Abstract
Background
Infection is an important cause of hospitalization and death in patients receiving dialysis. Few studies have examined the full range of infections experienced by dialysis patients. The purpose of this study was to examine the types, rates and risk factors for infection among older persons starting dialysis.
Study Design
Retrospective observational cohort study.
Setting and Participants
The cohort was assembled from the United States Renal Data System and included patients aged 65 to 100 years who initiated dialysis between 1/1/00 and 12/31/02. Exclusions included prior kidney transplant, unknown dialysis modality, or death, loss to follow-up, or transplant during the first 90 days of dialysis. Patients were followed until death, transplant, or study end 12/31/04.
Predictors
Baseline demographics, co-morbidities, serum albumin and hemoglobin.
Outcomes and Measurements
Infection-related hospitalizations were ascertained using discharge ICD-9-CM codes. Hospitalization rates were calculated for each type of infection. The Wei-Lin-Weissfeld Model was used to examine risk factors for up to 4 infection-related events.
Results
119,858 patients were included, 7,401 of whom were on peritoneal dialysis. During a median follow-up of 1.9 years, infection-related diagnoses were observed in approximately 35% of all hospitalizations. Approximately 50% of patients had at least one infection-related hospitalization. Rates (per 100 person-years) of pulmonary, soft tissue, and genitourinary infections ranged from 8.3 to 10.3 in patients on peritoneal dialysis and 10.2 to 15.3 in patients on hemodialysis. Risk factors for infection included older age, female sex, diabetes, heart failure, pulmonary disease, and low serum albumin.
Limitations
Use of ICD-9-CM codes, reliance on Medicare claims to capture hospitalizations, use of the Medical Evidence Form to ascertain co-morbidities, absence of data on dialysis access.
Conclusion
Infection-related hospitalization is frequent in older patients on dialysis. A broad range of infections – many unrelated to dialysis access – result in hospitalization in this population.
Keywords: Dialysis, Infection, Epidemiology, Kidney Failure
Infections are a frequent cause of hospitalization in persons with ESRD and the second leading cause of mortality after cardiovascular disease. Although overall hospital admission rates have stabilized in the ESRD population at approximately two hospitalizations per patient per year, the rate of infection-related hospitalizations has increased nearly 26% between 1993 and 2007.1 Among patients 65 years of age and older, the rates of infection-related hospitalizations are nearly as high as the rates of cardiovascular hospitalizations during the first year of hemodialysis.1 Despite the recognition that infections contribute substantially to morbidity and mortality of patients on dialysis, the majority of attention has focused on bacteremia and peritonitis, complications of hemodialysis and peritoneal dialysis access, respectively. Few studies have examined the broad range of infections, and these studies have been limited in part by the inclusion of select groups of patients2 or patients from a single center.3 Furthermore, published studies have not focused on older patients, a subgroup at increased risk for acquiring infection 4-6 and for having adverse outcomes after an infection.7 Between 1996 and 2003, the rate of dialysis initiation in persons aged 80 to 100 years increased by more than 50%; 8 as of 2007, the median age of incident dialysis patients was 64 years.1 We therefore examined the types, rates, and risk factors for infection-related hospitalizations and deaths in a cohort of incident hemodialysis and peritoneal dialysis patients aged 65 years or older. We hypothesized that older age, diabetes, and low serum albumin would be key predictors of infection in older patients on dialysis.
Methods
Patient Population
We performed a retrospective cohort study of incident dialysis patients who initiated hemodialysis or peritoneal dialysis between January 1, 2000 and December 31, 2002 and had no prior history of kidney transplant. The cohort was assembled from the United States Renal Data System (USRDS) and included patients between 65 and 100 years of age at the time of dialysis initiation and who survived, were not lost to follow-up, or transplanted during the first 90 days of dialysis. Patients with prior kidney transplants were excluded to avoid capturing transplant-related infections and because of possible ongoing immunosuppression, which would increase the risk of infection. Patients whose dialysis modality was unknown were also excluded because we had planned a priori to stratify analyses by modality of dialysis. We followed the cohort until death, kidney transplant, or study end on December 31, 2004.
The study was approved by the Committee on Human Research at the University of California, San Francisco and the Clinical Research Subcommittee of the Research and Development Committee at the San Francisco VA Medical Center. The research met the requirements to waive informed consent.
Data Source and Data Collection
The USRDS is a national database (capturing >99% of persons receiving maintenance dialysis in the US) that contains data on demographics, dialysis modality, prevalent medical conditions and biochemical studies at the time of dialysis initiation, along with follow-up that includes inpatient hospitalizations submitted to Medicare for reimbursement, transplantation status, and death.9 Demographics, co-existing medical illnesses, etiology of kidney failure, baseline laboratory studies, dialysis modality (after day 90 of dialysis) and cause of death were collected from the Patient Profile, Medical Evidence Form, and Prescription History Standard Analytic Files. The Transplant Standard Analytic File was used to determine the date of first transplant, if applicable. Infection-related hospitalizations were identified by examining the Hospitalization Standard Analytic File.
