Abstract
OBJECTIVE
To investigate if oral glutamine ameliorates exercise and postexercise nighttime hypoglycemia in type 1 diabetic adolescents.
RESEARCH DESIGN AND METHODS
Ten adolescents (15.2 ± 1.4 years [SD], A1C 6.9 ± 0.9%) on insulin pumps were studied. The subjects were randomized to receive a glutamine or placebo drink pre-exercise and at bedtime (0.25 g/kg/dose). A 3:00 p.m. exercise session consisted of four 15-min treadmill/5-min rest cycles. Pre-exercise blood glucose was 140–150 mg/dl and was monitored throughout the night. Studies were randomized crossover over 3 weeks.
RESULTS
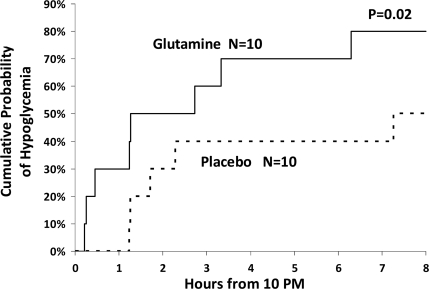
Blood glucose levels dropped comparably (52%) during exercise on both days. However, the overnight number of hypoglycemic events was higher on glutamine than placebo (≤70 mg/dl, P = 0.03 and ≤60, P = 0.05). The cumulative probability of nighttime hypoglycemia was increased on glutamine days (80%) versus placebo days (50%) (P = 0.02).
CONCLUSIONS
Glutamine increased the cumulative probability of postexercise overnight hypoglycemia compared with placebo in adolescents with type 1 diabetes. Whether glutamine may enhance insulin sensitivity postexercise requires further study in type 1 diabetes.
We observed a higher incidence of hypoglycemia during exercise and during the night following exercise versus after a sedentary day in adolescents with type 1 diabetes (1,2). Although hypoglycemia decreased by discontinuing the insulin pump during exercise, significant rebound hyperglycemia was observed (3).
Glutamine, the body's most abundant free amino acid, is thought to regulate intestinal protein synthesis and be a major source of carbon for gluconeogenesis (4). However, conflicting reported data suggest it can impair or accelerate recovery from hypoglycemia (5–7). In this pilot study we investigated if oral glutamine could ameliorate hypoglycemia during exercise and in the nighttime after exercise in children with type 1 diabetes.
RESEARCH DESIGN AND METHODS
Written consent was obtained after approval by the Wolfson Children's Hospital Institutional Review Committee. Ten adolescents (five boys and five girls; mean [SD] age 15.2 ± 1.4 years) with type 1 diabetes on insulin pump therapy were recruited. Mean diabetes duration was 6.2 ± 3.3 years; A1C, 6.9 ± 0.9%; with normal BMI, 76.9 ± 12.2 percentile. Subjects were on no other medications or dietary supplements.
Design
Regular dietary intake was maintained for at least 3 days prior to each admission to the clinical research center (CRC) and diabetes was managed as routine. Subjects were admitted mid-day, an intravenous line was placed, and blood glucose was titrated (mid 100 mg/dl) prior to 3:00 p.m. exercise. Children were randomized to receive a drink containing glutamine or placebo (PL, calorie- and nitrogen-free) before exercise and at bedtime (0.25 g/kg/dose). Patients and CRC staff were blinded to the type of drinks consumed. Sessions consisted of four 15-min treadmill cycles (heart rate ∼140 bpm) with 5-min rest breaks when blood glucose concentrations were checked for a total of 75 min. If blood glucose was <60 mg/dl, subjects consumed 15–30 g of carbohydrate and were not allowed back on the treadmill until blood >70 mg/dl. Insulin basal rates were continued during exercise. Afterward, subjects ate a snack and then dinner. Blood glucose was monitored hourly overnight from 8:00 p.m. to 8:00 a.m. Blood glucose ≤60 mg/dl prompted treatment with an oral carbohydrate; treatment was repeated as needed until >80 mg/dl. Fasting glutamine and ammonia concentrations were measured 16-h post-exercise the following morning. Subjects were discharged after breakfast and returned within 3 weeks for an identical study with either placebo or glutamine. The caloric/protein intake of the two CRC days was identical; visits were randomized crossover.
Assays
Blood glucose concentrations were measured with a Freestyle meter (Abbott Diabetes Care, Alameda, CA) and by glucose oxidase methods with a Beckman glucose analyzer (Beckman, Brea, CA). Plasma glutamine concentrations were measured by gas chromatography–mass spectrometry and ammonia using an automated chemistry analyzer.
Statistics
During exercise, hypoglycemia was considered if blood glucose was ≤70 mg/dl; if treated, the most recent previous blood glucose was carried forward 1 h in the calculations. Repeated-measures regression models were performed to compare glutamine concentrations and glucose values prior to exercise and the percentage drop during exercise, the overnight mean glucose, and the percentage of the hypoglycemic values of each visit. Rank scores (van der Waerden) were used to normalize skewed distributions. The proportions of subjects developing hypoglycemia during exercise on both visits were compared using a permutation test as was the time from 10:00 p.m. until the first laboratory glucose value ≤70 mg/dl on the 2 days; all analyses were controlled for a visit effect. SAS version 9.1 (SAS Institute, Cary, NC) and two-sided t tests were used.
