Abstract
Purpose
To evaluate the frequency and magnitude of binocular gain (and loss) for high contrast acuity, various low contrast spatial vision measures and contrast sensitivity in an elderly population.
Methods
Ninety-five individuals over the age of 70 (mean age 80.5 years, range 71.8 to 93.5) with acuity of 20/40 (logMAR 0.3) or better in at least one eye participated. Each individual was tested binocularly and then monocularly on high contrast acuity, various low contrast acuity measures and contrast sensitivity. Binocular gain for acuity measures was defined as better performance of one line or more under binocular conditions than with the better eye alone. Binocular loss was defined as poorer performance of one line or more binocularly than with the better eye alone. For contrast sensitivity, the criterion for binocular gain or loss was one letter triplet (0.15 log unit) or more difference. For each measure, the frequency of binocular gain and loss, as well as the mean gain or loss were determined.
Results
The mean difference between binocular and better eye monocular acuity was less than 2 letters for all measures, suggesting little gain or loss. However, the percent of individuals showing a line or more of gain or loss ranged from approximately 20% for high contrast acuity to 35.8% for low contrast acuity at low luminance. This indicates that for 1/5 to ⅓ of individuals, binocular vision is not well represented by monocular vision measures. All low contrast measures and contrast sensitivity show more binocular gain/loss than standard acuity. As has been previously reported, in the presence of large inter-ocular differences, binocular gain is not seen, but binocular loss does not necessarily occur.
Conclusions
For a significant portion of this elderly population, binocular performance is not well represented by better eye monocular measures. This indicates that to get a true sense of an individual’s vision function in daily life, one must measure vision binocularly.
Keywords: acuity, contrast sensitivity, aging, binocular summation, binocular inhibition
Binocular summation (or binocular gain) is the improvement in performance when viewing with both eyes compared to the better eye alone1,2. This gain in performance may reflect probability summation and/or neural summation of the signals from the two eyes1,2. The extent of binocular gain depends on many factors. For example, Home3 found more gain for low contrast than high contrast targets, and others have reported that binocular gain is spatial frequency dependent4,5. When the eyes are stimulated unequally as may occur in cataract or following cataract surgery, binocular loss, rather than gain, becomes more likely6-13. Binocular loss, as used here, refers to worse binocular vision performance than vision performance when viewing with the better eye alone. Studying patients with AMD, which often affects the eyes unequally, Faubert and Overbury14 and Valberg and Fosse15 found that approximately half of the patients showed binocular loss. This is consistent with reports that binocular summation declines with increasing inter-ocular difference (IOD) in sensitivity and that when IODs are sufficiently large the expectation is that binocular loss, rather than gain, will occure.g.16
The magnitude of binocular gain declines with age4,5,18,20. If binocular gain and loss are negligible in the aged, one may infer binocular performance from measures of monocular (better eye) performance. This has been suggested to be the case for high contrast acuity in older observers17. Others, however, report significant binocular summation of acuity among elders, and suggest that monocular measures do not accurately reflect binocular function, and thus ‘everyday’ performance in a substantial portion of the elderly20.
This study assessed the frequency and degree of binocular gain and loss for visual acuity in a group of older individuals. This group is older than those previously studied, and therefore may be expected to exhibit less binocular gain than has previously been reported for standard high contrast acuity. In addition to visual acuity, binocular gain and loss for low contrast spatial vision measures and contrast sensitivity were assessed in this older population. If a substantial portion of the group shows significant (beyond the coefficient of repeatability) binocular-monocular differences, this would have implications for clinical practice as well as for research, suggesting a need for binocular measurement of vision function in addition to monocular measures. It would be valuable to know whether or not better eye acuity is truly representative of binocular performance. It would also be helpful to know for which patients optimal visual task performance is achieved with one eye closed.
