 13 | −46 | −70 |
| Computer & Mathematical Science | 34 | −20 | −38 | 24 | −27 | −57 | 15 | −51 | −68 |
| Legal | 36 | −23 | −54 | 24 | −38 | −68 | 10 | −62 | −90 |
| Management | 35 | −32 | −54 | 23 | −54 | −78 | 10 | −75 | −101 |
NOTE: Negative values (shaded in grey) indicate cost savings.
R represents the effective reproductive number (R) of influenza within a workplace. This is the average number of secondary cases generated per primary case during the infectious period. The serologically confirmed influenza attack rate assumed for adults 18-49 in the above scenarios was 6.6% (95% CI: 3.2%-10.0%).
Trivalent Inactivated Vaccine (TIV) Scenarios
When R=0, vaccination was never cost saving. When R was held constant and the probability of symptomatic illness and subsequent productivity loss is ≤ 50%, the cost per employee vaccinated increased with increasing wage. The cost per employee vaccinated decreased with increasing wage when the percent of symptomatic illness was ≥ 65%. As R and the percentage of symptomatic illness increased, the cost per employee vaccinated decreased; employee vaccination was cost saving for the median wage American worker in all TIV and LAIV scenarios when R=1.2 or 1.6, and cost saving to near cost-neutral for occupations with lower median hourly wages. Per employee cost decreased with increasing age across all simulations, e.g. cost was lower for 65+ year old employees than for 50-64 year olds, and lower still compared to 18-49 year olds, for whom the cost per employee vaccinated was highest across all scenarios.
Live Attenuated Influenza Virus (LAIV) Scenarios
Results for simulations with LAIV are presented in Table 4. The median cost per employee is for adults ages 18-49 only, as LAIV isn't FDA licensed for use in older adults.[37] For a given R, when the probability of symptomatic illness and subsequent productivity loss is ≤ 50%, the cost per employee vaccinated increases with increasing hourly wage. The cost per employee vaccinated decreases with increasing wage when the percent of symptomatic illness is ≥ 65%.
Cost per employee vaccinated was slightly higher for LAIV scenarios than for TIV and yielded cost savings across fewer of the major occupational groups, owing to the higher cost of the LAIV vaccine.
Pandemic Influenza Scenarios
Another set of scenarios explored pandemic scenarios with higher serologic attack rates of 20% and 30% (data not shown). For pandemic scenarios with an attack rate of 20% and TIV where protection to the unvaccinated was not considered (R=0), employee vaccination generated cost savings across all age and occupational groups (median price per employee vaccinated ranging from −$598 to −$25). When R increased to 1.2 the cost savings increased (range: −$843 to −$66 per employee vaccinated), and when R=1.6, the cost savings were higher still (range: −$882 to −82). An attack rate of 30% yielded even greater cost savings per employee vaccinated: when R=0 the range was −$1,116 to −$44; a higher R of 1.2 yielded a range of −$1,200 to −$110, and R=1.6 yielded the highest cost savings of −$1,273 to −$132 per employee vaccinated
All scenarios across all occupational groups using LAIV (in the 18-49 year old age group only) yielded cost savings. When the attack rate was 20% and R=0 the savings per employee vaccinated ranged from −$615 to −$15. An R of 1.2 yielded greater cost savings with a range from −$829 to −$57 per employee, and scenarios where R=1.6 resulted in the greater savings (range: −$995 to $68 per employee vaccinated). Use of LAIV during a pandemic with an attack rate of 30% offered increased cost savings compared to scenarios with lower attack rates; when R=0 the range across occupational groups was −$1,095 to −$39 per vaccinated employee. Increasing R to 1.2 resulted in higher cost savings (range: −$1,354 to −$103 per vaccinee), and an R of 1.6 yielded even greater cost savings of −$1,494 to −$117 per employee vaccinated.
During a pandemic scenario with an elevated influenza attack rate both TIV and LAIV yielded cost savings for employees in all 22 major occupational groups, regardless of whether transmission in the workplace is accounted for. These savings were slightly less for LAIV than TIV scenarios because of the higher cost of the LAIV vaccine.
