Abstract
Objective
MyStudentBody.com-Nutrition (MSB-N) is an Internet-based nutrition and physical activity education program for college students.
Method
Students from six universities (N = 476) in the U.S. were randomly assigned in the fall of 2005 to one of three groups: MSB-N (Experimental I), MSB-N plus Booster (Experimental II), or an attention placebo control group.
Results
Experimental I and II group participants increased their fruit and vegetable intake by .33 and .24 servings, respectively, relative to the control group at post-test. Both experimental groups improved their motivation to change eating behaviors (p < .05) and were also more likely to increase their social support and self-efficacy for dietary change (p’s < .05). Experimental groups also improved their attitude toward exercise (p < .05), but no behavioral changes in physical activity were noted.
Conclusion
MyStudentBody.com-Nutrition is an effective Internet-based program that may have wide applicability on college campuses for nutrition education and promoting change in health behaviors.
Keywords: nutrition, education, Internet, college, fruit, vegetable, motivation, physical activity
It is now well established that poor eating habits and limited physical activity in adolescence are directly linked to serious health consequences later in life such as osteoporosis, obesity, hyperlipedemia, and diabetes (Bazzano, 2006; Hallal et al., 2006). Most Americans do not eat the recommended amounts of fruits and vegetables (Guenther et al., 2006; Striegel-Moore et al., 2006) and college students, in particular, have poor dietary habits and low activity levels (CDC, 2000; Kolodinsky et al., 2007; Larson et al., 2007). Recently, the American College Health Association reported that only 7% of 3,718 college students ate five or more fruits and vegetables a day and 43.6% reported vigorous exercise for 20 minutes or moderate exercise for 30 minutes on only 3 or fewer days of the previous week (ACHA, 2006). Vigorous physical activity declines markedly from high school to college (Nelson, Gortmaker, Subramanian, & Wechler, 2007). These data suggest that interventions are needed to improve health behaviors in this age group.
Today’s college students are one of the most wired groups in the nation, with many having started computer use between the ages of 5 and 8 (Madden & Jones, 2002). Computer technology has become a viable means of gathering and disseminating nutrition and physical activity education (Ahern, 2007; Brug et al., 2003). To our knowledge, a stand-alone Internet-based nutrition and physical activity education program for college students has not yet been empirically tested. Previous reports by this team (Cousineau et al., 2004; 2006) have described extensive preliminary work that guided the development of MyStudentBody.com-Nutrition (MSB-N). MSB-N is an Internet program that incorporates computer-based technology and specifically targets the unique needs of college students. This report details the efficacy testing of this program in a randomized controlled clinical trial.
Our primary hypothesis was that participants exposed to MSB-N would demonstrate improved nutrition behaviors relative to participants in the control condition. As secondary hypotheses, we expected that participants in the experimental condition would demonstrate a) improvements in motivation to change health behaviors; b) increased nutrition knowledge; c) more frequent physical activity; d) improved social support and attitudes related to healthy eating; and e) improved attitudes toward exercise. We also included a booster session condition in order to assess the effects of providing access to the website for an additional time after the initial intervention period, hypothesizing that the booster group would show greater and longer lasting improvement in outcomes compared to the intervention group.
Method
Screening Participants and Procedure
During the fall of 2005, trained research assistants (RAs) used sign-up tables in high traffic areas to recruit students at each of following six campuses in the U.S.: Northeastern University, College of Charleston, Florida Atlantic University, University of Missouri - St. Louis and Columbia campuses, and Florida International University. Any student who walked by the table and expressed interest was asked to give consent to participate in the screening and to provide contact information. S/he then answered several short screening questions that addressed the inclusion criteria (see below). Because screening was done in this way (i.e., students choosing to stop at the table if interested), we do not have any information about the students who chose not to participate.
Screening measures were scored to determine eligibility for the efficacy study. Inclusion criteria were: (1) enrollment as a full-time undergraduate student, and (2) age 18 to 24. Students who were currently attending formal diet programs or who were on a special monitored diet were excluded.
Participants
Of the 800 students who were screened, 606 were eligible to participate and were contacted to participate in the efficacy study; of these, 476 (79%) students agreed to participate in the study. The number of participants was similar among the six universities. Once screening was complete and eligibility was determined, assessment occurred at 4 time points: (1) baseline (before they began the first web session); (2) post-test (after completing the second web session); (3) 3-month follow-up; and (4) 6-month follow-up assessment.
Measures
These measures, unless otherwise noted, were given at each of the 4 assessment points as listed above.
The Food Frequency Questionnaire
(FFQ; Thompson et al., 2004) is a 16-item measure that assesses fruit and vegetable intake (F&V), percent energy from fat, and grams of fiber consumed in the last 30 days. Response options range from once a month to several times a day for each question. This scale has been found to have good reliability and validity (Thompson et al., 2004). Participants also responded to a single-item measuring the number of servings of fruit and vegetables consumed per day (“How many servings of fruits and vegetables do you usually eat each day?”). Because of an inadvertent data entry error when setting up the online assessment, the questions for the FFQ were mistakenly left out of the post-test assessment, but were included in the 3- and 6-month follow-up assessments.
Stages of Dietary and Physical Activity Change
(SOC; Calfas et al., 2002; Glanz et al., 1998; Greene et al., 1999) is a 14-item validated questionnaire that assesses readiness to increase fruit and vegetable intake, decrease intake of dietary fat, and increase participation in physical activity. Participants are categorized into one of five stages (Precontemplation, Contemplation, Preparation, Action, or Maintenance) on the three measures. Stage of change measures what people think about changing their behaviors and their interest in change, rather than measures of actual behaviors. From this perspective, stage of change can be used as a measure of cognitive and behavioral engagement with the change process.
Nutrition Knowledge Test
(Zawila et al., 2003) is a validated questionnaire originally designed for the female college athlete population which was modified to be more applicable to a general college population. Five questions were added that assessed consequence-related knowledge of nutrition information (e.g., “Getting added calcium helps to prevent bone density problems later in life”; Wansink et al., 2005), for a total of 63 questions. Scores could range from 0 (none correct) to 63 (all correct), with higher scores indicating greater nutrition knowledge.
International Physical Activity Questionnaire
(IPAQ; Craig et al., 2003) is a 27-item measure assessing the frequency of physical activity. The IPAQ has been tested in 12 countries (Booth, 2000) with over 2000 participants. The test-retest reliability was good (rho=0.8) and the criterion validity was acceptable when activity estimates were compared against accelerometer readings (rho=0.3). Vigorous and moderate intensity activities (at least 10 minutes in duration) are measured separately in hours, minutes, and days. One measure of the volume of activity can be computed by weighting each type of activity by its energy requirements, defined in METs, to yield a score in MET-minutes. Computation of the total score requires summation of the duration (in minutes) and frequency (days) of walking, moderate-intensity and vigorous intensity activities.
Social Support, Encouragement and Self-Efficacy for Dietary Changes
(Steptoe et al., 2004) focuses on psychological and social support received by family, friends, and co-workers when making dietary changes (6 items) and self-efficacy for eating fruits and vegetables (3 items). The social support items are scored from 1 (no help) to 5 (a great deal of help) and scale scores range from 6 to 30, with higher scores indicating greater support. The self-efficacy scores range from 3–15, with higher scores indicating greater self-efficacy. There was also a single item to assess encouragement by a close other to make dietary changes that was scored from 1 (never) to 4 (frequently) with greater scores indicating more encouragement. Cronbach alpha coefficients were 0.84 for the family social support questions, 0.78 for the scale focusing on social support from others, and 0.81 for self-efficacy.
Exercise Benefits/Barriers
(Sechrist et al., 1987) is a 43-item validated questionnaire that measures perceived benefits (29 items) and perceived barriers (14 items) to exercise using a 4-point scale (strongly agree, agree, disagree, strongly disagree). Benefits scores can range from 29–116 and Barriers scores can range from 14–56. Median scores in the normative sample were 87 (Benefits) and 41 (Barriers). Cronbach’s alpha of 0.95 was obtained in a study of healthy adults (Sechrist et al., 1987).