Infection-related hospitalizations were examined after the first 90 days of dialysis to maximize the number of patients with Medicare as the primary payer and minimize the number of patients changing dialysis modality (as a large percent of patients change dialysis modality in the first 90 days of dialysis). Infection-related hospitalizations of interest included hospitalizations for septicemia, bacteremia, endocarditis, pulmonary infections (e.g., viral pneumonia, bacterial pneumonia, influenza with respiratory manifestations, abscess of lung or mediastinum), genitourinary infections (e.g., urinary tract infection, pyelonephritis, peri-nephric abscess), gastrointestinal infections (e.g., diverticulitis, C difficile colitis, peri-rectal abscess, cholecystitis), peritonitis, soft tissue infections (e.g., cellulitis, necrotizing fascitis, gangrene), and joint or bone infections (e.g., infective arthritis, osteomyelitis). Infection-related hospitalizations were coded using International Classification of Disease 9th revision Clinical Modification (ICD-9-CM) discharge diagnosis codes 10 (Item S1, available as online supplementary material associated with this article at www.ajkd.org). We examined all discharge diagnoses for each hospitalization, and participants were classified as having an infection-related hospitalization if any of the discharge diagnoses included an infection of interest. Therefore, we defined infection-related hospitalizations as those hospitalizations for which infection was either the primary reason for hospitalization or was a secondary complication of hospitalization.
Death was classified as infection-related if the listed cause(s) of death included: pulmonary infection (bacterial, fungal, or other), septicemia (due to vascular access, peripheral vascular disease, gangrene, or other), peritonitis (septicemia due to peritonitis, fungal), infection, viral infection (hepatitis B, viral hepatitis, other viral hepatitis or other), AIDS, or tuberculosis (Item S1).
Statistical Analysis
Because of large expected differences in baseline characteristics between patients initiated on hemodialysis and those initiated on peritoneal dialysis and because the different modalities may predispose to different infections, we analyzed these groups separately. We compared baseline patient characteristics with respect to dialysis modality using mean and standard deviations for continuous variables and proportions for categorical variables.
We examined the number of infection-related hospitalizations per patient and the number of infection-related diagnoses per hospitalization. Multiple infection-related diagnoses per hospitalization were captured for each patient, and all hospitalizations during follow-up were examined for infection-related diagnoses. To calculate the rates of each type of infection (e.g., pulmonary, genitourinary, gastrointestinal, etc.), the number of hospitalizations within a specific infection category were divided by the total person-time of follow-up.
We examined the overall rates of infection-related hospitalization during follow-up. To examine whether rates differed over time, we further examined the rates of infection-related hospitalizations in three month intervals. Risk factors associated with up to four infection-related events per patient (event defined as infection-related hospitalization or death) were evaluated using an extension of the Cox Proportional Hazards Model, the Wei-Lin-Weissfeld Model.11 The Wei-Lin-Weissfeld model was selected as opposed to other models for repeated hospitalizations (e.g., Anderson-Gill or Prentice, Williams, and Peterson) to focus on the overall average risk associated with baseline demographics, co-morbidities and biochemical measures and to minimize the potential bias introduced by models (e.g., Prentice, Williams, and Peterson) that condition on previous hospitalization and result in progressively smaller risk strata over time or by models (e.g., Anderson-Gill) that assume prior hospitalization does not alter the risk of subsequent hospitalization. Covariates in the multivariable Wei-Lin-Weissfeld model were determined a priori and included: age, gender, race (white, black, Asian or other), and history of diabetes, hypertension, heart failure, ischemic heart disease, pulmonary disease, cancer, or inability to ambulate or transfer, and baseline serum albumin and hemoglobin concentrations. If a patient did not have a documented serum albumin concentration (27%) or hemoglobin concentration or hematocrit (5%), then these variables were classified into a missing category, which was included in the final model. If a patient’s race was unknown (0.03%), then race was classified as other. In the Wei-Lin-Weissfeld models, patients were censored at the time of transplant, death not related to infection, or study end. To test the proportional hazards assumption, we examined correlations of Schoenfeld residuals with time functions. Because dialysis modality was not updated during follow-up, a sensitivity analysis, where patients were censored at the time of dialysis modality change, was performed to examine whether risk estimates changed substantially. All analyses were conducted using SAS 9.2 statistical software (www.sas.com).