Employee Incentive
Although not conducted as an explicit analysis, the added cost of employee incentives for vaccination can be estimated by adding the cost of the incentive (per employee) to the relevant median incremental cost in Table 3 or 4. This approach allows flexibility in the interpretation and application of our results, without the limitation of a fixed incentive cost. For example, if an employer was interested in the offering an incentive (such as a $10 gift card) to employees who accept vaccination $10 should be added to the medianincremental cost of vaccination per employee.
Discussion
Our study suggests that employer-supported workplace-based influenza vaccination can be relatively inexpensive (<$35 per vaccinated employee) or cost saving for employers, even when ignoring the benefits of vaccination to unvaccinated employees. These findings hold across a wide variety of occupational groups. For many occupational groups, vaccination may even be cost saving; employers could gain money by implementing such programs. Factoring in the potential benefits of vaccination for the unvaccinated only improves the cost savings of vaccination programs. Certain employers will realize a greater return on influenza vaccination, especially those investing heavily in the productivity of their employees.
Improving access, by means of an employer sponsored in-house program or paid time to seek vaccination, may also serve as an incentive to increase vaccine uptake; employees may be reluctant to pay out-of-pocket for the influenza vaccine or take time off from work for immunization if it will affect their pay or accrued personal time. Future studies are needed to further delineate the impact of incentives on vaccine uptake among the general non-healthcare working population.
Because adults spend a large amount of time at their place of work, an employer's decision to implement a workplace-based influenza vaccination program can have broad impact on the health of individuals, a workplace and the total population. The health of employees is central to workplace productivity, and subsequently, local, national and global economies and infrastructure. The CDC and OSHA have recommended that businesses and employers develop preparedness plans for seasonal and pandemic influenza that prioritize employee vaccination.[9-10] Employee vaccination programs are an example of engineering work practice controls — enduring and effective interventions that do not rely on individual behavior change. Employers who subsidize workplace vaccination programs stand to see significant a significant return on their investment, particularly during a severe influenza season or pandemic when employee productivity may be interrupted by influenza-related absenteeism.
Employers collectively bearing the costs of influenza immunization could alleviate some of the burden on the already strained public health and medical systems. Studies have implied that many businesses are not currently implementing influenza vaccination programs, even though recent concerns of a pandemic have motivated some businesses to develop pandemic influenza preparedness plans.[14, 17, 38-39] One potential problem is that existing studies have been from specific workplaces at specific locations. For example, a study of a Malaysian petrochemical plant demonstrated that workplace vaccination clearly decreased influenza-like illness rates and absenteeism.[26] A cost-benefit analysis of a workplace vaccination program at a Brazilian pharma-chemical company yielded a net benefit of $121,441 or $35.45 per vaccinated employee in 1997 U.S. dollars.[25] A clinical trial at six North Carolina textile plants showed that a vaccination program saved $22.36 per lost workday and $2.58 per dollar invested.[18] A prospective observational study at a Columbian bank estimated an employer savings of $6.40 to $25.80 US per vaccinated employee. A vaccine campaign at First Data Resources Limited in Basildon, Essex UK, resulted in substantial decreases in influenza-like illness.[40] It is not clear, however, if employers view results from a limited number of workplaces as being applicable to their unique setting.
Constructing economic models from the employer's perspective can help employers understand the value of vaccination. Many existing economic models that take the perspective of society and third party payors may be helpful in making policy and insurance coverage and reimbursement decisions but may not motivate individual employers. Although cost-effectiveness models can provide important information to policy-makers, employers may not be interested in translating these to their individual situations. The focus of most individual employers is to maintain the profitability of their businesses, especially in difficult economic climates. While demonstrating the worth of a public health or medical intervention to society may appeal to the altruism of some employers, demonstrating the potential positive impact of an intervention on a business's profit and loss statements may be an easier argument to make.
Rather than make decisions, computational models provide information to help employers make decisions with respect to their own set of unique circumstances. In the end, people—not computational models—make decisions, but models can help elucidate relationships, factors, and effects that are not readily apparent and provide rough benchmarks. Employers can then adapt model findings accordingly and implement appropriately tailored solutions.
Limitations
All computational simulation models simplify real life situations and cannot completely represent every possible event and outcome that may result from vaccination or influenza. Data inputs for our model came from different studies with varying sample sizes and quality of design. Our model used distributions of parameters and may not fully reflect the socio-demographic, operational, and financial heterogeneity of an individual workplace.
