Abstract
Social support has been reliably related to better physical health outcomes. One influential model suggests that social support is related to lower cardiovascular disease mortality because it reduces the potentially deleterious consequences of cardiovascular reactivity during acute stress. However, received support and perceived support are separable constructs and epidemiological research suggests variability in links between received support and health. This is important because most social support and acute laboratory stress studies are essentially based on the receipt of support. In this paper, we focus on the conceptualization of received support and its implications for understanding links to support laboratory reactivity paradigms. This analysis highlights the role of theoretically important task, recipient, and provider categories of factors that moderate the effectiveness of received support, as well as the need to examine links between naturalistic perceptions of support and cardiovascular reactivity during stress.
Social support has been reliably related to lower rates of morbidity and mortality, especially from cardiovascular disease (Berkman, Glass, Brissette, & Seeman, 2000; Cohen, 1988; Uchino, 2004). A critical question in this area relates to the underlying biological mechanisms that may be responsible for such links (Uchino, 2004). One prominent perspective is the stress-buffering model of support which suggests that social support may reduce mortality by decreasing harmful cardiovascular reactions during stress (Kamarck, Jennings, and Manuck, 1990). This conceptual link is important because through this reactivity-buffering process, social support may reduce both the development of cardiovascular disease (morbidity) and its clinical course (mortality).
There are at least two important assumptions that may dramatically influence the plausibility of links between social support and reactivity in the laboratory. First, is the assumption that cardiovascular reactivity influences cardiovascular disease. Of course, cardiovascular reactivity is an “intermediate” health endpoint that researchers hypothesize to be linked to health. Although more work is needed, there is preliminary evidence for links between reactivity and cardiovascular disease in both healthy and clinical populations (Treiber, Kamarck, Schneiderman, Sheffield, Kapuku, & Taylor 2003). Second, it is assumed that the operationalization of support in epidemiological studies is similar to those studies modeling support and reactivity in laboratory stress studies. This is the issue that we will focus on in the present review.
Epidemiological Links Between Social Support and Health
The two major operationalizations of functional support in epidemiological studies include general perceived and received support. Perceived support refers to one's potential access to social support, whereas received support refers to the reported receipt of support resources usually during a specific time frame (Dunkel-Schetter & Bennett, 1990). It is important to note that these two dimensions do not appear to be interchangeable (Wills & Shinar, 2000). For instance, these aspects of support are not highly correlated and beneficial effects of perceived support may be obtained in the absence of any actual support being provided (Cohen, 1988). Indeed, the separability of perceived and received support is well-documented (Wills & Shinar, 2000; Uchino, 2009). Of particular importance is that these measures of support are often associated with different physical health outcomes in epidemiological work. There is consistent evidence linking general perceived social support with reduced disease development (i.e., incidence) and mortality, especially from cardiovascular disease (e.g., Orth-Gomér, Rosengren, & Wilhelmsen, 1993). However, measures of received support have been quite variable in their links to physical health (Uchino, 2004). In fact, a number of studies find it to be associated with higher mortality rates, an effect that does not appear to simply reflect higher levels of support mobilization for those most unhealthy to begin with (e.g., Forster & Stoller, 1992; Sabin, 1993).
A General Model of Received Support and Health
The inconsistent epidemiological findings linking received support to health outcomes is important because much of the prior support and laboratory reactivity studies examined manipulations of received support. We have argued that perceived support and received support appear to have different antecedent processes and thus are separable constructs with distinct issues for consideration in their application. More specifically, perceived support appears to have its origins in positive early family environments (e.g., nurturance, lack of conflict) and hence co-develops along with other positive psychosocial processes (e.g., self-esteem, social skills, Flaherty & Richman, 1986; Sarason, Sarason, & Shearin, 1986; Shaw, Krause, Chatters, Connell, & Ingersoll-Dayton, 2004).
On the other hand, received support is more likely to represent a situational factor that is sought and / or provided in response to stress (Barrera, 2000). This conceptualization is consistent with various coping models that include support seeking as a potential coping resource (Carver, Scheier, & Weintraub, 1989; Thoits, 1986). Viewed in this way, received support is simply one of many different problem- and emotion-focused coping strategies (e.g., planning, self-medication) available to the individual during stress. This conceptual distinction has important implications for the modeling of received support in the laboratory and the conditions under which it might be beneficial, or in some cases even harmful. That is, the efficacy of received support (like any coping response) may be influenced by the context in which stress and “supportive” interpersonal exchanges occur (Berg & Upchurch, 2007). For instance, Lehman, Ellard, and Wortman (1986) have reported that bereaved individuals report a significant amount of unhelpful support attempts (e.g., encouraging quicker recovery). They have argued that individuals interacting with the bereaved may experience considerable anxiety as they do not want to say anything that might further upset the person. Thus, even though individuals may know how to be helpful, this anxiety may interfere with the retrieval of effective support skills (Lehman et al., 1986).