Results
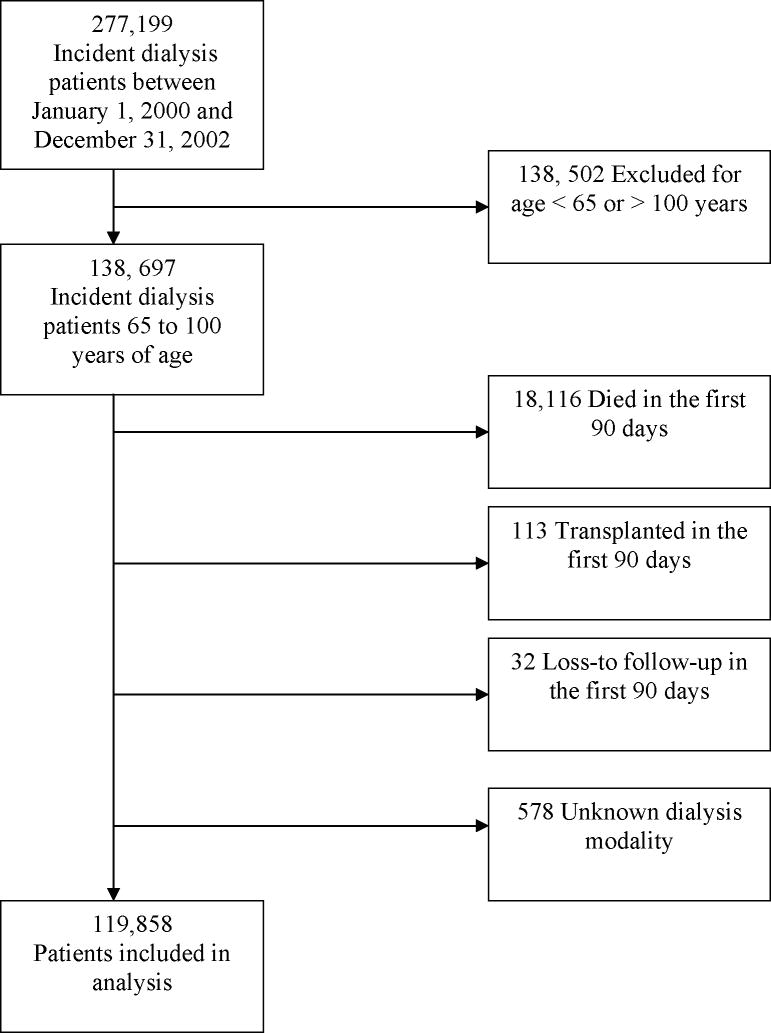
After exclusions, a total of 119,858 incident dialysis patients were included in the cohort, of whom 7,401 patients were on peritoneal dialysis (Figure 1). As described in other cohorts, patients on peritoneal dialysis tended to be younger and were more likely to be white and male (Table 1). The median follow-up time was 1.9 years. Infection-related diagnoses were observed in 34 and 36% of all hospitalizations in patients on hemodialysis and peritoneal dialysis, respectively.
Figure 1.
Cohort Selection. Number of older patients newly starting dialysis between January 1, 2000 and December 31, 2002 included in the study after exclusions.
Table 1.
Baseline Characteristics of Older Patients on Dialysis
| Hemodialysis (n=112,457) | Peritoneal Dialysis (n=7,401) | |
|---|---|---|
| Age, mean years ± sd | 75.3 ± 6.5 | 73.6 ± 6.0 |
| Male, n (%) | 57,567 (51) | 4,156 (56) |
| Race, n (%) | ||
| Asian | 4,045 (4) | 290 (4) |
| Black | 25,756 (23) | 895 (12) |
| White | 80,532 (72) | 6,093 (82) |
| Other | 2,124 (2) | 123 (2) |
| Etiology of Kidney Disease n (%) | ||
| Diabetes | 49,501 (44) | 3,202 (43) |
| Hypertension | 38,622 (34) | 2,361 (32) |
| Glomerulonephritis | 6,661 (6) | 699 (9) |
| Cystic kidney disease | 1,300 (1) | 163 (2) |
| Urologic | 3,321 (3) | 216 (3) |
| Other | 13,052 (12) | 760 (10) |
| Comorbid Conditions | ||
| Diabetes, n (%) | 61,543 (55) | 3,855 (52) |
| Hypertension, n (%) | 89,523 (80) | 6,026 (81) |
| Ischemic Heart Disease, n (%) | 37,682 (34) | 2,336 (32) |
| COPD, n (%) | 11,336 (10) | 561 (8) |
| Heart Failure, n (%) | 44,419 (40) | 2,360 (32) |
| Cancer, n (%) | 9,275 (8) | 525 (7) |
| Inability to Ambulate or Transfer, n (%) | 5,202 (5) | 115 (2) |
| Laboratory values | ||
| Serum Albumin, mean g/dl ± sd | 3.1 ± 0.6 | 3.5 ± 0.6 |
| Hemoglobin, mean g/dl± sd | 10.0 ± 1.7 | 10.6 ± 1.8 |
| MDRD eGFR,* mean ml/min/1.73m2 | 10.1 ± 5.2 | 10.6 ± 5.3 |
Modification in Diet and Renal Disease estimated Glomerular Filtration Rate
Note: Values shown are mean +/- SD or no. (%). Conversion factor for units: serum albumin and hemoglobin in g/dl to g/l, x10; eGFR in ml/min/1.73m2 to ml/s/1.73m2, x0.01667.
Abbreviations: COPD, Chronic Obstructive Pulmonary Disease; eGFR, estimated glomerular filtration rate; MDRD, Modification of Diet in Renal Disease.