Procedure
Four hundred seventy six students were randomized using computer software to one of three groups: 1) Experimental I participants (n = 165) were instructed to use MSB-N for two web sessions; 2) Experimental II participants (Booster; n = 164) were instructed to use MSB-N for two web sessions and a subsequent booster session; and 3) Control Condition participants (n = 147) were instructed to use an interactive anatomy education website for two web sessions. Once randomization was complete, RAs telephoned eligible students and offered participation times at a campus computer lab. All assessments were completed on the Internet at a secure website using Perseus® software. During the first session, participants signed the IRB approved informed consent form and then completed the baseline assessment and the first web session (~45 minutes). Participants then scheduled a second 1.5 hour meeting for two weeks later, during which they completed the second web session (~45 minutes) and the post-test assessment. Participants in the Experimental II (booster) group were asked to log on to the website remotely for 45 minutes approximately 3 weeks after completion of the post-test assessment. They were told to visit any areas of the site that were of interest to them.
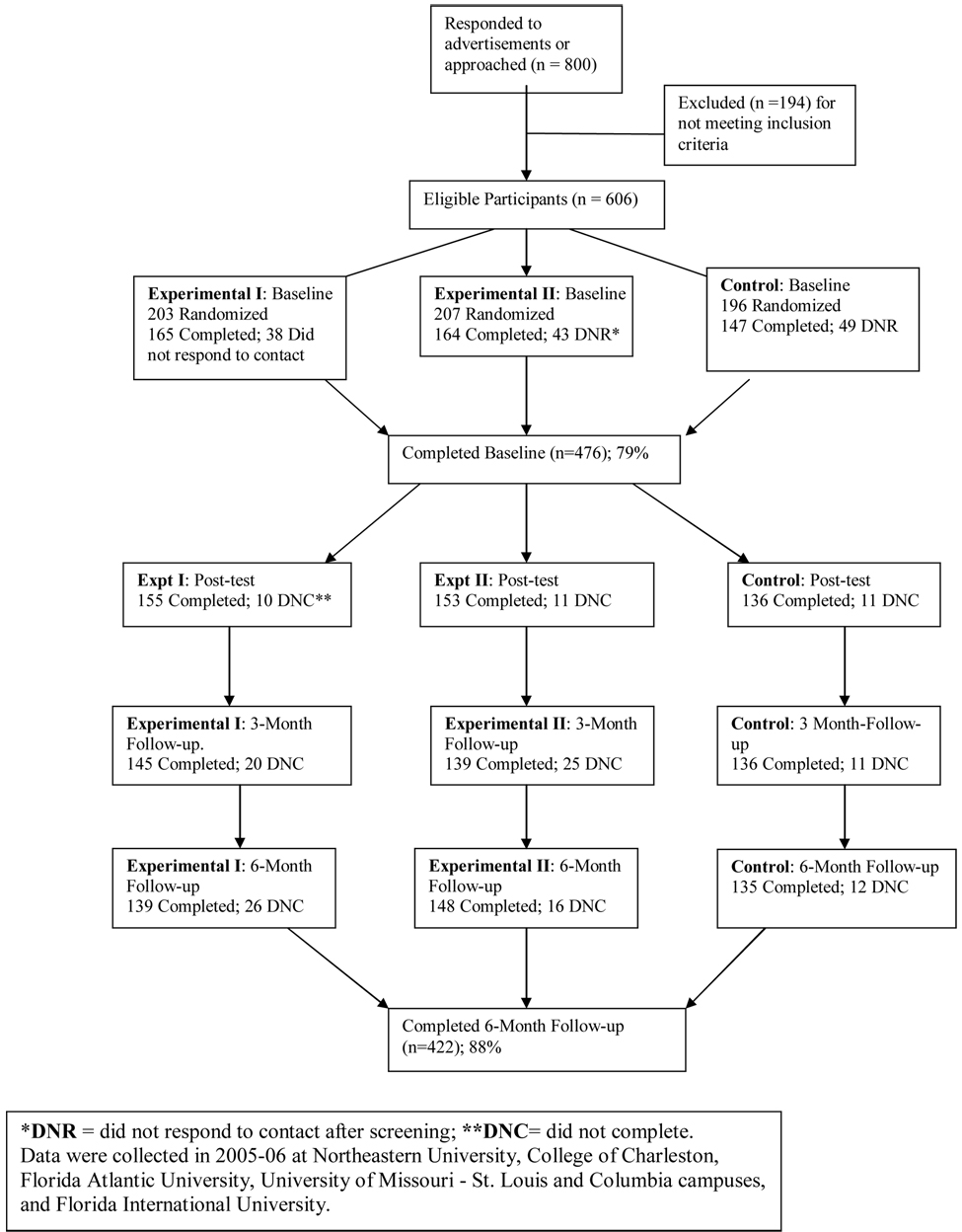
At both web sessions all participants were given a detailed instruction sheet listing all of the areas of the website they needed to visit and complete. They were required to fill in a checklist verifying they had visited these sections and an onsite RA was present to both oversee the web sessions and to answer questions. Three and six months after completing the baseline session all participants were emailed a link to complete the follow-up assessment online. Minimal subject attrition resulted in a sample size of 422 at the 6-month assessment (i.e., 88% response rate; see Figure 1).
Figure 1.
Consort diagram.
In return for their participation, participants received twenty-five dollars for completing the baseline assessment, forty dollars for completing the post-test assessment, forty dollars for completing the 3-month follow-up and fifty-five dollars for completing the 6-month follow-up assessments. All participants in the control condition were given access to MSB-N upon completion of the study.
Intervention
The website, MSB-N, is an interactive Internet-based program designed to provide nutrition and physical activity education and was specifically developed for college students. MSB-N is comprised of: (1) three information links (Ask the Expert, Student Voices, College News); (2) Rate Myself assessment (questions that are part of the website that are used to provide feedback to the user); (3) four main topic pages (Nutrition 101, Eating on the Run, Weighing In, Fitness); and (4) Resources. Participants were instructed to log into the site and begin by completing the Rate Myself questionnaires, which assessed current dietary intake and patterns as well as physical activity levels and beliefs. Participants were then directed to visit the four main topic pages, which contained text-based and audio information, interactive activities, and goal-setting areas.
Statistical Analysis
Recruitment occurred until a total of 800 college students at the 6 universities (approximately 150 per campus) were screened for participation. This number was determined by a power analysis that took into account the sample size needed in order to achieve a small to medium effect size in our primary outcome variables.
Mixed models (Verbeke & Molenberghs, 2000) were used to estimate differences among the three groups (Experimental I and II and Control) at each measurement time after baseline (i.e., post-test, 3 months, and 6 months). Mixed models account for the repeated measures by modeling the structure of association among the repeated measures (Bryk & Raudenbush, 1992). For example, measures of the same participant taken between baseline and post-test assessments may be more highly associated than are measures taken six months later; the strength of association among two measures decreases with increasing time between them. In addition to accounting for the repeated measurements, the direct likelihood estimation technique of mixed models provides unbiased estimates in the presence of missing data at the time points after baseline (Beunckens et al., 2005).
For each outcome, the primary analysis was a mixed model estimating differences among groups and time points, adjusting for gender, baseline BMI, school, pretest measurement of the outcome and group by time interactions. Tests of significance were one-sided and performed at the α=0.05 level. For each outcome measure, tests of group differences at posttest, 3, and 6 months were conducted. Secondary analyses to explore interactions among group, gender, race/ethnicity and baseline BMI that might help to predict changes in nutrition and exercise behavior were conducted using decision tree methods (Kraemer, 1992).
Results
Baseline Characteristics
Racial/ethnic composition of the sample was 58% non-Hispanic white, 14% non-Hispanic black, 15% Hispanic, 6% Asian and 7% other or multiple race/ethnicity or unknown. Table 1 summarizes the baseline characteristics of the study sample. Preliminary analyses revealed no differences in the study samples from the six university sites. At baseline, participants reported eating approximately 3 servings of fruits and vegetables per day and engaging in a moderate degree of physical activity. The only difference between the groups at baseline was found on the benefits of exercise scale, where scores were greater in the Control group than in either Experimental group (p’s < 0.03), while the two Experimental groups did not differ from one another. All results reported below adjust for baseline measures of the outcome variables.
