Abstract
Implants designed for enhanced flexion offer the prospect of improved function after total knee replacement (TKR). Whereas most studies evaluating these implants have focused on the range of knee flexion achieved, this study investigated the quality of function in deep knee flexion. The influences of residual pain and maximum flexion angle on function in deep knee flexion were also examined. Eighty-three patients (100 knees) were prospectively followed for 1 year after TKR with a rotating-platform posterior-stabilized high-flexion prosthesis. Range of motion was measured and Knee Society scores were calculated. A questionnaire evaluated residual knee pain and function in high-flexion activities. Mean Knee Society score was 95, and mean knee flexion was 125°, yet 20% of patients could neither kneel, nor squat, nor sit on their heels. Fifty-seven percent were able to kneel without significant difficulty; 69% were able to squat without significant difficulty; and 46% were able to sit on their heels without significant difficulty. Function in deep flexion correlated with pain scores but did not correlate with knee flexion angles or Knee Society scores. Results 1 year after TKR with a rotating-platform posterior-stabilized high-flexion prosthesis are encouraging, but one in five patients remain significantly limited in high-flexion activities.
Keywords: functional outcome, high flexion, mobile bearing, patient satisfaction, rotating platform, total knee arthroplasty
Introduction
The success and durability of primary total knee replacement (TKR) have encouraged broadening indications, including the use of TKR in patients who are young and active and in those who have significant pain but relatively preserved motion. The inability of traditional prosthetic knees to consistently achieve flexion beyond 115° [1–8] raises concerns about functional limitations in these more demanding patients. Desire for improved function has encouraged innovation in prosthetic design, resulting in a new generation of “high-flexion” knee replacements. In turn, marketing by surgeons and implant manufacturers has amplified patient demand for these “high-performance” knee replacements.
The majority of studies evaluating high-flexion knee prostheses [9–13] have focused on measuring the degree of knee flexion obtained, rather than directly evaluating knee function in deep-flexion activities. Although high-flexion designs may improve functional outcomes for some patients [14], this has not been consistently demonstrated [15–17]. The availability of these implants may give surgeons and patients false hopes and expectations about the performance of prosthetic knees in high-demand and high-flexion activities. Unmet expectations may ultimately lead to dissatisfaction with the surgical outcome [18]. Furthermore, the RP-F is a new prosthesis with few published results. One-year follow-up is not sufficient to support positive statements of safety and efficacy after TKR, but in light of a recent report of premature failures with another high-flexion prosthesis [19], an audit for unexpected adverse outcomes with this design seems warranted. Finally, although changes in implant design have focused attention on improving maximum knee flexion, previous studies have questioned the influence of maximum knee flexion angle on function after TKR [20, 21], implicating a more important role for residual knee pain.
The primary goal of this study was to document the quality of pain relief and function achieved 1 year after TKR using the PFC Sigma RP-F prosthesis (DePuy Orthopedics, Inc., Warsaw, IN, USA), which incorporates a posterior-stabilized, rotating-platform, high-flexion design. Particular attention was given to evaluating function in activities requiring deep knee flexion. The second goal of this study was to investigate the safety and efficacy of this new prosthesis at short-term follow-up using standard Knee Society clinical and radiographic criteria, including range of motion. The third goal of this study was to measure any association between knee function in deep-flexion activities and either knee flexion angle or residual knee pain. The final goal of this study was to determine whether the Knee Society Score [22], a score that was developed when arthroplasty patients typically presented with lower functional demands, is an appropriate tool for assessing the results of “high-performance” knee replacements. Specifically, we question whether Knee Society scores of 99 or 100 underestimate difficulty of performing demanding recreational or high-flexion activities.
Materials and methods
Approval for this prospective study was granted by the hospital Institutional Review Board. Patients scheduled to have TKR performed by the senior author (CSR) were offered the RP-F prosthesis and invited to participate in the study. Exclusion criteria were severe biplanar deformity, preoperative knee flexion less than 60°, lack of available implants or instrumentation, patient refusal to participate in the study, and inability of the research team to contact the patient prior to surgery. During the study period, the senior author performed primary TKR on 298 patients. One hundred of these patients received the new prosthesis and were enrolled in the study. Only one set of high-flexion instruments was available at our hospital when this implant was initially introduced, so lack of available instrumentation was the most common reason for patient exclusion. Of the 100 patients initially enrolled in the study, ten later declined to fill out study instruments; three lived or moved abroad and did not return for clinical evaluation; and another four were lost to follow-up, leaving 83 subjects (50 female, 33 male) with minimum 1-year clinical and radiographic follow-up. Mean age was 68 years (range 47–84), which was similar to the mean age (69 years) of all patients undergoing TKR in the senior author’s practice during the enrollment period. Sixty percent of study patients were female, and 40% were male. This was no different from the gender distribution for patients receiving other TKR implants during the study period. Preoperative diagnosis was degenerative joint disease in all patients. Seventeen patients received bilateral TKR; thus, 100 knees were available for analysis.