Approximately 50% of patients on hemodialysis and peritoneal dialysis had at least one infection-related hospitalization (i.e., one or more infection-related discharge diagnosis). Approximately 25% had one infection-related hospitalization, and approximately 25% had two or more infection-related hospitalizations (Figure 2). Among patients with infection-related hospitalizations, only one infectious diagnosis was coded for most hospitalizations (Figure 3).
Figure 2.
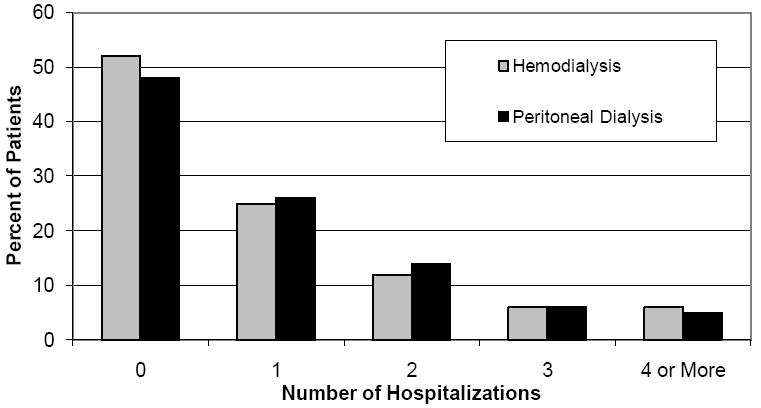
Distribution of the Number of Infection-Related Hospitalizations. Proportion of patients on hemodialysis or peritoneal dialysis with 0, 1, 2, 3, or 4 or more hospitalizations for infection during follow-up.
Figure 3.
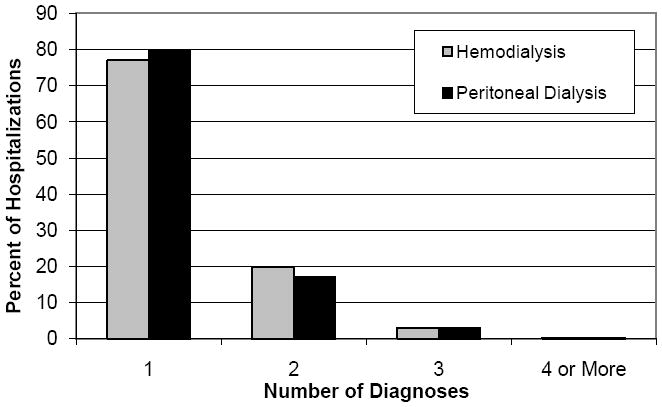
Distribution of the Number of Infection Diagnoses per Infection-Related Hospitalization. Proportion of patients on hemodialysis or peritoneal dialysis with 1, 2, 3, or 4 or more infection specific diagnoses during a hospitalization for infection.
We identified a wide range of infections including sepsis, pulmonary, genitourinary, gastrointestinal, and soft tissue infections. As expected, patients on peritoneal dialysis had higher rates of peritonitis, whereas patients on hemodialysis had higher rates of bacteremia. Among patients on hemodialysis at the beginning of the study, the rates (per 100 person-years) of specific infection-related hospitalizations were: 17.6 for septicemia, 15.3 for pulmonary, 3.7 for gastrointestinal, 12.3 for genitourinary and 10.2 for soft-tissue infection. Among peritoneal dialysis patients, the rate of specific infection-related hospitalizations (per 100 person-years) was: 10.6 for septicemia, 10.3 for pulmonary, 4.7 for gastrointestinal, 8.3 for genitourinary and 8.8 for soft-tissue infections (Figure 4). Thus, there was a substantial burden of non-access related infection in both groups.
Figure 4.
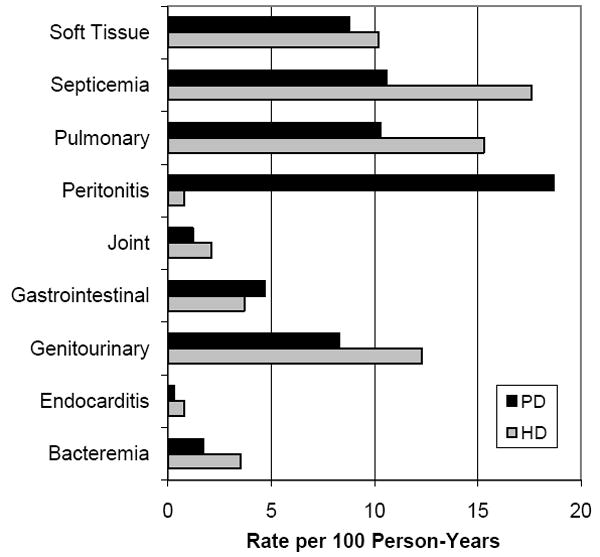
Types and Rates of Infection-Related Hospitalizations. The rates (per 100 person-years) of specific types of infections observed in patients receiving hemodialysis or peritoneal dialysis.