RESULTS
Plasma glutamine concentrations were >50% higher the morning after glutamine administration (316 μmol/l) as compared with placebo (200 μmol/l, P < 0.001).
Exercise
Mean blood glucose concentrations prior to exercise were comparable on the glutamine and placebo day (143 ± 31 mg/dl vs. 162 ± 54, respectively; P = 0.44) with a similar percentage drop from baseline during exercise of 52 ± 15% glutamine versus 52% ± 9% placebo (P = 0.84). There was a comparable number of subjects that developed hypoglycemia during exercise on the glutamine (n = 6) or placebo day (n = 7).
Overnight
Mean nighttime postexercise low-glucose levels (≤70 mg/dl or ≤60 mg/dl) were more frequent after glutamine than after placebo (≤70 mg/dl: glutamine, 19%; placebo, 15%; P = 0.03; and ≤60 mg/dl: glutamine, 7.7%; placebo, 3.6%; P = 0.05). The cumulative probability of overnight hypoglycemia was increased on the glutamine day (80%) compared with the placebo day (50%, P = 0.02) (Fig. 1).
Figure 1.
Cumulative probability of nighttime hypoglycemia (≤70 mg/dl) if the same adolescents with type 1 diabetes took glutamine or placebo before afternoon exercise and at bedtime.
Safety
Glutamine is tasteless and odorless, so it was well tolerated. Plasma ammonia concentrations the morning after the studies were similar (glutamine: 40.2 ± 15.3 μmol/l; placebo: 41.2 ± 16.1 μmol/l, P = NS).
CONCLUSIONS
The pilot study data suggest that glutamine supplementation increases the likelihood of nighttime hypoglycemia in adolescents with type 1 diabetes after performing heavy exercise.
Morning glutamine concentrations 16-h post-exercise were >50% higher during the glutamine day versus the placebo day, however these concentrations were still below normal compared with healthy, age-matched control subjects or adolescents with type 1 diabetes measured at rest (P < 0.001) (8) and similar to those of healthy adults after prolonged exercise (9). It is possible that glutamine is low due to increased use in gluconeogenesis or use as a buffer or due to increased cortisol secretion, which enhances splanchnic glutamine utilization (10). This relative glutamine depletion after exercise requires further study.
In our study, glutamine did not affect blood glucose levels during exercise but increased the cumulative probability of nighttime hypoglycemia post-exercise. Indirect evidence suggests glutamine may indeed enhance insulin sensitivity in other experimental and clinical situations associated with insulin resistance including in the intensive care unit with trauma patients (11,12) and in children with cystic fibrosis on growth hormone (13). Glutamine increased insulin signaling/sensitivity in skeletal muscle in experimental animals (14), and oral glutamine increased nonoxidative glucose disposal in healthy exercising subjects (15).
Our pilot study, however, has several limitations including its small sample size, the low concentrations of glutamine achieved, and no direct measurement of insulin sensitivity. These results are nonetheless intriguing as the investigation of nutritional, nonpharmacological avenues to improve diabetes control is important and deserves further study, particularly in teenagers who have increased insulin resistance. In the aggregate, these data are congruent with the positive effect of glutamine on insulin sensitivity.
In conclusion, oral glutamine administration was associated with a higher incidence of nighttime post-exercise hypoglycemia as compared with placebo in a pilot group of adolescents with type 1 diabetes. Whether glutamine supplementation affects peripheral and/or hepatic insulin sensitivity requires further study in children with type 1 diabetes.
Acknowledgments
This work was funded by grants from the National Institutes of Health's Eunice Kennedy Shriver National Institute of Child Health and Human Development: U10HD041918-06 (to N.M.) and HD041906-02 (to D.X.).
No potential conflicts of interest relevant to this article were reported.
N.M. is the principal investigator of the studies. She wrote the grant, recruited the subjects, carried out the experiments, analyzed the data, and wrote the paper. D.X. is the principal biostatistician of the study and helped analyze the data and create the graphs and wrote the statistical section. L.A.F. is a co-investigator and helped recruit and treat the patients in the CRC and reviewed and critiqued the manuscript. K.E. is the lead study coordinator in charge of all implementation aspects of the study. D.D. is a co-investigator who assisted N.M. in grant writing, data analysis and interpretation and assisted in the writing of the paper.
Parts of this study were presented in abstract form at the 69th Scientific Sessions of the American Diabetes Association, New Orleans, Louisiana, 5–9 June 2009.