The surgical procedure was standardized using a medial parapatellar approach. The soft tissues were handled with care to avoid unnecessary trauma; however, no specific effort was made to limit or monitor the length of the incision. Patellar resurfacing was uniformly performed. Regional anesthesia and periarticular soft tissue injection was used to limit postoperative pain, and a standardized perioperative pain control and physical therapy regimen was utilized [23].
Clinician assessment of the surgical outcome was performed by an arthroplasty fellow (VS) or an orthopedic physician assistant (JW) during routine clinical examination at minimum 1-year follow-up. Range of motion was measured utilizing a goniometer; maximum passive flexion was recorded, as was any flexion contracture greater than 5°. Knee Society scores [22] were calculated using a standardized form. All complications were noted. These assessments were not formally blinded. Weight-bearing radiographs with careful control of knee rotation were performed on 12 by 18-in. digital cassettes and reviewed for coronal alignment and presence of radiolucent lines [24] by one of two orthopedic trainees (MH, VS) who were blinded to clinical results at the time of radiographic assessment. Alignment was measured using the angle tool on the digital imaging software.
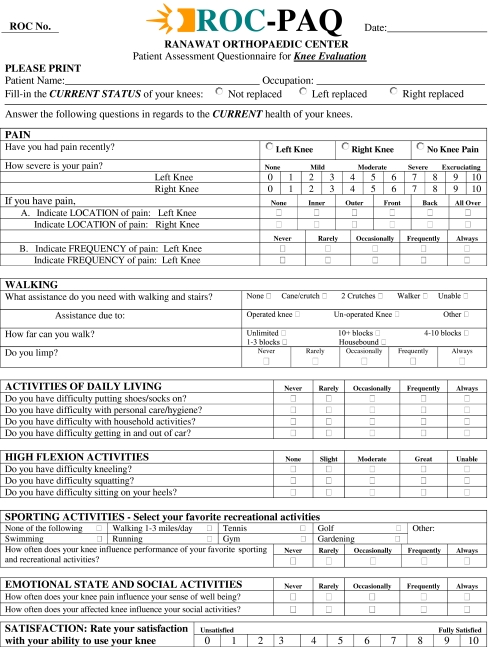
Patients were asked to complete a patient assessment questionnaire (PAQ) [25] at minimum 1-year postoperatively (Fig. 1). The PAQ was given to patients on the day of clinical assessment. If the PAQ was not returned promptly, a second copy was mailed to the patient and followed up with telephone calls as needed to encourage completion and return of the questionnaire. The PAQ was designed to measure pain, walking ability, function in low-demand activities, function in high-demand activities, function in deep-flexion activities, and overall patient satisfaction. Visual analog pain scores of 0 or 1 were considered no pain; scores of 2 or 3 were considered mild pain; scores of 4–6 were considered moderate pain; scores of 7 or 8 were considered severe pain; and scores of 9 or 10 were considered excruciating pain. Patients who scored their satisfaction 0–4 were considered dissatisfied, whereas those who scored their satisfaction 5–10 were considered satisfied. Formal validation of a modified version of the PAQ is currently underway, but we believe this instrument has high face validity.
Fig. 1.
