Abstract
Computed tomography colonography (CTC) in colorectal cancer (CRC) screening has two roles: one present and the other potential. The present role is, without any further discussion, the integration into established screening programs as a replacement for barium enema in the case of incomplete colonoscopy. The potential role is the use of CTC as a first-line screening method together with Fecal Occult Blood Test, sigmoidoscopy and colonoscopy. However, despite the fact that CTC has been officially endorsed for CRC screening of average-risk individuals by different scientific societies including the American Cancer Society, the American College of Radiology, and the US Multisociety Task Force on Colorectal Cancer, other entities, such as the US Preventive Services Task Force, have considered the evidence insufficient to justify its use as a mass screening method. Medicare has also recently denied reimbursement for CTC as a screening test. Nevertheless, multiple advantages exist for using CTC as a CRC screening test: high accuracy, full evaluation of the colon in virtually all patients, non-invasiveness, safety, patient comfort, detection of extracolonic findings and cost-effectiveness. The main potential drawback of a CTC screening is the exposure to ionizing radiation. However, this is not a major issue, since low-dose protocols are now routinely implemented, delivering a dose comparable or slightly superior to the annual radiation exposure of any individual. Indirect evidence exists that such a radiation exposure does not induce additional cancers.
Keywords: Computed tomography colonography, Colon neoplasms, Colon polyps, Colorectal cancer screening, Computed tomography colonography safety, Computed tomography colonography accuracy, Computed tomography colonography radiation exposure, Computed tomography colonography cost-effectiveness
INTRODUCTION
It is now 16 years since Vining et al[1] presented the first virtual images of the colon at the 1994 meeting of the Society of Gastrointestinal Radiologists. This marked the birth of “virtual colonoscopy” (VC), an intriguing name useful for marketing to patients, providers and the public, or “CT colonography” (CTC), the name most radiologists prefer.
When discussing the role of CTC in colorectal cancer (CRC) screening, it is necessary to separate the present and existent role from the potential one.
The present role is, without any further discussion, the integration into established screening programs as a replacement for barium enema (BE) in the case of incomplete colonoscopy (CC). In fact, since 2006 the American Gastroenterological Association (AGA) Clinical Practice and Economics Committee has endorsed CTC as the method of choice for colon investigation in cases of incomplete colonoscopy[2] and numerous evidence exists in the literature showing a clear superiority of CTC over BE in the detection of CRC and polyps[3-5]. It is also clear that performing CTC in patients with a positive Fecal Occult Blood Test (FOBT) would not be an efficient triage technique in terms of cost-effectiveness, due to the high prevalence of clinically relevant colonic lesions[6,7].
The potential role of CTC is to act as a first-line CRC screening modality. In this regard, it was in March 2008 that CTC obtained its major success: the American Cancer Society (ACS), the US Multi-Society Task Force on Colorectal Cancer and the American College of Radiology (ACR) released consensus guidelines on CRC screening for average-risk individuals. These guidelines distinguished diagnostic tests into two groups: those able to detect CRC, thus potentially reducing mortality (FOBT; Fecal Immunochemical stool Testing, FIT; and stool DNA testing), and those able to detect both polyps and cancer, thus potentially reducing both the incidence of and the mortality from CRC. This latter group of tests includes CC, sigmoidoscopy, BE and - for the first time - also CTC, with the recommendation that it be performed every 5 years starting at 50 years of age[8]. Unfortunately, this position did not remain unequivocal: in fact, the US Preventive Services Task Force (USPSTF) considered the evidence insufficient because of the unknown impact of both extra-colonic findings and radiation exposure, the poor data on cost and cost-effectiveness, and the still unsolved problem of ideal bowel preparation[9]. Other associations, such as the Asia Pacific Working Group on Colorectal Cancer[10] and the American College of Gastroenterology[11], consider CTC a second-line screening test for those unwilling or unable to undergo CC and for those in whom CC was incomplete. Furthermore, in 2008 in the USA, the Centers for Medicare and Medicaid Services denied the reimbursement of screening exams done with CTC[12].
These facts mean on one hand that CTC is considered useful by clinicians, but, on the other hand, that radiologists have much to do until this imaging method is implemented for screening, as testified by a survey conducted among US primary care physicians (PCP)[13]. When asked which diagnostic tests they perceive as being very effective in reducing CRC mortality, 22% answered CTC vs 95% CC; and when asked which test they would recommend for CRC screening, most respondents indicated CC (95%) and FOBT (80%), but only about 5% answered CTC.
