Abstract
Poor mental health accounts for considerable disease burden among young people globally. We investigated the prevalence and determinants of affective disorders among rural Zimbabwean youth in 2006. We undertook a cross-sectional survey among 1495 Zimbabwean youth aged 15–23 (median 18) from 12 rural communities in three provinces in south-eastern Zimbabwe. Mental health was assessed using the Shona Symptom Questionnaire (SSQ), a locally validated 14-item indigenous screening tool for affective disorders, notably depression and anxiety disorders. Participants scoring ≥8/14 were considered at risk of being affected and ≥11 as at risk of being severely affected. Most participants (93.1%) completed the SSQ. Of these, 51.7% (95%CI:49.0–54.3%) scored ≥8/14 and 23.8% (95%CI:21.5–26.0%) scored ≥11. Affective disorders were independently associated with household poverty (adjusted odds ratio (AOR) 1.9, 95%CI:1.4–2.7), living in a female-headed household (AOR 1.3, 95%CI:1.0–1.7), having moved home within last 5 years (AOR 1.4, 95%CI:1.0–1.9) and feeling stigmatized (AOR being shunned by others 3.7, 95%CI:2.5–5.7). There was a strong linear association between risk of affective disorders and sexual risk taking (ever sex AOR 1.5, 95%CI:1.0–2.4, and 2.8, 95%CI:1.9–4.2 for affected and severely affected, respectively, test for trend P < 0.001; ≥2 lifetime partners AOR 2.3, 95%CI:1.1–4.8 and 5.4, 95%CI:2.7–10.7, test for trend P < 0.001). This study indicates high levels of psychological morbidity among rural Zimbabwean youth which was associated with sexual risk taking. Interventions to prevent, identify and treat mental health disorders in this vulnerable population are urgently required. In HIV-endemic countries, such interventions may also help reduce HIV transmission.
Keywords: Adolescence, Mental health, Sexual behavior, HIV seroprevalence, Zimbabwe
Introduction
It is estimated that around 450 million people suffer from mental or behavioral disorders worldwide and that one in four people will become mentally unwell at some time during their lives [1]. Many first become unwell when they are young, although their illness often goes unrecognised until later life. Despite this lack of recognition, affective disorders such as depression and anxiety, still account for a large proportion of the disease burden in young people in all societies [2]. The causes are multi-factorial and include biological, social and psychological factors. In East and Southern Africa, where HIV infection is endemic, young people face particular challenges, with high rates of orphaning and exposure to illness and death of family members. Rural to urban migration is common, often leading to disintegration of the extended family. Poverty is widespread [3]. In addition to the indirect effects of HIV on mental health, HIV is itself a direct cause of anxiety and depression [2]. Half of new HIV infections now occur in 15–24 year olds with young women bearing the brunt of early infection [4]. In addition to the cost of psychological morbidity per se, affective disorders in young people are strongly associated with other health and social problems including low educational attainment, unemployment, alcohol and drug abuse, violence, sexual abuse and poor sexual and reproductive health [5]. Where HIV is endemic, poor sexual health translates to an increased risk of acquiring (and subsequently transmitting) HIV.
Evidence of the prevalence of affective disorders remains poor in developing countries. The Regai Dzive Shiri Trial was a community randomized trial of a multi-component adolescent reproductive health intervention being conducted in 30 rural communities in south-east Zimbabwe. The trial measured the impact of the intervention on the prevalence of HIV, HSV-2 and unintended pregnancy among young people living in these communities. Baseline data for this trial were collected in 2003 from young people enrolled in their second year of secondary schools [6]. Of these pupils, 35.0% (95%CI: 33.9–36.2) reported that they had lost one or both parents. Orphans were at greatly increased risk of HIV compared to non-orphans (age-sex adjusted odds ratio (OR) 3.4; 95%CI: 1.9–6.1) [7]. Data collected subsequently from 60 trial participants through in-depth qualitative interviews suggested that orphaning was associated with having had to move from one family member’s household to another in the past 5 years and stigma. During these interviews, participants also expressed feelings of depression and anxiety about the future. We therefore expanded the objectives of the interim survey for the trial to explore factors associated with HIV vulnerability more broadly, including its association with mental health. In this paper we report on the mental health burden of young people in rural Zimbabwe as measured in the interim trial survey.
Methods
Study Population
In 2003, the Regai Dzive Shiri baseline survey was conducted in 30 rural communities in seven districts in three provinces in rural Zimbabwe (Masvingo, Manicaland and Mashonaland East). Eighty-six percent (n = 6791) of Form 2 pupils (in their second year of secondary school following 7 years of primary schooling) attending 82 secondary schools in the trial communities took part. In 2006, the interim survey, within which this study was nested, was conducted in 12 of the 30 study communities, selected by restricted randomization to ensure balance between intervention and control arms of the trial and between the three provinces. Survey participants were eligible if they were cohort members who had participated in the baseline survey and were currently residing in these communities.
Data Collection
Following written informed consent, interim survey participants were asked to self-complete a questionnaire in Shona (the indigenous language), which collected detailed demographic, economic, behavioral and mental health information using the Shona Symptom Questionnaire (SSQ). The SSQ, a locally validated, 14-item, indigenous measure used to screen for those at risk of affective disorders, including depressive and generalized anxiety disorders, was included in this questionnaire [8–11]. The SSQ was developed and validated among patients attending primary care clinics and traditional medical practitioners in Harare and combines elements that reflect both the concerns of the health care provider (includes items from WHO Self-Report Questionnaire) and those that are socio-culturally meaningful to the patient [12]. The aim of the SSQ is to measure psychiatric morbidity. Participants were asked to respond to whether or not they felt that each of the 14 statements applied to them ‘always’, ‘sometimes’ or ‘never’ during the previous week. The SSQ was originally validated against a gold standard that required diagnosis of a mental disorder by a health care worker and a score of 12 or more on the Revised Clinical Interview Schedule (CISR) [8]. Compared with this gold standard, the sensitivity and specificity of the SSQ, using a cut-off of ≥8 of 14 items, were 63% and 83%, respectively.
