Abstract
OBJECTIVE
Nitric oxide (NO) is a key metabolic and vascular regulator. Its production is stimulated by insulin. A reduced urinary excretion of NO products (NOx) is frequently found in type 2 diabetes, particularly in association with nephropathy. However, whether the decreased NOx excretion in type 2 diabetes is caused by a defective NOx production from arginine in response to hyperinsulinemia has never been studied.
RESEARCH DESIGN AND METHODS
We measured NOx fractional (FSR) and absolute (ASR) synthesis rates in type 2 diabetic patients with diabetic nephropathy and in control subjects, after l-[15N2-guanidino]-arginine infusion, and use of precursor–product relationships. The study was conducted both before and after an euglycemic hyperinsulinemic (∼1,000–1,200 pmol/l) clamp.
RESULTS
In type 2 diabetes, NOx FSR was reduced both under basal (19.3 ± 3.9% per day, vs. 22.9 ± 4.5% per day in control subjects) and hyperinsulinemic states (24.0 ± 5.6% per day, vs. 37.9 ± 6.4% per day in control subjects; P < 0.03 by ANOVA). Similarly, in type 2 diabetes, NOx ASR was lower than in control subjects under both conditions (basal, 0.32 ± 0.06 vs. 0.89 ± 0.34 mol per day; hyperinsulinemia, 0.35 ± 0.07 vs. 1.15 ± 0.38 mol per day; P = 0.01 by ANOVA). In type 2 diabetes, the ability of insulin to stimulate both the FSR (4.7 ± 3.2% per day) and the ASR (0.03 ± 0.04 mol per day) of NOx was several-fold lower than that in control subjects (15.0 ± 2.9% per day and 0.25 ± 0.07 mol per day, P < 0.03 and P < 0.02, respectively). Also the fraction of arginine flux converted to NOx (basal, 0.22 ± 0.05% vs. 0.65 ± 0.25%; hyperinsulinemia, 0.32 ± 0.06% vs. 1.03 ± 0.33%) was sharply reduced in the patients (P < 0.01 by ANOVA).
CONCLUSIONS
In type 2 diabetic patients with nephropathy, intravascular NOx synthesis from arginine is decreased under both basal and hyperinsulinemic states. This defect extends the concept of insulin resistance to NO metabolism.
Nitric oxide (NO) is a key regulatory molecule with extensive metabolic, vascular, and cellular effects (1–6). The regulation of NO metabolism is particularly important in type 2 diabetes, because activation of NO synthase (NOS) is under insulin control through the Akt pathway (3,5). Thus, disturbances of NO generation may be a consequence of insulin resistance affecting also the vascular response (3). An impaired NO metabolism is found in type 2 diabetes (7–10), in particular in the presence of nephropathy (11). A reduced urinary excretion of nitric oxide–related products, such as nitrites and nitrates, collectively termed as [NOx], has been reported in type 2 diabetic patients with nephropathy (12,13). Conversely, microalbuminuria is associated with impaired endothelial function in type 2 diabetic subjects (14). Hyperglycemia may also play a role in the decreased NO production in type 2 diabetes, because high glucose per se inhibited endothelial NOS activity in the glomeruli, through a protein kinase C–associated mechanism (15). Moreover, high glucose and/or the associated advanced glycosylation end products decreased NOS expression (11). Urinary NOx production is reduced in nondiabetic renal disease (16), although also increased plasma nitrate concentrations have been reported in type 2 diabetes, as well as in the Metabolic Syndrome (17,18), thus questioning the validity of urinary methods to assess whole-body NOx production.
Because the stimulation of NOS activity by insulin is impaired in muscle of type 2 diabetic patients (19), investigations on the response to the hormone of whole-body NO production in type 2 diabetes is of key relevance. An impaired NO generation in type 2 diabetes may be another feature of insulin resistance (3).
We recently developed a precursor–product, stable isotope method to measure whole-body synthesis of NO-related compounds in vivo (20). Therefore, the aim of this study was twofold: 1) to measure NOx production rate (both fractional and absolute), as well as the rate of arginine conversion to NOx, in type 2 diabetic patients with diabetic nephropathy and 2) to study the effects of acute hyperinsulinemia on these parameters.
RESEARCH DESIGN AND METHODS
Eight male type 2 diabetic patients with diabetic nephropathy and ten male nondiabetic healthy volunteers, comparable for age and BMI, were recruited. Their clinical and biochemical characteristics are reported in Table 1. All subjects had been adapted for at least one month to a diet containing ∼50% calories as carbohydrate, ∼20% as proteins, and ∼30% as lipids. Protein intake was ∼80–100 g per day and was not restricted in any subject. In the day before the study, all subjects consumed a low-nitrate diet to minimize the contribution of exogenous nitrates to whole-body NOx turnover.
TABLE 1.
Clinical and biochemical characteristics of the type 2 diabetic and control subjects studied
| T2DM (n = 8) | Control subjects (n = 10) | |
|---|---|---|
| Age (years) | 63 ± 3 | 52 ± 6 |
| BMI (kg/m2) | 28.9 ± 0.8 | 26.4 ± 0.8 |
| Disease duration (years) | 17 ± 2 | |
| HbA1C (%) | 8.38 ± 0.29† | 5.44 ± 0.23 |
| Fasting glucose (mmol/l) | 12.1 ± 1.0† | 4.8 ± 0.1 |
| Fasting insulin (pmol/l) | 99 ± 18† | 46 ± 8 |
| Plasma creatinine (μmol/l) | 105 ± 11† | 75 ± 2 |
| Glomerular filtration rate (measured) (ml/m2 · min) | 85 ± 6 | |
| Glomerular filtration rate (calculated) (ml/m2 · min) | 86 ± 9 | 117 ± 13 |
| Albuminuria (g/day) | 1.9 ± 0.6† | <0.03 |
| Total cholesterol (mmol/l) | 4.9 ± 0.3 | 4.9 ± 0.3 |
| HDL cholesterol (mmol/l) | 1.2 ± 0.1 | 1.3 ± 0.1 |
| Triglycerides (mmol/l) | 1.8 ± 0.4 | 1.1 ± 0.2 |
| TNF-α (pg/ml) | 150 ± 50 | 80 ± 14 |
| IL-6 (pg/ml) | 68 ± 49 | 10 ± 3 |
| IL-8 (pg/ml) | 72 ± 12† | 27 ± 5 |
| IL-10 (pg/ml) | 0.37 ± 0.09 | 0.44 ± 0.11 |
| hsCRP (mg(L) | 3.73 ± 1.48 | 0.73 ± 0.23 |
*P < 0.05.
