Abstract
Yersinia pestis is a virulent human pathogen and potential biological weapon. Despite a long history of research on this organism, there is no licensed vaccine to protect against pneumonic forms of Y. pestis disease. In the present study, plasmids were constructed to express cholera toxin A2/B chimeric molecules containing the LcrV protective antigen from Y. enterocolitica and Y. pestis. These chimeras were expressed and purified to high yields from the supernatant of transformed E. coli. Western and GM1 ELISA assays were used to characterize the composition, receptor-binding and relative stability of the LcrV-CTA2/B chimera in comparison to cholera toxin. In addition, we investigated the ability of the Y. pestis LcrV-CTA2/B chimera to bind to and internalize into cultured epithelial cells and macrophages by confocal microscopy. These studies indicate that the uptake and trafficking of the LcrV antigen from the chimera is comparable to the trafficking of native toxin. Together these findings report that stable, receptor-binding, non-toxic LcrV-cholera toxin A2/B chimeras can be expressed at high levels in E. coli and purified from the supernatant. In addition, the internalization of antigen in vitro reported here supports the development of these molecules as novel mucosal vaccine candidates.
Keywords: cholera toxin, Yersinia pestis, mucosal adjuvant, A2B chimera, expression, trafficking
Introduction
Yersinia pestis is the agent of bubonic and pneumonic plague. This notorious bacterium has been the cause of over 200 million deaths from pandemics that have ravaged human populations throughout history. Today however, reported cases of Y. pestis infection in the U.S. are uncommon, and rapid treatment with antibiotics is effective at preventing most fatalities [1]. Despite the infrequency of disease, Y. pestis has been labeled a Category A bioterrorism agent by the Centers of Disease Control, and there is renewed urgency for the development of a protective vaccine against pneumonic forms of disease. Evidence suggests that this highly infectious organism has been used effectively in the past as a biological weapon [2]. There is no licensed vaccine available for general populations in the U.S. against plague. A formalin-killed whole cell preparation is currently available for military personnel and researchers at high risk, however studies have determined that this vaccine is only effective against bubonic plague and offers no protection against the easily transmitted pneumonic forms of disease [3; 4]. A live attenuated vaccine has also been in use since the early 1900’s and is highly protective, however the safety of this strain still remains in question [5].
Antibodies have been shown to play a key role in protection against this pathogen, and improved vaccines have focused on subunit preparations that contain the purified Y. pestis surface proteins F1 and LcrV [6]. The F1 antigen (encoded by caf1) is a capsular protein with antiphagocytic properties [7]. The LcrV antigen (or V antigen, encoded by lcrV) is a secreted protein detected on the surface of the bacterium and thought to have a key structural and regulatory role in type III secretion [8; 9]. A mixture of these proteins resulted in significant protection in the mouse, and a fusion of the two antigens is showing much promise as a parentally delivered vaccine [10; 11; 12; 13]. Studies with F1 and LcrV in non-human primates have been contradictory however, showing protection in cynomolgus macaques, but failing to protect African green monkeys from Yersinia pestis challenge [14]. In addition, the current intramuscular candidates target the induction of systemic immunity alone and induction of mucosal IgA to enhance protection against airborne infection and pneumonic disease requires the use of a separate adjuvant [15]. Despite these limitations, LcrV and F1 remain the most promising and well characterized plague vaccine candidates. LcrV and F1 are also expressed by other pathogenic strains of Yersinia, and there exists the added benefit that plague vaccines may offer cross protection against Y. enterocolitica, which is a common cause of food-borne gastroenteritis in the U.S. [16].
The bacterial enterotoxins, including cholera toxin (CT) and E. coli heat-labile toxin (LTI), offer a unique mechanism for the induction of both systemic and mucosal immune responses against subunit vaccine candidates [17; 18; 19]. CT, expressed by Vibrio cholerae, is a large heteromeric protein consisting of a receptor-binding pentameric B subunit (CTB) and an active A subunit (CTA). CTB binds to ganglioside receptors on host intestinal cells and triggers uptake of CT by retrograde endocytosis through the Golgi apparatus to the endoplasmic reticulum. The CTA1 domain is then translocated to the cytoplasm, where it activates adenylate cyclase and induces the secretion of fluids into the lumen of the small intestine. CT, and the structurally and functionally related LTI, are also potent immunostimulatory molecules that can bind to and target immune effector cells [20; 21]. Although not completely understood, CT immunomodulation is believed to involve the activation of antigen presenting cells, promotion of B-cell isotype switching, and upregulation of co-stimulatory and MHC class II expression [22]. These responses are the result of CTB receptor interactions with effector cells, such as dendritic cells, that promote antigen presentation and cellular activation [23]. Addition of CT and LTI to LcrV and F1 preparations has been explored and found to enhance IgA induction conferred by F1 and LcrV subunit vaccines [24; 25]. In addition, these adjuvants aid in the induction of cellular responses that also are a key component of protection [14; 24]. While toxigenic CT is clearly a more potent adjuvant, non-toxic CTB by itself is also an effective delivery vehicle and many reports suggest it may act as an immunostimulatory adjuvant on its own [18; 26]. CTB is a component of the current Vibrio cholerae vaccine (WC-rBS) produced in Sweden and licensed in many countries. This CTB-based vaccine is well tolerated with a good safety record [27].
In 1992, Jobling and Holmes reported the construction of CTA2/ CTB chimeras in an effort to develop stable holotoxin-like vaccine candidates with the antigen of interest replacing the toxic portion of the molecule and coupled to the B subunit [28]. These molecules possess a number of advantages for use as mucosal vaccines, including; the absence of the toxic domain, non-covalent association of the vaccine antigen to a functional CTB subunit, and maintenance of the ER-targeting KDEL motif. Evidence from studies on Entamoeba histolytica and Proteus mirabilis suggest that the structure of these A2/B chimeras is optimal for antigen uptake and presentation for the induction of specific humoral responses [29; 30; 31]. Additional chimeras constructed using CT, LTI and E. coli LTIIb enterotoxins have been reported and characterized in the mouse model by others [32; 33; 34; 35; 36]. For the production of these molecules in E. coli, plasmids are constructed that express antigens of interest covalently fused to the cholera toxin A2 domain (CTA2), and the full length CTB peptide. These peptides are directed for secretion to the periplasmic space by the presence of an N-terminal leader sequence. Earlier studies suggested that the E. coli LTIIB leader was very efficient at directing CT chimeras to the E. coli periplasm [29]. Translocation to the periplasm is essential for proper disulfide and hydrogen bonding to create a holotoxin-like molecule containing five CTB subunits that are non-covalently associated with one antigen-CTA2 fusion [37; 38]. Enhanced production of CTB over the CTA2 fusion is not completely understood, but may result from post-transcriptional regulation [26]. These chimeric constructs have proven to be a useful approach to the efficient production of detoxified yet immunogenic mucosal vaccines.
In these studies we present the construction and characterization of CT chimeras containing the LcrV antigen from Y. enterocolitica and Y. pestis (LcrV-CTA2/B). These chimeras were purified from the supernatant of transformed E. coli using D-galactose affinity chromatography, and found to have receptor-binding capability and stability comparable to native CT. In addition, we have characterized the ability of these chimeras to traffic the LcrV antigen into tissue culture cells using confocal microscopy. Successful trafficking in vitro is consistent with the goal of effective antigen delivery to antigen-presenting cells and induction of protective humoral and cellular responses in vivo. The purpose of these studies was to initiate the development of CT chimeras as novel mucosal Yersina vaccines. Despite the promise of current Y. pestis subunit vaccines, the development of better adjuvants that will support novel routes of delivery, induce mucosal IgA and cellular immune responses, and remain stable under challenging environmental conditions are significant goals for the improvement of these vaccines.
