Abstract
Background
Despite the growing burden of injuries in LMICs, there are still limited primary epidemiologic data to guide health policy and health system development. Understanding the epidemiology of injury in developing countries can help identify risk factors for injury and target interventions for prevention and treatment to decrease disability and mortality.
Aim
To estimate the epidemiology of the injury seen in patients presenting to the government hospital in Kampala, the capital city of Uganda.
Methods
A secondary analysis of a prospectively collected database collected by the Injury Control Centre-Uganda at the Mulago National Referral Hospital, Kampala, Uganda, 2004-2005.
Results
From 1 August 2004 to 12 August 2005, a total of 3,750 injury-related visits were recorded; a final sample of 3,481 records were analyzed. The majority of patients (62%) were treated in the casualty department and then discharged; 38% were admitted. Road traffic injuries (RTIs) were the most common causes of injury for all age groups in this sample, except for those under 5 years old, and accounted for 49% of total injuries. RTIs were also the most common cause of mortality in trauma patients. Within traffic injuries, more passengers (44%) and pedestrians (30%) were injured than drivers (27%). Other causes of trauma included blunt/penetrating injuries (25% of injuries) and falls (10%). Less than 5% of all patients arriving to the emergency department for injuries arrived by ambulance.
Conclusions
Road traffic injuries are by far the largest cause of both morbidity and mortality in Kampala. They are the most common cause of injury for all ages, except those younger than 5, and school-aged children comprise a large proportion of victims from these incidents. The integration of injury control programs with ongoing health initiatives is an urgent priority for health and development.
Keywords: Road traffic, Injuries, Developing country, Trauma, Uganda
Introduction
Injuries are responsible for an increasing share of morbidity and mortality in low- and middle-income countries (LMICs) where they currently account for 11% of the total disability-adjusted life years [1]. Injuries also have an enormous socioeconomic impact both at the household and national level. There are great disparities in the prevention and care of injuries worldwide, with 1 to 2 million preventable deaths in severely injured patients and 90% of deaths from road traffic injuries occurring in low- and middle-income countries [2, 3]. Children are disproportionately affected as well. In sub-Saharan African children over 5, injuries account for more deaths than HIV, tuberculosis, and malaria combined [4].
Understanding the epidemiology of injury can help identify risk factors for injury and target interventions for prevention and treatment to decrease disability and mortality. Despite the growing burden of injuries in LMICs, however, there remain limited primary epidemiologic data to guide health policy and health system development [5, 6]. Even if a health facility capable of providing quality emergency care exists, the absence of formal prehospital care in resource-constrained settings, along with multiple barriers to care such as social, educational, cultural, and financial factors, prevents access to these facilities.
To improve epidemiologic surveillance of injuries in Uganda, the Injury Control Centre-Uganda established a trauma registry in 1998, after piloting and validating an instrument for data collection. This registry has been used in five Ugandan hospitals since 1998 [7, 8]. Similar registries have also been established in other countries in the region [9]. Since then, a number of injury prevention interventions such as seat belt laws in motor vehicles, helmet laws for motorcyclists, speed bumps, improved street lighting, and school and household-based interventions for children have been implemented. Efforts to improve trauma care have included trauma courses for hospital-based personnel and some first aid courses for police [10]. In addition, a national injury policy has been drafted by the Ministry of Health [11]. There has, however, been no formal epidemiologic analysis of the potential collective impact of these interventions since the trauma registry was first implemented.
The goal of this study was to estimate the current epidemiology of injury in the capital city of Kampala by using data at Mulago National Referral Hospital, especially the most common causes of injury, and the prevalence of intentional and unintentional injury.
Methods
The database for this study was constructed from prospectively collected data from the Injury Control Centre-Uganda, which is a private organization that is funded by both public and private sources; trained nurses, clinical officers, or doctors in the casualty (or emergency) department of the Mulago National Referral Hospital completed a one-page form (described previously in the literature [8]) on each patient presenting to the casualty department, recording information on the patient condition, status, demographics (age, sex, residence, occupation), several clinical variables (blood pressure, pulse, respiratory rate, and neurological status), as well as causes and place of injury, severity of injury, and outcome. Two weeks after initial presentation, the health care providers or records clerks completed the patient disposition from the casualty (treated and discharged from casualty, admitted, transferred to higher level facility, died in casualty, dead on arrival) as well as the disposition for those admitted (discharged, died, still in the hospital, transferred, or other). This registry was checked for accuracy by a hospital surgeon or senior doctor, and the data were entered into Excel (Microsoft, 2005), cleaned, and managed by the Injury Control Centre-Uganda.
