Abstract
Objective
Recent research has linked depression to cardiac mortality, and shown a high burden of persistent depressive symptomatology among cardiac patients. The objective of this study was to longitudinally examine the prevalence and course of depressive symptomatology among women and men for 1 year after a cardiac event, and the effect of cardiac rehabilitation (CR) on this trajectory.
Methods
Nine hundred thirteen unstable angina (UA) and myocardial infarction patients from 12 coronary care units were recruited, and follow-up data were collected at 6 and 12 months. Measures included CR participation, medication usage, and the Beck Depression Inventory (BDI). The longitudinal analysis was conducted using SAS PROC MIXED.
Results
At baseline there were 277 (31.3%) participants with elevated depressive symptomatology (BDI ≥ 10), 131 (25.2%) at 6 months, and 107 (21.7%) at 1 year. Overall, approximately 5% were taking an antidepressant medication, and 20% attended CR over their year of recovery. Participants with greater depressive symptomatology participated in significantly fewer CR exercise sessions (r = −0.19, p =.02), and minimal psychosocial interventions were offered. The longitudinal analysis revealed that all participants experienced reduced depressive symptomatology over their year of recovery (p =.04), and younger, UA participants with lower family income fared worst (ps < 0.001). CR did not have an effect on depressive symptomatology over time, but women who attended CR were significantly more depressed than men (p =.01).
Conclusion
Depressed cardiac patients are undertreated and their symptomatology persists for up to 6 months. CR programs require greater resources to ensure that depressed participants adhere to exercise regimens, and are screened and treated for their elevated symptomatology.
Keywords: cardiac event, depressive symptoms, longitudinal study, gender, cardiac rehabilitation
INTRODUCTION
Although depression has been implicated in the occurrence of coronary events, there also exists a strong association between depression and cardiac mortality in patients with established heart disease (1,2). Depressive symptoms and major depressive disorders are common in patients with acute coronary syndromes (ACS) (3,4). The prevalence of major depression ranges from 15% to 23% (5), which is approximately threefold higher than age-matched community-based prevalence studies (5,6). Recovery from major depression associated with ACS is extremely poor (1), with many patients remaining depressed 6 months later (7). Moreover, it is generally shown that women experience greater depressive symptomatology after a myocardial infarction (MI) than men (8), and that this symptomatology may more detrimentally affect women’s prognosis (9).
Several mechanisms elucidating the association between depression and ACS have been proposed, although the specific link remains unknown. One prominent mechanism links comorbid depression with reduced likelihood of adhering to recommended behavior changes such as increased exercise, medication adherence, and nutrition self-management (10–12). Until we resolve the question of whether treating depression improves cardiac prognosis (13,14), efforts should focus on enhancing adherence to these evidence-based cardiac therapies. Cardiac rehabilitation (CR) is an effective multifactorial program of structured exercise and evidence-based interventions to reduce risk, improve psychosocial well-being, and increase adherence to these behavior changes (15). Although exercise itself has lasting beneficial effects on depressive symptomatology and clinical depression (16), guidelines for comprehensive CR programs also promote screening and treating depression (or referring patients for treatment) (17). Unfortunately, CR is widely underutilized, particular among women (18), and even among those experiencing greater depressive symptomatology (19).
CR programs have been shown to be effective in reducing depression after a coronary event (20) among women (5,21). In one study, the prevalence of depression in women dropped from 23% to 12% after a comprehensive CR program (5). CR does not relate to decreased symptomatology for all participants, however, because one study reported that although just less than one half of participants experienced reduced depression, approximately one quarter became more depressed, and one third remained unchanged (22). Another study found that depression was improved only in the short-term after CR (23).
The relationship among gender, CR, and depression is clearly a complex one, and further prospective studies are needed. The objective of this study was to longitudinally examine the prevalence and course of depressive symptomatology among women and men for 1 year after ACS, and the effect of CR on this trajectory.
METHODS
Design and Procedure
This was a longitudinal observational study, following participants from admission for ACS, and assessing them at 6 months and 1 year later. Participants were recruited in the coronary care unit (CCU) by a research nurse on the second to fifth day of hospitalization. Inclusion criteria consisted of diagnosis with confirmed MI or unstable angina (UA), and being 18 years of age or older. Exclusion criteria were being medically unstable, and unable to read or speak English. Those who met study criteria and agreed to participate signed a consent form and were provided with a self-report questionnaire. Consent was also obtained to link participant’s self-report questionnaire data with their clinical data. Participants were followed up by mail at home 6 months and 1 year later and were asked to complete a self-report questionnaire with respect to depressive symptomatology and CR participation in the intervening 6 months.