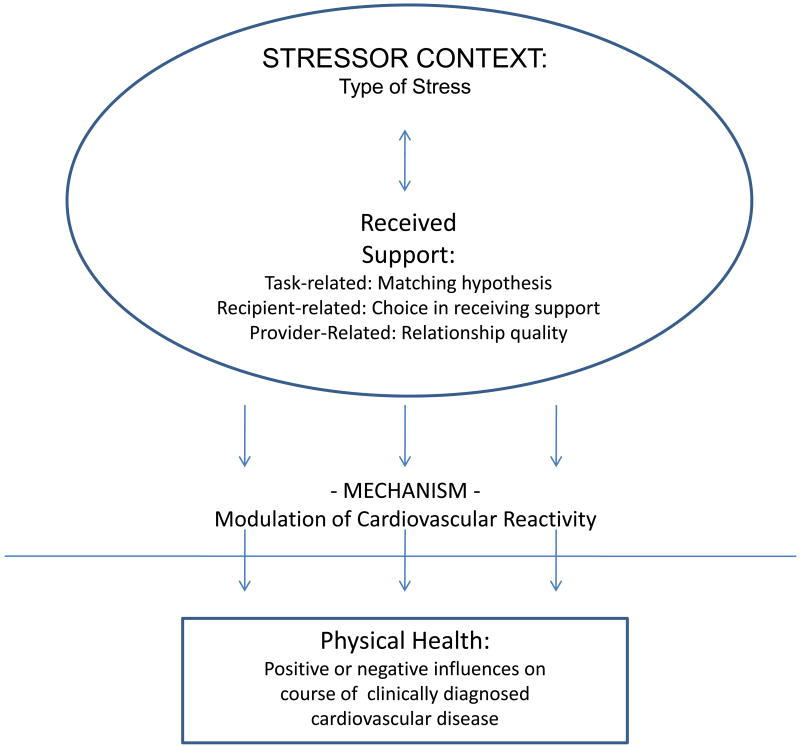
We have thus proposed a general model on the health effects of received support (Uchino, 2009). Applied to the support-reactivity hypothesis, as shown in the top half of Figure 1, there are at least three important classes of contextual processes linking received support to reactivity: (1) task-related factors such as the type of support and its match to the needs associated with distinct stressor, (2) recipient-related factors like whether one has chosen to receive the support, and (3) provider-related factors such as the quality of the relationship (Barbee, Gulley, & Cunningham, 1990; Dunkel-Schetter & Skokan, 1990; Wills & Shinar, 2000). These contextual processes may then influence cardiovascular disease in a protective or harmful fashion by modulating cardiovascular reactivity during stress.
Figure 1.
General framework on the categories of factors influencing the efficacy of received support and its potential links to health.
Cardiovascular reactivity may then influence either the development or clinical course of diagnosed cardiovascular disease as these processes are separable (e.g., initial vascular injury in comparison to ischemia / arrhythmia; Krantz & Manuck, 1984; Rozanski, Blumenthal, & Kaplan, 1999). However, as shown in Figure 1, we hypothesize that received support should be associated only with the course of clinically diagnosed cardiovascular disease which can be either beneficial or detrimental depending on the contextual processes noted above. We do not predict that received support influences the development of cardiovascular disease because (a) of the variability associated with the effectiveness of received support in coping with stress, (b) of the potential for stress to erode support even from close relationships (Bolger, Foster, Vinokur, & Ng, 1996), and (c) it is just one of many coping options available to individuals. These theoretical issues have important implications for the inconsistent epidemiological links observed between received support and mortality and its subsequent modeling in laboratory contexts.
Links to Laboratory Reactivity Studies
In general, laboratory studies suggest that received support decreases cardiovascular reactivity during acute stress (Gerin, Pieper, Levy, & Pickering, 1992; Lepore, Allen, & Evans, 1993). In these laboratory studies, either a friend or stranger (i.e., experimenter, confederate) provides the participant with support while they are undergoing a standardized stress task (e.g., speech). The most common support provided has been emotional support conveyed in a non-threatening manner that matches the needs of the current situation (e.g., esteem-building). In fact, the receipt of emotional support is typically viewed as more nurturant and less controlling than either informational or tangible support (Trobst, 2000). Consistent with these findings, a meta-analysis by Thorsteinsson and James (1999) found that received support was related to lower heart rate, systolic blood pressure (SBP), and diastolic blood pressure (DBP) reactivity. However, several moderators of this association were also found (Thorsteinsson & James, 1999). In particular, effect sizes differed as a function of evaluation potential of the support provider (i.e., low vs. high), mode of support (i.e., silent vs. active), and type of task (i.e., speech vs. math). These findings, along with subsequent work in the area highlight the importance of the support context when assessing links between received support and laboratory stress reactivity (e.g., Craig & Deichert, 2002; Holt-Lunstad, Uchino, Smith, & Hicks, 2007; O'Donovan & Hughes, 2008; Phillips, Gallagher, & Carroll, 2009).
