Abstract
BACKGROUND
Despite its proven benefits and need, women are significantly less likely to participate in and complete cardiac rehabilitation (CR) than men. The purpose of this study was to quantitatively investigate sex differences in CR barriers by participation status.
METHODS
1496 cardiac outpatients (n=430, 28.7% female) of 97 cardiologists completed a mailed survey to discern CR participation. Respondents were asked to rate 19 CR barriers on a 5-point Likert scale.
RESULTS
529 (43%) respondents self-reported participating in CR, with men being more likely to participate (ps<.05). There was no significant sex difference in total number of CR barriers, but differences in individual barriers were found. For CR participants, t-tests revealed significant sex differences in the perception of exercise as tiring or painful (p=.042) and work responsibilities (p=.013). For CR non-participants, women rated the following barriers as greater than men: transportation (p=.025), family responsibilities (p=.039), lack of CR awareness (p=.036), experiencing exercise as tiring or painful (p=.002), and comorbidities (p=.009).
CONCLUSIONS
While overall women do not perceive greater barriers to CR participation than men, the nature of their barriers differ, particularly among non-participants. Beliefs about the value of CR, awareness and exercise parameters are modifiable barriers which should be addressed among women.
Keywords: cardiac rehabilitation, gender, barriers
Introduction
Heart disease is the leading cause of morbidity and mortality for women1, 2. Cardiac rehabilitation (CR) is an outpatient secondary prevention program composed of structured exercise training and comprehensive education and counseling which addresses cardiac risk3. CR has been shown to reduce mortality by 25%4, 5, to reduce the need for re-hospitalization and the use of interventional procedures, and to have beneficial effects on cardiac risk factors, exercise capacity, psychosocial well-being, and health behaviors6–9, all in a cost-effective manner10–12. Studies of CR outcomes have generally revealed no major differences between men and women in terms of changes in risk factors, functional capacity and quality of life 9, 13–18
Despite its proven benefits and need, women are significantly less likely to participate in and complete CR13, 19–22. In the United States and Canada21, approximately 15–30% of eligible patients participate in CR, with the rate for women being much lower at 11–20%23. The percentage of women in CR is 20% lower than what would be expected based on coronary morbidity data17, 24. This is despite the fact that clinical practice guidelines3, 25, and those specifically developed for women with CVD26 recommend that women participate in CR post-acute coronary syndrome or revascularization intervention.
The reasons why women are missing from CR programs are multifactorial, and include health system, provider and patient-level factors27. While there have been descriptive studies on women’s barriers to CR participation28–30, and a few descriptive studies comparing women’s and men’s CR barriers31–33, there is a dearth of quantitative studies assessing sex differences in CR barriers. One Canadian study did compare sex differences among 86 male and 43 female CR participants, and 30 male and 31 female non-participants34. In their examination of 12 potential barriers, results revealed that women were more likely to rate comorbidities as a CR barrier, and to rate encouragement from adult children and attention to health promotion as factors that facilitated CR utilization than men. The purpose of the current study was to extend this previous work by conducting a larger multi-site study of sex differences in CR barriers, similarly comparing barriers among patients who participate and those who do not.
Methods
Design and Procedure
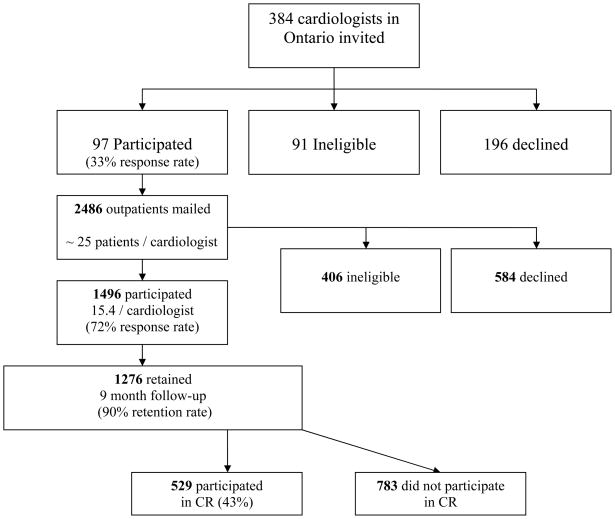
This study represents secondary analysis of data from a prospective study of outpatients nested within cardiologists 35. Upon receiving ethics approval from participating institutions, a sample of non-pediatric cardiologists from major centres in the Windsor to Ottawa corridor of Ontario, Canada was generated through a national physician registry, Canadian Medical Directory Online (www.mdselect.com). All 384 cardiologists were mailed an invitation to participate. Ninety-seven consenting cardiologists were visited by a research assistant to extract a retrospective, consecutive sample of approximately 20 each of their coronary artery disease (CAD) outpatients (see Figure 1). With informed consent by the patients, basic clinical data was recorded from their charts, and they were mailed a self-report survey assessing sociodemographic characteristics. Nine months later, participants were mailed a second follow-up survey assessing self-reported CR utilization and barriers.
Figure 1.
