Abstract
OBJECTIVE
We examined the relationships of visceral fat area (VFA), subcutaneous fat area, and waist circumference, determined using computed tomography (CT), and BMI with metabolic risk factors in a large Japanese population.
RESEARCH DESIGN AND METHODS
Study subjects comprised 6,292 men and women who participated in the Hitachi Health Study and received CT examinations in 2007 and 2008.
RESULTS
Regarding the clustering of metabolic risk factors, the odds ratios (ORs) for the VFA quintiles were 1.0 (ref.), 2.4, 3.4, 5.0, and 9.7 for men and 1.0 (ref.), 1.5, 2.6, 4.6, and 10.0 for women (P < 0.001 for trends in both sexes). For the highest quintiles, the OR for VFA was 1.5 to 2 times higher than those of the other anthropometric indexes in both sexes.
CONCLUSIONS
We demonstrated a superior performance of VFA to predict the clustering of metabolic risk factors compared with other anthropometric indexes.
Metabolic syndrome (MS) has been growing globally with the clusters of obesity, high blood pressure, impaired lipid metabolism, and hyperglycemia. Individuals with MS have a higher risk of cardiovascular disease and a subsequent increase in disease mortality or morbidity (1–3). For the diagnosis of MS, waist circumference (WC) is almost always used as one of the criteria, and this measure is typically used as a simplified measure of the visceral fat area (VFA) (4–7). Visceral fat is regarded as an endocrine organ that secretes adipocytokines and other vasoactive substances that can influence the risk of developing traits of MS (8). A few studies have shown the impact of visceral fat on MS and its components in large-scale epidemiological research efforts (9). The present study analyzed the epidemiological impact of VFA compared with that of subcutaneous fat area (SFA), WC, and BMI against the clustering of metabolic risk factors and its components.
RESEARCH DESIGN AND METHODS
Of 17,606 employees and their spouses who, after more than 12 h of fasting, underwent a health examination in Hitachi, Ibaraki Prefecture, between 2007 and 2008, we analyzed data for 6,292 subjects (5,606 men and 686 women), aged 26 to 75 years, who underwent a computed tomography (CT) examination, answered a questionnaire on lifestyle and health, and did not have a history of serious illness (cancer, cerebrovascular disease, or myocardial infarction). VFA, SFA, and WC were measured using a CT scanner according to a protocol described elsewhere (10). The present study was approved by the ethics committee of the National Center for Global Health and Medicine. Written informed consent was obtained from all subjects.
In this study, subjects with two or more of the four risk factors (high blood pressure, high triglyceride, low HDL cholesterol, and hyperglycemia) defined in the criteria of the National Cholesterol Education Program's Adult Treatment Panel III guidelines in 2005 (6), except for WC, were defined as having the clustering of metabolic risk factors. Subjects currently receiving treatment for hyperlipidemia, hypertension, or diabetes were deemed as having the respective risk factors, regardless of the biochemical values.
We divided the subjects into quintiles (Q1 to Q5) according to each anthropometric value and calculated the odds ratio (OR) of the clustering of metabolic risk factors and its components adjusted for age, smoking habits, alcohol consumption, and regular physical activity using a logistic regression analysis, with Q1 as the reference. All analyses were performed using SPSS for Windows, Version 15.0 (SPSS, Chicago, IL).
RESULTS
The mean VFA was 123.7 ± 51.2 cm2 in men and 85.1 ± 45.2 cm2 in women. The mean SFA was 134.8 ± 56.6 cm2 in men and 182.5 ± 72.9 cm2 in women. The ratio of VFA to SFA was ∼1:1 for men and 1:2 for women. The mean WC was 86.4 ± 8.3 cm in men and 83.2 ± 9.2 cm in women. The mean BMI was 24.1 ± 3.0 kg/m2 in men and 23.0 ± 3.3 kg/m2 in women. The prevalence of the clustering of metabolic risk factors was 46.0% in men and 30.0% in women.
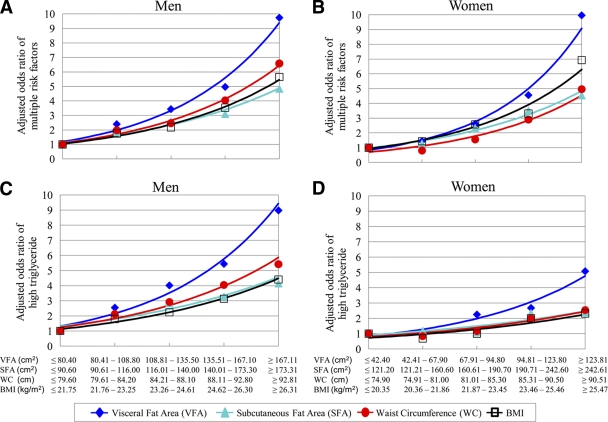
In Fig. 1, the ORs for the clustering of metabolic risk factors are shown according to each anthropometric index. The OR was 1.5 to 2 times higher for the Q5 VFA category than for the other Q5 categories for both men and women. The OR (95% CI) of the VFA quintiles were, respectively, 1.0, 2.4 (2.0–2.9), 3.4 (2.8–4.2), 5.0 (4.1–6.0), and 9.7 (8.0–11.9) for men and 1.0, 1.5 (0.7–3.2), 2.6 (1.3–5.3), 4.6 (2.3–9.1), and 10.0 (5.0–19.9) for women (P < 0.001 for trends in both sexes). According to the SFA quintiles, ORs were, respectively, 1.0, 1.8 (1.5–2.2), 2.6 (2.2–3.1), 3.1 (2.6–3.7), and 4.8 (4.0–5.8) for men and 1.0, 1.3 (0.7–2.5), 2.3 (1.3–4.3), 3.5 (1.9–6.4), and 4.5 (2.5–8.4) for women (P < 0.001 for trends in both sexes).