Moderators of the links between received support in the laboratory and cardiovascular reactivity are consistent with a contextual approach, and also suggest important avenues for future work based on the broader literature. As shown in Figure 1, one important class of contextual processes is task-related factors as represented by the matching hypothesis of support (Cutrona & Russell, 1990). This model predicts that the effectiveness of support depends on the match between the stressor demands and type of support received. More specifically, the matching hypothesis predicts that instrumental support should be most effective for controllable events (e.g., preparing for a job interview), whereas emotional support should be most effective for uncontrollable events (e.g., job layoff; Cutrona & Russell, 1990).
In most existing reactivity studies emotional support is received and matches well the needs of the laboratory stressor context. However, a few studies have varied the type of support provided in order to directly compare the efficacy of different types of received support (Craig & Deichert, 2002; Uno, Uchino, & Smith, 2002; Wilson, Kliewer, Bayer, Jones, Welleford, Heiney, & Sica, 1999). These studies examined the matching hypothesis in the context of gender differences in preference for support (i.e., recipient factors). For instance, Flaherty and Richman (1989) argue that socialization processes result in women both preferring and benefiting more from the specific dimension of emotional support. Likewise, it has been argued that men may benefit more from instrumental support, especially from other men (Craig & Deichert, 2002). Results from two studies suggest that men receiving instrumental support had lower cardiovascular reactivity compared to when they received emotional support (Craig & Deichert, 2002; Wilson et al., 1999). Uno and colleagues (2002) also found that women under stress showed lower cardiac output reactivity when provided with emotional support from a purely supportive friend.
There are other important task-related factors that may influence the efficacy of received support. The meta-analysis by Thorsteinsson and James (1999) suggests the importance of task-related evaluation potential and the type of task performed. According to a contextual view of received support, task evaluation potential interferes with received support by making salient performance goals (Snydersmith & Cacioppo, 1992). Similarly, the math task may be associated with lower effect sizes because support providers can more easily evaluate how well the participant is performing (Snydersmith & Cacioppo, 1992). Basically, high task-related evaluation potential may increase threats to self and offset any benefits one might expect to see even in situations in which the “proper” support was received.
Recipient-related factors can also influence links between received support and lab-based cardiovascular reactivity. As noted above, the studies on gender differences may also reflect the influence of recipient preferences for support that are associated with gender. In addition, Phillips and colleagues (2009) found that women had lower cardiovascular reactivity when receiving emotional support from male friends, but higher reactivity when receiving emotional support from female friends. These results were interpreted as reflecting heightened evaluation from a close, similar other (Phillips et al., 2009).
Based on the broader literature on received support, there are several other recipient-related processes that appear important to investigate in future reactivity studies. One important factor is whether or not support is actually chosen by the recipient (Bolger & Amarel, 2007). There is a distinction between anterogatory (prior to seeking support) and postrogatory (after decision is made to seek support) phases of the support process. It has been argued that received support is more likely to be beneficial in the postrogatory phase where the choice to seek support has been made (Bolger & Amarel, 2007). In the absence of the decision to seek support, simply providing an individual with it may threaten their sense of esteem by communicating feelings of inefficacy or producing feelings of guilt or indebtedness (Bolger & Amarel, 2007; Fisher & Nadler, 1986). As a result, Bolger and colleagues (2000, 2007) have argued that “invisible support” (i.e., support given that is not noticed as such) may be especially beneficial in the anterogatory phase because it does not result in negative psychological reactions that can override support. This is important because all prior received support and reactivity studies that we are aware of have simply provided support in the anterogatory phase. It might be predicted that the effects of support on reactivity would be even stronger once the choice to receive support has been made and hence participants are more receptive to it.
A second recipient-related factor that may be important to consider in future support and reactivity work is the goals of the recipient (Horowitz Krasnoperova, Tater, Hansen, Person, Glavin, & Nelson, 2000). Horowitz and colleagues (2000) argue that the person seeking support wants something (i.e., has a goal) and more beneficial influences might be obtained if the support provider is able to understand such goals and the appropriate response (e.g., action-facilitating support for agentic problems). They found that when the goals of the recipient were matched with the preferred support type, satisfaction with support was greater.