The most current full year of data available at this time is from July 2004 to August 2005. Prospective injury data were no longer recorded after 2005 due to lack of funding, and at this time, these data represent the most recent injury epidemiology seen at Mulago National Referral Hospital, a government hospital. Since 2008, efforts to restart the hospital trauma registry have been revived.
All patients seen at Mulago National Referral Hospital that were recorded in the database in the 12-month period from 1 July 2004–1 August 2005 were included in the data set, which was queried for descriptive statistics of all injuries to characterize patients by age, gender, type of injury, location of injury, intent, mode of arrival, distance, injury severity, and disposition.
The Kampala Trauma Score (KTS) was chosen to categorize severity of injury. This score has been validated and was revised in 2004, where previous definitions of mild, moderate, and severe injuries (which were KTS scores of 14–16, 11–13, and <11, respectively) were simplified to fit on a 10-point scale, with mild injury defined as KTS 8–10, moderate injury as KTS 5–7, and severe injury as KTS <5.
This study protocol was approved by the Mulago National Referral Hospital Research Committee, the Uganda National Council of Science and Technology, and the Institutional Review Board of the University of California, San Francisco.
Results
From 1 August 2004 to 12 August 2005, a total of 3,750 injury-related visits were recorded. We excluded those that had no disposition from the casualty department (n = 51) and those with missing values for disposition at 2 weeks (n = 218), together representing 7% of our sample. A total of 3,481 records were analyzed.
General characteristics
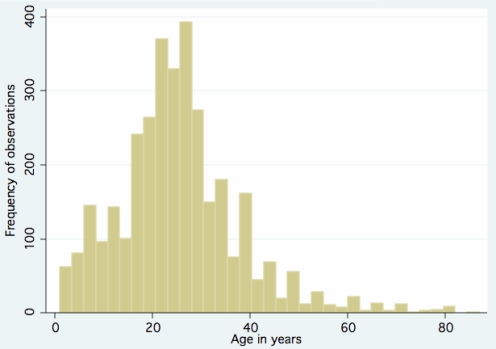
Injured patients seen at this hospital had a mean age of 25 years, and 74% were male. Figure 1 shows the age distribution of injured patients.
Fig. 1.
Age distribution of injured patients presenting to the hospital
Patient disposition
The majority of patients (n = 2,144, 62%) were treated in the casualty department and then discharged. Thirty-eight percent (n = 1,315) were admitted. The proportion of admitted patients to all presenting patients was similar for all age groups. Although 2 patients were dead on arrival, 15 patients (0.4%) were alive when presenting to the casualty ward but died before being admitted. Five patients (0.1%) were transferred (although the data do not indicate where or why).
Most common causes of injury
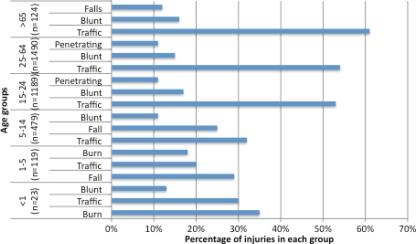
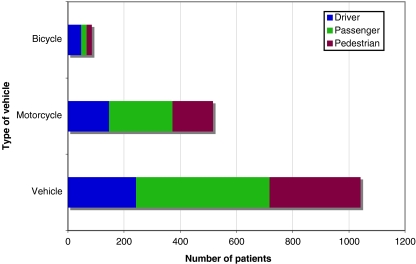
Road traffic injuries were the most common causes of injury for all age groups in this sample except for those under 5, and accounted for 49% of total injuries. Blunt injuries accounted for 15% and accounted for the second most common cause of injury in all patients 15 years and above. Penetrating injury was seen more often in patients between the ages of 15 and 64. Poisonings, choking or hanging, drowning, and sexual assault were rarely reported (all less than 1%). Figure 2 describes the top three causes of injury by age group. Within traffic injuries (Fig. 3), more passengers (44%) and pedestrians (30%) were injured than were drivers (27%).