METHODS
Subjects
Participants in this study were a subset of 95 of the SKI21 longitudinal study sample, a random sample of community-dwelling elders. The subset (assembled for other study purposes) was selected to have acuity correctable to 20/40 or better in at least one eye. There were no other inclusion/exclusion criteria. All subjects underwent subjective refraction at the time of testing and wore optimal correction for near or distance, as appropriate, for all testing. Subjects meeting the acuity criterion ranged in age from 71.8 to 93.5 years of age, with a mean sample age of 80.5 years. Sixty percent are female. The median binocular, better eye, and worse eye acuities were 0.04, 0.00 and 0.12 logMAR which correspond to 20/22, 20/20 and 20/26 in Snellen notation.
The study adhered to the Declaration of Helsinki and was approved by the Smith-Kettlewell Eye Research Institute and the California Pacific Medical Center Institutional Review Board. All subjects gave informed written consent.
Procedures
High and low contrast acuity tests (Bailey-Lovie charts22 at 10 ft), contrast sensitivity (Pelli-Robson Chart23 at 10 ft), low contrast acuity at reduced luminance (SKILL Card24 dark chart; 15% contrast, 15 cd/m2, at 16 inch test distance) low contrast acuity in the presence of surrounding glare (Berkeley glare test25, 10% contrast acuity chart at 16 inches) were measured in that order. Each of the tests was scored letter-by-letter. All scores were converted to logarithmic units (logMAR for acuity tests or log contrast sensitivity). Each letter on an acuity chart has a value of 0.02 logMAR; each letter on the contrast sensitivity chart has a value of 0.05 log units.
Each subject was tested binocularly, then with right eye, then with left eye on each measure. This testing order is selected to be the same as used by Rubin et. al.17 and Azen et. al.20 to facilitate comparison of results. For monocular testing, the non-tested eye was covered with an opaque (black) occluder. Time was allowed for light adaptation before testing of a previously patched eye. With the exception of the SKILL Card, and the Berkeley Glare test chart, of which there are only single versions available, different versions of the tests were used for consecutive measures (binocular, right eye, left eye). A rigorous forced-choice testing procedure was used. Participants were required to guess, even if the letters seemed illegible, until at least 3 of 5 letters on an acuity chart line or an entire triplet of letters on the Pelli-Robson Chart were not named correctly. All testing was done with optimal refractive error correction in place for the test distance. Given the potential for learning, measuring binocularly first may result in a slight underestimate of binocular gain. However, given that the right eye was measured before the left eye, yet the performance right eye was slightly better (1.82 letters, median of all measures) than the left eye suggests that, if learning occurred, it was negligible. For the glare chart, of which there is a single version the right eye was 1.6 letters (0.03 log units) better than left. The SKILL Card showed no training effect between right and left eyes, despite the repeated use of the same chart. A training effect between monocular and binocular testing is likely to be very small if present for all measures. This may reflect the fact that other chart(s) were read between repetitions of the same test.
In accord with previous research17,20 and test-retest repeatability27, for high contrast distance acuity, binocular gain is defined here as binocular performance at least one line (5 letters, 0.1 log unit) better than performance with the better eye alone. Binocular loss is one line or more poorer acuity binocularly than with the better eye. The coefficients of repeatability of the Berkeley glare test28, low contrast acuity26 and SKILL dark chart (unpublished data) are all ±0.138 log units; the criterion difference for binocular gain or loss was set at 7 or more letters (0.14 log units) for these measures. For contrast sensitivity, gain and loss criteria are differences between binocular and better eye monocular performance of at least 0.15 log unit (one letter triplet of the Pelli-Robson Chart).27
RESULTS
Frequency of Binocular Gain or Loss
Table 1 presents the percent of participants showing binocular gain (2nd column), binocular loss (3rd column), or either (4th column). Several points are worth noting. On average (across measures), 22.7% of individuals show significant differences between better eye and binocular performance. For these individuals monocular (better eye) measures do not well represent binocular performance, i.e. performance under real world conditions. Binocular loss occurs (17.9% of cases) much more frequently than binocular gain (2.1 % of cases) for high contrast acuity in this sample of elders chosen to have acuity of 20/40 or better in at least one eye. The finding indicates that high contrast acuity does not tend to produce binocular gain in this population of elders with good acuity in at least one eye. In only 3 cases was monocular acuity so close to the limits of the chart (so good), for ceiling effects to preclude potential binocular gain, so ceiling effects are not responsible for the low rate of binocular gain. In sharp contrast are the findings for contrast sensitivity; for this measure binocular gain is 5 times as frequent as binocular loss. For each of the other low contrast acuity measures, binocular gain and loss occur at more similar rates. The highest frequencies of binocular–monocular difference are seen for the SKILL Dark Chart, with over one third showing a difference of at least 7 letters between binocular and better eye monocular acuity.