Keeping in mind these facts, the potential role of CTC in CRC screening will be discussed in the next paragraphs, taking into consideration that an ideal screening test is not yet available and that any screening test is a compromise among four major variables: efficacy, compliance, safety and cost.
EFFICACY
The issue of diagnostic accuracy of CTC for CRC and polyps has been debated for a long time, because of the conflicting results in some of the papers published in the literature[14-16]. This has been recently confirmed by a meta-analysis showing that “CTC is highly specific for the detection of colorectal polyps and tumors” and that “some studies reported high sensitivities, but the results of the studies were highly heterogeneous, while the studied variables explained only part of this discrepancy”[17].
These results led researchers to design three important studies: two large, multicenter trials testing the performance of CTC in comparison with CC in respectively asymptomatic subjects at average risk, i.e. a typical screening population [the American College of Radiology Imaging Network (ACRIN) trial performed in the USA][18] and in a mixed population of asymptomatic subjects at risk higher-than-average and in patients referred for a positive FOBT [Italian Multicenter Polyps Accuracy CTC study (IMPACT) trial][19]; and one multicenter trial [Special Interest Group in Gastrointestinal and Abdominal Radiology (SIGGAR) trial run in the UK] conducted on symptomatic patients with the aim to detect CRC[20]. In particular, the ACRIN trial tried to minimize the variables possibly affecting CTC performance. For this reason only ≥ 16-row MDCT scanners were used, patients were administered oral contrast agent for stool tagging together with cathartic agent and training of the radiologists observing the images was an important component of the study. In particular, CTC readers were obligated to have read at least 500 cases, or to have attended a 1.5-d training course, and all had to pass a certified exam in which they detected at least 90% of adenomas 1 cm or larger in 50 cases. More than half of the readers had to undergo additional training in order to pass the certified exam initially and, with additional training, all the readers eventually passed.
Results from ACRIN and IMPACT have been recently published[18,19], whereas those from SIGGAR[20] are still under data analysis. Both the ACRIN and IMPACT trials reported per-patient sensitivity of 90% for polyps > 10 mm and 78%-84% for polyps larger than 6 mm; per-patient specificity was extremely high as well, over 85% independently of lesion size (Table 1). The major drawback of ACRIN was represented by the poor positive predictive value (PPV) (23% for polyps ≤ 10 mm), which might negatively affect a screening program, leading to useless CC, with patient discomfort, embarrassment of radiologists, potential risk of complications and increased costs. Unfortunately there is no explanation for these data, unless one would claim a psychological attitude to overcall in order to reach the threshold of 90% for clinically significant polyps despite a loss in specificity. A definitely better PPV was documented in the IMPACT trial (62% for lesions larger than 6 mm) as well as in studies obtained in high-experience centers, the University of Wisconsin (PPV, 91.5%) and a group of Korean hospitals (PPV, 69% for lesions > 6 mm and 92% for those > 10 mm)[21,22].
Table 1.
Results from major trials on a per-patient basis: sensitivity, specificity, positive and negative predictive values
| Multicenter trials | All polyp size | Polyps (≥ 5 mm) | Polyps (≥ 6 mm) | Polyps (≥ 7 mm) | Polyps (≥ 8 mm) | Polyps (≥ 9 mm) | Polyps (≥ 10 mm) |
| Per patient sensitivity | |||||||
| ACRIN | N/A | 65% | 78% | 84% | 87% | 90% | 90% |
| IMPACT | N/A | N/A | 85% | 86% | 88% | 91% | 91% |
| Munich | 84% | 91% | N/A | N/A | N/A | N/A | 92% |
| Per patient specificity | |||||||
| ACRIN | N/A | 89% | 88% | 87% | 87% | 86% | 86% |
| IMPACT | N/A | N/A | 88% | 87% | 86% | 85% | 85% |
| Munich | 47% | 93% | N/A | N/A | N/A | N/A | 98% |
| Per patient PPV | |||||||
| ACRIN | N/A | 45% | 40% | 35% | 31% | 25% | 23% |
| IMPACT | N/A | N/A | 62% | N/A | N/A | N/A | N/A |
| Munich | 48% | N/A | 70% | N/A | N/A | N/A | 79% |
| Per patient NPV | |||||||
| ACRIN | N/A | 95% | 98% | 99% | 99% | 99% | 99% |
| IMPACT | N/A | N/A | 96% | N/A | N/A | N/A | N/A |
| Munich | 84% | N/A | 98% | N/A | N/A | N/A | 99% |
Results are categorized according to polyp size. PPV: Positive predictive value; NPV: Negative predictive value; N/A: Not assessable.
