Abstract
Background
If dysplasia is found on biopsies during surveillance colonoscopy for ulcerative colitis (UC), many experts recommend colectomy given the substantial risk of synchronous colon cancer. The objective was to learn if UC patients’ perceptions of their colon cancer risk and if their preferences for elective colectomy match with physicians’ recommendations if dysplasia was found.
Methods
A self-administered written survey included 199 patients with UC for at least 8 years (mean age 49 years, 52% female) who were recruited from Dartmouth-Hitchcock (n = 104) and the University of Chicago (n = 95). The main outcome was the proportion of patients who disagree with physicians’ recommendations for colectomy because of dysplasia.
Results
Almost all respondents recognized that UC raised their chance of getting colon cancer. In all, 74% thought it was “unlikely” or “very unlikely” to get colon cancer within the next 10 years and they quantified this risk to be 23%; 60% of patients would refuse a physician’s recommendation for elective colectomy if dysplasia was detected, despite being told that they had a 20% risk of having cancer now. On average, these patients would only agree to colectomy if their risk of colon cancer “right now” were at least 73%.
Conclusions
UC patients recognize their increased risk of colon cancer and undergo frequent surveillance to reduce their risk. Nonetheless, few seem prepared to follow standard recommendations for elective colectomy if dysplasia is found. This may reflect the belief that surveillance alone is sufficient to reduce their colon cancer risk or genuine disagreement about when it is worth undergoing colectomy.
Keywords: ulcerative colitis, colectomy, colon cancer, dysplasia, patient preferences
Because of their substantially increased risk of developing colon cancer, patients with ulcerative colitis (UC) undergo frequent surveillance with colonoscopy.1 For patients who have had the disease for 8 years or more the general recommendation is for colonoscopy every 1–2 years.2 This surveillance includes not only visual inspection for lesions, but random biopsies of normal-appearing mucosa to find flat “invisible” lesions that are dysplastic. The American College of Gastroenterology recommends total colectomy if cancer or high-grade dysplasia is identified.2 Moreover, based on the finding that low-grade dysplasia is associated with a 20% chance of synchronous cancer, most experts also recommend offering total colectomy for low-grade dysplasia.3–5
While experts agree that the risk of cancer in the setting of dysplasia is sufficiently high to warrant total colectomy, do patients with UC agree? Do they believe the risk of a synchronous cancer is high enough to warrant undergoing total colectomy, with its substantial morbidity? To answer this question we surveyed patients with longstanding UC at 2 academic medical centers to learn their perception of their colon cancer risk and when this risk is high enough for them to agree to elective colectomy.
MATERIALS AND METHODS
Sample and Survey Administration
To include patients eligible for undergoing frequent colonoscopy surveillance, we recruited patients with UC with a minimum duration of 8 years at 2 academic medical centers (Dartmouth-Hitchcock Medical Center, Lebanon, NH, University of Chicago, Chicago, IL). At Dartmouth-Hitchcock we identified patients by searching administrative databases for ICD-9 codes 556.x and confirmed the diagnosis and duration of disease by chart review. Eligible patients were mailed questionnaires from May through November of 2007. Nonresponders were mailed a second questionnaire after about 8 weeks. The response rate was 57% (104 out of 182 participated). At the University of Chicago, 95 consecutive patients attending the Inflammatory Bowel Disease Center clinic who had UC for a minimum of 8 years were invited to participate at routine clinic visits over this same time period. All patients participated. Participants at both sites were offered a $10 gift card for completing the survey.
Survey Instrument
This self-administered written questionnaire was designed to cover 4 domains: knowledge about colon cancer risk; experience with colonoscopy; risk threshold for colectomy; and personal history of UC. Drafts of the survey were reviewed with patients with UC using cognitive interviews (think-aloud protocols) to test for comprehension and revised based on feedback. The final survey included 45 questions (included in the Appendix).