Focus group discussions were held with community members to formulate culturally-appropriate questions to measure stigma. Issues included terminology that identified individuals as inanimate objects, increased household chores compared with peers, and being given second-hand rather than new clothes.
Trial participants were also asked to provide a finger-prick blood sample which was tested for antibodies to HIV using a validated HIV testing algorithm [13] (two ELISAs with western blot for discrepant results). Young women were each asked to provide a urine sample, which was tested on site for pregnancy using the Cortez OneStep hCG Rapidip InstaTest®.
Statistical Methods
Data were entered into an MS Access database and range and consistency checks carried out. Statistical analyses were performed using Stata 9.2 (College Station, TX).
The internal consistency of the SSQ scale was assessed by calculating the intra-class correlation coefficient (Cronbach’s alpha) to ensure that the SSQ psychometric properties in this population-based sample were as expected from its use in other settings. High internal consistency is traditionally defined as alpha >0.7. Cronbach’s alpha was maximal when all 14 items from the scale were included (∝ = 0.83), suggesting that the instrument items are measuring the same underlying construct (mood). Only participants who completed all 14 items were assessed. Previously validated cutoffs were used; participants who answered affirmatively (‘always’ or ‘sometimes’) to ≥8 of the 14 statements were defined as ‘at risk of being affected’, and those scoring ≥11 were defined as ‘at risk of being severely affected’ [8].
Factors associated with affective disorders were examined on univariate analysis. Categorical data were analysed using chi-square tests, and logistic regression was used to determine unadjusted odds ratios. Continuous data were categorized where appropriate.
Factors that were significantly associated with affective disorders on univariate analysis (P < 0.10) and other variables where existing knowledge provided evidence for inclusion were included in a multivariate model adjusted for a priori confounders (age, gender, education, marital status and district) and for each other. Variables that were not independently associated with affective disorders after adjustment (P > 0.10) were excluded from the model. The same analysis was repeated to identify risk factors for severely affected participants (score of 11 or more on SSQ scale).
The association between affective disorders and sexual and other risk behaviors were explored on univariate and multivariate analysis adjusting for a priori confounders as previously defined. Specifically the odds of various risk behaviors were calculated by severity of risk of affective disorder (SSQ < 8, SSQ = 8–10, SSQ ≥ 11), and tests for trend were used to assess possible linear associations between risk of severity and these behaviors.
Ethics Approval
Ethical approval was obtained from the Medical Research Council of Zimbabwe and the ethics committees of University College London and the London School of Hygiene and Tropical Medicine.
Results
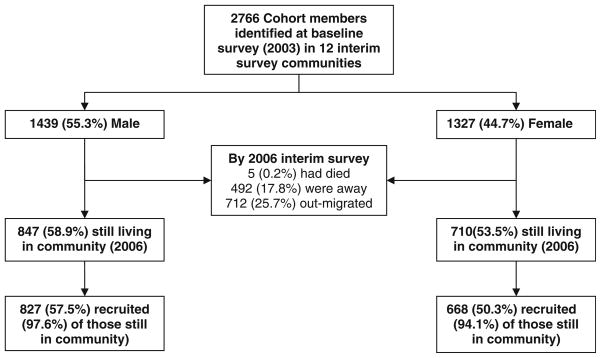
Of 1,557 cohort participants still living in the study communities, 1,495 (96%) took part in the interim survey (Fig. 1). When baseline survey characteristics were compared between participants and non-participants, interim survey participants were more likely than non-participants to be male (55% vs 48%; P < 0.001) and were younger (26% < 15 years vs 20%; P < 0.001) and less likely to be orphaned (64% vs 66% P = 0.016) but were no more or less likely to be sexually active (P = 0.088).
Fig. 1.
Flow chart showing participation in interim survey
General Characteristics of Interim Survey Participants
Overall, 45% of participants were female (Table 1). Participants were aged between 15 and 23 years (mean 18.2 years), 4.3% (95%CI: 3.3–5.3%) were married (7.6% of females and 1.6% of males) and 87% (95%CI: 84.8–88.3%) had completed Year 4 of secondary school. Overall 40% (95%CI: 37.5–42.6%) reported that they had lost one or both parents. Poverty assessed using a variety of measures, was widespread. For example 20% (95%CI: 18.2–22.3%) of participants reported that an adult in their home had skipped a meal in the previous week in order for there to be enough food for children in their household.
Table 1.