Fig. 2.
Most common causes of injuries by age group
Fig. 3.
Patients presenting to the hospital from road traffic injuries by type of vehicle and status in vehicle
Occupation
Students (20%) and casual laborers (17%) were the most frequent victims of trauma. Civil servants and private employees comprised 11% of victims and small business owners 10%.
Place of injury
Fifty-nine percent of injuries occurred on the road or street, and 25% occurred in the home. This pattern was similar for both sexes. Roads or streets were named as the most common place of injury for all ages, except those aged less than 15, for whom the home was the most common place of injury. For women, 35% of injuries occurred at home compared to 21% for men (p < 0.05).
Intent
Seventy-two percent of injuries were unintentional. After excluding animal/snakebites, blunt force (56%) and stabs or cuts (19%) comprised the majority of intentional injuries, with a similar pattern for both genders. Nine victims sought care for sexual assault. Five of the nine patients were treated and discharged at the casualty department, and four were admitted, three of whom were subsequently discharged. One died in the hospital. Five of the assaults were alcohol-related incidents.
Nine cases of domestic violence were reported. Given that domestic violence is rarely reported, possible domestic violence cases were noted if injuries occurred at home and were reported to be intentional. Based on these two criteria, 328 injuries were identified, compared with the actual reported number of nine victims of domestic violence. Some of these injuries were reported as animal or snakebites, which have been shown to be associated in published literature [12]. Even when these injuries were excluded, 223 cases remained with 58% from blunt force, 20% from penetrating injuries such as stabs/cuts, and the rest from falls, burns, and other causes.
Mode of arrival
Less than 5% of all patients arriving to the emergency department for injuries arrived by ambulance. The majority of patients (50%) came by private vehicle, and 22% were brought in by the police. Twelve percent came by bicycle or motorcycle, and 10% came by foot. Patients with more severe injuries as determined by a low initial Kampala Trauma Score (KTS, see Table 1) were more likely (p < 0.01) to arrive by ambulance than those who were less severely injured (higher KTS).
Table 1.
Kampala trauma score
| Category | Value |
|---|---|
| a. Age | |
| ≤5 | 1 |
| 6-55 | 2 |
| >55 | 1 |
| b. Number of serious injuries | |
| 0 | 3 |
| 1 | 2 |
| 2 or more | 1 |
| c. Systolic blood pressure (mmHg) | |
| >89 | 4 |
| 0-89 | 3 |
| 1-49 | 2 |
| Undetectable | 1 |
| d. Respiratory rate (breaths/min) | |
| 10-29 | 3 |
| ≥30 | 2 |
| ≤9 | 1 |
| e. Neurological status (AVPU system*) | |
| Alert | 4 |
| Responds to verbal stimuli | 3 |
| Responds to painful stimuli | 2 |
| Unresponsive | 1 |
KTS total = a+b+c+d+e
Notes: Possible range for KTS is 5–16
5 = Most severely injured
16 = The least severely injured
*The AVPU system is a simplified version of the Glasgow Coma Scale
For patients that were eventually admitted, 9.8% (95% CI 8.2, 11.4) came by ambulance. Of these admitted patients, more severely ill patients had 1.2 times the likelihood (95% CI 1.1, 1.4) of being taken to the hospital in an ambulance compared to those with lower severity (higher KTS).
Distance
Sixty-five percent of injured people brought to Mulago Hospital were from the district of Kampala. Of those who were injured in Kampala and brought to Mulago Hospital, 33% were admitted as compared to 46.7% of those who were injured outside of Kampala (p < 0.01 for difference).
Injury classification, severity, and outcome
Table 2 shows that 92% of the patients were mildly injured and only 1% of the sample severely injured. At 2 weeks, 67% of admitted patients had been discharged, 26% were still in the hospital, 6% had died, and 1% had left against medical advice. Seventy-five percent of the patients who died of trauma in the hospital had head injury. Chest injury accounted for 17% of trauma deaths. A total of 72 patients died, which comprised 2% of the admitted patients. For those who died, the most common cause was road traffic injuries (n = 41) (Table 3), which constituted over half of the fatalities. A multivariable regression (including age, sex, mechanism, occupation, place of injury, mode of arrival, and distance) looking at outcome of death in the hospital did not show any correlation with any variables except for KTS, where each lower KTS point was correlated with a decrease of 5% in the chance of survival (95% CI, 4.9%–5.7%).
