Abstract
Mesenchymal stem cells (MSC) are multipotent postnatal stem cells, involved in the treatment of ischemic vascular diseases. We investigate the ability of MSC, exposed to short-term hypoxic conditions, to participate in vascular and tissue regeneration in an in vivo model of hindlimb ischemia. Transplantation of hypoxic preconditioned murine MSC (HypMSC) enhanced skeletal muscle regeneration at day 7, improved blood flow and vascular formation compared to injected nonpreconditioned MSC (NormMSC). These observed effects were correlated with an increase in HypMSC engraftment and a putative role in necrotic skeletal muscle fiber clearance. Moreover, HypMSC transplantation resulted in a large increase in Wnt4 (wingless-related MMTV integration site 4) expression and we demonstrate its functional significance on MSC proliferation and migration, endothelial cell (EC) migration, as well as myoblast differentiation. Furthermore, suppression of Wnt4 expression in HypMSC, abrogated the hypoxia-induced vascular regenerative properties of these cells in the mouse hindlimb ischemia model. Our data suggest that hypoxic preconditioning plays a critical role in the functional capabilities of MSC, shifting MSC location in situ to enhance ischemic tissue recovery, facilitating vascular cell mobilization, and skeletal muscle fiber regeneration via a paracrine Wnt-dependent mechanism.
Introduction
Bone marrow mesenchymal stem cells (MSC) can be isolated from bone marrow-derived mononuclear cells, expanded in vitro and have been shown to possess functional multilineage differentiation capacity.1 MSC have been shown to differentiate into pericytes,2 vascular endothelial cells (EC),3,4 and cardiomyocytes,5 and their transplantation has improved recovery from ischemia in rat hindlimb and swine dilated cardiomyopathy models.6 Their precocious role in the formation and the maintenance of neovessels has been studied extensively.2,7 Such reports have led to the hypothesis that MSC may be used in the treatment of ischemic cardiovascular pathologies. One major limitation demonstrated in both animal and human experiments has been the inability to maintain a large number of cells after grafting into hypoxic sites. In the present study, we employed a strategy of low oxygen (O2)-preconditioning of MSC before tissue implantation. We hypothesized that creating this hypoxic environment might mimic the stem cell niche microenvironment in vivo which others have hypothesized to likely create a hypoxic cavity.8 We chose to study 1% O2 concentration because it has been reported as the level found in vivo in bone marrow stem cell niche areas.9 Moreover, data from animal studies have demonstrated a role of hypoxic gradients in stem cell trafficking in ischemic tissue.10 On the molecular level, temporary oxygen deprivation is known to regulate gene transcription and differentiation of stem cells.11,12
Several reports suggest that the Wnt (wingless-related MMTV integration site) pathway plays a role in maintaining hematopoietic stem cell self-renewal and pluripotency.13,14 The Wnt family of genes encodes over 20 cysteine-rich secreted glycoproteins to regulate canonical and noncanonical signaling pathways.15 The canonical Wnt pathway regulates gene expression due to the stabilization and nuclear localization of J3 catenin. We have previously demonstrated that MSC have a structural role in forming a precocious network and facilitating neovessel recruitment in an angiogenic model and reported that overexpression of a soluble modulator of Wnt functions, secreted frizzled-related protein 1 (sFRP-1), in MSC, enhanced their angiogenic capacities.2 Experimental manipulation of a pluripotent mouse embryonal carcinoma stem cell line via another secreted Wnt modulator, sFRP-2, identified the Wnt pathway in cardiomyogenic differentiation.16 Wnt3a activation modulated proliferation and differentiation of human MSC and murine embryonic mesenchymal cells.17,18 Recently, another study demonstrated a role of the Wnt signaling pathway in the acquisition of the invasion property of human MSC.19 These data have been particularly important to help elucidate the molecular mechanism that enables MSC to contribute to tissue regeneration under ischemic conditions.
In the present study, we compare the ability, of hypoxic preconditioned murine MSC (HypMSC) and nonpreconditioned MSC (NormMSC), to engraft into ischemic tissue and assessed the ability of these cells to participate in skeletal tissue and vascular regeneration. A subacute murine limb ischemia model was used to mimic the clinical setting of critical limb ischemia in patients. Our results demonstrate that HypMSC have a greater capacity for engraftment in ischemic tissue compared to NormMSC. HypMSC also improved skeletal muscle regeneration and induced more neoangiogenesis, and elicited significant improvement in blood flow as compared to NormMSC. Localization of HypMSC compared to NormMSC suggests that HypMSC participate in the remodeling of the stromal environment via structural interactions, first in encircling necrotic myocytes and then shaping a tight network around EC along growing neovessels. This preferential localization led us to speculate that MSC could functionally interact via paracrine effectors with myocytes and EC. Our data demonstrates that MSC express Wnt4 and in vivo Wnt4 transcripts were significantly increased in ischemic muscles engrafted with HypMSC whereas in muscle engrafted with NormMSC no significant increase was detected. We tested the biological activity of Wnt4 in vitro and found that it could stimulate EC migration, myogenic differentiation, and MSC proliferation but had no effect on EC proliferation. Importantly, inhibition of Wnt4 expression in MSC abrogated HypMSC-induced vascular regeneration. Our data provides strong evidence that Wnt signaling could be an important factor in the mechanism by which MSC contribute to tissue regeneration, as well as vessel formation and stabilization. As such, hypoxia preconditioning of MSC could be an attractive therapeutic approach for the treatment of ischemic vascular diseases.
Results
Vascular and muscle regeneration of the ischemic hindlimb was improved after transplantation of HypMSC versus NormMSC
We examined the comparative effectiveness of transplanted murine HypMSC versus NormMSC for vascular and ischemic muscle regeneration after femoral ligation in C57BL/6J mice. Three groups were set up: a control sham group receiving saline injection, a NormMSC group receiving by intramuscular injection 0.5 × 106 MSC cultured in normoxia (20% O2) and a HypMSC group transplanted with 0.5 × 106 MSC pretreated during 36 hours in a reduced oxygen tension (1% O2).
HypMSC-enhanced vascular response. Blood flow recovery in the limb of HypMSC-treated animals was significantly improved when compared with sham-treated animals or NormMSC-treated animals (Figure 1a,b).