Materials and Methods
Bacterial strains, vectors and construction of plasmids
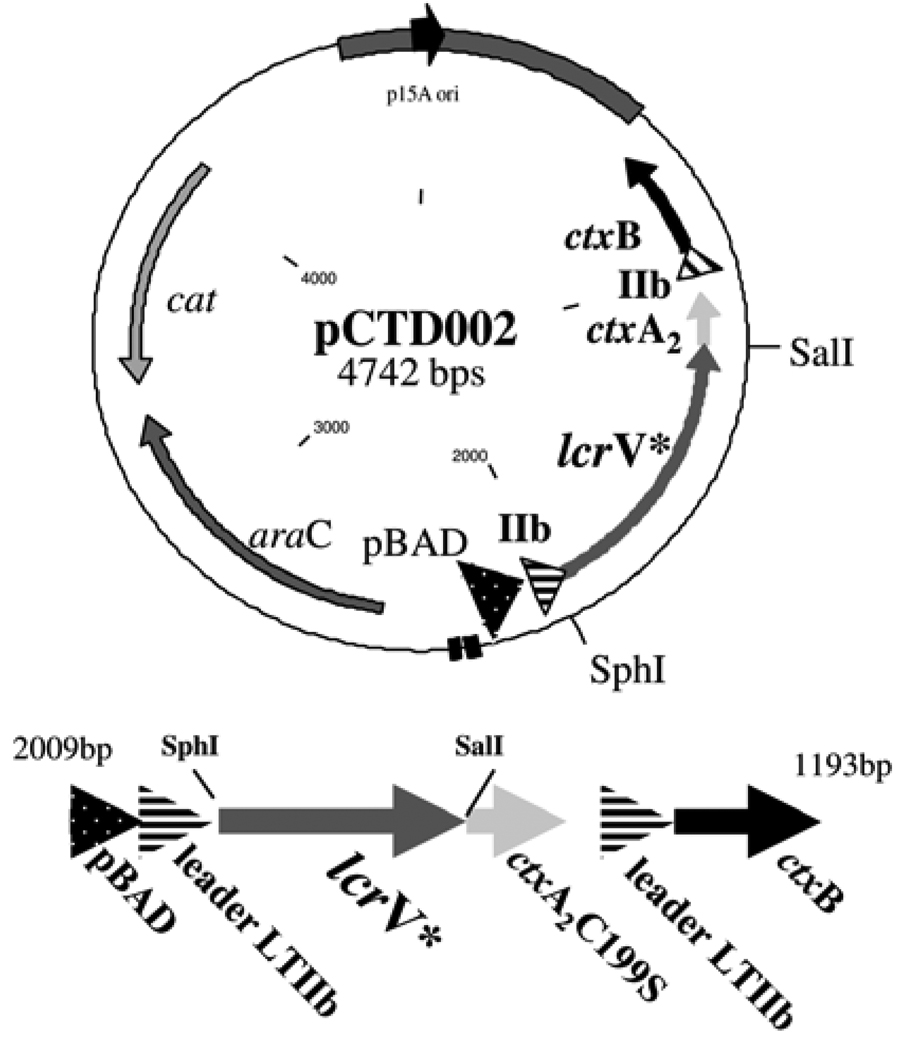
E. coli TE1 is a ΔendA derivative of TX1 [F'::Tn10 proA+B+ lacIq Δ(lacZ)M15, glnV44 Δ(hsdM-mcrB)5 Δ(lac-proAB)thi] [29]. This strain was used for the cloning of recombinant plasmids as well as expression of fusion proteins. E. coli Origami [F-, ompT, hsdSB(rB-,mB-), dcm, Δ(sr1-recA), 306::Tn10, gal] (Novagen, Madison, WI) was also used for fusion protein expression. Cultures were maintained on Luria-Bertani agar plates supplemented with the appropriate antibiotics. Antibiotics were added at a concentration of 35 µg/ml to select for chloramphenicol resistance (Cmr). A clinical isolate of Yersinia enterocolitica (Idaho Dept of Health and Welfare, Boise, ID) and the Y. pestis vaccine strain (KIM5) were used to isolate lcrV from genomic plasmid DNA. To make the Y. enterocolitica LcrV-CTA2/B expression plasmid, pCTD002 was constructed from the parental vector, pARLDR19 (kindly supplied by R.K.Holmes, UCHSC, Aurora, CO). pARLDR19 contains the E. coli LTIIb toxin leader sequence upstream of a multiple cloning site and the sequence encoding the CTA2 domain. The CTA2 domain has a mutation that results in the removal of a cysteine to prevent aberrant disulfide interactions (C199S). Downstream from this peptide sequence is ctxB, which also contains the LTIIB leader sequence. Both the ctxA2 fusion and the ctxB sequences are expressed from the same arabinose-inducible pBAD promoter [39]. Primers were designed to amplify a truncated form of lcrV from the Y. enterocolitica genomic prep and to add SphI and SalI restriction sites to the 5’ and 3’ ends respectively. The lcrV molecule was truncated at nucleotide 812 to create LcrV that is 54 amino acids shorter from the C-terminus of the protein (LcrV*, Figure 1 and 2). The primer sequences with restriction sites in bold are as follows: forward (SphI) 5’-GCAACCTGCATGC GATTAGAGCCTACGAACAA-3’ and reverse (SalI) 5’-GTTCGTAGTCGACGTGGCAAAGTGAGATAATTC-3’. The amplicon and pARLDR19 plasmid were digested with SphI and SalI. The digestion products were cleaned with a Qiagen PCR purification kit (Qiagen, Valencia CA) and ligated with T4 DNA ligase overnight at room temperature. The ligation mixture was then transformed into competent E. coli Origami (Novagen, Madison WI). To make the Y. pestis LcrV-CTA2/B expression plasmid, pCTD007 was constructed utilizing Y. pestis KIM5 DNA (kindly supplied by G. Hampikian, Boise State University, Boise, ID) as a template and the pARLDR19 parental vector with the same cloning strategy as described for pCTD002.
Figure 1.
Structure and operon organization of A) cholera toxin and B) plasmid pCTD002 for LcrV-CTA2/B chimera expression. The CTA2 domain that is incorporated with fusion proteins in CT-like chimeras corresponds to amino acids 195–240 (blue). The toxic CTA1 domain not present in CT chimeras corresponds to amino acids 1–194 (light grey). CTB pentamer is shown with three subunits (dark grey). The ER-targeting KDEL motif at the C-terminus is shown in red. The lcrV incorporated into pCTD002 is from Y. enterocolitica and is truncated at nucleotide 812 and thus amino acid 270 to remove the C-terminal 54 amino acids of LcrV (lcrV*).
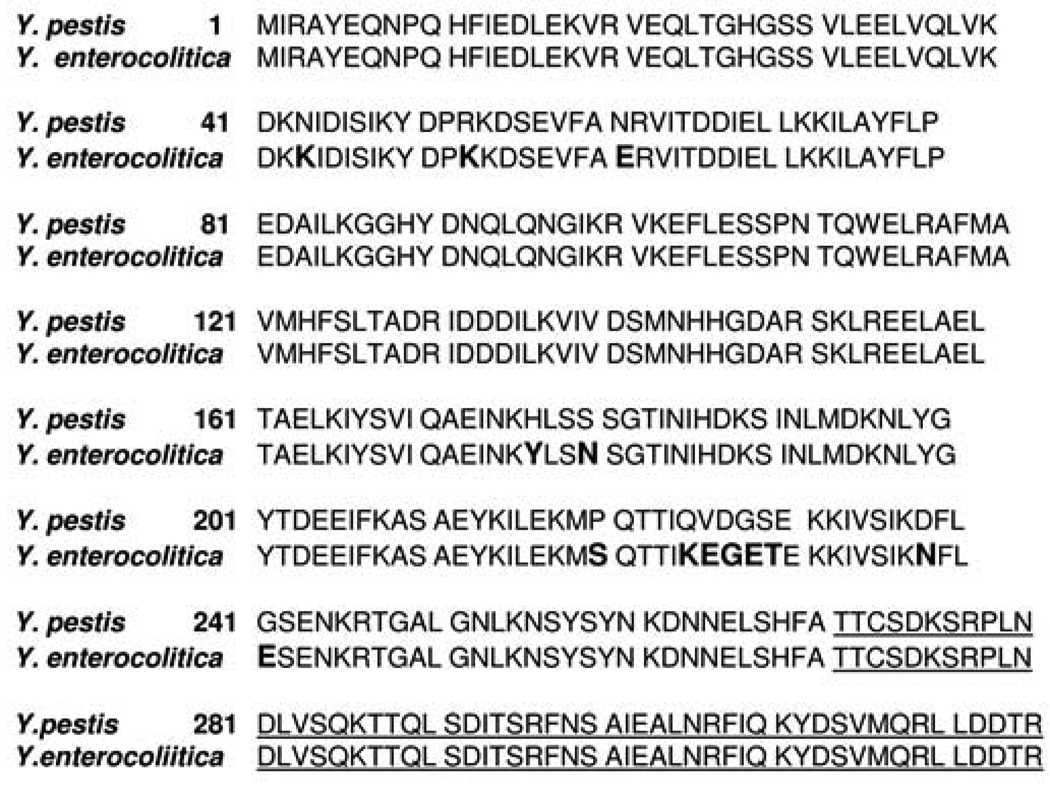
Figure 2.