However, the negative predictive values in both the ACRIN and the IMPACT trials was rather high, approaching 100%; this is extremely important in order to reassure negative patients about the significance of the examination.
Excellent results were also obtained in the Munich Colorectal Cancer Prevention Trial[23], a single-center study where around 300 asymptomatic subjects underwent low-dose CTC in comparison with other screening tests (CC, sigmoidoscopy and FOBT).
It is noteworthy to mention that in a screening project offered by the University of Wisconsin[24], after 2 years of recruitment over 3000 subjects of two different, non-randomized groups underwent CTC and CC. The detection rate for advanced adenomas was 3.2% for CTC and 3.4% for CC (difference not statistically significant), with the advantage of a large reduction in the number of polypectomies in the CTC group without any complication as opposed to seven perforations which occurred in the CC group.
Despite the good results there are still some open issues under debate within the radiological as well as the gastroenterological communities. These are the significance of diminutive (< 6 mm) polyps, the management of intermediate (6-9 mm) lesions, the detection rate for non-polypoid, flat lesions and the impact of the extra-colonic findings.
According to a very recent systematic review[25] of published studies reporting the distribution of advanced adenomas in asymptomatic screening cohorts, diminutive polyps have a minimal clinical impact. In fact, the frequency of advanced lesions among patients whose largest polyp was ≤ 5 mm, 6-9 mm, < 10 mm, and > 10 mm in size was 0.9%, 4.9%, 1.7%, and 73.5%, respectively (Figure 1). As a consequence, a 6-mm polyp size threshold for polypectomy referral would identify over 95% of subjects with advanced adenomas, whereas a 10-mm threshold would identify 88% of cases. From a cost-effectiveness point of view, detection and removal of all polyps including those smaller than 5 mm, would be very inefficient, with a cost per year of life gained > $460 000[26], absolutely unacceptable in terms of cost-effectiveness. It is also true that this approach, not removing diminutive polyps, necessitates an extensive education of patients and PCP. In fact, according to a recently published survey[27], the majority of patients, PCP and gastroenterologists would not choose to follow up small polyps identified by CTC with CC because of the fear of missing precancerous lesions.
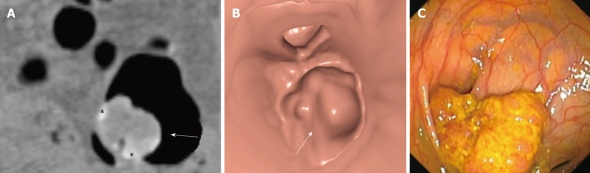
Figure 1.
Sessile polyp: adenoma with low-grade dysplasia. A: Coronal reformatted image showing a polypoid lesion (arrow), partly surrounded by tagged fluid (asterisks); B: The same lesion as shown on 3D endoluminal view (arrow); C: Conventional colonoscopy.
The management of intermediate (6 to 9 mm) lesions is also under debate, despite the fact that today any polyp 6 mm or larger should be preferably referred for CC and polypectomy, also according to ACS CRC screening guidelines[2]. However, evidence does exist from cost-effectiveness[28] as well as follow-up[29] studies indicating that, for the future, polyp follow-up might be an alternative to referral for CC and polypectomy. These data have been recently reinforced by studies conducted with CC and subsequent polypectomy, where the rate of advanced adenoma in 6-9 mm polyps was demonstrated to be 6.6%[30].