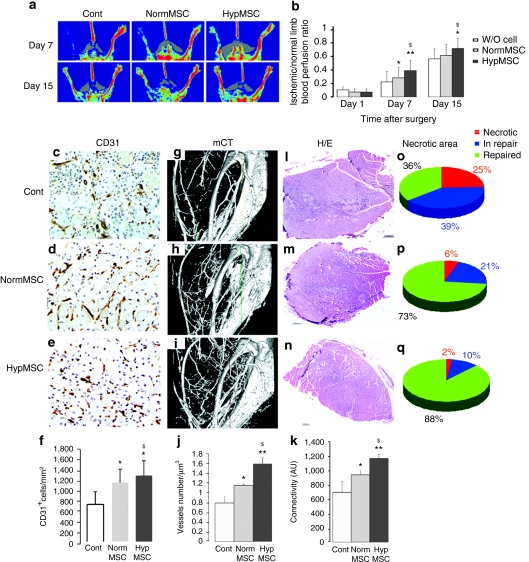
Figure 1.
Augmented vascular regeneration by intramuscular transplantation of MSC in a hindlimb ischemia model. (a) Images of representative LPDI in sham mice (control W/O cell) and in HypMSC or NorMSC transplanted groups at day 7 (n = 21) and day 15 (n = 15) after ischemia. (b) Quantitative analysis of hindlimb blood perfusion by calculating the ischemic/normal limb perfusion ratios after the induction of hindlimb ischemia. Blood perfusion of the ischemic hindlimb markedly increased in the HypMSC and NormMSC group 1 week after transplantation. LPDI index in the HypMSC group was the highest among the three groups at day 7 and day 15. Data are means ± SEM; *P < 0.05 and *P < 0.01 versus control; $P < 0.05 versus NormMSC. (c–f) Vessel numbers were calculated after CD31 immunolabeling in the control, NormMSC, and HypMSC groups. *P < 0.00001 versus control; $P < 0.001 versus NormMSC. (g–i) Reconstructed micro-CT images of control, NormMSC, or HypMSC-injected hindlimb 7 days after ischemia in age- and gender-matched mice (tm3 resolution). Note marked increase in (j) vessel number and in (k) connectivity in HypMSC-treated mice versus NormMSC-treated mice and control mice. Data are % ± SEM; *P < 0.05 and **P < 0.001 versus control; $P < 0.05 versus NormMSC. n = 6 in each group. Repaired surface measurement of control and MSC group (n = 6 in each group) in hindlimb ischemic mice. (l–q) Representative repaired surface and necrotic area were quantified as ratio of necrotic or in repair or repaired surface out of total muscle area. cont., control; HypMSC, hypoxic preconditioned murine MSC; LPDI, laser doppler perfusion imaging; MSC, mesenchymal stem cells; NormMSC, nonpreconditioned MSC; W/O, without.
The therapeutic action of HypMSC was also evident at the angiogenic level, as evidenced by quantification of only viable muscle, excluding angiogenesis involved in an inflammatory response to granulation tissue. At day 15, there was an increase in CD31+ capillary number in HypMSC-treated muscles compared respectively with that in sham-treated control (P < 10‐5) and in NormMSC groups (P < 10‐3) at day 15 (Figure 1c–f). These results suggest a potent role of HypMSC in new-vessel formation. Consistent with improved limb perfusion and capillary density, micro scanner (microcomputed tomography) analysis of the whole arterial network revealed the global impact of HypMSC on vessel formation in the hindlimb after ischemia. Images showed a greater number of vessels in HypMSC-treated hindlimb compared to NormMSC or sham-treated injected hindlimb at day 8 after the insult (Figure 1g–k). We calculated a twofold increase in the vessel number (number of vessels/µm3, P < 0.01) and a 1.7-fold increase in their connectivity and branching (P < 0.01) in the HypMSC-treated hindlimb compared with sham-treated control animals whereas NormMSC-treated animals were at an intermediate level (P < 0.05) (Figure 1j–k).
HypMSC-enhanced muscle regeneration. Histological evaluation of muscle tissue, performed to analyze the impact of HypMSC transplantation on the repair process, revealed that administration of either HypMSC or NorMSC accelerated the repair process. At day 7, almost no overt necrotic area was found in either of the MSC-treated groups, whereas necrotic muscle fibers were markedly observed in sham-treated muscles (25% out of total muscle surface). However, HypMSC engraftment had a significant beneficial effect on muscle regeneration when compared with NormMSC-treated group. Less than 10% of the histological area in the ischemic muscle were still actively regenerating in HypMSC-treated tissue whereas in the NormMSC-treated group, the process was delayed with over 21% of the total muscle surface was still actively regenerating (Figure 1l–q).
Hypoxic pretreatment modified MSC engraftment in ischemic hindlimb
MSC were infected with a lentivirus encoding for the GFP gene [green fluorescent protein (GFP)-MSC] and expression was followed as a marker of viable GFP+ MSC.2 HypMSC robustly engrafted the adductor and tibial muscles in large patches, as revealed by direct fluorescence at day 7 (Supplementary Figure S1a) or anti-GFP immunohistochemistry at day 14 (Supplementary Figure S1b).