Characteristics of interim survey participants (n = 1495; 827 male, 668 female)
| Characteristic | Male |
Female |
Total |
|||
|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | |
| Demographic and household | ||||||
| Age | ||||||
| Less than 18 years | 162 | (19.6) | 225 | (33.7) | 387 | (25.9) |
| 18 years old | 269 | (32.5) | 279 | (41.8) | 548 | (36.7) |
| 19 years old | 247 | (29.9) | 132 | (19.8) | 379 | (23.4) |
| 20 years old or more | 149 | (18.0) | 32 | (4.8) | 181 | (12.1) |
| Ever been married | 13 | (1.6) | 50 | (7.6) | 63 | (4.3) |
| Completed Form 4 | 721 | (88.8) | 556 | (83.9) | 1,277 | (86.7) |
| Still in school | 170 | (20.6) | 88 | (13.2) | 258 | (17.3) |
| Orphanhood | ||||||
| Both parents alive | 469 | (59.7) | 390 | (60.3) | 859 | (60.0) |
| Maternal orphan | 60 | (7.6) | 39 | (6.0) | 99 | (6.9) |
| Paternal orphan | 164 | (20.9) | 152 | (23.5) | 316 | (22.1) |
| Both parents dead | 92 | (11.7) | 66 | (10.2) | 158 | (11.0) |
| Moved in the last 5 years | 163 | (20.1) | 179 | (27.2) | 342 | (23.3) |
| Female headed household | 239 | (30.5) | 254 | (40.0) | 493 | (34.7) |
| Socio-economic status and poverty | ||||||
| House made of poles and mud or mud bricks | 756 | (92.4) | 586 | (88.4) | 1,342 | (90.6) |
| Grass roof | 286 | (35.2) | 181 | (27.3) | 467 | (31.6) |
| Cannot afford washing soap | 181 | (21.9) | 129 | (19.3) | 310 | (20.7) |
| Absent from school no money for fees | 470 | (56.8) | 354 | (53.0) | 824 | (55.1) |
| Gone day without food in last week | 172 | (21.1) | 102 | (15.5) | 274 | (18.6) |
| Adult skipped a meal in the last week | 173 | (21.3) | 124 | (18.9) | 297 | (20.3) |
| Reported sexual behaviour | ||||||
| Age of first sex | ||||||
| Never had sex | 688 | (87.1) | 579 | (88.8) | 1,267 | (87.8) |
| 15 years and under | 26 | (3.3) | 11 | (1.7) | 37 | (2.6) |
| 16 years and older | 76 | (9.6) | 62 | (9.5) | 138 | (9.6) |
| ≥2 lifetime partners (of those who reported having had sex) | 49 | (48.5) | 13 | (18.6) | 62 | (36.3) |
| Biomarkers (with [95%CI]) | ||||||
| HIV prevalence | 3 | (0.4) [0.0–0.8] | 15 | (2.2) [1.1–3.4] | 18 | (1.2) [0.6–1.8] |
| Pregnant | N/A | 16 | (2.4) [1.2–3.6] | |||
HIV prevalence was 2.2% in young women (95%CI: 1.1–3.4%) and 0.4% (95%CI: 0.0–0.8%) in young men. Overall 2.4% (n = 16; 95%CI: 1.2–3.6%) of the young women were pregnant; 12.5% of young women reported being sexually active compared with 15.4% of young men (P = 0.12).
Mental Health
Response rates for completion of the mental health scale were high; 93.1% of survey participants completed all 14 items while only 1.7% (n = 26; 18 males; 8 females) did not complete any. Of those who completed the scale, 51.7% (95%CI 49.0–54.3%) scored ≥ 8 on the SSQ and were considered at risk of affective disorders; 23.8% (95%CI: 21.5–26.0%) were classified as at risk of severe affective disorders (scoring ≥ 11). Table 2 shows the responses to each item on the SSQ scale by gender. Of note, 10.1% of participants (95%CI: 8.6–11.7%) reported that they had felt like committing suicide either sometimes or always within the previous week (males = 8.5%, females = 12.1%, P = 0.023), with 1.2% (95%CI: 0.6–1.7) reporting that they had ‘always’ felt like committing suicide in the previous week.
Table 2.
Shona symptom questionnaire (SSQ): item response rates by gender and overall response
| Shona symptom questionnaire items | Males |
Females |
||||||
|---|---|---|---|---|---|---|---|---|
| N | Always | Sometimes | Never | N | Always | Sometimes | Never | |
| There were times in which I was thinking deeply or thinking about many things (thinking too much). | 801 | 11.9% | 66.5% | 21.6% | 653 | 11.6% | 64.9% | 23.4% |
| I found myself sometimes failing to concentrate | 800 | 6.3% | 60.3% | 33.5% | 653 | 5.1% | 61.6% | 33.4% |
| I lost my temper or got annoyed over trivial matters | 796 | 2.0% | 59.4% | 38.6% | 649 | 4.9% | 56.9% | 38.2% |
| I had nightmares or bad dreams | 801 | 3.9% | 62.8% | 33.3% | 653 | 5.8% | 68.2% | 26.0% |
| I sometimes saw or heard things which others could not see or hear | 801 | 1.4% | 26.6% | 72.0% | 651 | 2.8% | 21.5% | 75.7% |
| My stomach was aching | 801 | 4.9% | 51.8% | 43.3% | 651 | 3.8% | 60.1% | 36.1% |
| I was frightened by trivial things | 802 | 3.0% | 39.9% | 57.1% | 653 | 2.6% | 40.6% | 56.8% |
| I sometimes failed to sleep or lost sleep | 802 | 3.6% | 49.1% | 47.3% | 653 | 2.6% | 46.9% | 50.5% |
| There were moments when I felt life was so tough that I cried or wanted to cry | 804 | 7.5% | 53.4% | 39.2% | 654 | 8.0% | 54.3% | 37.8% |
| I felt run down (tired) | 789 | 3.4% | 64.1% | 32.5% | 645 | 1.6% | 63.7% | 34.7% |
| At times I felt like committing suicide | 802 | 0.9% | 7.6% | 91.5% | 653 | 1.5% | 10.6% | 87.9% |
| I was generally unhappy with things that I would be doing each day | 801 | 2.4% | 48.8% | 48.8% | 650 | 3.5% | 41.5% | 54.9% |
| My work was lagging behind (impairment of functioning) | 802 | 5.2% | 44.3% | 50.5% | 650 | 5.1% | 35.9% | 59.1% |
| I felt I had problems in deciding what to do | 802 | 5.5% | 50.3% | 44.3% | 654 | 4.9% | 47.6% | 47.6% |
| SSQ scores | ||||||||
| Completed all 14 items | 768 | 92.9% | 624 | 93.4% | ||||
| Scored 8 or more (at risk of being affected) | 399 | 51.9% | [95%CI: 48.4–55.5%] | 320 | 51.3% | [95%CI: 47.3–55.2%] | ||
| Scored 11 or more (at risk of being severely affected) | 188 | 24.5% | [95%CI: 21.4–27.5%] | 143 | 22.9% | [95%CI: 19.6–26.2%] | ||
Factors Associated with Being at Risk of Affective Disorders
The factors associated with being at risk of affective disorders are shown in Table 3. There was no significant difference in prevalence by age (P = 0.146), gender (P = 0.803), marital status (P = 0.143) or level of education (P = 0.066) but there were significant differences in prevalence by district (P < 0.001) with the poorest district (Buhera) having the highest rates of risk for affective disorders.