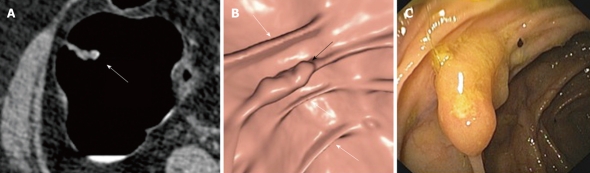
A potential disadvantage of CTC would be the possible impaired ability to detect non-polypoid, flat lesions (Figure 2). This issue deserves some consideration. First of all, flat lesions represent a subset of sessile polyps, and according to a recent publication[31] the overall prevalence in a screening population is around 5.8% (if flat lesions are defined as those with a height not exceeding 0.5 of the diameter[32]). However, within this definition, slightly elevated lesions are also included, which, in some cases, may be classified as sessile. For this reason, an elevation not higher than 3 mm is often used, especially for small lesions not larger than 2-3 cm. The other important remarks are that “completely flat lesions are exceedingly rare” and that depressed lesions are less than 1% of all colorectal lesions and only a quarter of those are observed in a screening population. This means that the majority of non-polypoid lesions are at least slightly elevated and this works in favor of the possible detection with CTC. Unfortunately, at the moment only few and conflicting data about the sensitivity of CTC for flat lesions are available. At the beginning disappointing results were published[33,34], because of technical limitations as well as readers’ experience. More recently, better results were reported, with sensitivity in the range of 80%-90% for flat adenocarcinomas[32,35]. These results seem to be confirmed by a recent retrospective analysis of the data from the ACRIN trial showing a sensitivity of 89% for flat adenomas ≤ 6 mm (at the prospective analysis, sensitivity was 68%) (Fidler J, presented at ACRIN meeting, October 1, 2009).
Figure 2.
Non-polypoid (flat) lesion: advanced adenoma. A: On 2D axial computed tomography image an irregularly thickened fold (arrow) is detected; B: On 3D endoluminal image the lesion is better appreciated (black arrow), in particular if compared with the normal adjacent colonic folds (white arrows); C: The same lesion at colonoscopy before removal.
The impact of extra-colonic findings will be discussed in the paragraph concerning costs.
COMPLIANCE (ADHESION TO A SCREENING PROGRAM)
Compliance means adhesion of healthy individuals to a screening program. This is a very complex issue, long debated in the literature and presently without a solution, since virtually in any Western country a high proportion of adults 50 years of age or older have not undergone any CRC screening test[36]. Colonoscopy, considered to be the most effective screening method, suffers from a very low participation rate. Very recent data from Italy[37] underline the difficulties and barriers in implementing a CC population screening, at least through primary care. Reported participation in a CC screening arm was extremely low in Southern Italy (2.8%), and higher, but still disappointing, in North-Central Italy (12.4%).
To increase screening uptake is extremely important, since the adhesion rate of the invited population directly affect the efficiency of the program. For example, if we consider that the efficacy of CC in reducing the incidence of CRC is around 76%[38], the efficiency with regard to CRC prevention rate, considering an adhesion rate of 20%, drops to 15% (76% × 20% = 15%).
The question is whether CTC would be able to increase screening uptake. The three most common deterrents that patients expressed about receiving CC were bowel preparation, embarrassment and fear of discomfort[39,40]. The advantage of CTC is the use of a gentler preparation or unprepped (laxative-free) examination[41]. Furthermore, the pain related to colon distension by air may be minimized by the use of carbon dioxide delivered by an electronic pump. The use of carbon dioxide is also associated with a faster absorption, making the patient more comfortable immediately after the examination[42].
Unfortunately, only few data are available regarding adhesion rate and CTC. In a study conducted in Western Australia[43], 2000 people were invited and 28.4% accepted to undergo CTC for screening, with 62% of them preferring CTC over optical colonoscopy. The fact remains that we need data resulting from real screening experiences.
SAFETY
CTC is a safe test, definitely safer than colonoscopy. The results of different surveys show a perforation rate associated with CTC ranging between 0.06% and 0.08%[44,45], even lower in screening[46], compared with 0.1%-0.2% for diagnostic colonoscopy[47]. It should also be noted that the comparison between CTC and CC is very difficult, with the risk of overestimating the clinically significant perforations at CTC, because of the much higher sensitivity of CT in the detection of even tiny air bubbles. In fact, most of the perforations reported in a UK survey[44] were treated conservatively, without surgical intervention. CTC complications in most of the cases are due to technical factors, such as the use of a rigid catheter for bowel distension (now replaced by thin rubber devices), manual distension with air (now minimized by the use of an electronic pump delivering carbon dioxide and able to control pressure and volume), inexpert personnel and incorrect patient selection.
Other complications occasionally reported have been vasovagal reactions due to colonic overdistention[48].