†P < 0.02 or less vs. control subjects. T2DM, type 2 diabetic subjects.
All the diabetic subjects and five control subjects were hypertensive (the latter affected by essential hypertension) and treated with combinations of hypotensive drugs, such as ACE inhibitors (in three type 2 diabetes and five control subjects), ARBs (in five type 2 diabetes subjects), calcium antagonists (in three type 2 diabetes subjects), β-blockers (in three type 2 diabetes and two control subjects), and diuretics (in three type 2 diabetes and two control subjects). Four diabetic subjects and one control subject were also treated with statins. All drugs were suspended the night before the study day. The antidiabetic treatment in the patients consisted of diet alone (two subjects), oral hypoglycemic agents (four subjects, two with glybenclamide, one with metformin, and one with glybenclamide, metformin, and pioglitazone), intermediate-acting insulin plus metformin (one patient), and split insulin doses (one patient). The antidiabetic therapy was suspended the night before the study day. The control subjects had no history of either diabetes or impaired glucose tolerance, and their fasting plasma glucose, HbA1c, and general blood chemistry were normal. The urinary albumin excretion rate was measured on at least two 12-h urine collections. The type 2 diabetic patients had, by definition, an increased albumin excretion rate (five in the macroalbuminuria and three in the microalbuminuria range). The glomerular filtration rate (GFR) in the diabetic subjects was determined by 51Cr–EDTA infusion (21), and in both study groups it was estimated also using the Cockcroft-Gault formula (22). The type 2 diabetic patients had either a normal (GFR > 80 ml/m2 · min, n = 5) or a moderately impaired renal function (i.e., a GFR between 60 and 80 ml/m2 · min, n = 3).
Aims, benefits, and potential risks of the study were explained in detail, and each subject signed an informed consent. The protocol was approved by the Ethical Committee of the Medical Faculty at the University of Padova, Italy, and it was performed according to the Helsinki Declaration (as revised in 1983).
All subjects were admitted to the Metabolic Unit of the Department of Metabolic Diseases at 7:00 a.m. on the study day, after the overnight fast. The diabetic subjects were moderately hyperglycemic (Table 1). An 18-gauge polyethylene catheter was placed in an antecubital vein of the right arm, for isotope, insulin, and glucose infusion. A contralateral wrist vein was cannulated in a retrograde fashion, and the hand was placed in a box heated at 55°C throughout the study, for venous-arterialized blood sampling.
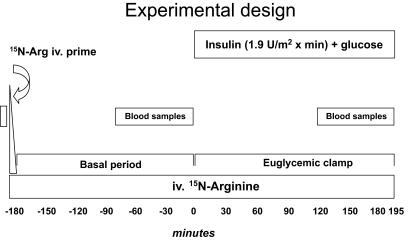
After a baseline blood sample (Figs. 1 and 2), a primed (2.4 μmol/kg), continuous (0.04 μmol/kg · min) infusion of l-[15N2-guanidino]-arginine (15N2-arginine, sterile and pyrogen-free) (MassTrace, Woburn, MA; isotope purity = 99%) was started at ∼07:30 a.m. (defined as −180 min). Blood samples were drawn every 30 min for ∼2 h, to assess the achievement of steady state in blood isotope enrichment (data not shown). In the diabetic group, after 100 min from the start of isotope infusion, five blood samples were collected every 20 min (i.e., between −80 min and 0 min), for measurements of whole-blood isotope enrichments of NOx and arginine, as well as for plasma substrate and hormone concentrations (Figs. 2 and 3, upper panels). In the control group, there were minor changes in blood sampling, which started 120 min after the initiation of isotope infusion (i.e., at −60 min) and was spaced by 15-min intervals (i.e., five samples) for blood isotope enrichments of NOx, and by 30-min intervals (three samples) for blood arginine, plasma substrate, and hormone concentrations (Figs. 2 and 3, lower panels).
FIG. 1.
Schematic depiction of the experimental design.
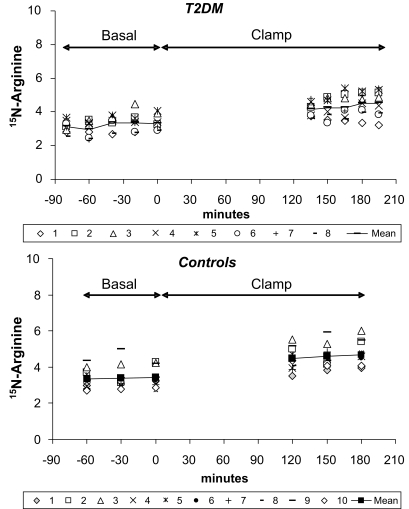
FIG. 2.
Whole-blood TTR values of 15N-arginine at steady state in the basal and in the clamp period, reported as individual values in the type 2 diabetic (T2DM) (upper panel, n = 8) and in the control subjects (bottom panel, n = 10). Continued lines indicate the mean values of each group.
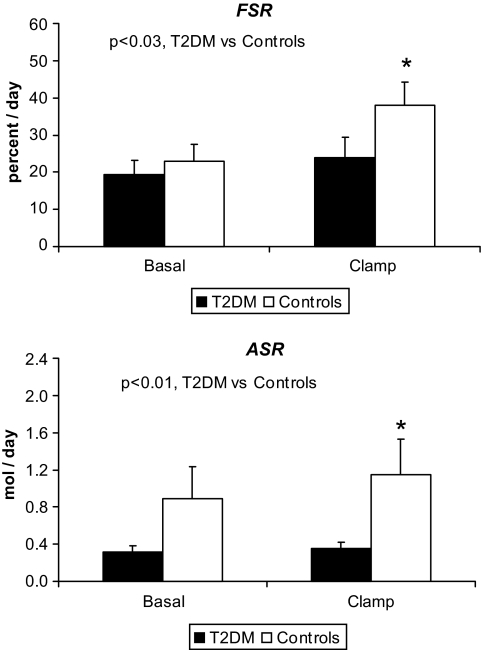
FIG. 3.