Participant Recruitment Flow Diagram
Participants
One thousand, four hundred and ninety-six recent and consecutive CAD outpatients consented to participate in this study (430 female [28.7%]; 1496/[2486-406]=72% response rate; see Figure 1). This represents a mean of 15.43±2.22 patients per cardiologist. CAD diagnosis was confirmed based on indication in patient chart of detailed history, focused physical examination, diagnostic ECG changes (i.e., Q waves, and/or ST-T segment changes), and/or troponin levels above the 99th percentile of normal. Patients who had undergone percutaneous coronary interventions (PCIs), acute coronary bypass (ACB), or concurrent valve repair were also eligible. Reasons for ineligibility based on the larger study were as follows (n=406): lack of English language proficiency (n =145; 35.7%), incorrect contact information (n=86; 21.2%), no CAD diagnosis (n=37; 9.1%), expired (n=34; 8.4%), orthopedic, neuromuscular, cognitive or vision impairment (n=33; 8.1%), non-recent index event or treatment (n =18; 4.4%), ineligibility for cardiac rehabilitation (CR) based on Canadian guidelines3 (n =6; 1.5%), previous attendance at CR (n =5; 1.2%), non-dysphoric psychiatric conditions (n=3, 0.7%), and other reasons (n=39; 9.6%).
Measures
Sociodemographic variables assessed in the baseline survey included age, sex, ethnocultural background (open-ended and forced choice), work status, level of education, and gross annual family income. Clinical data including previous clinical events, disease severity and risk factors were extracted from outpatient charts.
In the 9-month follow-up survey, respondents were asked whether or not they participated in CR (yes/no), and the percentage of prescribed sessions they attended (i.e., degree of participation). Patients who responded that they did not participate in CR were asked to list the reasons why in open-ended fashion.
Dependent Variable
CR barriers were assessed in the 9-month follow survey through 19 investigator-generated items, which were developed based on a review of the literature and pilot-tested36. Items assessed attitudinal, logistic and health system CR barriers. Sample items included distance, time constraints, and having exercise equipment at home. Respondents were asked to rate the reasons for not attending CR or for missing sessions if they did attend, hence the items were relevant to both CR participants and non-participants. Responses were made on a 5-point Likert-type scale from ‘strongly disagree’ to ‘strongly agree’, with higher scores indicating the item represents a greater barrier. The Cronbach’s alpha reliability was .91. A total mean barriers score was computed to reflect the average rating of all 19 barriers overall.
Statistical Analyses
All analyses were conducted using SPSS 15.037. Sociodemographic and clinical differences in those retained at the 9-month follow-up versus declining and ineligible study participants (i.e., non-retained) were tested with chi-square and analysis of variance as appropriate. Reliability analysis of the CR barrier items was conducted using Cronbach’s alpha. Sex differences in CR participation were tested. Specifically, a chi-square analysis was used to test for sex differences in CR participation status. A t-test was used to test for sex differences in degree of participation (i.e., percentage of prescribed sessions attended) among CR participants. A t-test was then employed to test for a significant difference in the total number of CR barriers by participation status.
A descriptive examination of the CR barrier items was performed by sex. Open-ended reasons for not participating in CR were coded. The file was then stratified by CR participation status, and sex differences in total individual CR barriers were investigated using t-tests. P-values of <.05 were used to denote significance. Given the exploratory nature of these analyses, a correction for multiple comparisons was not used.
Results
Respondent Characteristics