The main potential drawback of screening with CTC is the exposure to ionizing radiation[49] and the consequent theoretical risk of inducing cancer. The risk is theoretical because there are still many uncertainties with regard to the true effects of ionizing radiation at low doses, such as those used in diagnostic radiology[50,51]. According to the Health Physics Society[52], “below 5-10 rem (50-100 mSv) (which includes occupational and environmental exposures), risks of health effects are either too small to be observed or are nonexistent”; and the French Academy report[53] stated that the linear no-threshold (LNT) hypothesis for assessing the risk associated with low doses is not based on scientific evidence. However, in contrast, the International Commission on Radiological Protection (ICRP)[54] and the Biological Effects of Ionizing Radiation (BEIR) VII report[55] considered LNT as the best method to assess low dose exposures, in order to be more conservative and more protective towards patients because of the multiple uncertainties. Unfortunately even if this hypothesis may be true it cannot be proved since we have little direct evidence of harm below 100 mSv.
Even if the LNT hypothesis is considered the most accurate, the problem of radiation exposure of patients undergoing CTC seems to be minimal. In fact, the mean exposure in the case of a screening examination has been calculated in a recent survey[56] to be around 5-6 mSv, which is twice the normal background radiation exposure in the US (2.5-3.0 mSv per year)[57]. In addition we have to consider, in a screening scenario, that CTC should be repeated every 5 years, not earlier. For a radiation dose of around 5-8 mSv at age 50 years, the lifetime risk of death from cancer varies between 0.02% and 0.03%[58]. If we think about cost/benefit of the examination, this minor risk should be compared with the theoretical risk of CRC in average risk individuals, which is around 5%[59].
A more precise idea about the amount of radiation exposure comes from a comparison with other categories of workers continuously exposed to low dose radiation, such as, for example, airline crews and nuclear workers. As an example, the value of 5-6 mSv, to be received in a screening scenario every 5 years, should be compared with radiation exposure of airline crews, who are submitted to an average of 5 mSv per year every single year of their activity, with a long life exposure close to 80 mSv. A recent survey of airline pilots from eight different European countries has shown no increase in mortality from radiation-induced cancers over a 30-year period of time[60]. Similar data were observed in nuclear workers in two recently published experiences[61,62].
COSTS
Cost analysis is a very difficult task, especially in the absence of real data and based only on mathematical models. Among the studies published in the literature[63-69] 5 out of 7 are in favor of CC and only two were able to demonstrate a better cost-effectiveness of CTC. A recent review of the literature[70] has pointed out the profound differences among the models as well as the weakness of such an approach, where a minimal variation of a single input may completely alter the final results. As an example, if the cost ratio between CTC and CC is ≤ 0.7, the model is usually in favor of CTC, but if the cost of CTC is higher than 80% of the cost of CC, it will be CC which is the most cost effective method. Another very important issue, adhesion rate, is never taken into account in the models, where it is considered to be equal among the different screening tests, although this is probably not the case. In addition, differences in healthcare systems, reimbursement, cost of the equipment and personnel are other important variables affecting the final outcome.
When considering cost, the issue of extra-colonic findings should be taken into account. The detection of extra-colonic findings can be considered a potential advantage of CTC, since previously unknown life-threatening diseases, which are not insignificant[71], can be diagnosed and treated, with a clear impact on patients’ life expectancy. However, the major problem is the extra time necessary for reporting these findings and the cost induced by unnecessary investigation of common benign abnormalities, especially because of their high prevalence[72,73]. In a recent publication[74], the mean cost per patient was $31.02 for nonsurgical and $67.54 for surgical work-up procedures. Although extra-colonic findings have been traditionally regarded as an additional cost, they have been recently considered as a potential benefit (i.e. detection of unsuspected abdominal aortic aneurysm or renal cancer), able to improve CTC cost-effectiveness[75].
CONCLUSION
In conclusion, CTC has a present role in CRC screening programs, i.e. the replacement of BE in the case of incomplete colonoscopy. The potential role is the proposal of CTC as a first-line CRC screening modality. In this setting, CTC has clear advantages, such as accuracy, safety and subject acceptance. Further research should be warranted to clarify, in particular, two aspects: the uptake rate of the general population and the real cost and benefits derived from a CTC screening program.