Whole-blood TTR values of 15NOx in the basal and in the clamp period, reported as individual values in the type 2 diabetic (T2DM) (upper panel, n = 8) and in the control subjects (bottom panel, n = 10). From the change in TTR versus time in each experimental period, the slopes reported in Table 3 have been calculated.
Thereafter, an euglycemic hyperinsulinemic clamp was started as described elsewhere (20) (Fig. 1). Briefly, regular insulin (Humulin R, Eli Lilly, Indianapolis, IN) was infused at the rate of 1.9 mU/kg · min−1 for 180 min. In the first 10 min, the rate of insulin infusion was doubled to rapidly prime the insulin pool. Plasma glucose concentration was monitored every 10 min. In the nondiabetic subjects, euglycemia (between 4.7 and 5 mmol/l) was maintained by a variable exogenous 20% dextrose infusion, whereas in the diabetic subjects, blood glucose was allowed to decrease from the basal values and reached the euglycemic range within 74 ± 9 min. Thereafter, blood glucose values were maintained between 4.7 and 5 mmol/l by dextrose infusion, for an additional 120 min. Therefore, the total duration of the clamp period was 180 min in the control subjects and ∼195 min in the diabetic patients (Figs. 1 and 2). After ∼120 min–135 min from the start of the insulin infusion, five additional blood samples were again drawn every 15 min, for the measurements at the new steady state.
Analytical measurements.
Blood (3 ml) was collected into preweighed chilled tubes containing 3 ml of 20% perchloric acid (w/vol), vigorously shaken, and immediately kept on ice. An additional 2 ml of blood were collected into preweighed chilled tubes containing 4 ml of absolute ethanol, gently shaken and kept on ice. Another 2 ml of blood were also collected into chilled tubes containing 50 μl of EDTA (6% w/vol), gently mixed, and kept on ice. All tubes were centrifuged within 1 h and reweighed, and the supernatant was stored at −80°C until assay.
Whole-blood 15N2-arginine enrichment was measured from 1 ml of the perchloric acid extract, titrated to alkaline pH with 6 N KOH and eluted through an AG 50W-X8 resin with 4 N NH4OH. The eluate was analyzed by gas chromatography mass spectrometry (model 5,973, Agilent, Palo Alto, CA) as trifluoroacetyl derivative using positive chemical ionization, by monitoring the fragments (m/z) [479/477]. Enrichments were expressed as tracer-to-tracee ratio (TTR) (23). Whole-blood NOx enrichments were determined in the supernatant of the ethanol-containing tubes as nitrobenzene derivative (24), by gas chromatography combustion-isotope ratio mass spectrometry (Delta Plus GC-C-IRMS, ThermoElectron, Bremen, Germany), as described in detail elsewhere (20). Blood NOx concentrations were determined from the ethanol supernatant (25), using a commercial assay (Nitrate/Nitrite Colorimetric Assay kit, Cayman Chemical Co., Ann Arbor, MI), after correction of blood dilution by weight differences, and accounting for blood specific weight. Plasma insulin and amino acid concentrations were determined as reported in ref (20). TNF-α, IL-6, Il-8 and Il-10, and hsCRP were measured using commercial assays. hsCRP was measured by an automated immunonephelometric assay (Dade-Behring, Marburg, Germany). TNF-α, IL 6, Il-8, and Il-10 were measured by an ELISA (Biosciences, MD).
Calculations.
The arginine rate of appearance (Ra) was calculated according to a standard steady-state formula (20,23):
where i is l-[15N2-guanidino]-arginine tracer infusion rate (in μmol/kg · min); TTRi is the isotope enrichment (as TTR) of the infused tracer; and TTRwb is whole-blood 15N2-arginine TTR (corrected for the natural preinfusion value), in either the basal or the insulin infusion period. A near steady state in blood arginine TTR was attained in both the basal and the hyperinsulinemic periods (Fig. 2). Arginine flux was also expressed on a 24-h basis to calculate the fraction of daily 15NOx production from [15N2]-arginine (see below).
The fractional synthesis rate (FSR) of NOx conceptually corresponds to the percent of the circulating pool newly synthesized over the unit of time (20,23), and it was calculated as follows:
where: dTTR(15NOx) is the derivative with respect to time (dt) of the change of whole-blood NOx TTR values, which were calculated on 4–5 time points in the basal state as well as in the insulin-infusion period, respectively (Figs. 1 and 2). The 15N-Arg TTR is the mean blood 15N-arginine TTR within the same experimental periods. The factor (1,440) converts the results to 24 h, and (100) expresses them on a percent basis.
The absolute synthesis rate of NOx (ASR) (in mmol per day) is then calculated by multiplying FSR times the total NOx pool, which is the product between the average whole-blood NOx concentration (in mmol/l) of each experimental period and the nitrate distribution volume (in liters), taken as 28% of body weight (26).
Statistical analysis.
The two-way ANOVA for repeated measurements was used to compare basal and clamp periods between diabetic and control subjects. The post hoc Tukey test was used to test changes versus basal within each group. The two-tailed Student t test for unpaired data was used to compare two sets of single data points (i.e., the delta changes versus basal after the clamp). Analyses were performed on the log transformations when data distribution was not normal. Regression analysis was performed using simple linear relationships, by the Statistica Software (Version 6, StatSoft, Tulsa, OK). A P value < 0.05 was considered statistically significant. Data have been expressed as mean ± SE.
RESULTS
Substrates, hormones, insulin-mediated glucose disposal, and isotope enrichments.