Participants
Consecutive patients who were diagnosed with a MI or UA in 12 coronary care units (CCUs) across south central Ontario, Canada were approached for the study. Some participating hospitals were urban teaching hospitals (n = 206 participants; 22.6%), whereas others were community hospitals located in medium- and small-sized cities (n = 707 participants; 77.4%). Characteristics of participants (n = 913) and nonparticipants (n = 882) are shown in Table 1. Of the almost 1,800 patients approached, participants were significantly younger than those who refused or were ineligible to participate (t = −13.08, p <.001). Significantly more males agreed to participate than females (χ2 (1) = 14.00, p <.001), and more married and fewer widowed individuals agreed to participate (χ2 (1) = 21.46, p <.001).
TABLE 1.
Nurse-Reported Baseline Characteristics of Participants Versus Nonparticipants (Ineligible, Refused)
| Variable | Participant (%) (n = 913) | Nonparticipant (%)(n = 882) |
|---|---|---|
| Sex (% female) | 320 (35.0%) | 385 (43.7%)* |
| Marital status (% married) | 667 (73.1%) | 551 (62.5%)* |
| Diagnosis (% myocardial infarct) | 478 (52.4%) | 490 (55.6%) |
| Age (mean ± SD) | 61.89 (12.00) | 69.38 (12.25)* |
p <.001
Nine hundred thirteen patients (590 males, 323 females; 69% response rate) consented to participate in the study. Their ages ranged from 31 to 93 years with a mean age of 61.9 ± 12.00 years. Seventy-four percent of the participants (n = 664) were married, and 45% (n = 340) had a family income more than $50,000 CAD (ie, approximately $32,000 USD) annually. Fifty-three percent (n = 482) had a confirmed MI, and 47% (n = 424) were diagnosed as UA after appropriate diagnostic tests.
Five hundred forty-one patients participated in the study at 6 months, and 522 participated 1 year later; 55 had died, and 320 refused, could not be located, or were ineligible because of medical conditions (60% retention rate). Compared with nonparticipants at 1 year postischemic event, participants were more educated (χ2 = 4.04, p <.05), and older (t = 3.34, p =.001; Table 2). These differences were thus controlled for in our longitudinal analysis.
TABLE 2.
Baseline Characteristics of Participants at 1-Year Follow-up
| Variable | Retained (%) (n = 522) | Not Retained (%) (n = 391) |
|---|---|---|
| Sex (% female) | 171 (32.8%) | 141 (37.7%) |
| Marital status (% married) | 395 (75.7%) | 264 (67.5%) |
| Family income (%<50K CAD) | 242 (54.5%) | 180 (57.5%) |
| Education (% above high school) | 176 (34.4%) | 100 (27.9%)* |
| Site (% teaching hospital) | 116 (22.2%) | 84 (22.4%) |
| Killip class (% class >1) | 84 (17.0%) | 51 (14.5%) |
| Diagnosis (% myocardial infarct) | 293 (56.2%) | 186 (47.6%) |
| Age (mean ± SD) | 62.94 ± 10.90 | 60.26 ± 13.10* |
p <.05
Measures
The self-report surveys consisted of questions regarding sociodemographic characteristics, medical history, CR participation, medication usage, in addition to depression measures. The sociodemographic data included age, sex, marital status, education, and family income. CR participation was assessed at 6 months, by asking participants whether they had been referred and participated in a CR program (yes/no), and what types of psychosocial services were offered and utilized. At 12 months, participants were asked whether any healthcare provider had asked if they suffer from depression, and to check from a list the reasons they attribute for their depressive symptomatology (they were instructed to check all that apply). At 6 and 12 months, participants were asked to list all their current medications. These were scanned and antidepressant medications were coded. Survey data were linked with prospectively and contemporaneously collected clinical data compiled by CCU nurses. This included diagnosis, presentation profile (incorporating relevant medical history, and presenting problem), and Killip class (24).
Depressive symptoms were assessed longitudinally by the Beck Depression Inventory (BDI (25)), a reliable and well-validated 21-item scale using a forced-choice four-alternative response format that has been widely used in the general population, and in chronic illness populations including cardiac patients (26–30). Higher scores reflect greater depressive symptomatology. The internal consistency of the BDI was α = 0.87 at baseline, 0.88 at 6 months, and 0.87 at 1 year in the current sample.
Statistical Analyses
Data were cleaned and screened to evaluate statistical assumptions. Most statistical analyses were performed with SPSS 11.0, and the longitudinal analysis was performed with SAS v. 8.2. A descriptive examination of the variables was performed, and differences in CR utilization and treatments by depressive symptomatology were analyzed with χ2, t tests, and Pearson correlations as appropriate. Because of the right-skewness of the BDI scores, the longitudinal data analysis was performed on the logarithm of the scores. We choose the appropriate covariance structure using Akaike Information Criterion (AIC) for our longitudinal model. The residual assumptions (normality and equal variances) were checked after the model was fit to the data.
RESULTS
Differences in Participant Characteristics Based on Self-reported Depressive Symptomatology
Table 3 describes the participant characteristics based on depression scores at baseline, 6 months, and 1 year. As shown, there were significant differences for all variables in at least one time point.
TABLE 3.
