Abstract
This is a report of post-treatment findings from a completed randomized pilot study testing the preliminary efficacy of The Mothers and Toddlers Program (MTP), a 12 week attachment-based individual parenting therapy for mothers enrolled in substance abuse treatment and caring for children ages birth to 36 months. Forty-seven mothers were randomized to MTP versus the Parent Education Program (PE) – a comparison intervention providing individual case management and child guidance brochures. At post-treatment, MTP mothers demonstrated better reflective functioning in the Parent Development Interview, representational coherence and sensitivity, and caregiving behavior than PE mothers. Partial support was also found for proposed mechanisms of change in the MTP model. Together, preliminary findings suggest that attachment-based interventions may be more effective than traditional parent training for enhancing relationships between substance using women and their young children.
Keywords: Substance abuse, Parent training, Mother-child relations, Attachment, Intervention
Introduction
Although not all mothers seeking substance abuse treatment have difficulties with parenting, substance abusing women, as a group, are twice as likely as non-substance abusing women to lose custody of their children because of child neglect (Department of Health and Human Services, 1999). Research has shown that, although some are able to provide home environments and parenting that support their children's development, most are at greater risk for maladaptive parenting (Mayes & Truman, 2002). Parenting problems observed during children's first 3 years of life include poor attachment, responsiveness, adaptability and structure juxtaposed with heightened physical activity, provocation, and intrusiveness (Burns, Chethik, Burns, & Clark, 1997; Hans, Bernstein, & Henson, 1999). Maternal perspectives about parenting have shown limited understanding of basic child development and ambivalent feelings about having/keeping children (Mayes & Truman, 2002; Murphy & Rosenbaum, 1999).
Parenting interventions for substance abusing women
Only a handful of clinical trials involving substance abusing parents have been reported (for reviews see Kerwin, 2005; Suchman, Pajulo, DeCoste, & Mayes, 2006). Intervention approaches range from skills training to advocacy for basic needs (e.g., food and shelter). Although parents’ well-being (e.g., substance use, psychiatric distress) has often improved, improvement in parent-child dyadic interactions or in child adjustment has been rare. One possible explanation is a failure to emphasize the underlying (often tenuous) emotional quality of the mother-child relationship. Given that women with substance use disorders commonly have developmental histories involving insecure attachment (Luthar & Walsh, 1995), parenting interventions may need to address attachment issues first before targeting behavior management skills. Without first improving a parent's capacity to recognize and respond sensitively to children's emotional cues, interventions for substance using mothers may do little to strengthen the mother-child relationship.
An attachment perspective on parenting
Attachment research suggests that maternal insensitivity and unresponsiveness to child emotional cues are often a function of the caregiver's own unmet attachment needs stemming from the caregiver's own experience with early caregivers. Stored memories or psychological “representations” of these early caregiving experiences are thought to become the prototype for newly formed relationships, including the next generation of caregiving relationships, guiding the new mother's expectations of herself and her child and strongly influencing the mother's parenting behavior (for further discussion, see Suchman, Mayes, Conti, Slade, & Rounsaville, 2004). For parents whose attachment needs went largely unmet, these enduring memories are often characterized by distortion and denial that are thought to help protect the mother against psychological fear and pain. However, these defensive strategies may also prevent the mother from recognizing and responding sensitively to her own child's emotional signals, particularly signals of distress (e.g., crying, clinging, hitting or running away). Instead, child emotional cues are likely to trigger the mother's unmet attachment needs, emotional distress, and avoidance of the stressful stimulus (Suchman & Mayes, 2009). Early parenthood can also evoke maternal memories of early relationships so that they become more accessible during intervention.
Closely related to restricted/distorted mental representations is the compromised ability to mentalize about one's own and others’ behaviors. Reflective functioning – the capacity to recognize intentions and emotions underlying behaviour - is thought to be the mechanism by which maternal representations influence attachment patterns across generations (see Fonagy, Gergely, Jurist, & Target, 2002; Slade, Grienenberger, Bernbach, Levy, & Locker, 2005). Mothers who have inflexible/distorted representations are thought to make fewer accurate inferences about their children's underlying emotions (Slade, 2005, 2006) and to interact less sensitively when caring for their children (Grienenberger, Kelly, & Slade, 2005)
Maternal attachment deficits and substance abuse
Substance abusing mothers often have enduring, impoverished perceptions of early caregivers as uncaring and intrusive and limited capacities for mentalization. These deficits lead to increased parental aggression, neglect and custody loss (see Levy & Truman, 2002; Suchman, McMahon, Slade, & Luthar, 2005; Suchman, McMahon, Zhang, Mayes, & Luthar, 2006). High levels of parenting stress reported by substance using women has also accounted for parental aggression, neglect, poor limit setting and involvement, and failures to foster autonomy (see Harmer, Sanderson, & Mertin, 1999; Kelley, 1992, Kelley, 1998; Suchman & Luthar, 2001).
The impact of chronic drug use on stress regulation heightens vulnerability to parental malfunction by altering neurobiological hedonic reward systems that ordinarily assist with adaptation to stress (see Sinha, 2001; Volkow, Fowler, & Wang, 2003). The continuing presence of addictive substances drastically reduces this dopaminergic response to stress, leaving the addicted adult highly vulnerable to negative emotions and an absence of pleasure or reward ordinarily associated with caring for young children.
Evidence for attachment-based interventions with at-risk mothers of young children
Although our investigative team is among the first to introduce an attachment-based intervention for mothers with substance use disorders (see also Cassidy, Ziv, Stupica, Sherman, Butler, et al., 2010; Jenkins & Williams, 2008), evidence from intervention studies with high-risk non-substance-using parents have shown that this approach holds considerable promise, especially when maternal representations and reflective functioning are targeted. For example, in an ongoing evaluation of a home-visit parenting program targeting improvement in reflective functioning in at risk mothers of infants, improvements in reflective functioning have been reported at 12 and 18 month time points. At 24 months, only 8% of the children in the sample showed disorganized patterns of attachment (see Sadler, Slade, & Mayes, 2006; Slade, Sadler, Miller, & Ueng-McHale, 2009). Studies of attachment-based parenting interventions with at-risk mothers (including the Circle of Security and Watch, Wait, and Wonder) have shown that mental representations of caregiving and child attachment classification can change in response to intervention (Cohen, Muir, Lojkasek, Muir, Parker, Barwick, & Brown, 1999; Hoffman, Marvin, Cooper, & Powell, 2006; Toth, Rogosch, Manly, & Cicchetti, 2006).
The MTP Intervention
MTP is a 12-week individual psychotherapy intervention designed as an adjunct to outpatient substance abuse treatment. Mothers meet weekly with an individual clinician for one hour. Prior to the first therapy session, mothers complete a baseline assessment that includes measures of reflective functioning in the Parent Development Interview (Slade, Aber, Berger, Bresgi, & Kaplan, 2002), working model of the child in the Working Model of the Child Interview (Zeanah & Benoit, 1993), psychiatric symptoms and substance use. Mothers and children also complete a brief, videotaped, structured interaction to assess maternal sensitivity and responsiveness to child cues and child responsiveness to the mother (in the randomized pilot, these assessment procedures were used for both treatment conditions).
Developmental progression
MTP follows a developmental progression based on the theoretical mechanisms of attachment. The progression begins with a focus on building the therapeutic alliance to promote the mother's sense of being assisted and understood by the therapist. During an introductory meeting, the therapist explains that the purpose of the program is to support the mother in her role as parent so that her parenting experience can be more pleasurable and less stressful. The therapist explains her role to help the mother develop a better understanding of how these stresses impact her relationship with her child. The therapist also explains the limitations of her availability and that mothers may contact the program staff between sessions for additional assistance (i.e., crisis management).The therapist briefly explains that the program is grounded in attachment theory and introduces the central tenets that parent actions are strongly influenced by thoughts and feelings, and that children's actions are best understood by thinking about underlying thoughts, emotions and intentions. The therapist is attuned to the relationship and encourages the mother's efforts to openly discuss her concerns. The circumstances of everyday life (e.g., loss of housing, food, transportation and financial support) can be unstable at times and mothers often arrive at the clinic in the midst of a crisis. The therapist assists the mother with basic needs (e.g., food, shelter, child care, health and employment) when asked and offers strategies for coping with stress in order to demonstrate her willingness to be a helpful ally.
