Abstract
OBJECTIVE
We investigated the relationship between carbohydrate intake and postprandial blood glucose (BG) levels to determine the most influential meal for type 2 diabetic subjects treated with basal insulin and needing prandial insulin.
RESEARCH DESIGN AND METHODS
Three-day BG profiles for 37 type 2 diabetic subjects, with A1C levels of 7.7%, treated with sulfonylurea and metformin, and well titrated on insulin glargine, were analyzed using a continuous glucose monitoring system. Food intake from 680 meals was recorded and quantified during continuous glucose monitoring.
RESULTS
The median BG excursion (ΔBG) was higher at breakfast than at lunch or dinner (111 [81; 160] vs. 69.5 [41.5; 106] and 82.5 mg/dl [53; 119] mg/dl, P < 0.0001). There was a weak overall correlation between ΔBG and carbohydrate intake. Correlation improved when mealtime was taken into account. Simple relationships were established: ΔBG (mg/dl) = 65 × carbohydrate/body weight + 73 for breakfast (R2 = 0.20, P < 0.0001); the slope was reduced by half at lunch and by one-third at dinner. Twelve relevant variables likely to affect ΔBG were integrated into a polynomial equation. This model accounted for 49% of ΔBG variability. Two groups of patients were identified: responders, in whom ΔBG was well correlated with carbohydrate intake (R2 ≥ 0.30, n = 8), and nonresponders (R2 < 0.30, n = 29). Responders exhibited a greater insulinopenic profile than nonresponders.
CONCLUSIONS
The carbohydrate intake in responders clearly drives ΔBG, whereas, in nonresponders, other factors predominate. This sort of characterization should be used to guide therapeutic choices toward more targeted care with improved type 2 diabetes management.
In type 2 diabetes, large controlled clinical trials have shown that intensive treatment of diabetes can significantly decrease the development and/or progression of microvascular and macrovascular complications associated with the disease (1,2). Until recently, therapy has mainly focused on lowering A1C levels, with a strong emphasis on fasting plasma glucose levels (3). In the event of failure of oral antidiabetic treatment at a maximum dose, the addition of a single bedtime injection of a long-acting insulin analog is recommended to reduce A1C to below 7% (3,4). However, while combined basal insulin and oral antidiabetic drugs (OADs) usually normalize fasting glucose levels in the morning (5,6), A1C remains above 7% in around half of these patients. Failure to optimize glycemic control is mainly due to a persistent elevation in postprandial blood glucose (PPBG) levels (7). Interventional trials support the view that controlling fasting hyperglycemia is necessary but usually insufficient for achieving a target A1C of <7%, thus making control of postprandial hyperglycemia essential. Moreover, PPBG excursions lead to oxidative stress by generating reactive oxygen species and to inflammation and endothelial dysfunction (8); indeed, all these phenomena are involved in micro- and macrovascular diabetes complications. These data emphasize the need for good control of PPBG.
Guidelines have been proposed for the management of PPBG values, but there is currently no consensus regarding the target value, which is a peak value of <180 (5) or <140 mg/dl 2 h after meals (8,9). Many authors recommend a PPBG level of <140 mg/dl 2 h after the start of a meal, to achieve normal glucose tolerance according to the standards of oral glucose tolerance testing. A single injection of prandial insulin, in addition to basal insulin and OAD therapy, targeted at the main meal (i.e., the meal with the highest PPBG excursion), represents a stepwise approach toward intensifying insulin therapy. However, it is not always easy to determine the main meal of the day for any given patient, since this can vary according to country and customs and is also dependent on the individual patient's eating habits. It is nevertheless vital to ascertain the patient's main meal, to treat the principal daily PPBG excursion effectively.
Of the factors potentially affecting PPBG levels, total carbohydrate intake has been shown to be a consistent predictor of PPBG concentrations (10), in both single-meal (11) and mixed-meal studies (10). However, while PPBG excursion is directly linked to carbohydrate (CHO) levels in type 1 diabetes (12), the relationship is more complex in type 2 diabetes, primarily because of residual insulin secretion and insulin resistance. As a result, CHO alone is not a reliable predictor of glycemic excursion in type 2 diabetic subjects (13), thus suggesting the involvement of other factors.