Table 3.
Risk factors for being at risk of being affected (SSQ score ≥ 8) and at risk of being severely affected (SSQ score ≥ 11) (n = 1392 completing all 14 items)
| Factor | N | At risk of being affected (SSQ score = 8–14) |
At risk of being severely affected (SSQ score = 11–14) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | Crude† OR [95%CI] | Adjustedb OR [95%CI] | n | % | Crude† OR [95%CI] | Adjustedb OR [95%CI] | ||
| Age: | (P = 0.146) | (P = 0.217) | (P = 0.002)* | (P = 0.089) | |||||
| Less than 18 years | 367 | 172 | 46.9 | 1.0 | 1.0 | 61 | 16.6 | 1.0 | 1.0 |
| 18 years old | 515 | 282 | 54.8 | 1.4 [1.0–1.8] | 1.3 [0.9–1.8] | 136 | 26.4 | 1.8 [1.3–2.5] | 1.6 [1.1–2.3] |
| 19 years old | 350 | 182 | 52.0 | 1.2 [0.9–1.6] | 1.0 [0.7–1.4] | 94 | 26.9 | 1.8 [1.3–2.6] | 1.4 [1.0–2.2] |
| 20 years or older | 160 | 160 | 51.9 | 1.2 [0.8–1.8] | 0.8 [0.5–1.4] | 40 | 25.0 | 1.7 [1.1–2.6] | 1.1 [0.6–2.0] |
| Gender: | (P = 0.803) | (P = 0.270) | (P = 0.496) | (P = 0.368) | |||||
| Male | 768 | 399 | 52 | 1.0 | 1.0 | 188 | 24.5 | 1.0 | 1.0 |
| Female | 624 | 320 | 51.3 | 1.0 [0.8–1.2] | 0.9 [0.6–1.1] | 143 | 22.9 | 0.9 [0.7–1.2] | 0.9 [0.6–1.2] |
| Secondary education:a | (P = 0.065) | (P = 0.414) | (P = 0.617) | (P = 0.834) | |||||
| Years 2–3 | 183 | 106 | 57.9 | 1.0 | 1.0 | 46 | 25.1 | 1.0 | 1.0 |
| Completed year 4 or higher | 1203 | 609 | 50.6 | 0.7 [0.5–1.0] | 0.8 [0.6–1.3] | 282 | 23.4 | 0.9 [0.6–1.3] | 1.0 [0.7–1.7] |
| Marital status: | (P = 0.141) | (P = 0.900) | (P = 0.176) | (P = 0.904) | |||||
| Never married | 1322 | 681 | 51.5 | 1.0 | 1.0 | 311 | 23.5 | 1.0 | 1.0 |
| Currently/have been married | 57 | 35 | 61.4 | 1.5 [0.9–2.6] | 1.0 [0.4–2.1] | 18 | 31.6 | 1.5 [0.8–2.7] | 0.9 [0.4–2.2] |
| District: | (P < 0.001)* | (P = 0.018)* | (P = 0.075) | (P = 0.672) | |||||
| Mashonaland East—Chikomba | 216 | 112 | 51.9 | 1.0 | 1.0 | 57 | 26.4 | 1.0 | 1.0 |
| Manicaland—Buhera | 282 | 178 | 63.1 | 1.6 [1.1–2.3] | 1.6 [1.0–2.4] | 82 | 29.1 | 1.1 [0.8–1.7] | 1.2 [0.7–1.9] |
| Manicaland—Makoni | 148 | 83 | 56.1 | 1.2 [0.8–1.8] | 1.5 [0.9–2.4] | 37 | 25.0 | 0.9 [0.6–1.5] | 1.0 [0.6–1.7] |
| Masvingo—Gutu | 117 | 59 | 50.4 | 0.9 [0.6–1.5] | 1.3 [0.7–2.2] | 25 | 21.4 | 0.8 [0.4–1.3] | 1.0 [0.5–1.9] |
| Masvingo—Zaka | 458 | 201 | 43.9 | 0.7 [0.5–1.0] | 0.8 [0.6–1.3] | 90 | 19.7 | 0.7 [0.5–1.0] | 0.8 [0.5–1.3] |
| Masvingo—Masvingo rural | 171 | 86 | 50.3 | 0.9 [0.6–1.4] | 1.2 [0.7–1.9] | 40 | 23.4 | 0.9 [0.5–1.4] | 1.1 [0.6–1.9] |
| Household, mobility and SES: | |||||||||
| Orphanhood: | (P = 0.056) | (P = 0.522) | (P = 0.288) | (P = 0.371) | |||||
| Both parents alive | 803 | 398 | 49.6 | 1.0 | 1.0 | 181 | 22.5 | 1.0 | 1.0 |
| One or both parents dead | 547 | 300 | 54.8 | 1.2 [1.0–1.5] | 1.1 [0.8–1.5] | 137 | 25.1 | 1.1 [0.9–1.5] | 0.8 [0.6–1.2] |
| Female headed household: | (P = 0.038)* | (P = 0.074) | (P = 0.045)* | (P = 0.048)* | |||||
| No | 874 | 433 | 49.5 | 1.0 | 1.0 | 191 | 21.9 | 1.0 | 1.0 |
| Yes | 463 | 257 | 55.5 | 1.3 [1.0–1.6] | 1.3 [1.0–1.7] | 124 | 26.8 | 1.3 [1.0–1.7] | 1.4 [1.0–1.8] |
| Moved in last 5 years: | (P < 0.001)* | (P = 0.034)* | (P = 0.002)* | (P = 0.031)* | |||||
| No | 1060 | 515 | 48.6 | 1.0 | 1.0 | 230 | 21.7 | 1.0 | 1.0 |
| Yes | 320 | 195 | 60.9 | 1.7 [1.3–2.1] | 1.4 [1.0–1.9] | 97 | 30.3 | 1.6 [1.2–2.1] | 1.4 [1.0–2.0] |
| Adult skipped a meal in last week: | (P < 0.001)* | (P < 0.001)* | (P < 0.001)* | (P = 0.055) | |||||
| No | 1103 | 523 | 47.4 | 1.0 | 1.0 | 229 | 20.8 | 1.0 | 1.0 |
| Yes | 275 | 192 | 69.8 | 2.6 [1.9–3.4] | 1.9 [1.4–2.7] | 100 | 36.4 | 2.2 [1.6–2.9] | 1.4 [1.0–2.0] |
| Ability to afford soap: | (P < 0.001)* | (P = 0.115) | (P < 0.001)* | (P = 0.727) | |||||
| Can afford soap | 1131 | 548 | 48.5 | 1.0 | 1.0 | 250 | 22.1 | 1.0 | 1.0 |
| Cannot afford soap | 261 | 171 | 65.5 | 2.0 [1.5–2.7] | 1.3 [0.9–1.9] | 81 | 31 | 1.6 [1.2–2.1] | 0.9 [0.6–1.4] |
Chi–square P-value presented from univariate analysis
As cohort members all participants had completed at least Year 2 of secondary school
OR adjusted for a priori confounders (age, gender, marital status, education, district) and all factors independently associated with being at risk or severely at risk for common affected disorder (Likelihood ratton test P-value < 0.1) (i.e. Female headed house, moved house, skipped a meal, referred to in negative way, shunned by others, given more work, not given clothes)
P < 0.05
Other factors that remained independently associated with risk for affective disorders after adjusting for confounding variables were poverty, living in a female-headed household and having had to move from one household to another at least once in the last 5 years (Table 3).