Table 1.
The percentage of individuals showing binocular gain (2nd column), binocular loss (3rd column) or either (4th column) for each of the vision measures (1st column)
| Binocular Gain (%) |
Binocular Loss (%) |
Total % (Gain + Loss) |
|
|---|---|---|---|
| High contrast acuity | 2.1 | 17.9 | 20.0 |
| Low contrast acuity | 4.2 | 8.4 | 12.6 |
| Contrast sensitivity | 21.1 | 4.2 | 25.3 |
| SKILL dark chart | 19.0 | 16.8 | 35.8 |
| LC acuity in glare | 9.5 | 10.5 | 20.0 |
|
| |||
| Mean | 11.2 | 11.6 | 22.7 |
Dependence on Inter-Ocular Differences
Table 2 shows the distribution of interocular differences for each measure. Though the median IOD for each measure was approximately one to one and one half lines, occasionally very large IODs of a log unit or more were seen. Weak but statistically significant negative associations between interocular difference and binocular-monocular differences were found for some measures (contrast sensitivity (r2= 0.12;, p<0.0001) and low contrast acuity in glare (r2= 0.11, p <0.002)), but for other measures (high contrast acuity (p> 0.05), low contrast acuity (p=0.02) and SKILL Dark Chart acuity (p=0.02)) the associations were not statistically significant.a As an example, the association between binocular interaction and IOD for low contrast acuity at low luminance (SKILL dark chart) is presented in Figure 1. This figure illustrates several characteristics of the findings of all measures. In the absence of any IOD and even in the presence of fairly large IODs (up to about 0.5 log units (5 lines) for this measure) binocular gains and binocular losses both occur. At larger IODs (> 6 lines), many observers show no binocular advantage or disadvantage, but when binocular–monocular differences are present, only binocular loss occurs; binocular gain is not seen for any measure in the presence of such large IODs. At the largest IODs, some measures show binocular loss, whereas other measures show no difference between binocular and better eye measures as can be seen to be the case for the SKILL dark chart. However, so few individuals have IODs beyond 0.6 log unit, that the data can not really be used to determine what happens at extreme IODs.
Table 2.
Distribution of interocular differences (log units) for each vision measure (25th percentile, median, 75th percentile, 95th percentile, and maximum value)
| 25th | Median | 75th | 95th | Maximum | |
|---|---|---|---|---|---|
| High contrast acuity | 0.04 | 0.08 | 0.14 | 0.58 | 1.46 |
| Low contrast acuity | 0.04 | 0.10 | 0.18 | 0.70 | 1.40 |
| Contrast sensitivity | 0.05 | 0.05 | 0.15 | 0.91 | 1.60 |
| SKILL dark chart | 0.06 | 0.16 | 0.26 | 0.74 | 0.90 |
| LC acuity in glare | 0.06 | 0.14 | 0.22 | 0.92 | 1.14 |
Figure 1.