During follow-up, patients on hemodialysis experienced 109,792 infection-related hospitalizations (overall rate of 53 per 100 person-years) and patients on peritoneal dialysis experienced 7,404 infection-related hospitalizations (overall rate of 52 per 100 person-years). Among patients on hemodialysis, the rate of infection-related hospitalizations (per 100 person-years) was 66 for the first three months, 54 to 58 for months three through twelve, and then 52 to 53 for months twelve through twenty-four of follow-up. Among patients on peritoneal dialysis, the rate of infection-related hospitalizations (per 100 person-years) was 50 to 54 for the first nine months of follow-up and 55 to 61 for months nine through twenty-four of follow-up. During follow-up, 64 percent of patients died. Among patients who died, infection was the primary cause of death in 13% and was a contributing cause of death in an additional 5%.
In the multivariable Wei-Lin-Weissfeld models, risk factors were similar among patients on hemodialysis and peritoneal dialysis. Factors associated with a 10% or more increased risk of infection-related events for both modalities included: older age (age ≥ 75 as compared with age 65-< 75 years), female sex, diabetes, heart failure, pulmonary disease, and lower serum albumin (albumin < 3.5 as compared to ≥ 4 g/dl). The inability to ambulate or transfer was associated with a nearly 60% increase in risk of infection-related event in patients on hemodialysis whereas in patients on peritoneal dialysis a 26% increase in risk was observed, however, this was not statistically significant (p-value 0.1). Among patients on peritoneal dialysis, ischemic heart disease and cancer were additionally associated with a more than 10% increased risk of infection. The relation between hemoglobin and risk of infection was non-monotonic. Asian race was associated with a lower risk of infection-related events as compared with white race (Table 2).
Table 2.
Multivariable Models of Factors Associated with the Risk of Infection-Related Events in Patients on Hemodialysis and Peritoneal Dialysis†
| Hemodialysis | Peritoneal Dialysis | |||
|---|---|---|---|---|
| HR | (95% CI) | HR | (95% CI) | |
| Age, years | ||||
| 65 to < 75 | 1.00 | (ref) | 1.00 | (ref) |
| 75 to < 85 | 1.16 | (1.14, 1.18) | 1.11 | (1.03, 1.20) |
| ≥ 85 | 1.46 | (1.41, 1.51) | 1.36 | (1.12, 1.65) |
| Female | 1.18 | (1.15, 1.20) | 1.24 | (1.15, 1.33) |
| Race | ||||
| White | 1.00 | (ref) | 1.00 | (ref) |
| Black | 0.94 | (0.92, 0.96) | 0.96 | (0.86, 1.07) |
| Asian | 0.59 | (0.56, 0.63) | 0.60 | (0.49, 0.74) |
| Other | 0.98 | (0.91, 1.05) | 0.95 | (0.72, 1.26) |
| Comorbid Conditions | ||||
| Diabetes | 1.29 | (1.27, 1.32) | 1.45 | (1.34, 1.56) |
| Heart Failure | 1.23 | (1.20, 1.25) | 1.29 | (1.19, 1.40) |
| Hypertension | 0.88 | (0.86, 0.90) | 1.01 | (0.92, 1.11) |
| Ischemic Heart Disease | 1.08 | (1.06, 1.11) | 1.11 | (1.02, 1.21) |
| Pulmonary Disease | 1.32 | (1.28, 1.36) | 1.34 | (1.17, 1.53) |
| Cancer | 1.06 | (1.03, 1.10) | 1.21 | (1.05, 1.39) |
| Inability to Ambulate or Transfer | 1.58 | (1.52, 1.66) | 1.26 | (0.94, 1.68) |
| Albumin, g/dl | ||||
| < 2.5 | 1.53 | (1.46, 1.61) | 1.45 | (1.19, 1.77) |
| 2.5 to < 3.0 | 1.39 | (1.33, 1.45) | 1.46 | (1.27, 1.68) |
| 3.0 to < 3.5 | 1.25 | (1.20, 1.31) | 1.27 | (1.13, 1.43) |
| 3.5 to < 4.0 | 1.09 | (1.04, 1.14) | 1.12 | (0.99, 1.25) |
| ≥ 4 | 1.00 | (ref) | 1.00 | (ref) |
| Missing | 1.30 | (1.25, 1.36) | 1.24 | (1.10, 1.40) |
| Hemoglobin, g/dl | ||||
| < 8 | 1.01 | (0.97, 1.04) | 1.17 | (0.99, 1.37) |
| 8 to < 10 | 1.05 | (1.02, 1.07) | 1.15 | (1.06, 1.25) |
| 10 to < 12 | 1.00 | (ref) | 1.00 | (ref) |
| 12 to < 14 | 0.95 | (0.92, 0.99) | 0.97 | (0.87, 1.08) |
| ≥ 14 | 0.99 | (0.91, 1.07) | 0.87 | (0.68, 1.10) |
| Missing | 0.99 | (0.95, 1.04) | 1.10 | (0.92, 1.32) |
Adjusted for all listed variables
Note: Conversion factor for units: serum albumin and hemoglobin in g/dl to g/l, x10.