There are also support provider characteristics that need consideration (Holt-Lunstad et al., 2007). One key point is that conflict in relationships can undermine the effectiveness of received support. We have shown in a number of laboratory studies that the co-existence of positivity and negativity in provider relationships can decrease the efficacy of received support (Holt-Lunstad et al., 2007; Uno et al., 2002). For instance, Holt-Lunstad and colleagues (2007) randomly assigned participants to interact with an ambivalent friend (containing both positive and negative aspects) or supportive friend (containing primarily positive aspects). Individuals receiving support from an ambivalent friend did not appear to benefit from the support received as evidenced by their higher levels of SBP reactivity during a disclosure task.
Another important provider characteristics is represented by the type of relationship giving support. Gender has received some attention (e.g., Glynn, Christenfeld, and Gerin, 1999; Philip et al., 2009) while some laboratory reactivity studies have also varied whether a stranger or friend provides support (Christenfeld, et al., 1997; Phillips et al., 2009). In a controlled test of such differences, Christenfeld and colleagues (1997) trained friends and strangers to provide the same type of support to participants. Results during a subsequent laboratory stress assessment revealed that friends had a stronger stress-buffering effect on cardiovascular reactivity compared to strangers despite receiving the same objective support. These findings may be consistent with prior work on the quality of the relationship as friends are probably seen as higher quality relationships than strangers.
Finally, intriguing recent work suggesting that the goals of the support provider may have implications for links between receiving support and cardiovascular reactivity. Crocker and Canevello (2008) argue that individuals possess relationship goals that are compassionate (i.e., focus on supporting others, not to obtain something for the self) and/or self-image (i.e., focus is on defending a view of self or obtain something for the self) oriented. Importantly, individuals with compassionate goals tend to provide more effective support over time (Crocker & Canevello, 2008), perhaps due to their responsiveness (Maisel & Gable, 2009).
What next? Implications for Examining Support - Reactivity Links
The present analyses argues for the separability of perceived and received support. As noted above, most of the prior laboratory reactivity work has examined the receipt of support. Based on epidemiological work, such studies will have to pay close attention to the contextual factors that may moderate such links. These studies can clarify the conditions under which received support can have beneficial, null, or detrimental influences on health as indexed by their influence on cardiovascular reactivity. In fact, some of the inconsistencies in prior work may reflect such differences. Most prior studies examining these contextual moderators have included factors such as gender that have influences in several categories. However, this analysis makes clear that separating out such effects on these contextual categories will require more complex designs (e.g., both male and female recipients and providers). One strength of the present framework is it would allow for a more systematic investigation of such contextual variables based on task, recipient, and provider factors.
The present analysis also makes salient the need to more closely model the phenomenon of interest based on epidemiological work linking social support to morbidity and mortality. This issue is analogous to prior research examining the generalizability of lab-based cardiovascular reactivity. The reactivity hypothesis assumes that lab-based stress is an index of how individuals respond to stress in their daily life (Pickering & Gerin, 1990). In basic reactivity research, there has been a number of studies examining this issue with mixed results (e.g., Cornish, Blanchard, & Jaccard, 1994; Light, Turner, Hinderliter, & Sherwood, 1993). However, Kamarck and colleagues (2003) have recently shown that adopting a multilevel approach that models daily threats and factors present in both laboratory and field assessments (e.g., posture, activity) results in better correspondence. These findings suggest the potential utility of more closely matching laboratory support-reactivity protocols with epidemiological studies that utilize (a) existing network relationships (e.g., friends, spouse, other family), (b) naturalistic perceptions of support (see below), and (c) different patient populations (e.g., healthy and clinically diagnosed cardiovascular patients). Adopting such an approach more systematically can inform both literatures as reactivity researchers have argued for the need to better incorporate social processes in order to increase the generalizability of reactivity assessments (Lassner, Matthews, & Stoney, 1994).
We should note that the present conceptual analysis make salient several alternative ways of testing links between social support and reactivity. Given that perceived and received support are not redundant constructs, studies might also test whether naturalistic perceived support is related to cardiovascular reactivity during stress or if there are interactions between perceived and received support. There are several studies that have taken the first approach (Craig, Lynch, & Quartner, 2000; Hughes & Curtis, 2000; Nausheen, Gidron, Gregg, Tissarchondou, & Peveler, 2007; Roy, Steptoe, & Kirschbaum, 1998). In these studies, researchers have measured perceived network support and linked it to cardiovascular reactivity during acute stress. Results from these studies are not conclusive as several studies found perceptions of network support to predict greater cardiovascular reactivity (Hughes & Curtis, 2000; Roy et al., 1998), while others found it predicted decreased cardiovascular reactivity (Craig et al., 2000; Nausheen et al., 2007). However, it should be noted that Roy and colleagues (1998) also found perceived network support to predict quicker cardiovascular recovery which may reflect a “toughened” physiological response (Dienstbier, 1989). Moreover, a study by Hughes (2007) found that perceived network support predicted cardiovascular response habituation in women. These data highlight the potential utility of examining individual differences in perceived support in reactivity studies, as well as the need to consider other indices of cardiovascular function in laboratory protocols (e.g., habituation, recovery).
