Abstract
With the improvements in flexible instrumentation, hip arthroscopy is being increasingly used to treat a variety of hip pathology, including labral tears. However, up to this point, there has not been a case report of an anterior and a posterior labral tear successfully repaired arthroscopically. We present a case report of a 27-year-old male firefighter who presented to our institution with an anterior and posterior labral tear, as well as a cam lesion and loose body, following a traumatic hip dislocation. The purpose of this case report is to illustrate that both anterior and posterior labral tears can be repaired using hip arthroscopy. Anterior and posterior labral tears can be caused by a traumatic hip dislocation, and both can be successfully repaired using arthroscopic techniques.
Keywords: anterior, posterior, hip, labral tear, traumatic dislocation, arthroscopy repair
Introduction
Recently, with the improvement in flexible instrumentation in hip arthroscopy and due to the advancement of imaging modalities, hip arthroscopy has become increasingly utilized to treat various hip lesions, including labral tears. Robertson et al. performed a systematic review of the literature to determine patient satisfaction following arthroscopically managed labral tears and concluded that arthroscopic debridement of labral tears resulted in a patient satisfaction rate of approximately 67% at 3.5 years follow-up, and 50% of all patients had resolution of their mechanical symptoms [7]. Kelly et al. has described the surgical technique for arthroscopic labral repair [6]. However, all the previously reported literature has described arthroscopic repairs of anterior labral tears. We describe, in this case report, an anterior and a posterior labral tear following a traumatic hip dislocation that were both repaired arthroscopically with suture anchors.
Case report
A 27-year-old African-American male firefighter presented to our clinic 5 months after sustaining a right posterior hip dislocation while playing football. He was initially treated at an outside institution with closed reduction 2 h after the injury. He used crutches and was non-weight bearing for approximately 1 month. He had an magnetic resonance imaging (MRI) performed 1 month after the injury was sustained, and there was no evidence of osteonecrosis, so he was gradually weaned from his crutches and returned to full duty as a firefighter.
However, the patient continued to have intermittent groin pain, and what he perceived as instability of the hip with certain activities, such as when he tried to start running or during pivoting maneuvers. He continued to attend physical therapy, and his symptoms improved to the point that he was able to play in a recreational basketball league with minimal symptoms. However, his symptoms progressively worsened following a minor, atraumatic re-injury and limited him from participating in basketball and other recreational activities, prompting presentation to our institution for evaluation of his hip pain.
On initial physical exam, he walked with a non-antalgic gait and had a negative Trendelenberg sign. He had a negative Thomas test and could forward flex his hips to 120° bilaterally. He had 10° of internal rotation of his right hip compared to 15° in his left hip. External rotation of both hips was symmetric, and measured approximately 45°. He was nontender to palpation along his adductors, his rectus femoris, and the greater trochanter. He had pain with flexion and internal rotation of his right hip and had very minimal pain with the posterior apprehension test. He had no pain to anterior apprehension or to resisted hip flexion. Straight leg raise was negative. He had 5/5 hip abduction and adduction strength, in addition to 5/5 strength in extensor hallucis longus, tibialis anterior, and gastroc-soleus complex.
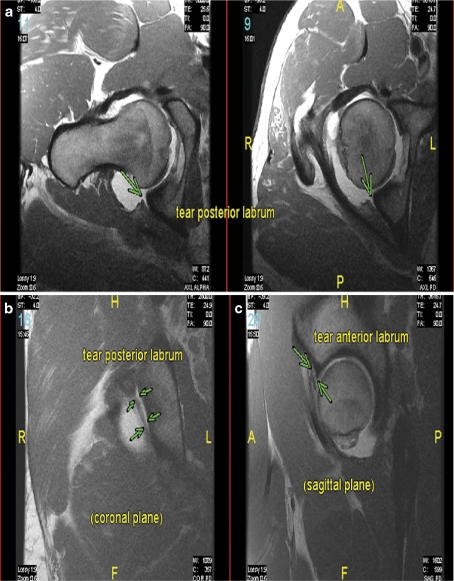
Radiographs taken from an outside institution demonstrated an os acetabuli on the right side [20], and a cross-over sign consistent with cephalad retroversion of the acetabulum. Extended long neck lateral (aka Dunn lateral), performed with the hip in 90° of flexion and 20° of abduction, showed evidence of cam impingement. A non-arthrogram MRI showed an anterior labral tear, as well as a posterior labral tear with capsular labral disruption, with a large effusion. Based on our initial assessment, we obtained a magnetic resonance arthrogram to further evaluate his posterior labral structures and to see if there was associated capsular attenuation or rupture. The MR arthrogram demonstrated findings consistent with a previous hip dislocation with a large tear of the posterior labrum with partially detached anterior and superior labrum as well (Fig. 1a-c). There was a femoral dysplastic bump arising from the anterior aspect of the femoral head/neck junction with an elevated alpha angle measuring 64° and a femoral anteversion angle of 5°. He also had evidence of pincer impingement and a loose body as well. In addition, he had a shearing injury to the cartilage of his femoral head. Given his radiographic findings and persistent symptoms, he was taken to the operating room for arthroscopic anterior labral repair with cam decompression, as well as a posterior labral repair with removal of the loose body.