By design, our model remained conservative about the benefits of employer-sponsored vaccination. It did not include a number of additional costs that could arise from influenza infection. First, we assumed employees to be otherwise healthy individuals who did not suffer extended work absences (more than one work week) or substantial absenteeism due to hospitalization for influenza; additionally, the productivity loss attributable to presenteeism (in the case of an ill employee who continues to work), including any time lost for an outpatient medical visit, was not accounted for. Second, our model did not address how the appearance of influenza, especially pandemic influenza, in a workplace may affect the productivity or attendance of healthy individuals and fears of infection may keep employees from showing up to work or impact productivity.[41-42] Third, the model assumed that employers would not bear any costs of treating influenza and its symptoms (e.g., over-the-counter medications, tissues, and insurance premiums) when employers may bear these costs. This is especially true of employers who contract with occupational physicians or maintain workplace health clinics.[43] To remain conservative about the benefits of vaccination, we only accounted for cases that could be generated directly by an employee becoming infected. In actuality, an infected employee could generate a cascade of cases (i.e., the employees whom he or she infected could in turn infect others). However, the number of resulting cases could vary substantially by different mixing patterns and vaccination coverage (employees could have been vaccinated outside the workplace). Preventing this cascade of cases would only add to the value of employee vaccination.
Not all workplaces will have the resources (e.g. computer equipment, meeting space, language translation services and funding) to implement more complex education programs utilizing computer- or internet-based content. Therefore, we chose freely available (on-line) content for our educational materials. However, individual employers may elect to incorporate different, more expensive educational programs, including print materials or sessions with health educators. When deciding whether to sponsor a workplace vaccination campaign, employers should review their individual company's financial circumstances, and how the amount of funding available compares to the cost of implementing a workplace vaccination program. The cost of vaccine and administration/disposal supplies, and healthcare worker wages may vary depending on the vaccine presentation (e.g., TIV and/or LAIV) offered and affect the overall cost of a program.
Salaries are an imperfect proxy for employee productivity; pay is not necessarily commensurate with an employee's worth to a firm and may underestimate the full value of an employee's time to the employer. Certain key personnel, especially those with supervisory roles or pivotal technical skills, may influence the productivity of many other employees. Employees that interface regularly with clients or other outside individuals (e.g., teachers with students, health care workers with patients, salespeople with customers, and restaurant personnel with diners) may have a great impact on the firm's return business and revenues. Model input parameters, such as attack rate and R, are not available for all 22 of the major occupational groups included in our analyses, which may limit our ability to fully capture workplace dynamics. The results of sensitivity analyses, including those for attack rate and R across a range of occupational groups, may be referenced as benchmarks for settings in which these parameters are known.
Conclusions
Implementing workplace seasonal or pandemic influenza vaccination appears to be relatively inexpensive and potentially cost-saving for a wide variety of employers in diverse industries. Because employees comprise a large proportion of the overall population and spend a substantial amount of time at work, employer decisions may be important for overall influenza control. While demonstrating the worth of an influenza vaccination to society may appeal to the altruism of some employers, demonstrating the potential positive impact of vaccination on a business's profit and loss statements provides relevance to individual employers who seek to maintain their firm's profitability throughout the influenza season. Individual employers could compare their prevailing conditions with the benchmarks in our model to help determine their optimal local vaccination strategies.