The Patient Assessment Questionnaire (PAQ) measured the surgical outcome as perceived by the patient. The version shown here has been reformatted to display on a single page, but the questions are unchanged
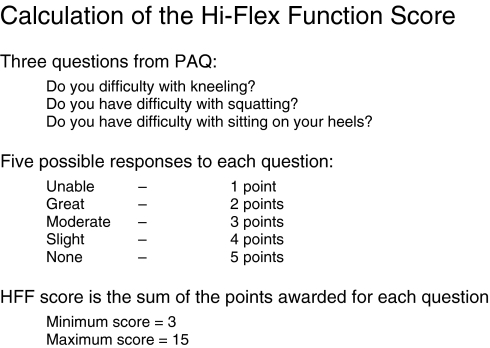
To simplify data analysis, a novel composite Hi-Flex Function (HFF) score (see Fig. 2) was generated combining the results of PAQ questions regarding kneeling, squatting, and sitting on heels. The minimum score of 3 reflected the inability to perform any of the three activities, whereas the maximum score of 15 reflected the ability to perform all three activities without difficulty. The purpose of this construct was to generate a single variable representing knee function in high-flexion activities, facilitating analysis of parameters that might correlate with function in deep flexion.
Fig. 2.
The Hi-Flex Function Score is calculated using patient responses to PAQ queries about three designated high-flex functions. Each activity is graded from 1 to 5 and the score for the three activities is summed. The minimum possible score is three, and the maximum possible score is 15
Pearson correlations and one-way ANOVA were used to screen for factors potentially associated with HFF score. Multivariate analysis was then utilized to determine the relative importance of these factors. Statistical significance was set a priori at p < 0.05.
Results
The PAQ revealed a broad spectrum of patient outcomes, ranging from modest improvement with persistent pain and disability to complete relief of pain with return to impairment-free function in demanding recreational and high-flexion activities. Patients reported moderate pain in 16% of operated knees and severe pain in 4% (see Table 1). Pain, when present, was most commonly localized to the anterior aspect of the knee, with 8% experiencing moderate anterior knee pain and 2% experiencing severe anterior knee pain. Routine activities of daily living were performed without difficulty by the vast majority of patients (see Table 2). High-demand and deep-flexion functions were achieved by many, but residual difficulty with these activities was common. Eighty percent of patients reported participating in one or more demanding recreational activities after TKR (see Table 3). Sixty-three percent of patients reported that their prosthetic knee rarely affected performance of these demanding activities, whereas 22% reported that the knee was limiting frequently or always (see Table 4). Function in deep flexion (see Table 5) was as follows: 57% were able to kneel without significant difficulty; 69% were able to squat without significant difficulty; and 46% were able to sit on their heels without significant difficulty. Nearly 80% of patients were able to perform at least one of these three high-flexion activities without significant difficulty.
Table 1.
Persistent knee pain
| How severe is your pain? | None | Mild | Moderate | Severe | Excruciating |
|---|---|---|---|---|---|
| Any pain | 62% | 18% | 16% | 4% | 0% |
| Anterior knee pain | 80% | 10% | 8% | 2% | 0% |
Table 2.
Function in daily life
| Do you have difficulty with | None | Slight | Moderate | Great | Unable |
|---|---|---|---|---|---|
| Putting on shoes and socks? | 57% | 23% | 17% | 1% | 2% |
| Personal care activities? | 72% | 14% | 12% | 1% | 0% |
| Household activities? | 52% | 24% | 18% | 1% | 5% |
| Getting in and out of a car? | 36% | 22% | 29% | 6% | 7% |
Table 3.
Favorite recreational activities
| Activity | Percent of patients participating |
|---|---|
| Swimming | 24% |
| Walking distances > 1 mile | 39% |
| Running | 2% |
| Tennis | 9% |
| Exercise at the gym | 20% |
| Golf | 17% |
| Gardening | 15% |
| Other activities | 9% |
| None of the above | 20% |
Table 4.
Social and recreational function
| How often does your knee influence | Never | Rarely | Occasionally | Frequently | Always |
|---|---|---|---|---|---|
| Your sense of well-being? | 45% | 23% | 19% | 7% | 6% |
| Your social activities? | 49% | 27% | 11% | 8% | 5% |
| Performance of your favorite sporting and recreational activities? | 35% | 28% | 16% | 11% | 11% |
Table 5.