The central therapeutic work begins where the mother is, psychologically. For example, if a mother appears overwhelmed by her relationship with her welfare worker, the therapist first assists with sorting out the facts and inviting the mother to make sense of her strong feelings. In this way, mentalization is used as a tool to restore the mother's sense of calmness before the focus shifts to the child. The therapist works to maintain a mentalizing stance toward the mother and child, conveying that each situation is best understood by making sense of the thoughts, wishes, intentions, and emotions underlying behavior (Fonagy et al., 2002). The therapist also encourages the mother to explore her own representations of herself and others (e.g., the child) to further identify personal meanings and misrepresentations. For example, if a mother says “I am a bad mother – I don’t know how to take care of my baby” the therapist asks if this attribution might help preempt the criticism of others or make sense of an overwhelming sense of guilt.
Mentalizing about behavior during therapy involves identifyiing underlying affective states (e.g., what was it like for you when your partner refused to help you with childcare) as well as how affective states influence behavior (e.g., do you think your frustration with your partner might have made it harder to get to work on time?) and relationships (e.g., Do you think your partner might have sensed your frustration and become even more hostile?). Mothers may at times resist the invitation to think about underlying mental states wondering aloud about the usefulness of focusing on thoughts rather than actions. In such instances, the therapist follows the mother's lead but will also attempt to revisit the value of mentalization as a tool for managing stress. When the mother is no longer preoccupied with a specific crisis, the therapist asks her to consider the impact of the situation on the child.
The purpose of exploring the mother's internal working model of her child and their relationship is to identify distorted or denied aspects of her mental representations and promote a shift toward greater emotional balance, sensitivity and flexibility in the representations. For example, if a mother is preoccupied about a single aspect of the child's personality (e.g., temper or stubbornness), the therapist will invite her to explore this perception in greater detail in order to understand its meaning, origins and its limits. Similarly, if a mother seems to have limited awareness of her child's emotional experiences, the therapist will invite her to consider what these underlying emotions might be and why they might be hard to access. The goal here is to support the mother in becoming more emotionally engaged and more fully aware of her child's emotional experiences and needs.
In focusing on the child, the therapist adopts a mentalizing stance similar to the stance she adopts for exploring the mother's behavior. That is, she speaks to the mother about the child as though the best way to understand the child's behavior is by considering the intentions, wishes and emotions that may be driving the child's behavior (Fonagy et al., 2002). This approach initially involves simple consideration of the child's affective states (e.g., how do you think he might have felt when you told him he couldn’t come with you to the store). It then progress to considering how the child's affective states influence his behavior (e.g., do you think he was crying because he wanted more time with you?), or relationships (e.g., I wonder if he sensed your frustration and then became overwhelmed). A number of techniques are used to bring the child's emotional needs to the mother's attention. Videotaped play sessions involving the mother and child are viewed to make retrospective inferences about underlying wishes, intentions and emotions during live interactions. The therapist preselects specific moments when the mother and child were emotionally in sync (or out of sync) with one another and encourages the mother to reflect on states of mind. This process helps to reinforce the separateness of minds and experience and the distinction between intrapersonal and interpersonal reality (Fonagy et al., 2002). Because substance using mothers often lack information about their child's developmental capacities at different ages, the therapist provides timely attachment-based developmental guidance to aid the mother's understanding and anticipating the child's behavior. There are also frequent opportunities to observe the mother and child together before or after therapy sessions. The therapist may mentalize or “speak for the child” in the mother's presence, suggesting to the mother what the child might be thinking or feeling at a given moment (e.g., “Mommy, where did you go? I was worried you wouldn’t come back”).
Given the 12-session limit, mothers do not always complete each stage of therapy. For some mothers, particularly those with longstanding interpersonal difficulties that make it difficult to trust treatment providers, engage fully in therapy, or focus on the child, treatment throughout the 12 sessions may focus solely on establishing a secure therapeutic alliance and supporting the mother's growing capacity for self-regulation. In these instances, the mother-child relationship is still expected to incur some, albeit more modest, benefit. The manual serves as a roadmap for the overall approach and progression through stages and provides guidance about specific strategies and techniques. Nonetheless, each mother's course of treatment is, inevitably, unique.
Randomized pilot study
Overview
The goals of the Stage I Therapy Development Study were to complete a draft of the MTP therapist manual, develop and pilot treatment fidelity/discrimination scales, and conduct a small randomized pilot to test the feasibility, acceptability, and preliminary efficacy of MTP and explore proposed mechanisms of change. In the randomized pilot, mothers received 12 sessions of MTP or Parent Education (PE), a comparison intervention providing individual case management and child development brochures. Both interventions involved weekly one-hour meetings with a counselor in conjunction with standard care at the substance use clinic.
Primary targeted outcomes included maternal reflective functioning and representations of the child. Secondary targeted outcomes included caregiving behavior, psychiatric distress and substance use. Child behavior during interaction sessions was also examined. Parenting assessments were completed at baseline, post-treatment, and 6-week follow up, psychiatric questionnaires at monthly intervals, and urine toxicology screens at weekly intervals.
A second objective was to examine proposed mechanisms of change in the MTP model. Using the MTP Treatment Fidelity Rating Scales we examined whether (1) higher levels of therapist adherence to the MTP model predicted greater improvement in primary targeted outcomes (reflective functioning and representation quality), and (2) improvement in primary outcomes led to improvement in maternal caregiving behavior.
Recruitment, informed consent and randomization
All mothers enrolled in outpatient substance use treatment and caring for a child between birth and 36 months of age were eligible to participate. Mothers who were actively suicidal, homicidal, severely cognitively impaired, disengaged from their substance use treatment or not fluent in English were excluded from participating. Mothers were recruited via clinician referrals, research staff visits to clinic groups and medication lines, and self-referral and screened for eligibility by a research trained research assistant. Eligible mothers met with the research coordinator during the same week to complete informed consent procedures during which mothers were informed that, after completing a baseline assessment, they would be randomly assigned to one of two parenting programs designed to assist them in managing parenting stress. Mothers were asked permission to access their clinic attendance records and utox results over the course of the study. A certificate of confidentiality was obtained to protect the confidentiality of all research records.
Sample
Of 56 mothers who consented to participate, 47 completed baseline measures and were randomized to treatment (23 MTP, 24 PE) (see demographic and psychiatric sample characteristics in Table 1). No significant demographic or psychiatric group differences (MTP vs. PE) occurred at baseline except for marital status; more mothers in the PE condition were single.
Table 1.
Sample Characteristics, (n = 47)
| Demographic characteristics | MTP (n = 23) Mean (SD) | PE (n = 24) Mean (SD) | t |
|---|---|---|---|
| Mother's age | 31.43 (6.46) | 28.88 (6.50) | -1.35 |
| Years of maternal education | 12.13 (1.18) | 12.54 (1.44) | 1.07 |
| Number of children | 2.30 (1.52) | 1.88 (.95) | -1.17 |
| Child age (months) | 18.74 (16.94) | 16.67 (10.27) | -.51 |
|
X2
|
|||
| % Minority | 22% | 38% | 1.40 |
| % Single | 43% | 83% | 8.08** |
| % Unemployed | 87% | 75% | 1.08 |
| % Methadone-medicated | 71% | 65% | .17 |
| % DCF-Involved | 61% | 58% | .03 |
| Child gender (% male) | 61% | 42% | 1.73 |
| Primary Substance Use Disorder | X2 | ||
| | |||
| Opiate | 74% | 71% | 5.48 |
| Cocaine | 13% | 21% | |
| Alcohol | 13% | 0% | |
| Cannabis | 0% | 8% | |
| Psychiatric Status | |||
| | |||
| Moderate depression | 30% | 33% | .05 |
| Moderate psychiatric distress | 48% | 62% | 1.02 |
|
t
|
|||
| Lifetime trauma exposurea | 3.22 (1.86) | 3.67 (2.14) | .77 |
| PTSD Symptoms | 2.32 (1.49) | 2.38 (1.31) | .14 |
p < .01 (two-tailed)
Total number of trauma exposure types (e.g., miscarriage, sudden loss, physical and sexual trauma).