Mean (SD) BDI Score Over Time Based on Participant Characteristics
| Variable | Baseline | 6 Months | 1 Year |
|---|---|---|---|
| Sex | |||
| Male | 7.59 (6.90) | 6.38 (6.38) | 5.91 (6.18) |
| Female | 10.72 (8.10)*** | 9.65 (8.78)*** | 8.25 (7.54)*** |
| Age (correlation) | −0.08* | −0.03 | −0.10* |
| Marital status | |||
| Married | 7.94 (6.72) | 6.73 (6.52) | 6.38 (6.33) |
| Other | 10.80 (9.04)*** | 9.60 (9.25)*** | 7.54 (7.80) |
| Education | |||
| High school or less | 9.02 (7.70) | 7.80 (7.61) | 6.95 (6.84) |
| Post-secondary education | 7.65 (6.74)* | 6.70 (6.97) | 6.02 (6.51) |
| Family income | |||
| < $50K per year | 9.29 (7.58) | 8.14 (8.01) | 7.66 (7.27) |
| >$50K per year | 7.45 (7.00)** | 6.12 (6.00)** | 5.75 (6.17)** |
| Killip classa | |||
| 1 | 8.32 (7.29) | 7.16 (7.31) | 6.45 (6.81) |
| 2, 3 or 4 | 10.56 (7.99)** | 8.30 (7.76) | 7.39 (6.49) |
| Diagnosisa | |||
| UA | 9.79 (7.67) | 8.83 (8.05) | 7.52 (7.28) |
| MI | 7.70 (7.19)*** | 6.27 (6.58)*** | 5.97 (6.18)* |
Nurse-recorded.
p <.05,
p <.01,
p <.001.
Prevalence, Incidence, Attribution, and Treatment of Depressive Symptomatology Over 1 Year Post-MI or UA
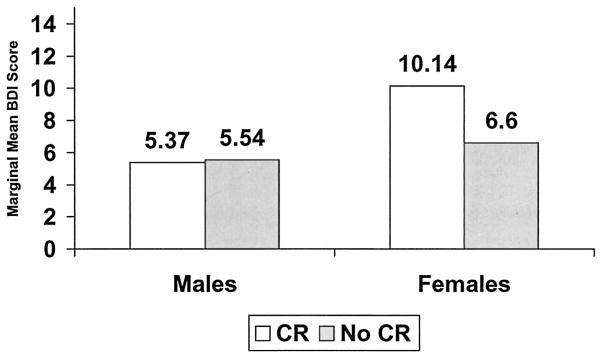
The mean (SD) BDI scores at baseline, 6 months, and 1 year were 8.68 (7.49), 7.43 (7.38), and 6.62 (6.70), respectively. Figure 1 displays the mean BDI scores over time based on sex and CR participation. We also computed a cut-off score for elevated depressive symptomatology (BDI ≥ 10), and at baseline there were 277 (31.3%) participants with elevated scores, 131 (25.2%) with elevated depression at 6 months, and 107 (21.7%) at 1 year. The mean baseline BDI score of participants with an elevated score at this time was 17.57 (6.76), the mean 6-month score in the elevated group was 17.49 (7.47), and at 1 year was 16.75 (6.71). Using the BDI severity categories, mean scores are presented in Figure 2.
Figure 1.
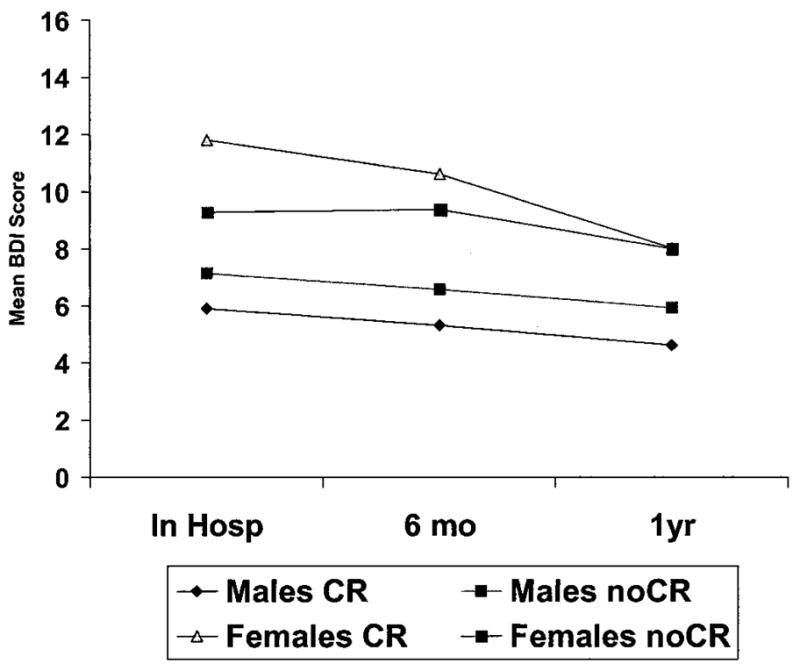
Mean BDI scores by time, sex, and CR participation.