Fig. 1.
a-c MR Arthrogram. a Oblique axial images were obtained, which demonstrated a torn posterior labrum (green arrows). b Coronal images also demonstrate the torn posterior labrum. c The sagittal images show a torn anterior labrum as well (green arrows)
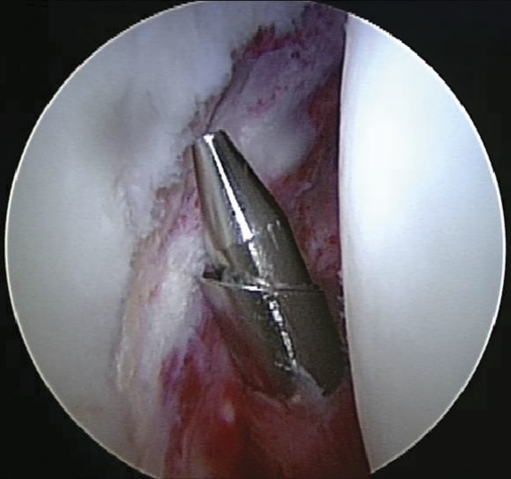
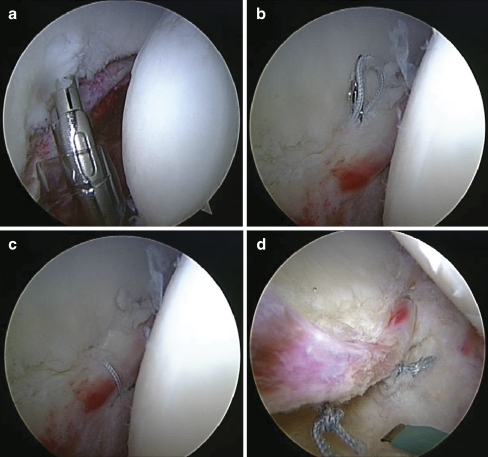
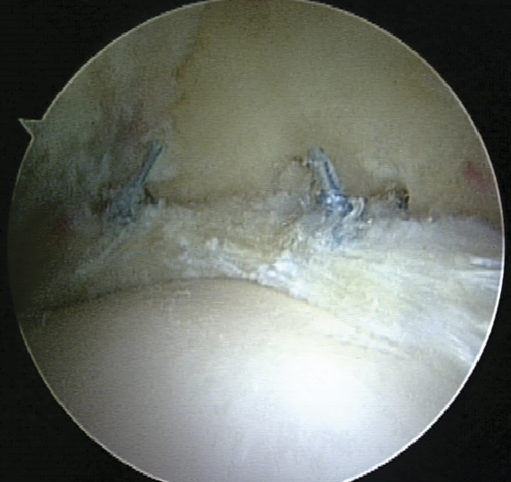
The patient was brought to the operating room and placed in the supine position on the fracture table and routine arthroscopy was performed as described by Byrd et al. [8]. A lateral portal was first established under fluoroscopic guidance, and then, using the Seldinger technique, a mid-anterior (midpoint between the classic anterolateral and anterior portals) [22] and posterior portal was established. A distal anterolateral accessory portal was also established. Arthroscopic examination of the central compartment demonstrated a full thickness cartilage lesion. The anterior aspect of femoral head had the appearance of a reverse Hill-Sachs lesion. There was a complete posterior labral tear with detachment of the posterior acetabulum, with attenuation of the capsule posteriorly as well (Fig. 2). There was also associated synovitis anterosuperiorly and posteriorly. A synovectomy was first performed. Then, the labrum was repaired sequentially starting with the posteroinferior most labrum (Fig. 3a-d), working up towards the anterosuperior labrum (Fig. 4). Four suture anchors were placed sequentially in the rim of the acetabulum through the distal anterolateral accessory portal. The distal location of this portal allows for a more anatomic placement of the anchor closer to the acetabular rim without concern for penetration into the joint. Placement of the posterior anchors was performed by viewing through the mid-anterior portal and passing sutures through the lateral portal. Placement of the more anterior anchors was performed by viewing through the lateral portal and passing sutures through the mid-anterior portal. There was an acetabular rim lesion anterosuperiorly, which was removed, and the rim was shaved down to a normal contour towards active delamination of the anterosuperior weight-bearing transition zone, which was debrided back to a stable ridge using a biter. The ligamentum teres was then debrided. We then moved to the peripheral compartment. A T-capsulotomy was performed at the most prominent portion of the cam lesion and then a cam decompression was performed (Fig. 5). The cartilage shear injury from the femoral head was identified in the peripheral compartment as well as a large loose body measuring 2 × 1 cm, which was removed. Both fluoroscopic and