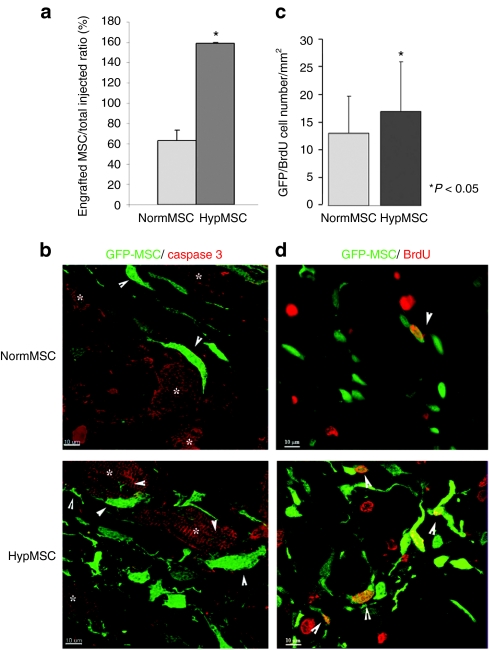
Hypoxic treatment improved MSC survival capacities in vivo. Real-time reverse transcription-PCR was performed using total RNA obtained from HypMSC- and NormMSC-injected muscles at day 7 after injury to determine the percentage of remaining GFP expression, and demonstrated that hypoxic pretreatment contributes to effective enhancement of MSC recruitment in vivo. In the HypMSC group, there was a significant increase in MSC engraftment at day 7 (150% of initially engrafted HypMSC) whereas in NormMSC group, the total number of MSC was not maintained after transplantation (63% of initially engrafted NormMSC) (Figure 2a). At day 7, caspase 3 labeling showed apoptotic muscle fibers surrounding by surviving Hyp and Norm GFP-MSC (Figure 2b). Double bromodeoxyuridine/GFP labeling revealed that bromodeoxyuridine incorporation rate was significantly increased in HypMSC group compared to NormMSC group (16.3 ± 8.1 versus 13.1 ± 6.6 bromodeoxyuridine/GFP + cells/mm2 P < 0.05) (Figure 2c–d).
Figure 2.
Engraftment, survival, and proliferation of MSC in ischemic hindlimb tissues. (a) Engraftment of GFP-MSC in muscle. The levels of GFP expression was determined by performing real-time RT-PCR. The percentage of engrafted MSC was assessed by the ratio of GFP level at day 7 with that of GFP level at D0 (initial MSC graft) (n = 4 in NormMSC and HypMSC groups). The histogram showed a higher persistence of MSC in the muscle at day 7 after injury in HypMSC-treated groups compared to NormMSC-treated group. *P < 0.05, n = 10. After 7 days of ischemia, (b) survival assay of MSC and (c–d) induction of MSC proliferation were assessed using respectively a double GFP (green)/caspase 3 (red) and a double GFP (green)/BrdU (red) immunofluorescent-labeling performed on NormMSC and HypMSC transplanted tissue sections. (b) Representative photomicrographs at day 7 after ischemia showed MSC (arrowhead) surrounding caspase 3 positive myocytes (white star). (c) The levels of double GFP/BrdU NormMSC and HypMSC (white arrowheads) were quantified and reported in histogram graphs. (d) Representative photomicrographs of ischemic hindlimb sections at day 7 after ischemia revealed a higher level of proliferating GFP-MSC in HypMSC-injected tissues compared to that in NormMSC-injected tissues. *P < 0.05, n = 10. BrdU, bromodeoxyuridine; GFP, green fluorescent protein; HypMSC, hypoxic preconditioned murine MSC; MSC, mesenchymal stem cells; NormMSC, nonpreconditioned MSC; RT, reverse transcription.
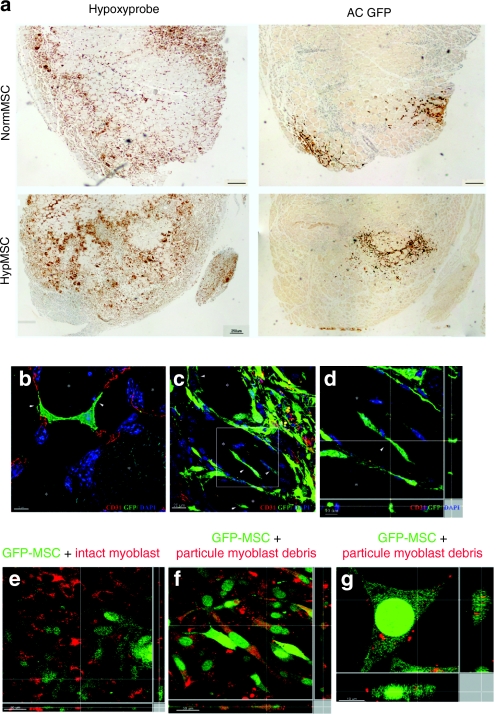
HypMSC were widespread in hypoxic zones and may play a macrophage-like function. HypMSC appeared to have a different pattern of engraftment as compared to NormMSC. To better understand this, we evaluated the scattering of MSC in hypoxic zones using the 2-nitroimidazole hypoxia marker, pimonidazole. Hypoxic sections of muscle produced a mottled staining with a characteristic hypoxic brown center. At day 7, a large number of GFP+ HypMSC were evenly distributed in deep hypoxic zones around necrotic myocytes whereas GFP+ NormMSC were consistently detected at the periphery of ischemic zones (Figure 3a and Supplementary Figure S2). The distribution of MSC around necrotic myocytes suggested a potential macrophage-like, phagocytic function for these cells. GFP immunofluorescent staining revealed that MSC harbor a phenotype with long filopodial protrusions that can encircle and penetrate into dead myocytes (Figure 3b–d). To evaluate the phagocytic capacity of MSC in regards to myocytes, in vitro experiments were conducted. Fluorescent microscopy examination revealed that GFP-MSC cocultured with necrotic cell bodies of PKH-labeled murine myoblasts (red) were able to robustly engulf part of the myoblast cell membranes (Figure 3f,g). GFP-MSC cocultured with non-necrotic PKH-labeled murine myoblasts (red) did not have this property (Figure 3e). At day 15, HypMSC appeared to be preferentially associated with capillaries and microvessels, behaving as perivascular cells shaping along the whole length of the vessel, covering growing CD31-forming tube-like structures, as mural cells (Supplementary Figure S3).
Figure 3.