Function in deep knee flexion
| Do you have difficulty with | None | Slight | Moderate | Great | Unable |
|---|---|---|---|---|---|
| Kneeling? | 18% | 22% | 17% | 14% | 29% |
| Squatting? | 14% | 27% | 28% | 7% | 24% |
| Sitting on your heels? | 13% | 14% | 18% | 14% | 40% |
One year after surgery, the safety and efficacy of the PFC Sigma RP-F prosthesis appeared comparable to previous implants, with no unexpected adverse outcomes or events. Traditional surgeon-derived outcome measures revealed substantial improvements from the preoperative state (see Table 6). Preoperatively, 45% of knees flexed beyond 120°, whereas postoperatively 81% flexed beyond 120° and 44% flexed beyond 130°. No patient had a flexion contracture greater than 5°. Mean coronal alignment of the tibial component was 90° (range 87–93°, standard deviation 1.6), and mean coronal alignment of the femur was 5.3° of valgus (range 3–8° of valgus, standard deviation 1.1°). Mean tibiofemoral valgus angle was 5.3° (range 3–7°, standard deviation 1.0°). There were no circumferential or progressive radiolucent lines and no other radiographic signs of compromised fixation. There were two surgical complications. One patient underwent manipulation under anesthesia for arthrofibrosis, obtaining range of motion from 5° of flexion to 105° of further flexion at 1-year follow-up. One patient underwent reoperation for anterior knee pain—no cause was identified at surgery, and the patient reported no amelioration of her symptoms. There were no other reoperations, no infections, and no cases of instability or fixation failure.
Table 6.
Objective results
| Preop | Postop | |
|---|---|---|
| Mean knee flexion in degrees (range) | 111° (60–130°) | 125° (90–150°) |
| Mean Knee Society Knee Score (range) | 56 (19–79) | 95 (69–100) |
| Mean Knee Society Function Score (range) | 59 (15–100) | 91 (35–100) |
Function in deep flexion correlated with visual analog scale (VAS) pain scores, but not with postoperative knee flexion angle. Surprisingly, patients with flexion of 130° or more scored lower on the Hi-Flex Function score than did those with flexion of 120° to 129° (p < 0.05), reflecting inferior function in deep-flexion activities (see Table 7). Patients with flexion less than 120° also had lower HFF scores than did those with flexion of 120–129°, but this observed difference did not achieve statistical significance (p = 0.085). The small number of patients with flexion less than 120° (n = 16) diminished the power of this comparison. Multivariate analysis using knee scores, pain, and knee flexion angles as the independent variables revealed that only pain was significantly associated with the HFF score (R = 0.41, p < 0.0001). The magnitude of correlation between pain and HFF scores was greater in patients with anterior knee pain (−0.48) than in patients without anterior knee pain (−0.22), and the presence of anterior knee pain was associated with a decreased HFF score (6.9 vs 9.1 for those without anterior knee pain, p = 0.009).
Table 7.
Relationship between passive knee flexion and hi-flex function score
| Maximum knee flexion angle | Mean HFF score |
|---|---|
| <120 | 7.4 |
| 120–129 | 9.9 |
| ≥130 | 7.4 |
The Knee Society Score was unable to detect poor function during demanding recreational activities. Of the 36 patients with Knee Society knee scores of 99 or 100 and function scores of 100, seven frequently or always had difficulty with demanding recreational activities; nine had great difficulty kneeling or were unable; eight had great difficulty squatting or were unable; and 12 had great difficulty sitting on their heels or were unable.
Discussion
Advertisements suggest that high-flexion total knee implants will deliver “high-performance” knees, but the functional outcomes of TKR utilizing these devices have not been established. The primary goal of this study was to document the quality of knee function 1 year after a high-flexion TKR, with an emphasis on function in deep knee flexion. A secondary goal was to assess outcomes according to the standard clinical and radiographic criteria of the Knee Society. A third goal was to assess the relative effects of residual pain and maximum knee flexion angle on functional outcome. The fourth goal was to assess the sensitivity of Knee Society scores to functional limitations important to high-demand patients.
Drawbacks to the present study include the lack of a comparison group, the exclusion of 17 patients because of incomplete follow-up data, and the short follow-up period. Although 1-year follow-up is insufficient to document the safety and efficacy of a prosthesis, improvements in knee function and motion do plateau by 1 year after TKR [26]. The study duration was therefore adequate to address functional outcomes [12]. A report [19] of early femoral loosening with the NexGen LPS-flex prosthesis (Zimmer, Warsaw, IN, USA) raised concerns about the longevity of high-flexion components—longer follow-up will be necessary to definitively address these concerns. Although the longevity of the PFC sigma RP-F prosthesis will not be established for many years, it was designed to deliver improved wear in those patients who do achieve deep flexion [27], with the prospect of greater durability if fixation is not compromised. The version of the PAQ utilized for this study did not distinguish between moderate-demand activities like gardening, golf, or gym exercise and very-high-demand activities like jogging and skiing. Nevertheless, our results highlight the fact that patients often have limitations in moderately demanding activities. Patients with severe biplanar deformity or severely limited preoperative motion were excluded from the study. This introduces a selection bias towards the inclusion of high-demand (and possibly high-functioning) patients. Low-demand patients were not formally excluded, so the functional outcomes of truly high-performance patients may exceed the mean outcomes observed. Nonetheless, our results give quantitative information from which patients and surgeons may develop informed expectations about the outcomes that are obtained by patients electing knee replacement surgery with this “high-performance” prosthesis.