We aimed to analyze the relationship between the quantity of carbohydrates ingested in a meal and subsequent PPBG excursion in type 2 diabetic subjects presenting good fasting blood glucose (FBG) levels. In this context, continuous glucose monitoring systems (CGMSs) allow a more expansive view of glycemic excursions at meals. We also sought to identify factors other than CHO that potentially affect this relationship and to study their respective roles in PPBG excursion. Finally, we attempted to create an equation for the prediction of postprandial excursion that integrates these various factors.
RESEARCH DESIGN AND METHODS
This was a prospective single-center observational study designed to determine the relationship between postprandial excursion and CHO intake in type 2 diabetic subjects on OADs and insulin glargine and presenting good basal glycemic control.
Study population
A total of 37 type 2 diabetic subjects were recruited at the Diabetes Department of the Sud-Francilien Hospital between 9 January 2007 and 24 June 2007, either during consultation or while they attended an outpatient clinic. The inclusion criteria were as follows:
On treatment with insulin glargine in combination with sulfonylurea and metformin at maximum tolerated doses for at least 3 months; no patients were taking prandial insulin, dipeptidyl peptidase 4 inhibitors, or glucagon-like peptide 1 analogs.
Mean FBG levels (at least 10 consecutive measurements before inclusion) of <120 mg/dl. For patients with FBG >120 mg/dl, the once-daily bedtime dose of glargine insulin was titrated to achieve a mean monthly FBG of <120 mg/dl before inclusion.
A1C >7%.
Stable treatment and diet over the previous 2 months.
Written informed consent before participating in the study.
Methods
Patients were asked to provide two series of 3- to 5-day CGMS blood glucose (BG) profiles no more than 1 month apart.
Study organization
Patients attended the outpatient clinic on the morning of day 1. They were required to fast before arriving.
The baseline characteristics were recorded on arrival and tests for A1C, BG value, and fasting lipids were performed before breakfast. Basal and glucagon-stimulated C-peptide levels were also measured.
CGMS
Continuous glucose readings were taken using a Medtronic MiniMed CGMS, which was initialized and calibrated by means of capillary self-monitoring of BG measurements. The CGMS sensor was inserted at the hospital before or just after lunch on day 1. In their homes, patients were required to calibrate the sensor a further three times on day 1 and then four times per day (before breakfast, lunch, and dinner and at bedtime) until day 4 or 5. They also had to record each meal and perform capillary glucose tests with a blood glucose meter six times per day: FBG when waking up in the morning just before breakfast and before (premeal) and 2 h after the start of each meal (2-h PPBG). On day 4 or 5, patients returned to the hospital to have the CGMS sensor removed, and the results were downloaded onto the physician's computer. At the same time, patient diaries for self-monitoring of BG levels and recording food intake were collected. A 24-h telephone hotline was available for patients during the CGMS profile phase.
We obtained a second CGMS profile, under similar conditions to the first, within 1 month.
Dietary survey
During each CGMS profile period, patients were asked to eat normally, without taking any snacks, and were asked to abstain from any physically demanding activities. Patients were free to follow their regular diets. They were asked to record precisely in a diary what they ate after each meal. Diaries with weighed food were then analyzed by two dietitians, to assess CHO, lipid, protein, and calorie intake at each meal. In cases of discrepancy between the two surveys, data were reviewed by both and a decision was taken together. To have a broad amplitude of CHO values and be able to accurately analyze the correlation between PPBG excursion and CHO amount, patients were asked to double the carbohydrate intake once a day in one of the three meals (breakfast, lunch, or dinner), based on the recommendations of the dietitian (“carbohydrate-loaded” meals) in both CGMS periods.
Data analysis
Descriptive analyses.
Data from all meals (n = 680) were first analyzed. For each type of meal (breakfast, lunch, and dinner), meal start times were superimposed (time 0) and mean 4-h postprandial BG profiles were then analyzed.