Acknowledgements
Supported by the National Institute of General Medical Sciences Models of Infectious Disease Agent Study (MIDAS) through grant 1U54GM088491-0109. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.U.S. Bureau of Labor Statistics Division of Labor Force Statistics . Current Population Survey: Employment status of the civilian noninstitutional population by age, sex, and race. Washington, D.C.: 2009. [Google Scholar]
- 2.Keech M, Beardsworth P. The impact of influenza on working days lost: a review of the literature. Pharmacoeconomics. 2008;26(11):911–24. doi: 10.2165/00019053-200826110-00004. [DOI] [PubMed] [Google Scholar]
- 3.Watkins RE, Cooke FC, Donovan RJ, Macintyre CR, Itzwerth R, Plant AJ. Tackle the problem when it gets here: pandemic preparedness among small and medium businesses. Qual Health Res. 2008 Jul;18(7):902–12. doi: 10.1177/1049732308318032. [DOI] [PubMed] [Google Scholar]
- 4.Mossong J, Hens N, Jit M, Beutels P, Auranen K, Mikolajczyk R, et al. Social contacts and mixing patterns relevant to the spread of infectious diseases. PLoS Med. 2008 Mar 25;5(3):e74. doi: 10.1371/journal.pmed.0050074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Edmunds WJ, O'Callaghan CJ, Nokes DJ. Who mixes with whom? A method to determine the contact patterns of adults that may lead to the spread of airborne infections. Proc Biol Sci. 1997 Jul 22;264(1384):949–57. doi: 10.1098/rspb.1997.0131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hens N, Goeyvaerts N, Aerts M, Shkedy Z, Van Damme P, Beutels P. Mining social mixing patterns for infectious disease models based on a two-day population survey in Belgium. BMC Infect Dis. 2009;9:5. doi: 10.1186/1471-2334-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Akazawa M, Sindelar JL, Paltiel AD. Economic costs of influenza-related work absenteeism. Value Health. 2003 Mar-Apr;6(2):107–15. doi: 10.1046/j.1524-4733.2003.00209.x. [DOI] [PubMed] [Google Scholar]
- 8.O'Reilly FW, Stevens AB. Sickness absence due to influenza. Occup Med (Lond) 2002 Aug;52(5):265–9. doi: 10.1093/occmed/52.5.265. [DOI] [PubMed] [Google Scholar]
- 9.U.S. Occupational Safety and Health Administration . Guidance on Preparing Workplaces for an Influenza Pandemic. U.S. Department of Labor; Washington, D.C.: 2009. [Google Scholar]
- 10.U.S. Centers for Disease Control and Prevention . Guidance for Businesses and Employers to Plan and Respond to the 2009-2010 Influenza Season. U.S. Department of Health and Human Services; Atlanta, GA: 2009. [Google Scholar]
- 11.Advisory Committee for Immunization Practices ACIP Provisional Recommendations for the Use of Influenza Vaccines. 2010 [cited 2010 June 23]; Available from: http://www.cdc.gov/vaccines/recs/provisional/downloads/flu-vac-mar-2010-508.pdf.
- 12.U.S. Centers for Disease Control and Prevention Seasonal Influenza (Flu) 2010 [cited 2010 April 7]; Available from: http://www.cdc.gov/flu/
- 13.Self-reported influenza vaccination coverage trends 1989 - 2008 among adults by age group, risk group, race/ethnicity, health-care worker status, and pregnancy status, United States, National Health Interview Survey (NHIS) Atlanta, GA: 2009. [Google Scholar]
- 14.Lee BY, Mehrotra A, Burns RM, Harris KM. Alternative vaccination locations: who uses them and can they increase flu vaccination rates? Vaccine. 2009 Jul 9;27(32):4252–6. doi: 10.1016/j.vaccine.2009.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Strunk C. Innovative workplace influenza program: boosting employee immunization rates. AAOHN J. 2005 Oct;53(10):432–7. [PubMed] [Google Scholar]