Table 2.
Injury severity of patients seen in casualty
| Category | KTS score | Number | % Sample |
|---|---|---|---|
| Mild | 8-10 | 3,135 | 92% |
| Moderate | 5-7 | 235 | 7% |
| Severe | <5 | 33 | 1% |
| 3,403 | 100% |
Table 3.
Fatal causes of injury
| Cause | Number | Percent |
|---|---|---|
| Road traffic | 41 | 56.9% |
| Burn | 12 | 16.7% |
| Blunt/penetrating injury | 11 | 15.2% |
| Fall | 7 | 9.7% |
| Sexual assault | 1 | 1.4% |
| Total | 72 | 100.0% |
Limitations
The goal of this study was to analyze the injuries of patients that presented to the tertiary care hospital of the capital city of Uganda. For a broader view of injury, it would be preferable to include data from all hospitals in Kampala; however, such data are not available since there is no systematic data collection across these facilities for trauma. Although Mulago Hospital receives 75% of injured victims in Kampala [8], most of the other hospitals in city are private and better resourced than the National Hospital, although they do not as reliably have the 24-h coverage of the National Hospital. It would be possible that they have better injury outcomes. In addition, limitations in facility-based care that could have affected outcomes were not evaluated in this study. Furthermore, we were unable to assess the number, characteristics, and types of trauma patients that did not present to this hospital because of the lack of a formal prehospital emergency system in Kampala.
Discussion
Several findings are notable in this study. Earlier reports of trauma registries in Uganda show that the young male population is most affected by trauma, and the findings of this more updated study confirm the impact on this age group. Similar to previous studies, the data also show that road traffic injuries are the most common cause of injury overall, except for in children aged 5 and younger [13]. Worldwide, road traffic injuries account for approximately 30% of all childhood injury deaths [14], which mirrors our finding of overall injured people presenting to the hospital. While these results are no doubt partly a reflection of the underlying demographic patterns in sub-Saharan Africa, with a relatively younger population compared to more developed countries, these findings still have important potential implications for public health and for poverty eradication.
First, children and the economically productive segments of the population are most affected by injury, but the precise impact on household poverty (e.g., income forgone, impact on family members, household wealth lost) is poorly characterized, even in other sub-Saharan African nations with a similar burden of injury [15]. Though there was no specific variable to capture wealth or socioeconomic status, the preponderance of students and casual laborers that were injured suggests that poorer and more vulnerable groups are affected by injury, keeping with prior reports [16]. This could be further analyzed either through closer evaluation of patients hospitalized with injuries or as part of community surveys or ongoing demographic surveillance programs. Previous work has suggested that injury costs Uganda 2% of the GDP per year; however, the prevention and care of injuries has not been highlighted by the Poverty Eradication Action Plan of the Ministry of Finance or recognized as a key health-related aspect of Uganda’s progress toward the Millennium Development Goals [11].
In addition, the impact on school-age children suggests that more coherent policies for the prevention and care of injuries must be integrated into child health programs, as has been previously suggested from prospective studies in children and reviews of surgical conditions in the region [14, 17–19]. In the under-5-years age group, the preponderance of burns and falls points to areas of further research for prevention and care. Since the majority of child injuries occurred at home, one might consider how a household-based injury prevention program could be designed and implemented. In addition, though prior reviews suggest that school-based education programs for injury prevention have limited effectiveness, this may need to be reconsidered. Multiple randomized controlled trials have shown that safety education can change pedestrian behavior in high-income countries, although the effects on injury rates are not known. However, there have been no large-scale studies on pedestrian education in low and middle-income countries. Such interventions may need to be considered potentially in combination with other, more effective interventions at the household and primary care level to address the injury epidemic in Kampala [20].