Table 1.
Baseline characteristics of participants. Data presented in the tables and figures were obtained during the 2005–06 academic year at the six participating colleges and universities as noted in Table 1.
| Characteristic | Experimental I (N = 165) | Experimental II (Booster) (N = 164) | Control (N = 147) | All Participants (N = 476) | |
|---|---|---|---|---|---|
|
Sex | |||||
| Male | 69 (41.8%) | 70 (42.7%) | 65 (44.2%) | 204 (42.9%) | |
| Female | 93 (56.4%) | 93 (56.7%) | 82 (55.8%) | 268 (56.3%) | |
| Unknown | 3 (1.8%) | 1 (0.6%) | 0 (0.0%) | 4 (0.8%) | |
|
Race | |||||
| Non-white | 68 (41.2%) | 67 (40.9%) | 59 (40.1%) | 194 (40.8%) | |
| White | 94 (57.0%) | 95 (57.9%) | 88 (59.9%) | 277 (58.2%) | |
| Unknown | 3 (1.8%) | 2 (1.2%) | 0 (0.0%) | 5 (1.1%) | |
|
Category of Body Mass Index (kg/m2) | |||||
| Underweight (< 18.5) | 11 (6.7%) | 7 (4.3%) | 6 (4.1%) | 24 (5.0%) | |
| Normal (18.5–24.9) | 98 (59.4%) | 91 (55.5%) | 91 (61.9%) | 280 (58.8%) | |
| Overweight (25–29.9) | 32 (19.4%) | 44 (26.8%) | 33 (22.4%) | 109 (22.9%) | |
| Obese (≥ 30) | 21 (12.7%) | 20 (12.2%) | 16 (10.9%) | 57 (12.0%) | |
| Unknown | 3 (1.8%) | 2 (1.2%) | 1 (0.7%) | 6 (1.3%) | |
| Age: mean (SD) years | 20.1 (1.7) | 20.0 (1.7) | 20.1 (1.7) | 20.1 (1.7) | |
|
School | |||||
| Northeastern University | 32 (19.4%) | 34 (20.7%) | 29 (19.7%) | 95 (20.0%) | |
| College of Charleston | 28 (17.0%) | 29 (17.7%) | 21 (14.3%) | 78 (16.4%) | |
| Florida Atlantic University. | 26 (15.8%) | 27 (16.5%) | 22 (15.0%) | 75 (15.8%) | |
| University of Missouri- St. Louis | 23 (13.9%) | 20 (12.2%) | 23 (15.6%) | 66 (13.9%) | |
| University of Missouri- Columbia | 28 (17.0%) | 27 (16.5%) | 28 (19.0%) | 83 (17.4%) | |
| Florida International University | 28 (17.0%) | 27 (16.5%) | 24 (16.3%) | 79 (16.6%) | |
Outcomes
We expected that relative to controls, participants exposed to MSB-N would demonstrate improved nutrition behaviors and secondarily, that experimental participants would demonstrate a) improvements in motivation to change health behaviors; b) increased nutrition knowledge; c) more frequent physical activity; d) improved social support and attitudes; and e) improved attitudes toward exercise.
Table 2 displays the means and standard errors of the continuous outcome measures at each assessment and Table 3 shows changes from baseline on the Stages of Change measures. Table 4 indicates differences between each intervention group and the control group at post-test.
Table 2.
Baseline mean (SE) and increase or decrease in the mean relative to Baseline (at Post-test, 3 and 6 months) for each continuous outcome measure by treatment group and time. For Post-test and 3 and 6 months, positive estimates indicate increases relative to Baseline while negative estimates indicate decreases. Data were collected in 2005–06 at Northeastern University, College of Charleston, Florida Atlantic University, University of Missouri - St. Louis and Columbia campuses, and Florida International University.
| Experimental I | Experimental II | Control | ||
|---|---|---|---|---|
| Daily servings or fruit and vegetables | ||||
| Baseline | 5.4 (0.2) | 5.2 (0.2) | 5.1 (0.2) | |
| Post-test | n/a* | n/a | n/a | |
| 3 months | −0.28 | 0.03 | −0.23 | |
| 6 months | −0.35 | −0.16 | −0.18 | |
| Percent of energy from fat | ||||
| Baseline | 30.7 (0.4) | 31.4 (0.4) | 31.9 (0.4) | |
| Post-test | n/a | n/a | n/a | |
| 3 months | −0.34 | −0.13 | −0.88 | |
| 6 months | 0.35 | −0.37 | −0.46 | |
| Single-item fruit and vegetable intake | ||||
| Baseline | 3.2 (0.1) | 3.0 (0.1) | 2.9 (0.1) | |
| Post-test | 0.45 | 0.46 | 0.17 | |
| 3 months | 0.24 | 0.32 | 0.21 | |
| 6 months | 0.13 | 0.40 | 0.39 | |
| Total MET minutes/week;physical activity | ||||
| Baseline | 1878 (80) | 1718 (71) | 1820 (81) | |
| Post-test | 174.77 | 63.08 | 113.46 | |
| 3 months | 49.67 | −7.36 | 48.61 | |
| 6 months | 112.75 | 133.41 | −68.00 | |
| Nutritional knowledge number correct | ||||
| Baseline | 44.0 (0.4) | 43.7 (0.4) | 43.6 (0.4) | |
| Post-test | 2.12 | 2.54 | 1.40 | |
| 3 months | 0.84 | 0.46 | 0.80 | |
| 6 months | 0.39 | 0.57 | 0.16 | |
| Social support for dietary changes score | ||||
| Baseline | 20.2 (0.3) | 20.3 (0.3) | 20.4 (0.3) | |
| Post-test | 0.16 | 0.22 | −0.60 | |
| 3 months | 0.52 | 0.44 | −0.33 | |
| 6 months | −0.52 | 0.19 | −0.92 | |
| Encouragement for dietary change score | ||||
| Baseline | 3.6 (0.1) | 3.5 (0.1) | 3.6 (0.1) | |
| Post-test | 0.07 | −0.05 | −0.26 | |
| 3 months | −0.06 | 0.00 | −0.10 | |
| 6 months | −0.27 | 0.09 | −0.14 | |
| Self efficacy to eat fruit and vegetables score | ||||
| Baseline | 9.7 (0.2) | 9.5 (0.2) | 9.2 (0.3) | |
| Post-test | 0.36 | 0.06 | −0.14 | |
| 3 months | −0.39 | −0.26 | −0.06 | |
| 6 months | −0.46 | 0.01 | 0.24 | |
| Barriers to exercise score | ||||
| Baseline | 41.2 (0.4) | 40.7 (0.4) | 40.7 (0.5) | |
| Post-test | −1.00 | −0.85 | −0.16 | |
| 3 months | −2.70 | −1.86 | −0.72 | |
| 6 months | −2.65 | −2.77 | −1.33 | |
| Benefits of exercise score | ||||
| Baseline | 46.7 (0.9) | 49.6 (0.8) | 50.7 (1.0) | |
| Post-test | 0.12 | 1.45 | 0.78 | |
| 3 months | 3.66 | 2.39 | −0.50 | |
| 6 months | 7.98 | 7.53 | 5.48 | |
Usable measurements for daily servings of fruit and vegetables and percent energy from fat were not available at Post-test.
Table 3.