MTP therapist training
MTP therapists were selected based on their clinical experience working with similar populations and willingness/ability to adopt a reflective stance with the patients. Four therapists - two masters- and two doctoral-level - provided MTP treatment. Each received extensive training in the treatment model prior to the study and weekly supervision from the Principal Investigator (N.S.) throughout the study. The MTP clinical team met bi-monthly with a co-investigator (L.M.) to review tapes of mother-child interactions. MTP therapists also received ongoing feedback on treatment fidelity from independent raters.
Parent Education (PE) – Comparison intervention
The comparison intervention was designed to match MTP on time spent with the counselor and maternal expectations for help with parenting. PE counselors helped mothers get connected to services (e.g. medical and pediatric care, child care and child guidance services, housing assistance, transportation, vocational training), and solve problems of daily living (e.g., organization and planning, managing conflicts with partner, family, drug counselor, and DCF worker) and make parenting-related decisions. PE mothers also received a pamphlet each week on a parenting topic of their choice. Pamphlets focused on common issues in caring for infants (e.g., soothing a crying baby, managing bedtime routines, and establishing routines and rituals) and toddlers (e.g., helping toddlers dress, managing bedtime battles, managing difficult behavior in public, and setting limits without using punishment). Pamphlets provided behavioral guidance at a 5th grade reading level without reference to underlying mental states or emotional needs.
Outpatient substance use treatment
As part of their ongoing substance use treatment, mothers had access to group cognitive-behavioral therapy, psychiatric services, substance replacement therapy (e.g., methadone, naltrexone and antibuse), medical care, vocational counseling, child care, transportation to the clinic and ongoing assistance with basic needs (e.g., housing, education, food, child care, legal aid, state and city welfare, and other entitlements). Treatment at the outpatient clinic was paid for by patients’ individual insurance or by the patients themselves (with payments based on a sliding fee scale).
Treatment outcome measures
Psychosocial evaluation
Mothers completed a 1.5 hour structured interview conducted by a trained research assistant during the baseline visit. The interview asks about family demographic information, developmental history, substance use and psychiatric history (including during pregnancy), family substance use and psychiatric history, medical history, legal involvement, employment history and reasons for seeking help with parenting. Information from this interview was used to establish primary substance use and psychiatric diagnoses and to identify baseline demographic and psychosocial characteristics of the sample.
Reflective Functioning
The Parent Development Interview (PDI; Slade et al., 2002) was used to measure the mother's capacity to mentalize about her own and her child's behavior. The PDI is a 1 hour semi-structured interview containing 17 questions designed to elicit narratives about commonly occurring, emotionally-challenging aspects of parenting (e.g., times when parent and her child were not getting along, when parent felt angry or guilty or when child needed attention). The interview includes specific probes about the mother's and child's internal experiences and how they might affect the relationship. The interview was digitally recorded, transcribed and then coded by a Ph.D. psychologist trained to reliability by the PI (e.g., interclass correlations ≥ .50 for each item on 15 independently rated protocols). The coder remained blind to treatment assignment and all other information about mother-child dyads. Responses on each of the 17 questions were rated on a 10-point scale representing the level of reflective functioning exhibited. (Coding methods were originally developed by Fonagy and colleagues [1998] for use with the Adult Attachment Interview [Main & Goldwyn, 1995] and then adapted for the PDI by Slade and colleagues [2005]). Ratings of 1 indicate absence of any recognition of mental states (i.e., events are described solely in terms of behavior and individuals solely in terms of global personality traits). Ratings of 3 indicate limited capacities to acknowledge mental states and absence of understanding about how mental states function. Ratings of 5 indicate presence of a rudimentary capacity for reflective functioning – basic understanding of how mental states work together and influence behavior. Ratings above 5 indicate increasingly elaborate and sophisticated understanding of how mental states function and influence behavior. The mean score for the 17 items was used to measure the mother's overall RF. Because it was expected that overall mean values would be low, highest RF levels were also examined and considered the best indication of the mother's capabilities. Likewise, low levels (below 3) were examined as indications of risk for child maltreatment.
Mental representations of the child
The Working Model of the Child Interview (WMCI; Zeanah & Benoit, 1993) was used to assess quality of the maternal representations of the child. The WMCI is a 1.5 hour semi-structured interview was designed to elicit a narrative of caregivers’ perceptions of their child and the caregiving relationship in parents caring for children from birth to 5 years of age. The interview includes questions about parent perceptions of the child's distinctive characteristics, characteristics of the relationship, and times when the child's attachment needs were likely to be activated (e.g., times when the child was upset, physically or emotionally hurt or separated from the mother). Specific probes (e.g., when is the last time that happened?) insure that the narrative is adequate for coding.
The interview was digitally recorded and then coded by a Ph.D. psychologist who was trained to reliability by the PI (interclass correlations ≥ .50 for items on 15 independently rated protocols) and was blind to treatment assignments and all other information and assessments about mother-child dyads. The three-part classification system ordinarily used with this instrument (Zeanah & Benoit, 1993) did not have the sensitivity necessary to detect small but meaningful shifts in representational quality. Protocols were therefore coded on five qualitative domains using a 5 – point scale (1 = not at all, 3 = moderate, 5 = extreme) that together represent the most important representational qualities (Zeanah & Benoit, 1993). These domains include: Openness (acceptance and flexibility in expectations for the child over time), Coherence (clarity and credibility of narrative), Caregiving Sensitivity (recognition and responsiveness to child's emotional distress), Acceptance (acknowledgement of parental role and responsibility and child's dependence on parent for safety and care) and Involvement (emotional investment versus indifference toward the relationship). On each scale, scores of three are considered average, scores lower than 3 represent clinical risk and scores above 3 represent optimal quality. Interclass correlations ranged ranged from .50 to .60.
Caregiving behavior
The Nursing Child Assessment Satellite Training (NCAST; Barnard & Eyres, 1979) interaction assessment is a widely-used, standardized, 73 binary-item tool used to observe and rate quality of caregiver-child interactions with children ages birth to 36 months. Mothers are asked to choose one task to teach the child (e.g., stringing beads, drawing shapes, etc.) from a list of tasks organized in increasing order of difficulty. The teaching session lasts 5 minutes. Teaching sessions were digitally recorded using remotely controlled cameras that captured views of mother and child on a split screen. Sessions were coded by a certified NCAST rater trained according to NCAST requirements to 80% reliability by the Project Director (a NCAST-certified instructor) and blind to treatment assignment and all other information about the mother-child dyads. Maternal behavior is coded on four behavioral dimensions (e.g., sensitivity to child cues, responsiveness to the child distress, social-emotional growth fostering and cognitive growth fostering) that are then summed to comprise the Total Caregiver Score. The Total Contingency Score is derived by summing items requiring caregiver contingent response to child cues. (Each total score was compared with NCAST norms).
Child behavior
Child behavior was assessed using the two child scales from the NCAST that respectively assess clarity of the child's cues and the child's efforts to engage the mother. The Child Total Score represents the sum of the two scales and the Child Contingency Score contains only those items requiring contingent response to the mother.
Maternal psychiatric symptoms
Although not primary targeted outcomes, group differences (MTP vs. PE) in depression and global psychiatric distress were examined to identify possible indirect treatment effects. The Beck Depression Inventory (BDI; Beck, Steer, & Brown, 1996) was used to assess maternal symptoms of depression. The BDI, a widely used 21-item questionnaire rated on a 4-point scale, yields a total score for depression ranging from 0 to 63, with scores of 13 - 19 indicating mild depression; 20 - 28 indicating moderate depression, and 29 - 63 indicating severe depression (Beck et al., 1996). The BDI has very good, well-documented psychometric properties including high internal consistency and construct validity (Beck et al., 1996). The composite Global Severity Index (GSI) from the Brief Symptom Inventory (BSI; Derogatis, 1993), a standardized, widely used, 90-item, 4-point, self-report measure, has demonstrated good reliability and validity (Derogatis, 1993). and was used to assess maternal global psychiatric distress. T scores above 60 on the GSI indicate risk for a clinical disorder.