HypMSC engraftment sites could assist MSC in their macrophagic-like role. (a) At day 4, hindlimb muscles transplanted with either NormMSC or HypMSC have large hypoxic zones as revealed using pimonidazole binding (Hypoxyprobe). Immunostaining of GFP-MSC with an antibody directed against GFP (AC anti-GFP) showed localization of NormMSC at the peripheral front of hypoxia although HypMSC displayed a scattered distribution inside hypoxia zone. MSC macrophagic activity. (b) Immunofluorescent analysis for GFP expression (green) with CD31 (red) on hindlimb tissue section at day 4, revealed that during muscle regeneration, GFP+ MSC (green) surrounded necrotic muscle fiber, harboring a spindle shape with long filopodial extensions. (c) Arrow heads point to MSC extensions, which enter through necrotic skeletal muscle fibers (d) close-up of the boxed region in the larger image. White stars indicate necrotic muscle fiber. Cell nuclei are stained with DAPI (blue). In vitro (e) GFP+ MSC were mixed with intact PKH-labeled skeletal muscle fibers or (f,g) in contact with PKH-labeled skeletal muscle fiber particulate debris. In presence of muscle fiber membrane debris, MSC have the capacity to phagocyte particles. (d–g) The cartoons at right and bottom end side represent perpendicular views of the confocal acquired images. (f,g) White lines show myocyte red particulate debris in GFP-MSC cytoplasm. AC,; GFP, green fluorescent protein; HypMSC, hypoxic preconditioned murine MSC; MSC, mesenchymal stem cells.
HypMSC paracrine Wnt-dependent effect on angiogenesis and muscle regeneration
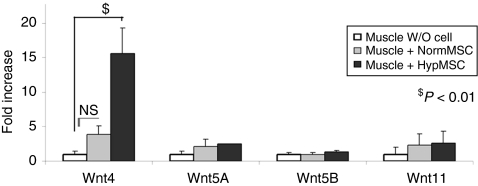
The effects of temporary hypoxia on Wnt factor expression were also investigated. Several studies have demonstrated a role of the Wnt pathway in vascular development20 as well as stem cell proliferation and maintenance.13 We hypothesized that MSC express Wnt and use the Wnt pathway as a mechanism for activation of muscle regeneration processes. Screening by reverse transcription-PCR for the expression of different Wnt transcripts revealed that MSC express Wnt4, 5A, 5B, and 11. In vivo, Wnt4 transcripts were significantly increased in HypMSC-injected muscles (ratio Wnt4/P0: 15.6 ± 5.2, P = 0.01 versus control tissues) whereas NormMSC implantation did not significantly increase Wnt4 transcripts (ratio Wnt4/P0: 3.8 ± 1.8, P = NS versus control tissues) (Figure 4). Wnt5A, 5B, and 11 expressions were not significantly modified in either HypMSC- and NormMSC-injected muscles compared with control muscle at day 7 after ischemia. Corroborating evidence was found in vitro where a specific strong upregulation of Wnt4 was detected after exposing MSC to hypoxia for 36 hours compared to normoxia-treated MSC (Wnt4/P0: 4.78 ± 1.8, P = 0.01 in comparison to control) (Supplementary Figure S4). In parallel, we report preconditioning effects on angiogenic growth factor expressions by HypMSC (Supplementary Figure S4a–c).
Figure 4.
Effects of HypMSC transplantation on Wnt gene expressions. Wnt4, 5A, 5B, and 11 expressions in hindlimb ischemic muscle were analyzed by performing real-time PCR. Hindlimb muscles transplanted with NormMSC (gray bars) or HypMSC (black bars) or without cells (sham group, white bars) were extracted at day 7 after ischemia. Values are means ± SD; n = 3; the assays were carried out in triplicate. *P < 0.05, §P < 0.01 versus control. HypMSC, hypoxic preconditioned murine MSC; NormMSC, nonpreconditioned MSC.
Functional validation of HypMSC secreted factors on cell functions
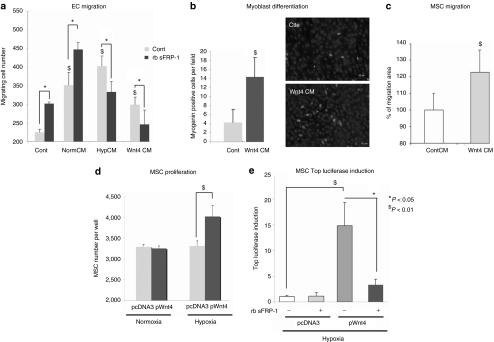
To further elucidate the functional paracrine and autocrine role of HypMSC secreted factors in vascular response and muscle regeneration enhancement, we studied the effect of ex vivo incubation of the different cellular components namely EC, muscle fibers, and MSC with HypMSC and Wnt4 conditioned medium (HypCM and Wnt4 CM, respectively).
HypMSC secreted factors and Wnt4 played a role on EC migration but not on EC proliferation. Transwell filters revealed that HypCM and Wnt4 CM induced significantly more migration of EC than did respectively CM from NormMSC (NormCM) and control CM (P < 0.05). Moreover, addition of a secreted Wnt antagonist, recombinant bovine sFRP-1, blocked the HypCM-induced migration suggesting that Wnt-dependent factors are the major active factors present in HypCM. (Figure 5a and Supplementary Figure S5). It is worth noting that recombinant bovine sFRP-1 enhanced migration of both NormCM-treated EC and control EC, which is in agreement with previous reports.21 Interestingly, HypCM had no effect on EAHy926 proliferation compared with CM from NormMSC (NorCM) (data not shown). Taken together, these results support a role of HypCM and Wnt4 on EC migration.
Figure 5.
Effect of HypCM and Wnt4 CM on cell properties. (a) Endothelial cell chemotactic migration was quantified using transwell filters. Fluorescent-labeled EAHy926 migrated in the presence in the lower chamber of either NormCM, HypCM, and Wnt4CM with or without rb sFRP-1 in the lower chamber. Migrated EC were then lysed and quantified on a fluorimeter. All the CM induced EAHy926 migration. *P < 0.05, $P < 0.01 versus control. rbsFRP-1 induced migration in NormCM assays and blocked HypCM and Wnt4CM induced EAHy926 migration (*P < 0.05). (b) Muscle fibers were cultured either in control CM (cont. CM) or in Wnt4 CM during 48 hours. Increase expression of myogenin assessed an effect of Wnt4 on myoblast differentiation. The numbers of myogenin-positive nuclei were reported on the graph. $P < 0.01. (c) The effect of Wnt4 on MSC migration was quantified after in an in vitro wound assay. Confluent MSC were wounded and placed during 16 hours in presence of either control CM (cont. CM) or Wnt4 CM. Analysis of Wnt4 effect on wound closure was measured as area of migration (µm2) on phase contrast microscopy images. $P < 0.01. (d) MSC proliferation of MSC was influenced by Wnt4 overexpression (pWnt4 versus pCDNA3, $P < 0.01) in hypoxia but not in normoxia. MSC were maintained during 24 hours either in normoxia or in hypoxia after transfection before counting. Values correspond to total cell numbers per well. (e) Wnt4 activates the TopFlash reporter in MSC. Cotransfection of MSC with TopFlash or FopFlash reporter and Wnt4 resulted in more than a 15-fold increase in TopFlash over FopFlash activity compared with MSC transfected with an empty vector (pcDNA3) in hypoxia condition ($P < 0.01). Adding of rb sFRP-1 blocked either Wnt4 overexpression induced TopFlash over FopFlash activity (*P < 0.05). The experiments were conducted in hypoxia. The error bars indicate on SD from the mean of triplicate samples. EC, endothelial cell; HypCM,; MSC, mesenchymal stem cells; rb, recombinant bovine; sFRP-1, secreted frizzled-related protein 1.
