Abstract
The increased risk of symptomatic progression towards osteoarthritis after chondral damage has led to the development of multiple treatment options for cartilage repair. These procedures have evolved from arthroscopic lavage and debridement, to marrow stimulation techniques, and more recently, to osteochondral autograft and allograft transplants, and autogenous chondrocyte implantation. The success of mosaicplasty procedures in the knee has led to its application to other surfaces, including the talus, tibial plateau, patella, and humeral capitellum. In this report, we present two cases of a chondral defect to the femoral head after a traumatic hip dislocation, treated with an osteochondral autograft (OATS) from the ipsilateral knee, and the inferior femoral head, respectively, combined with a surgical dislocation of the hip. At greater than 1 year and greater than 5 years of follow-up, MRI studies have demonstrated good autograft incorporation with maintenance of articular surface conformity, and both patients clinically continue to have no pain and full active range of motion of their respective hips. In our opinion, treatment of osteochondral defects in the femoral head surface using a surgical dislocation combined with an OATS procedure is a promising approach, as full exposure of the femoral head can be obtained while preserving its vasculature, thus enabling adequate restoration of the articular cartilage surface.
Keywords: hip dislocation, osteochondral autograft transplant, femoral head, osteochondral defect, osteochondral injury, mosaicplasty
Introduction
The increased risk of symptomatic progression towards osteoarthritis after chondral damage has led to the development of multiple treatment options for cartilage repair. These procedures have evolved from arthroscopic lavage and debridement, to marrow stimulation techniques, and more recently, to attempts at actual articular cartilage replacement including osteochondral autograft transplants (OATS), osteochondral allograft transplants, and autogenous chondrocyte implantation [1–3]. While full-thickness cartilage lesions involving subchondral bone have the potential to stimulate a self-healing reparative process, which is the scientific basis behind marrow stimulation techniques, the end result is the production of type I collagen, or fibrocartilage, which is known to be biomechanically inferior compared to hyaline cartilage [3–8].
Osteochondral transplant techniques, both autograft and allograft, involve the transfer of small bone plugs covered with normal hyaline articular cartilage into focal chondral defects, which then heal to the surrounding recipient tissue [9, 10]. Mosaicplasty (autogenous osteochondral grafting) was developed by Hangody and Karpati in the early 1990s, and its popularity has increased since its inception. The key to graft survival and viability is the presence of intact, healthy hyaline cartilage, as only viable chondrocytes can produce and maintain the extracellular matrix vital for load-bearing capacity [10]. A review of 831 mosaicplasties performed over 10 years at one institution found good-to-excellent results in 92% of patients with femoral condylar implantations, 87% with tibial resurfacing, 79% with patellar and/or trochlear mosaicplasties, and 94% of those with talar procedures [12, 13]. In addition, due to its success, mosaicplasty has been applied to other diarthrodial surfaces, including the tibial plateau, and the humeral capitellum. Mosaicplasty of the femoral head has been described; however, details regarding the surgical procedure and clinical outcome were not discussed [11]. In this report, we present two cases of a traumatic chondral defect to the femoral head, treated with an osteochondral autograft combined with a surgical dislocation of the hip [12].
Case report 1
The patient was an otherwise healthy 15-year-old male who presented 3.5 weeks after a motor vehicle accident in which he sustained a right posterior hip dislocation and cervical spine injury. He was a restrained, front-seat passenger in a vehicle which lost control off of the road at a speed of approximately 65 miles h−1. He lost consciousness and was taken to the emergency department where he was diagnosed with C2–C4 spine fractures and a posterior right hip dislocation. There was no neurological injury. His hip was reduced in the operating room, at which time a tibial traction pin was placed. After presentation (1 week), he underwent a C2–C4 cervical fusion. Prior to discharge, the tibial traction pin was removed and he was kept non-weight-bearing on his right lower extremity. Plain radiographs, CT scan, and MRI confirmed the presence of loose fragments in the joint, a slightly displaced osteochondral fracture of the weight-bearing aspect of the femoral head with depression of the articular surface, and areas of full-thickness cartilage loss (Figs. 1 and 2).