Maternal drug use
Although maternal drug use was not a primary outcome, group differences (MTP vs. PE) were examined to identify possible indirect treatment effects. Substance use was monitored weekly using results from urine toxicology (UTOX) screens conducted at the clinics and testing for presence of opiate, cocaine, and cannabis metabolites. For each month of participation in the study, beginning with Month 0 (the month prior to consent) and continuing through the end of the post-treatment assessment (Month 8), a score of “0” was assigned if no drug metabolites were present in any screens or a score of “1” if one or more screens tested positive for any drug metabolite during the month. Mothers received a score of “0” or “1” for each month of enrollment in the study.
Treatment fidelity
The MTP Treatment Fidelity Scales (Suchman et al., 2006) were developed and piloted to measure therapist adherence to MTP and discrimination of MTP vs. PE. The initial 24-item binary scale contained six subscales (Table 2). Two scale developers (the Project Director (C.D.) and a Ph.D. psychologist) independently coded 37 videotaped sessions to test interrater reliability. Two items from the original scale were rarely endorsed and therefore omitted. Interclass correlations for the six subscales were adequate (≥ .50) and retained in the final measure (see Table 2).
Table 2.
Results of analyses examining interrater reliability, and MTP vs. PE treatment fidelity and discrimination
| Scale | Sample Item | Interrater Reliability (ICC) (n = 37) | Treatment Fidelity Mean (SD) | F statistic for group differences | |
|---|---|---|---|---|---|
| MTP (n = 190) | PE (n = 23) | ||||
| 1. Secure Alliance | “Therapist communicates acceptance of mother's point of view, event though it might be aberrant.” | .59 | .75 (.12) | .53 (.16) | 62.33*** |
| 2. Developmental Guidance | “Therapist provides developmental guidance from an attachment perspective.” | .84 | .35 (.35) | .04 (.15) | 16.79*** |
| 3. Emotional Regulation | “Therapist assists mother to contain or regulate strong negative emotions.” | .65 | .63 (.33) | .22 (.29) | 32.27*** |
| 4. Focus on internal working model | “Therapist encourages mother to explore representations of her child and their relationship.” | .50 | .38 (.34) | .00 (.00) | 27.44*** |
| 5. Metallization for self / other | “Therapist encourages mother to explore mental states underlying her own behavior.” | .64 | .42 (.36) | .02 (.07) | 28.74*** |
| 6. Metallization for child | “Therapist explains or encourages mother to explore mental states underlying her child's behavior.” | .78 | .39 (.31) | .07 (.31) | 29.53*** |
p < .001 (two-tailed)
Once the 22-item scale was finalized, the Ph.D. psychologist who was blind to information about the mothers rated 153 additional MTP sessions and 23 randomly selected PE sessions. Adherence ratings from 190 MTP and 23 PE sessions were then available for examining treatment fidelity and discrimination. For each session, the proportion of items endorsed on each subscale (see Table 2) was computed. These six proportions represent therapist fidelity to the six MTP treatment components. Because MTP consists of six components expected to be present sequentially (not simultaneously) across sessions, an average treatment fidelity score of .35 was considered acceptable for each component. As shown in Table 2, the mean treatment fidelity score for MTP therapists across the 190 sessions ranged from .35% (Developmental Guidance) to .75 (Secure Alliance) with a median score of .37. Treatment discrimination was assessed in one-way analyses of variance comparing MTP and PE scores for each component. As shown in Table 2, group mean scores differed significantly for all six components.
Data analysis
Treatment outcomes
All outcome analyses were conducted using data from the full intention-to-treat sample. Analyses of covariance were used to test for group differences (MTP vs. PE) in each of the parenting and psychiatric outcomes after controlling for baseline differences. Child age and gender, maternal education and marital status were also held constant in all analyses of parenting outcomes while maternal education and marital status were held constant in analyses of psychiatric outcomes. Repeated measures analyses of covariance were used to examine group differences in positive urine toxicology screens across time. Because the pilot sample of 47 is small and lacks sufficient power to detect statistical difference, we used effect size (d) to detect meaningful differences for all outcomes using criteria suggested by Cohen (1988) (i.e., .20 represents a small effect, .50 a moderate effect, and .80 a large effect).
Mechanisms of change in the treatment model
Mechanisms of change were tested in a series of standard linear regression analyses that controlled for child age. First, we examined whether therapist fidelity to the MTP model predicted primary targeted outcome scores (reflective functioning and representation quality) for MTP mothers at post-treatment. Second, we examined whether improvement in maternal reflective functioning and mental representations, respectively, corresponded to improvement in caregiving behavior. Third, we examined whether improvement in caregiving behavior corresponded to change in child behavior. To calculate the measurement of improvement (or decline) from baseline to post-treatment, we used the residual variance remaining after variance due to baseline scores was removed from post-treatment scores. This method provides a reliable estimate of change unaffected by correlations between pre- and post-treatment scores (see Cohen and Cohen, 1983, pp. 413-425). Medium effects (e.g., R2 = .06) were considered meaningful.
Results
Attendance
In each condition (MTP and PE), 72% of the mothers completed the intervention. MTP completers attended 72% of their scheduled therapy sessions and assessments and 82% of their scheduled appointments at the treatment clinic. PE completers attended 78% of their scheduled PE sessions and assessments and 86% of their scheduled appointments at the treatment clinic (group attendance differences were non-significant).
Treatment outcomes
Reflective functioning and representations
All treatment outcomes are shown in Table 3. At post-treatment, MTP mothers showed moderately higher mean RF scores than PE mothers. Highest and lowest RF scores were also moderately higher for MTP mothers. Two representation domains – Coherence and Caregiving Sensitivity – showed small differences favoring MTP mothers.
Table 3.
Results of ANCOVA for outcomes controlling for child age, child gender, maternal education, marital status, and baseline scores (n = 47)
| MTP (n = 23) | PE (n = 24) | ||||||
|---|---|---|---|---|---|---|---|
| | |||||||
| Pre | Post | Pre | Post | ||||
| | |||||||
| Raw | Adjusted | Raw | Adjusted | d | |||
| | |||||||
| Reflective Functioning | |||||||
| | |||||||
| Mean RF | 3.16 (.45) | 3.33 (.46) | 3.35 (.33) | 3.10 (.48) | 3.11 (.46) | 3.09 (.33) | .56* |
| Highest RF | 5.04 (.93) | 5.25 (.79) | 5.24 (.51) | 4.88 (.74) | 4.92 (.72) | 4.93 (.51) | .43* |
| Lowest RF | 1.30 (.64) | 1.85 (.81) | 1.94 (.65) | 1.63 (.65) | 1.67 (.48) | 1.58 (.65) | .39* |
| Quality of Representations | |||||||
| | |||||||
| Coherence | 2.62 (.54) | 2.67 (.45) | 2.70 (.54) | 2.44 (.60) | 2.54 (.59) | 2.51 (.54) | .25† |
| Sensitivity | 2.36 (.64) | 2.64 (.45) | 2.68 (.58) | 2.46 (.74) | 2.52 (.71) | 2.49 (.58) | .23† |
| Acceptance | 2.76 (.63) | 2.83 (.56) | 2.83 (.48) | 2.69 (.62) | 2.73 (.57) | 2.74 (.48) | .13 |
| Involvement | 2.98 (.59) | 2.83 (.54) | 2.95 (.61) | 3.17 (.89) | 3.17 (.83) | 3.06 (.61) | .13 |
| Openness | 2.88 (.56) | 2.94 (.45) | 2.91 (.53) | 2.96 (.62) | 2.94 (.71) | 2.97 (.53) | .08 |
| Caregiving Behavior | |||||||
| | |||||||
| Total score | 35.82 (3.76) | 38.00 (3.33) | 38.08 (3.17) | 36.04 (4.45) | 36.17 (3.61) | 36.09 (3.16) | .44* |
| Total contingency | 13.23 (2.54) | 14.71 (1.59) | 14.75 (1.93) | 13.17 (2.79) | 13.13 (2.25) | 13.09 (1.93) | .61* |
| Child Behavior | |||||||
| | |||||||
| Total score | 19.55 (2.50) | 19.45 (1.92) | 19.46 (2.14) | 18.88 (2.72) | 19.29 (2.61) | 19.28 (2.14) | .06 |
| Total contingency | 9.50 (1.67) | 9.42 (1.36) | 9.43 (1.70) | 8.96 (1.99) | 9.29 (1.94) | 9.28 (1.69) | .06 |
| Psychiatric Severity | |||||||
| | |||||||
| Depression | 14.91 (9.50) | 12.65 (8.42) | 13.32 (6.09) | 16.88 (9.33) | 16.79 (8.90) | 16.15 (6.07) | .33† |
| Global Distressa | 58.30 (10.99) | 57.05 (8.20) | 58.15 (6.05) | 61.54 (11.02) | 61.13 (10.52) | 60.07 (6.05) | .22† |
|
d
|
|||||||
| Substance Useb | Time | Tx × Time | |||||
| | |||||||
| 32% | 06% | n/a | 29% | 06% | .40* | .00 | |
small effect (d =.20)
moderate effect (d = .50) (Cohen, 1988)
Italicized scores represent T-Scores.