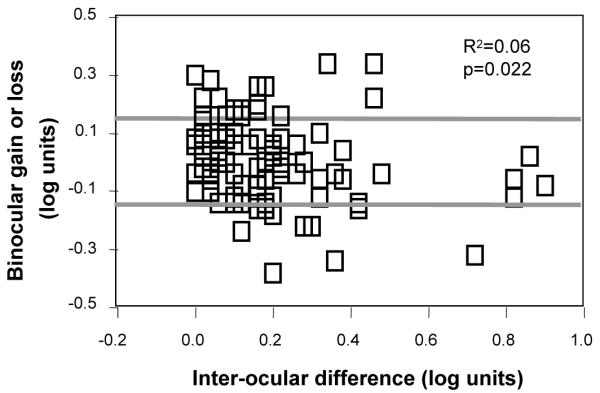
The degree of binocular gain (positive values) and loss (negative values) plotted as a function of interocular difference on this measure (SKILL dark chart acuity). Points falling above or below the region bounded by a rectangle represent significant gain (above) or loss (below).
Age Effects on Binocular Gain or Loss
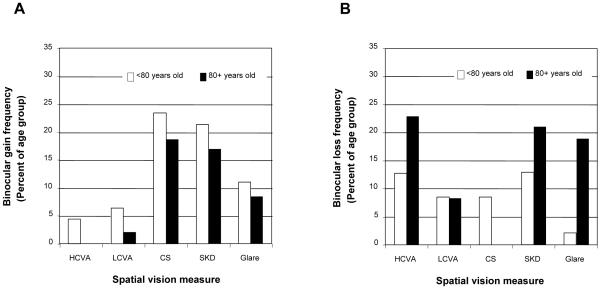
To determine whether an age effect on binocular gain or loss is present in our data set, subjects were divided into two age groups: <80 years (n= 48; mean age 76.6) and 80 years and above (n=47; mean age 84.3). Figure 2a shows that binocular gain tends to be less frequent among the older (80+) age group for all vision measures. Figure 2b shows that the binocular loss tends to be more frequent in the older group for three of five measures. None of those aged 80+ years show binocular loss of contrast sensitivity. This may be due to sampling, as so few individuals (4.2 %) show binocular loss for contrast sensitivity at any age in this aged sample. Together, the figures suggest that binocular gain frequency tends to decrease with age whereas the frequency of binocular loss tends to increase, though only for low contrast acuity in glare is inhibition significantly more common in the older group (Fisher’s Exact Test, p=0.008). For summation, none of the differences between age groups is statistically significant. The lack of significant differences between older and younger age groups may reflect the fact that the difference in age for the two groups in this study was only 7 years.
Figure 2.
The frequency of binocular gain (2a) or binocular loss (2b) for subjects less than eighty years old (white bars) and those 80 years and above (dark bars) for each of the 5 spatial vision measures. HCVA: High contrast visual acuity; LCVA: Low contrast visual acuity; CS: Contrast sensitivity; SKD: Low contrast acuity measured at reduced luminance using the SKILL dark chart; Glare: Low contrast acuity in the presence of surrounding glare. Note that binocular gain tends to be less common among the older age group (2a). Also note that for all measures except LCVA and CS, binocular loss is more common among the older age group so that the overall frequency of binocular effects remains relatively stable across age at approximately 20% on average across measures.
The trend toward decrease in the frequency of binocular gain in the older age group is not due to an increase in inter-ocular differences across age. The magnitudes of the inter-ocular differences for each measure are essentially the same in the two age groups (one letter difference between age groups for all acuity tests and less than one letter for contrast sensitivity).
To further examine the association between age, IOD and binocular gain or loss, logistic regression was used. For each vision measure, binocular gain and loss are considered separately. For each test, IOD and age were considered separately and in combination as predictors of binocular gain or loss. None of the results was statistically significant.