Demanding deep-flexion activities were achieved frequently, but not consistently. Fifty-seven percent of patients could kneel without significant difficulty; 69% could squat without significant difficulty; and 46% could sit on their heels without significant difficulty. These findings are in keeping with previous studies of the NexGen LPS-flex [14, 15] and NexGen CR-flex [17] high-flexion prostheses (Zimmer, Warsaw, IN, USA), in which 40% [15] to 46% [17] of patients could kneel and 80% could squat [12]. Although participation in demanding recreational activities was reported by 80% of our patients, 22% reported that their knee frequently or always affected performance of these activities. Nutton et al. [16] utilized electrogoniometry to measure knee flexion angles during functional activities, comparing recipients of the NexGen LPS-flex prosthesis to recipients of the standard NexGen LPS prosthesis (Zimmer, Warsaw, IN, USA). They found no difference between prostheses in active knee flexion and negligible differences in knee flexion during functional activities. The knee flexion angles achieved in the two groups (110° with the LPS-flex and 106° with the standard LPS) are not typical of reports examining modern TKR prostheses and techniques, which may limit the applicability of their findings. It is unclear whether the low flexion angles reported [16] are related to their technique of measurement, surgical technique, rehabilitation protocol, or patient population.
Range of motion was improved compared to our historical experience [3, 10, 25], with 80% of knees flexing beyond 120°. The mean postoperative knee flexion angle achieved with the PFC sigma RP-F prosthesis was 125°. This corroborates the results of a previous matched-pair study [10], which demonstrated a design-specific increase in postoperative range of motion with the RP-F implant as compared to the PFC sigma RP implant (DePuy Orthopedics, Inc., Warsaw, IN, USA). To our knowledge, no randomized trial has compared the RP-F prosthesis to the standard RP device. Studies of other “high-flexion” prostheses have not consistently revealed design-specific improvements in range of motion. Two randomized controlled trials [9, 16] comparing the NexGen LPS-flex prosthesis to the standard NexGen LPS prosthesis (Zimmer, Warsaw, IN, USA) found no difference in the range of motion achieved, whereas another randomized trial [11] found a mean of 13° more flexion with the LPS-flex. Similarly, other studies have found a mean of 9–12° more flexion with the LPS-flex [12, 14]. A randomized controlled trial [17] comparing 50 knees with the NexGen CR-flex to 50 knees with the standard NexGen CR (Zimmer, Warsaw, IN, USA) found no improvement in range of motion with the high-flexion cruciate-retaining implants. Similar results were observed in a consecutive case series of 177 knees, with no difference in range of motion between the NexGen CR and CR-flex designs [13]. No differences were found between NexGen CR-flex and LPS-flex prostheses with regards to range of motion or clinical scores [28].
Range of motion did not correlate with patient-reported function in high-flexion activities. This contrasts with the results of Argenson et al. [29], who found that knee flexion greater than 125° after high-flexion TKR was associated with improved patient-reported outcomes as measured by KOOS subscores. These authors did not specifically evaluate function in deep knee flexion, and we did not utilize the KOOS instrument. This difference in outcome measures could account for the difference in findings, although it is surprising that high knee flexion angles would correlate with improved general patient outcomes as measured by the KOOS but not with improved outcomes in deep-flexion activities. All but 16 of our TKRs achieved flexion of at least 120°. It is possible that our failure to identify an association between range-of-motion and function could be explained by a ceiling effect, with flexion beyond a certain degree having little effect on function. Alternatively, Argenson et al. also used a different rotating-platform, high-flexion, posterior-stabilized implant (NexGen LPS-Flex Mobile Bearing Knee, Zimmer, Warsaw, IN, USA). It is possible that differences between the two prostheses explain the discordant results. Nevertheless, future studies evaluating flexion after TKR should specifically evaluate function in high-flexion activities rather than focusing on knee flexion angle.