Aligned amino acid sequences of Yersinia pestis strain KIM5 and Yersinia enterocolitica strain 8081. Bold indicates differences. Underlined amino acids are not included in the LcrV*-CTA2/B chimeras [62; 63].
Expression and purification of chimeras
E. coli Origami cells with pCTD002, were grown in 1 L of Terrific Broth (12 g tryptone, 24 g yeast extract, 85 mM KH2PO4, 360 mM K2HPO4, 0.4% Glycerol, pH 7.2) until mid log phase (OD600 = 0.600–0.900), induced with 0.2% l-arabinose and allowed to grow overnight. Bacteria were pelleted at 14,000 ×g for 10 minutes and supernatants were collected. To the supernatants, 50% immobilized D-galactose Gel (Pierce, Rockford, IL) was added to each tube of supernatant and agitated at 4°C for 2 hours. Agarose was pelleted, resuspended in 1X PBS and added to a 5 ml column. Column beds were washed twice with 2 ml PBS, and eluted with 2 ml 1M d-galactose. Elutions were dialyzed against two changes of 1 L 1X PBS using Slide-A-Lyzer ® dialysis cassettes (Pierce) and concentrated using a 50 kD Amicon ® Ultra Centrifugal Filter Device (Millipore; Bedford, MA). For expression of the Y. pestis chimera, E. coli TE1 cells with pCTD007 were grown in 25 ml of Terrific Broth and induced as described above. The Y. pestis chimera was eluted into a final volume of 500 µl before dialysis and further characterization by SDS-PAGE. Final protein concentrations were calculated using a BCA Protein Assay Kit (Pierce). Purified chimeric proteins were stored at 4°C for less than 1 week or frozen in 5% glycerol for longer storage.
SDS and western analysis
Purified LcrV-CTA2/B chimeras were processed for western blot analysis. Protein preparations were boiled for two minutes in β-mercapto-ethanol and separated by 12% SDS-Polyacrylamide Gel Electrophoresis (SDS-PAGE). Proteins were transferred from the gels to nitrocellulose membranes. The membranes were incubated in one of the following antibodies diluted in western blot blocking buffer (1X PBS with 0.05% tween-20 and 5% skim milk): Rabbit anti-LcrV polyclonal antibody 1:4000 dilution (α-LcrV, kindly supplied by S. Little and J. Adamovicz, USAMRIID, Ft. Detrick, MD), rabbit anti-CTA polyclonal antibody 1:2500 dilution (α-CTA, kindly supplied by RK Holmes, UCHSC, Aurora, CO), or rabbit anti–CTB polyclonal antibody 1:5000 dilution (α-CTB, Abcam Inc., Cambridge, MA). Primary antibody was visualized using goat α-rabbit HRP-linked secondary (1:2500 dilution, Thermo-Fisher, Austin, TX) and SuperSignal® West Pico Chemiluminescent Substrate (Pierce).
GM1 ELISA
The ganglioside GM1 ELISA protocol was performed as described [40]. Briefly, ninety-six well micro-titer plates (Corning, Lowell, MA) were coated with 100 µl of 1.5µM GM1 (Alexis Biochemicals, San Diego CA) at room temperature overnight. Plates were washed three times with PBS-T (1X PBS with 0.05% tween-20) and blocked with 200 µl ELISA blocking buffer (1X PBS-T + 5% skim milk) then stored at −20°C until use. Serial two-fold dilutions of either native CT (MP Biomedicals, Solon OH) or LcrV-CTA2/B (from both pCTD002 Y. enterocolitica and pCTD007 Y. pestis) in ELISA blocking buffer were then added to the wells and incubated for 1 hour at room temperature. Plates were then washed three times in PBS-T and antibodies with affinity for either CTB (1:5000 in blocking buffer), CTA (1:2500 in blocking buffer) or LcrV (1:2500 in blocking buffer) were applied and allowed to incubate at room temperature for 1 hour. The plates were then washed times in PBS-T again and incubated with an HRP conjugated goat anti-rabbit IgG (Thermo Scientific, Rockford IL) for 1 hour at room temperature. The assay was developed with TMB-one reagent (Promega, Madison WI) for 30 minutes and the absorbance was recorded at 655 nm on a microplate reader. The stability GM1 ELISA was also performed as described previously [41]. GM1-coated ELISA plates were incubated as described above with dilutions of CT or LcrV-CTA2/B and then immediately incubated with shaking for 15 minutes with either PBS, PBS + 0.5% SDS or McIluvaine buffer at pH 5.5 (43.55 ml of 0.1M citric acid plus 56.45 ml of 0.2M Na2HPO4). Plates were incubated with primary and secondary antibodies, and developed as described above.
In vitro trafficking and confocal microscopy
Green monkey kidney cells (Vero, ATCC) and mouse macrophages (J774, ATCC) were grown in 2 ml of Dulbecco’s modified Eagle medium (DMEM high glucose) supplemented with pen/strep and 10% fetal bovine serum for 48 hours to subconfluence on uncoated coverslips at 37°C and 5% CO2. The cells were then washed in DMEM without serum and incubated in 40 µl of 10 µg/ml CT or 40 µl of 10 µg/ml LcrV-CTA2/B chimera in phosphate-buffered saline (PBS) at 4°C for 15 minutes to allow protein binding to the plasma membrane. Subsequently, some cultures were shifted to 37°C for 45 minutes to allow toxin internalization to occur. The cells were then immediately washed in PBS and fixed in 3.7% formaldehyde for 1 hour at room temperature. Coverslips were then washed and cells were permeabilized with 0.1% Triton X-100 in PBS at room temperature for 15 minutes. Cells were washed again and blocked overnight in 10% FBS at 4 °C before incubation with rabbit polyclonal α-CT (Sigma, St. Louis MO) or α-LcrV primary antibody and α-rabbit IgG FITC conjugated secondary antibody (Sigma, St. Louis, MO) at 37 °C for 1 hour each. For co-localization with the Golgi apparatus, goat polyclonal α-Golgi (58K ab19072, Abcam, Cambridge, MA) primary antibody and Texas Red labeled rabbit α-goat (ab 6739, Abcam) secondary antibodies were also added. Coverslips were washed extensively in PBS and mounted with Vectashield Hardset Mounting Medium with DAPI (Vector Laboratories, Burlingame CA) before visualization using a Zeiss LSM 510 META laser scanning confocal microscope (Carl Zeiss Inc., Thornwood NY). Images were acquired using a 100× Alpha Plan-Fluar 1.45oil DIC objective and a factory set Diode laser at 405 nm for detection of DAPI, an Argon laser at 488 nm for detection of FITC, and a HeNe laser at 543 nm for detection of Texas Red. Equivalent settings, including pinhole, filters and bandpass were used for all images. Image acquisition and processing was performed using the LSM 510 META software.