The present conceptual analysis also makes salient the importance of examining possible interactions between perceived and received support as these are not redundant constructs. There is only one such study we are aware of in the reactivity literature (O'Donovan & Hughes, 2008). These authors examined the potential interactions between perceived network support and a laboratory support manipulation. Consistent with the importance of such an approach, they found that only individuals low in perceived network support showed stress-buffering effects on cardiovascular reactivity when provided with laboratory support (O'Donovan & Hughes, 2008). These results are consistent with earlier research by Sarason and colleagues (1986) who found similar benefits for low perceived support individuals on measures of cognitive performance. These results suggest that individuals low in perceived support may benefit more from receiving support perhaps due to a higher need (Nausheen et al., 2007). It is also possible that individuals high in perceived support may not benefit because they are also high in other psychological processes (e.g., self-esteem) that may interfere with receiving support (Uchino, 2009). These data highlight the need to examine both types of support operationalizations (as well as their interaction) in future work. Such modeling can contribute to the broader social support literature and provide more links to existing epidemiological work.
The research on received support and reactivity using provider-related factors such as relationship quality or status (e.g., friend, stranger) also introduces a complexity into the general model depicted in Figure 1. That is, the distinction between general and relationship-specific perceptions of support (Lakey & Scoboria, 2005). These are not redundant constructs and relationship-specific assessments appear to more strongly reflect trait X situational influences (Lakey, McCabe, Fisicaro, & Drew, 1996). Given that relationship-specific measures contain a mix of both general support perceptions (i.e., trait) and received support (i.e., situational experiences with that relationship), we have argued that they may have more general influences on both the development and clinical course of cardiovascular disease (Uchino, 2009). Laboratory reactivity paradigms can test these predictions by examining links to different epidemiological outcomes (e.g., cardiovascular disease incidence or mortality) and / or testing different patient populations (e.g., healthy or diagnosed cardiovascular disease).
The present framework also highlights the conceptually important mediators of links between support and cardiovascular reactivity. For instance, in some cases receiving support may increase reactivity by threatening a person's sense of esteem or independence (Bolger & Amarel, 2007). In other cases it may be beneficial due to increases in perceived partner responsiveness (Reis, 2007). The present analysis provides a systematic conceptual approach to examining such pathways. Importantly, elucidating such psychological pathways is generally seen as one of the most important issues facing research on social support and health (House, 2001). Future research should also include an emphasis on delineating more complex physiological pathways. This is significant because cardiovascular reactivity also has links to immune-mediated inflammatory processes which in turn influence cardiovascular risk (e.g., Bosch, de Geus, Veerman, Hoogstraten, & Amerongen, 2003). Given what is already known about the basic influence of received support on reactivity (Thoreinstein et al., 1999), these paradigms can be expanded to model more integrative physiological pathways linking social support to cardiovascular disease.
Conclusions
The plausibility of links between social support and reactivity in the laboratory are based on several assumptions. One important assumption is that the operationalization of support in the laboratory, matches that of epidemiological studies that have found support to predict reduced cardiovascular morbidity and mortality. As argued in this review, most laboratory reactivity studies are operationalized based on the receipt of support. However, the prior epidemiological literature has shown a beneficial influence of perceived support, whereas the links between received support and health are more variable (Uchino, 2004). Future studies that examine laboratory reactivity protocols will need to model theoretically important contextual factors that appear to influence its effectiveness, along with associated mechanisms. In addition, an examination of naturalistic perceptions of support and its potential interaction with received support on reactivity will be important. One of the issues holding back progress on social support as a risk factor for disease is the complexity of the construct. Research that models this complexity can result in more specific models that might then guide interventions that utilize relationships to promote positive health outcomes.
Acknowledgments
Support for this paper was generously provided by grant numbers R01 HL085106 from the National Heart, Lung, and Blood Institute, and R21 AG029239 from the National Institute on Aging.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Bert N. Uchino, Department of Psychology and Health Psychology Program, University of Utah
McKenzie Carlisle, Department of Psychology and Health Psychology Program, University of Utah.
Wendy Birmingham, Department of Psychology and Health Psychology Program, University of Utah.