Main Outcome Measures
The primary outcome was the proportion of patients who would disagree with a doctor’s recommendation of immediate colectomy for dysplasia. To try to ensure understanding, we asked the question in 2 ways: as a yes–no question (“If my doctor told me that pre-cancerous changes predict that there is a 20% chance that I already have cancer somewhere in my colon (not detectable by colonoscopy), and they recommend having my entire colon removed and having a J-pouch surgery performed, I would agree to this recommendation”) and using a previously validated visual analog “magnifier” scale for assessing risk perceptions6 (I would agree to have my entire colon removed if my doctor told me that my chance of having colon cancer right now was at least…?). We only counted respondents as disagreeing if they answered both questions consistently: said “no” to the yes/no question and chose a threshold of 20% or higher on the visual analog scale. The 8% of patients who answered inconsistently were not included in the primary analysis.
Secondary outcomes included the patients’ perceptions of their risk of colon cancer (assessed with qualitative and quantitative perceptions on the magnifier visual analog scale) and the benefit of surveillance colonoscopy.
Analysis
Because results from the 2 academic medical center samples did not differ importantly, we only present combined descriptive results. The margin of error for all questions was <9%. Univariate logistic regression analyses were performed to identify factors to predict the refusal of colectomy. All analyses were performed using STATA (v. 10; College Station, TX).
RESULTS
Table 1 shows that 199 patients had a mean age of 49 and almost all (98%) had at least a high school education. Most (81%) had UC for more than 10 years and ranged from asymptomatic (32%) to extremely symptomatic (10% with more than 5 self-described flares of disease activity a year).
TABLE 1.
Results
| n=199* | |
|---|---|
| Patient Characteristics | |
| Age (mean, IQR) | 49 years (41–58) |
| Women | 52% |
| Education | |
| Some high school | 2% |
| High school diploma | 24% |
| College degree | 38% |
| Graduate degree | 36% |
| Duration of ulcerative colitis | |
| 8–10 years | 19% |
| 11–20 years | 44% |
| Longer than 20 years | 37% |
| Colon involvement | |
| Pancolitis | 21% |
| Left-sided colitis | 32% |
| Proctitis | 21% |
| Unsure | 27% |
| Flares per year | |
| 0 | 32% |
| 1–2 | 47% |
| 3–5 | 10% |
| More than 5 | 10% |
| Previous hospitalization for UC | 39% |
| Medication requirements | |
| Prior IV steroid use | 26% |
| Current immunomodulator use | 21% |
| Current infliximab use | 4% |
| Perceptions of Colon Cancer Risk | |
| How likely do you think it is that you will get colon cancer in the next 10 years? | |
| Certain | 0% |
| Very Likely | 3% |
| Likely | 23% |
| Unlikey | 55% |
| Very unlikely | 19% |
| How does ulcerative colitis affect your chance of getting colon cancer? It makes my chance: | |
| Much higher | 43% |
| A little higher | 48% |
| No difference | 7% |
| A little lower | 1% |
| Much lower | 2% |
| Chance of getting colon cancer in the next 10 years? (median, IQR) | 20% (8%–36%) |
| Chance of dying from colon cancer in the next 10 years? (median, IQR) | 2% (0.01%–11%) |
| Perceptions of the Benifit of Colonoscopy | |
| How would you describe how yearly colonoscopy affects your chance of dying from colon cancer? | |
| Does not change the chance | 2% |
| Decreases it a little | 10% |
| Decreases it a lot | 78% |
| Eliminates the chance | 10% |
| Chance of dying from colon cancer in the next 10 years if you never have a colonoscopy? (median, IQR) | 51% (11%–72%) |
| Chance of dying from colon cancer in the next 10 years if you have a colonoscopy every year? (median, IQR) | 6% (0.15%–21%) |
| Decreased chance of dying because of annual colonoscopy (median, IQR) | 30% (11%–55%) |
Item non-response <5%; IQR = interquartile range.
Perceived Risk of Colon Cancer
Almost all respondents recognized that UC raised their chance of getting colon cancer: 43% said it made their chance “much higher,” 48% “a little higher,” but most patients thought that it was still “unlikely” or “very unlikely” that they would get colon cancer in the near 10 years (Table 1). They quantified this risk as a median chance of 20%. Almost all undergo frequent colonoscopy (55% every 1–2 years; 35% every 3–5 years) and 78% believed doing so decreased their risk of colon cancer death “a lot”; 10% thought it entirely eliminated the risk. They quantified their chance of dying from colon cancer as 51% if they never had a colonoscopy and 5.5% if they have annual colonoscopy.