Participants at risk of affective disorders were more likely to report feeling stigmatised than those who were not at risk on both univariate and multivariate analysis (Table 4).
Table 4.
Association between stigma and being at risk (SSQ score ≥ 8) or severely at risk (SSQ score ≥ 11) of being affected (n = 1392 completing all 14 items)
| N | At risk of being affected (SSQ score = 8–14) |
At risk of being severely affected (SSQ score = 11–14) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | Crude† OR [95%CI] | Adjusteda OR [95%CI] | n | % | Crude† OR [95%CI] | Adjusteda OR [95%CI] | ||
| Sigma | |||||||||
| Referred to in negative way: | (P < 0.001)* | (P < 0.001)* | (P <0.001)* | (P < 0.001)* | |||||
| Never | 641 | 199 | 31.1 | 1.0 | 1.0 | 59 | 9.2 | 1.0 | 1.0 |
| Sometimes/always | 747 | 519 | 69.5 | 5.0 [4.0–6.4] | 3.5 [2.7–4.5] | 271 | 36.3 | 5.6 [4.1–7.6] | 3.6 [2.6–5.0] |
| Shunned by others: | (P < 0.001)* | (P < 0.001)* | (P <0.001)* | (P < 0.001)* | |||||
| Never | 1108 | 484 | 43.7 | 1.0 | 1.0 | 196 | 17.7 | 1.0 | 1.0 |
| Sometimes/always | 276 | 230 | 83.3 | 6.4 [4.6–9.0] | 3.7 [2.5–5.4] | 133 | 48.2 | 4.3 [3.2–5.7] | 2.3 [1.7–3.2] |
| Given more work than others in house: | (P < 0.001)* | (P = 0.028)* | (P <0.001)* | (P = 0.003)* | |||||
| Never | 1010 | 451 | 44.7 | 1.0 | 1.0 | 174 | 17.2 | 1.0 | 1.0 |
| Sometimes/always | 375 | 264 | 70.4 | 2.9 [2.3–3.8] | 1.4 [1.0–1.9] | 155 | 41.3 | 3.4 [2.6–4.4] | 1.6 [1.2–2.2] |
| Not given clothes like others in house: | (P < 0.001)* | (P < 0.001)* | (P <0.001)* | (P < 0.001)* | |||||
| Never | 865 | 358 | 41.4 | 1.0 | 1.0 | 129 | 14.9 | 1.0 | 1.0 |
| Sometimes/always | 521 | 359 | 68.9 | 3.1 [2.3–3.8] | 2.0 [1.6–2.7] | 200 | 38.4 | 3.6 [2.7–4.6] | 2.2 [1.6–3.1] |
| Given less food than others in house: | (P < 0.001)* | (P = 0.299) | (P <0.001)* | (P = 0.308) | |||||
| Never | 1222 | 589 | 48.2 | 1.0 | 1.0 | 250 | 20.5 | 1.0 | 1.0 |
| Sometimes/always | 159 | 122 | 76.7 | 3.5 [2.4–5.2] | 1.3 [0.8–2.1] | 76 | 47.8 | 3.6 [2.5–5.0] | 1.2 [0.8–1.9] |
Chi-square P-value presented from univariate analysis
OR adjusted for a priori confounders (age, gender, marital status, education, district) and all factors independently associated with being at risk or severely at risk for common affected disorder (Likelihood ratton test P-value < 0.1) (i.e. Female headed house, moved house, skipped a meal, referred to in negative way, shunned by others, given more work, not given clothes)
P < 0.05
Risky Sexual Behavior Associated with Common Affective Disorders
Whilst not significantly associated with HIV infection, which was relatively uncommon in this cohort of school students, being at risk for affective disorders was associated with behavioral factors that increase susceptibility to HIV. After adjusting for a priori confounders, participants at risk of having affective disorders (i.e. those with an SSQ score of 8–10) were 1.5 times as likely to report ever having sex than those who were not at risk, and those who were at risk of severe affective disorders (SSQ score ≥ 11) were almost 3 times as likely to report ever having sex than those not at risk (Table 5). They were also more likely to report multiple sexual partners, a younger age of sexual debut, and use of drugs or alcohol. Young women at risk of affective disorders were more likely to be pregnant on their urine test. Tests for trend showed strong evidence of an association between the severity of risk for affective disorders and each of these behaviorial factors that remained even after adjusting for a priori confounders (Table 5).
Table 5.