Figure 2.
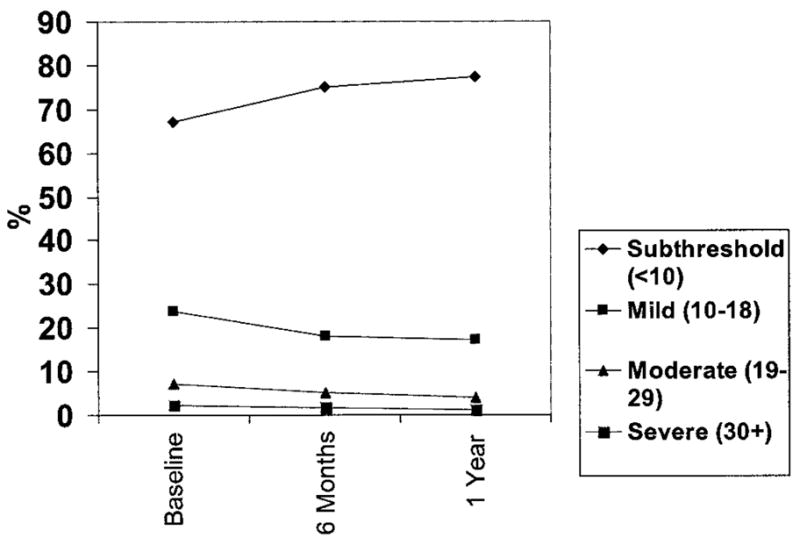
BDI depressive category by time.
Of the 31.3% participants with elevated depression at baseline, 62.2% of them continued to have elevated depression at 6 months, and 79.6% of those respondents continued to be depressed at 12-month follow-up. At 6-month follow-up, 12.3% of participants who did not have elevated depression at baseline had developed elevated symptoms. Of these, 57.1% persisted at 1 year. At 12-month follow-up there were 3.8% new participants with elevated depression who had not experienced depressive symptomatology earlier.
Participants were also asked what factors caused persistent feelings of depression or discouragement in the year after their ACS. The most frequent reason attributed was uncertainty about the future due to heart condition (n = 137; 27.3%), followed by knowledge of the heart condition (n = 122; 24.3%), reduced activity due to heart condition (n = 96; 19.1%), ongoing symptoms of heart condition (n = 70; 13.9%), comorbid conditions (n = 69; 13.7%), family problems unrelated to heart condition (n = 59; 11.8%), side effects of cardiac medications (n = 56, 11.2%), readmission to hospital for heart condition (n = 52; 10.4%), heart-healthy dietary changes (n = 50, 10.0%), work-related problems (n = 30, 6.0%), quitting smoking (n = 23, 4.6%; or 26.4% of current smokers), other challenging life changes (n = 23; 4.6%), lack of information provision by healthcare providers (n = 18; 3.6%), lack of help from family or friends with lifestyle changes (n = 15; 3.0%), and other factors (n = 11; 2.2%).
One hundred twenty (24.7%) participants reported that they had been asked by a healthcare provider over the past year whether or not they had been depressed. The most frequent healthcare providers to ask about depression were family physicians (n = 109, 79.0%), followed by cardiologists (n = 49, 35.5%), nurses in the CCU (n = 39, 28.3%), other physicians in the CCU (n = 20, 14.5%), or other healthcare providers (n = 19, 13.8%). Almost 70% (69.8%; n = 85) of participants who had an elevated depression score at baseline were not asked about depression by a healthcare provider by 1 year.
When asked at baseline whether a doctor had prescribed an antidepressant before or during their current admission, 4.6% responded affirmatively. At 6 months, participants were asked to list all their current medications. These were scanned and coded. Twenty-five (4.6%) reported taking an antidepressant. This increased to 30 (5.7%) participants listing an antidepressant at 1 year postevent (17 of these participants were taking an antidepressant at both 6 months and 1 year).
At 6 months, 149 (28.1%) participants had been referred to a CR program. There was no significant difference in physician referral pattern based on depressive symptomatology (t = 0.26, p =.80). Participants were also asked whether they attended a CR program, and 109 (21.6%) participants had. When asked how many CR sessions they attended on a scale from 1 (none) to 5 (all), the mean score was 3.40 (SD = 1.61). Participants with greater depressive symptomatology at 6 months participated in significantly fewer CR sessions than less depressed participants (r = −0.19, p =.02). Participants who attended CR were equally as likely to be taking an antidepressant (4.6%) as CR nonparticipants (5.0%; χ2 (1) = 0.04, p =.85). Participants were asked to outline the types of psychosocial services offered at the CR program and whether or not they utilized them. Stress management classes were offered to 63 participants (51.2%) and were used by 45 (35.5%) respondents. Support groups were offered to 30 (24.4%) participants and were used by 21 (17.1%) of respondents.