Footnotes
Peer reviewer: Dr. John B Schofield, MB, BS, MRCP, FRCP, Department of Cellular Pathology, Preston Hall, Maidstone, Kent, ME20 7NH, United Kingdom
S- Editor Wang YR L- Editor Logan S E- Editor Ma WH
References
- 1.Vining DJ, Gelfand DW. Non-invasive colonoscopy using helical CT scanning. 3D reconstruction and virtual reality. Syllabus of the 23rd Annual Meeting Society of gastrointestinal Radiologists, Maui, Hawaii, 13-18 February. 1994. [Google Scholar]
- 2.Position of the American Gastroenterological Association (AGA) Institute on computed tomographic colonography. Gastroenterology. 2006;131:1627–1628. doi: 10.1053/j.gastro.2006.09.043. [DOI] [PubMed] [Google Scholar]
- 3.Johnson CD, MacCarty RL, Welch TJ, Wilson LA, Harmsen WS, Ilstrup DM, Ahlquist DA. Comparison of the relative sensitivity of CT colonography and double-contrast barium enema for screen detection of colorectal polyps. Clin Gastroenterol Hepatol. 2004;2:314–321. doi: 10.1016/s1542-3565(04)00061-8. [DOI] [PubMed] [Google Scholar]
- 4.Rockey DC, Paulson E, Niedzwiecki D, Davis W, Bosworth HB, Sanders L, Yee J, Henderson J, Hatten P, Burdick S, et al. Analysis of air contrast barium enema, computed tomographic colonography, and colonoscopy: prospective comparison. Lancet. 2005;365:305–311. doi: 10.1016/S0140-6736(05)17784-8. [DOI] [PubMed] [Google Scholar]
- 5.Sosna J, Sella T, Sy O, Lavin PT, Eliahou R, Fraifeld S, Libson E. Critical analysis of the performance of double-contrast barium enema for detecting colorectal polyps > or = 6 mm in the era of CT colonography. AJR Am J Roentgenol. 2008;190:374–385. doi: 10.2214/AJR.07.2099. [DOI] [PubMed] [Google Scholar]
- 6.Sali L, Falchini M, Bonanomi AG, Castiglione G, Ciatto S, Mantellini P, Mungai F, Menchi I, Villari N, Mascalchi M. CT colonography after incomplete colonoscopy in subjects with positive faecal occult blood test. World J Gastroenterol. 2008;14:4499–4504. doi: 10.3748/wjg.14.4499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liedenbaum MH, van Rijn AF, de Vries AH, Dekker HM, Thomeer M, van Marrewijk CJ, Hol L, Dijkgraaf MG, Fockens P, Bossuyt PM, et al. Using CT colonography as a triage technique after a positive faecal occult blood test in colorectal cancer screening. Gut. 2009;58:1242–1249. doi: 10.1136/gut.2009.176867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Levin B, Lieberman DA, McFarland B, Smith RA, Brooks D, Andrews KS, Dash C, Giardiello FM, Glick S, Levin TR, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. CA Cancer J Clin. 2008;58:130–160. doi: 10.3322/CA.2007.0018. [DOI] [PubMed] [Google Scholar]
- 9.Screening for colorectal cancer: U. S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2008;149:627–637. doi: 10.7326/0003-4819-149-9-200811040-00243. [DOI] [PubMed] [Google Scholar]
- 10.Sung JJ, Lau JY, Young GP, Sano Y, Chiu HM, Byeon JS, Yeoh KG, Goh KL, Sollano J, Rerknimitr R, et al. Asia Pacific consensus recommendations for colorectal cancer screening. Gut. 2008;57:1166–1176. doi: 10.1136/gut.2007.146316. [DOI] [PubMed] [Google Scholar]
- 11.Rex DK, Johnson DA, Anderson JC, Schoenfeld PS, Burke CA, Inadomi JM. American College of Gastroenterology guidelines for colorectal cancer screening 2009 [corrected] Am J Gastroenterol. 2009;104:739–750. doi: 10.1038/ajg.2009.104. [DOI] [PubMed] [Google Scholar]
- 12.Mitka M. Virtual colonoscopy dealt setback with rejection for coverage by Medicare. JAMA. 2009;301:1327–1328. doi: 10.1001/jama.2009.404. [DOI] [PubMed] [Google Scholar]