- 16.Lester RT, McGeer A, Tomlinson G, Detsky AS. Use of, effectiveness of, and attitudes regarding influenza vaccine among house staff. Infect Control Hosp Epidemiol. 2003 Nov;24(11):839–44. doi: 10.1086/502146. [DOI] [PubMed] [Google Scholar]
- 17.Singleton JA, Poel AJ, Lu PJ, Nichol KL, Iwane MK. Where adults reported receiving influenza vaccination in the United States. Am J Infect Control. 2005 Dec;33(10):563–70. doi: 10.1016/j.ajic.2005.03.016. [DOI] [PubMed] [Google Scholar]
- 18.Campbell DS, Rumley MH. Cost-effectiveness of the influenza vaccine in a healthy, working-age population. J Occup Environ Med. 1997 May;39(5):408–14. doi: 10.1097/00043764-199705000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Rothberg MB, Rose DN. Vaccination versus treatment of influenza in working adults: a cost-effectiveness analysis. Am J Med. 2005 Jan;118(1):68–77. doi: 10.1016/j.amjmed.2004.03.044. [DOI] [PubMed] [Google Scholar]
- 20.Bridges CB, Thompson WW, Meltzer MI, Reeve GR, Talamonti WJ, Cox NJ, et al. Effectiveness and cost-benefit of influenza vaccination of healthy working adults: A randomized controlled trial. JAMA. 2000 Oct 4;284(13):1655–63. doi: 10.1001/jama.284.13.1655. [DOI] [PubMed] [Google Scholar]
- 21.Nichol KL, Lind A, Margolis KL, Murdoch M, McFadden R, Hauge M, et al. The effectiveness of vaccination against influenza in healthy, working adults. N Engl J Med. 1995 Oct 5;333(14):889–93. doi: 10.1056/NEJM199510053331401. [DOI] [PubMed] [Google Scholar]
- 22.Olsen GW, Steinberg ME, Ley CA. Worksite influenza immunization programs. Insight into the implementation and cost-benefit. AAOHN J. 2005 Mar;53(3):105–10. [PubMed] [Google Scholar]
- 23.Mixeu MA, Vespa GN, Forleo-Neto E, Toniolo-Neto J, Alves PM. Impact of influenza vaccination on civilian aircrew illness and absenteeism. Aviat Space Environ Med. 2002 Sep;73(9):876–80. [PubMed] [Google Scholar]
- 24.Nichol KL, D'Heilly SJ, Greenberg ME, Ehlinger E. Burden of influenza-like illness and effectiveness of influenza vaccination among working adults aged 50-64 years. Clin Infect Dis. 2009 Feb 1;48(3):292–8. doi: 10.1086/595842. [DOI] [PubMed] [Google Scholar]
- 25.Burckel E, Ashraf T, de Sousa Filho JP, Forleo Neto E, Guarino H, Yauti C, et al. Economic impact of providing workplace influenza vaccination. A model and case study application at a Brazilian pharma-chemical company. Pharmacoeconomics. 1999 Nov;16(5 Pt 2):563–76. doi: 10.2165/00019053-199916050-00012. [DOI] [PubMed] [Google Scholar]
- 26.Samad AH, Usul MH, Zakaria D, Ismail R, Tasset-Tisseau A, Baron-Papillon F, et al. Workplace vaccination against influenza in Malaysia: does the employer benefit? J Occup Health. 2006 Jan;48(1):1–10. doi: 10.1539/joh.48.1. [DOI] [PubMed] [Google Scholar]
- 27.Morales A, Martinez MM, Tasset-Tisseau A, Rey E, Baron-Papillon F, Follet A. Costs and benefits of influenza vaccination and work productivity in a Colombian company from the employer's perspective. Value Health. 2004 Jul-Aug;7(4):433–41. doi: 10.1111/j.1524-4733.2004.74006.x. [DOI] [PubMed] [Google Scholar]
- 28.UC Berkeley School of Public Health Center for Infectious Disease Preparedness Concepts for the Prevention and Control of Microbial Threats - 2. 2006 [cited 2010 April 18]; Available from: http://www.idready.org/slides/01epiconceptsII-notes.pdf.
- 29.Panagiotopoulos T. Herd Immunity and Vaccination. [cited 2010 April 18]; Available from: http://www.pitt.edu/~super1/lecture/lec1181/001.htm.