Second, our findings also show that, within road traffic injuries, more passengers are injured compared to drivers in both motorcycle and vehicular injuries in Kampala. Not only are road traffic injuries the most common cause of injury, they are also responsible for the majority of fatal injuries that occurred in this study. This is in contrast to previous findings showing that pedestrians were the most commonly injured in road traffic injuries in urban Uganda. Prior studies have also shown the high impact on vulnerable road users such as pedestrians and motorcycle drivers [16, 21]. The increased numbers of non-driver injuries reflect the pattern of transport in Uganda, where few individuals own their own vehicles, and most use large vehicles that ferry numerous passengers at a time. This pattern provides a strong argument for interventions that increase the road safety of these large transportation vehicles.
This is also in keeping with prior work documenting that more passengers per crash are injured in LMICs compared to higher income countries. The authors have also noted that multiple casualty injuries are more the norm than the exception, and this has implications for the design of prehospital systems and the training and protocols in the casualty ward, which must be ready to receive several severely injured patients at a time.
Third, very few patients (less than 5%) were brought to the hospital by ambulance, with the majority of injured patients brought in private cars, by the police, and by bystanders. This rate has not changed significantly since earlier reports from the registry, suggesting that there has been limited progress in the development of a formal prehospital system. Though ambulances do exist in Kampala, they are privately run, and families must be able to afford the cost, which the majority cannot. Others have suggested that the majority of potentially avertable deaths in severely injured patients occur in the prehospital setting [2]. In Kampala, records of fatalities from the prehospital setting are captured by the police or by the public city mortuary. An analysis of trauma-related deaths from mortuary data may help to clarify the proportion of deaths and disabilities that may have been preventable by improved prehospital care. In the absence of an ambulance-based prehospital system, prior work has suggested that in regions of high injury incidence, initiatives to improve knowledge and skills of lay responders may be a feasible, cost-effective, and critical first step towards developing a formal emergency system [22]. These initiatives deserve further study [23, 24].
Finally, a primary finding of prior analysis is the preponderance of minor injuries presenting to the National Hospital, congesting the hospital and perhaps impeding the care of more severely injured patients. Our findings show a similar pattern and suggest that a more organized prehospital system might triage patients with less severe injuries to other health centers to decongest the tertiary care facility. This would require more thorough evaluation of the capacity of lower level health facilities to receive and care for injured patients. Qualitative interviews with Kampala residents during this study indicated that most patients prefer to attend Mulago Hospital because it is a government hospital with highly subsidized health care, unlike the only other options in the city, which are all private hospitals. Nevertheless, many injured patients still do not seek care because of other barriers to access to care, whether these are cultural, social, economic, or geographic. Prior work has suggested that up to 80% of patients with fractures present first to a traditional healer before coming to a hospital [25, 26]. Causes of this health-seeking behavior need to be further identified.
Hospital-based registries are limited because they do not capture injured patients who do not interact with the health system. A community survey in Ghana showed that 30% of patients with severe injuries did not access formal care [27]. Prior community surveys in Kampala have demonstrated that large proportion of injured patients die without reaching care, with a mortality rate of 2.2/1,000 per year, which is higher than that seen in this data [28]. There were 72 deaths recorded in the trauma registry, which is likely to be a gross underestimate of total deaths from injuries since a large proportion of deaths are likely to have occurred in the prehospital setting. Hospital-based death data should be analyzed with police and city mortuary data to calculate a better estimate of injury mortality in Kampala.
A large proportion of trauma deaths was due to head injuries in this study. Improving access to emergency neurosurgical care may have the potential to prevent a substantial proportion of these deaths. Prior reports have suggested that the human resources and infrastructure for neurosurgical care are very limited in sub-Saharan Africa. A more detailed mortality audit at the hospital level may help to determine how to improve care for patients with head injuries who reach the hospital [29]. Other strategies to decrease trauma mortality in similar settings have included the introduction of a trauma education course for health personnel [30]. This intervention is currently underway in Uganda, and an understanding of its effectiveness will add greatly to the provision of injury care in Kampala.