Results
To produce a novel Yersinia mucosal vaccine candidate in E. coli, we cloned the lcrV antigen from Y. enterocolitica into the pARLDR19 vector for cholera toxin chimera expression [42]. The resulting plasmid expresses a truncated version of LcrV (LcrV* pCTD002, Figure 1) covalently fused to the cholera toxin A2 domain (CTA2), and CTB. Both peptides are directed for secretion to the periplasm, and holotoxin formation, using the E. coli LTIIB toxin leader sequence. The lcrV gene was truncated in pCTD002 to remove hydrophobic residues from the resulting peptide that may interfere with chimera secretion. The dominant protective epitopes of LcrV have been found within the central region of the molecule that is retained within the truncated LcrV chimera, and the sequences that were removed do not contain known B or T cell epitopes [43; 44; 45]. In addition, residues from the C-terminus of LcrV have been found to have negative immunomodulatory properties [46]. Originally we focused on the use of LcrV from Y. enterocolitica due to regulations obtaining and storing strains of Y. pestis and for proof of principal studies. However, while the LcrV antigen is largely conserved between strains of Y. pestis, certain strains of Y. enterocolitica produce an antigenically distinct LcrV [47; 48; 49]. This variation is most notably within a hypervariable region between amino acids 225-and 232 [50]. Sequencing suggests our clinical isolate of Y. enterocolitica is most closely related to strain 8081 serotype 08 and that there are sequence variations between the Y. enterocolitica LcrV and Y. pestis LcrV within this hypervariable region (Figure 2). While these antigenic differences have not been shown to eliminate cross-protection, they may reduce the efficacy of a targeted Y. pestis vaccine [48]. Thus we also constructed a Y. pestis LcrV-CTA2/B chimera using genomic DNA obtained from the KIM5 strain. This plasmid, pCTD007, also utilized the parental vector pARLDR19 and the same cloning strategy as described above for pCTD002.
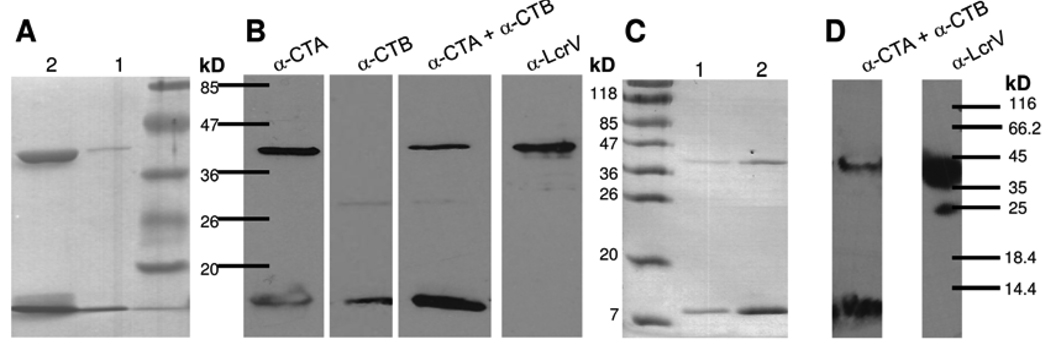
Induction of plasmids pCTD002 and pCTD007 and purification from the periplasmic space resulted in very low to negligible yields of chimeric protein. However, when induced cells were pelleted and the media supernatant fraction was analyzed, the complete LcrV-CTA2/B molecule from pCTD002 was found at high concentrations. We purified the supernatant using D-galactose agarose column chromatography. D-galactose will bind pentameric CTB, and thus co-purification of the CTA2 fusion is indicative of the production of folded chimera (Figure 3A). Western blot analysis of the purified LcrV-CTA2/B chimera from pCTD002 supported the proper toxin composition of this chimera and its reactivity to polyclonal LcrV antibodies (Figure 3B). Purification of the LcrV-CTA2/B chimera from the supernatant of cells transformed with pCTD007 also resulted in efficient chimera expression with the expected reactivity (Figure 3C, D). The resulting yield was 2–3 mg of chimera from one liter of starting culture.
Figure 3.
SDS-PAGE and western blot analysis of the purification of the LcrV-CTA2/B chimeras. A) SDS-PAGE of d-galactose agarose elutions 1 and 2 of the Y.enterocolitica LcrV-CTA2/B chimera (pCTD002). B) Western blot analysis of the Y.enterocolitica chimera using α-CTA, α-CTB and α-LcrV antibodies. C) SDS-PAGE of d-galactose agarose elutions 1 and 2 of the Y. pestis LcrV-CTA2/B chimera (pCTD007) from 25 ml of starting culture. Bands at 38kD represent the LcrV-CTA2 fusion, and bands at 11.5kD represent CTB monomeric subunits.
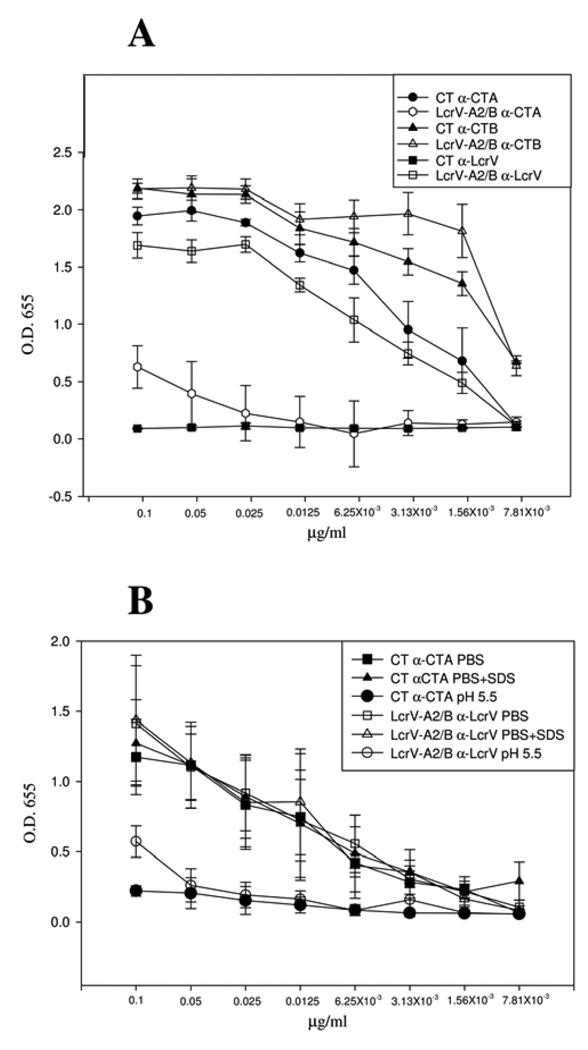
To better characterize the receptor-binding specificity and stability of the purified LcrV-CTA2/B chimeras, we performed ganglioside GM1 ELISA assays. GM1 is the native receptor for CT, and ELISA assays for the characterization of this toxin based on GM1 have been described previously [40; 41]. We compared wild-type CT to LcrV-CTA2/B from Y. pestis utilizing polyclonal α-CTA, α−CTB and α-LcrV antibodies (Figure 4A). These studies suggest that the chimera expresses the expected composition, subunit ratio and antibody reactivity. In addition, they reveal the ability of the chimeric molecule to bind to GM1 with an affinity comparable to CT. We also characterized the relative stability of the molecule by exposure to low concentrations of SDS as well as acidic pH (Figure 4B). Similar to CT, the chimera was unaffected by incubation in 0.5% SDS, however exposure to pH 5.5 was able to disrupt both the chimera and native CT. The Y. enterocolitica chimera from pCTD002 revealed similar characteristics from GM1 ELISA assays (data not shown).
Figure 4.
GM1 ELISA comparing the receptor binding affinities and stability of the LcrV-CTA2/B chimera and CT. A) GM1 affinity ELISA using α-CTA, α-CTB and α-LcrV primary antibodies (error bars are based on n=4). B) GM1 stability ELISA using α-CTA and α-LcrV and varying buffer conditions (error bars are based on n=2).