The best function in deep flexion was observed in patients with knee flexion of 120–129°—patients with greater knee flexion had lower mean Hi-Flex Function scores. Ritter et al. [30] observed a similar phenomenon after cruciate-retaining TKR with an older device; patients who achieved 128–132° of motion demonstrated less pain and better functional scores than those with 133–150° of motion. Ritter et al. [30] suggested that inferior clinical outcomes in knees achieving the highest flexion angles could be a spurious result of the small number of knees achieving motion beyond 133°. Our corroborating findings suggest but do not confirm the alternative possibility of a real defect in these knees. Perhaps subtle flexion instability or quadriceps dysfunction may be present in a subset of patients who achieve high knee flexion angles, allowing passive flexion but limiting functional activities. Alternatively, these patients may experience more anterior knee pain, limiting utilization of the motion achieved. Studies combining patient-reported outcomes with objective functional assessment and in vivo kinematic data could advance our understanding of this phenomenon.
Whereas the relationship between HFF score and knee flexion was nonlinear, the relationship between HFF score and VAS pain was clear. Greater residual knee pain, particularly anterior knee pain, was associated with inferior function in high-flexion activities. Previous authors have noted that femoral component design features associated with decreased anterior knee pain have been associated with improved extensor mechanism function in activities requiring knee flexion [31].
It is reassuring that Knee Society scores were equivalent to those achieved with traditional implant designs, and there was no observed increase in the complication rate at short-term follow-up. Nevertheless, Knee Society scores did not correlate with patient-reported function in deep flexion. We identified significant functional deficits within the subgroup of patients scoring 99 or 100 on the KSS, suggesting that this scoring system is inadequate for the evaluation of knee replacements designed for high performance. High patient expectations and the inability of the KSS to detect limitations in the performance of demanding activities may account for some portion of the documented discrepancy between surgeon and patient-assessed outcomes after TKR [32–34]. More rigorous clinician-assessed outcome measures are needed to complement patient-derived outcome scores.
High flexion after total knee replacement is not a guarantee. Even with meticulous surgical technique, excellent component alignment and the use of a high-flexion prosthesis, many patients will not regain the ability to perform deep-flexion activities. Anterior knee pain continues to affect a subset of patients and is associated with inferior function in activities that require deep flexion. Patients with knees flexing beyond 130° do not typically realize functional benefits superior to those achieved by patients flexing at least 120°. With the RP-F high-flexion implant, it appears that function in deep flexion is more likely to be limited by residual pain than by restricted motion. Previous experience [10] suggests that changes in component design can improve range of motion after total knee replacement. Future efforts to improve implant design or surgical technique may focus on reducing anterior knee pain to facilitate utilization of the full range of flexion achieved.
Footnotes
One or more of the authors (ASR, CSR) have received funding from DePuy, a Johnson & Johnson Company (Warsaw, IN, USA).
Each author certifies that his or her institution has approved the reporting of these cases, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participating in the study was obtained.
Level of Evidence: Level IV: Prospective Case Series.