Results shown are time- and treatment × time effects for repeated measures analysis of variance.
Caregiving behavior
Total Caregiver and Contingency Scores were also moderately higher for MTP mothers than PE mothers. Compared with the NCAST national norms for Total Caregiving, (Mean = 56.13, SD = 8.88; Barnard & Ayres, 1979) MTP mothers scored approximately 2.25 SD's below the norm at baseline and 2 SD's below the norm at post-treatment. PE mothers scored approximately 2.25 SD's below the norm at both baseline and post-treatment. Compared with NCAST norms for Total Contingency (Mean = 16.09, SD = 3.64; Barnard & Ayres, 1979), MTP mothers scored 1 SD below the norm at baseline and .5 SD below the norm at post-treatment. PE mothers scored 1 SD below the norm at both baseline and post-treatment.
Child behavior
At post-treatment, there were no overall MTP vs PE differences in child behavior. At baseline, mean Total Scores for both groups fell approximately 1 SD above the NCAST national norm for children of mothers with a high school education (Mean = 15.44, SD = 4.29; Barnard & Ayres, 1979). Children's mean Total Contingency scores for both groups at baseline also fell approximately 1 SD above the NCAST national norm (Mean = 6.76, SD = 2.95 Barnard & Ayres, 1979).
Psychiatric symptoms and substance use
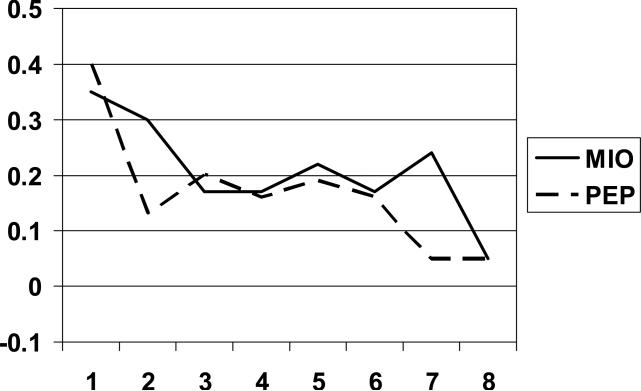
Small group differences in depression and psychiatric distress indicated that MTP mothers reported fewer symptoms at post-treatment. Both MTP and PE mothers showed moderate reduction in drug use at post-treatment (see Figure 1).
Figure 1.
Substance use during the first treatment phase.
Mechanisms of change
Treatment dose and primary outcomes
Large effects and beta weights indicate that therapist fidelity to the MTP model was associated with improvement in overall, highest, and lowest RF scores (see Table 5). A moderate and small effect, respectively, and corresponding beta weights indicate that therapist fidelity was also related to improvement in representational caregiving sensitivity and coherence.
Table 4.
Results of linear regression analyses testing MTP therapist adherence as a predictor of parenting outcomes after controlling for child age (n = 23)
Standardized beta weights
small effect (r2 =.01)
medium effect (r2 =.06)
large effect (r2 =.14), (Cohen, 1988)
Reflective functioning, representations and caregiving behavior
Improvement in RF corresponded to improvement in caregiving behavior (Total Caregiver and Contingency scores) as indicated by small-to-large effects and beta weights (see Table 6). Medium effects and beta weights also indicated associations between (a) representational coherence and Total Contingency and (b) representational caregiving sensitivity and Total Caregiving and Contingency scores.
Discussion
In this randomized pilot study, a preliminary test of the Mothers and Toddlers Program (MTP), an attachment-based parenting intervention for mothers in substance use treatment and caring for children between birth and 3 years of age was conducted and a treatment fidelity scale was developed to examine treatment integrity, discrimination and proposed mechanisms of change. MTP proved to be acceptable and feasible and showed preliminary promise for improving maternal reflective functioning, representations, and caregiving behavior. Preliminary evidence also confirmed treatment integrity, discrimination and proposed mechanisms of change.
Feasibility and acceptability
Difficulty engaging mothers in substance use treatment is a common problem across many programs (see Suchman et al., 2006). Given the potential assessment burden of this study (e.g., two attachment interviews and an observed interaction session), its feasibility and acceptability to the patients and the clinic were relatively high. The high completion rate may be explained by several factors: Mothers in both conditions had the opportunity to form a trusting relationship with an individual counselor and often commented about the support and comfort they experienced in the relationship. The research staff and clinicians also went to great lengths to insure that the program site was a comfortable and inviting space. Each interview room was repainted and furnished comfortably and the clinic child care room was renovated to include age-appropriate stations (e.g., toddler-size kitchen, furniture, cushions, tunnels and tent box mats for crawling) for interactive play. Drinks and snacks were available to mothers and children when they arrived. Common barriers to treatment were addressed by giving mothers taxi and bus vouchers, providing child care, and conducting the program on site where mothers were already enrolled in substance use treatment. Mothers who volunteered to participate were a self-selected motivated sample. Referring clinicians may have also been biased toward motivated mothers. Subject payments increased across time, providing further incentive to complete the study.
Treatment outcomes
Reflective functioning
At post-treatment, MTP mothers showed moderately better improvement in RF than PE mothers. Clinically, this finding suggests that MTP mothers were more able to mentalize for themselves and their children. The range of mentalization scores (e.g., the lowest and highest scores) was also higher for MTP than PE mothers suggesting that MTP mothers were able to achieve higher levels of mentalization and adopted a non-mentalizing stance less frequently. This boost in the low end of the RF spectrum for MTP mothers may be especially important for preventing emotional dysregulation and relapse.
Representation quality
At post-treatment, MTP mothers showed somewhat higher caregiving sensitivity and coherence in representations although the effect size for each finding was small. Increased coherence in representations suggests that MTP mothers were perceiving their children's characteristics with greater detail and clarity and were better able to understand their children's characteristics and behavior within a meaningful context. Increased caregiving sensitivity in representations suggests that MTP mothers were more able to recognize their children's emotional needs under duress (e.g., times when children were sick, injured or separated from the mother). These improvements were small and no improvements were found in other representation qualities (e.g., acceptance, involvement, or openness). It is possible that further representational shifts will be evident at the 6-week follow up after having a chance to consolidate.
Caregiving behavior
As predicted, higher levels of reflective functioning and representation quality in MTP mothers corresponded with better caregiving behavior at post-treatment. Previous randomized trials testing outpatient and home visit parenting interventions that directly target behavioral change in substance using mothers of young children have not generally shown marked improvement in caregiving behaviors (see, for example, Huebner, 2002; Black, Nair, Kight, Wachtel, Roby, & Schuler, 1004; Schuler, Nair, Black, & Kettinger, 2000; Schuler, Nair, & Black, 2002; for a review, see Suchman et al., 2006). In this study, even though it was not directly targeted in MTP, caregiving behavior was better among MTP mothers at post-treatment. Although preliminary, these findings support the general tenet of attachment theory that parenting behavior is, in part, a function of underlying intentions and expectations about the caregiving relationship that, upon changing, may also precipitate change in caregiving behavior.