Baseline mean (SE) and increase or decrease in the mean relative to Baseline (at Post-test, 3 and 6 Months) for Stage of Change measures.* Data were collected in 2005–06 at Northeastern University, College of Charleston, Florida Atlantic University, University of Missouri - St. Louis and Columbia campuses, and Florida International University.
| Experimental I | Experimental II | Control | ||
|---|---|---|---|---|
| Percent of participants advancing 1 or more stages from baseline on fruit/vegetables | ||||
| Baseline | n/a † | n/a | n/a | |
| Post-test | 35.5% | 35.3% | 16.4% | |
| 3 Months | 26.0% | 26.2% | 24.1% | |
| 6 Months | 30.1% | 27.3% | 23.8% | |
| Percent of participants advancing 1 or more stages from baseline on dietary fat | ||||
| Baseline | n/a | n/a | n/a | |
| Post-test | 27.7% | 32.7% | 17.9% | |
| 3 Months | 26.8% | 29.5% | 19.0% | |
| 6 Months | 35.0% | 21.1% | 18.0% | |
| Percent of participants advancing 1 or more stages from baseline on physical activity | ||||
| Baseline | n/a | n/a | n/a | |
| Post-test | 23.9% | 26.1% | 24.6% | |
| 3 Months | 25.2% | 27.9% | 24.1% | |
| 6 Months | 26.8% | 24.2% | 31.1% | |
The Stages of Changes measures presented in Table 3 show percent advanced one or more stages in comparison with baseline. By definition there was no change at baseline. Because participants could revert to baseline (or lower) levels at 3 or 6 months, it is possible for the percentage advancing one or more stages to decrease over time.
Table 4.
Difference between the Experimental I and II groups compared with the Control group at post-test, adjusting for the outcome measure at baseline and gender, baseline BMI and school.‡
Data were collected in 2005–06 at Northeastern University, College of Charleston, Florida Atlantic University, University of Missouri - St. Louis and Columbia campuses, and Florida International University.
| Outcome measures | Experimental I vs. Control at post-test | Experimental II vs. Control at post-test |
|---|---|---|
| Daily servings of fruit and vegetables | n/a † | n/a |
| Percent of energy from fat | n/a | n/a |
| Single-item fruit & vegetable intake | 0.33 (0.12) ** | 0.24 (0.12) * |
| Total MET minutes/week of physical activity | 92.19 (112.23) | −139.81 (111.32) |
| Nutritional knowledge number correct | 0.87 (0.52) | 1.07 (0.52) * |
| Social support for dietary changes score | 0.41 (0.44) | 0.44 (0.44) |
| Encouragement for dietary change score | 0.35 (0.12) ** | 0.15 (0.12) |
| Self efficacy to eat fruit and vegetables score | 0.71 (0.33) * | 0.40 (0.33) |
| Barriers to exercise score | −0.82 (0.55) | −0.70 (0.56) |
| Benefits of exercise score | −1.62 (1.38) | 0.78 (1.38) |
| Advanced 1 or more stages from baseline on fruit/vegetables | 7.06 (2.94,16.97) **** | 7.45 (3.10,17.91) **** |
| Advanced 1 or more stages from baseline on fat | 2.43 (1.08,5.49) * | 3.37 (1.50,7.55) ** |
| Advanced 1 or more stages from baseline on physical activity | 1.58 (0.65,3.84) | 1.34 (0.55,3.26) |
p<0.05
p<0.01
p<0.001
p<0.0001
For all outcomes except stages of change, differences are reported as the estimated mean (SE) difference between the Experimental and control groups at post-test (positive sign indicates that the value was greater in the Experimental group). For stages of change, differences are reported as an odds ratio (95% CI) indicating the odds of advancing one or more stages in each Experimental group compared with the control group.
The fruit and vegetable and fat intake scale measures were not available at post-test.
Hypothesis 1 – Nutrition Behaviors
The single item measure of fruit and vegetable intake indicated that the Experimental I and II participants increased their intake relative to the control group at posttest (p < 0.01). The single-item measure of fruit and vegetable intake did not differ among the groups at 3 or 6 months. Analyses of the FFQ indicated no changes in fruit and vegetable intake or fat intake among any of the groups at 3 or 6 months (the measure was not available at post-test).
Hypothesis 2a – Motivation to change health behaviors
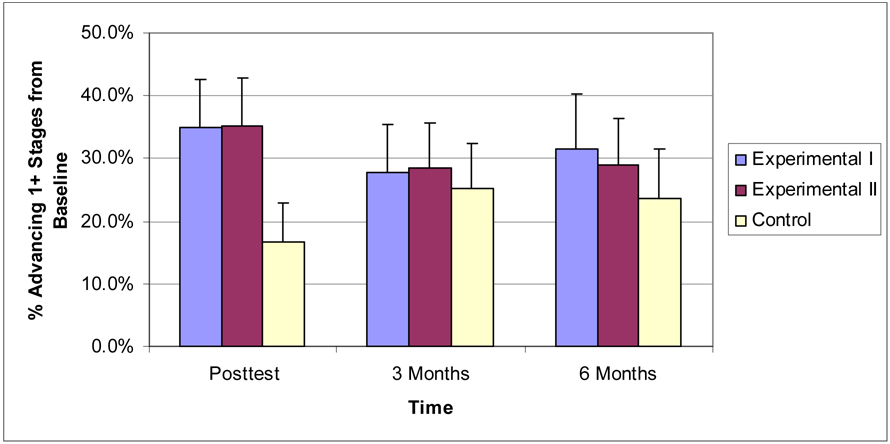
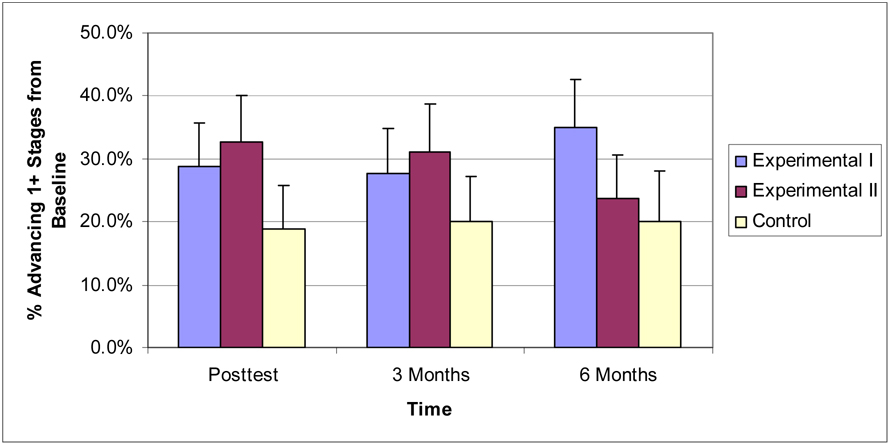
Compared to participants in the Control group, those exposed to MSB-N were more likely to advance a stage in readiness to change fruit and vegetable (F&V) consumption at post-test (p’s < 0.0001) and those in the Experimental I group were also more likely than Controls to advance a stage at 6 months (p < 0.05). Compared to the Control group at post-test, Experimental I and II participants were more likely to report an improvement in readiness to change dietary fat intake (p < 0.05). Experimental II participants were also more likely than Controls to advance a stage on dietary fat at 3 months (p’s < 0.05), while at 6 months a greater percentage of Experimental I participants advanced relative to Controls (p < 0.001; see Figure 2 and Figure 3). Stage of change for physical activity was not affected by the intervention.
Figure 2.
Percent advancing one or more stages compared with baseline on Fruit & Vegetables Stages of Change. Error bars represent the upper limit of the 95% CI. Data were collected in 2005–06 at Northeastern University, College of Charleston, Florida Atlantic University, University of Missouri - St. Louis and Columbia campuses, and Florida International University.
Figure 3.
Percent advancing one or more stages compared with baseline on Fats Stages of Change. Error bars represent the upper limit of the 95% CI. Data were collected in 2005–06 at Northeastern University, College of Charleston, Florida Atlantic University, University of Missouri - St. Louis and Columbia campuses, and Florida International University.
Hypothesis 2b – Nutrition Knowledge
At post-test, participants in the Experimental II group had significantly greater knowledge scores than those in the Control group (p < 0.05).
Hypothesis 2c- Physical Activity
There were no differences between experimental and control participants in physical activity at any time point.
Hypothesis 2d – Social support and self-efficacy for dietary behaviors
Compared with the Control group, at post-test, participants in the Experimental I group had significantly greater scores for encouragement for dietary change (p < 0.01) and self efficacy to eat fruit and vegetables (p < 0.05). At 6 months, participants in the Experimental II group scored higher than those in the Control group on social support for dietary changes (p < 0.05).