Analysis of correlation
The overall correlation between postprandial blood glucose excursion (ΔPBG) and CHO intake was assessed for all patients. Four criteria were used to study ΔPBG: 1) PPBGmax(0–4 h)–preprandial BG (or FBG for breakfast), 2) 2-h PPBG–preprandial BG (or FBG for breakfast), 3) AUC(0–3 h), and 4) AUC(0–4 h). The first criterion exhibited the best correlation between CHO and ΔPBG; it was thus considered as representative of ΔPBG and was selected for subsequent analyses. These analyses of correlation were repeated, substituting CHO intake for the ratio of CHO content/body weight. Similar analyses were repeated, taking into account the mealtime (breakfast, lunch, and dinner).
Modeling analysis
To ensure data reliability, only results from the first 3 days of each CGMS profile were used for modeling (n = 593).
Selected variables
Variables likely to affect ΔPBG were collected for each patient, i.e., 1) demographics (age, sex); 2) variables associated with the meal (CHO, lipid and protein content, time of meals and type of meals [normal or “carbohydrate-loaded”]); 3) variables associated with metabolic control (A1C, FBG, and premeal BG values); and 4) variables affecting insulin resistance evaluation (basal and stimulated C-peptide, waist circumference, BMI, waist-to-hip ratio, and the coefficient of insulin sensitivity [K] [K = basal insulin dose/0.35 × weight in kilograms] [12]). In the event of a good correlation between two of these variables, only the most relevant one was selected for subsequent analyses.
Whole population
The aforementioned variables were studied in a polynomial equation. The polynomial equation that gave the best prediction was assessed using a stepwise method (with a significance level for entry value and for a stay value in the model equal to 0.10). A mixed model analysis of variance using an autoregressive correlation structure with patients as a random factor was also tested to take into account the potential correlation between each patient's measurements. The two main factors affecting ΔPBG (CHO intake and mealtime) were incorporated as fixed factors. All of these models were compared for their ability to predict variability in ΔPBG.
Individual relationships
The correlation between carbohydrate intake and ΔPBG was also studied for each patient, and all patients were classified according to the degree of correlation between ΔPBG and CHO intake.
Statistical analysis
Sample size.
We planned to recruit 40 patients to obtain at least 30 complete evaluable observations; this would result in a total of 540 usable prandial values (30 patients, two CGMS profiles with nine meals per patient that could be analyzed), thus rendering 180 values for each of the three meals available for analysis.
Data analysi.
SPSS 15 for Windows was used for descriptive statistical analysis, and the results were reported as mean ± SD if the data followed normal distributions; comparisons were thus performed using a one-way ANOVA; otherwise, data were presented as the median and interquartile range (median [interquartile range]), and comparisons were performed using a Kruskal-Wallis one-way ANOVA. Statistical significance for two-sided tests was set at P < 0.05.
SAS 9.1 for Windows XP was used for modeling analyses. All models were compared using the R2 coefficients for polynomial and linear equations or Akaike's information criteria for mixed models, with the best prediction being considered for the highest R2 coefficients and for the lowest Akaike's information criteria values, respectively.
RESULTS
Study population
The 37 type 2 diabetic subjects (25 men, 12 women) included in the study were treated with sulfonylurea, metformin, and glargine insulin and exhibited good initial glycemic control. These patients were aged 64 ± 6 years; they had a BMI of 29.3 ± 4 kg/m2, and the mean A1C level at baseline was 7.7 ± 0.8%.
The baseline C-peptide value was 2.4 ± 1.1 ng/ml and glargine dose was 33 units/day (20; 44).
Three- to five-day BG profiles of the 37 type 2 diabetic subjects were recorded using a CGMS. Profiles were recorded once (n = 5) or twice (n = 32). The median interval between the two series of data was 11 days (11; 18).