In the fasting state, the type 2 diabetic subjects had significantly greater glucose, HbA1c, insulin, and creatinine plasma concentrations than control subjects (Table 1). In the type 2 diabetic patients, the mean albumin excretion rate was ∼2 g per day, and their GFR was ∼25% lower (albeit not significantly, P > 0.05) than the calculated values in control subjects.
During the clamp, plasma insulin was acutely raised by ∼10 times versus basal values in both the diabetic (to 1,240 ± 70 pmol/l) and the control subjects (to 1,037 ± 117 pmol/l), to similar values in both groups. In the type 2 diabetic patients, plasma glucose was slowly decreased to near euglycemia (∼4.7–5 mmol/l) that was then maintained at this level throughout the study. At steady-state (i.e., in the last 30 min of the clamp period, average values), plasma glucose concentrations were similar between the type 2 diabetes (4.83 ± 0.05 mmol/l) and the control subjects (4.96 ± 0.12 mmol/l), whereas the insulin-mediated glucose disposal (i.e., the “M” value) was 4.48 ± 0.56 mg/kg · min in the type 2 diabetes subjects and 6.98 ± 0.84 mg/kg · min in the control subjects (P = 0.032 between the two groups), indicating insulin resistance in type 2 diabetes. Similar results were obtained when the glucose disposal rate was normalized over the average insulin concentration (expressed as the [M/I] value, i.e., in mg/kg/μU of plasma insulin) (type 2 diabetes, 0.0262 ± 0.0030; control subjects, 0.0519 ± 0.0069; P < 0.01 between the two).
Plasma amino acid concentrations are reported in Table 2. Hyperinsulinemia reduced, as expected, the concentrations of most amino acids. Interestingly, arginine decreased significantly in the control but not in the type 2 diabetes group. Taurine concentrations were greater, whereas those of asparagine and threonine were lower in type 2 diabetes than in control subjects. No differences between the groups in total and branched-chain amino acids were detected. As a group, the type 2 diabetic subjects had increased concentrations of inflammatory cytokines (Table 1), although only the difference in IL-8 levels was significant.
TABLE 2.
Plasma amino acid average concentrations (in μmol/l) in the postabsorptive state and after the euglycemic hyperinsulinemic clampa
| Basal |
Clamp |
|||
|---|---|---|---|---|
| T2DM (n = 8) | Control subjects (n = 10) | T2DM (n = 8) | Control subjects (n = 10) | |
| Taurine | 126 ± 12‡ | 61 ± 9 | 137 ± 20‡ | 47 ± 6 |
| Asparagine | 9 ± 2‡ | 20 ± 4 | 7 ± 1‡ | 13 ± 2* |
| Threonine | 99 ± 7† | 116 ± 6 | 63 ± 6*† | 67 ± 5* |
| Serine | 87 ± 3 | 107 ± 9 | 63 ± 4* | 65 ± 4* |
| Glycine | 154 ± 9 | 173 ± 13 | 143 ± 9 | 134 ± 7 |
| Alanine | 306 ± 16 | 303 ± 25 | 254 ± 9 | 226 ± 11* |
| Citrulline | 35 ± 3 | 31 ± 2 | 24 ± 1* | 18 ± 1* |
| Valine | 250 ± 12 | 227 ± 17 | 173 ± 11* | 133 ± 12* |
| Methionine | 17 ± 1 | 20 ± 2 | 9 ± 1* | 14 ± 2* |
| Isoleucine | 70 ± 5 | 58 ± 4 | 30 ± 4* | 18 ± 2* |
| Leucine | 129 ± 5 | 137 ± 11 | 61 ± 5* | 69 ± 8* |
| Tyrosine | 49 ± 4 | 55 ± 4 | 29 ± 2* | 29 ± 2* |
| Phenylalanine | 49 ± 2 | 46 ± 2 | 34 ± 2* | 29 ± 2* |
| Ornitine | 62 ± 4 | 57 ± 4 | 40 ± 6* | 43 ± 4* |
| Lysine | 173 ± 5 | 176 ± 10 | 131 ± 7* | 122 ± 11* |
| Histidine | 68 ± 3 | 67 ± 4 | 58 ± 2* | 52 ± 4* |
| Arginine | 68 ± 3 | 91 ± 16 | 48 ± 6 | 50 ± 7* |
| Total AA | 1,749 ± 26 | 1,726 ± 61 | 1,304 ± 57* | 1,117 ± 49* |
| BCAA | 447 ± 20 | 423 ± 31 | 264 ± 20* | 220 ± 20* |
aBCAA = Branched-chain amino acids. Glutamine, glutamate, and proline were not determined.
*P < 0.05 or less vs. basal (by ANOVA, post hoc Tukey test).
†P < 0.05.
‡P < 0.02 or less, type 2 diabetic vs. control subjects (by ANOVA, either interaction or group effect). T2DM, type 2 diabetic subjects.
NO and arginine kinetics.
Near steady-state conditions in blood 15N-arginine enrichments were attained in both periods (Fig. 2). In subjects with type 2 diabetes, postabsorptive whole-blood NOx concentrations (81 ± 18 μmol/l) were ∼50% lower (P < 0.05) than in control subjects (162 ± 35 μmol/l). After hyperinsulinemia, NOx concentrations were significantly decreased in the latter (to 128 ± 24 μmol/l, P < 0.05 vs. basal), whereas the decrease in the patients (to 65 ± 10 μmol/l) was not significant (P > 0.15 vs. basal). There was an overall significant difference between the two groups in NOx concentrations (P = 0.025 by ANOVA, group effect).
In the type 2 diabetic patients, basal arginine flux was not different from that of control subjects, and it was suppressed by hyperinsulinemia, to the same extent in both groups (Table 3). Blood 15NOx TTR increased progressively with time in both groups (Fig. 3), with this increase being satisfactorily described by linear relationships with a mean correlation coefficient (r) of ≥0.9 in both groups (Table 3). In the type 2 diabetic subjects, the increase of 15NOx TTR versus time during the clamp was significantly lower (P < 0.01 by ANOVA for interaction) than that in control subjects. To translate these figures into the NOx FSR, the slopes need to be divided over the steady-state 15N-arginine enrichment, as described in the Research Design and Methods section (see Eq. 2).