Conclusion
Road traffic injuries are by far the largest cause of both morbidity and mortality seen in the government hospital in Kampala. They are the most common cause of injury for all ages except those less than 5, and school-aged children comprise a large proportion of victims from these incidents. The preponderance of minor injuries seen at the National Hospital suggests that lower level facilities could be better equipped to handle these injuries to decongest the National Hospital. The development of prehospital trauma care should be a high priority area given that less than 5% of patients arrived by ambulance. Our data show that injuries of the head, face, and neck account for a large proportion of injured patients, and is the most common body part injured in both discharged and admitted (and those who died in the hospital) patients. While more research needs to be done on appropriate and effective interventions, our findings point to patterns of injury that should be targeted in future injury control programs. The integration of injury control programs with ongoing health initiatives is an urgent priority for health and development.
Acknowledgement
None
Conflicts of interest None.
Funding None
Biography
Dr. Renee Hsia is an emergency physician who has worked extensively in sub-Saharan Africa both clinically and for research, and is currently an Assistant Professor of Emergency Medicine at the University of California, San Francisco (UCSF). This relationship with the Mulago Hospital was first developed by Dr. Doruk Ozgediz, who was Assistant Professor of Surgery at UCSF, and spent over a year living in Uganda to help collect this data from the trauma registry. Mr. Milton Mutto was the executive director of the Injury Control Center- Uganda at the time, which was originally started under the aegis of Dr. Olive C. Kobusingye, who went from the ICC-U to the Regional Office for Africa at the World Health Organization, based in Harare, Zimbabwe. Drs. Sudha Jayaraman (UCSF) and Patrick Kyamanywa have spent significant periods of time in Kampala also helping analyze the data and develop this study.
References
- 1.Laxminarayan R, Mills AJ, Breman JG, Measham AR, Alleyne G, Claeson M, et al. Advancement of global health: key messages from the Disease Control Priorities Project. Lancet. 2006;367(9517):1193–1208. doi: 10.1016/S0140-6736(06)68440-7. [DOI] [PubMed] [Google Scholar]
- 2.Mock CN, Jurkovich GJ, nii-Amon-Kotei D, Arreola-Risa C, Maier RV. Trauma mortality patterns in three nations at different economic levels: implications for global trauma system development. J Trauma. 1998;44(5):804–812. doi: 10.1097/00005373-199805000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Krug E. Road traffic injury fact sheet. Geneva: World Health Organization; 2004. [Google Scholar]
- 4.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367(9524):1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 5.Lagarde E. Road traffic injury is an escalating burden in Africa and deserves proportionate research efforts. PLoS Med. 2007;4(6):e170. doi: 10.1371/journal.pmed.0040170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hofman K, Primack A, Keusch G, Hrynkow S. Addressing the growing burden of trauma and injury in low- and middle-income countries. Am J Public Health. 2005;95(1):13–17. doi: 10.2105/AJPH.2004.039354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andrews C, Kobusingye O, Lett R. Road traffic accident injuries in Kampala. East Afr Med J. 1999;76(4):189–194. [PubMed] [Google Scholar]
- 8.Kobusingye O, Lett R. Hospital trauma registries in Uganda. J Trauma. 2000;48:498–502. doi: 10.1097/00005373-200003000-00022. [DOI] [PubMed] [Google Scholar]
- 9.Taye M, Munie T. Trauma registry in Tikur Anbessa Hospital, Addis Ababa, Ethiopia. Ethiop Med J. 2003;41(3):221–226. [PubMed] [Google Scholar]
- 10.Lett R, Kobusingye OC, Asingwire N, Ssengooba F. Trauma team training course: evaluation of Ugandan implementation. Afr Saf Promot. 2004;2:78–92. [Google Scholar]
- 11.Injury Policy. Kampala: Ministry of Health, 2004