Association between psychological morbidity and sexual behaviour
|
n (%) reporting behaviour/outcome |
At risk (SSQ score 8–10) |
Severely at risk (SSQ score 11–14) |
||||||
|---|---|---|---|---|---|---|---|---|
| Mentally healthy | At risk (SSQ = 8–10) | Severely at risk (SSQ = 11–14) | P-value test for trend | Crude OR [95%CI] | Adjusted* OR [95%CI] | Crude OR [95%CI] | Adjusted* OR [95%CI] | |
| Ever had sex | 67 (10.0) | 54 (14.0) | 75 (22.7) | P < 0.001 | 1.5 [1.0–2.2] | 1.5 [1.0–2.4] | 2.6 [1.8–3.8] | 2.8 [1.9–4.2] |
| 2 or more lifetime partners | 14 (2.1) | 17 (4.5) | 31 (9.7) | P < 0.001 | 2.2 [1.1–4.5] | 2.3 [1.1–4.8] | 5.0 [2.6–9.6] | 5.4 [2.7–10.7] |
| Sexual debut aged 15 or younger | 11 (1.7) | 13 (3.4) | 12 (3.8) | P = 0.034 | 2.1 [0.9–4.7] | 2.0 [0.9–4.5] | 2.3 [1.0–5.4] | 2.2 [1.0–5.2] |
| Positive pregnancy result (females only) | 3 (1.0) | 4 (2.3) | 9 (6.3) | P = 0.002 | 2.3 [0.5–10.5] | 3.4 [0.7–16.8] | 6.7 [1.8–25.3] | 8.0 [1.9–33.8] |
| Ever tried drugs or alcohol | 180 (26.9) | 140 (36.3) | 132 (40.4) | P < 0.001 | 1.5 [1.2–2.0] | 1.7 [1.3–2.2] | 1.8 [1.4–2.4] | 2.0 [1.5–2.7] |
Adjusted OR adjusted for a priori confounders only (age, gender, marital status, education and district)
Discussion
In this paper we report on data collected from school-going youth in rural south-east Zimbabwe which indicate a high prevalence of anxiety and depression, which was associated with behavioral risk factors for HIV acquisition and transmission. Zimbabwe has one of the most sustained and severe HIV epidemics in the world, resulting in widespread morbidity and mortality and leading to high rates of orphaning and family disruption. Perhaps not surprisingly, we found that having moved to different family members’ homes, being from a poor household and feeling stigmatized, all factors that applied more to orphans than non-orphans, were strongly associated with affective disorders. However, being orphaned was not directly associated with being at risk of an affective disorder, suggesting that it is these factors and not the experience of orphanhood per se that is associated with poor mental health.
Of particular importance in this community, where HIV is common, is the fact that participants at risk for affective disorders were more likely to report being sexually active, having earlier sexual debut and having more lifetime sexual partners than those not at risk. We also demonstrated a strong linear association between severity of risk for affective disorders and riskiness of behavior. Studies in the US have also shown a relationship between psychological distress and risky sexual behaviors. In the National Longitudinal Study of Adolescent Health, Waller and colleagues found that girls experience more depressive symptoms than boys and that every reported risk behavior studied (including sexual and drug abuse) was related to an increase in depressive symptoms [14]. Two other studies also show that adolescents girls are at an increased risk for HIV if they are psychologically distressed [15, 16]. More recently, research in southern Africa has demonstrated a relationship between psychological distress and risky sexual behaviors. In South Africa a study among youth indicated that after adjusting for demographic characteristics, youth reporting the presence of either depression, alcohol abuse or post traumatic stress disorder were at increased risk of forced sex (AOR = 2.53 95%CI 1.64–4.02); transactional sex (AOR = 2.88; 95%CI 1.6–4.02), but also increased condom use (AOR = 2.07; 95%CI 1.29–6.48) [17]. In Zimbabwe, children aged 12–17 were interviewed as part of a nationally representative survey of orphans and vulnerable children. Maternal and paternal orphans who scored higher on the psychosocial distress scale reported earlier onset of sexual activity (boys AOR = 1.36; 95%CI 1.06–1.75; girls AOR = 1.23; 95%CI 1.10–1.50) [18].
With regards to stigma, those at risk clearly felt more stigmatized than those not at risk. However, in a cross-sectional survey it is difficult to determine the direction of effect. Poor mental health is a cause of stigma in its own right, while being stigmatized by others for being poor or orphaned may likewise lead to mental health disorders.
The importance of using culturally appropriate scales is increasingly recognized [19]. The Shona Symptom Questionnaire is a well-validated mental health scale which was initially developed for use as a screening tool in adult patients presenting to a primary care clinic or traditional healer [8–11]. The SSQ has been used in other population-based settings where results in clinic patients and general population participants were found to be similar (personal communication Dixon Chibanda). The internal consistency of the scale in this survey was high, with a Cronbach’s alpha of 0.83 suggesting that the items in the scale were indeed measuring similar constructs (mood) in this population. While the cut-offs for these affective disorders were defined at the time of the original validation and have been used in various populations in Zimbabwe, these cut-offs have not specifically been validated for use in young people. However, the majority of participants in our study were aged 18 or over, and even if the cut-offs used in this population are over-inclusive, raising them by one or two points would still indicate high levels of psychological morbidity in this population. For example, if the cut-off is raised to 11 or more (being at risk for severely affected) then the prevalence is 23.8%.
The SSQ was originally designed to be administered with a response option of yes/no. In the current study, we expanded the response options to examine the intensity of a participant’s response, asking them to state whether they experienced particular feelings always, sometimes or never. Expanding the response categories may have increased the proportion of participants who were categorized as at risk overall, in that a participant may be more likely to respond ‘sometimes’ to a question rather than ‘yes’. However, in a subsequent population-based survey run in some of the same districts in 2007 as part of the evaluation of the Zimbabwe Government’s National Behavior Change Strategy, similar rates were detected among a representative sample of 18–24 year olds (55% at risk of being affected, at risk 24% of being severely affected) using the ‘yes/no’ response option rather than ‘always/sometime/never’ (data not shown).