TABLE 3.
Steady-state, average isotope TTR of whole-blood 15N arginine; change (i.e., the slope) of whole-blood 15NOx TTR vs. time (dt, in min) (x 103); and their correlation coefficients (R); arginine Ra (in μmol/kg · min); and whole-blood average NOx concentrations (in μmol/l), in the basal state and after the hyperinsulinemic hyperglycemic clamp, in the type 2 diabetic and control subjects
| Basal |
Clamp |
|||
|---|---|---|---|---|
| T2DM (n = 8) | Control subjects (n = 10) | T2DM (n = 8) | Control subjects (n = 10) | |
| 15N-Arginine TTR | 3.24 ± 0.16 | 3.35 ± 0.21 | 4.41 ± 0.24§ | 4.43 ± 0.18§ |
| 15NOx slopes | 0.438 ± 0.090‡ | 0.520 ± 0.098 | 0.688 ± 0.126*‡ | 1.133 ± 0.166§ |
| R of the 15NOx slopes | 0.92 ± 0.03 | 0.90 ± 0.02 | 0.92 ± 0.03 | 0.89 ± 0.02 |
| Arginine flux | 1.13 ± 0.06 | 1.28 ± 0.05 | 0.84 ± 0.06§ | 0.98 ± 0.04§ |
| NOx concentrations | 81 ± 1† | 162 ± 36 | 65 ± 10† | 128 ± 24§ |
*P < 0.05 and
§P < 0.015 or less, clamp vs. basal (by ANOVA, post hoc Tukey test).
†P < 0.025 and
‡P < 0.01 or less, type 2 diabetic vs. control subjects (by ANOVA, either interaction or group effect). T2DM, type 2 diabetic subjects.
In the fasting state, NOx FSR in the type 2 diabetic patients (19.3 ± 3.9% per day) was ∼15% lower than that in control subjects (22.9 ± 4.5% per day) (Fig. 4). After hyperinsulinemia, NOx FSR did not increase in the patients (to 24.0 ± 5.6% per day, not significant versus baseline), whereas it increased significantly in the control subjects (to 37.9 ± 6.4% per day, P < 0.001 vs. baseline by the paired t test; P < 0.03 by ANOVA between groups, interaction effect). These differences between groups were maintained also when subject #2, who exhibited somehow extreme data, as reported in the lower panel of Fig. 3, was excluded. An inverse relationship between NOx FSR during the clamp and plasma creatinine within the entire subjects' set was found (R = −0.52, P < 0.05).
FIG. 4.
(Upper panel) NOx FSR, expressed as percent of pool per day, and (bottom panel) NOx ASR (expressed as mol per day), in the type 2 diabetic (black bars, n = 8) and in the control subjects (white bars, n = 10) in the basal and in the clamp periods. Asterisks indicate a significant change versus basal (P < 0.005 by ANOVA, post hoc Tukey test) within a group, whereas the P values indicate the significant difference between the two groups by considering both periods together (by ANOVA, either interaction or group effect).
Basal NOx ASR in the type 2 diabetes patients (0.32 ± 0.06 mol per day) was ∼1/3 of the control value (0.89 ± 0.34 mol per day), and it increased only by ∼10% (to 0.35 ± 0.07 mol per day, not significant versus basal), as opposed to a ∼30% increase in control subjects (to 1.15 ± 0.38 mol per day, P < 0.01 vs. basal; P < 0.01 by ANOVA, group effect) (Fig. 4).
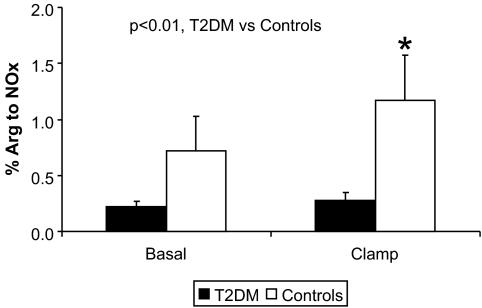
The fraction of arginine converted to NOx was significantly increased by hyperinsulinemia in the control but not in the diabetic group (Fig. 5). In the patients, such a change was ∼three- to fourfold lower (basal, 0.22 ± 0.05%, versus clamp, 0.32 ± 0.06%) than the corresponding values in the control subjects (basal, 0.65 ± 0.25%, versus clamp, 1.03 ± 0.33%, respectively; P < 0.01 by ANOVA, interaction effect).
FIG. 5.
Fraction of arginine converted to NOx in the type 2 diabetic (black bars, n = 8) and in the control subjects (white bars, n = 10) in the basal and in the clamp periods. The asterisk indicates a significant change versus basal (P < 0.001 by ANOVA, post hoc Tukey test), whereas the P value within the figure indicates the significant difference between the two groups by considering both periods together (by ANOVA, interaction effect).
When the data of the diabetic subjects (all with hypertension) were compared just with those of the five hypertensive, nondiabetic subjects, the differences between the two groups were somewhat blunted but still significant as regards both the increase of NOx FSR after the clamp (+12.0 ± 4.4% per day in the hypertensive control subjects, versus 4.68 ± 3.2% per day in the type 2 diabetes patients; P < 0.05) and the fractional arginine conversion to NOx (still twofold greater in control subjects; P < 0.05 by ANOVA for interaction), whereas NOx concentrations and ASR were of intermediate values and no longer significantly different from those of the type 2 diabetes group. Interestingly, in the nondiabetic, hypertensive subjects, the insulin-mediated glucose disposal (5.01 ± 0.33 mg/kg · min) was no longer different from that of the type 2 diabetic patients (4.48 ± 0.56 mg/kg · min), showing a comparable degree of insulin resistance.
DISCUSSION
This study shows that, in type 2 diabetic patients with nephropathy, whole-body NOx synthesis is decreased and is not appropriately stimulated by hyperinsulinemia. The fractional conversion of arginine to NOx is also impaired and not normally enhanced by insulin. This is the first study directly showing a decreased whole-body NOx synthesis and a decreased conversion of arginine to NOx, in type 2 diabetes in response to insulin.