Longitudinal Analysis of Depressive Symptomatology
The longitudinal model predicting depression from baseline through 6 months and 1 year is presented in Table 4. The BDI scores were right skewed, and therefore the outcome for the longitudinal model is based on the logarithm of the BDI scores, which was normally distributed. Based on the AIC criterion, we chose the unstructured covariance for our model. There was a significant gender by CR participation interaction, and the resultant estimated marginal means are presented in Figure 3. Post-hoc Bonferroni tests revealed a significant difference in marginal BDI scores between female CR participants and male participants (p =.01), and between female CR participants and male CR nonparticipants (p =.01). All other interactions with time were assessed, and because they were not significant they were excluded from the model. Depressive symptomatology was significantly greater in those participants with a family income less than CAD$50,000/yr (marginal mean = 7.69) than those with greater income (marginal mean = 5.81), in participants less than 60 years old (estimated marginal mean = 7.81) than in older participants (estimated marginal mean = 5.87), and in participants with a diagnosis of UA (marginal mean = 7.32) vs. MI (marginal mean = 6.05). The effect of time was also significant, with estimated marginal BDI scores of 7.32 at baseline, 6.55 at 6 months, and 6.17 at 1 year. Post-hoc contrasts revealed significant differences from baseline to 6 months (p =.01), and between baseline and 1 year (p<.001), but no significant difference between 6 months and 1 year (p =.18).
TABLE 4.
Longitudinal Model Predicting Depressive Symptomatology
| Variable | Coefficient | Standard Error | t value | p value |
|---|---|---|---|---|
| Intercept | 2.08 | 0.18 | 11.69 | < 0.0001 |
| Gender (female)a | 0.63 | 0.21 | 3.05 | — |
| CR participationb | 0.03 | 0.10 | 0.34 | — |
| Gender*CR participation | −0.46 | 0.23 | −2.01 | 0.0378 |
| Family income (>$50k) | −0.28 | 0.08 | −3.28 | 0.0010 |
| Age(>60) | −0.26 | 0.08 | −3.31 | 0.0006 |
| Killip class (class 1) | −0.06 | 0.11 | −0.56 | 0.6071 |
| Diagnosis (MI) | −0.20 | 0.08 | −2.57 | 0.0293 |
| Marital status (married) | −0.18 | 0.11 | −1.71 | 0.0874 |
| Education (college, univ) | 0.02 | 0.08 | 0.21 | 0.9534 |
| Time | ||||
| Time 1 | 0.17 | 0.05 | 3.60 | 0.0004 |
| Time 2 | 0.06 | 0.04 | 1.35 | 0.1836 |
| Time 3 | — | — | — | — |
Not listed because the interaction is significant.
The overall effect for site is tested with the F test
Figure 3.
Gender × interaction in depression.
DISCUSSION
Depressive symptomatology spontaneously improved over the year of recovery for all participants, and this did not differ based on disease severity or CR participation.
Younger participants and those with lower family income were significantly more likely to be depressed. Adjustment to ACS can be more difficult in younger patients, considering the uncertain future in those suffering prematurely from a chronic disease, and the heightened demands of work and family roles (31). The greater prevalence of depression among participants with lower family income is particularly worrisome, considering this group also experiences limited access to cardiac treatment (18) and a greater burden of mortality (32).
The lack of expected interaction between CR and time suggests, first, that CR programs in the region may be failing to screen and treat depression as promoted in clinical practice guidelines (17,33). In a recent provincial pilot project (34), it was determined that less than 50% of CR programs had services to treat depression. In this sample, only approximately 20% to 30% of the CR participants reported utilizing psychosocial services while in their program, and CR participants were not more likely to be taking antidepressant medication than CR nonparticipants. Considering that meta-analyses confirm that CR is successful in reducing psychosocial distress when compared with controls (35,36), clearly we need to provide these programs with greater resources to treat depressive symptomatology (ie, staffing models incorporating registered psychologists or psychiatrists). Second, the lack of interaction also suggests that exercise itself was not effective in alleviating depression, as supported in the literature (16). However, we did find that depressed participants were less likely to adhere to the CR program and participate in the weekly sessions than were nondepressed participants. Future research is needed to design and evaluate interventions to increase CR adherence among depressed participants to ensure that they achieve the mental health gains associated with physical activity.
Our findings counter those of Lavie and Milani (5,20), which showed significant reductions in depression after CR. Although it is true that CR participants in this study did improve over time, so did CR nonparticipants. Their study did not incorporate a control group, had a shorter follow-up of 3 months, and assessed participants from a single CR site (which did not include a treatment program for depression). As mentioned above, the fact that we did not find a significant difference in depressive symptomatology over time based on CR participation could be due to the fact that few CR programs in the region screen and treat depression, but it could also be due to the fact that depression remits in both CR participants and controls after 6 to 12 months. Regardless of CR participation, patients had reduced depressive symptomatology between hospitalization and 1 year later (but not between 6 months and 1 year). However, the 6- to 12-month burden of depression represents a lengthy (and avoidable) time period for patients to suffer untreated, considering that the safety and efficacy of antidepressant (14) and psychotherapeutic (13) treatments in alleviating depression in cardiac populations have been established.