Hypothesis 2e – Attitudes toward exercise
On the barriers to exercise scale, the Experimental I group scored significantly lower than the Control group at 3 months (p < 0.01), and at 6 months, both Experimental I and Experimental II scored lower than the Control group (p < 0.05). For the benefits of exercise scale, Experimental I and II participants scored higher than Controls at 3 months (p < 0.05), and at 6 months, Experimental I participants’ scores were significantly higher than controls’ scores on this measure (p’s<0.05).
Effect sizes for significant findings ranged from 0.11 to 0.19, indicating small effect sizes based on definitions provided by Cohen (1988). Exploratory decision tree analyses revealed no interactions among group, gender, race/ethnicity and baseline BMI in relation to changes in nutrition and exercise behavior.
Discussion
This study demonstrated increases in fruit and vegetable consumption, positive changes in motivation to change dietary behaviors, and greater nutrition knowledge in participants in the MSB-N conditions relative to controls. In addition, significant differences were found between intervention and control groups on measures of social support, self-efficacy, and encouragement for dietary change. Barriers and benefits of exercise evidenced change in the intervention groups relative to the control group.
When using the single-item measure of fruit and vegetable consumption, both experimental groups reported significantly higher fruit and vegetable intake than did controls at post-test. We did not find sustained reports of higher F&V consumption, suggesting that in order to maintain dietary changes with college students, more intense efforts are likely needed.
The findings on stage of change were some of the most robust results in the study. Both experimental groups advanced in their perceived readiness to increase fruit and vegetable consumption as well as to decrease dietary fat intake. These results suggest that one important benefit of this Internet-based intervention was to help college students increase their motivation to make dietary changes, which if implemented, could have a significant impact on health (Diclemente et al., 2004; Hwang, 1999; Lampe, 1999; Spencer et al., 2006; Velicer et al., 2006).
In addition to the behavioral and motivational effects, the intervention also appeared to impact measures of encouragement of, and social support for, dietary changes. The positive association between social support and better nutrition has been reported elsewhere (Kelsey et al., 1996; Lloyd et al., 1995; Steptoe et al., 2004; Wolfe, 2004), and may be particularly important for college students who are transitioning away from family and spending the majority of their time with peers.
Self-efficacy is an important variable in many areas of health change behaviors (Bandura, 2004; Wangberg, 2007) and was found to increase in the Experimental I group relative to the control group. Steptoe et al. (2004) found that dietary self-efficacy was associated with concurrent F&V intake, but did not predict consumption 12 months after the intervention. The methodology employed in this study, i.e., making multiple visits to the website, may have been helpful in increasing self-efficacy because participants had a period in which to try out new behaviors as well as the ability to set goals for themselves that could be updated upon return to the website.
Although behavioral changes in physical activity were not found, the experimental groups did score lower on the barriers to exercise measure at the 3-month follow-up (Experimental I) and the 6-month follow-up (both groups). This minimal impact on physical activity may be due to the fact that fitness was less emphasized on the website than nutrition (i.e., only one main topic area was devoted to fitness whereas three were related to nutrition). Alternatively, there may have been a ceiling effect, as our sample had fairly high levels of physical activity at the start of the study. This suggests that the program might be more beneficial for groups less likely to be physically active, such as minority college students (Blanchard et al., 2008). That computer use is in fact a sedentary activity makes an online intervention to encourage physical activity challenging (Marks et al., 2006). It may be that Internet-based programs will need to include use of incentives, sign-up for campus activities, or video games that make use of activity to further increase the efficacy of such an intervention (Lanningham-Foster et al., 2006).
Comparisons of our findings to others in the literature is difficult, as many nutrition-and physical activity-related Internet-based programs tend to target specific issues, such as diabetes prevention and care (Long et al., 2006; Wangberg, 2007) or weight loss (Gold et al., 2007, Rothert et al., 2006). One college-focused intervention combined four stage-based newsletters, one motivational interview, and an individually tailored e-mail follow-up over a 4-month period (Richards, Kattleman, & Ren, 2006), resulting in an increase in fruit and vegetable consumption in the intervention group of one serving a day compared to 0.4 servings a day in the control group. Woodall et al. (2007), in a study using e-mail messages to encourage the use of a nutrition education website with adults in rural settings, found that those who responded to the messages by using the site increased their fruit and vegetable intake by 1.69 servings, relative to the non-responders. Studies that have tested online interventions with adolescents have shown increases in F&V in some cases (e.g., Baranowski et al., 2003) and no change in others (Haerens et al., 2007; Mangunkusumo et al., 2007). A recent review of computer-tailored nutrition education programs for children, adolescents and adults (Kroeze, Werkman, & Brug, 2006) found that 12 of 17 programs reported positive intervention effects, with effect sizes that varied across studies from small (0.14; Winett et al., 1997) to relatively large (0.48; Campbell et al., 1999). A review of behavioral interventions to modify fruit and vegetable intake reported that 17 or 22 studies found positive results, with an average increase of 0.6 servings per day (Ammerman, Lindquist, Lohr, & Hersey, 2002). Our finding of an increase of .33 serving per day is less than previous reports, which is likely related to a number of factors that vary among studies, including the amount of time spent using the website, the degree of tailoring available on the site, the addition of in-person contact, the extent to which the program is integrated into classroom activities, and the actual content that makes up the website.
This same review by Kroeze et al. (2006) also looked at the effectiveness of randomized controlled trials using computer-tailored education for physical activity and found that only 3 of 11 physical activity programs yielded positive results, with effects sizes that ranged from 0.01 (Vandelanotte et al., 2005) to 0.42 (Marcus et al., 1998). Similarly, van den Berg and colleagues (2007) found only 10 eligible studies for their review of Internet-based physical activity interventions, only 5 of which were judged to be of good methodological quality. Of these, 4 compared Internet-based interventions to wait list controls, and only 2 found in favor of the intervention. One of those two studies reported effect sizes, which were small in magnitude (Plotnikoff et al., 2005). Our null findings regarding physical activity appear to be in keeping with other published reports, emphasizing the difficulty of changing physical activity using online programs and the need to consider adding motivational devices (e.g., pedometers) to increase their effectiveness.
The use of a booster session condition appeared to have little impact, which may have to do with the degree to which participants used the website during the booster session. As participants were requested to return to the site at a remote location (i.e., they did not return to the computer lab), it is not clear how much time was actually spent on the site during this extra session. Use of booster sessions in health promotion programs has been encouraged (Elder et al., 2006; Sutton, 2007; Wiehe et al., 2005), but specific procedures have not been well articulated or evaluated.
The long-term maintenance of our intervention effects on behavioral measures was not strong; however, the attitudinal measures did show some longer-term effects. Long-term maintenance of behavioral changes has been a problem in a number of nutrition education studies (Ahern, 2007). Our results suggest that in order to enhance and sustain dietary change, college students may need frequent support over time.
The clinical significance of this study is strongest in relation to the findings of participants’ increased readiness to make changes to both F&V and fat intake, relative to controls. Many recent studies have shown that greater readiness to change relates directly to change in dietary behaviors (Campbell et al., 2008; Di Noia, Schinke, Prochaska, & Contento, 2006; Henry, Reimer, Smith, & Reicks, 2006; Nitzke et al., 2007; Robinson et al., 2008) and is often a first step toward making difficult behavioral changes. Thus, although we found only a modest increase in fruit and vegetable consumption, we posit that a program that increases participants’ motivation is an important addition to the relatively sparse offerings in online nutrition education available to university students (Cousineau et al., 2004). The use of this program in combination with university courses and environmental and policy changes may result in improved nutritional behaviors in college students.
Study Strengths and Limitations
There are both strengths and limitations to this study. Strengths include the relatively large sample, low attrition rate, the ease of use and short completion time of the program, and the multiple domains assessed in the outcome measures. Additionally, participants came from geographically diverse groups and no site differences were observed. Over 40% of our participants were ethnic minority students and we used an attention control group to take into account the effect of participation. However, many of our effects were small in magnitude and this raises the question of clinical versus statistical significance. The use of two to three intervention periods is less than is usually recommended in order to effect long-term change in dietary habits. Moreover, our data was self-report, our measures related to fats did not distinguish between types of fat, and we had missing data for a crucial time point on one key measure.