Postprandial blood glucose profiles
Data from 680 meals were analyzed for the whole population. Mean postprandial BG profiles adjusted for the start of meals are given in Fig. 1. The median BG excursion was significantly higher at breakfast than at lunch and dinner (111 [81; 160] vs. 69.5 [41.5; 106] and 82.5 [53; 119] mg/dl, P < 0.0001), for a median CHO intake of 52 [40; 70], 77 [53; 113], and 72 [50; 98] g at breakfast, lunch, and dinner, respectively. Maximum PPBG excursion occurred around 110 min after the beginning of the meal. However, the time to peak excursion was significantly shorter at breakfast than at lunch or dinner (95 [75; 120] vs. 120 [80; 180] min, and 125 [95; 190] min, P < 0.0001).
Figure 1.
The 4-h PPBG profiles: the start times of all meals (breakfasts, lunches, and dinners) were superimposed in the analysis (time 0). PPBG analysis was then performed over a period of 4 h from time 0. Median ΔBG was significantly higher at breakfast than at lunch and dinner (111 [81; 160] vs. 69.5 [41.5; 106] and 82.5 [53; 119] mg/dl, P < 0.0001). Median peak BG excursion was reached 110 min (80; 165) after the start of meals, but differed according to meal type (95 [75; 120] min at breakfast vs. 120 [80; 180] min at lunch and 125 [95; 190] min at dinner, P < 0.0001).
Relationship between postprandial BG excursion and CHO intake.
The initial overall analysis of the 680 meals showed a weak correlation between BG excursion and CHO intake, whatever the representations of postprandial BG excursion (R2: 0.06–0.09); however, PPBGmax(0–4 h)–preprandial BG (or FBG for breakfast), designed as ΔBG, showed the best correlation and was thus used for subsequent analyses. This correlation improved slightly after an adjustment for body weight (data not shown).
The correlation between ΔBG and CHO improved when the mealtime was taken into account, with better correlation for breakfast and dinner than for lunch. Using the regression curve equation for each meal, a simple overall relationship was established between ΔBG and CHO intake. For breakfast, ΔBG (mg/dl) = 65 × carbohydrate/body weight + 73 (R2 = 0.20, P < 0.0001); the slope was reduced by half at lunch (a = 32, constant b = 43, R2 = 0.09, P < 0.0001) and by one-third at dinner (a = 53, constant b = 36, R2 = 0.2, P < 0.0001).
These correlation analyses indicated that, for the same CHO content, ΔBG was twice as high at breakfast and two-thirds higher at dinner than at lunch. These linear approaches were then completed with multivariate polynomial analyses to increase the predictive ability of the model.
ΔBG modeling
The data for the first 3 days of the BG profiles were analyzed for ΔBG modeling.
Whole population: development of a polynomial equation
Available relevant criteria likely to affect BG excursion were listed, and 12 of them were integrated into a polynomial equation. These variables included CHO content (g), mealtime (breakfast, lunch, or dinner), type of meal (carbohydrate-loaded, postcarbohydrate-loaded, or normal meals), BMI (kg/m2), baseline C-peptide (ng/ml), coefficient of insulin sensitivity (K), protein content (g), A1C (%), preprandial BG (or FBG for breakfast) value (mg/dl), age (years), waist circumference (cm), and waist-to-hip ratio. We checked that these 12 variables were not too highly correlated to continue the analysis (pair-wise correlation coefficients always below 0.65). ΔBG was finally expressed as follows:
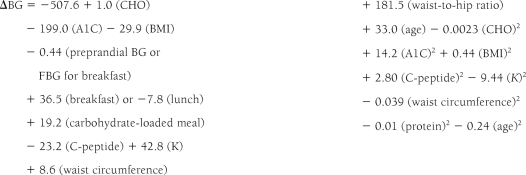 |
with R2 = 49%; this suggested that 49% of ΔBG variability could be accounted for using this model. The variables with the greatest bearing on BG excursion were CHO intake and mealtime, with respective contributions of 15 and 9% to ΔBG variability. Analysis of the other three criteria for PPBG excursion [PPBG2h–preprandial BG (or FBG for breakfast), AUC(0–3 h), and AUC(0–4 h)] showed similar results, with R2 coefficients of around 0.50 (0.49–0.52). Thus, half of ΔBG variability can be accounted for using the selected variables.