References
- 1.Anouchi YS, McShane M, Kelly F, Jr, Elting J, Stiehl J. Range of motion in total knee replacement. Clin Orthop. 1996;331:87–92. doi: 10.1097/00003086-199610000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Emerson RH, Jr, Ayers C, Head WC, Higgins LL. Surgical closing in primary total knee arthroplasties: flexion versus extension. Clin Orthop. 1996;331:74–80. doi: 10.1097/00003086-199610000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Ranawat CS, Luessenhop CP, Rodriguez JA. The press-fit condylar modular total knee system. Four-to-six-year results with a posterior-cruciate-substituting design. J Bone Joint Surg Am. 1997;79:342–8. doi: 10.2106/00004623-199703000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Buehler KO, Venn-Watson E, D’Lima DD, Colwell CW., Jr The press-fit condylar total knee system: 8- to 10-year results with a posterior cruciate-retaining design. J Arthroplasty. 2000;15:698–701. doi: 10.1054/arth.2000.8189. [DOI] [PubMed] [Google Scholar]
- 5.Chen AL, Mujtaba M, Zuckerman JD, Jeong GK, Joseph TN, Wright K, Cesare PE. Midterm clinical and radiographic results with the Genesis I total knee prosthesis. J Arthroplasty. 2001;16:1055–1062. doi: 10.1054/arth.2001.27667. [DOI] [PubMed] [Google Scholar]
- 6.Ritter MA, Harty LD, Davis KE, Meding JB, Berend ME. Predicting range of motion after total knee arthroplasty: clustering, log-linear regression, and regression tree analysis. J Bone Joint Surg Am. 2003;85:1278–1285. doi: 10.2106/00004623-200307000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Barrington JW, Sah A, Malchau H, Burke DW. Contemporary cruciate-retaining total knee arthroplasty with a pegged tibial base plate. Results at a minimum of ten years. J Bone Joint Surg Am. 2009;91:874–878. doi: 10.2106/JBJS.G.01609. [DOI] [PubMed] [Google Scholar]
- 8.Lachiewicz PF, Soileau ES. Fifteen-year survival and osteolysis associated with a modular posterior stabilized knee replacement. A concise follow-up of a previous Report. J Bone Joint Surg Am. 2009;91:1419–1423. doi: 10.2106/JBJS.H.01351. [DOI] [PubMed] [Google Scholar]
- 9.Kim YK, Sohn KS, Kim JS. Range of motion of standard and high-flexion posterior stabilized total knee prostheses. A prospective, randomized study. J Bone Joint Surg Am. 2005;87:1470. doi: 10.2106/JBJS.D.02707. [DOI] [PubMed] [Google Scholar]
- 10.Gupta SK, Ranawat AS, Shah V, Zikria BA, Zikria JF, Ranawat CS. The P.F.C. sigma RP-F TKA designed for improved performance: a matched-pair study. Orthopedics. 2006;29(9 Suppl):S49. [PubMed] [Google Scholar]
- 11.Weeden SH, Schmidt R. A randomized, prospective study of primary total knee components designed for increased flexion. J Arthroplasty. 2007;22:349. doi: 10.1016/j.arth.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 12.Bin SI, Nam TS. Early results of high-flex total knee arthroplasty: comparison study at 1 year after surgery. Knee Surg Sports Traumatol Arthrosc. 2007;15:350–5. doi: 10.1007/s00167-006-0202-y. [DOI] [PubMed] [Google Scholar]
- 13.Minoda Y, Aihara M, Sakawa A, Fukuoka S, Hayakawa K, Ohzono K. Range of motion of standard and high-flexion cruciate retaining total knee prostheses. J Arthroplasty. 2009;24(5):674–680. doi: 10.1016/j.arth.2008.02.015. [DOI] [PubMed] [Google Scholar]
- 14.Huang HT, Su JY, Wang GJ. The early results of high-flex total knee arthroplasty: a minimum of 2 years of follow-up. J Arthroplasty. 2005;20(5):674. doi: 10.1016/j.arth.2004.09.053. [DOI] [PubMed] [Google Scholar]
- 15.Seon JK, Song EK, Lee JY. Comparison of range of motion of high-flexion prosthesis and mobile bearing prosthesis in total knee arthroplasty. Orthopaedics. 2005;28(10):s1247. doi: 10.3928/0147-7447-20051002-08. [DOI] [PubMed] [Google Scholar]
- 16.Nutton RW, Linden ML, Rowe PJ, Gaston P, Wade FA. A prospective randomised double-blind study of functional outcome and range of flexion following total knee replacement with the NexGen standard and high flexion components. J Bone Joint Surg Br. 2008;90:37–42. doi: 10.1302/0301-620X.90B1.19702. [DOI] [PubMed] [Google Scholar]