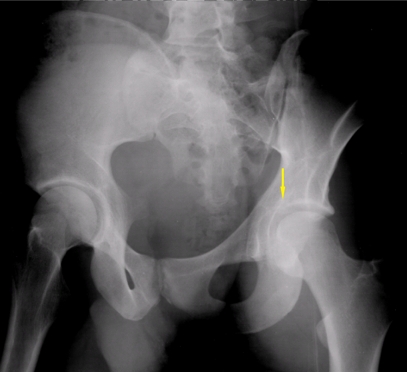
Fig. 1.
A preoperative AP radiograph of the pelvis demonstrating no appreciable abnormality in the contour of the femoral head
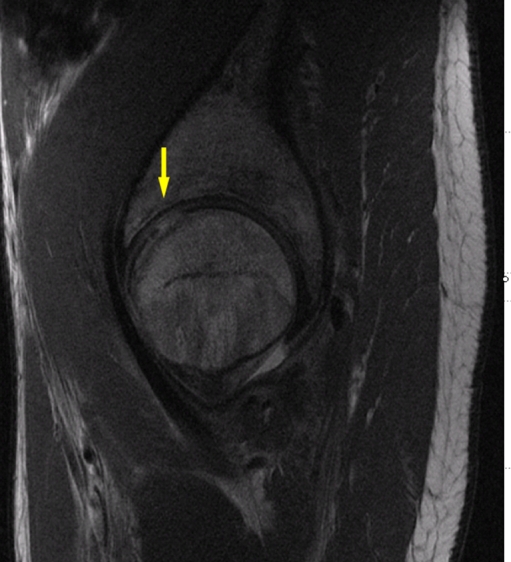
Fig. 2.
A sagittal section of the patient’s MRI demonstrating an area of full-thickness cartilage loss in the anterior-superior weight-bearing zone of the femoral head
The patient presented to our clinic approximately 1 month after his initial injury. After the traumatic posterior dislocation (5.5 weeks), the patient underwent a right hip surgical dislocation with fixation of the osteochondral defect and osteochondral autograft transplantation from the ipsilateral knee to the femoral head. Surgical exposure was performed using a Kocher–Langenbeck incision [13], followed by a surgical hip dislocation with a trochanteric osteotomy [12, 14] (Fig. 3a, b). The hip was dislocated anteriorly, and a 3 × 3 cm defect where the cartilage had been impacted into the femoral head was visualized (Fig. 4). While there was a stable component to the cartilage, there was an area in the anterior-superior weight-bearing region with exposed subchondral bone where the cartilage was completely absent. Several loose fragments within the capsule were identified and excised, and all cartilage fragments were removed from the joint. No significant acetabular cartilage or labral pathology was appreciated. At this point, the cartilage injury on the femoral head was debrided back to stable ridges. The stable osteochondral lesion appeared well perfused, as significant bleeding was appreciated from the subchondral surface. While the chondral lesion was slightly rotated, the contour of its borders still matched that of the neighboring cartilage. Therefore, the decision was made to stabilize the lesion with bioabsorbable SmartNails (ConMed Linvatec, Largo, FL, USA), each 1.5 mm × 2 cm in length, placed around the periphery. Initially, two of the SmartNails were utilized to lock the lesion into a stabilized position, away from the neighboring cartilage defect.
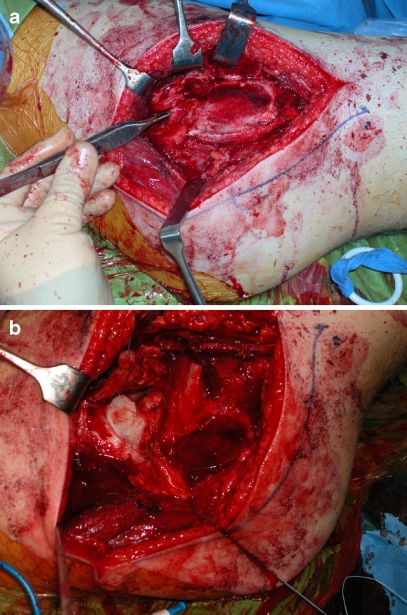
Fig. 3.
Intraoperative images demonstrating the trochanteric osteotomy (a) and exposure of the femoral head (b) prior to dislocating the femoral head anteriorly
Fig. 4.