As shown in Table 1, there were 360 (83.7%) females and 902 (85.4%) males retained in the sample at the 9 month follow-up. Reasons for ineligibility (n=92) at this assessment point were as follows: unable to reach/incorrect contact information (n=37; 40.2%), expired (n=24; 26.1%), new onset of an orthopedic, neuromuscular, cognitive, psychiatric or vision impairment (n=6; 6.5%), and other reasons (n=25; 27.2%) such as too ill to participate or moved out of the province/country. There were no significant sex differences in participant status at baseline or 9 month follow-up, such that women were just as likely to participate as men. However, participants retained at the 9 month follow up were significantly more likely to be white, older, married, retired, with a family income greater than $50,000, have greater functional status, and more likely to be classified in CCS class II–IV than patients who declined or were ineligible.
Table 1.
Characteristics of Participating, Ineligible and Declining Outpatients at 9 Month Follow Up Assessment (N=1496)
| Characteristic | Retained Participants |
Ineligibles (n=92) | Declined (n=142) | ||
|---|---|---|---|---|---|
| Males (n=902) | Females (n=360) | Total (n=1262) | |||
| Age (mean ± SD) | 66.92 ± 10.76 | 68.44 ± 11.97‡ | 67.36 ± 11.13 | 66.37 ± 13.31 | 64.21 ± 12.47§§ |
| Sex (% female) | - | 360 (100) | 360 (28.5) | 26 (28.3) | 43 (30.3) |
| BMI† (mean ± SD) | 27.61 ± 4.97 | 27.36 ± 6.39 | 27.53 ± 5.41 | 27.80 ± 5.82 | 27.63 ± 5.63 |
| Marital status† (%married) | 707 (79.0)‡‡‡ | 200 (55.9) | 907 (72.4)§§§ | 54 (59.3) | 83 (59.7) |
| Ethnocultural background† (% minority) | 133 (14.7) | 40 (11.1) | 173 (13.7)§§§ | 21 (23.1) | 38 (26.8) |
| Education† (% >high school) | 484 (54.4) | 182 (51.7) | 666 (53.6) | 40 (44.4) | 72 (52.2) |
| Family income† (% ≥ $50,000CAD) | 431 (51.9)‡‡‡ | 125 (39.3) | 556 (48.4)§§ | 27 (31.8) | 45 (37.8) |
| Work status† (% retired) | 478 (53.3) | 217 (61.0)‡‡ | 695 (55.5)§§ | 37 (41.1) | 61 (44.2) |
| Systolic BP mm Hg (mean ± SD) | 130.34 ± 18.44 | 133.50 ± 20.79‡ | 131.24 ± 19.18 | 135.10 ± 21.13 | 130.08 ± 19.53 |
| Diastolic BP mm Hg (mean ± SD) | 74.27 ± 10.38 | 75.15 ± 9.69 | 74.52 ± 10.19 | 77.32 ± 12.87§ | 73.12 ± 10.51 |
| Total Cholesterol/HDL Ratio | 3.75 | 3.41 | 3.67 | 4.06 | 3.63 |
| HDL mmol/L (mean ± SD) | 1.13 ± .32 | 1.52 ± .54‡‡‡ | 1.22 ± .42 | 1.08 ± .29 | 1.18 ± .30 |
| LDL mmol/L (mean ± SD) | 2.23 ± .89 | 2.62 ± .92‡‡ | 2.32 ± .91 | 2.12 ± .99 | 2.49 ± .91 |
| NYHA Class II–IV (%) | 63 (49.2) | 19 (46.4) | 82 (48.6) | 5 (41.7) | 6 (30.0) |
| CCS angina class 2–4 (%) | 194 (81.4) | 65 (83.3) | 259 (81.9)§ | 7 (58.4) | 27 (71.0) |
| Multi-vessel Disease (>1 diseased coronary arteries) | 283 (81.6)‡ | 75 (72.1) | 358 (79.4) | 25 (83.3) | 36 (81.8) |
| Duke Activity Status Index† (mean ± SD) | 39.28 ± 15.53‡‡‡ | 31.55 ± 15.25 | 37.07 ± 15.83 | 28.75 ± 18.85§§ | 34.82 ± 16.26 |
| Current or Previous MI | 436 (89.5) | 137 (85.6) | 573 (88.6) | 45 (88.2) | 70 (87.5) |
| Current or Previous PCI | 409 (90.7) | 140 (88.6) | 549 (90.1) | 39 (88.6) | 59 (95.2) |
| Current or Previous ACB | 289 (81.4) | 69 (78.4) | 358 (80.8) | 19 (67.9) | 33 (80.5) |
| Current or Previous HF | 118 (72.8) | 59 (79.7) | 177 (75.0) | 19 (86.4) | 24 (77.4) |
| Current or Previous Arrhythmia | 184 (83.6) | 92 (89.3) | 276 (85.4) | 26 (89.7) | 30 (83.3) |
| Current or Previous of Valve repair/replacement | 134 (84.8) | 62 (87.3) | 196 (85.6) | 14 (77.8) | 27 (79.4) |
Note: Percentages take into account missing data for some variables.
BMI, Body Mass Index; BP, blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein; CCS, Canadian Cardiovascular Society; NYHA, New York Heart Association. MI, Myocardial Infarction; PCI, Percutaneous Coronary Intervention; ACB, Acute Coronary Bypass; HF, Heart Failure.
denotes data from patient report.
Significant difference between participants, ineligibles and decliners;
p<.05;
p<.01;
p<.001
Significant difference between male and female participants;
p<.05;
p<.01;
p<.001
CR Participation Status by Sex
Overall, 133 (36.9%) female and 396 (43.9%) male respondents participated in CR (p=.028). Men self-reported participating in 86.24±24.36% of prescribed sessions, with women reporting participating in 80.68±27.20% of sessions (p=.038).
CR Barriers by Participation Status
A total mean barriers score was computed (see Table 2). CR non-participants reported a significantly greater number of barriers than CR participants (p<.001).
Table 2.
Mean and Standard Deviation of CR Barriers by Sex and Participation Status
| CR Barrier | CR Non-Participants | CR Participants | Total | ||||
|---|---|---|---|---|---|---|---|
| Males (n=507) | Females (n=226) | Total (n=733) | Males (n=396) | Females (n=133) | Total (n=529) | (N=1222) | |
| Distance | 2.71 ± 1.40 | 2.82 ± 1.49 | 2.74 ± 1.43 | 1.80 ± 1.13 | 1.93 ± 1.25 | 1.83 ± 1.16 | 2.25 ± 1.36 |