Restricting ΔBG modeling to a simple first-degree equation using the six main variables resulted in simplified expression of ΔBG: ΔBG = 46 + 0.6 (CHO) + [46 (breakfast) or −12 (lunch)] − 2 (BMI) − 3.6 (C-peptide) + 12 (A1C) − 0.34 (preprandial BG or FBG for breakfast). This model accounted for 38% of ΔBG variability.
A mixed-effect model was suggested to take into account the probable correlation between repeated measures in the same patient. Analysis was conducted on CHO intake and mealtime, both of which were independent factors (P < 0.0001), but use of this linear model did not improve the predictive value.
Individual data
A regression curve between CHO intake and ΔBG was traced for each patient, and the R2 coefficient of determination was considered. Individual data analysis revealed high inter-individual variability, with certain patients, labeled “responders,” showing good correlation between ΔBG and carbohydrate intake (R2 ≥ 0.30, n = 8) and others, termed “nonresponders,” exhibiting poor correlation (R2 < 0.30, n = 29) (Fig. 2).
Figure 2.
Linear relationship between CHO intake based on weight and ΔBG for a responder (A) (good correlation between CHO intake/weight and ΔBG) and for a nonresponder (B) (no correlation between CHO intake/weight and ΔBG).
There was no difference regarding the duration of the disease between responder and nonresponder patients. Responders were leaner than nonresponders (BMI 26.5 ± 3.1 vs. 30.1 ± 3.9 kg/m2, P = 0.019); they had higher median PPBG excursions (ΔBG, 103 [62; 151] vs. 85 [53; 124] mg/dl, P = 0.001) and had a lower median CHO intake (60 [43; 91] vs. 67 [48; 96] g, P = 0.027). Their median lipid intake was also higher (26 [16; 40] vs. 22 [12; 32] g, P = 0.001). There was no difference in the median calorie content per meal (635 [425; 892] vs. 614 [396; 838] kcal/meal, P = 0.247), but the median calorie content per meal and per kilo significantly differed between the two populations (7.92 [5.34; 11.52] vs. 7.25 [4.61; 9.82] kcal/meal/kg, P = 0.03). Among responders, there was a trend toward a lower basal C-peptide value (1.8 ± 0.7 vs. 2.4 ± 1.3 ng/ml, P = 0.11) and a lower glargine dose (20 [18; 42] vs. 35 [24; 44] units, P = 0.245).
CONCLUSIONS
There is increasing evidence that PPBG excursion has a harmful effect on arterial wall (8) and is involved in both the microvascular (14) and macrovascular complications of diabetes (15). Strategies to minimize PPBG concentrations are thus essential to reduce complications in type 2 diabetic subjects. Our study was conducted in a population of type 2 diabetic subjects with good baseline fasting BG levels and took into account only those factors affecting PPBG excursions. Many factors influence PPBG excursion, with CHO intake playing a key role. It is now accepted that the actual CHO content of meals is more important than the source or type of CHO (16). In addition to the CHO intake level, the time of the meal also contributes considerably to BG excursion. Pearce et al. (13) have shown that type 2 diabetic subjects on randomized dietary therapy, who even consume CHO throughout the day (70 g CHO per meal), displayed a higher BG excursion at breakfast than at lunch or dinner. Similarly, in our study, the highest median BG excursion was observed for breakfast. However, one of our main findings was that for the same CHO intake the peak BG excursion was two times greater at breakfast and was two-thirds greater at dinner than at lunch. The higher BG excursion after breakfast may be due to the “dawn phenomenon,” a dysregulation of the normal circadian hormonal patterns resulting in increased hepatic glucose output and decreased glucose utilization.