An intraoperative image demonstrating cartilage impaction along with exposed subchondral bone in the anterior-superior portion of the femoral head
Focus was then directed to the full-thickness cartilage defect in the anterior-superior weight-bearing zone of the femoral head, adjacent to the stabilized osteochondral defect. There was a linear lesion that measured approximately 2 cm in length and was tapered down from approximately 8 to 5 mm in width. It was felt that three osteochondral plugs would be required upon sizing, and the recipient site was prepared using the Arthrex osteochondral autograft transplant system (Arthrex, Naples, FL, USA). Next, a small lateral arthrotomy was performed at the level of the knee joint approximately 3 cm in length. Three osteochondral plugs were harvested using the Arthrex osteochondral autograft transplant harvesting system—8, 7, and 5 mm in size, respectively.
The donor osteochondral plugs were then transplanted to the area of full-thickness cartilage loss adjacent to the stabilized osteochondral defect. The 8-mm plug was placed most superiorly, followed by the 7-mm plug, then the 5-mm plug. Good contour of the articular cartilage surface and to the neighboring osteochondral defect was obtained. A third SmartNail was then used to fix the ostechondral defect (Fig. 5). A smooth articular contour was achieved after placement of the osteochondral plugs. At the completion of the procedure there were some areas of residual cartilage injury with residual exposed bone at the level of the fovea and also inferiorly in the non-weight-bearing region of the joint. As these foci were not in weight-bearing regions, cartilage transplant was not believed to be necessary, but microfracture procedures were performed to stimulate fibrocartilage in-growth. Of note, consistent bleeding from the femoral head was appreciated throughout the procedure. The donor autograft sites were then back filled with OBI plugs (Osteobiologics Inc., San Antonio, TX, USA), where again, a smooth contour was achieved with the neighboring cartilage.
Fig. 5.
An intraoperative image of the femoral head after placement of the donor osteochondral plugs and three SmartNails
Post-operatively, the patient was kept non-weight-bearing for 6 weeks and then progressed to weight-bearing as tolerated. At 12 weeks post-operatively, the patient was ambulating with the use of a cane without any pain, had minimal symptoms, and plain radiographs demonstrated an overall reasonable contour of the femoral head and good preservation of the joint space (Fig. 6). An MRI performed at 24 weeks post-operatively demonstrated well-incorporated autograft plugs and intact cartilage over the plugs with smooth interfaces with the remaining bone. Thinning of cartilage and moderate bony irregularity was noted anteriorly related to the fracture, but no reactive signal underlying the bone was present. At 1 year follow-up, the patient has no complaints of pain, good mechanics with ambulation, and has returned to running and physical activity without difficulty.
Fig. 6.
A postoperative AP radiograph of the patient’s pelvis demonstrating an anatomic contour of the femoral head and well-preserved joint space
Case report 2
The patient was an otherwise healthy 21-year-old male who presented 10 days after a skiing accident in which he suffered a left posterior hip dislocation. He attempted a jump in which he was performing a 360° turn, when he landed on his left leg while his body continued to rotate. He stated that his ski bindings did not release, and he twisted and fell forward onto the ground. He was taken to the emergency department where he was diagnosed with a left posterior hip dislocation, Pipkin type II femoral head fracture, with multiple intra-articular bony fragments. Approximately 1.5 h after the accident, he was taken to the operating room where he underwent closed reduction of the left hip. He was discharged the next morning, non-weight-bearing on the left lower extremity. Plain radiographs, CT scan, and MRI confirmed the presence of a vertically oriented femoral head fracture extending above and below the fovea in the coronal plane, with bony fragments in the posterosuperior aspect of the joint, as well as posteroinferior. In addition, significant cartilaginous injury was appreciated at the apex of the fracture fragment superiorly (Figs. 7 and 8).
Fig. 7.