- 17.Seon JK, Park SJ, Lee KB, Yoon TR, Kozanek M, Song EK. Range of motion in total knee arthroplasty: a prospective comparison of high-flexion and standard cruciate-retaining designs. J bone Joint Surg Am. 2009;91:672–9. doi: 10.2106/JBJS.H.00300. [DOI] [PubMed] [Google Scholar]
- 18.Kim TK, Chang CB, Kang YG, Kim SJ, Seong SC. Causes and Predictors of Patient’s Dissatisfaction After Uncomplicated Total Knee Arthroplasty. J Arthroplasty. 2009;24(2):263–271. doi: 10.1016/j.arth.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 19.Han HS, Kang SB, Yoon KS. High incidence of loosening of the femoral component in legacy posterior stabilised-flex total knee replacement. J Bone Joint Surg Br. 2007;89:1457–61. doi: 10.1302/0301-620X.89B11.19840. [DOI] [PubMed] [Google Scholar]
- 20.Miner AL, Lingard EA, Wright EA, Sledge CB, Katz JN. Group. Knee range of motion after total knee arthroplasty: how important is this as an outcome measure? J Arthroplasty. 2003;18:286–294. doi: 10.1054/arth.2003.50046. [DOI] [PubMed] [Google Scholar]
- 21.Meneghini RM, Pierson JL, Bagsby D, Ziemba-Davis M, Berend ME, Ritter MA. Is there a functional benefit to obtaining high flexion after total knee arthroplasty? J Arthroplasty. 2007;22:43–46. doi: 10.1016/j.arth.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 22.Dorr IJN, Scott RD LD, Scott WN. Rationale of the knee society clinical rating system. Clin Orthop. 1989;248:13–4. [PubMed] [Google Scholar]
- 23.Parvataneni HK, Ranawat AS, Ranawat CS. The use of local periarticular injections in the management of postoperative pain after total hip and knee replacement: a multimodal approach. Instr Course Lect. 2007;56:125–131. [PubMed] [Google Scholar]
- 24.Ewald FC. The knee society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop. 1989;248:9–12. [PubMed] [Google Scholar]
- 25.Rasquinha VJ, Ranawat CS, Cervieri CL, Rodriguez JA. The press-fit condylar modular total knee system with a posterior cruciate-substituting design a concise follow-up of a previous report. J Bone Joint Surg Am. 2006;88:1006–1010. doi: 10.2106/JBJS.C.01104. [DOI] [PubMed] [Google Scholar]
- 26.Ritter MA, Berend ME, Harty LD, Davis KE, Meding JB, Keating EM. Predicting range of motion after revision total knee arthroplasty: clustering and log-linear regression analyses. J Arthroplasty. 2004;19:338–43. doi: 10.1016/j.arth.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 27.Ranawat AS, Gupta SK, Ranawat CS. The P.F.C. sigma RP-F total knee arthroplasty: designed for improved performance. Orthopedics. 2006;29(9 Suppl):S28. [PubMed] [Google Scholar]
- 28.Kim Y-H, Choi Y, Kwon OR, Kim J-S. Functional outcome and range of motion of high-flexion posterior cruciate-retaining and high-flexion posterior cruciate-substituting total knee prostheses. A prospective, randomized study. J Bone Joint Surg Am. 2009;91:753–760. doi: 10.2106/JBJS.H.00805. [DOI] [PubMed] [Google Scholar]
- 29.Argenson JN, Parratte S, Ashour A, Komistek RD, Scuderi GR. Patient-reported outcome correlates with knee function after a single-design mobile-bearing TKA. Clin Orthop. 2008;466:2669–76. doi: 10.1007/s11999-008-0418-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ritter MA, Lutgring JD, Davis KE, Berend ME. The effect of postoperative range of motion on functional activities after posterior cruciate-retaining total knee arthroplasty. J Bone Joint Surg Am. 2008;90:777–84. doi: 10.2106/JBJS.F.01022. [DOI] [PubMed] [Google Scholar]
- 31.Mahoney OM, McClung CD, Rosa MA, Schmalzried TP. The effect of total knee arthroplasty design on extensor mechanism function. J Arthroplasty. 2002;17:416–21. doi: 10.1054/arth.2002.32168. [DOI] [PubMed] [Google Scholar]
- 32.Bullens PHJ, Loon CJM, Malefijt MC, Laan RFJM, Veth RPH. Patient satisfaction after total knee arthroplasty: a comparison between subjective and objective outcome assessments. J Arthroplasty. 2001;16(6):740. doi: 10.1054/arth.2001.23922. [DOI] [PubMed] [Google Scholar]
- 33.Mancuso CA, Sculco TP, Wickiewicz TL, Jones EC, Robbins L, Warren RF, Williams-Russo P. Patients’ expectations of knee surgery. J Bone Joint Surg Am. 2001;83:1005. doi: 10.1302/0301-620X.83B7.12105. [DOI] [PubMed] [Google Scholar]
- 34.Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop. 2006;452:35–43. doi: 10.1097/01.blo.0000238825.63648.1e. [DOI] [PubMed] [Google Scholar]