Wnt4-induced skeletal myoblast differentiation. To explore the potential role of Wnt4 on skeletal muscle differentiation, intact primary murine skeletal myoblasts were cultured in the presence of Wnt4 CM for 16 hours and compared with myoblasts treated with control CM. The results revealed that the number of myogenin-expressing cells was significantly increased in Wnt4-treated myoblast culture compared to control condition (P < 0.01) (Figure 5b).
Autocrine role of Wnt4 promoted MSC proliferation, migration and Wnt canonical ß-catenin pathway activation. We then tested the hypothesis that enhancement of HypMSC engraftment could be due in part to Wnt4 upregulation. The role of Wnt4 as a potent inducer of MSC migration was demonstrated (Figure 5c). In addition, data revealed an effect of Wnt4 on the number of MSC but only under hypoxic conditions (Figure 5d). Moreover, Wnt4 was able to activate the canonical Wnt pathway as shown by T-cell factor-dependent transcriptional activity measured under hypoxic conditions; transfection of MSC with a plasmid coding for Wnt4 provoked a 15-fold increase in luciferase activity (Figure 5e). No activation was seen by using the corresponding control reporter with mutated T-cell factor binding sites. Inhibition of Wnt signaling using recombinant bovine sFRP-1 also effectively suppressed TopFlash luciferase reporter activities in response to Wnt4. Our data are consistent with the interpretation that Wnt4 signals are transduced via the canonical branch of the Wnt pathway and reveal that MSC respond to Wnt4 stimuli in a hypoxic environment.
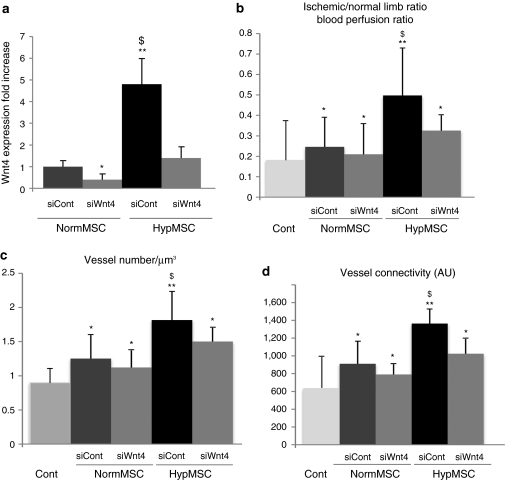
Suppression of Wnt4 expression in HypMSC prevented the vascular regenerative response induced by hypoxia pretreatment. An in vivo model of Wnt4 suppression was employed to demonstrate the importance of Wnt4 as a key paracrine factor mediating proangiogenic effects of HypMSCs. As such, we treated HypMSC with two small interfering RNA against Wnt4 (Figure 6a) and transplanted them into the mouse ischemic hindlimb model. We showed that siControl-treated HypMSC compared to siControl-treated NormMSC enhanced significantly the blood flow (P < 0.05) (Figure 6b), and vascular density (P < 0.05) and connectivity (P < 0.05) (Figure 6c–d). Treatment of HypMSC with small interfering RNA against Wnt4 abrogated the difference between HypMSC and NormMSC groups; either blood flow or vascular density and connectivity were not significantly different between siWnt4-treated HypMSC and siControl-treated NormMSC groups.
Figure 6.
Effect of Wnt4 knockdown on NormMSC or HypMSC treated with siControl (siCont) or with siWnt4. (a) On Wnt4 expression in vitro followed by performing real-time PCR. (b–d) On vascular effect induced by MSC: quantitative analysis of hindlimb blood perfusion by calculating the ischemic/normal limb perfusion ratios after the induction of (b) ischemia, and microCT quantification of (c) vessel number and (d) connectivity at D7 after injury in mice transplanted either with NormMSC or HypMSC treated with siControl (siCont) or with siWnt4 or not transplanted (cont.). Data are % ± SEM; *P < 0.05 and **P < 0.001 versus control. $P < 0.05 versus NormMSC. N = 9 in each group. cont. control; HypMSC, hypoxic preconditioned murine MSC; microCT, micro-computed tomography; MSC, mesenchymal stem cells; NormMSC, nonpreconditioned MSC.
Discussion
The influence of temporary hypoxic preconditioning of MSC on the stimulation of angiogenesis and muscle regeneration was investigated and the data revealed that ex vivo hypoxic preconditioning of MSC plays a unique role in the enhancement of vessel formation and repair of the necrotic zone after a hindlimb ischemia via a Wnt-dependent pathway.