A preoperative internal (obturator) oblique view of the left hip, demonstrating an intra-articular bony fragment in the left hip
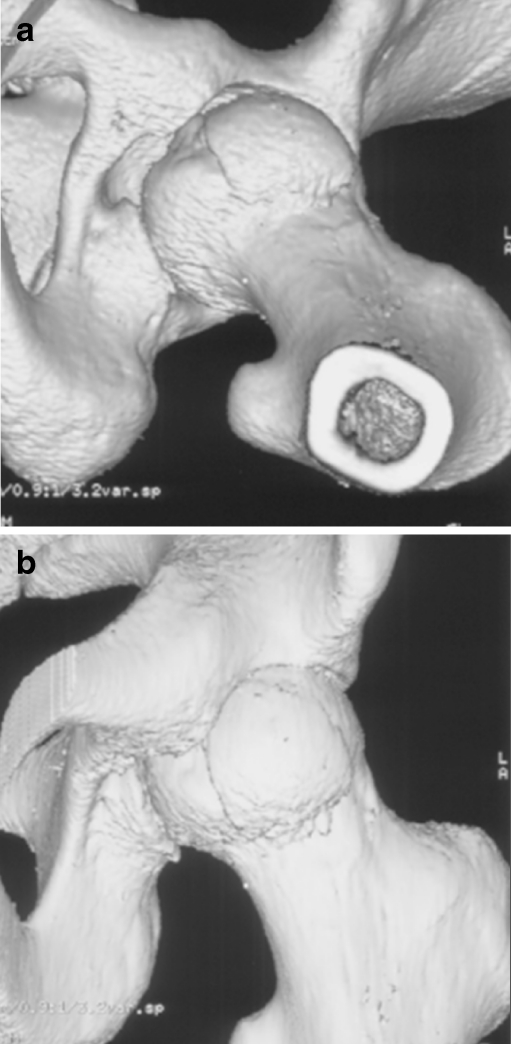
Fig. 8.
Preoperative 3D reconstructed images demonstrating a vertically oriented femoral head fracture extending above and below the fovea in the coronal plane
After the traumatic dislocation (11 days), the patient underwent a left hip surgical dislocation with fixation of the femoral head fracture and osteochondral autograft transplantation from the inferior aspect of the femoral head. Exposure was performed using a Kocher–Langenbeck incision and a surgical hip dislocation with a trochanteric osteotomy [12–14]. After performing a Z-shaped capsulotomy over the anterior aspect of the femoral neck, the hip was dislocated anteriorly. A large osteochondral fracture was appreciated measuring approximately 3 × 3 cm, which had been displaced distally and superiorly (Fig. 9). It was reduced into its anatomical position and fixed using three, 2.7 mm PLA Bionix screws (Bionix Incorporation, Toledo, OH, USA). Countersinking was performed to bring the screw heads just below the surface of the articular cartilage (Fig. 10). After the osteochondral fracture was stabilized, an area in the anterior-superior weight-bearing region of the femoral head, at the apex of the fragment just above the fovea, with exposed subchondral bone was noted. Several loose bony fragments were identified within the capsule and posterior labrum, and they were removed from the joint. In addition, a very small, posteroinferior avulsion fracture of the acetabular wall, approximately 6 mm × 1 cm, along with a small, posterioinferior tear of the labrum were appreciated. Both the avulsion fracture and labral tear were deemed to be too small to repair, and not clinically significant, and thus were excised. The remainder of the anterosuperior labrum was intact.
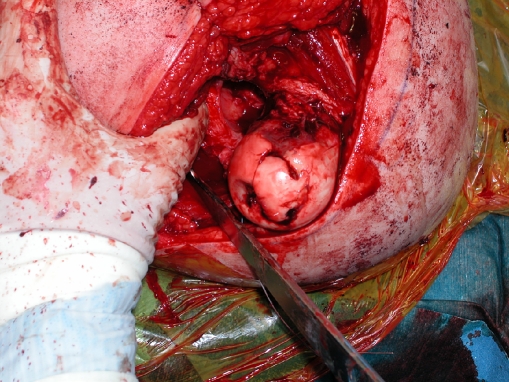
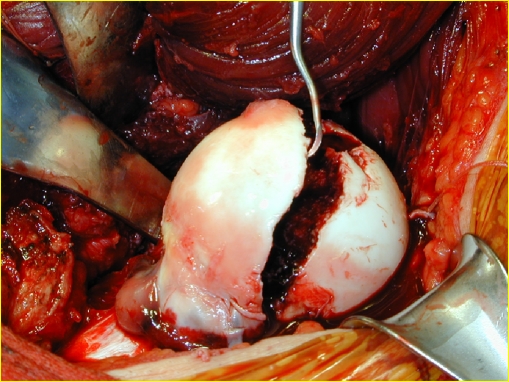
Fig. 9.