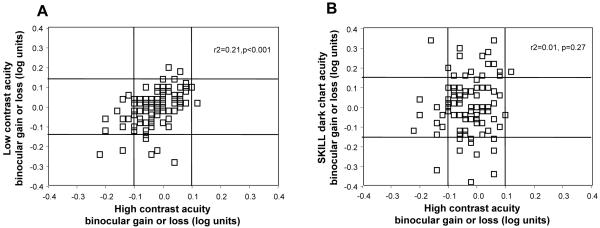
Agreement Between Measures
If an individual shows binocular gain (or loss) on one measure, does s/he show the same phenomenon on other measures? This is not necessarily the case, as is evident from the different frequencies of binocular gain and loss between measures (Table 1). The two measures that show the strongest association of binocular gain and loss are high and low contrast acuity (Figure 3a), r2=0.21, p<0.0001). Nonetheless, there are numerous individuals who show binocular loss for high contrast acuity but no binocular–monocular difference for low contrast acuity (Figure 3a, first column, second row). Others show binocular gain or loss for low contrast acuity but not for high contrast acuity (middle column, first and third rows.) Only two individuals show gain for both measures and none shows loss for both measures. The agreement between binocular gain or loss for high contrast acuity and the SKILL dark chart (Figure 3b) is poorer (r2=0.013, p=0.27) with many individuals showing binocular monocular differences on one measure but not the other, and 2 showing binocular gain for SKILL dark chart acuity and binocular loss for high contrast acuity. Contrast sensitivity and acuity in glare also show only weak correspondence (statistically non-significant linear regressions) of gain and loss with high contrast acuity (r2=0.03, p=0.08 and r2=0.02, p=0.21 respectively) and many individuals with conflicting results.
Figure 3.
Agreement between measures. a) The agreement between binocular gain or loss on high contrast acuity and low contrast acuity. b) The agreement between binocular gain or loss on SKILL dark chart acuity and contrast sensitivity. The central region indicates no binocular gain or loss on either measure. Points on the line bounding the central region and outside the region indicate binocular gain or loss on the measure(s) indicated along the axes. Points in the 3 regions along the 45 degree line show agreement between the two measures. The central region indicates no binocular gain or loss on either measure. Regions off the diagonal indicate gain or loss for one measure but not the other (the four arms of the cross) or loss on one measure and gain on the other (upper left and lower right regions).
DISCUSSION
This study examined the advantage (binocular gain) or disadvantage (binocular loss) of elders viewing binocularly rather than monocularly with the better eye. We find that 12.6% - 35.8% of the population shows a significant difference between monocular (better eye) and binocular performance, depending on the measure tested. Low contrast acuity showed the lowest frequency of binocular gain/loss, 12.6%. We find a higher rate of binocular gain/loss for all of the other measures (Table 1). Binocular gain is least common for high contrast acuity (2.11%). This is consistent with the findings of Home (1978), who reported more summation in the acuity domain for low contrast than high contrast letters. This may also account for the disproportionate amount of gain (vs. loss) for contrast sensitivity.
The SKILL Card dark chart (a measure of low contrast acuity at reduced luminance) showed the highest rate of binocular gain or loss (35.8%). Thus for more than 1/3 of elders, for low contrast targets at low luminance (15cd/m2), monocular better eye vision function differs significantly from binocular vision.
The frequency of binocular gain and loss for high contrast acuity in this study is similar to that of previous studies looking at binocular vs. monocular high contrast acuity in elders17,20. Rubin et. al.17, reported that 15% showed binocular gain or loss. Azen et. al.20 report binocular gain or loss for visual acuity in 23% of their sample, while in the present study, we find binocular gain or loss in 20% of the sample. Thus, the three studies are in relatively good agreement. What differs among studies are the percentages of binocular gain vs. loss. Azen et al.20 report prevalence rates of summation and inhibition of 21% and 2% respectively. Of the 15% of people showing gain or loss in the study by Rubin et. al., 10% showed binocular gain and 5% showed loss. (Rubin, personal communication). The current study found that 2 percent showed binocular gain and 18% showed binocular loss. The two latter groups differ in age by 25 years, with Rubin’s sample falling in the middle in terms of age. Could this account for the differences in relative rates of binocular gain vs. loss in the three samples?