- 12.Ascione FR, Weber CV, Thompson TM, Heath J, Maruyama M, Hayashi K. Battered pets and domestic violence: animal abuse reported by women experiencing intimate violence and by nonabused women. Violence Against Women. 2007;13(4):354–373. doi: 10.1177/1077801207299201. [DOI] [PubMed] [Google Scholar]
- 13.Kobusingye OC, Guwatudde D, Owor G, Lett R. Citywide trauma experience in Kampala, Uganda: a call for intervention. Inj Prev. 2002;8:133–136. doi: 10.1136/ip.8.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World report on child injury prevention. Geneva: World Health Organization; 2008. [PubMed] [Google Scholar]
- 15.Mock CN, Boland E, Acheampong F, Adjei S. Long-term injury related disability in Ghana. Disabil Rehabil. 2003;25(13):732–741. doi: 10.1080/0963828031000090524. [DOI] [PubMed] [Google Scholar]
- 16.Hyder AA, Peden M. Inequality and road-traffic injuries: call for action. Lancet. 2003;362(9401):2034–2035. doi: 10.1016/S0140-6736(03)15145-8. [DOI] [PubMed] [Google Scholar]
- 17.Bickler SW, Rode H. Surgical services for children in developing countries. Bull World Health Organ. 2002;80(10):829–835. [PMC free article] [PubMed] [Google Scholar]
- 18.Shen C, Sanno-Duanda B, Bickler SW. Pediatric trauma at a government referral hospital in The Gambia. West Afr J Med. 2003;22(4):287–290. doi: 10.4314/wajm.v22i4.28048. [DOI] [PubMed] [Google Scholar]
- 19.Hyder AA, Labinjo M, Muzaffar SS. A new challenge to child and adolescent survival in urban Africa: an increasing burden of road traffic injuries. Traffic Inj Prev. 2006;7(4):381–388. doi: 10.1080/15389580600942965. [DOI] [PubMed] [Google Scholar]
- 20.Duperrex O, Roberts I, Bunn F. Safety education of pedestrians for injury prevention. Cochrane database of systematic reviews (Online) 2002(2):CD001531 [DOI] [PMC free article] [PubMed]
- 21.Ameratunga S, Hijar M, Norton R. Road-traffic injuries: confronting disparities to address a global-health problem. Lancet. 2006;367(9521):1533–1540. doi: 10.1016/S0140-6736(06)68654-6. [DOI] [PubMed] [Google Scholar]
- 22.Tiska MA, Adu-Ampofo M, Boakye G, Tuuli L, Mock CN. A model of prehospital trauma training for lay persons devised in Africa. Emerg Med J. 2004;21:237–239. doi: 10.1136/emj.2002.002097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Husum H, Gilbert M, Wisborg T, Heng Y, Murad M. Rural prehospital trauma systems improve trauma outcome in low-income countries: a prospective study from North Iraq and Cambodia. J Trauma. 2003;54(6):1188–1196. doi: 10.1097/01.TA.0000073609.12530.19. [DOI] [PubMed] [Google Scholar]
- 24.Kobusingye OC, Hyder AA, Bishai D, Joshipura M, Hicks ER, Mock C, et al. Emergency Medical Services. In: Jamison DT, et al., editors. Disease control priorities in developing countries. 2. New York and Oxford: Oxford University Press; 2006. [Google Scholar]
- 25.Alonge TO, Dongo AE, Nottidge TE, Omololu AB, Ogunlade SO. Traditional bonesetters in south western Nigeria–friends or foes? West Afr J Med. 2004;23(1):81–84. doi: 10.4314/wajm.v23i1.28091. [DOI] [PubMed] [Google Scholar]
- 26.Onuminya A. The role of the traditional bone-setter in primary fracture care in Nigeria. S Afr Med J. 2004;94(8):652–658. [PubMed] [Google Scholar]
- 27.Mock CN, nii-Amon-Kotei D, Maier RV. Low utilization of formal medical services by injured persons in a developing nation: health service data underestimate the importance of trauma. J Trauma. 1997;42(3):504–511. doi: 10.1097/00005373-199703000-00019. [DOI] [PubMed] [Google Scholar]
- 28.Kobusingye O, Guwatudde D, Lett R. Injury patterns in rural and urban Uganda. Inj Prev. 2001;7(1):46–50. doi: 10.1136/ip.7.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Khamlichi A. Neurosurgery in Africa. Clin Neurosurg. 2005;52:214–217. [PubMed] [Google Scholar]
- 30.Ali J, Adam R, Butler AK, Chang H, Howard M, Gonsalves D, et al. Trauma outcome improves following the advanced trauma life support program in a developing country. J Trauma. 1993;34(6):890–898. doi: 10.1097/00005373-199306000-00022. [DOI] [PubMed] [Google Scholar]