The authors are grateful to Shawn Sweeten for laboratory technical assistance and to Shiela Smith and the expert nursing staff of the Wolfson Children's Hospital CRC for the expert care of our subjects.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. Tansey MJ, Tsalikian E, Beck RW, Mauras N, Buckingham BA, Weinzimer SA, Janz KF, Kollman C, Xing D, Ruedy KJ, Steffes MW, Borland TM, Singh RJ, Tamborlane WV: Diabetes Research in Children Network (DirecNet) Study Group. The effects of aerobic exercise on glucose and counterregulatory hormone concentrations in children with type 1 diabetes. Diabetes Care 2006;29:20–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tsalikian E, Mauras N, Beck RW, Tamborlane WV, Janz KF, Chase HP, Wysocki T, Weinzimer SA, Buckingham BA, Kollman C, Xing D, Ruedy KJ: Diabetes Research in Children Network (DirecNet) Study Group. Impact of exercise on overnight glycemic control in children with type 1 diabetes mellitus. J Pediatr 2005;147:528–534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Diabetes Research in Children Network (DirecNet) Study Group, Tsalikian E, Kollman C, Tamborlane WB, Beck RW, Fiallo-Scharer R, Fox L, Janz KF, Ruedy KJ, Wilson D, Xing D, Weinzimer SA: Prevention of hypoglycemia during exercise in children with type 1 diabetes by suspending basal insulin. Diabetes Care 2006;29:2200–2204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hankard RG, Haymond MW, Darmaun D: Role of glutamine as a glucose precursor in fasting humans. Diabetes 1997;46:1535–1541 [DOI] [PubMed] [Google Scholar]
- 5. Battezzati A, Benedini S, Fattorini A, Piceni Sereni L, Luzi L: Effect of hypoglycemia on amino acid and protein metabolism in healthy humans. Diabetes 2000;49:1543–1551 [DOI] [PubMed] [Google Scholar]
- 6. Souza HM, Borba-Murad GR, Curi R, Galletto R, Bazotte RB: Combined administration of glucose precursors is more efficient than that of glucose itself in recovery from hypoglycemia. Res Commun Mol Pathol Pharmacol 2001;110:264–272 [PubMed] [Google Scholar]
- 7. Garcia RF, Gazola VA, Barrena HC, Hartmann EM, Berti J, Toyama MH, Boschero AC, Carneiro EM, Manso FC, Bazotte RB: Blood amino acids concentration during insulin induced hypoglycemia in rats: the role of alanine and glutamine in glucose recovery. Amino Acids 2007;33:151–155 [DOI] [PubMed] [Google Scholar]
- 8. Hankard RG, Haymond MW, Darmaun D: Role of glucose in the regulation of glutamine metabolism in health and in type 1 insulin-dependent diabetes. Am J Physiol Endocrinol Metab 2000;279:E608–E613 [DOI] [PubMed] [Google Scholar]
- 9. Gleeson M: Dosing and efficacy of glutamine supplementation in human exercise and sport training. J Nutr 2008;138:2045S–2049S [DOI] [PubMed] [Google Scholar]
- 10. Thibault R, Welch S, Mauras N, Sager B, Altomare A, Haymond M, Darmaun D: Corticosteroids increase glutamine utilization in human splanchnic bed. Am J Physiol Gastrointest Liver Physiol 2008;294:G548–G553 [DOI] [PubMed] [Google Scholar]
- 11. Déchelotte P, Hasselmann M, Cynober L, Allaouchiche B, Coëffier M, Hecketsweiler B, Merle V, Mazerolles M, Samba D, Guillou YM, Petit J, Mansoor O, Colas G, Cohendy R, Barnoud D, Czernichow P, Bleichner G: L-alanyl-L-glutamine dipeptide-supplemented total parenteral nutrition reduces infectious complications and glucose intolerance in critically ill patients: the French controlled, randomized, double-blind, multicenter study. Crit Care Med 2006;34:598–604 [DOI] [PubMed] [Google Scholar]
- 12. Bakalar B, Duska F, Pachl J, Fric M, Otahal M, Pazout J, Andel M: Parenterally administered dipeptide alanyl-glutamine prevents worsening of insulin sensitivity in multiple-trauma patients. Crit Care Med 2006;34:381–386 [DOI] [PubMed] [Google Scholar]
- 13. Darmaun D, Hayes V, Schaeffer D, Welch S, Mauras N: Effects of glutamine and recombinant human growth hormone on protein metabolism in prepubertal children with cystic fibrosis. J Clin Endocrinol Metab 2004;89:1146–1152 [DOI] [PubMed] [Google Scholar]
- 14. Prada PO, Hirabara SM, de Souza CT, Schenka AA, Zecchin HG, Vassallo J, Velloso LA, Carneiro E, Carvalheira JB, Curi R, Saad MJ: L-glutamine supplementation induces insulin resistance in adipose tissue and improves insulin signalling in liver and muscle of rats with diet-induced obesity. Diabetologia 2007;50:1949–1959 [DOI] [PubMed] [Google Scholar]
- 15. Bowtell JL, Gelly K, Jackman ML, Patel A, Simeoni M, Rennie MJ: Effect of oral glutamine on whole body carbohydrate storage during recovery from exhaustive exercise. J Appl Physiol 1999;86:1770–1777 [DOI] [PubMed] [Google Scholar]