Of great interest is the finding that women who attended CR were significantly more depressed than men who attend CR. This contradicts findings by Brezinka et al. (37) in the Netherlands, which reported no significant gender differences in depression at entry into a CR program in a matched sample of 231 male and female ischemic patients. We know that women have a rate of depression 2 times that of men in the general population (38) and in the cardiac population (39), but it is intriguing why more depressed women but fewer depressed men get referred to CR. The process of referral into CR is not systematic, and is based on both physician referral patterns and patient characteristics (40). Our results revealed no significant differences in physician referral patterns based on severity of depressive symptomatology, suggesting that patient preferences are at play. Perhaps depressed female patients seek the social support that can be found in a CR program (41), in their efforts to “tend-and-befriend”(42,43). This finding should be replicated in future studies utilizing a matched sample of male and female cardiac patients, and assessing social support. Regardless of this effect, depressed participants are less likely to adhere to the CR program, leaving room for intervention to maximize recovery.
A few study limitations should be emphasized. First, although the longitudinal multisite nature of this study was an asset, the design was limited by nonrandomization to CR. Because the CR participation of patients at multiple sites may at first glance serve as a confound with regard to program components and length, CR programs across the regions generally followed the same model of care due to a government-sponsored pilot project (34). Second, the generalizability of the study is limited by the differences between participants and refusers. In particular, dropouts were more likely to be less educated, younger, and more depressed than were participants who remained in the study for the full year. However, we controlled for these differences in our longitudinal model. Moreover, this loss of participants over time (due also to mortality) generates caution in our finding that depression wanes naturally over the course of recovery, and invites further research. Third, our measure of depressive symptomatology assessed severity only, and does not provide diagnostic information. This leads to our fourth limitation concerning the self-report nature of the assessments for depressive symptomatology, in addition to CR participation, antidepressant usage, and discussions with healthcare providers regarding such symptomatology. It is possible that the cognitive symptoms of depression may have affected their report of symptomatology and behavior (eg, medication adherence). The inclusion of clinical interviews and independent CR participation verification is warranted in future work. Finally, this study failed to report or control for other psychiatric or medical comorbidities.
In conclusion, approximately one third of these ACS participants experienced elevated depressive symptomatology. This depression persisted up to six months, and was not significantly alleviated in approximately two thirds of those affected. These depressed patients were grossly undertreated, with 5% using antidepressant medication, and 20% attending CR. It was unfortunate that although most CR programs provide exercise interventions, which have beneficial effects on depressive symptomatology, the majority of CR programs did not provide psychotherapeutic treatments. It remains to be seen whether treating depression improves cardiac prognosis, but it is incumbent on us to address the burden of depression experienced by many cardiac patients, to improve their quality of life and well-being.
Acknowledgments
We gratefully acknowledge the Heart and Stroke Foundation of Ontario and Samuel Lunenfeld Foundation for research grants to investigate gender differences in CCU patients to Drs. Abbey and Stewart, and the CIHR Institute of Gender and Health Fellowship, which supported Dr. Grace. We also acknowledge Linda Green and the CCU nurses for their diligence in participant recruitment.
Glossary
- CR
cardiac rehabilitation
- UA
unstable angina
- MI
myocardial infarction
- ACS
acute coronary syndromes
- CCU
coronary care unit
- CAD
Canadian dollars
- USD
U.S. dollars
- BDI
Beck Depression Inventory
References