We hypothesized that the 1% oxygen atmosphere in which MSC were maintained could condition them to survive in a hypoxic environment in vivo as reported in vitro.22,23 Oxygen tension in bone marrow compartments has been reported to be very low as in injured tissue, suggesting that tissue hypoxia may be a fundamental mechanism governing stem cell recruitment and retention.10 As a result, we demonstrated that hypoxic pretreatment can more effectively overcome the hurdle of cell death after implantation than normoxic conditioning, promoting MSC survival, and proliferation in situ. HypMSC engrafted robustly in ischemic tissue and their proliferation index in ischemic sites was superior to that of NormMSC. The decline MSC number that has been previously described could be due to cytokine secretion and tissue remodeling24 or immune rejection by the host as they expressed GFP a well-known immunogen.25
MSC have been successively administered as a treatment in both animal studies6,24,26 and human clinical trials.27,28 Studies showed their possible contribution to vascular structures and skeletal muscle in vivo. For example, injection of MSC in a rat model of dilated cardiomyopathy revealed that some of the MSC were differentiated into cardiomyocytes.6 The application of MSC improves wound healing regeneration through differentiation.24 Recent studies suggest that monocytes under activation could express EC markers and form tube-like structures.29 The setting of hypoxic preconditioning in this study did not enhance cell differentiation into EC, as HypMSC kept their pericyte-like properties and behaved as perivascular cells as reported.2,30 Their tissue localization led us to hypothesize a potential macrophage-like role in which they participate in phagocytosis of necrotic muscle fibers. Our data indicates that MSC have the ability to participate in the phagocytic process of muscle fibers in vitro and to encircle and send extensions into necrotic muscle fibers in vivo, which could indicate that these cells participate in clearing skeletal muscle cellular debris. This process has similarities with previously published data which demonstrated that macrophages reorganize their actin cytoskeleton to form phagocytic lamellipodia structures to engulf apoptotic cells.31 Moreover, at early time points, MSC appear to play a role in neovessel formation encircling EC in capillaries and microvessels and participating in their stabilization as previously described.32,33 Our results support the notion that MSC play a cooperative role in both myocyte regeneration and vascular formation by structural and functional interaction with both myocytes and EC.
As MSC have been shown to secrete a large quantity of angiogenic factors,34 we investigated the potential involvement of paracrine and/or endocrine factors produced by MSC. Previous reports have demonstrated that conditioned medium from MSC can promote EC migration, differentiation, and survival.35 Our data indicate that conditioned medium from HypMSC is more effective than conditioned medium from NormMSC in inducing EC migration as well as MSC proliferation and migration. As the Wnt signaling pathway has been shown to play a role in stem cell fate,13 muscle regeneration,36 vascular formation,37 and invasion capacity of MSC,19 we hypothesized that this pathway may be involved in the mechanism involved in this process. Our study identified that Wnt4 was specifically overexpressed in vitro in conditioned media from HypMSC and that, in vivo, injection of HypMSC into the ischemic hindlimb strongly induced Wnt4 expression. We also demonstrate that Wnt4 exerts an effect on myoblast differentiation, in vitro. We have established a role of Wnt4 as a potent mediator in vascular regeneration as it affects EC migration. It is worth noting that Wnt4 conditioned medium could affect MSC migration and proliferation but only under hypoxic conditions through a canonical J3 catenin-dependent Wnt signaling. Thus, it is likely that, in situ, residual tissue hypoxia confers responsiveness of MSC to environmental signals. Moreover, Wnt4 signaling was shown to stimulate myogenic proliferation and differentiation during chick development38 and satellite cell proliferation in skeletal muscle in myostatin-knockout mice.39 Finally, we demonstrate here that, knockdown of Wnt4 expression resulted in inhibition of the beneficial impact of HypMSC on vascular regeneration compared with that induced by NormMSC. Collectively, these results strongly support the hypothesis that Wnt4 secreted by MSC is an important factor in mediating tissue regeneration in the setting of ischemia.
In conclusion, we have demonstrated that hypoxic preconditioning of MSC before transplantation could be a potent strategy in overcoming the current limitations in the field of regenerative medicine. This study suggests that many of the cellular functions associated with the ability of MSC to regenerate ischemic tissue are often not expressed constitutively by MSC but rather only transiently. MSC respond to contextual signals according to their microenvironment.
Materials and Methods
MSC2,26 were treated for 36 hours at 1% O2 in a hypoxia chamber (HypMSC) (C21 Proox chamber; BioSpherix, Lacona, New York) or maintained at 20% O2 (NormMSC) before being injected into a mouse ischemic hindlimb. Mice were randomly assigned to three treatment groups. One group underwent sham treatment (i.e., aperture and saline injection) (control group). The other groups received injection of either 0.5 × 106 NormMSC or HypMSC. Detailed description of materials, animal procedures, MSC preparation, hindlimb ischemia model, tissue collection and preparation for biochemical assays, laser doppler perfusion imaging, microcomputed tomography analysis, immunohistochemistry, macrophagic assays, and in vitro cell functional assays can be found in the Supplementary Materials and Methods.
SUPPLEMENTARY MATERIAL Figure S1. MSC detection. Figure S2. Double immunolabeling of GFP and CD31 in ischemic tissues at day 7 and day 15 after injury transplanted with either NormMSC or HypMSC. Figure S3. MSC harbored a pericyte-like phenotype after implantation in ischemic muscle at day 7. Figure S4. Effect of HypMSC transplantation on growth factor gene expressions and induction of growth factor and Wnt factors in HypMSC vs NormMSC. Figure S5. Effect of HypCM or Wnt4 CM on EC wound migration. Materials and Methods.
Supplementary Material
MSC detection.
Double immunolabeling of GFP and CD31 in ischemic tissues at day 7 and day 15 after injury transplanted with either NormMSC or HypMSC.
MSC harbored a pericyte-like phenotype after implantation in ischemic muscle at day 7.
Effect of HypMSC transplantation on growth factor gene expressions and induction of growth factor and Wnt factors in HypMSC vs NormMSC.
Effect of HypCM or Wnt4 CM on EC wound migration.