Nitric oxide is likely to be involved in the defective insulin-mediated stimulation of blood flow in type 2 diabetes (3,27) as well as in the pathogenesis of diabetic nephropathy (11). The stimulation of NOS activity is a downstream effect of Akt activation by insulin; therefore, insulin resistance may be the cause of the reduced nitric oxide production in type 2 diabetes. Insulin insufficiently stimulated NOS activity in skeletal muscle of type 2 diabetic subjects (19). Our whole-body data agree with previous reports in muscle. Because arginine concentrations (Table 2) and flux (Table 3) were similar in both groups, the impaired NOx production was not substrate-limited, but rather related to a defective arginine conversion to NOx.
The site of NOx production is likely the endothelial cells, which express the bulk of constitutive NOS activity responsible for NO release into the bloodstream (3,5). In vascular endothelial cells, insulin stimulates NO production in a dose-dependent fashion through the phosphatidylinositol 3 (PI-3)-kinase/protein kinase B (Akt) pathway (28). In arteriolar muscle cells, NOS activation by insulin is dependent on a normally responsive IRS-1/PI-3 pathway (28). Conversely, insulin resistance at this level impairs insulin-mediated vasodilation and results in endothelial dysfunction (29). Because muscle is a key site of insulin resistance in diabetes, it can be suggested that the endothelial cells involved are mainly those of skeletal muscle. Indeed, basal and insulin-stimulated muscle NOS activity was impaired in well-controlled type 2 diabetic subjects, paralleling the severity of insulin resistance (19). In our study, we did not measure the activity of the IRS-1/PI-3/Akt pathway, because no muscle biopsy was performed. However, the previously referenced reports would indicate muscle endothelial cells as key sites of such resistance.
NOx concentrations were reduced by hyperinsulinemia despite the increase of NOx synthesis. Such an observation may indicate that insulin, besides its stimulatory effect on NOx production, also increased NOx removal. Such an hypothesis is intriguing and not directly proven so far. Alternatively, other insulin-induced changes (such as the exogenous glucose infusion, the modification of plasma amino acids and other substrate concentrations, or others) might be involved and need to be specifically investigated. On the other hand, because high glucose inhibits NOS activity per se (15), the acute insulin-induced glucose decrease was not responsible for the blunted increase of NO production observed in the patients.
The diabetic subjects were treated with hypoglycemic agents. Moreover, all of them, and half of the control subjects too, were also treated with pressure-lowering agents and with statins. These drugs may affect NOS activity (30–33). Nevertheless, the type 2 diabetic patients, who were more heavily and extensively treated than the control subjects, exhibited a decreased NOx production, suggesting that, despite therapy, they had an impaired NOS activity.
Whether the observed defects in NOx metabolism are due to diabetes itself, to the accompanying nephropathy, or to insulin resistance, possibly amplified by hypertension (34), cannot be concluded from our experiments. In order to account at least in part for hypertension as a potentially confounding factor, we enrolled in the nondiabetic, control group also hypertensive subjects (five of ten), otherwise clinically and metabolically healthy. When compared with the diabetic group, the NOx and arginine kinetic data of these nondiabetic, hypertensive subjects were somehow intermediate with respect to the whole control group. Nevertheless, significant differences versus the type 2 diabetic patients, in both NOx FSR and in the fractional arginine conversion to NOx, were maintained. Interestingly, these nondiabetic, hypertensive subjects were insulin resistant as regards glucose disposal, as much as the type 2 diabetic subjects. Thus, it cannot be excluded that hypertension per se (and/or the associated insulin resistance) played at least a partial role in the defects observed in type 2 diabetes. Hypertension, however, is an invariable finding in type 2 diabetes with nephropathy (35); therefore, it would be impossible to distinguish between the effects of diabetes per se from those of hypertension in these patients. The relationships between hypertension and NO turnover should be further investigated.
We intentionally chose to study type 2 diabetic subjects who were also likely to exhibit alterations in NOx homeostasis and metabolism, i.e., patients with nephropathy. It is possible that nephropathy itself had some effect. In this respect, we found an inverse relationship between NOx FSR during the clamp and plasma creatinine within the entire subjects' set. Additional studies in type 2 diabetic patients without nephropathy, as well as in nondiabetic subjects with other forms of nephropathy, are required to answer this question, particularly as regards the insulin effect. In this regard, we previously reported a decreased basal NOx synthesis in type 2 diabetic patients without nephropathy (10), although the response to insulin was not tested.
The increase of inducible NOS by endotoxin and/or inflammatory states is associated with impaired insulin-stimulated muscle glucose uptake (36–40). Although our type 2 diabetic patients did not exhibit overt signs of inflammation, measured cytokines tended to be greater in the patients than in control subjects, although only the increase of IL-8 was significant (Table 1). However, an increased inducible NOS activity would be associated with an increased NOS generation, opposite to what was observed in our study.
Plasma amino acid concentrations were grossly not different between diabetic and control subjects (Table 2), and they were roughly suppressed to the same extent in both groups, with the exception of taurine (greater in the diabetic group) and asparagine and threonine (lower in the patients). None of these amino acids are known to modulate NOx metabolism. Plasma taurine concentrations may be increased in insulin-resistant states (41). Asparagine was found to be increased in type 2 diabetic patients, contrary to our findings (42). The reasons for these discrepancies are unknown, possibly depending on the patients' specific characteristics. To our knowledge, no data on plasma threonine concentrations in response to insulin are available. On the other hand, total, branched-chain, and most other amino acid plasma concentrations were not significantly different between the groups. Therefore, plasma amino acid levels should not be related to any of the basic findings on NOx metabolism of our study.
In conclusion, whole-blood NOx production from arginine, and its response to insulin, are decreased in type 2 diabetes with nephropathy, likely representing an additional feature of insulin resistance. Such a defect can be responsible for the decreased NOx concentration and the altered vascular responses found in type 2 diabetes, and it can be linked to the pathophysiology of diabetic nephropathy.