Azen et al.20 noted a significant dependence on age of differences in binocular and better eye acuities. Compared to participants younger than age 65, their older participants were 3 times more likely to experience binocular loss (3% vs. 1%). However, there was no difference between age groups in the frequency of binocular gain (21% for both age groups). We separated the participants of our older sample into those < 80 years of age and those aged 80 years and older (Figure 2 a,b). We find that, for all spatial vision measures except contrast sensitivity, the frequency of binocular loss was slightly higher for the older age group, consistent with the findings of Azen et. al.20 for high contrast acuity. However, contrary to Azen et al.20, we find that for all measures, the frequency of binocular gain tended to be lower in the older age group. These results are compatible with the idea that age differences may contribute to the differences in patterns of binocular gain vs. loss among studies. The age difference between our older and younger sub-samples was small, perhaps explaining why the trends towards decreased gain and increased binocular loss are not significant in most cases. Only for low contrast acuity in glare was the increased inhibition in glare significant. The increased binocular inhibition in the older age group may reflect an increased prevalence of monocular cataract, and the resulting light scatter, in that age group. Closing the cataractous eye would be expected to improve vision in the presence of glare by a fellow non-cataractous eye.
In addition to the effect of age, it is also possible that our inclusion criterion of at least 20/40 (LogMAR ≤0.3) biased the acuity findings toward more loss than gain. However, the impact of ceiling effects is minimal, as only 3 individuals had such good better eye monocular acuity that they could not show significant gain due to limitations in the size of the chart’s smallest letters.
Some may argue that, because of probability summation alone, binocular performance should exceed monocular performance. If one accepts this premise, then frequency of binocular loss would be higher than reported here. If this increased prevalence of binocular loss is considered, then binocular measurement becomes even more important.
It is often assumed that in the absence of large inter-ocular differences (IODs) in standard high contrast acuity (or whatever measure is being examined), binocular gain may occur, and that in the presence of larger inter-ocular differences in sensitivity binocular loss would be seen. However, we find, in accord with previous studies17,20 that in the absence of any IOD or in the presence of small IODs, gain and loss both occur. With large inter-ocular differences, binocular gain is not seen, as expected. When these large IODs are present, binocular loss is found for some measures but is not seen for other measures; in the latter case, binocular acuities and better eye monocular acuities are similar. These findings are in agreement those of Rubin (Rubin, personal communication), who found binocular loss for high contrast acuity in 2% of those with small or absent IODs and 8-13% (depending on IOD) with larger IODS.
The average difference between binocular and better eye acuity in the three studies under discussion are: less than 3 letters in Azen et al.’s20 study, less than 2 letters in the present study and less than 1 letter in Rubin et al17. It is important not to be misled by the rather small mean differences between binocular and better eye high contrast acuity. As is often the case, the mean doesn’t well represent what is happening at the level of the individual. Like Azen et. al.20, we believe that the prevalence of significant binocular gain or loss or is the more useful measure, and is more appropriate for clinical application. Each of these studies finds a significant proportion (15 to 23%) of the population for whom the better eye high contrast acuity does not well represent binocular acuity (differs by more than expected based on the coefficients of repeatability, 1 line). The present study finds that 1 in 5 of our sample showed significant differences between binocular and monocular high contrast acuities. Higher frequencies of binocular gain and loss were seen for contrast sensitivity (25.3%) and for SKILL Dark chart acuity measures (36%). Given that we operate in the world binocularly, it is important at the individual level to accurately know performance under this viewing condition.. This conclusion differs from that of Rubin et. al.17 who state (p. 3327) that “The binocular acuities of older individuals can be inferred from measures of monocular acuity.”