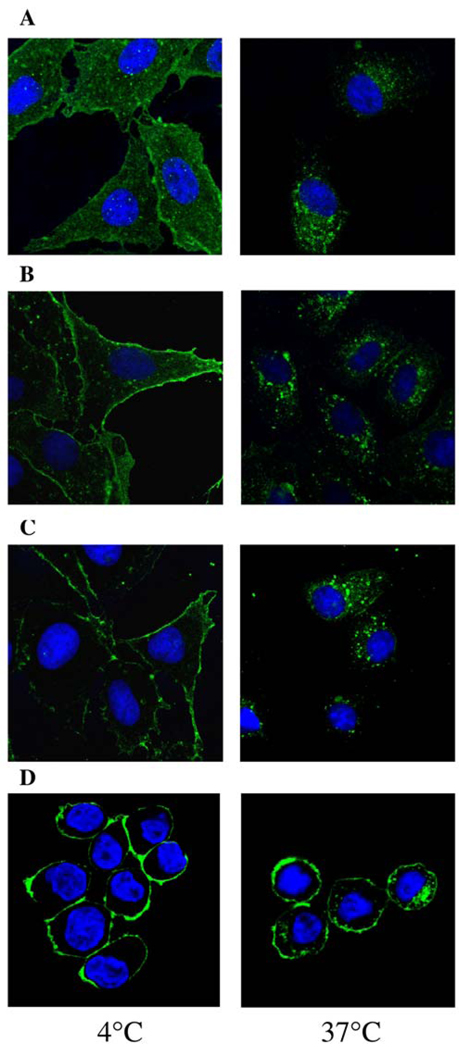
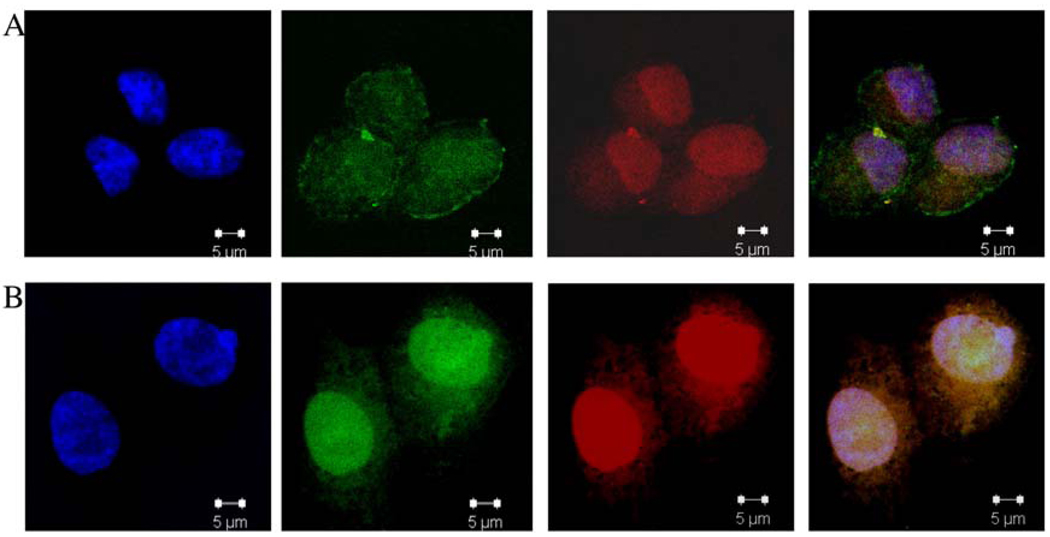
In addition to specific immunostimulatory effects, CT and CTB can induce immune responses by acting as effective antigen delivery vehicles. To determine if the LcrV-CTA2/B chimera was able to bind to tissue culture cells and promote the internalization of the LcrV antigen in a manner similar to native CTA, we characterized the in vitro trafficking of these molecules by confocal microscopy. As shown in Figure 5A, incubation of CT on Vero epithelial cells at 4°C resulted in binding to the cell surface but inhibition of endocytosis and no internalization. Incubation of cell cultures at 37°C for 45 minutes resulted in uptake of CT to a perinuclear compartment consistent with retrograde trafficking to the Golgi or endoplasmic reticulum that has been previously described [51; 52]. Incubation of the LcrV-CTA2/B chimera at 4°C similarly revealed binding to the cell surface, and shifting to 37°C permitted internalization of cholera domains as determined by the use of an α-CT polyclonal antibody (Figure 5B). Characterization of LcrV antigen trafficking using the α-LcrV antibody indicated that this component of the chimera is also efficiently internalized to a perinuclear cellular compartment in these cells (Figure 5C). The LcrV internalization can be blocked by pre-incubation of the Vero cells with CTB (data not shown). In addition to epithelial cells, we also wanted to analyze LcrV trafficking on immune effector cells. The J774 mouse macrophage cell line was used to demonstrate internalization of LcrV promoted by incubation with the chimera at 37°C for 45 minutes (Figure 5D). Trafficking was not as visible and potentially not as efficient on these cells, however uptake of LcrV was evident. Lastly, to determine cellular compartmentalization, we performed a co-localization analysis of LcrV with the Golgi apparatus using 58K-specific antibodies on Vero epithelial cells (Figure 6). Consistent with the route taken by the native CTA subunit, these results suggest that the chimera promotes LcrV trafficking to the Golgi at 37°C. Together, these studies support the native receptor-binding ability and relative stability of the LcrV-CTA2/B chimera. In addition, microscopy reveals the capacity of this molecule to promote the internalization and trafficking of the LcrV antigen on different CT-sensitive cells.
Figure 5.
Confocal microscopy of LcrV-CTA2/B trafficking on tissue culture cells. Cells were incubated with LcrV-CTA2/B from Y. pestis for 45 minutes at either 4°C to inhibit endocytosis or 37°C to promote uptake and compared to CT trafficking. A) CT with α-CT primary antibody on Vero cells, B) LcrV-A2/B with α-CT primary antibody on Vero cells, C) LcrV-CTA2/B with α-LcrV primary antibody on Vero cells and D) LcrV-A2/B with α-LcrV primary antibody on J774 cells.
Figure 6.
Confocal microscopy and cellular co-localization of LcrV with the Golgi apparatus. LcrV-CTA2/B was incubated at A) 4°C and B) 37°C for 45 minutes on Vero cells. Antibodies were α-LcrV and α-58K Golgi primary and α-rabbit FITC and α-goat Texas Red secondary. Panels show filters for DAPI, FITC, Texas Red and overlap.
Discussion
The LcrV antigen located at the tip of the type III secretion needle is essential for Yersinia pathogenesis and has been found to be a promising candidate vaccine antigen in a number of studies [3]. Two potential Y. pestis vaccines based on recombinant LcrV subunit have been found highly immunogenic in mice and have entered phase I and phase II clinical trials, however they have been limited by inconsistent protection studies in non-human primates [14; 53]. In addition, these vaccines must be delivered via intramuscular injection and contain a separate adjuvant. In this work we have reported the construction and early characterization of potential mucosal Y. pestis and Y. enterocolitica vaccine candidates based upon non-toxic chimeric fusions with cholera toxin. These molecules were found to be efficiently expressed in the supernatant of transformed E. coli cultures. In addition, the LcrV-CTA2/B chimeras contained the expected subunit composition, reacted as expected against polyclonal antisera, and retained receptor-binding capability and stability consistent with wild-type CT. Lastly, the chimera made with the Y. pestis antigen, was able to effectively deliver LcrV to CT-susceptible epithelial cells and macrophages in vitro.
While the production of CT chimeras from E. coli has been reported previously, efficient expression in the supernatant using the LTIIb leader sequence was unexpected and novel. Secretion to the periplasmic space of CT, LTI, and presumably LTIIb, toxin subunits in wild-type strains of V. cholerae or E. coli occurs through the general secretory pathway. After folding into holotoxin, secretion of the toxin out of the cell is then believed to occur through a specific type II mechanism [54]. This type II system is reportedly not present in E. coli K-12 strains and thus most toxin, or toxin subunits, expressed in these strains remains within the periplasmic space [55]. This is consistent with our experiences and chimera production from the LTIIb leader that we have previously reported in E. coli TE1 strains [42]. Thus the mechanism by which the LcrV-CTA2/B chimera is efficiently secreted external to the cell is currently unknown, however this is a favorable location for vaccine purification from E. coli because it allows for improved elimination of endotoxin. It is possible that this is a specific characteristic conferred by fusion to the LcrV antigen. However, future studies will focus on the optimization and mechanism of this extracellular expression.