Child behavior
Although child behavior was not a targeted outcome, clarity of children's cues and responsiveness to the mother were examined at post-treatment. No group differences were found in Children's Total or Contingency scores. It may be that children will show a delayed response to intervention at the 6-week follow up assessment after having had more time to adjust to improvements in the maternal caregiving.
Psychiatric symptoms and substance use
Although maternal psychiatric status was not directly targeted in the MTP intervention, depression and global psychiatric distress were examined for possible indirect effects given the emphasis of MTP on distorted representations and emotional regulatory processes. Small effects indicated that MTP mothers experienced slightly better outcomes for both depression and global psychiatric distress at the end of 12 sessions. Baseline levels of depression and psychiatric distress throughout the study represented moderate (but not severe) elevation, which may explain why effects were small. Maternal substance use was also not directly targeted in MTP but examined for possible indirect effects given expected associations between mentalization, emotional regulation and relapse (see Fonagy et al., 2002; Sinha, 2001). Both groups showed notable improvement in overall substance use over time. It is possible that concurrent enrollment in treatment for substance use promoted abstinence and prevented relapse for mothers in both groups in the study. Future analysis of follow up data will help identify possible group differences in sustained or delayed effects.
Mechanisms of change
A second overall objective of this study was to conduct preliminary examinations of proposed mechanisms of change in the MTP treatment model to determine if the treatment approach is working as predicted. Preliminary evidence indicated that therapist fidelity to the MTP treatment model led to greater improvement in maternal RF and representation quality in two domains (e.g., Coherence and Caregiving Sensitivity). There was also evidence that improvement in RF and the two representational domains was associated with improvement in caregiving behavior. Taken together, these findings provide preliminary support for the proposed mechanisms of change in the MTP treatment model. That is, the findings provide partial support for the premise that improvement in the mother's capacity to make inferences about intentions and emotions underlying her own and her child's behavior corresponds to improvement in her capacity to interact sensitively and contingently with her infant/toddler. As well, enhancement in the coherence and sensitivity of her representations of the child corresponds with improvement in her sensitivity and contingency during interactions. Causal inferences about these associations will need to be tested in future work as the concurrent assessment of change in these domains precludes any conclusions about temporal effects. It is plausible that changes in behavior preceded changes in RF and representations or that all changes occurred simultaneously. Future analysis of data from the second treatment and follow up phases will help clarify the temporal order of change mechanisms.
Conclusions
This study has demonstrated the preliminary feasibility and acceptability of MTP as an adjunct attachment-based intervention for mothers in substance use treatment as well as its potential promise for directly improving maternal reflective functioning and representation quality and indirectly improving caregiving behavior. A scale for measuring therapist fidelity was also successfully developed and found to predict improvement in one the two primary targeted domains – reflective functioning and representation quality. Finally preliminary support for proposed mechanisms of change was evident. Taken together, these findings have important implications for future intervention development for parents who have substance use disorders. Unlike previous intervention trials that have not demonstrated improvement in maternal caregiving behavior (see Suchman et al., 2004, 2006), the results of this pilot study suggest that caregiving behavior of mothers with substance use histories with their very young children can improve when maternal attachment vulnerabilities are directly targeted in individual therapy, even in a relatively short-term intervention. Moreover, this intervention format was easily adapted (and well-received) as an adjunct treatment to standard outpatient substance use services where mothers typically enroll in treatment for an average of 12 weeks. These findings demonstrate the feasibility of addressing parenting deficits and substance abuse simultaneously (rather than solely targeting abstinence).
It will be important to know if these benefits were sustained and if any delayed benefits – in other aspects of representations or child behavior – are evident at the 6-week follow up (these data will be reported in a forthcoming publication, see Suchman, DeCoste, McMahon, Rounsaville, & Mayes, 2010). It is also important, at this early stage of treatment development, not to over-generalize or over-interpret the efficacy of MTP as findings from this small trial may be difficult to replicate. A larger, formal randomized clinical trial with sufficient power to detect statistically significant findings and with a longer follow up period is the next step toward determining the efficacy of this promising intervention.
Table 5.
Results of linear regression analyses testing improvement in reflective functioning and representation quality as predictors of improvement in caregiving behavior in MTP mothers after controlling for child age (n = 23)
| Total Caregiving | Total Contingency | |||
|---|---|---|---|---|
| | ||||
| R2 Δ | ß a | R2 Δ | ß a | |
| Reflective functioning | ||||
| Mean RF | .04* | .20 | .01† | .12 |
| Highest RF | .16** | .40 | .16** | .39 |
| Lowest RF | .11** | .36 | .07* | .29 |
Standardized beta weights
small effect (r2 =.01)
medium effect (r2 =.06)
large effect (r2 =.14), (Cohen, 1988)
Acknowledgments
Preparation of the manuscript was funded by grants from the National Institutes of Health (R01DA017294, K02 DA023504). We wish to thank Arietta Slade, Carolyn Parler-McCrae, Julie Scott, Jessie Borelli, Daryn David, and the patients and staff of the APT Foundation for their contributions and support.
References
- Abidin RR. Parenting Stress Index: Professional Manual. 3rd ed. Psychological Assessment Resources; Odessa, FL: 1995. [Google Scholar]
- Allen JG, Fonagy P, Bateman AW. Mentalizing in clinical practice. American Psychiatric Publishing; Washington, DC: 2008. [Google Scholar]
- Barnard KE, Eyres SJ, editors. Child health assessment, Part 2: The first year of life. U.S. Government Printing Office; Washington, D.C.: 1979. (Publication Number DHEW No. HRA 79-25) [Google Scholar]
- Barrett AE, Turner RJ. Family structure and substance use problems in adolescence and early adulthood: examining explanations for the relationship. Addiction. 2006;101:109–120. doi: 10.1111/j.1360-0443.2005.01296.x. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of PErsonality & Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Burns KA, Chethik L, Burns WJ, Clark R. The early relationship of drug abusing mothers and their infants: An assessment at eight to twelve months of age. Journal of Clinical Psychology. 1997;53:279–287. doi: 10.1002/(sici)1097-4679(199704)53:3<279::aid-jclp11>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory Manual. 2nd ed. The Psychological Corporation; NY: 1996. [Google Scholar]
- Black MM, Nair P, Kight C, Wachtel R, Roby P, Schuler M. Parenting and early development among children of drug-abusing women: Effects of home intervention. PEdiatrics. 1994;94:440–448. [PubMed] [Google Scholar]
- Cassidy J, Ziv Y, Stupica B, Sherman LJ, Butler H, Karfgin A, Cooper G, Hoffman KT, Powell B. An attachment perspective on incarcerated parents and their children. Attachment and Human Development. 12 in press. (XX-XX) [Google Scholar]
- Catalano RR, Gainey RR, Fleming CB, Haggerty KP, Johnson NO. An experimental intervention with families of substance abusers: One-year follow-up of the focus on families project. Addiction. 1999;94:241–254. doi: 10.1046/j.1360-0443.1999.9422418.x. [DOI] [PubMed] [Google Scholar]
- Catalano RR, Haggerty KP, Gainey RR, Hoppe MJ. Reducing parental risk factors for children's substance misuse: preliminary outcomes with opiate-addicted parents. Substance Use and Misuse. 1997;32:699–721. doi: 10.3109/10826089709039371. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Lawrence Erlbaum Associates; Hillsdale, NJ: 1988. [Google Scholar]
- Cohen J, Cohen P. Applied multiple regression / correlation analysis for the behavioral sciences. 2nd edition Lawrence Erlbaum Associates; Hillsdale, NJ: 1983. [Google Scholar]
- Cohen NJ, Muir E, Lojkasek M, Muir R, Parker CJ, Barwick M, Brown M. Watch, wait, and wonder: Testing the effectiveness of a new approach to mother-infant psychotherapy. Infant Mental Health Journal. 1999;20:429–451. [Google Scholar]
- Derogatis LR. Brief Symptom Inventory: Administration, scoring, and procedures manual. 3rd ed. National Computer Systems; Minneapolis, MN: 1993. [Google Scholar]
- Department of Health and Human Services Blending PErsPEctives and building common ground: a report to congress on substance abuse and child protection. Apr, 1999.