Allison A. Vaughn, Department of Psychology, San Diego State University
References
- Barbee AP, Gulley MR, Cunningham MR. Support seeking in personal relationships. Journal of Social and Personal Relationships. 1990;7:531–540. [Google Scholar]
- Barrera M., Jr . Social support research in community psychology. In: Rappaport J, Seidman E, editors. Handbook of Community Psychology. N. Y.: Kluwer Academic/Plenum Publishers; 2000. pp. 215–245. [Google Scholar]
- Berg CA, Upchurch R. A developmental-contextual model of couples coping with chronic illness across the lifespan. Psychological Bulletin. 2007;133(6):920–954. doi: 10.1037/0033-2909.133.6.920. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Social Science and Medicine. 2000;51:843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Bolger N, Amarel D. Effects of social support visibility on adjustment to stress: Experimental evidence. Journal of Personality and Social Psychology. 2007;92(3):458–475. doi: 10.1037/0022-3514.92.3.458. [DOI] [PubMed] [Google Scholar]
- Bolger N, Foster M, Vinokur AD, Ng R. Close relationships and adjustment to a life crisis: The case of breast cancer. Journal of Personality and Social Psychology. 1996;70:283–294. doi: 10.1037//0022-3514.70.2.283. [DOI] [PubMed] [Google Scholar]
- Bolger N, Zuckerman A, Kessler RC. Invisible support and adjustment to stress. Journal of Personality and Social Psychology. 2000;79:953–961. doi: 10.1037//0022-3514.79.6.953. [DOI] [PubMed] [Google Scholar]
- Bosch JA, de Geus EJC, Veerman ECI, Hoogstraten J, Nieuw Amerongen V. Innate secretory immunity in response to laboratory stressors that evoke distinct patterns of cardiac autonomic activity. Psychosomatic Medicine. 2003;65:245–258. doi: 10.1097/01.psy.0000058376.50240.2d. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology. 1989;56:267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- Cohen S. Psychosocial models of the role of social support in the etiology of physical disease. Health Psychology. 1988;7:269–297. doi: 10.1037//0278-6133.7.3.269. [DOI] [PubMed] [Google Scholar]
- Cornish P, Blanchard E, Jaccard J. The relationship between 24-hour ambulatory blood pressures and laboratory measures of cardiovascular reactivity. Biofeedback and Self-Regulation. 1994;19:193–209. doi: 10.1007/BF01721067. [DOI] [PubMed] [Google Scholar]
- Craig FW, Lynch JJ, Quartner JL. The perception of available social support is related to reduced cardiovascular reactivity in phase II cardiac rehabilitation patients. Integrative Physiological and Behavioral Science. 2000;35:272–283. doi: 10.1007/BF02688790. [DOI] [PubMed] [Google Scholar]
- Craig FW, Deichert NT. Can male-provided social support buffer the cardiovascular responsivity to stress in men? It depends on the nature of the support provided. International Journal of Men's Health. 2002;1:105–118. [Google Scholar]
- Christenfeld N, Gerin W, Linden W, Sanders M, Mathur J, Deich JD, Pickering TG. Social support effects on cardiovascular reactivity: Is a stranger as effective as a friend? Psychosomatic Medicine. 1997;59:388–398. doi: 10.1097/00006842-199707000-00009. [DOI] [PubMed] [Google Scholar]
- Crocker J, Canevello A. Creating and undermining social support in communal relationships: The role of compassionate and self-image goals. Journal of Personality and Social Psychology. 2008;95:555–575. doi: 10.1037/0022-3514.95.3.555. [DOI] [PubMed] [Google Scholar]
- Cutrona CE, Russell DW. Type of social support and specific stress: Towards a theory of optimal matching. In: Sarason BR, Sarason IG, Pierce GR, editors. Social support: An interactional view. N. Y.: John Wiley and Sons; 1990. pp. 319–366. [Google Scholar]
- Dienstbier RA. Arousal and physiological toughness: Implications for mental and physical health. Psychological Review. 1989;96:84–100. doi: 10.1037/0033-295x.96.1.84. [DOI] [PubMed] [Google Scholar]
- Dunkel-Schetter C, Bennett TL. Differentiating the cognitive and behavioral aspects of social support. In: Sarason BR, Sarason IG, Pierce GR, editors. Social support: An interactional view. N. Y.: John Wiley and Sons; 1990. pp. 267–296. [Google Scholar]
- Dunkel-Schetter C, Skokan LA. Determinants of social support provision in personal relationships. Journal of Social and Personal Relationships. 1990;7:437–450. [Google Scholar]
- Flaherty J, Richman J. Gender differences in the perception and utilization of social support: Theoretical perspectives and an empirical test. Social Science and Medicine. 1989;28:1221–1228. doi: 10.1016/0277-9536(89)90340-7. [DOI] [PubMed] [Google Scholar]