- 13.Klabunde CN, Lanier D, Nadel MR, McLeod C, Yuan G, Vernon SW. Colorectal cancer screening by primary care physicians: recommendations and practices, 2006-2007. Am J Prev Med. 2009;37:8–16. doi: 10.1016/j.amepre.2009.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pickhardt PJ, Choi JR, Hwang I, Butler JA, Puckett ML, Hildebrandt HA, Wong RK, Nugent PA, Mysliwiec PA, Schindler WR. Computed tomographic virtual colonoscopy to screen for colorectal neoplasia in asymptomatic adults. N Engl J Med. 2003;349:2191–2200. doi: 10.1056/NEJMoa031618. [DOI] [PubMed] [Google Scholar]
- 15.Cotton PB, Durkalski VL, Pineau BC, Palesch YY, Mauldin PD, Hoffman B, Vining DJ, Small WC, Affronti J, Rex D, et al. Computed tomographic colonography (virtual colonoscopy): a multicenter comparison with standard colonoscopy for detection of colorectal neoplasia. JAMA. 2004;291:1713–1719. doi: 10.1001/jama.291.14.1713. [DOI] [PubMed] [Google Scholar]
- 16.Rockey DC, Paulson E, Niedzwiecki D, Davis W, Bosworth HB, Sanders L, Yee J, Henderson J, Hatten P, Burdick S, et al. Analysis of air contrast barium enema, computed tomographic colonography, and colonoscopy: prospective comparison. Lancet. 2005;365:305–311. doi: 10.1016/S0140-6736(05)17784-8. [DOI] [PubMed] [Google Scholar]
- 17.Chaparro M, Gisbert JP, Del Campo L, Cantero J, Maté J. Accuracy of computed tomographic colonography for the detection of polyps and colorectal tumors: a systematic review and meta-analysis. Digestion. 2009;80:1–17. doi: 10.1159/000215387. [DOI] [PubMed] [Google Scholar]
- 18.Johnson CD, Chen MH, Toledano AY, Heiken JP, Dachman A, Kuo MD, Menias CO, Siewert B, Cheema JI, Obregon RG, et al. Accuracy of CT colonography for detection of large adenomas and cancers. N Engl J Med. 2008;359:1207–1217. doi: 10.1056/NEJMoa0800996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Regge D, Laudi C, Galatola G, Della Monica P, Bonelli L, Angelelli G, Asnaghi R, Barbaro B, Bartolozzi C, Bielen D, et al. Diagnostic accuracy of computed tomographic colonography for the detection of advanced neoplasia in individuals at increased risk of colorectal cancer. JAMA. 2009;301:2453–2461. doi: 10.1001/jama.2009.832. [DOI] [PubMed] [Google Scholar]
- 20.Halligan S, Lilford RJ, Wardle J, Morton D, Rogers P, Wooldrage K, Edwards R, Kanani R, Shah U, Atkin W. Design of a multicentre randomized trial to evaluate CT colonography versus colonoscopy or barium enema for diagnosis of colonic cancer in older symptomatic patients: the SIGGAR study. Trials. 2007;8:32. doi: 10.1186/1745-6215-8-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pickhardt PJ, Taylor AJ, Kim DH, Reichelderfer M, Gopal DV, Pfau PR. Screening for colorectal neoplasia with CT colonography: initial experience from the 1st year of coverage by third-party payers. Radiology. 2006;241:417–425. doi: 10.1148/radiol.2412052007. [DOI] [PubMed] [Google Scholar]
- 22.An S, Lee KH, Kim YH, Park SH, Kim HY, Kim SH, Kim N. Screening CT colonography in an asymptomatic average-risk Asian population: a 2-year experience in a single institution. AJR Am J Roentgenol. 2008;191:W100–W106. doi: 10.2214/AJR.07.3367. [DOI] [PubMed] [Google Scholar]
- 23.Graser A, Stieber P, Nagel D, Schäfer C, Horst D, Becker CR, Nikolaou K, Lottes A, Geisbüsch S, Kramer H, et al. Comparison of CT colonography, colonoscopy, sigmoidoscopy and faecal occult blood tests for the detection of advanced adenoma in an average risk population. Gut. 2009;58:241–248. doi: 10.1136/gut.2008.156448. [DOI] [PubMed] [Google Scholar]
- 24.Kim DH, Pickhardt PJ, Taylor AJ, Leung WK, Winter TC, Hinshaw JL, Gopal DV, Reichelderfer M, Hsu RH, Pfau PR. CT colonography versus colonoscopy for the detection of advanced neoplasia. N Engl J Med. 2007;357:1403–1412. doi: 10.1056/NEJMoa070543. [DOI] [PubMed] [Google Scholar]