Figure 1.
ORs for high triglyceride and the clustering of metabolic risk factors according to the quintiles (Q1–Q5) of VFA, SFA, WC, and BMI adjusted for age, smoking habits (never, current, past), alcohol consumption (nondrinker, drinker consuming two go or less per day [a go is a conventional unit of alcohol intake in Japan and contains ∼23 g of ethanol], or consuming more than two go per day), and regular fitness habit (yes/no). The symbols are the estimated ORs using Q1 as the reference category. The curves are fitted by the logistic regression models. The slope for VFA is significantly steeper than those for SFA, WC, and BMI on high triglyceride and on clustering of metabolic risk factors (P < 0.05) except for that on the clustering of metabolic risk factors in women. (A high-quality digital representation of this figure is available in the online issue.)
The OR for a high triglyceride level, a low HDL level, high blood pressure, and hyperglycemia increased with increasing quintile categories of each anthropometric index. The OR (95% CI) of the Q5 VFA category for a high triglyceride level was 9.0 (7.3–11.1) in men and for a low HDL level was 7.1 (4.8–10.5) in men and 11.0 (4.0–30.1) in women, exhibiting extremely high ORs.
The slope for VFA is significantly steeper than those for SFA, WC, and BMI on high triglyceride and on clustering of metabolic risk factors (P < 0.05) except for the slope on the clustering of metabolic risk factors in women.
CONCLUSIONS
In the present study, a stronger association between an increasing VFA and the clustering of metabolic risk factors and its components than for an increasing SFA, WC, or BMI was observed. Among metabolic risk factors, a high triglyceride level in men and a low HDL cholesterol level in both men and women showed particularly strong associations with VFA.
BMI and WC are used clinically to measure obesity, but do not exactly reflect visceral adiposity. A previous report showed that some individuals with a normal BMI and WC actually had an excessive amount of visceral fat and metabolic risk factors (11). In our study, the ORs for the clustering of metabolic risk factors were similar for BMI and WC in men, but the OR for WC was lower than that for BMI (which was similar to that for SFA) in women. The OR of VFA and SFA differed according to sex. Furthermore, a stronger correlation was observed between WC and SFA than between WC and VFA. Fox et al. (9) reported similar results. These findings suggest that WC measurements in women may have the same meaning as SFA measurements, explaining the similarity of the OR for the clustering of metabolic risk factors in WC and SFA.
The present study adds evidence to support an important role for VFA in the pathogenesis of metabolic risk factor clustering in Japanese adults. Further studies are needed to confirm this association prospectively and to examine the impact of VFA on the risk of cardiovascular disease.
Acknowledgments
This study was supported by a grant from the Ministry of Health, Labor and Welfare of Japan.
No potential conflicts of interest relevant to this article were reported.
Y.M. derived the hypothesis, collated data from the Hitachi Health Study trials, planned and performed the analyses, and wrote the manuscript. T.N. and S.Y. collected data. T.Y. advised on analyses and commented on drafts of the manuscript. T.N., Y.T., T.Y., M.N., and T.M. contributed to the interpretation and discussion of the results. This report was critically reviewed and subsequently approved by all authors.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, Salonen JT: The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA 2002;288:2709–2716 [DOI] [PubMed] [Google Scholar]
- 2. Isomaa B, Almgren P, Tuomi T, Forsén B, Lahti K, Nissén M, Taskinen MR, Groop L: Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 2001;24:683–689 [DOI] [PubMed] [Google Scholar]
- 3. Grundy SM, Brewer HB, Jr, Cleeman JI, Smith SC, Jr, Lenfant C: American Heart Association, National Heart, Lung, and Blood Institute. American Heart Association, National Heart, Lung, and Blood Institute. Definition of metabolic syndrome: report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation 2004;109:433–438 [DOI] [PubMed] [Google Scholar]
- 4. World Health Organization. Definition, Diagnosis and Classification of Diabetes and its Complications: Report of a WHO consultation. Geneva, World Health Org., 1999 [Google Scholar]
- 5. A new worldwide definition of the metabolic syndrome [article online], 2005. Brussels, Belgium, International Diabetes Federation. Available from http://www.idf.org/node/1271?unode=1120071E-AACE-41D2–9FA0-BAB6E25BA072. Accessed 3 July 2009 [Google Scholar]
- 6. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC, Jr, Spertus JA, Costa F: American Heart Association, National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005;112:2735–2752 [DOI] [PubMed] [Google Scholar]
- 7. Matsuzawa Y: Metabolic syndrome—definition and diagnostic criteria in Japan. J Atheroscler Thromb 2005;12:301. [DOI] [PubMed] [Google Scholar]
- 8. Wajchenberg BL: Subcutaneous and visceral adipose tissue: their relation to the metabolic syndrome. Endocr Rev 2000;21:697–738 [DOI] [PubMed] [Google Scholar]
- 9. Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich-Horvat P, Liu CY, Vasan RS, Murabito JM, Meigs JB, Cupples LA, D'Agostino RB, Sr, O'Donnell CJ: Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation 2007;116:39–48 [DOI] [PubMed] [Google Scholar]
- 10. Yamamoto S, Nakagawa T, Matsushita Y, Kusano S, Hayashi T, Irokawa M, Aoki T, Korogi Y, Mizoue T: Visceral fat area and markers of insulin resistance in relation to colorectal neoplasia. Diabetes Care 2010;33:184–189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ross R, Rissanen J, Hudson R: Sensitivity associated with the identification of visceral adipose tissue levels using waist circumference in men and women: effects of weight loss. Int J Obes Relat Metab Disord 1996;20:533–538 [PubMed] [Google Scholar]