- 30.U.S. Department of Health and Human Services FLU.GOV. 2010 doi: 10.3109/15360288.2015.1037530. [cited 2010 April 7]; Available from: http://www.flu.gov. [DOI] [PubMed]
- 31.Ling LM, Chow AL, Lye DC, Tan AS, Krishnan P, Cui L, et al. Effects of early oseltamivir therapy on viral shedding in 2009 pandemic influenza A (H1N1) virus infection. Clin Infect Dis. 2010 Apr 1;50(7):963–9. doi: 10.1086/651083. [DOI] [PubMed] [Google Scholar]
- 32.Patrozou E, Mermel LA. Does influenza transmission occur from asymptomatic infection or prior to symptom onset? Public Health Rep. 2009 Mar-Apr;124(2):193–6. doi: 10.1177/003335490912400205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lau LL, Cowling BJ, Fang VJ, Chan KH, Lau EH, Lipsitch M, et al. Viral shedding and clinical illness in naturally acquired influenza virus infections. J Infect Dis. 2010 May 15;201(10):1509–16. doi: 10.1086/652241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carrat F, Vergu E, Ferguson NM, Lemaitre M, Cauchemez S, Leach S, et al. Time lines of infection and disease in human influenza: a review of volunteer challenge studies. Am J Epidemiol. 2008 Apr 1;167(7):775–85. doi: 10.1093/aje/kwm375. [DOI] [PubMed] [Google Scholar]
- 35.U.S. Bureau of Labor Statistics . Employee Tenure in 2008. U.S. Department of Labor; Washington, D.C.: 2008. (Report No.: USDL 08-1344). [Google Scholar]
- 36.May 2008 OES Estimates Occupational Employment Statistics (OES) Survey: Bureau of Labor Statistics, Department of Labor. 2008 [Google Scholar]
- 37.MedImmune I. HIGHLIGHTS OF PRESCRIBING INFORMATION: FluMist® Influenza Vaccine Live, Intranasal. Gaithersburg, MD: 2009. [Google Scholar]
- 38.Smith PW, Hansen K, Spanbauer L, Shell DF. Pandemic influenza preparedness: a survey of businesses. Am J Infect Control. 2007 Sep;35(7):484–5. doi: 10.1016/j.ajic.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 39.D'Heilly SJ, Nichol KL. Work-site-based influenza vaccination in healthcare and non-healthcare settings. Infect Control Hosp Epidemiol. 2004 Nov;25(11):941–5. doi: 10.1086/502324. [DOI] [PubMed] [Google Scholar]
- 40.Leighton L, Williams M, Aubery D, Parker SH. Sickness absence following a campaign of vaccination against influenza in the workplace. Occup Med (Lond) 1996 Apr;46(2):146–50. doi: 10.1093/occmed/46.2.146. [DOI] [PubMed] [Google Scholar]
- 41.Blendon RJ, Koonin LM, Benson JM, Cetron MS, Pollard WE, Mitchell EW, et al. Public response to community mitigation measures for pandemic influenza. Emerg Infect Dis. 2008 May;14(5):778–86. doi: 10.3201/eid1405.071437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Keech M, Scott AJ, Ryan PJ. The impact of influenza and influenza-like illness on productivity and healthcare resource utilization in a working population. Occup Med (Lond) 1998 Feb;48(2):85–90. doi: 10.1093/occmed/48.2.85. [DOI] [PubMed] [Google Scholar]
- 43.Schultz AB, Chen CY, Edington DW. The cost and impact of health conditions on presenteeism to employers: a review of the literature. Pharmacoeconomics. 2009;27(5):365–78. doi: 10.2165/00019053-200927050-00002. [DOI] [PubMed] [Google Scholar]
- 44.U.S. Department of Health and Human Services Centers for Disease Control and Prevention Adult Influenza Vaccine Price List. 2010 [cited 2010 April 8]; Available from: http://www.cdc.gov/vaccines/programs/vfc/cdc-vac-price-list.htm#adult.
- 45.CDC Possible Side-effects from Vaccines. 2009 August 11; 2009 [cited 2009 August 17]; Available from: [Google Scholar]
- 46.Molinari NA, Ortega-Sanchez IR, Messonnier ML, Thompson WW, Wortley PM, Weintraub E, et al. The annual impact of seasonal influenza in the US: measuring disease burden and costs. Vaccine. 2007 Jun 28;25(27):5086–96. doi: 10.1016/j.vaccine.2007.03.046. [DOI] [PubMed] [Google Scholar]
- 47.Demicheli V, Rivetti D, Deeks JJ, Jefferson TO. Vaccines for preventing influenza in healthy adults. Cochrane Database Syst Rev. 2004;(3):CD001269. doi: 10.1002/14651858.CD001269.pub2. [DOI] [PubMed] [Google Scholar]
- 48.Ferguson NM, Cummings DA, Fraser C, Cajka JC, Cooley PC, Burke DS. Strategies for mitigating an influenza pandemic. Nature. 2006 Jul 27;442(7101):448–52. doi: 10.1038/nature04795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.LaForce FM, Nichol KL, Cox NJ. Influenza: virology, epidemiology, disease, and prevention. Am J Prev Med. 1994;10(Suppl):31–44. [PubMed] [Google Scholar]