The studies reported here utilized microscopy to characterize the intracellular trafficking of vaccine antigens facilitated by cholera toxin. We have reported the trafficking of fluorescent proteins on CT chimeras previously [42]. In addition, a study on the trafficking of antigens conjugated to the E. coli LTIB subunit used microscopy to show that epitopes could be delivered to the MHC class I pathway using this toxin [56]. Our results support these findings and indicate that the LcrV antigen, presented via non-covalent association with CTB on a chimera, can be effectively delivered into cultured epithelial cells. The resulting perinuclear localization of the antigen suggests that it is trafficked in a manner similar to that of CTA, and co-localization revealed that a significant amount of LcrV resides within the Golgi appartatus after a short incubation. These results support current evidence that the holotoxin-like structure of a CTA2/B chimeric molecule is optimal for the delivery of antigens to immune effector cells and presentation to the MHC class II, or potentially the MHC class I, pathway. Toxigenic CT and the CTB subunit have been found to induce a Th2 or mixed Th1/Th2 type response depending on the antigen that is delivered, the route of delivery and configuration of recombinant vaccine [22; 57; 58]. Additional studies to clarify antigen trafficking and presentation, as well as comparisons to the trafficking of unbound or covalently bound antigen with CT are necessary to better characterize the delivery mechanism and route of CT chimeras. Delivery to MHC class I and Th1 induction would be an important observation of chimera antigen trafficking, and a desirable characteristic for novel vaccine adjuvants. For Y. pestis, the induction of specific antibodies and a Th2 response is known to be essential for protection against systemic disease, however cellular responses have been found to enhance this response and the use of adjuvants that can stimulate both humoral and cellular responses is optimal [14]. Utimately, in vitro studies can only provide limited information on vaccine efficacy, and animal trials, which are currently in development, must be completed to determine the antigenicity and protective capabilities of this vaccine candidate.
There are three human pathogenic species of Yersina, and while they are closely related there are numerous genetic variations resulting in significant differences in clinical outcome. Y. enterocolitica and Y. pseudotuberculosis are causes of food and water-borne gastroenteritis, however these infections are usually self-limiting and rarely cause systemic disease. In contrast, Y. pestis bacteremia develops rapidly after infection and has a mortality rate, if untreated, from 60–90% [1]. One common characteristic among these strains is their ability to resist phagocytic killing through the expression of a type III secretion system and the LcrV antigen. We initially choose to construct CT chimeras based on the Y. enterocolitica LcrV molecule to facilitate preliminary studies and develop bactericidal assays in vitro under BSL2 conditions. However, it was determined that this molecule contains a hypervariable region with significant differences between species. Thus, we also utilized the Y. pestis sequence to construct a targeted plague vaccine. Studies suggest that there may be cross-protection between different LcrV variants, however, ultimately it may be important to include multiple variants of LcrV in a subunit vaccine for protection against different pathogenic Yersinia species [48; 49].
There are many advantages to the development of purified protein subunit vaccines that are less variable, have fewer side effects and can be delivered mucosally. CT, LTI and their respective B subunits have been incorporated into trials of both human and veterinary mucosal vaccines for a number of years and remain the gold-standard prototypic mucosal adjuvants [59; 60; 61]. In addition, CT and LTI are large, remarkably stable, easily purified, and can be manipulated to eliminate toxicity. We have found that many of these advantages, including the induction of both cellular and humoral responses, are also expressed by non-toxic chimeras. While there are promising Yersinia vaccine candidates currently undergoing clinical trials, the LcrV-CTA2/B chimeric molecules we have constructed have the significant advantage of mucosal administration and potential IgA induction. Oral or nasal administration is an important goal in vaccine development that effectively reduces infection rates, decreases overall cost and induces protective mucosal antibody responses. In addition, oral or nasal administration reduces or eliminates the need for trained health care workers, which is an important consideration for a vaccine that may target military personnel in the field. Lastly, the continued development of improved vaccine adjuvants that are less toxic, stimulate mucosal or Th1-type immune responses, and allow for novel delivery routes remains an urgent priority for vaccine research.
Acknowledgments
Much appreciation goes to Dr. Randall K. Holmes and Dr. Mike Jobling (UCHSC, Denver) for use of constructs and continued support. In addition, we would like to thank Raquel Brown (Boise State University) for confocal microscopy training, and Stephen Little (USAMRIID) for supplying us with the LcrV antibody. This work was supported by a 2007 Mountain States Tumor Institute Small Project grant, an NIH/Idaho INBRE grant (#P20RR016454) and an NSF Major Research Instrumentation grant (#0619793).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Prentice MB, Rahalison L. Plague. Lancet. 2007;369:1196–1207. doi: 10.1016/S0140-6736(07)60566-2. [DOI] [PubMed] [Google Scholar]
- 2.Inglesby TV, Dennis DT, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, Fine AD, Friedlander AM, Hauer J, Koerner JF, Layton M, McDade J, Osterholm MT, O'Toole T, Parker G, Perl TM, Russell PK, Schoch-Spana M, Tonat K Working Group on Civilian Biodefense. Plague as a biological weapon: medical and public health management. Jama. 2000;283:2281–2290. doi: 10.1001/jama.283.17.2281. [DOI] [PubMed] [Google Scholar]
- 3.Titball RW, Williamson ED. Yersinia pestis (plague) vaccines. Expert Opin Biol Ther. 2004;4:965–973. doi: 10.1517/14712598.4.6.965. [DOI] [PubMed] [Google Scholar]
- 4.Cohen RJ, Stockard JL. Pneumonic plague in an untreated plague-vaccinated individual. Jama. 1967;202:365–366. [PubMed] [Google Scholar]
- 5.Meyer KF, Smith G, Foster L, Brookman M, Sung M. Live, attenuated Yersinia pestis vaccine: virulent in nonhuman primates, harmless to guinea pigs. J Infect Dis. 1974;129 Suppl:S85–S12. doi: 10.1093/infdis/129.supplement_1.s85. [DOI] [PubMed] [Google Scholar]
- 6.Titball RW, Williamson ED. Vaccination against bubonic and pneumonic plague. Vaccine. 2001;19:4175–4184. doi: 10.1016/s0264-410x(01)00163-3. [DOI] [PubMed] [Google Scholar]
- 7.Rodrigues CG, Carneiro CM, Barbosa CT, Nogueira RA. Antigen F1 from Yersinia pestis forms aqueous channels in lipid bilayer membranes. Braz J Med Biol Res. 1992;25:75–79. [PubMed] [Google Scholar]
- 8.Holmstrom A, Olsson J, Cherepanov P, Maier E, Nordfelth R, Pettersson J, Benz R, Wolf-Watz H, Forsberg A. LcrV is a channel size-determining component of the Yop effector translocon of Yersinia. Mol Microbiol. 2001;39:620–632. doi: 10.1046/j.1365-2958.2001.02259.x. [DOI] [PubMed] [Google Scholar]
- 9.Pettersson J, Holmstrom A, Hill J, Leary S, Frithz-Lindsten E, von Euler-Matell A, Carlsson E, Titball R, Forsberg A, Wolf-Watz H. The V-antigen of Yersinia is surface exposed before target cell contact and involved in virulence protein translocation. Mol Microbiol. 1999;32:961–976. doi: 10.1046/j.1365-2958.1999.01408.x. [DOI] [PubMed] [Google Scholar]