Abbreviations: CI, confidence interval; HR, hazard ratio; ref, reference
In the sensitivity analysis allowing patients to be censored at the time of dialysis modality change, material changes in risk estimates were observed only among peritoneal dialysis patients and only for select predictors. Censoring at the time of modality change resulted in several predictors being associated with an increased risk of infection-related event; inability to ambulate or transfer was associated with a 42% increase in risk (HR, 1.42 [95% CI, 1.04-1.94]), compared to a 26% increase (HR, 1.26 [95% CI, 0.94-1.68]) in the primary model, age ≥ 85 (as compared to age 65-< 75) was associated with a 46% increase in risk (HR, 1.46 [95% CI, 1.20-1.78]) compared to 36% in the primary model (HR, 1.36 [95% CI, 1.12-1.65]) and albumin < 2.5 g/dl (as compared to an albumin ≥ 4 g/dl) was associated with a 56% increase in risk (HR, 1.56 [95% CI, 1.26-1.93]) of infection-related event as compared to 45% in the primary model (HR, 1.45 [95% CI, 1.19-1.77]). Otherwise, censoring at the time of dialysis modality change did not result in a significant alteration of risk estimates.
Discussion
In our study of older patients new to dialysis, we found that infection-related hospitalization (i.e., hospitalization primarily for infection or complicated by infection) occurred frequently. Importantly, one-half of patients aged 65 years or older had at least one infection-related hospitalization during a median follow-up of nearly two years. Among patients on hemodialysis, rates of infection-related hospitalization were highest early in the course of dialysis whereas patients on peritoneal dialysis were observed to have higher rates of infection later in their course. Furthermore, high rates of specific non-access related infections (e.g., pulmonary, soft tissue, and genitourinary) were observed among patients treated with both dialysis modalities. Our findings reinforce the importance of understanding that patients on dialysis experience a high burden of infection-related complications beyond those related to dialysis access and highlight that older dialysis patients are at high risk for acquiring a number of serious infections.
Few studies have examined the total burden of infections in dialysis patients and these studies have been limited by the inclusion of selected patient populations and the lack of delineation of specific types and rates of infection. In the Hemodialysis (HEMO) Study, the investigators found that a spectrum of infections contributed to infection-related hospitalizations.2 The rates of specific infections in our study are not directly comparable to those in the HEMO Study due in part to differences in the classification of infections. In addition, findings from the HEMO study may be less generalizable, as the participants were younger, more likely to be African American and had a low prevalence of catheters for vascular access as compared with the general hemodialysis population.2 Our findings expand on those of the HEMO Study, as we examined an unselected population of older hemodialysis (and peritoneal dialysis) patients.
Chavers et al. examined rates of infection-related hospitalizations, defined as any hospitalization in which infection was the principal diagnosis, in incident pediatric and adult patients with ESRD. These authors found that the 36-month cumulative incidence of infection-related hospitalizations was 53% and 52% in patients on hemodialysis and peritoneal dialysis, respectively. 12 We examined principal and secondary diagnoses, and delineated the specific types of infections contributing to the observed high rates of hospitalization.
We identified older age, female sex, diabetes, heart failure, pulmonary disease, and lower serum albumin as clinically important (i.e., relative increase in risk of 10% or more) risk factors for infection-related events in patients on hemodialysis or peritoneal dialysis. Inability to ambulate or transfer was a particularly important risk factor for infection among patients on hemodialysis. Cancer and ischemic heart disease were also associated with an increased risk of infection although the strength of association was notably higher in patients on peritoneal dialysis. Older age,4, 6 diabetes, 2, 3, 5, 6 heart failure, 4, 5 pulmonary disease,4, 5 inability to ambulate or transfer,4, 5 low serum albumin,2-5, 13 and cancer 4, 5 have been associated with an increased risk of specific or overall infections in previous studies of patients on dialysis. Most studies have not found a difference in the risk of infection by sex.2, 3, 5, 6 A possible explanation for the importance of sex in our analysis is the inclusion of genitourinary infections, which may be more likely to occur in women. Very low serum albumin concentrations (i.e., albumin less than 2.5 g/dl) were associated with a marked risk of infection-related events in patients on hemodialysis or peritoneal dialysis. Although hypoalbuminemia could be a consequence rather than a cause of infection, we believe that the observed association between albumin and infection is not completely explained by reverse causality, because we examined up to four infection-related events in relation to baseline measures of albumin; thus our results suggest that baseline albumin measures are an important marker for long-term infection risk. Interestingly, Asian race was associated with a substantial decrease in the risk of infection, a finding observed in other USRDS studies.4, 5 Differences in risk and outcomes of infection have not been extensively studied in the Asian dialysis population; it is unclear whether these findings represent differences in risks or consequences of infection in Asian patients, or confounding by hospitalization practices in different US regions (the majority of Asian patients on dialysis in the US reside in the west coast and the west coast has lower rates of hospitalization).