The weak correlation between glycemic excursion and CHO intake at individual meals suggests that factors other than CHO and mealtime are involved in PPBG excursion. Variables likely to affect PPBG levels were selected to model PPBG excursion. A 12-variable polynomial equation was derived, allowing a prediction of up to 50% of ΔBG variability. Some of the selected variables have already been shown to be involved in PPBG excursion. Protein (10) and lipid consumption (17), preprandial glucose level (18), and second meal effects (19) can also modify the effects of CHO on PPBG concentrations (13). The degree of insulin resistance also affects PPBG excursion considerably. In type 2 diabetic subjects, insulin resistance is mostly due to an absence of glucagon prandial secretion suppression (20), leading to an increase in hepatic glucose production (21). Several variables used to assess insulin resistance were included in our models: waist circumference, waist-to-hip ratio, BMI, weight, insulin sensitivity coefficient (K), and C-peptide. Insulin resistance, which differed widely from one patient to another, also contributed to ΔBG variability.
The remaining 50% of ΔBG variability may be due to parameters not assessed in our study. The glycemic index of food and the dietary glycemic load may also be involved; these factors would allow the prediction of the relative ranking of PPBG and insulin responses to mixed meals (22). However, in a meta-analysis of randomized controlled trials, diets with a lower glycemic index were associated with only a modest improvement in A1C (−0.43%) (23). Cooking methods, processing methods, and the form of foods also influence PPBG excursion to a lesser extent. As well as meal composition, gastric emptying contributes to PPBG values (21), possibly via incretin factors. The gastric emptying rate, which has been shown to be influenced by diabetes (24), can induce some variation in peak ΔBG levels and the time at which peak ΔBG levels occur. In our study, peak BG excursion occurred around 110 min after the start of meals versus 45 min in healthy volunteers (25), and we observed a diverse range of values. Pearce et al. (13) reported similar variation in maximum glucose response times to a CHO load, with differences in the observed lag time of up to 105 min.
One of the main hurdles to a more accurate prediction of BG excursion is the wide variation in inter-individual data. Based on individual data, two groups of patients were identified: responders to CHO intake, in whom ΔBG correlated closely with CHO intake, and nonresponders, who showed a lower correlation. Responders were leaner than nonresponders and tended to have lower BMI or waist-to-hip ratios and lower C-peptide values. Responders had significantly higher PPBG excursions than nonresponders, whereas their CHO intake was significantly lower. One cannot rule out the possibility that responders might have reduced CHO intake to limit BG excursions. Responders tended to consume more lipids per meal, but the calorie intake did not differ significantly from that of nonresponders. While the low number of responders underscores the need for caution, these subjects had a more insulinopenic profile than nonresponders, who exhibited higher insulin resistance.
The strength of this study is based on the use of a CGMS, which allows detection of dynamic changes in BG concentrations unidentifiable using intermittent self-monitoring of blood glucose. This study was conducted in “typical” type 2 diabetic outpatients eating as normal, and we took care to limit sources of variability during the CGMS profile phase (no snacks and no abnormal physical exertion during this phase).
The aim of this study was to assess the relationship between BG excursion and CHO intake in ambulatory subjects with type 2 diabetes. Several conclusions can be drawn from our study: 1) breakfast seems to be the principal meal in France, i.e., the meal incurring the highest BG excursion. For the same CHO intake, compared with lunchtime, BG excursion was twice as high at breakfast and two-thirds higher at dinner. 2) BG excursion can be predicted fairly well using an equation incorporating CHO, lipid, and protein intake and mealtimes; preprandial BG values (or FBG for breakfast); A1C; basal C-peptide; BMI; waist-to-hip ratio; and age. 3) Two categories of patients were indentified according to degree of correlation between BG values and CHO intake. In insulinopenic patients, CHO intake clearly causes an increase in PPBG, whereas, in insulin-resistant patients, factors other than the CHO load predominate. This type of patient profile characterization should be used to guide therapeutic choices, favoring more targeted care and improved type 2 diabetes management.
Acknowledgments
This work was supported by an unrestricted grant from sanofi-aventis. G.C. is a consultant for sanofi-aventis.
No other potential conflicts of interest relevant to this article were reported.