- 10.Williamson ED, Flick-Smith HC, Lebutt C, Rowland CA, Jones SM, Waters EL, Gwyther RJ, Miller J, Packer PJ, Irving M. Human immune response to a plague vaccine comprising recombinant F1 and V antigens. Infect Immun. 2005;73:3598–3608. doi: 10.1128/IAI.73.6.3598-3608.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goodin JL, Nellis DF, Powell BS, Vyas VV, Enama JT, Wang LC, Clark PK, Giardina SL, Adamovicz JJ, Michiel DF. Purification and protective efficacy of monomeric and modified Yersinia pestis capsular F1-V antigen fusion proteins for vaccination against plague. Protein Expr Purif. 2007;53:63–79. doi: 10.1016/j.pep.2006.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Powell BS, Andrews GP, Enama JT, Jendrek S, Bolt C, Worsham P, Pullen JK, Ribot W, Hines H, Smith L, Heath DG, Adamovicz JJ. Design and testing for a nontagged F1-V fusion protein as vaccine antigen against bubonic and pneumonic plague. Biotechnol Prog. 2005;21:1490–1510. doi: 10.1021/bp050098r. [DOI] [PubMed] [Google Scholar]
- 13.Heath DG, Anderson GW, Jr, Mauro JM, Welkos SL, Andrews GP, Adamovicz J, Friedlander AM. Protection against experimental bubonic and pneumonic plague by a recombinant capsular F1-V antigen fusion protein vaccine. Vaccine. 1998;16:1131–1137. doi: 10.1016/s0264-410x(98)80110-2. [DOI] [PubMed] [Google Scholar]
- 14.Smiley ST. Current challenges in the development of vaccines for pneumonic plague. Expert Rev Vaccines. 2008;7:209–221. doi: 10.1586/14760584.7.2.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones T, Adamovicz JJ, Cyr SL, Bolt CR, Bellerose N, Pitt LM, Lowell GH, Burt DS. Intranasal Protollin/F1-V vaccine elicits respiratory and serum antibody responses and protects mice against lethal aerosolized plague infection. Vaccine. 2006;24:1625–1632. doi: 10.1016/j.vaccine.2005.09.052. [DOI] [PubMed] [Google Scholar]
- 16.Robins-Browne RM. Yersinia enterocolitica. Washington, DC: ASM Press; 1997. [Google Scholar]
- 17.Rappuoli R, Pizza M, Douce G, Dougan G. Structure and mucosal adjuvanticity of cholera and Escherichia coli heat-labile enterotoxins. Immunol Today. 1999;20:493–500. doi: 10.1016/s0167-5699(99)01523-6. [DOI] [PubMed] [Google Scholar]
- 18.Holmgren J, Czerkinsky C, Lycke N, Svennerholm AM. Strategies for the induction of immune responses at mucosal surfaces making use of cholera toxin B subunit as immunogen, carrier, and adjuvant. Am J Trop Med Hyg. 1994;50:42–54. [PubMed] [Google Scholar]
- 19.Lycke N, Holmgren J. Strong adjuvant properties of cholera toxin on gut mucosal immune responses to orally presented antigens. Immunology. 1986;59:301–308. [PMC free article] [PubMed] [Google Scholar]
- 20.Pizza M, Giuliani MM, Fontana MR, Monaci E, Douce G, Dougan G, Mills KHG, Rappuoli R, Del Giudice G. Mucosal vaccines: non toxic derivatives of LT and CT as mucosal adjuvants. Vaccine. 2001;19:2534–2541. doi: 10.1016/s0264-410x(00)00553-3. [DOI] [PubMed] [Google Scholar]
- 21.Salmond RJ, Luross JA, Williams NA. Immune modulation by the cholera-like enterotoxins. Expert Rev Mol Med. 2002;2002:1–16. doi: 10.1017/S1462399402005057. [DOI] [PubMed] [Google Scholar]
- 22.Hajishengallis G, Arce S, Gockel CM, Connell TD, Russell MW. Immunomodulation with enterotoxins for the generation of secretory immunity or tolerance: applications for oral infections. J Dent Res. 2005;84:1104–1116. doi: 10.1177/154405910508401205. [DOI] [PubMed] [Google Scholar]
- 23.Schnitzler AC, Burke JM, Wetzler LM. Induction of cell signaling events by the cholera toxin B subunit in antigen-presenting cells. Infect Immun. 2007;75:3150–3159. doi: 10.1128/IAI.00581-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Uddowla S, Freytag LC, Clements JD. Effect of adjuvants and route of immunizations on the immune response to recombinant plague antigens. Vaccine. 2007;25:7984–7993. doi: 10.1016/j.vaccine.2007.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eyles JE, Elvin SJ, Westwood A, Lebutt CS, Alpar HO, Somavarapu S, Williamson ED. Immunisation against plague by transcutaneous and intradermal application of subunit antigens. Vaccine. 2004;22:4365–4373. doi: 10.1016/j.vaccine.2004.02.049. [DOI] [PubMed] [Google Scholar]
- 26.Sanchez J, Holmgren J. Cholera toxin structure, gene regulation and pathophysiological and immunological aspects. Cell Mol Life Sci. 2008;65:1347–1360. doi: 10.1007/s00018-008-7496-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tacket CaS, Cholera vaccines D. Elsievier; 2008. [Google Scholar]
- 28.Jobling MG, Holmes RK. Fusion proteins containing the A2 domain of cholera toxin assemble with B polypeptides of cholera toxin to form immunoreactive and functional holotoxin-like chimeras. Infect Immun. 1992;60:4915–4924. doi: 10.1128/iai.60.11.4915-4924.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jobling MG, Palmer LM, Erbe JL, Holmes RK. Construction and characterization of versatile cloning vectors for efficient delivery of native foreign proteins to the periplasm of Escherichia coli. Plasmid. 1997;38:158–173. doi: 10.1006/plas.1997.1309. [DOI] [PubMed] [Google Scholar]
- 30.Sultan F, Jin LL, Jobling MG, Holmes RK, Stanley SL., Jr Mucosal immunogenicity of a holotoxin-like molecule containing the serine-rich Entamoeba histolytica protein (SREHP) fused to the A2 domain of cholera toxin. Infect Immun. 1998;66:462–468. doi: 10.1128/iai.66.2.462-468.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li X, Erbe JL, Lockatell CV, Johnson DE, Jobling MG, Holmes RK, Mobley HL. Use of translational fusion of the MrpH fimbrial adhesin-binding domain with the cholera toxin A2 domain, coexpressed with the cholera toxin B subunit, as an intranasal vaccine to prevent experimental urinary tract infection by Proteus mirabilis. Infect Immun. 2004;72:7306–7310. doi: 10.1128/IAI.72.12.7306-7310.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Harakuni T, Sugawa H, Komesu A, Tadano M, Arakawa T. Heteropentameric cholera toxin B subunit chimeric molecules genetically fused to a vaccine antigen induce systemic and mucosal immune responses: a potential new strategy to target recombinant vaccine antigens to mucosal immune systems. Infect Immun. 2005;73:5654–5665. doi: 10.1128/IAI.73.9.5654-5665.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gockel CM, Russell MW. Induction and recall of immune memory by mucosal immunization with a non-toxic recombinant enterotoxin-based chimeric protein. Immunology. 2005;116:477–486. doi: 10.1111/j.1365-2567.2005.02246.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hajishengallis G, Hollingshead SK, Koga T, Russell MW. Mucosal immunization with a bacterial protein antigen genetically coupled to cholera toxin A2/B subunits. J Immunol. 1995;154:4322–4332. [PubMed] [Google Scholar]
- 35.Hatic SO, 2nd, McCann JA, Picking WD. In vitro assembly of novel cholera toxin-like complexes. Anal Biochem. 2001;292:171–177. doi: 10.1006/abio.2001.5084. [DOI] [PubMed] [Google Scholar]
- 36.Sanchez J, Wallerstrom G, Fredriksson M, Angstrom J, Holmgren J A potential new strategy to generate immunostimulants for vaccination. Detoxification of cholera toxin without removal of its immunoadjuvanticity by the addition of (STa-related) peptides to the catalytic subunit. J Biol Chem. 2002;277:33369–33377. doi: 10.1074/jbc.M112337200. [DOI] [PubMed] [Google Scholar]