- 1.Hemingway H, Marmot M. Evidence based cardiology: psychosocial factors in the aetiology and prognosis of coronary heart disease: systematic review of prospective cohort studies. BMJ. 1999;318:1460–7. doi: 10.1136/bmj.318.7196.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smith T, Ruiz J. Psychosocial influences on the development and course of coronary heart disease: current status and implications for research and practice. J Consult Clin Psychol. 2002;70:548–68. doi: 10.1037//0022-006x.70.3.548. [DOI] [PubMed] [Google Scholar]
- 3.Abbey S, Stewart DE. Gender and psychosomatic aspects of ischemic heart disease. J Psychosom Res. 2000;48:417–23. doi: 10.1016/s0022-3999(99)00112-9. [DOI] [PubMed] [Google Scholar]
- 4.Hance M, Carney RM, Freedland KE, Skala J. Depression in patients with coronary heart disease: a 12-month follow-up. Gen Hosp Psychiatry. 1996;18:61–5. doi: 10.1016/0163-8343(95)00100-x. [DOI] [PubMed] [Google Scholar]
- 5.Lavie C, Milani R, Cassidy M, Gilliland Y. Effects of cardiac rehabilitation and exercise training programs in women with depression. Am J Cardiol. 1999;83:1480–83. doi: 10.1016/s0002-9149(99)00127-7. [DOI] [PubMed] [Google Scholar]
- 6.Blazer DG, Kessler RC, McGonagle K, Swartz M. The prevalence and distribution of major depression in a national community sample: the national comorbidity survey. Am J Psychiatry. 1994;151:979–86. doi: 10.1176/ajp.151.7.979. [DOI] [PubMed] [Google Scholar]
- 7.Ladwig KH, Roll G, Breithardt G, Budde T, Borggrefe M. Post-infarction depression and incomplete recovery 6 months after acute myocardial infarction. Lancet. 1994;343:20–3. doi: 10.1016/s0140-6736(94)90877-x. [DOI] [PubMed] [Google Scholar]
- 8.Schwartzman JB, Glaus KD. Depression and coronary heart disease in women: Implications for clinical practice and research. Prof Psychol Res Pract. 2000;31:48–57. [Google Scholar]
- 9.Frasure-Smith N, Lesperance F, Talajic M. The impact of negative emotions on prognosis following myocardial infarction: is it more than depression? Health Psychol. 1995;14:388–98. doi: 10.1037//0278-6133.14.5.388. [DOI] [PubMed] [Google Scholar]
- 10.Arnold E. The stress connection: women and coronary heart disease. Crit Care Nurs Clin North Am. 1997;9:565–75. [PubMed] [Google Scholar]
- 11.Ziegelstein R, Fauerbach J, Stevens S, Romanelli J, Ritcher D, Bush D. Patients with depression are less likely to follow recommendations to reduce cardiac risk during recovery from a myocardial infarction. Arch Intern Med. 2000;160:1818–23. doi: 10.1001/archinte.160.12.1818. [DOI] [PubMed] [Google Scholar]
- 12.Carney RM, Freedland KE, Jaffe AS. Insomnia and depression prior to myocardial infarction. Psychosom Med. 1990;52:603–9. doi: 10.1097/00006842-199011000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Writing Committee for the ENRICHD Investigators. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the enhancing recovery in coronary heart disease patients (ENRICHD) randomized trial. JAMA. 2003;289:3106–16. doi: 10.1001/jama.289.23.3106. [DOI] [PubMed] [Google Scholar]
- 14.Glassman A, O’Connor C, Califf R. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA. 2002;288:701–9. doi: 10.1001/jama.288.6.701. [DOI] [PubMed] [Google Scholar]
- 15.Jolliffe JA, Rees K, Taylor RS, Thompson D, Oldridge N, Ebrahim S. Exercise-based rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2001;(4) doi: 10.1002/14651858.CD001800. [DOI] [PubMed] [Google Scholar]
- 16.Babyak M, Blumenthal J, Herman SKP, Doraiswamy M, Moore K, et al. Exercise treatment for major depression: maintenance of therapeutic benefit at 10 months. Psychosom Med. 2000;62:633–8. doi: 10.1097/00006842-200009000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Stone JA, Cyr C, Friesen M, Kennedy-Symonds H, Stene R, Smilovitch M. Canadian guidelines for cardiac rehabilitation and atherosclerotic heart disease prevention: a summary. Can J Cardiol. 2001;17(suppl B):3B–30B. [PubMed] [Google Scholar]
- 18.Grace SL, Abbey S, Shnek Z, Irvine J, Franche RL, Stewart D. Cardiac rehabilitation II: referral and participation. Gen Hosp Psychiatry. 2002;24:127–34. doi: 10.1016/s0163-8343(02)00179-2. [DOI] [PubMed] [Google Scholar]
- 19.Carney RM, Freedland KE, Eisen SA, Rich MW, Jaffe AS. Major depression and medication adherence in elderly patients with coronary artery disease. Health Psychol. 1995;14:88–90. doi: 10.1037//0278-6133.14.1.88. [DOI] [PubMed] [Google Scholar]
- 20.Milani R, Lavie C, Cassidy M. Effects of cardiac rehabilitation and exercise training programs on depression in patients after major coronary events. Am Heart J. 1996;132:726–32. doi: 10.1016/s0002-8703(96)90304-x. [DOI] [PubMed] [Google Scholar]
- 21.Johnston M, Foulkes J, Johnston DW, Pollard B, Gudmundsdottir H. Impact on patients and partners of inpatient and extended cardiac counseling and rehabilitation: a controlled trial. Psychosom Med. 1999;61:225–33. doi: 10.1097/00006842-199903000-00015. [DOI] [PubMed] [Google Scholar]