Previous studies in Zimbabwe and elsewhere in the region have demonstrated high rates of depression in adults and associations between depression and life stressors such as poverty, bereavement and exposure to ill health. A study in the 1980s of Zimbabwean rural and urban clinic attendees found that 26% of 16–60 year olds had signs of psychological disorder [20] and that rates were similar between urban and rural communities. A more detailed study of 172 randomly selected female city-dwellers conducted in the mid 1990s found that 31% of women were depressed [21] and that this high rate of depression was associated with a high rate of adverse life events and difficulties [22], including relationship difficulties, infertility, bereavement and entrapment in a difficult situation. These findings are in keeping with studies from other developing countries which show that in adverse circumstances rates of depression may exceed 50% [23]. More recently, in South Africa, 9.1% of respondents aged 18 and over in a nationally representative sample reported suicide ideation, rates that are similar to those reported here [24]. In Zimbabwe, as in many other developing countries with high rates of HIV-associated morbidity and mortality, life stressors are a common aspect of daily life. The prevailing economic challenges no doubt increase this stress as families that were previously able to function fall below the poverty line. In the 2005–2006 Zimbabwe Demographic and Health Survey [25] some of these stressors were quantified; it found that there has been a dramatic increase in the rates of orphaning since the previous DHS survey in 1999 with 24% of children now reporting having lost one or both parents. There was evidence that the rate of childhood malnutrition, a marker of family poverty, has also risen substantially from 21% in 1994 to 28% in 2005/6 as have age-specific adult mortality rates [26].
The overall survey response rate was lower than we had hoped as a result of out-migration from the study communities, a consequence of the high rates of mobility within Zimbabwe. However, we believe our interim survey participants are broadly representative of school-going youth living in the rural communities where the study was set. Our cohort initially enrolled 87% of eligible participants in the community. Three years after the cohort was recruited, almost all cohort members still living in the study communities (96%) took part. Of note, only school-going adolescents were eligible for recruitment into the original cohort. Adolescents from poorer families and orphans not attending school will, if anything, be under-represented suggesting that our estimates of risk of affective disorders represent minimum levels. Survey participants were broadly similar to non-participants with respect to characteristics measured at baseline. We have found that moving to different family members’ homes in the previous 5 years, something that happens frequently to orphaned children who are moved between different branches of their extended family, is associated with increased rates of psychological morbidity, making it unlikely that non-respondents would have had much lower rates of poor mental health than respondents.
There is increasing recognition of the burden of poor mental health among young people and the devastating impact it has on development [1]. In Southern Africa, where HIV combined with the more general stresses of poverty and rapid social and economic changes have had damaging effects, the burden of psychological morbidity is particularly high. While there is widespread recognition of the need to alleviate poverty, reduce rates of HIV and minimise its consequences, these goals are hard to attain and are unlikely to be achieved in the near future. Zimbabwe has one of the most severe and sustained HIV epidemics with some of the highest rates of orphaning in the region. This data suggests that psychological interventions to prevent, identify, and treat mental health disorders in young people in Zimbabwe and likely more widely in sub-Saharan Africa need to be prioritized. Widespread provision of specialist mental health services in the region is unaffordable and unrealistic but there is some evidence to suggest that non-specialist community-based psychological services can make an impact on the psychological well-being of young people which will likely also impact on other social and behavioral outcomes. In countries where HIV is common, the additional risk of acquiring HIV and subsequently transmitting the virus makes implementing and rigorously evaluating such programmes an even more urgent priority.
Contributor Information
Lisa F. Langhaug, Email: lisa.langhaug@gmail.com, Centre for Sexual Health and HIV Research, Research Department of Infection and Population Health, University College London, Mortimer Market Centre, off Capper Street, London WC1E 6JB, UK
Sophie J. Pascoe, MRC Tropical Epidemiology Group, London School of Hygiene and Tropical Medicine, Keppel Street, London WC1E 7HT, United Kingdom
Webster Mavhu, Department of Community Medicine, College of Health Sciences, University of Zimbabwe, PO Box A1679, Avondale, Harare, Zimbabwe.
Godfrey Woelk, Department of Community Medicine, College of Health Sciences, University of Zimbabwe, PO Box A1679, Avondale, Harare, Zimbabwe.
Lorraine Sherr, Department of Infection and Population Health, Royal Free and University College Medical School, Upper Third Floor, Royal Free Hospital, Rowland Hill Street, London NW3 2PF, United Kingdom.