The finding that a substantial number of individuals exhibit binocular gain for low contrast targets indicates that monocular assessment would result in an under-estimate of the individual’s function as they go about daily life. On the other hand, a substantial prevalence of inhibition is also seen for low contrast targets, particularly among the oldest old. This latter finding suggests that these individuals may function better with the worse eye closed or patched under certain circumstances when viewing low contrast targets, In this sample with good high contrast acuity in at least one eye binocular gain or loss for low contrast spatial vision measures cannot be well predicted from the gain or loss of high contrast acuity. Individuals may show summation or inhibition for one measure, but not another. This implies that for an individual patient, some tasks may best be performed binocularly while others may best be done monocularly. Only by measuring each task both binocularly and monocularly will the clinician understand the vision function of the individual patient.
In summary, binocularly measured vision function differs significantly from monocularly measured vision function in a substantial proportion of elderly individuals. Whether an individual exhibits binocular gain or loss depends on a number of factors including the individual’s age, interocular differences in sensitivity for the task, and the particular vision function being assessed. A substantial portion of the elderly population, particularly the oldest old, may perform more poorly or better on tasks than is indicated by better eye measures.
ACKNOWLEDGMENTS
Supported by NIH EY 09588 to JAB and by SKERI.
Footnotes
The criterion for significance was set at set at p<0.01 to allow for multiple comparisons.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Campbell FW, Green DG. Monocular versus binocular visual acuity. Nature. 1965;208:191–2. doi: 10.1038/208191a0. [DOI] [PubMed] [Google Scholar]
- 2.Blake R, Fox R. The psychophysical inquiry into binocular summation. Percept Psychophys. 1973;14:161–85. [Google Scholar]
- 3.Home R. Binocular summation: a study of contrast sensitivity, visual acuity and recognition. Vision Res. 1978;18:579–85. doi: 10.1016/0042-6989(78)90206-7. [DOI] [PubMed] [Google Scholar]
- 4.Pardhan S. A comparison of binocular summation in young and older patients. Curr Eye Res. 1996;15:315–9. doi: 10.3109/02713689609007626. [DOI] [PubMed] [Google Scholar]
- 5.Gagnon RW, Kline DW. Senescent effects on binocular summation for contrast sensitivity and spatial interval acuity. Curr Eye Res. 2003;27:315–21. doi: 10.1076/ceyr.27.5.315.17225. [DOI] [PubMed] [Google Scholar]
- 6.Gilchrist J, McIver C. Fechner’s paradox in binocular contrast sensitivity. Vision Res. 1985;25:609–13. doi: 10.1016/0042-6989(85)90167-1. [DOI] [PubMed] [Google Scholar]
- 7.Gilchrist J, Pardhan S. Binocular contrast detection with unequal monocular illuminance. Ophthalmic Physiol Opt. 1987;7:373–7. [PubMed] [Google Scholar]
- 8.Pardhan S, Gilchrist J. The effect of monocular defocus on binocular contrast sensitivity. Ophthalmic Physiol Opt. 1990;10:33–6. [PubMed] [Google Scholar]
- 9.Pardhan S, Gilchrist J. Binocular contrast sensitivity with monocular glare disability. Ophthalmic Physiol Opt. 1990;10:37–9. [PubMed] [Google Scholar]
- 10.Pardhan S, Gilchrist J, Douthwaite W, Yap M. Binocular inhibition: psychophysical and electrophysiological evidence. Optom Vis Sci. 1990;67:688–91. doi: 10.1097/00006324-199009000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Pardhan S, Gilchrist J. The importance of measuring binocular contrast sensitivity in unilateral cataract. Eye. 1991;5:31–5. doi: 10.1038/eye.1991.6. [DOI] [PubMed] [Google Scholar]