| Cost | 2.31 ± 1.21 | 2.46 ± 1.37 | 2.36 ± 1.26 | 1.54 ± .87 | 1.60 ± .96 | 1.56 ± 0.89 | 1.93 ± 1.14 |
| Transportation problems |
2.42 ± 1.35 | 2.85 ± 1.49§ | 2.55 ± 1.41 | 1.69 ± 1.02 | 1.78 ± 1.09 | 1.72 ± 1.04 | 2.09 ± 1.28 |
| Family responsibilities | 2.13 ± 1.13 | 2.46 ± 1.32§ | 2.23 ± 1.19 | 1.88 ± 1.17 | 2.05 ± 1.28 | 1.92 ± 1.20 | 2.06 ± 1.20 |
| I didn’t know about cardiac rehabilitation | 2.95 ± 1.45 | 3.30 ± 1.42§ | 3.05 ± 1.44 | 1.43 ± .77 | 1.48 ± .74 | 1.44 ± 0.76 | 2.32 ± 1.43 |
| I don’t need cardiac rehabilitation | 3.18 ± 1.27 | 3.05 ± 1.22 | 3.15 ± 1.25 | 1.60 ± .91 | 1.54 ± .83 | 1.58 ± 0.89 | 2.42 ± 1.34 |
| I already exercise at home | 3.58 ± 1.18§§§ | 3.06 ± 1.21 | 3.44 ± 1.22 | 2.38 ± 1.41 | 2.18 ± 1.18 | 2.33 ± 1.36 | 2.94 ± 1.39 |
| I already exercise in my community | 3.13 ± 1.29§§ | 2.67 ± 1.22 | 3.00 ± 1.29 | 2.05 ± 1.24 | 1.86 ± 1.04 | 2.00 ± 1.19 | 2.53 ± 1.34 |
| I find exercise tiring or painful | 2.63 ± 1.30 | 3.05 ± 1.32§§ | 2.75 ± 1.32 | 1.95 ± 1.12 | 2.23 ± 1.26‡ | 2.03 ± 1.16 | 2.42 ± 1.30 |
| It was not offered in my first language | 1.82 ± 1.05 | 1.84 ± 1.07 | 1.83 ± 1.05 | 1.34 ± .56 | 1.39 ± .61 | 1.35 ± 0.57 | 1.58 ± .87 |
| Time constraints | 2.16 ± 1.15 | 2.32 ± 1.25 | 2.20 ± 1.19 | 1.83 ± 1.12 | 1.86 ± 1.11 | 1.84 ± 1.12 | 2.02 ± 1.17 |
| Work responsibilities | 2.28 ± 1.28 | 2.15 ± 1.21 | 2.24 ± 1.26 | 2.11 ± 1.34‡ | 1.76 ± 1.08 | 2.02 ± 1.28 | 2.13 ± 1.28 |
| My heart condition is not that serious | 2.90 ± 1.24 | 2.83 ± 1.20 | 2.88 ± 1.23 | 1.79 ± 1.03 | 1.78 ± .91 | 1.79 ± 1.00 | 2.39 ± 1.25 |
| Other health problems prevent me from going | 2.30 ± 1.30 | 2.66 ± 1.35§§ | 2.41 ± 1.31 | 1.90 ± 1.19 | 2.05 ± 1.26 | 1.94 ± 1.20 | 2.18 ± 1.28 |
| It won’t improve my health | 2.14 ± 1.03 | 2.38 ± 1.10 | 2.20 ± 1.05 | 1.49 ± .76 | 1.49 ± .75 | 1.49 ± 0.76 | 1.87 ± .99 |
| My doctor doesn’t encourage me to attend | 2.85 ± 1.25 | 3.05 ± 1.20 | 2.91 ± 1.24 | 1.55 ± .84 | 1.56 ± .74 | 1.55 ± 0.81 | 2.25 ± 1.25 |
| Many people with heart problems don’t go to cardiac rehab, and they are fine | 2.69 ± 1.08 | 2.61 ± 1.04 | 2.67 ± 1.07 | 1.70 ± .92 | 1.81 ± .91 | 1.73 ± 0.92 | 2.21 ± 1.10 |
| I am confident I can manage my heart problem on my own | 2.97 ± 1.16§§ | 2.67 ± 1.13 | 2.88 ± 1.16 | 1.87 ± 1.04 | 1.81 ± .95 | 1.85 ± 1.02 | 2.41 ± 1.21 |
| The illness of a close relative or other caregiving responsibilities | 1.97 ± .97 | 1.93 ± 1.09 | 1.96 ± 1.01 | 1.62 ± .87 | 1.79 ± 1.01 | 1.67 ± 0.91 | 1.80 ± .97 |
| Total | 2.93 ± .88 | 3.00 ± .89 | 2.95 ± .85 | 1.95 ± .90 | 1.90 ± .70 | 1.95 ± .88 | 2.53 ± 1.01 |
Significant difference between male and female CR non-participants;
p<.05;
p<.01;
p<.001
Significant difference between male and female CR participants;
p<.05;
p<.01;
p<.001
NOTE: CR barriers scored on a Likert-type scale 1=strongly disagree, 2 = disagree, 3= neither, 4 = agree, 5= strongly agree)
Sex Differences in CR Barriers
Regardless of participation status, the most strongly endorsed CR barrier items by male respondents were engaging in an exercise routine at home or in the community, confidence in self-managing their condition, perceived lack of need, and perceptions that their condition is not serious enough to warrant CR participation. The least strongly endorsed CR barriers by men were that CR was not offered in their first language, the illness of a close relative and perceptions that CR would not improve their health. The most strongly endorsed barriers by females were lack of need due to home exercise routine, perception of exercise as tiring or painful, lack of CR awareness, comorbidities, perception that their condition is not serious enough to warrant CR participation, and lack of encouragement to attend by their physician. The least strongly endorsed CR barriers by women were that CR was not offered in their first language, the illness of a close relative and work responsibilities.
CR non-participants were also asked in open-ended fashion for reasons why they did not attend. Responses were coded and stratified by sex. Responses other than those included in the 19 item investigator-generated list of CR barriers reported by men included no interest in group activities (n=2, 1.1%) and overbooked CR (n=1, .5%). Other responses by women included lack of motivation/interest (n=3, 2.7%), no desire to leave home (n=2, 1.8%), and age (n=1, .5%).