An intraoperative image demonstrating a large, Pipkin type II femoral head osteochondral fracture
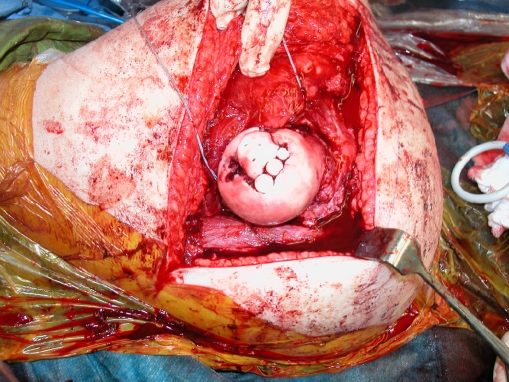
Fig. 10.
An intraoperative image demonstrating placement of a 2.7-mm PLA Bionix (Bionix Incorporation, Toledo, OH, USA) screw for fixation of the osteochondral fragment. Three screws were placed in total
At this point, the full-thickness cartilaginous injury at the apex of the fracture, in the anterior-superior weight-bearing zone of the femoral head, was debrided back to stable ridges. This zone of injury was approximately 10 mm in size, and it was determined that a 10 mm osteochondral plug would be suitable for repair. The recipient site was prepared using the Arthrex osteochondral autograft transplant system (Arthrex, Naples, FL, USA). One 10-mm plug was harvested from the most inferior, non-weight-bearing portion of the femoral head using the Arthrex osteochondral autograft transplant harvesting system.
The donor osteochondral plug was then transplanted to the area of full-thickness cartilage loss adjacent to the stabilized femoral head fracture. The donor plug was impacted into place, and a smooth articular contour was achieved after placement (Fig. 11). It was noted that on the most inferior portion of the large femoral head fragment, there was an area of residual cartilage injury with residual exposed bone, however no procedure was directed towards this region as it was located in the non-weight-bearing region of the joint. Of note, consistent bleeding from the femoral head was appreciated throughout the procedure.
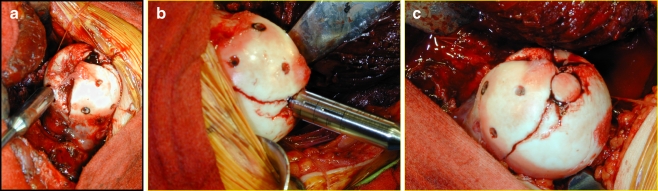
Fig. 11.
Intraoperative images demonstrating the zone of injury at the anterior-superior weight-bearing dome, and harvesting of the osteochondral autograft plug from the inferior aspect of the femoral head (a, b). An image demonstrating a smooth articular contour of the femoral head after impaction of the donor plug (c)
Post-operatively, the patient was kept non-weight-bearing for approximately 6 weeks, and then was gradually progressed to weight-bearing as tolerated. Physical therapy included cycling and swimming, and at 12 weeks post-operatively, the patient was able to ambulate with minimal pain and without assistance. Radiographs at that time demonstrated good preservation of the joint space and anatomic contour of the femoral head. Radiographs and a MRI performed at 1 year post-operatively demonstrated a well-incorporated autograft plug with minimal fibrillation and no evidence of osteonecrosis (Figs. 12 and 13). A slightly displaced anterior labral tear was present, but at over 5 years of follow-up, the patient continues to have no complaints of pain and has returned to his baseline physical activities without difficulty.
Fig. 12.
An AP pelvis radiograph at 1 year post-operatively demonstrating good preservation of the joint space and anatomic contour of the femoral head
Fig. 13.