Future studies will be needed to determine whether improvements can be sustained over a longer period, whether self-reported intention to change will translate into behavior, and whether MSB-N is superior when compared to other nutrition education programs. School-based policies that encourage healthy eating have been studied to a greater extent in middle and high schools (Cullen et al., 2007; Davee et al., 2005; Neumark-Sztainer et al., 2005), than in the college environment (Brown et al., 2005; Shive & Morris, 2006). Findings from these studies have indicated that policy changes about the nutrient content of vending machine and a la carte items, social marketing campaigns that provide sample foods and information about healthy eating, and participation in prepaid meal plans have all proved beneficial to sustaining healthy changes in the food environment for students. The current intervention could easily be incorporated into nutrition, health and fitness courses, provided at wellness clinics, and offered in the freshmen orientation or first-year general education courses in an effort to address the poor nutrition and physical activity habits common to college students. In conjunction with broader environmental changes on campuses (e.g., better choices for fresh produce in cafeterias, posted information about the benefits of healthy eating and exercise), such interventions may assist in widespread changes.
In conclusion, MyStudentBody.com-Nutrition appears to be a brief and effective Internet-based program that can promote some dietary changes in knowledge, attitudes, and behaviors in college students. Such a program is likely to have wide applicability on university campuses in the efforts to increase healthy eating in this population.
Checklist of items to include when reporting a randomized trial
|
PAPER SECTION And topic |
Item | Description | Reported on page # |
|---|---|---|---|
| TITLE & ABSTRACT | 1 | How participants were allocated to interventions (e.g., "random allocation", "randomized", or "randomly assigned"). | 1–2 |
|
INTRODUCTION Background |
2 | Scientific background and explanation of rationale. | 3–4 |
|
METHODS Participants |
3 | Eligibility criteria for participants and the settings and locations where the data were collected. | 4, Table 1 |
| Interventions | 4 | Precise details of the interventions intended for each group and how and when they were actually administered. | 6–7 |
| Objectives | 5 | Specific objectives and hypotheses. | 3–4 |
| Outcomes | 6 | Clearly defined primary and secondary outcome measures and, when applicable, any methods used to enhance the quality of measurements (e.g., multiple observations, training of assessors). | 4–6 |
| Sample size | 7 | How sample size was determined and, when applicable, explanation of any interim analyses and stopping rules. | 4 |
| Randomization -- Sequence generation | 8 | Method used to generate the random allocation sequence, including details of any restriction (e.g., blocking, stratification). | 6 |
| Randomization -- Allocation concealment | 9 | Method used to implement the random allocation sequence (e.g., numbered containers or central telephone), clarifying whether the sequence was concealed until interventions were assigned. | N/A |
| Randomization -- Implementation | 10 | Who generated the allocation sequence, who enrolled participants, and who assigned participants to their groups. | 6 |
| Blinding (masking) | 11 | Whether or not participants, those administering the interventions, and those assessing the outcomes were blinded to group assignment. When relevant, how the success of blinding was evaluated. | 6 |
| Statistical methods | 12 | Statistical methods used to compare groups for primary outcome(s); Methods for additional analyses, such as subgroup analyses and adjusted analyses. | 7 |
| RESULTS Participant flow |
13 | Flow of participants through each stage (a diagram is strongly recommended). Specifically, for each group report the numbers of participants randomly assigned, receiving intended treatment, completing the study protocol, and analyzed for the primary outcome. Describe protocol deviations from study as planned, together with reasons. | 6–7, Figure 1 |
| Recruitment | 14 | Dates defining the periods of recruitment and follow-up. | 4,7 |
| Baseline data | 15 | Baseline demographic and clinical characteristics of each group. | Table 1 |
| Numbers analyzed | 16 | Number of participants (denominator) in each group included in each analysis and whether the analysis was by "intention-to-treat". State the results in absolute numbers when feasible (e.g., 10/20, not 50%). | Table 2 |
| Outcomes and estimation | 17 | For each primary and secondary outcome, a summary of results for each group, and the estimated effect size and its precision (e.g., 95% confidence interval). | 8–9, Table 3 |
| Ancillary analyses | 18 | Address multiplicity by reporting any other analyses performed, including subgroup analyses and adjusted analyses, indicating those prespecified and those exploratory. | N/A |
| Adverse events | 19 | All important adverse events or side effects in each intervention group. | none |
| DISCUSSION Interpretation |
20 | Interpretation of the results, taking into account study hypotheses, sources of potential bias or imprecision and the dangers associated with multiplicity of analyses and outcomes. | 9–12 |
| Generalizability | 21 | Generalizability (external validity) of the trial findings. | 12 |
| Overall evidence | 22 | General interpretation of the results in the context of current evidence. | 9–12 |
Acknowledgments
This research was supported, in part, by SBIR grant R44 DK061870-02A1 funded by the National Institute of Diabetes & Digestive & Kidney Diseases (NIDDK). Portions of this manuscript were completed while Debra Franko on sabbatical as a Distinguished Research Fellow at the Institute for Advanced Study and the School of Psychological Science at La Trobe University, Melbourne, Australia. The authors would like to thank Julie Brevard and the participating colleges and universities for their contributions to the study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no conflict of interest or relevant financial relationships.
Contributor Information
Debra L. Franko, Northeastern University
Tara M. Cousineau, Inflexxion, Inc.
Meredith Trant, Inflexxion, Inc.
Traci Craig Green, Inflexxion, Inc.
Diana Rancourt, Inflexxion, Inc.
Douglas Thompson, Northeastern University
Jessica Ainscough, Inflexxion, Inc.
Laurie B. Mintz, University of Missouri, Columbia
Michelle Ciccazzo, Florida International University
References
- Ahern DK. Challenges and opportunities of eHealth Research. Am J Prev Med. 2007;32:S75–S82. doi: 10.1016/j.amepre.2007.01.016. [DOI] [PubMed] [Google Scholar]
- American College Health Association. American College Health Association National College Health Assessment Spring 2005 Reference Group Data Report (Abridged) J Am Coll Health. 2006;55:5–16. doi: 10.3200/JACH.55.1.5-16. [DOI] [PubMed] [Google Scholar]
- Ammerman AS, Lindquist CH, Lohr KN, Hersey J. The efficacy of behavioral interventions to modify dietary fat and fruit and vegetable intake: a review of the evidence. Prev Med. 2002;35:25–41. doi: 10.1006/pmed.2002.1028. [DOI] [PubMed] [Google Scholar]
- Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31:143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Baranowski T, Baranowski J, Cullen KW, Marsh T, Islam N, Zakeri I, Honess-Morreale L, deMoor C. Squire's Quest! Dietary outcome evaluation of a multimedia game. Am J Prev Med. 2003;24:52–61. doi: 10.1016/s0749-3797(02)00570-6. [DOI] [PubMed] [Google Scholar]
- Bazzano LA. The high cost of not consuming fruits and vegetables. J Am Diet Assoc. 2006;106:1364–1368. doi: 10.1016/j.jada.2006.06.021. [DOI] [PubMed] [Google Scholar]
- Beunckens C, Molenberghs G, Kenward MG. Direct likelihood analysis versus simple forms of imputation for missing data in randomized clinical trials. Clinical Trials. 2005;2:379–386. doi: 10.1191/1740774505cn119oa. [DOI] [PubMed] [Google Scholar]
- Blanchard C, Fisher J, Sparling P, Nehl E, Rhodes R, Courneya K, Baker F. Understanding physical activity behavior in African American and Caucasian college students: an application of the theory of planned behavior. J Am Coll Health. 2008;56:341–346. doi: 10.3200/JACH.56.44.341-346. [DOI] [PubMed] [Google Scholar]
- Booth M. Assessment of physical activity: an international perspective. Res Q Exerc Sport. 2000;71(2 Suppl):S114–S120. [PubMed] [Google Scholar]
- Brown LB, Dresen RK, Eggett DL. College students can benefit by participating in a prepaid meal plan. J Am Diet Assoc. 2005;105:445–448. doi: 10.1016/j.jada.2004.12.030. [DOI] [PubMed] [Google Scholar]
- Brug J, Oenema A, Campbell M. Past, present and future of computer-tailored nutrition education. Am J Clin Nutrition. 2003;77 suppl:1028S–1034S. doi: 10.1093/ajcn/77.4.1028S. [DOI] [PubMed] [Google Scholar]
- Bryk AS, Raudenbush SW. Hierarchical linear models: Applications and data analysis methods. New York: Sage publications; 1992. [Google Scholar]
- CDC. Promoting lifelong healthy eating: Eating habits of the nation's youth. 2000 http://www.cdc.gove/nccdphp/dash/nutraag.htm.