REFERENCES
- Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, et al. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284:143–147. doi: 10.1126/science.284.5411.143. [DOI] [PubMed] [Google Scholar]
- Dufourcq P, Descamps B, Tojais NF, Leroux L, Oses P, Daret D, et al. Secreted frizzled-related protein-1 enhances mesenchymal stem cell function in angiogenesis and contributes to neovessel maturation. Stem Cells. 2008;26:2991–3001. doi: 10.1634/stemcells.2008-0372. [DOI] [PubMed] [Google Scholar]
- Muguruma Y, Yahata T, Miyatake H, Sato T, Uno T, Itoh J, et al. Reconstitution of the functional human hematopoietic microenvironment derived from human mesenchymal stem cells in the murine bone marrow compartment. Blood. 2006;107:1878–1887. doi: 10.1182/blood-2005-06-2211. [DOI] [PubMed] [Google Scholar]
- Oswald J, Boxberger S, Jørgensen B, Feldmann S, Ehninger G, Bornhäuser M, et al. Mesenchymal stem cells can be differentiated into endothelial cells in vitro. Stem Cells. 2004;22:377–384. doi: 10.1634/stemcells.22-3-377. [DOI] [PubMed] [Google Scholar]
- Toma C, Pittenger MF, Cahill KS, Byrne BJ., and, Kessler PD. Human mesenchymal stem cells differentiate to a cardiomyocyte phenotype in the adult murine heart. Circulation. 2002;105:93–98. doi: 10.1161/hc0102.101442. [DOI] [PubMed] [Google Scholar]
- Nagaya N, Kangawa K, Itoh T, Iwase T, Murakami S, Miyahara Y, et al. Transplantation of mesenchymal stem cells improves cardiac function in a rat model of dilated cardiomyopathy. Circulation. 2005;112:1128–1135. doi: 10.1161/CIRCULATIONAHA.104.500447. [DOI] [PubMed] [Google Scholar]
- Abramsson A, Lindblom P., and, Betsholtz C. Endothelial and nonendothelial sources of PDGF-B regulate pericyte recruitment and influence vascular pattern formation in tumors. J Clin Invest. 2003;112:1142–1151. doi: 10.1172/JCI18549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore KA., and, Lemischka IR. Stem cells and their niches. Science. 2006;311:1880–1885. doi: 10.1126/science.1110542. [DOI] [PubMed] [Google Scholar]
- Chow DC, Wenning LA, Miller WM., and, Papoutsakis ET. Modeling pO(2) distributions in the bone marrow hematopoietic compartment. II. Modified Kroghian models. Biophys J. 2001;81:685–696. doi: 10.1016/S0006-3495(01)75733-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ceradini DJ, Kulkarni AR, Callaghan MJ, Tepper OM, Bastidas N, Kleinman ME, et al. Progenitor cell trafficking is regulated by hypoxic gradients through HIF-1 induction of SDF-1. Nat Med. 2004;10:858–864. doi: 10.1038/nm1075. [DOI] [PubMed] [Google Scholar]
- .Kovacevic-Filipovic M, Petakov M, Hermitte F, Debeissat C, Krstic A, Jovcic G, et al. Interleukin-6 (IL-6) and low O(2) concentration (1%) synergize to improve the maintenance of hematopoietic stem cells (pre-CFC) J Cell Physiol. 2007;212:68–75. doi: 10.1002/jcp.21003. [DOI] [PubMed] [Google Scholar]
- Potier E, Ferreira E, Andriamanalijaona R, Pujol JP, Oudina K, Logeart-Avramoglou D, et al. Hypoxia affects mesenchymal stromal cell osteogenic differentiation and angiogenic factor expression. Bone. 2007;40:1078–1087. doi: 10.1016/j.bone.2006.11.024. [DOI] [PubMed] [Google Scholar]
- Reya T, Duncan AW, Ailles L, Domen J, Scherer DC, Willert K, et al. A role for Wnt signalling in self-renewal of haematopoietic stem cells. Nature. 2003;423:409–414. doi: 10.1038/nature01593. [DOI] [PubMed] [Google Scholar]
- Malhotra S., and, Kincade PW. Wnt-related molecules and signaling pathway equilibrium in hematopoiesis. Cell Stem Cell. 2009;4:27–36. doi: 10.1016/j.stem.2008.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhanot P, Brink M, Samos CH, Hsieh JC, Wang Y, Macke JP, et al. A new member of the frizzled family from Drosophila functions as a Wingless receptor. Nature. 1996;382:225–230. doi: 10.1038/382225a0. [DOI] [PubMed] [Google Scholar]
- Zhang Z, Deb A, Zhang Z, Pachori A, He W, Guo J, et al. Secreted frizzled related protein 2 protects cells from apoptosis by blocking the effect of canonical Wnt3a. J Mol Cell Cardiol. 2009;46:370–377. doi: 10.1016/j.yjmcc.2008.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Boer J, Wang HJ., and, Van Blitterswijk C. Effects of Wnt signaling on proliferation and differentiation of human mesenchymal stem cells. Tissue Eng. 2004;10:393–401. doi: 10.1089/107632704323061753. [DOI] [PubMed] [Google Scholar]
- Derfoul A, Carlberg AL, Tuan RS., and, Hall DJ. Differential regulation of osteogenic marker gene expression by Wnt-3a in embryonic mesenchymal multipotential progenitor cells. Differentiation. 2004;72:209–223. doi: 10.1111/j.1432-0436.2004.07205003.x. [DOI] [PubMed] [Google Scholar]
- Neth P, Ries C, Karow M, Egea V, Ilmer M., and, Jochum M. The Wnt signal transduction pathway in stem cells and cancer cells: influence on cellular invasion. Stem Cell Rev. 2007;3:18–29. doi: 10.1007/s12015-007-0001-y. [DOI] [PubMed] [Google Scholar]
- Zerlin M, Julius MA., and, Kitajewski J. Wnt/Frizzled signaling in angiogenesis. Angiogenesis. 2008;11:63–69. doi: 10.1007/s10456-008-9095-3. [DOI] [PubMed] [Google Scholar]
- Dufourcq P, Couffinhal T, Ezan J, Barandon L, Moreau C, Daret D, et al. FrzA, a secreted frizzled related protein, induced angiogenic response. Circulation. 2002;106:3097–3103. doi: 10.1161/01.cir.0000039342.85015.5c. [DOI] [PubMed] [Google Scholar]