S.F. wrote the manuscript, researched data, and contributed to discussion. D.D. researched data and contributed to discussion. C.P. researched data. J.-P.R. contributed to discussion. M.B. and B.B. researched data and contributed to discussion. C.P. and E.R. contributed to discussion. F.M. researched data. M.V.-V. contributed to discussion. G.C. contributed to discussion and reviewed/edited the manuscript.
Parts of this study were presented in abstract form at the Association de Langue Française pour l'Etude du DIAbète et des Maladies métaboliques (ALFEDIAM) congress, Bruxelles, March 2008, and at the 44th annual meeting of the European Association for the Study of Diabetes, Rome, Italy, 8–11 September 2008.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. UKPDS. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33): UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998;352:837–853 [PubMed] [Google Scholar]
- 2. Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA: 10-Year follow-up of intensive glucose control in type 2 diabetes (UKPDS 80): UK Prospective Diabetes Study (UKPDS) Group. N Engl J Med 2008;359:1577–1589 [DOI] [PubMed] [Google Scholar]
- 3. Nathan DM, Buse JB, Davidson MB, Heine RJ, Holman RR, Sherwin R, Zinman B: Management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2009;32:193–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. American Diabetes Association. Standards of medical care in diabetes: 2009. Diabetes Care 2009;32(Suppl. 1):S13–S61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Riddle MC, Rosenstock J, Gerich J: Insulin Glargine 4002 Study Investigators, on behalf of the Insulin Glargine 4002 Study Investigators. The treat-to-target trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care 2003;26:3080–3086 [DOI] [PubMed] [Google Scholar]
- 6. Yki-Järvinen H, Kauppinen-Mäkelin R, Tiikkainen M, Vähätalo M, Virtamo H, Nikkilä K, Tulokas T, Hulme S, Hardy K, McNulty S, Hänninen J, Levänen H, Lahdenperä S, Lehtonen R, Ryysy L: Insulin glargine or NPH combined with metformin in type 2 diabetes: the LANMET study. Diabetologia 2006;49:442–451 [DOI] [PubMed] [Google Scholar]
- 7. Monnier L, Colette C, Dunseath GJ, Owens DR: The loss of postprandial glycemic control precedes stepwise deterioration of fasting with worsening diabetes. Diabetes Care 2007;30:263–269 [DOI] [PubMed] [Google Scholar]
- 8. Ceriello A, Colagiuri S, Gerich J, Tuomilehto J: Guideline Development Group. Guideline for management of postmeal glucose. Nutr Metab Cardiovasc Dis 2008;18:S17–S33 [DOI] [PubMed] [Google Scholar]
- 9. Rodbard HW, Blonde L, Braithwaite SS, Brett EM, Cobin RH, Handelsman Y, Hellman R, Jellinger PS, Jovanovic LG, Levy P, Mechanick JI, Zangeneh F: AACE Diabetes Mellitus Clinical Practice Guidelines Task Force: American Association of Clinical Endocrinologists (AACE) Medical Guidelines for Clinical Practise for the management of Diabetes Mellitus. Endocr Pract 2007;13(Suppl. 1):1–68 [DOI] [PubMed] [Google Scholar]
- 10. Gannon MC, Nuttall FQ, Westphal SA, Fang S, Ercan-Fang N: Acute metabolic response to high-carbohydrate, high-starch meals compared with moderate-carbohydrate, low-starch meals in subjects with type 2 diabetes. Diabetes Care 1998;21:1619–1626 [DOI] [PubMed] [Google Scholar]