dynamic arthroscopy was then used to confirm the restoration of normal offset that was restored at the junction between the femoral head and neck. There was no further impingement; however, there was some posterior subluxation when the hip was flexed beyond 70° presumably due to persistent capsular laxity. The portals were removed, and patient was taken to the recovery room without any complications.
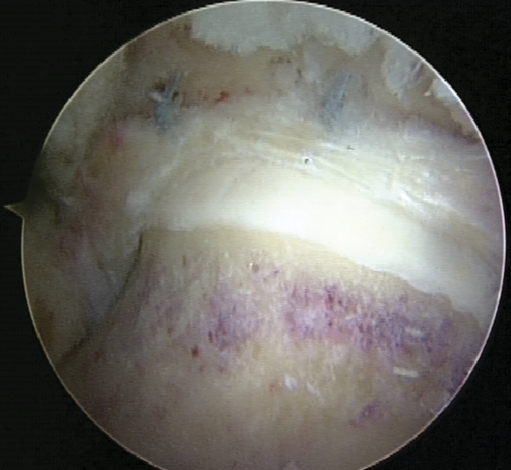
Fig. 2.
Arthroscopic image of the right hip, viewing through the midanterior portal, demonstrating the posterior labral tear
Fig. 3.
a Posterior labral repair shows placement of the suture anchor. b Suture passage was performed. c Standard arthroscopic knot tying was performed through a cannula. d A total of four suture anchors were placed and a final postoperative image was obtained
Fig. 4.
Anterior labral repair using suture anchor technique
Fig. 5.
Arthroscopic view in the peripheral compartment status post osteoplasty
Postoperatively, he was initially placed in a brace with crutches; however, given his subluxation with extreme flexion, we did not start him on the CPM or the bike. On postoperative day 10, the brace was removed with the instruction to avoid extremes of flexion to allow for tightening of the posterior capsule. However, he was kept on crutches for a total of 4 weeks. At his 6 month follow-up, he had returned to near-full activity, including running and had minimal pain with no further instability episodes.
Discussion
The labrum is triangular fibrocartilage that lies circumferentially around the acetabular perimeter and becomes attached to the transverse acetabular ligament posteriorly and anteriorly [5]. The majority of case series in North America describe anterior labral tears, and the mechanism is usually an external force that is applied to a hyper-extended and externally rotated hip [5]. There are multiple etiologies for labral tears of the hip including femoroacetabular impingement, trauma, dysplasia, osteoarthritis, psoas impingement, and hip instability. Traumatic hip instability is a spectrum ranging from hip subluxation to dislocation with or without associated injuries. Hip dislocation is most common after motor vehicle accidents, but has also been described in sports including dancing, football, soccer, basketball, skiing, biking, gymnastics, and rugby [14]. The usual mechanism for dislocation during sports is a forward fall on the knee while the hip is flexed or a blow from behind, while the athlete is down on all four limbs [14]. A posterior labral tear is usually associated with a hip dislocation and, in our experience, anterior labral tears occur as well [14].