- Kim HW, Haider HK, Jiang S., and, Ashraf M. Ischemic preconditioning augments survival of stem cells via miR-210 expression by targeting caspase-8-associated protein 2. J Biol Chem. 2009;284:33161–33168. doi: 10.1074/jbc.M109.020925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin Y, Kato T, Furu M, Nasu A, Kajita Y, Mitsui H, et al. Mesenchymal stem cells cultured under hypoxia escape from senescence via down-regulation of p16 and extracellular signal regulated kinase. Biochem Biophys Res Commun. 2010;391:1471–1476. doi: 10.1016/j.bbrc.2009.12.096. [DOI] [PubMed] [Google Scholar]
- Wu Y, Chen L, Scott PG., and, Tredget EE. Mesenchymal stem cells enhance wound healing through differentiation and angiogenesis. Stem Cells. 2007;25:2648–2659. doi: 10.1634/stemcells.2007-0226. [DOI] [PubMed] [Google Scholar]
- Andersson G, Denaro M, Johnson K, Morgan P, Sullivan A, Houser S, et al. Engraftment of retroviral EGFP-transduced bone marrow in mice prevents rejection of EGFP-transgenic skin grafts. Mol Ther. 2003;8:385–391. doi: 10.1016/s1525-0016(03)00210-7. [DOI] [PubMed] [Google Scholar]
- Derval N, Barandon L, Dufourcq P, Leroux L, Lamazière JM, Daret D, et al. Epicardial deposition of endothelial progenitor and mesenchymal stem cells in a coated muscle patch after myocardial infarction in a murine model. Eur J Cardiothorac Surg. 2008;34:248–254. doi: 10.1016/j.ejcts.2008.03.058. [DOI] [PubMed] [Google Scholar]
- Horwitz EM, Prockop DJ, Fitzpatrick LA, Koo WW, Gordon PL, Neel M, et al. Transplantability and therapeutic effects of bone marrow-derived mesenchymal cells in children with osteogenesis imperfecta. Nat Med. 1999;5:309–313. doi: 10.1038/6529. [DOI] [PubMed] [Google Scholar]
- Wollert KC, Meyer GP, Lotz J, Ringes-Lichtenberg S, Lippolt P, Breidenbach C, et al. Intracoronary autologous bone-marrow cell transfer after myocardial infarction: the BOOST randomised controlled clinical trial. Lancet. 2004;364:141–148. doi: 10.1016/S0140-6736(04)16626-9. [DOI] [PubMed] [Google Scholar]
- Chen H, Campbell RA, Chang Y, Li M, Wang CS, Li J, et al. Pleiotrophin produced by multiple myeloma induces transdifferentiation of monocytes into vascular endothelial cells: a novel mechanism of tumor-induced vasculogenesis. Blood. 2009;113:1992–2002. doi: 10.1182/blood-2008-02-133751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Au P, Tam J, Fukumura D., and, Jain RK. Bone marrow-derived mesenchymal stem cells facilitate engineering of long-lasting functional vasculature. Blood. 2008;111:4551–4558. doi: 10.1182/blood-2007-10-118273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakaya M, Kitano M, Matsuda M., and, Nagata S. Spatiotemporal activation of Rac1 for engulfment of apoptotic cells. Proc Natl Acad Sci USA. 2008;105:9198–9203. doi: 10.1073/pnas.0803677105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tigges U, Hyer EG, Scharf J., and, Stallcup WB. FGF2-dependent neovascularization of subcutaneous Matrigel plugs is initiated by bone marrow-derived pericytes and macrophages. Development. 2008;135:523–532. doi: 10.1242/dev.002071. [DOI] [PubMed] [Google Scholar]
- Dufourcq P, Leroux L, Ezan J, Descamps B, Lamazière JM, Costet P, et al. Regulation of endothelial cell cytoskeletal reorganization by a secreted frizzled-related protein-1 and frizzled 4- and frizzled 7-dependent pathway: role in neovessel formation. Am J Pathol. 2008;172:37–49. doi: 10.2353/ajpath.2008.070130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasper G, Dankert N, Tuischer J, Hoeft M, Gaber T, Glaeser JD, et al. Mesenchymal stem cells regulate angiogenesis according to their mechanical environment. Stem Cells. 2007;25:903–910. doi: 10.1634/stemcells.2006-0432. [DOI] [PubMed] [Google Scholar]
- Hung SC, Pochampally RR, Chen SC, Hsu SC., and, Prockop DJ. Angiogenic effects of human multipotent stromal cell conditioned medium activate the PI3K-Akt pathway in hypoxic endothelial cells to inhibit apoptosis, increase survival, and stimulate angiogenesis. Stem Cells. 2007;25:2363–2370. doi: 10.1634/stemcells.2006-0686. [DOI] [PubMed] [Google Scholar]
- Polesskaya A, Seale P., and, Rudnicki MA. Wnt signaling induces the myogenic specification of resident CD45+ adult stem cells during muscle regeneration. Cell. 2003;113:841–852. doi: 10.1016/s0092-8674(03)00437-9. [DOI] [PubMed] [Google Scholar]
- Ezan J, Leroux L, Barandon L, Dufourcq P, Jaspard B, Moreau C, et al. FrzA/sFRP-1, a secreted antagonist of the Wnt-Frizzled pathway, controls vascular cell proliferation in vitro and in vivo. Cardiovasc Res. 2004;63:731–738. doi: 10.1016/j.cardiores.2004.05.006. [DOI] [PubMed] [Google Scholar]
- Takata H, Terada K, Oka H, Sunada Y, Moriguchi T., and, Nohno T. Involvement of Wnt4 signaling during myogenic proliferation and differentiation of skeletal muscle. Dev Dyn. 2007;236:2800–2807. doi: 10.1002/dvdy.21327. [DOI] [PubMed] [Google Scholar]
- Steelman CA, Recknor JC, Nettleton D., and, Reecy JM. Transcriptional profiling of myostatin-knockout mice implicates Wnt signaling in postnatal skeletal muscle growth and hypertrophy. FASEB J. 2006;20:580–582. doi: 10.1096/fj.05-5125fje. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
MSC detection.
Double immunolabeling of GFP and CD31 in ischemic tissues at day 7 and day 15 after injury transplanted with either NormMSC or HypMSC.
MSC harbored a pericyte-like phenotype after implantation in ischemic muscle at day 7.
Effect of HypMSC transplantation on growth factor gene expressions and induction of growth factor and Wnt factors in HypMSC vs NormMSC.
Effect of HypCM or Wnt4 CM on EC wound migration.