- Calfas KJ, Sallis JF, Zabinski MF, Wilfley DE, Rupp J, Prochaska JJ, Thompson S, Pratt M, Patrick K. Preliminary evaluation of a multi-component program for nutrition and physical activity change in primary care: PACE+ for adults. Prev Med. 2002;34:153–161. doi: 10.1006/pmed.2001.0964. [DOI] [PubMed] [Google Scholar]
- Campbell MK, Honess-Morreale L, Farrell D, Carbone E, Brasure M. A tailored multimedia nutrition education pilot program for low-income women receiving food assistance. Health Educ Res. 1999;14:257–267. doi: 10.1093/her/14.2.257. [DOI] [PubMed] [Google Scholar]
- Campbell MK, McLerran D, Turner-McGrievy G, Feng Z, Havas S, Sorensen G, Buller D, Beresford SA, Nebeling L. Mediation of adult fruit and vegetable consumption in the National 5 A Day for Better Health community studies. Ann Behav Med. 2008;35:49–60. doi: 10.1007/s12160-007-9002-y. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd Ed. New York: Lawrence Erlbaum; 1988. [Google Scholar]
- Cousineau TM, Franko DL, Ciccazzo M, Goldstein M, Rosenthal E. Web-based nutrition education for college students: Is it feasible? Eval Program Planning. 2006;29:23–33. doi: 10.1016/j.evalprogplan.2005.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cousineau TM, Goldstein M, Franko DL. A collaborative approach to nutrition education for college students. J Amer Coll Health. 2004;53:79–84. doi: 10.3200/JACH.53.2.79-84. [DOI] [PubMed] [Google Scholar]
- Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P. International Physical Activity Questionnaire: 12-country reliability and validity. Med Sci Sports Exer. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- Cullen KW, Hartstein J, Reynolds KD, Vu M, Resinicow K, Greene N, White MA. Studies to Treat or Prevent Pediatric Type 2 Diabetes Prevention Study Group, 2007. Improving the school food environment: results from a pilot study in middle schools. J Am Diet Assoc. 2007;107:484–489. doi: 10.1016/j.jada.2006.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davee AM, Blum JE, Devore RL, Beaudoin CM, Kaley LA, Leiter JL, Wigand DA. The vending and a la carte policy intervention in Maine public high schools. Prev Chronic Dis. 2005;2 Spec no: A14 Epub 2005 Nov 1. [PMC free article] [PubMed] [Google Scholar]
- Diclemente CC, Schlundt D, Gemmell L. Readiness and stages of change in addiction treatment. Am J Addict. 2004;13:103–119. doi: 10.1080/10550490490435777. [DOI] [PubMed] [Google Scholar]
- Di Noia J, Schinke SP, Prochaska JO, Contento IR. Application of the transtheoretical model to fruit and vegetable consumption among economically disadvantaged African-American adolescents: preliminary findings. Am J Health Promot. 2006;20:342–348. doi: 10.4278/0890-1171-20.5.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder JP, Ayala GX, Campbell NR, Arredondo EM, Slymen DJ, Baquero B, Zive M, Ganiats TG, Engleberg M. Long-term effects of a communication intervention for Spanish-dominant Latinas. Am J Prev Med. 2006;31:159–166. doi: 10.1016/j.amepre.2006.04.001. [DOI] [PubMed] [Google Scholar]
- Glanz K, Kristal AR, Tilley BC, Hirst K. Psychosocial correlates of healthful diets among male auto workers. Cancer Epidemiology, Biomarkers & Prevention. 1998;7:119–126. [PubMed] [Google Scholar]
- Gold BC, Burke S, Pintauro S, Buzzell P, Harvey-Berino J. Weight loss on the web: A pilot study comparing a structured behavioral intervention to a commercial program. Obesity. 2007;15:155–164. doi: 10.1038/oby.2007.520. [DOI] [PubMed] [Google Scholar]
- Greene GW, Rossi SR, Rossi JS, Velicer WF, Fava JL, Prochaska JO. Dietary applications of the stages of change model. J Amer Diet Assoc. 1999;99:673–678. doi: 10.1016/S0002-8223(99)00164-9. [DOI] [PubMed] [Google Scholar]
- Guenther PM, Dodd KW, Reedy J, Krebs-Smith SM. Most Americans eat much less than recommended amounts of fruits and vegetables. J Am Diet Assoc. 2006;106:1371–1379. doi: 10.1016/j.jada.2006.06.002. [DOI] [PubMed] [Google Scholar]
- Hallal PC, Victora CG, Azevedo MR, Wells JC. Adolescent physical activity and health: a systematic review. Sports Med. 2006;16:1019–1030. doi: 10.2165/00007256-200636120-00003. [DOI] [PubMed] [Google Scholar]
- Henry H, Reimer K, Smith C, Reicks M. Associations of decisional balance, processes of change, and self-efficacy with stages of change for increased fruit and vegetable intake among low-income, African-American mothers. Am Diet Assoc. 2006;106:841–849. doi: 10.1016/j.jada.2006.03.012. [DOI] [PubMed] [Google Scholar]
- Hwang MY. Why you should eat more fruits and vegetables. JAMA. 1999;282:1304. [Google Scholar]
- Kelsey KS, Kirkley BG, DeVelis RF, Earp JA, Ammerman AS, Keyserling TC. Social support as a predictor of dietary change in a low-income population. Health Educ Res. 1996;11:383–395. [Google Scholar]
- Kolodinsky J, Harvey-Berino JR, Berlin L, Johnson RK, Reynolds TW. Knowledge of current dietary guidelines and food choice by college students; better eaters have higher knowledge of dietary guidance. J Am Diet Assoc. 2007;107:1409–1413. doi: 10.1016/j.jada.2007.05.016. [DOI] [PubMed] [Google Scholar]
- Kraemer HC. Evaluating Medical Tests. Newbury Park, CA: Sage Publications; 1992. [Google Scholar]
- Kroeze W, Werkman A, Brug J. A systematic review of randomized trials on the effectiveness of computer-tailored education on physical activity and dietary behaviors. Ann Behav Med. 2006;31:205–223. doi: 10.1207/s15324796abm3103_2. [DOI] [PubMed] [Google Scholar]
- Lampe JW. Health effects of vegetables and fruit: Assessing mechanisms of action in human experimental studies. Am J Clin Nutr. 1999;72:912–921. doi: 10.1093/ajcn/70.3.475s. [DOI] [PubMed] [Google Scholar]
- Lanningham-Foster L, Jensen TB, Foster RC, Redmond AB, Walker BA, Heinz D, Levine JA. Energy expenditure of sedentary screen time compared with active screen time for children. Peds. 2006;118:e1831–e1835. doi: 10.1542/peds.2006-1087. [DOI] [PubMed] [Google Scholar]
- Larson NI, Neumark-Sztainer D, Hannan PJ, Story M. Trends in adolescent fruit and vegetable consumption, 1999–2004; Project EAT. Am J Prev Med. 2007;32:147–150. doi: 10.1016/j.amepre.2006.10.011. [DOI] [PubMed] [Google Scholar]
- Lloyd HM, Paisley CM, Mela DJ. Barriers to the adoption of reduced-fat diets in a UK population. J Amer Diet Assoc. 1995;95:316–322. doi: 10.1016/s0002-8223(95)00082-8. [DOI] [PubMed] [Google Scholar]
- Long JD, Armstrong ML, Amos E, Shriver B, Roman-Shriver C, Feng D, Harrison L, Luker S, Nash A, Blevins MW. Pilot using World Wide Web to prevent diabetes in adolescents. Clin Nurs Res. 2006;15:67–79. doi: 10.1177/1054773805282446. [DOI] [PubMed] [Google Scholar]
- Madden M, Jones S. [May 22, 2007];The internet goes to college. Pew Internet and American Life Project. 2002 at http://www.pewinternet.org/PPF/r/71/report_display.asp.