Acknowledgments
This study was supported by a 2001 FIRB Grant of the Italian Ministero dell'Università e della Ricerca Scientifica and by a research grant (“Assegno di ricerca”) from the University of Padova (“Development and application of a new method to measure nitric oxide synthesis in humans”), 2002.
No potential conflicts of interest relevant to this article were reported.
P.T. researched data, performed the studies, and wrote the manuscript. D.C., A.Cos., M.V., and A.Cor. performed the studies. R.M. and L.P. researched data and reviewed/edited the manuscript. E.I. performed the studies and contributed to discussion. A.A. researched data and contributed to discussion. M.V. performed the studies, contributed to discussion, and reviewed/edited the manuscript.
We acknowledge Dr. Daniela Vianello, from the Department of Medical and Surgical Sciences, University of Padova, for NOx blood measurements, and Dr. Maria Cristina Marescotti, from the Department of Clinical and Experimental Medicine, University of Padova, for cytokine measurements.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Moncada S, Higgs A. The L-arginine-nitric oxide pathway. N Engl J Med 1993;329:2002–2012 [DOI] [PubMed] [Google Scholar]
- 2.Kleinbongard P, Keymel S, Kelm M. New functional aspects of the L-arginine-nitric oxide metabolism within the circulating blood. Thromb Haemost 2007;98:970–974 [PubMed] [Google Scholar]
- 3.Muniyappa R, Quon MJ. Insulin action and insulin resistance in vascular endothelium. Curr Opin Clin Nutr Metab Care 2007;10:523–530 [DOI] [PubMed] [Google Scholar]
- 4.Ware JA, Heistad DD. Seminars in medicine of the Beth Israel Hospital, Boston. Platelet-endothelium interactions. N Engl J Med 1993;328:628–635 [DOI] [PubMed] [Google Scholar]
- 5.Vincent MA, Montagnani M, Quon MJ. Molecular and physiologic actions of insulin related to production of nitric oxide in vascular endothelium. Curr Diab Rep 2003;3:279–288 [DOI] [PubMed] [Google Scholar]
- 6.Antunes F, Boveris A, Cadenas E. On the mechanism and biology of cytochrome oxidase inhibition by nitric oxide. Proc Natl Acad Sci U S A 2004;101:16774–16779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Honing ML, Morrison PJ, Banga ES, Rabelink TJ. Nitric oxide availability in diabetes mellitus. Diabetes Metab Rev 1998;14:241–249 [DOI] [PubMed] [Google Scholar]
- 8.Vanizor B, Orem A, Karahan SC, Kiran E, Erem C, Aliyazicioğlu R, Uydu HA. Decreased nitric oxide end-products and its relationship with high density lipoprotein and oxidative stress in people with type 2 diabetes without complications. Diabetes Res Clin Pract 2001;54:33–39 [DOI] [PubMed] [Google Scholar]
- 9.Watkins CC, Sawa A, Jaffrey S, Blackshaw S, Barrow RK, Snyder SH, Ferris CD. Insulin restores neuronal nitric oxide synthase expression and function that is lost in diabetic gastropathy. J Clin Invest 2000;106:373–384; Erratum in J Clin Invest 2000;106:803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Avogaro A, Toffolo G, Kiwanuka E, de Kreutzenberg SV, Tessari P, Cobelli C. L-arginine-nitric oxide kinetics in normal and type 2 diabetic subjects: a stable-labelled 15N arginine approach. Diabetes 2003;52:795–802 [DOI] [PubMed] [Google Scholar]
- 11.Goligorsky MS, Chen J, Brodsky S. Workshop: endothelial cell dysfunction leading to diabetic nephropathy: focus on nitric oxide. Hypertension 2001;37:744–748 [DOI] [PubMed] [Google Scholar]
- 12.Earle KA, Mehrotra S, Dalton RN, Denver E, Swaminathan R. Defective nitric oxide production and functional renal reserve in patients with type 2 diabetes who have microalbuminuria of African and Asian compared with white origin. J Am Soc Nephrol 2001;12:2125–2130 [DOI] [PubMed] [Google Scholar]
- 13.Prabhakar S, Starnes J, Shi S, Lonis B, Tran R. Diabetic nephropathy is associated with oxidative stress and decreased renal nitric oxide production. J Am Soc Nephrol 2007;18:2945–2452 [DOI] [PubMed] [Google Scholar]
- 14.Stehouver CD, Henry RM, Dekker JM, Nijpels G, Heine RJ, Bouter LM. Microalbuminuria is associated with impaired endothelium dependent, flow mediated vasodilation in elderly individuals without and with diabetes: further evidence for a link between microalbuminuria and endothelial dysfunction-the Hoorn Study. Kidney Int 2004;92:S42–S44 [DOI] [PubMed] [Google Scholar]
- 15.Chu S, Bohlen HG. High concentration of glucose inhibits glomerular endothelial eNOS through a PKC mechanism. Am J Physiol Renal Physiol 2004;287:F384–F392 [DOI] [PubMed] [Google Scholar]
- 16.Baylis C. Arginine, arginine analogs and nitric oxide production in chronic kidney disease. Nat Clin Pract Nephrol 2006;2:209–220 Review [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maejima K, Nakano S, Himeno M, Tsuda S, Makiishi H, Ito T, Nakagawa A, Kigoshi T, Ishibashi T, Nishio M, Uchida K. Increased basal levels of plasma nitric oxide in type 2 diabetic subjects. Relationship to microvascular complications. J Diabetes Complications 2001;15:135–143 [DOI] [PubMed] [Google Scholar]
- 18.Zahedi AS, Ghasemi A, Azizi F. Serum nitric oxide metabolites in subjects with metabolic syndrome. Clin Biochem 2008;41:1342–1347 [DOI] [PubMed] [Google Scholar]