CR Barriers by Sex and Participation Status
The mean score for total number of CR barriers for males was 2.52±1.01 and for females was 2.57±.99. There was no significant sex difference in total number of CR barriers (p=.46). There were also no sex difference in total barriers for CR participants (p =.75) or for CR non-participants (p=.52; means shown in Table 2). However, as shown, there were significant differences in individual barrier items by sex. Male CR participants were significantly more likely to rate work responsibilities as a barrier than females. Female CR participants were significantly more likely to rate the tiring or painful nature of exercise as a barrier than males. Among patients not participating in CR, males rated the following barriers significantly more highly than did females: already exercising at home or in the community, and confidence in self-managing their condition. Female CR non-participants rated the following barriers significantly more highly than did males: transportation, family responsibilities, lack of CR awareness, perceiving exercise as tiring or painful, and comorbid conditions.
Discussion
In this quantitative study investigating sex differences in CR barriers, it was demonstrated that while women may not have a greater number of CR barriers overall, the nature of their CR barriers may differ from those of men. Moreover, sex differences in barriers may be more prominent among CR non-participants than participants.
Overall there were no significant differences in total number of CR barriers. This is contrary to the previous literature which highlights women’s CR barriers28–30, 34, although sex differences had yet to be tested through an overall barrier scale. This finding is surprising given that women are significantly less likely to enroll and participate in CR13, 19–22. It is possible that unmeasured barriers may be accounting for women’s lower CR participation. Indeed, through open-ended responses women identified lack of motivation/interest and old age for example as additional barriers not assessed in the scale. These findings should be used to develop a more comprehensive and psychometrically-validated scale of CR barriers which is relevant to both men and women.
There were however significant sex differences in several individual CR barriers. When examining differences in barriers among CR participants, there were only 2 individual items which differentiated between men and women. That men reported work as a greater CR barrier than women is supported by previous research suggesting that women are less likely to return to paid work than men38. Also replicating previous research39, women were more likely to report the experience of exercise as tiring or painful as a CR barrier. This sex difference was also found among CR non-participants. Clearly there is need to take into consideration women’s lower exercise capacity14, greater comorbidities40 and exercise preferences39, 41 when discussing and providing them with an exercise prescription. Cardiovascular benefits are accrued through accumulation of activity through short bouts42 and from lower intensity activities such as walking, as well as lifestyle activities more generally43.
Many sex differences in barriers among CR non-participants were identified, and most are supported in previous literature. For instance, because women often have lower socioeconomic status and are older at the time of a cardiac event44–46, they may be less likely to have access to a car than men, leading to greater transportation barriers28, 29, 32, 33,47. Moreover, women are more often the family caregivers than men, leaving less time for disease self-management. For example, women may have a spouse with health problems for whom they provide care, may provide care to grandchildren, and often take the main responsibility for household chores28. Women more often suffer from comorbidities40, 48 such as osteoporosis, diabetes and urinary incontinence, which can all serve as deterrents to exercise in CR programs28, 30, 33, 34 due to fear of falling, concerns regarding foot care and accidents respectively.
Men’s barriers to CR participation were home and community exercise participation, and efficacy in self-managing their cardiac condition. Indeed, previous research has shown that men often have greater exercise and diet self-efficacy than women24, 49, and that availability of their own exercise equipment and belief they can carry out CR recommendations at home33, 50 are related to lower CR utilization. However, the benefits of CR participation including comprehensive risk reduction and multi-disciplinary support for heart-healthy behavior changes should be stressed to promote greater uptake among men as well. While cardiac patients may be highly motivated to change their behavior following a cardiac event, recent evidence shows this decays over time51.
While previous research has suggested financial barriers to CR participation among women28, 29, this was not demonstrated in our study. This is likely due to the fact that participants were recruited in Ontario, Canada where CR services are covered through provincial health insurance. Moreover, previous research has identified time constraints as a significant barrier to CR participation among women30, however we found no sex difference in this barrier. Time constraints were not among the most strongly endorsed barriers among men or women, suggesting this barrier may be less prominent than previously reported. Finally, language barriers were likely rated as low by respondents due to the fact that English language proficiency was one of the study inclusion criteria.
Caution is warranted when interpreting these results, mainly due to measurement issues, generalizability, and potential error. First, because there is no psychometrically-validated scale of CR barriers, investigator-generated items were used. However, these items had been pilot-tested, were based on a review of the literature, and showed high internal reliability. Future research is required to test and validate a CR barriers measure. For instance, use of a conceptual model such as Andersen’s Behavioral Model of Healthcare Utilization52 to ensure scale representation of areas of influence on CR participation from a patient to health system level, use of a qualitative process of barrier identification in men and women, and tests of the validity and reliability of such a scale may be explored. Second, characteristics of our retained sample were different than patients who were lost-to-follow-up, and there were differences between retained male and female participants. Replication is warranted to ensure generalizability, and to ensure that the CR barrier differences identified are not a function of the sex differences in sociodemographic and clinical characteristics. In addition, it is possible that the cardiologists who choose to participate in the study had more positive views of CR compared to those cardiologists who did not participate. Hence, this may also affect the generalizability of the current study’s findings. Third, when examining sex differences in CR barrier items, 19 comparisons were made, and this introduces the potential for inflated error rates. Again, replication is warranted, using a more conservative statistical approach such as a Bonferroni correction. Finally, due to the nature of the study design, causal conclusions cannot be drawn.
Future research is needed to explore interventions to promote greater CR participation among women, and men. Some sex-specific recommendations to overcome some of the identified CR barriers are made in a recent review53, such as provision of childcare or home help, and offering exercise variety and choice. Automatic referral in particular shows promise in increasing CR utilization overall54, 55, but whether it can overcome the sex differential remains to be tested and demonstrated. Currently our group is prospectively comparing automatic referral modes to usual referral with an adequately powered sample of women to test this possibility. Clearly there are barriers related to both the health system and patient preferences and attitudes56 which must be addressed through multi-level interventions.