- 37.Streatfield SJ, Sandkvist M, Sixma TK, Bagdasarian M, Hol WG, Hirst TR. Intermolecular interactions between the A and B subunits of heat-labile enterotoxin from Escherichia coli promote holotoxin assembly and stability in vivo. Proc Natl Acad Sci U S A. 1992;89:12140–12144. doi: 10.1073/pnas.89.24.12140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hardy SJ, Holmgren J, Johansson S, Sanchez J, Hirst TR. Coordinated assembly of multisubunit proteins: oligomerization of bacterial enterotoxins in vivo and in vitro. Proc Natl Acad Sci U S A. 1988;85:7109–7113. doi: 10.1073/pnas.85.19.7109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Guzman LM, Belin D, Carson MJ, Beckwith J. Tight regulation, modulation, and high-level expression by vectors containing the arabinose PBAD promoter. J Bacteriol. 1995;177:4121–4130. doi: 10.1128/jb.177.14.4121-4130.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sanchez J, Holmgren J, Svennerholm AM. Recombinant fusion protein for simple detection of Escherichia coli heat-stable enterotoxin by GM1 enzyme-linked immunosorbent assay. J Clin Microbiol. 1990;28:2175–2177. doi: 10.1128/jcm.28.10.2175-2177.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rodighiero C, Aman AT, Kenny MJ, Moss J, Lencer WI, Hirst TR. Structural basis for the differential toxicity of cholera toxin and Escherichia coli heat-labile enterotoxin. Construction of hybrid toxins identifies the A2-domain as the determinant of differential toxicity. J Biol Chem. 1999;274:3962–3969. doi: 10.1074/jbc.274.7.3962. [DOI] [PubMed] [Google Scholar]
- 42.Tinker JK, Erbe JL, Holmes RK. Characterization of fluorescent chimeras of cholera toxin and Escherichia coli heat-labile enterotoxins produced by use of the twin arginine translocation system. Infect Immun. 2005;73:3627–3635. doi: 10.1128/IAI.73.6.3627-3635.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hill J, Leary SE, Griffin KF, Williamson ED, Titball RW. Regions of Yersinia pestis V antigen that contribute to protection against plague identified by passive and active immunization. Infect Immun. 1997;65:4476–4482. doi: 10.1128/iai.65.11.4476-4482.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pullen JK, Anderson GW, Jr, Welkos SL, Friedlander AM. Analysis of the Yersinia pestis V protein for the presence of linear antibody epitopes. Infect Immun. 1998;66:521–527. doi: 10.1128/iai.66.2.521-527.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Quenee LE, Berube BJ, Segal J, Elli D, Ciletti NA, Anderson D, Schneewind O. Amino acid residues 196–225 of LcrV represent a plague protective epitope. Vaccine. 2010;28:1870–1876. doi: 10.1016/j.vaccine.2009.11.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Overheim KA, Depaolo RW, Debord KL, Morrin EM, Anderson DM, Green NM, Brubaker RR, Jabri B, Schneewind O. LcrV plague vaccine with altered immunomodulatory properties. Infect Immun. 2005;73:5152–5159. doi: 10.1128/IAI.73.8.5152-5159.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Branger CG, Fetherston JD, Perry RD, Curtiss R., 3rd Oral vaccination with different antigens from Yersinia pestis KIM delivered by live attenuated Salmonella typhimurium elicits a protective immune response against plague. Adv Exp Med Biol. 2007;603:387–399. doi: 10.1007/978-0-387-72124-8_36. [DOI] [PubMed] [Google Scholar]
- 48.Branger CG, Torres-Escobar A, Sun W, Perry R, Fetherston J, Roland KL, Curtiss R., 3rd Oral vaccination with LcrV from Yersinia pestis KIM delivered by live attenuated Salmonella enterica serovar Typhimurium elicits a protective immune response against challenge with Yersinia pseudotuberculosis and Yersinia enterocolitica. Vaccine. 2009;27:5363–5370. doi: 10.1016/j.vaccine.2009.06.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Anisimov AP, Dentovskaya SV, Panfertsev EA, Svetoch TE, Kopylov PK, Segelke BW, Zemla A, Telepnev MV, Motin VL. Amino acid and structural variability of Yersinia pestis LcrV protein. Infect Genet Evol. 2009 doi: 10.1016/j.meegid.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Roggenkamp A, Geiger AM, Leitritz L, Kessler A, Heesemann J. Passive immunity to infection with Yersinia spp. mediated by anti-recombinant V antigen is dependent on polymorphism of V antigen. Infect Immun. 1997;65:446–451. doi: 10.1128/iai.65.2.446-451.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bastiaens PI, Majoul IV, Verveer PJ, Soling HD, Jovin TM. Imaging the intracellular trafficking and state of the AB5 quaternary structure of cholera toxin. Embo J. 1996;15:4246–4253. [PMC free article] [PubMed] [Google Scholar]
- 52.Majoul IV, Bastiaens PI, Soling HD. Transport of an external Lys-Asp-Glu-Leu (KDEL) protein from the plasma membrane to the endoplasmic reticulum: studies with cholera toxin in Vero cells. J Cell Biol. 1996;133:777–789. doi: 10.1083/jcb.133.4.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Quenee LE, Schneewind O. Plague vaccines and the molecular basis of immunity against Yersinia pestis. Hum Vaccin. 2009;5 doi: 10.4161/hv.9866. [DOI] [PubMed] [Google Scholar]
- 54.Sandkvist M, Michel LO, Hough LP, Morales VM, Bagdasarian M, Koomey M, DiRita VJ, Bagdasarian M. General secretion pathway (eps) genes required for toxin secretion and outer membrane biogenesis in Vibrio cholerae. J Bacteriol. 1997;179:6994–7003. doi: 10.1128/jb.179.22.6994-7003.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tauschek M, Gorrell RJ, Strugnell RA, Robins-Browne RM. Identification of a protein secretory pathway for the secretion of heat-labile enterotoxin by an enterotoxigenic strain of Escherichia coli. Proc Natl Acad Sci U S A. 2002;99:7066–7071. doi: 10.1073/pnas.092152899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.De Haan L, Hearn AR, Rivett AJ, Hirst TR. Enhanced delivery of exogenous peptides into the class I antigen processing and presentation pathway. Infect Immun. 2002;70:3249–3258. doi: 10.1128/IAI.70.6.3249-3258.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lavelle EC, Jarnicki A, McNeela E, Armstrong ME, Higgins SC, Leavy O, Mills KH. Effects of cholera toxin on innate and adaptive immunity and its application as an immunomodulatory agent. J Leukoc Biol. 2004;75:756–763. doi: 10.1189/jlb.1103534. [DOI] [PubMed] [Google Scholar]
- 58.Eriksson K, Fredriksson M, Nordstrom I, Holmgren J. Cholera toxin and its B subunit promote dendritic cell vaccination with different influences on Th1 and Th2 development. Infect Immun. 2003;71:1740–1747. doi: 10.1128/IAI.71.4.1740-1747.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cox E, Verdonck F, Vanrompay D, Goddeeris B. Adjuvants modulating mucosal immune responses or directing systemic responses towards the mucosa. Vet Res. 2006;37:511–539. doi: 10.1051/vetres:2006014. [DOI] [PubMed] [Google Scholar]
- 60.Holmgren J, Czerkinsky C. Mucosal immunity and vaccines. Nat Med. 2005;11:S45–S53. doi: 10.1038/nm1213. [DOI] [PubMed] [Google Scholar]
- 61.Holmgren J, Czerkinsky C, Eriksson K, Mharandi A. Mucosal immunisation and adjuvants: a brief overview of recent advances and challenges. Vaccine. 2003;21 Suppl 2:S89–S95. doi: 10.1016/s0264-410x(03)00206-8. [DOI] [PubMed] [Google Scholar]
- 62.Thomson NR, Howard S, Wren BW, Holden MT, Crossman L, Challis GL, Churcher C, Mungall K, Brooks K, Chillingworth T, Feltwell T, Abdellah Z, Hauser H, Jagels K, Maddison M, Moule S, Sanders M, Whitehead S, Quail MA, Dougan G, Parkhill J, Prentice MB. The complete genome sequence and comparative genome analysis of the high pathogenicity Yersinia enterocolitica strain 8081. PLoS Genet. 2006;2:e206. doi: 10.1371/journal.pgen.0020206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hu P, Elliott J, McCready P, Skowronski E, Garnes J, Kobayashi A, Brubaker RR, Garcia E. Structural organization of virulence-associated plasmids of Yersinia pestis. J Bacteriol. 1998;180:5192–5202. doi: 10.1128/jb.180.19.5192-5202.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]