Our study had several strengths. First, we examined a large cohort of older patients on dialysis, a group of dialysis patients who differ from the general dialysis population in their baseline risk and outcome following infection. Older (age 65 years and older) patients currently constitute nearly half of the dialysis population and require specific study due to differences in the prevalence of co-morbid illnesses and disease outcomes. Second, we examined numerous types of infection to understand better the true burden of infectious disease in this population and describe the specific types, rates and risk factors for infections observed in older dialysis patients. Finally, our analysis using the Wei-Lin-Weissfeld approach accounted for multiple hospitalizations rather than examining time to first infection-related hospitalization. Complications involving repeated infections frequently portend an inexorable decline toward debility and ultimately death in persons with chronic disease; analyses ignoring repeat hospitalizations would not capture the full spectrum or magnitude of risk factors for these outcomes. Even within a relatively short follow-up period, an estimated one in four patients were hospitalized repeatedly for infection.
Our study also had several limitations. First, we used ICD-9-CM codes to identify infections, rather than validated clinical criteria for each infectious disease-related diagnosis because the size of the study population and data source prohibited individual chart review. Although this may have resulted in some misclassification of infections, our findings should accurately reflect the clinicians’ diagnoses at discharge and provide an overview of infection types in this population, serving as an initial framework for further study of this complex field. Second, we did not update dialysis modality during follow-up and instead examined patients with respect to their dialysis modality after the first 90 days of dialysis. Therefore, the findings of our study relate to dialysis modality early in the course of dialysis, and some of the observed infections in each dialysis modality may have occurred after transitioning to another dialysis modality. However, this misclassification of modality would be expected to obscure rather than enhance any modality-related differences in types and rates of infection. Furthermore, in our sensitivity analysis where patients were censored at the time of modality change, we found that in general the risk estimates remained overall the same or were somewhat higher. Third, we relied exclusively on baseline measures of biochemical data, such as serum albumin (because no follow-up laboratory determinations were available); this approach limits the interpretation of the association between serum albumin and risk of infection, likely minimizing the association. Despite our reliance on baseline measures of albumin, an approximately 25 to 50 % increased risk of infection was observed for patients with baseline serum albumin concentrations < 3.5 g/dl. Fourth, baseline co-morbidity data were ascertained from the Medical Evidence Form, which may result in underascertainment of co-morbid illnesses, which could attenuate the magnitude of risk estimates.14 Fifth, we relied on Medicare claims to ascertain infection-related hospitalizations (77% of the patients in our cohort had Medicare as the primary payer at study start). Although patients may have changed to Medicare as the primary payer during follow-up, our findings presumably underestimate the true rate of infection-related hospitalizations. We did not have data on dialysis access type and therefore cannot make inference about the effect of dialysis access type on the risk of infection-related hospitalization. Nonetheless, one of the primary aims of our study was to highlight the burden of non-access-related infections. Finally, we did not examine rates of infection during the first 90 days of dialysis and our findings do not apply to the earliest months of dialysis therapy. Despite these limitations, the USRDS is an important source of dialysis-related research, assisting researchers and clinicians in understanding the clinical course of patients on dialysis, providing the framework for more in-depth patient-oriented studies.
The findings from our study demonstrate that serious infections are a frequent complication in older dialysis patients, and non-access-related infections contribute significantly to hospitalization and death in patients on dialysis. Our findings likely underestimate the number of serious infections in this population, as we relied on Medicare claims to capture inpatient hospitalizations and potentially serious infections can be managed with outpatient intravenous or intraperitoneal antibiotics. The ESRD population continues to grow15 and consists of a large proportion of older patients on dialysis.1, 8 Given the high rates of infection-related hospitalizations and death in older dialysis patients, the associated costs, 16, 17 and the potential cardiovascular consequences of infection in patients on dialysis5, 18 we need to understand better those infectious disease-related-complications that result in significant morbidity and mortality and to develop effective preventive and treatment strategies in this high risk population.
Supplementary Material
Acknowledgments
Support: This publication was made possible by Contract Number N01-DK-7-0005 from the National Institute of Diabetes and Digestive and Kidney Diseases, Grant Number UL1 RR024146 from the National Center for Research for Medical Research, and by the Department of Veterans’ Affairs Research Service.
Footnotes
Part of this work was previously presented as a Poster Presentation at the American Society of Nephrology Renal Week 2008 in Philadelphia, PA. The contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH. The interpretation and reporting of the data presented here are the responsibility of the authors and in no way should be seen as an official policy or interpretation of the United States government.
Financial Disclosure: The authors declare that they have no relevant financial interests.