Because of the labrum’s relative avascularity, in theory, it has a relatively low healing potential when it is torn [5]. Thus, until recently, labral tears were most commonly treated with partial limbectomy and debridement, with good results reported. Robertson et al. performed a systematic review on patients with symptomatic labral tears that were managed by arthroscopic debridement, and found that the patient satisfaction rate is approximately 67% at 3.5 years follow-up [7]. On the other hand, some authors argue that by removing the acetabular labrum, one alters the normal physiology and stability of the hip joint, and several authors have even showed an association between labral tears and the early onset of osteoarthritis [15–17]. As a result, some authors now advocate developing repair strategies for labral tears, especially peripheral tears which have been shown to have the highest vascularity [13]. To examine the healing potential of the acetabular labrum, Philipon et al. studied ten sheep, which underwent arthroscopic labral repair using a single-suture anchor, and showed histologic evidence of healing by fibrovascular repair tissue and/or direct reattachment through new bone formation [11].
The technique of arthroscopic labral repair in humans has been described in the literature [6, 12] and has recently been advocated for treatment of labral tears. Kelly et al. described the technique for labral repair using suture anchors. At this time, the long-term outcomes after labral repair are not known. However, Heyworth et al. showed an association between failed labral repair and failure to address impingement lesions [9]. In fact, in that paper, he reviewed 24 revision hip arthroscopy cases and found 19/24 patients who failed initial repair had an untreated or undertreated bony impingement lesions. Our patient had a cam impingement lesion and an alpha angle of 64°. Thus, a cam decompression osteoplasty was performed. Although there is no data at this time, it is our hypothesis that a cam lesion may actually predispose a patient to hip dislocation, in that the lesion serves as lever when the hip is flexed. Further biomechanics research will be required to prove this hypothesis.
This is the first report of an article describing the technique of arthroscopic anterior and posterior labral repairs. Part of this is due to the fact that many times, the posterior labral tear heals, as it is often associated with a bony posterior acetabular rim fracture [21]. However, this patient did not have a posterior acetabular lip fracture and a complete capsular disruption had occurred, which may have accounted for the lack of healing. In addition, his cam lesion and ligamentum teres injury may have led to continued instability, which may also explain the persistent posterior labral tear. Pain after a traumatic hip dislocation may have several etiologies including labral tears, articular cartilage injury, ligamentum teres disruption, loose bodies, etc. The patient described in this case report had continued pain after an extensive trial of non-operative treatment. We describe the first report of an arthroscopic anterior and posterior labral repair using suture anchors in combination with a cam decompression with successful results in the short term. Long-term follow-up is required. In addition, one should investigate whether cam lesions are a predisposing risk factor for posterior hip dislocations.
Footnotes
Dr. Kelly is a consultant for Pivot Medical and an Educational Advisor for Smith and Nephew. Dr. Cross and Dr. Shindle have nothing to disclose
Each author certifies that his or her institution has approved the reporting of this case and that all investigations were conducted in conformity with ethical principles of research.