In conclusion, while women may not have a greater number of CR barriers overall, the nature of their CR barriers differ from those of men. These include transportation barriers, family responsibilities, experience with exercise as tiring or painful, lack of CR awareness, and comorbidities. Future research to test means to overcome these barriers is needed.
Acknowledgments
This research was supported by Canadian Institutes of Health Research (CIHR) grant #MOP-74431. Dr. Grace is also supported by CIHR salary award # MSH-80489, Ms. Gravely-Witte is supported by Ontario Women’s Health Council/CIHR Institute of Gender and Health scholarship #DOW-85531, and Ms. Kayaniyil and Ms. Brual by a Heart and Stroke Foundation Masters Studentship.
Contributor Information
Sherry L. Grace, Email: sgrace@yorku.ca, York University, University Health Network Women’s Health Program and University of Toronto.
Shannon Gravely-Witte, Email: sgravely@yorku.ca, York University.
Sheena Kayaniyil, Email: sckayani@yorku.ca, York University.
Janette Brual, Email: j_brual@yorku.ca, York University.
Neville Suskin, Email: neville.suskin@lhsc.on.ca, London Health Sciences Center and University of Western Ontario.
Donna E. Stewart, Email: donna.stewart@uhn.on.ca, University Health Network Women’s Health Program and University of Toronto.
References
- 1.Pilote L, Dasgupta K, Guru V, et al. A comprehensive view of sex-specific issues related to cardiovascular disease. CMAJ. 2007;176:S1–44. doi: 10.1503/cmaj.051455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Heart Association. Heart disease and Stroke Statistics—2005 update. 2005. [Google Scholar]
- 3.Canadian Association of Cardiac Rehabilitation. Canadian guidelines for cardiac rehabilitation and cardiovascular disease prevention: Enhancing the science, refining the art. Winnipeg, MB: CACRC; 2004. [Google Scholar]
- 4.Taylor RS, Brown A, Ebrahim S, et al. Exercise-based rehabilitation for patients with coronary heart disease: Systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004;116:682–692. doi: 10.1016/j.amjmed.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 5.Jolliffe JA, Rees K, Taylor RS, Thompson D, Oldridge N, Ebrahim S. Exercise-based rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2001;(1):CD001800. doi: 10.1002/14651858.CD001800. [DOI] [PubMed] [Google Scholar]
- 6.Clark AM, Hartling L, Vandermeer B, McAlister FA. Meta-analysis: Secondary prevention programs for patients with coronary artery disease. Ann Intern Med. 2005;143:659–672. doi: 10.7326/0003-4819-143-9-200511010-00010. [DOI] [PubMed] [Google Scholar]
- 7.Jobin J. Long-term effects of cardiac rehabilitation and the paradigms of cardiac rehabilitation. J Cardiopulm Rehabil. 2005;25:103–106. doi: 10.1097/00008483-200503000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Brown A, Taylor R, Noorani H, Stone J, Skidmore B. Exercise-based cardiac rehabilitation programs for coronary artery disease: A systematic clinical and economic review. Ottawa, ON: Canadian Coordinating Office for Health Technology Assessment; 2003. Technology Report no. 34. [Google Scholar]
- 9.Lavie CJ, Milani RV. Effects of cardiac rehabilitation and exercise training on exercise capacity, coronary risk factors, behavioral characteristics, and quality of life in women. Am J Cardiol. 1995;75:340–343. doi: 10.1016/s0002-9149(99)80550-5. [DOI] [PubMed] [Google Scholar]
- 10.Lee AJ, Strickler GK, Shepard DS. The economics of cardiac rehabilitation and lifestyle modification: A review of literature. J Cardiopulm Rehabil Prev. 2007;27:135–142. doi: 10.1097/01.HCR.0000270694.94010.8b. [DOI] [PubMed] [Google Scholar]
- 11.Papadakis S, Oldridge NB, Coyle D, et al. Economic evaluation of cardiac rehabilitation: A systematic review. Eur J Cardiovasc Prev Rehabil. 2005;12:513–520. doi: 10.1097/01.hjr.0000186624.60486.e8. [DOI] [PubMed] [Google Scholar]
- 12.Carlson JJ, Johnson JA, Franklin BA, VanderLaan RL. Program participation, exercise adherence, cardiovascular outcomes, and program cost of traditional versus modified cardiac rehabilitation. Am J Cardiol. 2000;86:17–23. doi: 10.1016/s0002-9149(00)00822-5. [DOI] [PubMed] [Google Scholar]
- 13.Arthur HM. Rehabilitation. Can J Cardiol. 2001;17 (Suppl D):57D–62D. [PubMed] [Google Scholar]
- 14.O’Farrell P, Murray J, Huston P, LeGrand C, Adamo K. Sex differences in cardiac rehabilitation. Can J Cardiol. 2000;16:319–325. [PubMed] [Google Scholar]