- 22.Uniken Venema-Van Uden MM, Zoeteweij MW, Erdman R, Van den Berg G. Medical, social and psychological recovery after cardiac rehabilitation. J Psychosom Res. 1989;33:651–6. doi: 10.1016/0022-3999(89)90072-x. [DOI] [PubMed] [Google Scholar]
- 23.Yoshida T, Kohzuki M, Yoshida K, Hiwatari M, Kamimoto M, Yamamoto C. Physical and psychological improvements after phase II cardiac rehabilitation in patients with myocardial infarction. Nurs Health Sci. 1999;1:163–70. doi: 10.1046/j.1442-2018.1999.00021.x. [DOI] [PubMed] [Google Scholar]
- 24.Killip T, Kimball JT. Treatment of myocardial infarction in a coronary care unit: a two year experience with 250 patients. Am J Cardiol. 1967;20:457–64. doi: 10.1016/0002-9149(67)90023-9. [DOI] [PubMed] [Google Scholar]
- 25.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 26.Steer RA, Cavalieri TA, Leonard DM, Beck AT. Use of the Beck Depression Inventory for primary care to screen for major depression disorders. Gen Hosp Psychiatry. 1999;21:106–11. doi: 10.1016/s0163-8343(98)00070-x. [DOI] [PubMed] [Google Scholar]
- 27.Frasure-Smith N, Lesperance F, Talajic M. Depression following myocardial infarction: impact on six-month survival. JAMA. 1993;270:1819–25. [PubMed] [Google Scholar]
- 28.Shnek ZM, Irvine J, Stewart DE, Abbey SE. Psychological factors and depressive symptoms in ischemic heart disease. Health Psychol. 2001;20:141–5. doi: 10.1037//0278-6133.20.2.141. [DOI] [PubMed] [Google Scholar]
- 29.Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 30.Frasure-Smith N. In-hospital symptoms of psychological stress as predictors of long-term outcome after acute myocardial infarction in men. Am J Cardiol. 1991;67:121–7. doi: 10.1016/0002-9149(91)90432-k. [DOI] [PubMed] [Google Scholar]
- 31.LaCharity L. The experiences of younger women with coronary artery disease. J Women’s Health Gender-Based Med. 1999;8:773–85. doi: 10.1089/152460999319101. [DOI] [PubMed] [Google Scholar]
- 32.Alter DA, Naylor CD, Austin P, Tu JV. Effects of socioeconomic status on access to invasive cardiac procedures and on mortality after acute myocardial infarction. N Engl J Med. 1999;341:1359–67. doi: 10.1056/NEJM199910283411806. [DOI] [PubMed] [Google Scholar]
- 33.Wenger NK, Froelicher ES, Smith LK, Ades PA, Berra K, Blumenthal JA, et al. Cardiac rehabilitation as secondary prevention. Agency for Health Care Policy and Research and National Heart, Lung, and Blood Institute. Clin Pract Guidel Quick Ref Guide Clin. 1995;(17):1–23. [PubMed] [Google Scholar]
- 34.Cardiac Care Network. The Ontario cardiac rehabilitation pilot project: report and recommendations. Toronto, ON: 2002. http://www.ccn.on.ca/rehabpublic/FinalReport_PDF_Sept30_02_FINALpassword.pdf. [Google Scholar]
- 35.Dusseldorp E, van Elderen T, Maes S, Meulman J, Kraaij V. A meta-analysis of psychoeducational programs for coronary heart disease patients. Health Psychol. 1999;18:506–19. doi: 10.1037//0278-6133.18.5.506. [DOI] [PubMed] [Google Scholar]
- 36.Linden W, Stossel C, Maurice J. Psychosocial interventions for patients with coronary artery disease: a meta-analysis. Arch Intern Med. 1996;156:745–52. [PubMed] [Google Scholar]
- 37.Brezinka V, Dusseldorp E, Maes S. Gender differences in psychosocial profile at entry into cardiac rehabilitation. J Cardiopulm Rehabil. 1998;18:445–9. doi: 10.1097/00008483-199811000-00007. [DOI] [PubMed] [Google Scholar]
- 38.Nolen-Hoeksema S, Larson J, Grayson C. Explaining the gender difference in depressive symptoms. J Pers Soc Psychol. 1999;77:1061–72. doi: 10.1037//0022-3514.77.5.1061. [DOI] [PubMed] [Google Scholar]
- 39.Frasure-Smith N, Lesperance F, Juneau M, Talajic M, Bourassa MG. Gender, depression, and one-year prognosis after myocardial infarction. Psychosom Med. 1999;61:26–37. doi: 10.1097/00006842-199901000-00006. [DOI] [PubMed] [Google Scholar]
- 40.Grace SL, Evindar A, Kung T, Scholey P, Stewart DE. Automatic referral to cardiac rehabilitation. Med Care. 2004;42:661–9. doi: 10.1097/01.mlr.0000129901.05299.aa. [DOI] [PubMed] [Google Scholar]
- 41.Dracup K. Cardiac rehabilitation: the role of social support in recovery and compliance. In: Shumaker SA, Czajkowski SM, editors. Social support and cardiovascular disease. New York, NY: Plenum Press; 1994. pp. 333–53. [Google Scholar]
- 42.Taylor S, Klein L, Lewis B, Gruenewald T, Gurung F, Updegraff J. Biobehavioral responses to stress in females: tend-and-befriend, not fight-or-flight. Psychol Rev. 2000;107:411–29. doi: 10.1037/0033-295x.107.3.411. [DOI] [PubMed] [Google Scholar]
- 43.Hill K. Promoting exercise compliance: a cognitive-behavioral approach. Women Ther. 2002;25:75–90. [Google Scholar]