- Forster LE, Stoller EP. The impact of social support on mortality: A seven-year follow-up of older men and women. The Journal of Applied Gerontology. 1992;11:173–186. [Google Scholar]
- Gerin W, Pieper C, Levy R, Pickering TG. Social support in social interaction: A moderator of cardiovascular reactivity. Psychosomatic Medicine. 1992;54:324–336. doi: 10.1097/00006842-199205000-00008. [DOI] [PubMed] [Google Scholar]
- Glynn LM, Christenfeld N, Gerin W. Gender, social support, and cardiovascular response to stress. Psychosomatic Medicine. 1999;61:234–242. doi: 10.1097/00006842-199903000-00016. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad JL, Uchino BN, Smith TW, Hicks A. On the Importance of Relationship Quality: The Impact of Ambivalence in Friendships on Cardiovascular Functioning. Annals of Behavioral Medicine. 2007;33:278–290. doi: 10.1007/BF02879910. [DOI] [PubMed] [Google Scholar]
- Horowitz LM, Krasnoperova EN, Tater DG, Hansen MB, Person EA, Galvin KL, Nelson KL. The way to console may depend on the goal: Experimental studies of social support. Journal of Experimental Social Psychology. 2000;37:49–61. [Google Scholar]
- House JS. Social isolation kills, but how and why? Psychosomatic Medicine. 2001;63:273–274. doi: 10.1097/00006842-200103000-00011. [DOI] [PubMed] [Google Scholar]
- Hughes BM. Social support in ordinary life and laboratory measures of cardiovascular reactivity: Gender differences in habituation-sensitization. Annals of Behavioral Medicine. 2007;34:166–176. doi: 10.1007/BF02872671. [DOI] [PubMed] [Google Scholar]
- Hughes BM, Curtis R. Quality and quantity of social support as differential predictors of cardiovascular reactivity. The Irish Journal of Psychology. 2000;21:16–31. [Google Scholar]
- Kamarck TW, Manuck SB, Jennings JR. Social support reduces cardiovascular reactivity to psychological challenge: A laboratory model. Psychosomatic Medicine. 1990;52:42–58. doi: 10.1097/00006842-199001000-00004. [DOI] [PubMed] [Google Scholar]
- Kamarck TW, Schwartz JE, Janicki DL, Shiffman S, Raynor DA. Correspondence between laboratory and ambulatory measures of cardiovascular reactivity: A multilevel modeling approach. Psychophysiology. 2003;40:675–683. doi: 10.1111/1469-8986.00069. [DOI] [PubMed] [Google Scholar]
- Krantz DS, Manuck SB. Acute physiologic reactivity and risk of cardiovascular disease: A review and methodologic critique. Psychological Bulletin. 1984;96:435–464. [PubMed] [Google Scholar]
- Lakey b, McCabe KM, Fisicaro SA, Drew JB. Environmental and personal determinants of support perceptions: Three generalizability studies. Journal of Personality and Social Psychology. 1996;70:1270–1280. doi: 10.1037//0022-3514.70.6.1270. [DOI] [PubMed] [Google Scholar]
- Lakey B, Scoboria A. The relative contribution of trait and social influences to the links among perceived social support, affect, and self-esteem. Journal of Personality. 2005;73(2):361–388. doi: 10.1111/j.1467-6494.2005.00312.x. [DOI] [PubMed] [Google Scholar]
- Lassner JB, Matthews KA, Stoney CM. Are cardiovascular reactors to asocial stress also reactors to social stress? Journal of Personality and Social Psychology. 1994;66:69–77. doi: 10.1037//0022-3514.66.1.69. [DOI] [PubMed] [Google Scholar]
- Lehman DR, Ellard JH, Wortman CB. Social support for the bereaved: Recipients' and providers' perspectives on what is helpful. Journal of Consulting and Clinical Psychology. 1986;54:438–446. [Google Scholar]
- Lepore SJ, Allen KA, Evan GW. Social support lowers cardiovascular reactivity to an acute stressor. Psychosomatic Medicine. 1993;55:518–524. doi: 10.1097/00006842-199311000-00007. [DOI] [PubMed] [Google Scholar]
- Light KC, Turner JR, Hinderliter AL, Sherwood A. Race and gender comparisons: II. Predictions of work blood pressure from laboratory baseline and cardiovascular reactivity measures. Health Psychology. 1993;12:366–375. doi: 10.1037//0278-6133.12.5.366. [DOI] [PubMed] [Google Scholar]
- Maisel NC, Gable SL. The paradox of received support: The importance of responsiveness. Psychological Science. 2009;20:928–932. doi: 10.1111/j.1467-9280.2009.02388.x. [DOI] [PubMed] [Google Scholar]
- Nadler A, Fisher JD. The role of threat to self-esteem and perceived control in recipient reaction to help: Theory development and empirical validation. In: Berkowitz L, editor. Advances in Experimental Social Psychology. N. Y.: Academic Press; 1986. pp. 81–122. [Google Scholar]
- Nausheen B, Gidron Y, Gregg A, Tissarchondou HS, Peveler R. Loneliness, social support, and cardiovascular reactivity to laboratory stress. Stress. 2007;10:37–44. doi: 10.1080/10253890601135434. [DOI] [PubMed] [Google Scholar]