Richard J. Hayes, MRC Tropical Epidemiology Group, London School of Hygiene and Tropical Medicine, Keppel Street, London WC1E 7HT, United Kingdom
Frances M. Cowan, Centre for Sexual Health and HIV Research, Research Department of Infection and Population Health, University College London, Mortimer Market Centre, off Capper Street, London WC1E 6JB, UK
References
- 1.World Health Organization DoMHaSA and Prevention Research Centre of the Universities of Nijmegen and Maastrict. Prevention of mental disorders: Effective interventions and policy options: summary report. 2004. [Google Scholar]
- 2.Patel V, Flisher AJ, Hetrick S, McGorry P. Mental health of young people: A global public health challenge. Lancet. 2007;369:1302–1313. doi: 10.1016/S0140-6736(07)60368-7. [DOI] [PubMed] [Google Scholar]
- 3.Patel V, Kleinman A. Poverty and common mental disorders in developing countries. Bulletin of the World Health Organization. 2003;81:609–615. [PMC free article] [PubMed] [Google Scholar]
- 4.Ross DA, Dick B, Ferguson J, editors. WHO technical report series No. 938. 2006. Preventing HIV/AIDS in young people: Systematic reviews of the evidence from developing countries. [PubMed] [Google Scholar]
- 5.Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, et al. No health without mental health. Lancet. 2007;370(9590):859–877. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- 6.Cowan FM, Pascoe SJS, Langhaug LF, Dirawo J, Chidiya S, Jaffar S, et al. The Regai Dzive Shiri project: A cluster randomised controlled trial to determine the effectiveness of a multi-component community based hiv prevention intervention for rural youth in Zimbabwe—study design and baseline results. Tropical Medicine and International Health. 2008;13(10):1235–1244. doi: 10.1111/j.1365-3156.2008.02137.x. [DOI] [PubMed] [Google Scholar]
- 7.Pascoe SJS, Langhaug LF, Dirawo J, Jaffar S, Hayes RJ, Cowan FM. HIV among orphans and vulnerable children in rural Zimbabwe: data from the Regai Dzive Shiri project adolescent reproductive health trial in rural Zimbabwe. 16th ISSTDR; Amsterdam. 2005. [Google Scholar]
- 8.Patel V, Simunyu E, Gwanzura F, Lewis G, Mann A. The shona symptom questionnaire: The development of an indigenous measure of common mental disorders in Harare. Acta Psychiatrica Scandinavia. 1997;95:469–475. doi: 10.1111/j.1600-0447.1997.tb10134.x. [DOI] [PubMed] [Google Scholar]
- 9.Patel V, Mann A. Etic and emic criteria for non-psychotic mental disorder: A study of the cisr and care provider assessment in Harare. Social Psychiatry and Psychiatric Epidemiology. 1997;32:84–89. doi: 10.1007/BF00788925. [DOI] [PubMed] [Google Scholar]
- 10.Patel V, Musara T, Butau T, Murambara P, Fuyane S. Concepts of mental illness and medical pluralism in Harare. Psychological Medicine. 1995;25:485–493. doi: 10.1017/s0033291700033407. [DOI] [PubMed] [Google Scholar]
- 11.Patel V, Gwanzura F, Simunyu E, Lloyd K, Mann A. The phenomenology and explanatory models of common mental disorder: A study in primary care in Harare, Zimbabwe. Psychological Medicine. 1995;25(1191):1199. doi: 10.1017/s003329170003316x. [DOI] [PubMed] [Google Scholar]
- 12.Lewis G, Pelosi A, Araya R. Measuring psychiatric disorder in the community: A standard assessment for use by lay interviewers. Psychological Medicine. 1992;22:465–486. doi: 10.1017/s0033291700030415. [DOI] [PubMed] [Google Scholar]
- 13.U.S. Department of Health and Human Services, Public Health Services, and Center for Disease Control and Prevention. Serologic assays for human immunodeficiency virus antibody in dried blood specimens collected on filter paper. 2000. [Google Scholar]
- 14.Waller MW, Hallfors DD, Halpers CT, Iritani BJ, Ford CA, Guo G. Gender differences in associations between depressive symptoms and patterns of substance use and risky sexual behavior among a nationally representative sample of U.S. adolescents. Archives of Women’s Mental Health. 2006;9:139–150. doi: 10.1007/s00737-006-0121-4. [DOI] [PubMed] [Google Scholar]
- 15.DiClemente RJ, Wingoood GM, Crosby RA, Sionean C, Brown LK, Rothbaum B, et al. A prospective study of psychological distress and sexual risk behavior among black adolescent females. Pediatrics. 2001;108:1–6. doi: 10.1542/peds.108.5.e85. [DOI] [PubMed] [Google Scholar]
- 16.Leher JA, Shrier LA, Gortmaker S, Buka S. Depressive symptoms as a longitudinal predictor of sexual risk behaviors among US middle and high school students. Pediatrics. 2006;118:189–200. doi: 10.1542/peds.2005-1320. [DOI] [PubMed] [Google Scholar]
- 17.Smit J, Myer L, Middelkoop K, Seedat S, Wood R, Bekker LG, et al. Mental health and sexual risk behaviors in a South African township: A community-based cross-sectional study. Public Health. 2006;120(6):534–542. doi: 10.1016/j.puhe.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 18.Nyamukapa CA, Gregson SA, Lopman B, Saito S, Watts HJ, Monasch R, et al. HIV-Associated orphanhood and children’s psychosocial distress: Theoretical framework tested with data from Zimbabwe. American Journal of Public Health. 2008;98(1):133–141. doi: 10.2105/AJPH.2007.116038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hanlon C, Medhin G, Alem A, Araya M, Abdulahi A, Tesfaye M, et al. Measuring common mental disorders in women in Ethiopia: Reliability and construct validity of the comprehensive psychopathological rating scale. Social Psychiatry and Psychiatric Epidemiology. 2008;43:653–659. doi: 10.1007/s00127-008-0342-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reeler AP, Williams H, Todd C. Psychopathology in primary care patients: A four year study in rural and urban settings in Zimbabwe. Central African Journal of Medicine. 1993;39:1–7. [PubMed] [Google Scholar]
- 21.Abas M, Broadhead J. Depression and anxiety among women in an urban setting in Zimbabwe. Psychological Medicine. 1997;27:59–71. doi: 10.1017/s0033291796004163. [DOI] [PubMed] [Google Scholar]
- 22.Broadhead J, Abas M. Life events, difficulties and depression among women in an urban setting in Zimbabwe. Psychological Medicine. 1998;28:29–38. doi: 10.1017/s0033291797005618. [DOI] [PubMed] [Google Scholar]
- 23.Patel V, Abas M, Broadhead J, Todd C, Reeler AP. Depression in developing countries: Lessons from Zimbabwe. British Medical Journal. 2001;322:482–484. doi: 10.1136/bmj.322.7284.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Joe S, Stein DJ, Seedat S, Herman A, Williams DR. Prevalence and correlates of non-fatal suicidal behavior among South Africans. The British Journal of Psychiatry. 2008;192:310–311. doi: 10.1192/bjp.bp.107.037697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Central Statistical Office and Macro International Inc. Zimbabwe demographic and health survey 2005–2006: Preliminary report. Calverton, Maryland: Macro International Inc; 2006. [Google Scholar]
- 26.Central Statistical Office and Macro International Inc. Zimbabwe demographic and health survey 1999. Calverton, Maryland: Macro International Inc; 2000. [Google Scholar]