- 15.Balady GJ, Jette D, Scheer J, Downing J. Changes in exercise capacity following cardiac rehabilitation in patients stratified according to age and gender. results of the Massachusetts association of cardiovascular and pulmonary rehabilitation multicenter database. [Accessed 5/1/2007];J Cardiopulm Rehabil. 1996 16:38–46. doi: 10.1097/00008483-199601000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Cannistra LB, Balady GJ, O’Malley CJ, Weiner DA, Ryan TJ. Comparison of the clinical profile and outcome of women and men in cardiac rehabilitation. Am J Cardiol. 1992;69:1274–1279. doi: 10.1016/0002-9149(92)91220-x. [DOI] [PubMed] [Google Scholar]
- 17.Ades PA, Waldmann ML, Polk DM, Coflesky JT. Referral patterns and exercise response in the rehabilitation of female coronary patients aged greater than or equal to 62 years. Am J Cardiol. 1992;69:1422–1425. doi: 10.1016/0002-9149(92)90894-5. [DOI] [PubMed] [Google Scholar]
- 18.O’Callaghan WG, Teo KK, O’Riordan J, Webb H, Dolphin T, Horgan JH. Comparative response of male and female patients with coronary artery disease to exercise rehabilitation. Eur Heart J. 1984;5:649–651. doi: 10.1093/oxfordjournals.eurheartj.a061721. [DOI] [PubMed] [Google Scholar]
- 19.Suaya JA, Shepard DS, Normand SL, Ades PA, Prottas J, Stason WB. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. 2007;116:1653–1662. doi: 10.1161/CIRCULATIONAHA.107.701466. [DOI] [PubMed] [Google Scholar]
- 20.Shanks LC, Moore SM, Zeller RA. Predictors of cardiac rehabilitation initiation. Rehabil Nurs. 2007;32:152–157. doi: 10.1002/j.2048-7940.2007.tb00169.x. [DOI] [PubMed] [Google Scholar]
- 21.Grace SL, Abbey SE, Shnek ZM, Irvine J, Franche RL, Stewart DE. Cardiac rehabilitation II: Referral and participation. Gen Hosp Psychiatry. 2002;24:127–134. doi: 10.1016/s0163-8343(02)00179-2. [DOI] [PubMed] [Google Scholar]
- 22.Bittner V, Sanderson BK. Women in cardiac rehabilitation. J Am Med Womens Assoc. 2003;58:227–235. [PubMed] [Google Scholar]
- 23.Jackson L, Leclerc J, Erskine Y, Linden W. Getting the most out of cardiac rehabilitation: A review of referral and adherence predictors. Heart. 2005;91:10–14. doi: 10.1136/hrt.2004.045559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schuster PM, Waldron J. Gender differences in cardiac rehabilitation patients. Rehabil Nurs. 1991;16:248–253. doi: 10.1002/j.2048-7940.1991.tb01229.x. [DOI] [PubMed] [Google Scholar]
- 25.Wenger NK, Froelicher ES, Smith LK, et al. Cardiac rehabilitation as secondary prevention. agency for health care policy and research and national heart, lung, and blood institute. Clin Pract Guidel Quick Ref Guide Clin. 1995;(17):1–23. [PubMed] [Google Scholar]
- 26.Mosca L, Banka CL, Benjamin EJ, et al. Evidence-based guidelines for cardiovascular disease prevention in women: 2007 update. J Am Coll Cardiol. 2007;49:1230–1250. doi: 10.1016/j.jacc.2007.02.020. [DOI] [PubMed] [Google Scholar]
- 27.Scott LA, Ben-Or K, Allen JK. Why are women missing from outpatient cardiac rehabilitation programs? A review of multilevel factors affecting referral, enrollment, and completion. J Womens Health. 2002;11:773–791. doi: 10.1089/15409990260430927. [DOI] [PubMed] [Google Scholar]
- 28.Heid HG, Schmelzer M. Influences on women’s participation in cardiac rehabilitation. Rehabil Nurs. 2004;29:116–121. doi: 10.1002/j.2048-7940.2004.tb00327.x. [DOI] [PubMed] [Google Scholar]
- 29.Marcuccio E, Loving N, Bennett SK, Hayes SN. A survey of attitudes and experiences of women with heart disease. Women’s Health Issues. 2003;13:23–31. doi: 10.1016/s1049-3867(02)00193-7. [DOI] [PubMed] [Google Scholar]
- 30.Plach SK. Women and cardiac rehabilitation after heart surgery: Patterns of referral and adherence. Rehabil Nurs. 2002;27:104–109. doi: 10.1002/j.2048-7940.2002.tb01998.x. [DOI] [PubMed] [Google Scholar]
- 31.Farley RL, Wade TD, Birchmore L. European journal of cardiovascular nursing. Vol. 2. Amsterdam: Elsevier; 2003. Factors influencing attendance at cardiac rehabilitation among coronary heart disease patients; p. 205. [DOI] [PubMed] [Google Scholar]
- 32.Radley A, Grove A, Wright S, Thurston H. Problems of women compared with those of men following myocardial infarction. Coronary Health Care. 1998;2:202–209. [Google Scholar]
- 33.Halm M, Penque S, Doll N, Beahrs M. Women and cardiac rehabilitation: Referral and compliance patterns. J Cardiovasc Nurs. 1999;13:83–92. doi: 10.1097/00005082-199904000-00008. [DOI] [PubMed] [Google Scholar]
- 34.Lieberman L, Meana M, Stewart D. Cardiac rehabilitation: Gender differences in factors influencing participation. J Womens Health. 1998;7:717–723. doi: 10.1089/jwh.1998.7.717. [DOI] [PubMed] [Google Scholar]