Sagittal MRI image at 1 year post-operatively, demonstrating a well-incorporated autograft plug with no focal full-thickness defect and consistent cartilaginous signal and architecture throughout the femoral head
Discussion
OATS involves the transfer of small bone plugs covered with intact hyaline articular cartilage into focal chondral defects, which then heal to the surrounding recipient tissue [9, 15]. The goal is to remove healthy articular cartilage of non-weight-bearing portions of the knee and transplant them to more critical, weight-bearing regions of the affected joint. Since its introduction, OATS procedures have grown in popularity, as results have been promising. Horas et al. prospectively followed 40 patients following OATS procedures to the knee and demonstrated an increase in Lysholm knee score from approximately 29 pre-operatively to 72 post-operatively at 2 years follow-up [16]. Delcogliano et al. evaluated 24 patients in which osteochondral grafts were used to treat chondral lesions in the knee, and found 75% to have satisfactory results at average follow-up of 2.3 years [17]. Hangody et al. obtained far superior results, stating good-to-excellent results in 92% of patients at 10 years follow-up after OATS procedures to the knee [11]. Successful results, combined with the motivation to correct potentially debilitating chondral lesions, has led to the expansion of the use of OATS procedures in other surfaces such as the patella, tibia, talus, elbow (capitellum, trochlea, radial head), and even use in the metatarsal head has been described [18–20]. In this report, we presented two cases of a traumatic chondral defect to the femoral head, and the previously undescribed use of a surgical hip dislocation combined with an osteochondral autograft from the ipsilateral knee, and inferior aspect of the femoral head, to repair these lesions [12–14].
During a review of the literature, two separate reports were found to describe the use of osteochondral autograft transplants to the femoral head. Hangody et al. mentioned in their review that osteochondral transplant had been performed in six femoral heads. However, their technique and results from these procedures were not described [11]. Another case has been reported in which a 28-year-old man was found to have a deep osteochondral defect of the femoral head posteriorly, caused by joint penetration of a resorbable screw used in a prior ORIF of the acetabulum. The patient was treated with mosaicplasty to the femoral head, with autologous donor grafts taken from the lateral border of the lateral femoral condyle [21]. However, in contrast to our cases, this patient suffered a femoral head osteochondral defect after iatrogenic injury and malreduction of a posterior acetabular rim fracture. In addition, the patient presented with a defect in the posterior, non-weight-bearing portion of the femoral head. In the cases presented in this report, the indication for the procedure was a traumatic, focal chondral injury in the anterior-superior weight-bearing portion of the femoral head. Perhaps the most notable difference between the case reported by Hart et al. and ours was the surgical exposure utilized. Hart et al. recreated the initial approach utilized during the prior ORIF of the acetabular fragment: a Kocher–Langenbeck approach using a T-shaped posterior capsulotomy. It was noted that the defect on the posterior aspect of the femoral head could be visualized without the hip being dislocated, but the extent and location of their T-shaped capsulotomy was not described in detail. Thus, it is unclear how injuries to the deep branch of the medial femoral circumflex artery (MFCA) and the inferior gluteal artery were prevented. The risk of injury to this vital blood supply, as it penetrates the capsule at the level of the conjoint tendon, is high when using a posterior capsulotomy, thus increasing the risk of avascular necrosis in the future [22].
In our cases, a surgical dislocation was specifically used with the intent of preserving the blood supply and to fully expose the anterior-superior weight-bearing surface of the femoral head. The advantages of a surgical hip dislocation are that it provides a wide exposure to allow inspection of the entire femoral head and to treat concomitant labral or acetabular pathology, while minimizing the risk of avascular necrosis. Ganz et al. developed an operative technique in which full exposure of the femoral head could be obtained while avoiding division of the external rotator muscles and keeping the obturator externus intact, thus protecting the MFCA. Ganz et al. combined a posterior approach with a trochanteric flip osteotomy, exposing the hip anteriorly and dislocating in the same direction, while preserving the integrity of the external rotator muscles, and thus the blood supply to the femoral head. In 213 hips over a 7-year period, he reported no events of avascular necrosis using this procedure [12].
In the cases presented, utilizing this anterior surgical hip dislocation allowed preservation of the blood supply, which was confirmed intraoperatively, while providing full visualization of the femoral head. Obtaining full visualization of the femoral head allows greater accuracy in the placement of the donor graft and provides a more universal appreciation of articular conformity. During an OATS procedure, accurate placement of the autograft is essential, as chondrocyte loss can occur if the plug is placed slightly prominent, increasing the amount of shear at the interface between the donor plug and the recipient cartilage [23, 24]. Thus, utilization of a surgical hip dislocation during this procedure not only limits the risk of future avascular necrosis, but also provides increased accuracy during autograft placement.