- Egeland B, Weinfield NS, Bosquet M, Cheng VK. Remembering, repeating, and working through: Lessons from attachment-based interventions. In: Osofsky JD, Fitzgerald HE, editors. WAIMH Handbook of infant mental health: Vol. 4. Infant mental health in groups at high risk. John Wiley & Sons, Inc.; NY: 2000. pp. 38–89. [Google Scholar]
- Feldman R. Coding Interactive Behavior (CIB) manual. Bar-Ilan University; Ramat Gan, Israel: 1998. Unpublished manual. [Google Scholar]
- Fonagy P, Gergely G, Jurist E, Target M. Affect regulation, mentalization, and the development of the self. Other Press LLC; New York: 2002. [Google Scholar]
- Fonagy P, Target P, Steele H, Steele M. Reflective functioning manual: Version 5. University College London; 1998. Unpublished manuscript. [Google Scholar]
- Gibbons RD, Hedeker D, Elkin I, Waternaux C, Craemer H, Greenhouse J, Shea T, Imber S, Sotsky S, Watkins J. Some conceptual and statistical issues in analysis of longitudinal psychiatric data. Archives of General Psychiatry. 1993;50:739–750. doi: 10.1001/archpsyc.1993.01820210073009. [DOI] [PubMed] [Google Scholar]
- Grienenberger J, Kelly K, Slade A. Maternal reflective functioning, mother–infant affective communication, and infant attachment: Exploring the link between mental states and observed caregiving behavior in the intergenerational transmission of attachment. Attachment and Human Development. 2005;7:299–311. doi: 10.1080/14616730500245963. [DOI] [PubMed] [Google Scholar]
- Hans LL, Bernstein VJ, Henson LG. The role of psychopathology in the parenting of drug-dependent women. Development & Psychopathology. 1999;11:957–977. doi: 10.1017/s0954579499002400. [DOI] [PubMed] [Google Scholar]
- Harmer ALM, Sanderson J, Mertin P. Influence of negative childhood experiences on psychological functioning, social support, and parenting for mothers recovering from addiction. Child Abuse and Neglect. 1999;23:421–433. doi: 10.1016/s0145-2134(99)00020-4. [DOI] [PubMed] [Google Scholar]
- Hoff-Ginsberg E, Tardif T. Socioeconomic status and parenting. In: Bornstein M, editor. Handbook of parenting: Vol. 2. Biology and ecology of parenting. Lawrence Erlbaum Associates, Inc.; Mahwah, N.J.: 1995. pp. 161–188. [Google Scholar]
- Hoffman KT, Marvin RS, Cooper G, Powell B. Changing toddlers’ and preschoolers’ attachment classifications: the Circle of Security Intervention. Journal of Consulting and Clinical Psychology. 2006;74:1017–1026. doi: 10.1037/0022-006X.74.6.1017. [DOI] [PubMed] [Google Scholar]
- Howard J, Beckwith L. Rahdert ER, editor. Issues in subject recruitment and retention with pregnant and parenting substance-abusing women. Treatment for drug-exposed women and children: Advances in research methodology. 1996:68–86. NIDA Research Monograph 165. [PubMed] [Google Scholar]
- Hsieh FY. SSIZE: A sample size program for clinical and epidemiological studies [Computer program] Anaquest/BOC Health Care; Murray Hill, NJ: 1991. [Google Scholar]
- Huebner CE. Evaluation of a clinic-based parent education program to reduce the risk of infant and toddler maltreatment. Public Health Nursing. 2002;19:377–389. doi: 10.1046/j.1525-1446.2002.19507.x. [DOI] [PubMed] [Google Scholar]
- Jenkins C, Williams A. The mother-baby prenatal group: Nurturing reflective functioning in a methadone-maintenance clinic. Journal of Prenatal and Perinatal Psychology and Health. 2008;22:163–180. [Google Scholar]
- Kelley SJ. Parenting stress and child maltreatment in drug-exposed children. Child Abuse and Neglect. 1992;16:317–328. doi: 10.1016/0145-2134(92)90042-p. [DOI] [PubMed] [Google Scholar]
- Kelley SJ. Stress and coping behaviors of substance-abusing mothers. Journal of the Society of Pediatric Nurses. 1998;3:103–110. doi: 10.1111/j.1744-6155.1998.tb00215.x. [DOI] [PubMed] [Google Scholar]
- Kerwin ML. Collaboration between Child Welfare and Substance-Abuse Fields: Combined Treatment Programs for Mothers. Journal of Pediatric Psychology. 2005;30:581–597. doi: 10.1093/jpepsy/jsi045. [DOI] [PubMed] [Google Scholar]
- Levy DW, Truman S. Reflective functioning as mediator between drug use, parenting stress, and child behavior.. Paper presented at the College on Problems of Drug Dependence Annual Meeting; Quebec City, Quebec. June, 2002. [Google Scholar]
- Lewis RA, Haller DL, Branch D, Ingersoll KS. Retention issues involving drug-abusing women in treatment research. In: Rahdert ER, editor. Treatment for drug-exposed women and children: Advances in research methodology. 1996. pp. 110–122. NIDA Research Monograph 165. [PubMed] [Google Scholar]
- Luthar SS, Suchman NE. Relational Psychotherapy Mothers’ Group: A developmentally informed intervention for at-risk mothers. Development & Psychopathology. 2000;12:235–253. doi: 10.1017/s0954579400002078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, Suchman NE, Altomare M. Relational Psychotherapy Mothers Group: A randomized clinical trial for substance abusing mothers. Development and Psychopathology. 2007;19:243–262. doi: 10.1017/S0954579407070137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthar SS, Walsh KG. Treatment needs of drug-addicted mothers: Integrated parenting psychotherapy interventions. Journal of Substance Abuse Treatment. 1995;12:341–348. doi: 10.1016/0740-5472(95)02010-1. [DOI] [PubMed] [Google Scholar]
- MacPhee D. Knowledge of Infant Development Inventory: Survey of child care exPEriences manual. University of North Carolina; Chapel Hill: 2002. Unpublished manuscript. [Google Scholar]
- Main M, Goldwyn R. Adult attachment classification system. In: Main M, editor. Behavior and the Development of Representational Models of Attachment: Five Methods of Assessment. Cambridge University Press; 1995. [Google Scholar]
- Mayes LC, Carter AS, Stubbe D. Individual differences in exploratory behavior in the second year of life. Infant Behavior and Development. 1993;16:269–284. [Google Scholar]
- Mayes L, Truman S. Substance abuse and parenting. In: Bornstein M, editor. Handbook of parenting: Vol. 4. Social conditions and applied parenting. 2nd ed. Lawrence Erlbaum Associates; Mahwah, NJ: 2002. pp. 329–359. [Google Scholar]
- Murphy S, Rosenbaum M. Pregnant women on drugs: Combating stereotyPEs and stigma. Rutgers University Press; New Brunswick, NJ: 1999. [Google Scholar]
- McDevitt SC, Carey WB. Stability of ratings vs. perceptions of temperament from early infancy to 1-3 years. American Journal of Orthopsychiatry. 1981;51:342–345. doi: 10.1111/j.1939-0025.1981.tb01379.x. [DOI] [PubMed] [Google Scholar]
- Moore J, Finkelstein N. Parenting services for families affected by substance abuse. Child Welfare. 2001;80:221–238. [PubMed] [Google Scholar]
- National Center on Addiction and Substance Abuse . Women under the influence. Johns Hopkins University Press; Baltimore, MD: 2006. [Google Scholar]
- Nich C, Carroll KM. Now you see it, now you don't: A comparison of traditional versus random-effects regression models in the analysis of longitudinal follow-up data from a clinical trial. Journal of Consulting and Clinical Psychology. 1997;65:252–261. doi: 10.1037//0022-006x.65.2.252. [DOI] [PubMed] [Google Scholar]
- Parker G, Tupling H, Brown LB. A parental bonding instrument. British Journal of Medical Psychology. 1979;52:1–10. [Google Scholar]
- Rounsaville BJ, Carroll KM, Onken LS. A stage model of behavioral therapies research: Getting started and moving on from stage I. Clinical Psychology: Science and Practice. 2001;8:133–142. [Google Scholar]