Do Patients Agree with Experts for Colectomy Once Dysplasia Is Detected?
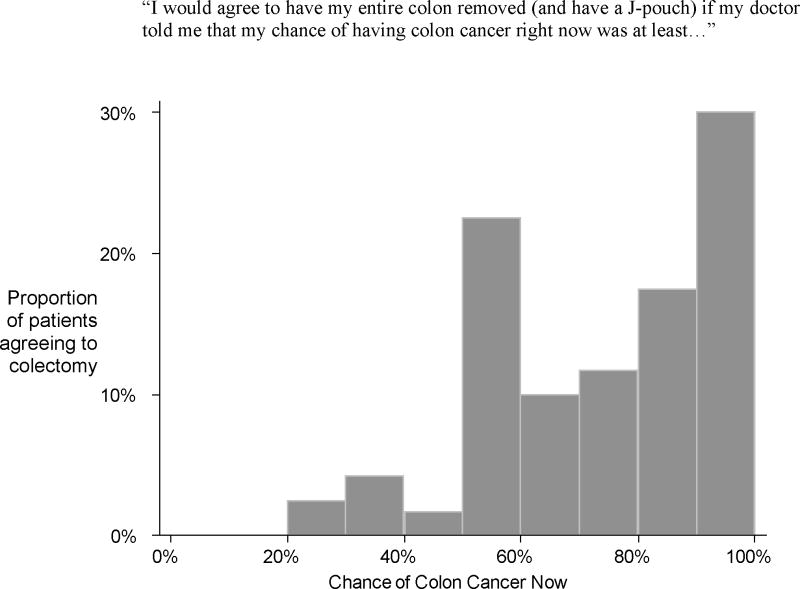
Sixty percent of patients would refuse a doctors’ recommendation for elective colectomy if dysplasia was detected, despite being told that they had a 20% risk of having a synchronous cancer now. On average, these patients would only agree to colectomy if their risk of colon cancer “right now” were at least 73% (SD 21.6). The distribution of the patients’ thresholds for colectomy is shown in Figure 1. Over half of the respondents (54%) said this risk would need to be even higher if a permanent external bag (ileostomy) was the only surgical option (i.e., they could not have restorative ileoanal J-pouch surgery).
FIGURE 1.
Distribution of patients’ thresholds for undergoing colectomy for the 120 patients who disagreed with the recommendation for colectomy. Patients were provided the following scenario: “After having a colonoscopy, your doctor could tell you that although they did not see a cancer, there are pre-cancerous changes in your colon. These pre-cancerous changes predict that you may already have cancer somewhere in your colon, but it is not detectable by colonoscopy. Therefore, your doctor recommends having your entire colon removed now. Your doctor suggests that you can have a surgery called a J-pouch. This surgery involves creating a pouch out of a portion of the remaining intestine and connecting it to the anus. You would not have an external bag, and you would move your bowels normally through your anus. On average, people who have a J-pouch have approximately 5–8 bowel movements/day.”
When asked in an open-ended question as to what would change their mind about having colectomy for dysplasia, the most frequent answers were: receiving a second opinion with the same recommendation (63%) and experiencing more symptoms of UC (20%). Nothing would change the minds of 4% of respondents.
Predictive Factors for Refusal of Colectomy
Univariate logistic regression analyses were performed to identify factors that would predict refusal of colectomy. Patients who did not think they would have to have their colon taken out over the next 10 years anyway “because of UC” were least likely to agree to colectomy for dysplasia (odds ratio 1.6, 95% confidence interval [CI] 1.1–2.3, P = 0.009). Factors not associated with refusal included: age, gender, disease duration, disease extent and severity, perception of colon cancer risk, and their worry about developing any type of cancer.
DISCUSSION
We found that patients with UC recognize that they have an increased risk of developing and dying from colon cancer. They undergo frequent surveillance; however, the majority of patients are not prepared to follow standard recommendations for colectomy if dysplasia is found.