Clinically, both patients are doing very well after their procedure, have no pain, full range of motion, and are able to ambulate independently without assistance and with good mechanics. Follow-up MRI studies have demonstrated good autograft incorporation with maintenance of articular surface conformity, and no significant complications have been noted at greater than 1 year follow-up and greater than 5 years of follow-up, respectively. In our opinion, treatment of osteochondral defects in the femoral head surface using a surgical dislocation combined with an OATS procedure is a promising approach, as full exposure of the femoral head can be obtained while preserving the vasculature to the femoral head, thus enabling adequate restoration of the articular cartilage surface. Future studies of a larger series of patients will further evaluate the effectiveness of this technique for traumatic osteochondral injury of the femoral head.
Acknowledgments
We would like to thank both Dr. Gregory R. Saboiero and Dr. Eric Bogner for their assistance in reviewing and preparing the images provided in this manuscript.
Footnotes
One author receives royalties from DePuy, Inc. (RLB), and one author is a paid consultant for Pivot Medical, Inc. (BTK). No other financial support was received for this study.
This report has received approval from the Institutional Review Board at the Hospital for Special Surgery.
References
- 1.Alford JW, Cole BJ. Cartilage restoration, part 2: Techniques, outcomes, and future directions. Am J Sports Med. 2005;33:443–460. doi: 10.1177/0363546505274578. [DOI] [PubMed] [Google Scholar]
- 2.Brittberg M, Lindahl A, Nilsson A, Ohlsson C, Isaksson O, Peterson L. Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med. 1994;331:889–895. doi: 10.1056/NEJM199410063311401. [DOI] [PubMed] [Google Scholar]
- 3.Steadman JR, Rodkey WG, Briggs KK. Microfracture to treat full-thickness chondral defects: Surgical technique, rehabilitation, and outcomes. J Knee Surg. 2002;15:170–176. [PubMed] [Google Scholar]
- 4.Alford JW, Cole BJ. Cartilage restoration, part 1: Basic science, historical perspective, patient evaluation, and treatment options. Am J Sports Med. 2005;33:295–306. doi: 10.1177/0363546504273510. [DOI] [PubMed] [Google Scholar]
- 5.Buckwalter JA, Mow VC, Ratcliffe A. Restoration of injured or degenerated articular cartilage. J Am Acad Orthop Surg. 1994;2:192–201. doi: 10.5435/00124635-199407000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Frisbie DD, Trotter GW, Powers BE, Rodkey WG, Steadman JR, Howard RD, Park RD, McIlwraith CW. Arthroscopic subchondral bone plate microfracture technique augments healing of large chondral defects in the radial carpal bone and medial femoral condyle of horses. Vet Surg. 1999;28:242–255. doi: 10.1053/jvet.1999.0242. [DOI] [PubMed] [Google Scholar]
- 7.Nehrer S, Spector M, Minas T. Histologic analysis of tissue after failed cartilage repair procedures. Clin Orthop Relat Res. 1999;365:149–162. doi: 10.1097/00003086-199908000-00020. [DOI] [PubMed] [Google Scholar]
- 8.Steadman JR, Briggs KK, Rodrigo JJ, Kocher MS, Gill TJ, Rodkey WG. Outcomes of microfracture for traumatic chondral defects of the knee: Average 11-year follow-up. Arthroscopy. 2003;19:477–484. doi: 10.1053/jars.2003.50112. [DOI] [PubMed] [Google Scholar]
- 9.Hangody L, Vasarhelyi G, Hangody LR, Sukosd Z, Tibay G, Bartha L, Bodo G. Autologous osteochondral grafting–technique and long-term results. Injury. 2008;39(Suppl 1):S32–9. doi: 10.1016/j.injury.2008.01.041. [DOI] [PubMed] [Google Scholar]