- SAS Institute, Inc. The GLIMMIX Procedure, June 2006. SAS Institute; Gary, NC: 2006. [Google Scholar]
- Sadler LS, Slade A, Mayes LC. Minding the baby. In: J. G. A..en, Fonagy P, editors. A mentalization-based parenting program. Handbook of mentalization-based treatment. John Wiley & Sons; Hoboken, NJ: 2006. [Google Scholar]
- Schuler ME, Nair P, Black MM, Kettinger L. Mother-infant interaction: effects of a home intervention and ongoing maternal drug use. Journal of Clinical Child Psychology. 2000;29:424–431. doi: 10.1207/S15374424JCCP2903_13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuler ME, Nair P, Black MM. Ongoing maternal drug use, parenting attitudes, and a home intervention: Effects on mother-child interaction at 18 months. Journal of Developmental and Behavioral PEdiatrics. 2002;23:87–95. doi: 10.1097/00004703-200204000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. Oxford University Press; New York: 2003. [Google Scholar]
- Sinha R. How does stress increase risk of drug abuse and relapse? Psychopharmacologogy. 2001;158:343–359. doi: 10.1007/s002130100917. [DOI] [PubMed] [Google Scholar]
- Slade A. Parental reflective functioning: An introduction. Attachment and Human Development. 2005;7:269–281. doi: 10.1080/14616730500245906. [DOI] [PubMed] [Google Scholar]
- Slade A. Reflective parenting programs: Theory and development. Psychoanalytic Inquiry. 2006;26:640–657. [Google Scholar]
- Slade A, Aber JL, Berger B, Bresgi I, Kaplan M. The Parent Development Interview – Revised. Yale Child Study Center; 2002. Unpublished manuscript. [Google Scholar]
- Slade A, Bernbach E, Grienenberger J, Levy D, Locker A. Addendum to Reflective Functioning Scoring Manual For Use with the Parent Development Interview. City University; New York: 2005. Unpublished manuscript. [Google Scholar]
- Slade A, Grienenberger J, Bernbach E, Levy D, Locker A. Maternal reflective functioning, attachment, and the transmission gap: A preliminary study. Attachment and Human Development. 2005;7:283–298. doi: 10.1080/14616730500245880. [DOI] [PubMed] [Google Scholar]
- Slade A, Sadler L, Miller MR, Ueng-McHale J. Maternal reflective functioning as a moderator of intervention effects in predicting infant attachment.. Paper presented at the biennial meeting of the Society for Research in Child Development; Denver, CO. April, 2009. [Google Scholar]
- Spielberger CD. State-Trait Anger Expression Inventory: Professional Manual. Psychological Assessment Resources; Odessa, FL: 1996. [Google Scholar]
- Stout RL, Wirtz PW, Carbonari JP, Del Boca FK. Ensuring balanced distribution of prognostic factors in treatment outcome research. Journal of Studies on Alcohol, Suppl. 1994;12:70–75. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- Suchman NE. Weekly Checklist of Services (WCS) Yale University School of Medicine; New Haven, CT: 1998. Unpublished Document. [Google Scholar]
- Suchman N. The Mothers and Toddlers Program: An attachment-based intervention for mothers in substance abuse treatment.. Invited presentation to the National Abandoned Infants Assistance Resources Center Strengthening Connections Conference; San Francisco, CA. 3/14/08.2008. [Google Scholar]
- Suchman NE, DeCoste C, Castiglioni N, Legow N, Mayes L. The Mothers and Toddlers Program: Preliminary findings from an attachment-based parenting intervention for substance abusing mothers. Psychoanalytic Psychology. 2008;25:499–517. doi: 10.1037/0736-9735.25.3.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchman NE, DeCoste C, Mayes L. The Mothers and Toddlers Program: An attachment-based parenting intervention for mothers in substance abuse treatment. In: Zeanah C, editor. Handbook of infant mental health. 3rd. ed. Guilford Press; New York: in press. [Google Scholar]
- Suchman N, DeCoste C, N., McMahon T, Rounsaville B, Mayes L. The Mothers and Toddlers Program, an attachment-based parenting intervention for substance-using women: Results at 6-week follow up from a randomized clinical pilot. Infant Mental Health Journal. doi: 10.1002/imhj.20303. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchman NE, Leigh D, DeCoste C. Reflective functioning: Self- and child-mentalisation components. 2009. Manuscript in preparation.
- Suchman NE, Luthar SS. The mediating role of parenting stress in methadone-maintained mothers’ parenting. Parenting: Science and Practice. 2001;1:285–315. doi: 10.1207/s15327922par0104_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchman N, Mayes L. Breaking the cycle: Reflective functioning and maladaptive attachment cycles of drug-addicted mothers and their infants.. Invited poster presentation for the SRCD biennial meeting; Denver, CO. April 4, 2009.2009. [Google Scholar]
- Suchman NE, Mayes L, Conti J, Slade A, Rounsaville B. Rethinking parenting interventions for drug dependent mothers: From behavior management to fostering emotional bonds. Journal of Substance Abuse Treatment. 2004;27:179–185. doi: 10.1016/j.jsat.2004.06.008. [DOI] [PubMed] [Google Scholar]
- Suchman NE, McMahon TJ, Slade A, Luthar SS. How early bonding, depression, illicit drug use, and perceived support work together to influence drug-dependent mothers’ caregiving. American Journal of Orthopsychiatry. 2005;75:431–445. doi: 10.1037/0002-9432.75.3.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchman NE, McMahon T, Zhang H, Mayes L, Luthar S. Drug dependent mothers and disruptions in child custody: An attachment perspective. Journal of Substance Abuse Treatment. 2006;30:197–204. doi: 10.1016/j.jsat.2005.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchman NE, Pajulo M, DeCoste C, Mayes LC. Parenting interventions for drug dependent mothers and their young children: The case for an attachment-based approach. Family Relations. 2006;55:211–226. doi: 10.1111/j.1741-3729.2006.00371.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchman NE, Rosenberg P, DeCoste C. The Mothers and Toddlers Program: Therapist Adherence Scale and Coding Procedures Manual. Yale University School of Medicine; New Haven, CT: 2006. Unpublished Document. [Google Scholar]
- Toth SL, Rogosch FA, Manly JT, Cicchetti D. The efficacy of toddler-parent psychotherapy to reorganize attachment in the young offspring of mothers with major depressive disorder: A randomized preventive trial. Journal of Consulting and Clinical Psychology. 2006;74:1006–1016. doi: 10.1037/0022-006X.74.6.1006. [DOI] [PubMed] [Google Scholar]
- van IJzendoorn MH, Juffer F, Duyvesteyn MGC. Breaking the intergenerational cycle of insecure attachment: A review of the effects of attachment-based interventions on maternal sensitivity and infant security. Journal of Child Psychology & Psychiatry. 1995;36:225–248. doi: 10.1111/j.1469-7610.1995.tb01822.x. [DOI] [PubMed] [Google Scholar]
- van Zeijl J, Mesman J, van IJzendoorn MH, Bakersman-Kranenburg MJ, Juffer F, Stolk MN, Koot HM, Alink LRA. Attachment-based intervention for enhancing sensitive discipline in mothers of 1- to 3-year-old children at risk for externalizing behavior problems: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2006;74:994–1005. doi: 10.1037/0022-006X.74.6.994. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Fowler JS, Wang GJ. The addicted human brain: insights from imaging studies. The Journal of Clinical Investigation. 2003;111:1444–1451. doi: 10.1172/JCI18533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeanah CH, Benoit D. Clinical applications of a parent perception interview in infant mental health. Infant Psychiatry. 1993;3:539–554. [Google Scholar]