- 19.Kashyap SR, Roman LJ, Lamont J, Masters BS, Bajaj M, Suraamornkul S, Belfort R, Berria R, Kellogg DL, Jr, Liu Y, DeFronzo RA. Insulin resistance is associated with impaired nitric oxide synthase activity in skeletal muscle of type 2 diabetic subjects. J Clin Endocrinol Metab 2005;90:1100–1105 [DOI] [PubMed] [Google Scholar]
- 20.Tessari P, Coracina A, Puricelli L, Vettore M, Cosma A, Millioni R, Cecchet D, Avogaro A, Tiengo A, Kiwanuka E. Acute effect of insulin on nitric oxide synthesis in humans: a precursor–product isotopic study. Am J Physiol Endocrinol Metab 2007;293:E776–E782 [DOI] [PubMed] [Google Scholar]
- 21.Miles DW, Mogensen CE, Gundersen HJ. Renal inulin clearance versus total plasma clearance of 51Cr-EDTA. Scand J Clin Lab Invest 1969;26:5–11 [DOI] [PubMed] [Google Scholar]
- 22.Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron 1976;16:31–41 [DOI] [PubMed] [Google Scholar]
- 23.Wolfe RR. Principles and practice of kinetics analysis. In Radioactive and Stable Isotope Tracers in Biomedicine. New York, Wiley-Liss, 1992, p. 62–70 [Google Scholar]
- 24.Green LC, Wagner DA, Glogowski J, Skipper PL, Wishnok JS, Tannenbaum SR. Analysis of nitrate, nitrite, and [15N]nitrate in biological fluids. Anal Biochem 1982;126:131–138 [DOI] [PubMed] [Google Scholar]
- 25.Ellis G, Adatia I, Yazdanpanah M, Makela SK. Nitrite and nitrate analyses: a clinical biochemistry perspective. Clin Biochem 1998;31:195–220 [DOI] [PubMed] [Google Scholar]
- 26.Jungersten L, Edlund A, Petersson AS, Wennmalm A. Plasma nitrate as an index of nitric oxide formation in man: analyses of kinetics and confounding factors. Clin Physiol 1996;16:369–379 [DOI] [PubMed] [Google Scholar]
- 27.Laakso M, Edelman SV, Brechtel G, Baron AD. Impaired insulin-mediated skeletal muscle blood flow in patients with NIDDM. Diabetes 1992;41:1076–1083 [DOI] [PubMed] [Google Scholar]
- 28.Zeng G, Quon MJ. Insulin-stimulated production of nitric oxide is inhibited by wortmannin. Direct measurement in vascular endothelial cells. J Clin Invest 1996;98:894–898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hsueh WA, Law RE. Insulin signaling in the arterial wall. Am J Cardiol 1999;84:21J–24J [DOI] [PubMed] [Google Scholar]
- 30.Hamilton SJ, Chew GT, Watts GF. Therapeutic regulation of endothelial dysfunction in type 2 diabetes mellitus. Diab Vasc Dis Res 2007;4:89–102 [DOI] [PubMed] [Google Scholar]
- 31.Morawietz H, Rohrbach S, Rueckschloss U, Schellenberger E, Hakim K, Zerkowski HR, Kojda G, Darmer D, Holtz J. Increased cardiac endothelial nitric oxide synthase expression in patients taking angiotensin-converting enzyme inhibitor therapy. Eur J Clin Invest 2006;36:705–712 [DOI] [PubMed] [Google Scholar]
- 32.Satoh M, Fujimoto S, Arakawa S, Yada T, Namikoshi T, Haruna Y, Horike H, Sasaki T, Kashihara N. Angiotensin II type 1 receptor blocker ameliorates uncoupled endothelial nitric oxide synthase in rats with experimental diabetic nephropathy. Nephrol Dial Transplant 2008;23:3806–3813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhou MS, Schuman IH, Jaimes EA, Raij L. Renoprotection by statins is linked to a decrease in renal oxidative stress, TGF-beta, and fibronectin with concomitant increase in nitric oxide bioavailability Am J Physiol Renal Physiol 2008;295:F53–F59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ferrannini E, Haffner SM, Stern MP. Essential hypertension: an insulin-resistant state. J Cardiovasc Pharmacol 1990;5(Suppl 15):S18–25 [PubMed] [Google Scholar]
- 35.Gurley SB, Coffman TM. The renin-angiotensin system and diabetic nephropathy. Semin Nephrol 2007;27:144–152 [DOI] [PubMed] [Google Scholar]
- 36.Kapur S, Bédard S, Marcotte B, Côté CH, Marette A. Expression of nitric oxide synthase in skeletal muscle: a novel role for nitric oxide as a modulator of insulin action. Diabetes 1997;46:1691–1700 [DOI] [PubMed] [Google Scholar]
- 37.Andersen K, Pedersen BK. The role of inflammation in vascular insulin resistance with focus on IL-6. Horm Metab Res 2008;40:635–639 [DOI] [PubMed] [Google Scholar]
- 38.Andreozzi F, Laratta E, Procopio C, Hribal ML, Sciacqua A, Perticone M, Miele C, Perticone F, Sesti G. Interleukin-6 impairs the insulin signaling pathway, promoting production of nitric oxide in human umbilical vein endothelial cells. Mol Cell Biol 2007;27:2372–2383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Navarro-González JF, Mora-Fernández C. The role of inflammatory cytokines in diabetic nephropathy. J Am Soc Nephrol 2008;19:433–442 [DOI] [PubMed] [Google Scholar]
- 40.Nathan C, Xie QW. Regulation of biosynthesis of nitric oxide. J Biol Chem 1994;269:13725–13728 [PubMed] [Google Scholar]
- 41.Wijekoon EP, Skinner C, Brosnan ME, Brosnan JT. Amino acid metabolism in the Zucker diabetic fatty rat: effects of insulin resistance and of type 2 diabetes. Can J Physiol Pharmacol 2004;82:506–514 [DOI] [PubMed] [Google Scholar]
- 42.Marchetti P, Masiello P, Benzi L, Cecchetti P, Fierabracci V, Giannarelli R, Gregorio F, Brunetti P, Navalesi R. Effects of metformin therapy on plasma amino acid pattern in patients with maturity-onset diabetes. Drugs Exp Clin Res 1989:15:565–570 [PubMed] [Google Scholar]