- 35.Grace SL, Gravely-Witte S, Brual J, et al. Contribution of patient and physician factors to CR referral: A prospective multi-level study. Nat Clin Pract Cardiovasc Med. doi: 10.1038/ncpcardio1272. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grace SL, Evindar A, Kung T, Scholey P, Stewart DE. Automatic referral to cardiac rehabilitation: Reducing disparities in uptake. Eur J Cardiovasc Prev Rehabil. 2004;11:89. [Google Scholar]
- 37.SPSS Inc. SPSS for windows. 2006. p. 15.0. [Google Scholar]
- 38.Brezinka V, Dusseldorp E, Maes S. Gender differences in psychosocial profile at entry into cardiac rehabilitation. J Cardiopulm Rehabil. 1998;18:445–449. doi: 10.1097/00008483-199811000-00007. [DOI] [PubMed] [Google Scholar]
- 39.Moore SM. Women’s views of cardiac rehabilitation programs. J Cardiopulm Rehabil. 1996;16:123–129. doi: 10.1097/00008483-199603000-00007. [DOI] [PubMed] [Google Scholar]
- 40.McPherson R. Coronary artery disease and women: Applying the guidelines for risk factor management. Can J Cardiol. 2000;16 (Suppl A):5A–10A. [PubMed] [Google Scholar]
- 41.Ruland CM, Moore SM. Eliciting exercise preferences in cardiac rehabilitation: Initial evaluation of a new strategy. Patient Educ Couns. 2001;44:283–291. doi: 10.1016/s0738-3991(00)00189-0. [DOI] [PubMed] [Google Scholar]
- 42.Jakicic JM, Wing RR, Butler BA, Robertson RJ. Prescribing exercise in multiple short bouts versus one continuous bout: Effects on adherence, cardiorespiratory fitness, and weight loss in overweight women. Int J Obes Relat Metab Disord. 1995;19:893–901. [PubMed] [Google Scholar]
- 43.Manson JE, Greenland P, LaCroix AZ, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347:716–725. doi: 10.1056/NEJMoa021067. [DOI] [PubMed] [Google Scholar]
- 44.Wenger NK. Clinical characteristics of coronary heart disease in women: Emphasis on gender differences. Cardiovasc Res. 2002;53:558–567. doi: 10.1016/s0008-6363(01)00511-9. [DOI] [PubMed] [Google Scholar]
- 45.Rosenfeld JA. Heart disease in women. gender-specific statistics and prevention strategies for a population at risk. Postgrad Med. 2000;107:111–6. doi: 10.3810/pgm.2000.5.15.1094. quiz 156. [DOI] [PubMed] [Google Scholar]
- 46.Limacher MC. Exercise and rehabilitation in women. indications and outcomes. Cardiol Clin. 1998;16:27–36. doi: 10.1016/s0733-8651(05)70381-7. [DOI] [PubMed] [Google Scholar]
- 47.Moore SM, Kramer FM. Women’s and men’s preferences for cardiac rehabilitation program features. J Cardiopulm Rehabil. 1996;16:163–168. doi: 10.1097/00008483-199605000-00003. [DOI] [PubMed] [Google Scholar]
- 48.Grace SL, Fry R, Cheung A, Stewart DE. Cardiovascular disease. BMC Womens Health. 2004;4 (Suppl 1):S15. doi: 10.1186/1472-6874-4-S1-S15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Blanchard CM, Rodgers WM, Courneya KS, Daub B, Knapik G. Does barrier efficacy mediate the gender-exercise adherence relationship during phase II cardiac rehabilitation? Rehabilitation Psychology. 2002;47:106–120. Available from: http://illumina.scholarsportal.info/ids70/gateway.php?mode=pdf&doi=10.1037%2F0090-5550.47.1.106&db=psycinfo-set-c&s1=3915f16b8524cf1cd8195aa23dda85a2&s2=3a0d5ba60ebda0fb4759e91b52f97ef9. [Google Scholar]
- 50.Mak YM, Chan WK, Yue CS. Barriers to participation in a phase II cardiac rehabilitation programme. Hong Kong Med J. 2005;11:472–475. [PubMed] [Google Scholar]
- 51.Reid RD, Morrin LI, Pipe AL, et al. Determinants of physical activity after hospitalization for coronary artery disease: The tracking exercise after cardiac hospitalization (TEACH) study. Eur J Cardiovasc Prev Rehabil. 2006;13:529–537. doi: 10.1097/01.hjr.0000201513.13343.97. [DOI] [PubMed] [Google Scholar]
- 52.Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? J Health Soc Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- 53.Beswick AD, Rees K, West RR, et al. Improving uptake and adherence in cardiac rehabilitation: Literature review. J Adv Nurs. 2005;49:538–555. doi: 10.1111/j.1365-2648.2004.03327.x. [DOI] [PubMed] [Google Scholar]
- 54.Grace SL, Scholey P, Suskin N, et al. A prospective comparison of cardiac rehabilitation enrollment following automatic vs. usual referral. J Rehabil Med. 2007;39:239–245. doi: 10.2340/16501977-0046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Arthur HM. Improving secondary prevention of cardiovascular disease through referral to cardiac rehabilitation. JCOM. 2006;13:572–577. [Google Scholar]
- 56.Witt BJ, Thomas RJ, Roger VL. Cardiac rehabilitation after myocardial infarction: A review to understand barriers to participation and potential solutions. Eura Medicophys. 2005;41:27–34. [PubMed] [Google Scholar]