Our study has important limitations. First, it is possible that patients simply did not understand the magnifier or the scenario. We tried to minimize this possibility by asking our primary question (about disagreeing with a doctor’s recommendation for colectomy given dysplasia) in 2 different ways and only including patients who gave internally consistent answers. Second, the scenarios posed in the questionnaire were hypothetical. Real-life decisions may be different, but studies in cancer patients comparing imagined versus actual health states show consistent beliefs about treatment before and during the experienced intervention.7,8 Finally, we cannot be sure about the generalizability of our findings. We only surveyed patients at 2 academic centers. Further, the participation rate in the Dartmouth sample was only 57% and the University of Chicago patients were a consecutive convenience sample.
Our findings suggest 2 important possibilities. In contrast to expert consensus, patients may believe that frequent colonoscopy itself affords them adequate protection against dying from colon cancer. On average, patients were extremely optimistic, estimating a 90% relative risk reduction in mortality if they undergo routine surveillance colonoscopy. Alternatively, patients may genuinely disagree about the level of cancer risk making colectomy worth it, given its complications and effects on quality of life. For patients who feel that it is unlikely they will ultimately need a colectomy because of their UC, it may be especially hard to accept the prospect of having a major surgery for a theoretical risk of cancer.
It is surprising that such a large proportion of UC patients disagree with physician recommendations for when they should undergo colectomy for a finding of dysplasia. The majority of these patients undergo colonoscopy surveillance. The purpose of this intense invasive surveillance is not only to look for cancer but to look for dysplasia with the intent of early surgery. Patients need to understand that goal. But the ultimate decision about if or when to undergo colectomy for low-grade dysplasia rests with patients. If patients do not understand the size of the risk they face they cannot possibly decide when surgery is worth it. It is the physician’s responsibility to properly communicate the current state of knowledge, and to help patients choose what is right for them.
Supplementary Material
Acknowledgments
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the National Institutes of Health. The authors declare no conflicts of interest.
Supported by the Foundation for Clinical Research in Inflammatory Bowel Disease. Dr. Siegel is supported by a CCFA career development award and by grant K23DK078678 from the National Institute of Diabetes and Digestive and Kidney Diseases.
Footnotes
Additional Supporting Information may be found in the online version of this article.
References
- 1.Eaden JA, Abrams KR, Mayberry JF. The risk of colorectal cancer in ulcerative colitis: a meta-analysis. Gut. 2001;48:526–535. doi: 10.1136/gut.48.4.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kornbluth A, Sachar DB. Ulcerative colitis practice guidelines in adults (update): American College of Gastroenterology, Practice Parameters Committee. Am J Gastroenterol. 2004;99:1371–1385. doi: 10.1111/j.1572-0241.2004.40036.x. [DOI] [PubMed] [Google Scholar]
- 3.Thomas T, Abrams KA, Robinson RJ, et al. Meta-analysis: cancer risk of low-grade dysplasia in chronic ulcerative colitis. Aliment Pharmacol Ther. 2007;25:657–668. doi: 10.1111/j.1365-2036.2007.03241.x. [DOI] [PubMed] [Google Scholar]
- 4.Ullman T, Croog V, Harpaz N, et al. Progression of flat low-grade dysplasia to advanced neoplasia in patients with ulcerative colitis. Gastroenterology. 2003;125:1311–1319. doi: 10.1016/j.gastro.2003.08.023. [DOI] [PubMed] [Google Scholar]
- 5.Itzkowitz SH, Present DH. Consensus conference: colorectal cancer screening and surveillance in inflammatory bowel disease. Inflamm Bowel Dis. 2005;11:314–321. doi: 10.1097/01.mib.0000160811.76729.d5. [DOI] [PubMed] [Google Scholar]
- 6.Woloshin S, Schwartz LM, Byram S, et al. A new scale for assessing perceptions of chance: a validation study. Med Decis Making. 2000;20:298–307. doi: 10.1177/0272989X0002000306. [DOI] [PubMed] [Google Scholar]
- 7.Jansen SJ, Kievit J, Nooij MA, et al. Stability of patients’ preferences for chemotherapy: the impact of experience. Med Decis Making. 2001;21:295–306. doi: 10.1177/0272989X0102100405. [DOI] [PubMed] [Google Scholar]
- 8.Llewellyn-Thomas HA, Sutherland HJ, Thiel EC. Do patients’ evaluations of a future health state change when they actually enter that state? Med Care. 1993;31:1002–1012. doi: 10.1097/00005650-199311000-00003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.