- 11. Sheard NF, Clark NG, Brand-Miller JC, Franz MJ, Pi-Sunyer FX, Mayer-Davis E, Kulkarni K, Geil P: Dietary carbohydrate (amount and type) in the prevention and management of diabetes: a statement by the American Diabetes Association. Diabetes Care 2004;27:2266–2271 [DOI] [PubMed] [Google Scholar]
- 12. Franc S, Dardari D, Boucherie B, Riveline JP, Biedzinski M, Petit C, Requeda E, Leurent P, Varroud-Vial M, Hochberg G, Charpentier G: Real-life application and validation of flexible intensive insulin-therapy algorithms in type 1 diabetes patients. Diabete Metab 2009;35:463–468 [DOI] [PubMed] [Google Scholar]
- 13. Pearce KL, Noakes M, Keogh J, Clifton PM: Affect of carbohydrate distribution on postprandial glucose peaks with the use of continuous glucose monitoring in type 2 diabetes. Am J Clin Nutr 2008;87:638–644 [DOI] [PubMed] [Google Scholar]
- 14. Shiraiwa T, Kaneto H, Miyatsuka T, Kato K, Yamamoto K, Kawashima A, Kanda T, Suzuki M, Imano E, Matsuhisa M, Hori M, Yamasaki Y: Post-prandial hyperglycemia is an important predictor of the incidence of diabetic microangiopathy in Japanese type 2 diabetic patients. Biochem Biophys Res Commun 2005;336:339–345 [DOI] [PubMed] [Google Scholar]
- 15. Bonora E: Postprandial peaks as a risk factor for cardiovascular disease: epidemiological perspectives. Int J Clin Pract 2002;129:5–11 [PubMed] [Google Scholar]
- 16. Franz MJ, Bantle JP, Beebe CA, Brunzell JD, Chiasson JL, Garg A, Holzmeister LA, Hoogwerf B, Mayer-Davis E, Mooradian AD, Purnell JQ, Wheeler M: American Diabetes Association. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes Care 2003;26:S51–S61 [DOI] [PubMed] [Google Scholar]
- 17. Garg A: High-monounsaturated-fat diets for patients with diabetes mellitus: a meta-analysis. Am J Clin Nutr 1998;67(Suppl.);577S–582S [DOI] [PubMed] [Google Scholar]
- 18. Nielsen H, Nielsen GL: Preprandial blood glucose values: influence on glycemic response studies. Am J Clin Nutr 1989;49:1243–1246 [DOI] [PubMed] [Google Scholar]
- 19. Jenkins DJ, Wolever TM, Taylor RH, Griffiths C, Krzeminska K, Lawrie JA, Bennett CM, Goff DV, Sarson DL, Bloom SR: Slow release dietary carbohydrate improves second meal tolerance. Am J Clin Nutr 1982;35:1339–1346 [DOI] [PubMed] [Google Scholar]
- 20. Dinneen S, Alzaid A, Turk D, Rizza R: Failure of glucagon suppression contributes to postprandial hyperglycaemia in IDDM. Diabetologia 1995;38:337–343 [DOI] [PubMed] [Google Scholar]
- 21. Gin H, Rigalleau V: Post-prandial hyperglycemia: post-prandial hyperglycemia and diabetes. Diabete Metab 2000;26:265–272 [PubMed] [Google Scholar]
- 22. Wolever TM, Yang M, Zeng XY, Atkinson F, Brand-Miller JC: Food glycemic index, as given in glycemic index tables, is a significant determinant of glycemic responses elicited by composite breakfast meals. Am J Clin Nutr 2006;83:1306–1312 [DOI] [PubMed] [Google Scholar]
- 23. Brand-Miller J, Hayne S, Petocz P, Colagiuri S: Low-glycemic index diets in the management of diabetes: a meta-analysis of randomized controlled trials. Diabetes Care 2003;26:2261–2267 [DOI] [PubMed] [Google Scholar]
- 24. Samsom M, Bharucha A, Gerich JE, Hermann K, Limmer J, Linke R, Maggs D, Schirra J, Vella A, Wörle HJ, Göke B: Diabetes mellitus and gastric emptying: questions and issues in clinical practice. Diabete Metab Res Rev 2009;25:502–514 [DOI] [PubMed] [Google Scholar]
- 25. Chapelot D, Marmonier C, Valensi P: Predicting more accurately the overall glucose response to a lunch meal by using the postprandial glucose peak. Metabolism 2007;56:37–43 [DOI] [PubMed] [Google Scholar]