- Mangunkusumo RT, Brug J, de Koning HJ, van der Lei J, Raat H. School-based Internet-tailored fruit and vegetable education combined with brief counseling increases children's awareness of intake levels. Public Health Nutr. 2007;10:273–279. doi: 10.1017/S1368980007246671. [DOI] [PubMed] [Google Scholar]
- Marcus BH, Bock BC, Pinto BM, Forsyth LH, Roberts MB, Traficante RM. Efficacy of an individualized, motivationally-tailored physical activity intervention. Ann Behav Med. 1998;20:174–180. doi: 10.1007/BF02884958. [DOI] [PubMed] [Google Scholar]
- Marks JT, Campbell MK, Ward DS, Ribisl KM, Woildemuth BN, Symons MJ. A comparison of Web and print media for physical activity promotion among adolescent girls. J Adolesc Health. 2006;39:96–104. doi: 10.1016/j.jadohealth.2005.11.002. [DOI] [PubMed] [Google Scholar]
- Nelson TF, Gortmaker SL, Subramanian SV, Wechsler H. Vigorous physical activity among college students in the United States. J Phys Act Health. 2007;4:495–508. [PubMed] [Google Scholar]
- Neumark-Sztainer D, French SA, Hannan PJ, Story M, Fulkerson JA. School lunch and snacking patterns among high school students: associations with school food environment policies. Int J Behav Nutr Phys Act. 2005;2:14. doi: 10.1186/1479-5868-2-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nitzke S, Kritsch K, Boeckner L, Greene G, Hoerr S, Horacek T, Kattelmann K, Lohse B, Oakland MJ, Beatrice P, White A. A stage-tailored multi-modal intervention increases fruit and vegetable intakes of low-income young adults. Am J Health Promot. 2007;22:6–14. doi: 10.4278/0890-1171-22.1.6. [DOI] [PubMed] [Google Scholar]
- Plotnikoff RC, Mccargar LJ, Wilson PM, Loucaides CA. Efficacy of an E-mail intervention for the promotion of physical activity and nutrition behavior in the workplace context. Am J Health Promot. 2005;19:422–429. doi: 10.4278/0890-1171-19.6.422. [DOI] [PubMed] [Google Scholar]
- Richards A, Kattleman KK, Ren C. Motivating 18–24-year-olds to increase their fruit and vegetable consumption. J Amer Diet Asso. 2006;106:1405–1411. doi: 10.1016/j.jada.2006.06.005. [DOI] [PubMed] [Google Scholar]
- Robinson AH, Norman GJ, Sallis JF, Calfas KJ, Rock CL, Patrick K. Validating stage of change measures for physical activity and dietary behaviors for overweight women. Int J Obes (Lond) 2008 May 20; doi: 10.1038/ijo.2008.65. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- Rothert K, Strecher VJ, Doyle LA, Caplan WM, Joyce JS, Jimison HB, Karm LM, Mims AD, Roth MA. Web-based weight management programs in an integrated health care setting: A randomized, controlled trial. Obesity. 2006;14:266–272. doi: 10.1038/oby.2006.34. [DOI] [PubMed] [Google Scholar]
- Sechrist KR, Walker SN, Pender NJ. Development and psychometric evaluation of the exercise benefits/barriers scale. Res Nur Health. 1987;10:357–365. doi: 10.1002/nur.4770100603. [DOI] [PubMed] [Google Scholar]
- Shive SE, Morris MN. Evaluation of the energize your life! Social marketing campaign pilot study to increase fruit intake among community college students. J Am Coll Health. 2006;55:33–39. doi: 10.3200/JACH.55.1.33-40. [DOI] [PubMed] [Google Scholar]
- Spencer L, Adams TB, Malone S, Roy L, Yost E. Applying the transtheoretical model to exercise: a systematic and comprehensive review of the literature. Health Promot Pract. 2006;7:428–443. doi: 10.1177/1524839905278900. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Perkins-Porras L, Rink E, Hilton S, Cappuccio FP. Psychological and social predictors of changes in fruit and vegetable consumption over 12 months following behavioral and nutrition education counseling. Health Psych. 2004;23:574–581. doi: 10.1037/0278-6133.23.6.574. [DOI] [PubMed] [Google Scholar]
- Striegel-Moore RH, Thompson DR, Affenito SG, Franko DL, Barton BA, Schreiber GB, Daniels SR, Schmidt M, Crawford PB. Fruit and Vegetable Intake: Few adolescent girls meet national guidelines: The National Heart, Lung, and Blood Institute (NHLBI) Growth and Health Study. Prev Med. 2006;42:223–228. doi: 10.1016/j.ypmed.2005.11.018. [DOI] [PubMed] [Google Scholar]
- Sutton JM. Prevention of depression in youth: A qualitative review and future suggestions. Clin Psychol Rev. 2007;27:552–571. doi: 10.1016/j.cpr.2007.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson FE, Midthune D, Subar AF, Kahle LL, Schatzkin A, Kipnis V. Performance of a short tool to assess dietary intakes of fruits and vegetables, percentage energy from fat and fibre. Pub Health Nutrition. 2004;7:1097–1106. doi: 10.1079/PHN2004642. [DOI] [PubMed] [Google Scholar]
- Vandelanotte C, De Bourdeaudhuij I, Sallis JF, Spittaels H, Brug J. Efficacy of sequential or simultaneous interactive computer-tailored interventions for increasing physical activity and decreasing fat intake. Ann Behav Med. 2005;29:138–146. doi: 10.1207/s15324796abm2902_8. [DOI] [PubMed] [Google Scholar]
- Van den Berg MH, Schoones JW, Vliet Vlieland TPM. Internet-based physical activity interventions: A systematic review of the literature. J Med Internet Res. 2007;9:e26. doi: 10.2196/jmir.9.3.e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velicer WF, Prochaska JO, Redding CA. Tailored communications for smoking cessation: past successes and future directions. Drug Alcohol Rev. 2006;25:49–57. doi: 10.1080/09595230500459511. [DOI] [PubMed] [Google Scholar]
- Verbeke G, Molenberghs G. Linear mixed models for longitudinal data. New York: Springer-Verlag; 2000. [Google Scholar]
- Wangberg SC. An Internet-based diabetes self-care intervention tailored to self-efficacy. Health Educ Res. 2007 April 5; doi: 10.1093/her/cym014. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- Wansink B, Westgren RE, Cheney MM. Hierarchy of nutritional knowledge that relates to the consumption of a functional food. Nutrition. 2005;21:264–268. doi: 10.1016/j.nut.2004.06.022. [DOI] [PubMed] [Google Scholar]
- Wiehe SE, Garrison MM, Christakis DA, Ebel BE, Ravara FP. A systematic review of school-based smoking prevention trials with long-term follow-up. J Adol Health. 2005;36:162–169. doi: 10.1016/j.jadohealth.2004.12.003. [DOI] [PubMed] [Google Scholar]
- Winett RA, Wagner JL, Moore JF, Walker WB, Hite LA, Leahy M, Neubauer T, Arbour D, Walberg J, Geller ES. An experimental evaluation of a prototype public access nutrition information system for supermarkets. Health Psychol. 1991;10:75–78. doi: 10.1037//0278-6133.10.1.75. [DOI] [PubMed] [Google Scholar]
- Wolfe WA. A review: maximizing social support--a neglected strategy for improving weight management with African-American women. Ethn Dis. 2004;14:212–218. [PubMed] [Google Scholar]
- Woodall WG, Buller DB, Saba L, Zimmerman D, Waters E, Hines JM, Cutter GR, Starling R. Effect of emailed messages on return use of a nutrition education website and subsequent changes in dietary behavior. J Med Internet Res. 2007;9:e27. doi: 10.2196/jmir.9.3.e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zawila LG, Steib CSM, Hoogenboom B. The female collegiate cross-country runner: Nutritional knowledge and attitudes. J Athletic Training. 2003;38:67–74. [PMC free article] [PubMed] [Google Scholar]