- 10.Kish G, Modis L, Hangody L. Osteochondral mosaicplasty for the treatment of focal chondral and osteochondral lesions of the knee and talus in the athlete. rationale, indications, techniques, and results. Clin Sports Med. 1999;18:45–66. doi: 10.1016/S0278-5919(05)70129-0. [DOI] [PubMed] [Google Scholar]
- 11.Hangody L, Fules P. Autologous osteochondral mosaicplasty for the treatment of full-thickness defects of weight-bearing joints: Ten years of experimental and clinical experience. J Bone Joint Surg Am. 2003;85-A(Suppl 2):25–32. doi: 10.2106/00004623-200300002-00004. [DOI] [PubMed] [Google Scholar]
- 12.Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124. doi: 10.1302/0301-620X.83B8.11964. [DOI] [PubMed] [Google Scholar]
- 13.Letournel E. of the acetabulum: A study of a series of 75 cases – les fractures du cotyle, etude d’une serie de 75 cas. J de chirurgie 82:47–87, 1961. (translated and substantially abridged) J Orthop Trauma. 2006;20:S15–9. [PubMed] [Google Scholar]
- 14.Gardner MJ, Suk M, Pearle A, Buly RL, Helfet DL, Lorich DG. Surgical dislocation of the hip for fractures of the femoral head. J Orthop Trauma. 2005;19:334–342. [PubMed] [Google Scholar]
- 15.Kish G, Hangody L. A prospective, randomised comparison of autologous chondrocyte implantation versus mosaicplasty for osteochondral defects in the knee. J Bone Joint Surg Br. 2004;86:619. [PubMed] [Google Scholar]
- 16.Horas U, Pelinkovic D, Herr G, Aigner T, Schnettler R. Autologous chondrocyte implantation and osteochondral cylinder transplantation in cartilage repair of the knee joint. A prospective, comparative trial. J Bone Joint Surg Am. 2003;85-A:185–192. doi: 10.2106/00004623-200302000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Delcogliano A, Caporaso A, Menghi A, Rinonapoli G, Chiossi S. Results of autologous osteochondral grafts in chondral lesions of the knee. Minerva Chir. 2002;57:273–281. [PubMed] [Google Scholar]
- 18.Ansah P, Vogt S, Ueblacker P, Martinek V, Woertler K, Imhoff AB. Osteochondral transplantation to treat osteochondral lesions in the elbow. J Bone Joint Surg Am. 2007;89:2188–2194. doi: 10.2106/JBJS.F.00299. [DOI] [PubMed] [Google Scholar]
- 19.Tsujii M, Hasegawa M, Hirata H, Uchida A. Subchondral insufficiency fracture of the second metatatarsal head in an elderly woman treated with autologous osteochondral transplantation. Arch Orthop Trauma Surg. 2008;128:689–693. doi: 10.1007/s00402-007-0381-0. [DOI] [PubMed] [Google Scholar]
- 20.Wahegaonkar AL, Doi K, Hattori Y, Addosooki A. Technique of osteochondral autograft transplantation mosaicplasty for capitellar osteochondritis dissecans. J Hand Surg Am. 2007;32:1454–1461. doi: 10.1016/j.jhsa.2007.08.016. [DOI] [PubMed] [Google Scholar]
- 21.Hart R, Janecek M, Visna P, Bucek P, Kocis J. Mosaicplasty for the treatment of femoral head defect after incorrect resorbable screw insertion. Arthroscopy. 2003;19:E1–5. doi: 10.1016/S0749-8063(03)00525-5. [DOI] [PubMed] [Google Scholar]
- 22.Gautier E, Ganz K, Krugel N, Gill T, Ganz R. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br. 2000;82:679–683. doi: 10.1302/0301-620X.82B5.10426. [DOI] [PubMed] [Google Scholar]
- 23.Cain EL, Clancy WG. Treatment algorithm for osteochondral injuries of the knee. Clin Sports Med. 2001;20:321–342. doi: 10.1016/S0278-5919(05)70309-4. [DOI] [PubMed] [Google Scholar]
- 24.Hunziker EB, Quinn TM. Surgical removal of articular cartilage leads to loss of chondrocytes from cartilage bordering the wound edge. J Bone Joint Surg Am. 2003;85-A(Suppl 2):85–92. doi: 10.2106/00004623-200300002-00011. [DOI] [PubMed] [Google Scholar]