Level of evidence: IV
References
- 1.Giza E, Mithofer K, Matthews H, et al. Hip fracture dislocation in football: a report of two cases and review of the literature. Br J Sports Med. 2004;38(4):E17. doi: 10.1136/bjsm.2003.005736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lamke LO. Traumatic dislocations of the hip. Follow-up on cases from the Stockholm area. Acta Orthop Scand. 1970;41(2):188–198. doi: 10.3109/17453677008991506. [DOI] [PubMed] [Google Scholar]
- 3.Mitchell JC, Giannoudis PV, Millner PA, et al. A rare fracture dislocation of the hip in a gymnast and review of the literature. Br J Sports Med. 1999;33(4):283–284. doi: 10.1136/bjsm.33.4.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chudik S, Lopez V. Hip dislocations in athletes. Sports Med Arthrosc Rev. 2002;10:123–133. doi: 10.1097/00132585-200210020-00004. [DOI] [Google Scholar]
- 5.Kelly BT, Williams RJ, III, Philippon MJ. Hip arthroscopy: current indications, treatment options, and management issues. Am J Sports Med. 2003;31(6):1020–1037. doi: 10.1177/03635465030310060701. [DOI] [PubMed] [Google Scholar]
- 6.Kelly BT, Weiland DE, Schenker ML, Philippon MJ. Arthroscopic labral repair in the hip: surgical technique and review of the literature. Arthroscopy. 2005;21:1496–1504. doi: 10.1016/j.arthro.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 7.Robertson WJ, Kadrmas WR, Kelly BT. Arthroscopic management of labral tears in the hip: a systematic review of the literature. Clin Orthop Relat Res. 2007;455:88–92. doi: 10.1097/BLO.0b013e31802c7e0f. [DOI] [PubMed] [Google Scholar]
- 8.Byrd JW, Jones KS. Hip arthroscopy in athletes. Clin Sports Med. 2001;20:749–761. doi: 10.1016/S0278-5919(05)70280-5. [DOI] [PubMed] [Google Scholar]
- 9.Heyworth BE, Shindle MK, Voos JE, Rudzki JR, Kelly BT. Radiologic and intraoperative findings in revision hip arthroscopy. Arthroscopy 2007;(12) 1295–1302. [DOI] [PubMed]
- 10.Lage LA, Patel JV, Villar RN. The acetabular labral tear: an arthroscopic classification. Arthroscopy. 1996;12:269–272. doi: 10.1016/S0749-8063(96)90057-2. [DOI] [PubMed] [Google Scholar]
- 11.Philippon MJ, Arnoczky SP, Torrie A. Arthroscopic repair of the acetabular labrum: a histologic assessment of healing in an ovine model. Arthroscopy. 2007;23(4):376–380. doi: 10.1016/j.arthro.2007.01.017. [DOI] [PubMed] [Google Scholar]
- 12.Murphy KP, Ross AE, Javernick MA, Lehman RA. Repair of the adult acetabular labrum. Arthroscopy. 2006;22:567.e1–567.e3. doi: 10.1016/j.arthro.2005.07.033. [DOI] [PubMed] [Google Scholar]
- 13.Petersen W, Petersen F, Tillmann B. Structure and vascularization of the acetabular labrum with regard to the pathogenesis and healing of labral lesions. Arch Orthop Trauma Surg. 2003;123:283–288. doi: 10.1007/s00402-003-0527-7. [DOI] [PubMed] [Google Scholar]
- 14.Shindle MK, Voos JE, Nho SJ, Heyworth BE, Kelly BT. Arthroscopic management of labral tears in the hip. J Bone Joint Surg. 2008;90:2–19. doi: 10.2106/JBJS.H.00686. [DOI] [PubMed] [Google Scholar]
- 15.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingment: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 16.McCarthy JC, Noble PC, Schuck MR, Wright J, Lee J. The role of labral lesions to the development of early degenerative hip disease. Clin Orthop Relat Res. 2001;393:25–37. doi: 10.1097/00003086-200112000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Tanzer M, Noiseux N. Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clin Orthop Relat Res. 2004;429:170–177. doi: 10.1097/01.blo.0000150119.49983.ef. [DOI] [PubMed] [Google Scholar]
- 18.Paterson I. The torn acetabular labrum; a block to reduction of a dislocated hip. J Bone Joint Surg Br. 1957;39:306–309. doi: 10.1302/0301-620X.39B2.306. [DOI] [PubMed] [Google Scholar]
- 19.Stiris MG. Magnetic resonance arthrography of the hip joint in patients with suspected rupture of the labrum acetabulare. Tidsskr Nor Laegeforen. 2001;121:698–700. [PubMed] [Google Scholar]
- 20.Manaster BJ, Zakel S. Imaging of femoral acetabular impingement syndrome. Clin Sports Med. 2006;25(4):635–657. doi: 10.1016/j.csm.2006.06.012. [DOI] [PubMed] [Google Scholar]
- 21.Moorman CT, 3rd, Warren RF, Hershman EB, Crowe JF, Potter HG, Barnes R, O'Brien SJ, Guettler JH. Traumatic posterior hip subluxation in American football. JBJS Am. 2003;85-A(7):1190–1196. doi: 10.2106/00004623-200307000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Robertson WJ, Kelly BT. The safe zone for hip arthroscopy: a cadaveric assessment of central, peripheral, and lateral compartment portal placement. Arthroscopy. 2008;24(9):1019–1026. doi: 10.1016/j.arthro.2008.05.008. [DOI] [PubMed] [Google Scholar]