- O'Donovan A, Hughes B. Access to social support in life and in the laboratory: Combined impact on cardiovascular reactivity to stress and state anxiety. Journal of Health Psychology. 2008;13:1019–1028. doi: 10.1177/1359105308095968. [DOI] [PubMed] [Google Scholar]
- Orth-Gomér K, Rosengren A, Wilhelmsen L. Lack of social support and incidence of coronary heart disease in middle-aged Swedish men. Psychosomatic Medicine. 1993;55:37–43. doi: 10.1097/00006842-199301000-00007. [DOI] [PubMed] [Google Scholar]
- Phillips AC, Gallagher S, Carroll D. Social support, social intimacy, and cardiovascular reactions to acute psychological stress. Annals of Behavioral Medicine. 2009;37:38–45. doi: 10.1007/s12160-008-9077-0. [DOI] [PubMed] [Google Scholar]
- Pickering TG, Gerin W. Cardiovascular reactivity in the laboratory and the role of behavioral factors in hypertension: A critical review. Annals of Behavioral Medicine. 1990;12:3–16. [Google Scholar]
- Reis HT. Steps toward the ripening of relationship science. Personal Relationships. 2007;14:1–23. [Google Scholar]
- Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99:2192–2217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- Roy MP, Steptoe A, Kirschbaum C. Life events and social support as moderators of individual differences in cardiovascular and cortisol reactivity. Journal of Personality and Social Psychology. 1998;75:1273–1281. doi: 10.1037//0022-3514.75.5.1273. [DOI] [PubMed] [Google Scholar]
- Sabin EP. Social relationships and mortality among the elderly. The Journal of Applied Gerontology. 1993;12:44–60. [Google Scholar]
- Sarason IG, Sarason BR, Shearin EN. Social support as an individual difference variable: Its stability, origins, and relational aspects. Journal of Personality and Social Psychology. 1986;50:845–855. [Google Scholar]
- Shaw BA, Krause N, Chatters LM, Connell CM, Ingersoll-Dayton B. Emotional support from parents early in life, aging, and health. Psychology and Aging. 2004;19:4–12. doi: 10.1037/0882-7974.19.1.4. [DOI] [PubMed] [Google Scholar]
- Snydersmith MA, Cacioppo JT. Parsing complex social factors to determine component effects: I. Autonomic activity and reactivity as a function of human association. Journal of Social and Clinical Psychology. 1992;11:263–278. [Google Scholar]
- Thoits PA. Social support as coping assistance. Journal of Consulting and Clinical Psychology. 1986;54(4):416–423. doi: 10.1037//0022-006x.54.4.416. [DOI] [PubMed] [Google Scholar]
- Thorsteinsson EB, James JE. A meta-analysis of the effects of experimental manipulations of social support during laboratory stress. Psychology and Health. 1999;14:869–886. [Google Scholar]
- Tracey KJ. The inflammatory reflex. Nature. 2002;420:853–859. doi: 10.1038/nature01321. [DOI] [PubMed] [Google Scholar]
- Treiber FA, Kamarck T, Schneiderman N, Sheffield D, Kapuku G, Taylor T. Cardiovascular reactivity and development of preclinical and clinical disease states. Psychosomatic Medicine. 2003;65:46–62. doi: 10.1097/00006842-200301000-00007. [DOI] [PubMed] [Google Scholar]
- Trobst KK. An interpersonal conceptualization and quantification of social support transactions. Personality and Social Psychology Bulletin. 2000;26:971–986. [Google Scholar]
- Uchino BN. Social support and physical health: Understanding the health consequences of our relationships. New Haven, CT: Yale University Press; 2004. [Google Scholar]
- Uchino BN. Understanding the links between social support and physical health: A lifespan perspective with emphasis on the separability of perceived and received support. Perspectives in Psychological Science. 2009;4:236–255. doi: 10.1111/j.1745-6924.2009.01122.x. [DOI] [PubMed] [Google Scholar]
- Uno D, Uchino BN, Smith TW. Relationship Quality Moderates the Effect of Social Support Given by Close Friends on Cardiovascular Reactivity in Women. International Journal of Behavioral Medicine. 2002;9:243–262. doi: 10.1207/s15327558ijbm0903_06. [DOI] [PubMed] [Google Scholar]
- Wills TA, Shinar O. Measuring perceived and received social support. In: Cohen S, Gordon L, Gottlieb B, editors. Social support measurement and intervention: A guide for health and social scientists. New York: Oxford University Press; 2000. pp. 86–135. [Google Scholar]
- Wilson DK, Kliewer W, Bayer L, Jones D, Welleford A, Heiney M, Sica DA. The influence of gender and emotional versus instrumental support on cardiovascular reactivity in African-American adolescents. Annals of Behavioral Medicine. 1999;21:235–243. doi: 10.1007/BF02884840. [DOI] [PubMed] [Google Scholar]