Supplementary Material Note: The supplementary material accompanying this article (doi:_______) is available at www.ajkd.org.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.U.S. Renal Data System. USRDS 2009 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; Bethesda, MD: 2009. [Google Scholar]
- 2.Allon M, Depner TA, Radeva M, et al. Impact of dialysis dose and membrane on infection-related hospitalization and death: results of the HEMO Study. J Am Soc Nephrol. 2003 Jul;14(7):1863–1870. doi: 10.1097/01.asn.0000074237.78764.d1. [DOI] [PubMed] [Google Scholar]
- 3.Aslam N, Bernardini J, Fried L, Burr R, Piraino B. Comparison of infectious complications between incident hemodialysis and peritoneal dialysis patients. Clin J Am Soc Nephrol. 2006 Nov;1(6):1226–1233. doi: 10.2215/CJN.01230406. [DOI] [PubMed] [Google Scholar]
- 4.Guo H, Liu J, Collins AJ, Foley RN. Pneumonia in incident dialysis patients--the United States Renal Data System. Nephrol Dial Transplant. 2008 Feb;23(2):680–686. doi: 10.1093/ndt/gfm474. [DOI] [PubMed] [Google Scholar]
- 5.Foley RN, Guo H, Snyder JJ, Gilbertson DT, Collins AJ. Septicemia in the United States dialysis population, 1991 to 1999. J Am Soc Nephrol. 2004 Apr;15(4):1038–1045. doi: 10.1097/01.asn.0000119144.95922.c4. [DOI] [PubMed] [Google Scholar]
- 6.Powe NR, Jaar B, Furth SL, Hermann J, Briggs W. Septicemia in dialysis patients: incidence, risk factors, and prognosis. Kidney Int. 1999 Mar;55(3):1081–1090. doi: 10.1046/j.1523-1755.1999.0550031081.x. [DOI] [PubMed] [Google Scholar]
- 7.Allon M, Radeva M, Bailey J, et al. The spectrum of infection-related morbidity in hospitalized haemodialysis patients. Nephrol Dial Transplant. 2005 Jun;20(6):1180–1186. doi: 10.1093/ndt/gfh729. [DOI] [PubMed] [Google Scholar]
- 8.Kurella M, Covinsky KE, Collins AJ, Chertow GM. Octogenarians and nonagenarians starting dialysis in the United States. Ann Intern Med. 2007 Feb 6;146(3):177–183. doi: 10.7326/0003-4819-146-3-200702060-00006. [DOI] [PubMed] [Google Scholar]
- 9.United States Renal Data System. Researcher’s Guide to the USRDS Database. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Disease; Bethesda, MD: 2006. [Google Scholar]
- 10.ICD-9-CM Professional for Physicians, Volumes 1 & 2. Ingenix; 2007. [Google Scholar]
- 11.Li QH, Lagakos SW. Use of the Wei-Lin-Weissfeld method for the analysis of a recurring and a terminating event. Stat Med. 1997 Apr 30;16(8):925–940. doi: 10.1002/(sici)1097-0258(19970430)16:8<925::aid-sim545>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 12.Chavers BM, Solid CA, Gilbertson DT, Collins AJ. Infection-related hospitalization rates in pediatric versus adult patients with end-stage renal disease in the United States. J Am Soc Nephrol. 2007 Mar;18(3):952–959. doi: 10.1681/ASN.2006040406. [DOI] [PubMed] [Google Scholar]
- 13.Wang Q, Bernardini J, Piraino B, Fried L. Albumin at the start of peritoneal dialysis predicts the development of peritonitis. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2003;41(3):664–669. doi: 10.1053/ajkd.2003.50128. [DOI] [PubMed] [Google Scholar]
- 14.Longenecker JC, Coresh J, Klag MJ, et al. Validation of comorbid conditions on the end-stage renal disease medical evidence report: the CHOICE study. Choices for Healthy Outcomes in Caring for ESRD. J Am Soc Nephrol. 2000 Mar;11(3):520–529. doi: 10.1681/ASN.V113520. [DOI] [PubMed] [Google Scholar]
- 15.Gilbertson DT, Liu J, Xue JL, et al. Projecting the number of patients with end-stage renal disease in the United States to the year 2015. J Am Soc Nephrol. 2005 Dec;16(12):3736–3741. doi: 10.1681/ASN.2005010112. [DOI] [PubMed] [Google Scholar]
- 16.Engemann JJ, Friedman JY, Reed SD, et al. Clinical outcomes and costs due to Staphylococcus aureus bacteremia among patients receiving long-term hemodialysis. Infect Control Hosp Epidemiol. 2005 Jun;26(6):534–539. doi: 10.1086/502580. [DOI] [PubMed] [Google Scholar]
- 17.Nissenson AR, Dylan ML, Griffiths RI, et al. Clinical and economic outcomes of Staphylococcus aureus septicemia in ESRD patients receiving hemodialysis. Am J Kidney Dis. 2005 Aug;46(2):301–308. doi: 10.1053/j.ajkd.2005.04.019. [DOI] [PubMed] [Google Scholar]
- 18.Ishani A, Collins AJ, Herzog CA, Foley RN. Septicemia, access and cardiovascular disease in dialysis patients: the USRDS Wave 2 study. Kidney Int. 2005 Jul;68(1):311–318. doi: 10.1111/j.1523-1755.2005.00414.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.