- 12.Taylor RH, Misson GP, Moseley MJ. Visual acuity and contrast sensitivity in cataract: summation and inhibition of visual performance. Eye (Lond) 1991;5(Pt 6):704–7. doi: 10.1038/eye.1991.129. [DOI] [PubMed] [Google Scholar]
- 13.Comas M, Castells X, Acosta ER, Tuni J. Impact of differences between eyes on binocular measures of vision in patients with cataracts. Eye. 2007;21:702–7. doi: 10.1038/sj.eye.6702305. [DOI] [PubMed] [Google Scholar]
- 14.Faubert J, Overbury O. Binocular vision in older people with adventitious visual impairment: sometimes one eye is better than two. J Am Geriatr Soc. 2000;48:375–80. doi: 10.1111/j.1532-5415.2000.tb04693.x. [DOI] [PubMed] [Google Scholar]
- 15.Valberg A, Fosse P. Binocular contrast inhibition in subjects with age-related macular degeneration. J Opt Soc Am (A) 2002;19:223–8. doi: 10.1364/josaa.19.000223. [DOI] [PubMed] [Google Scholar]
- 16.Pardhan S, Gilchrist J. Binocular contrast summation and inhibition in amblyopia. The influence of the interocular difference on binocular contrast sensitivity. Doc Ophthalmol. 1992;82:239–48. doi: 10.1007/BF00160771. [DOI] [PubMed] [Google Scholar]
- 17.Rubin GS, Munoz B, Bandeen-Roche K, West SK. Monocular versus binocular visual acuity as measures of vision impairment and predictors of visual disability. Invest Ophthalmol Vis Sci. 2000;41:3327–34. [PubMed] [Google Scholar]
- 18.Pardhan S. A comparison of binocular summation in the peripheral visual field in young and older patients. Curr Eye Res. 1997;16:252–5. doi: 10.1076/ceyr.16.3.252.15407. [DOI] [PubMed] [Google Scholar]
- 19.Owsley C, Sloane ME. Vision and aging. In: Boller F, Grafman J, editors. Handbook of Neuropsychology. Vol. 4. Elsevier; Amsterdam: 1990. pp. 229–49. [Google Scholar]
- 20.Azen SP, Varma R, Preston-Martin S, Ying-Lai M, Globe D, Hahn S. Binocular visual acuity summation and inhibition in an ocular epidemiological study: the Los Angeles Latino Eye Study. Invest Ophthalmol Vis Sci. 2002;43:1742–8. [PubMed] [Google Scholar]
- 21.Haegerstrom-Portnoy G, Schneck ME, Brabyn JA. Seeing into old age: vision function beyond acuity. Optom Vis Sci. 1999;76:141–58. doi: 10.1097/00006324-199903000-00014. [DOI] [PubMed] [Google Scholar]
- 22.Bailey IL, Lovie JE. New design principles for visual acuity letter charts. Am J Optom Physiol Opt. 1976;53:740–5. doi: 10.1097/00006324-197611000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Pelli DG, Robson JG, Wilkins AJ. The design of a new letter chart for measuring contrast sensitivity. Clin Vision Sci. 1988;2:187–99. [Google Scholar]
- 24.Haegerstrom-Portnoy G, Brabyn J, Schneck ME, Jampolsky A, The SKILL Card An acuity test of reduced luminance and contrast. Smith- Kettlewell Institute Low Luminance. Invest Ophthalmol Vis Sci. 1997;38:207–18. [PubMed] [Google Scholar]
- 25.Bailey IL, Bullimore MA. A new test for the evaluation of disability glare. Optom Vis Sci. 1991;68:911–7. doi: 10.1097/00006324-199112000-00001. [DOI] [PubMed] [Google Scholar]
- 26.Lovie-Kitchin JE. Validity and reliability of visual acuity measurements. Ophthalmic Physiol Opt. 1988;8:363–70. doi: 10.1111/j.1475-1313.1988.tb01170.x. [DOI] [PubMed] [Google Scholar]
- 27.Lovie-Kitchin JE, Brown B. Repeatability and intercorrelations of standard vision tests as a function of age. Optom Vis Sci. 2000;77:412–20. doi: 10.1097/00006324-200008000-00008. [DOI] [PubMed] [Google Scholar]
- 28.Elliott DB, Bullimore MA. Assessing the reliability, discriminative ability, and validity of disability glare tests. Invest Ophthalmol Vis Sci. 1993;34:108–19. [PubMed] [Google Scholar]