- 25.Hassan C, Pickhardt PJ, Kim DH, Di Giulio E, Zullo A, Laghi A, Repici A, Iafrate F, Osborn J, Annibale B. Systematic review: distribution of advanced neoplasia according to polyp size at screening colonoscopy. Aliment Pharmacol Ther. 2010;31:210–217. doi: 10.1111/j.1365-2036.2009.04160.x. [DOI] [PubMed] [Google Scholar]
- 26.Pickhardt PJ, Hassan C, Laghi A, Zullo A, Kim DH, Iafrate F, Morini S. Small and diminutive polyps detected at screening CT colonography: a decision analysis for referral to colonoscopy. AJR Am J Roentgenol. 2008;190:136–144. doi: 10.2214/AJR.07.2646. [DOI] [PubMed] [Google Scholar]
- 27.Shah JP, Hynan LS, Rockey DC. Management of small polyps detected by screening CT colonography: patient and physician preferences. Am J Med. 2009;122:687.e1–687.e9. doi: 10.1016/j.amjmed.2009.01.028. [DOI] [PubMed] [Google Scholar]
- 28.Pickhardt PJ, Hassan C, Laghi A, Zullo A, Kim DH, Iafrate F, Morini S. Clinical management of small (6- to 9-mm) polyps detected at screening CT colonography: a cost-effectiveness analysis. AJR Am J Roentgenol. 2008;191:1509–1516. doi: 10.2214/AJR.08.1010. [DOI] [PubMed] [Google Scholar]
- 29.Pickhardt PJ, Kim DH. Colorectal cancer screening with CT colonography: key concepts regarding polyp prevalence, size, histology, morphology, and natural history. AJR Am J Roentgenol. 2009;193:40–46. doi: 10.2214/AJR.08.1709. [DOI] [PubMed] [Google Scholar]
- 30.Lieberman D, Moravec M, Holub J, Michaels L, Eisen G. Polyp size and advanced histology in patients undergoing colonoscopy screening: implications for CT colonography. Gastroenterology. 2008;135:1100–1105. doi: 10.1053/j.gastro.2008.06.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Soetikno RM, Kaltenbach T, Rouse RV, Park W, Maheshwari A, Sato T, Matsui S, Friedland S. Prevalence of nonpolypoid (flat and depressed) colorectal neoplasms in asymptomatic and symptomatic adults. JAMA. 2008;299:1027–1035. doi: 10.1001/jama.299.9.1027. [DOI] [PubMed] [Google Scholar]
- 32.Pickhardt PJ, Nugent PA, Choi JR, Schindler WR. Flat colorectal lesions in asymptomatic adults: implications for screening with CT virtual colonoscopy. AJR Am J Roentgenol. 2004;183:1343–1347. doi: 10.2214/ajr.183.5.1831343. [DOI] [PubMed] [Google Scholar]
- 33.Van Gelder RE, Nio CY, Florie J, Bartelsman JF, Snel P, De Jager SW, Van Deventer SJ, Laméris JS, Bossuyt PM, Stoker J. Computed tomographic colonography compared with colonoscopy in patients at increased risk for colorectal cancer. Gastroenterology. 2004;127:41–48. doi: 10.1053/j.gastro.2004.03.055. [DOI] [PubMed] [Google Scholar]
- 34.Park SH, Ha HK, Kim AY, Kim KW, Lee MG, Kim PN, Shin YM, Byeon JS, Yang SK, Kim JH, et al. Flat polyps of the colon: detection with 16-MDCT colonography--preliminary results. AJR Am J Roentgenol. 2006;186:1611–1617. doi: 10.2214/AJR.04.1889. [DOI] [PubMed] [Google Scholar]
- 35.Park SH, Kim SY, Lee SS, Bogoni L, Kim AY, Yang SK, Myung SJ, Byeon JS, Ye BD, Ha HK. Sensitivity of CT colonography for nonpolypoid colorectal lesions interpreted by human readers and with computer-aided detection. AJR Am J Roentgenol. 2009;193:70–78. doi: 10.2214/AJR.08.2234. [DOI] [PubMed] [Google Scholar]
- 36.Use of colorectal cancer tests--United States, 2002, 2004, and 2006. MMWR Morb Mortal Wkly Rep. 2008;57:253–258. [PubMed] [Google Scholar]
- 37.Lisi D, Hassan CC, Crespi M. Participation in colorectal cancer screening with FOBT and colonoscopy: an Italian, multicentre, randomized population study. Dig Liver Dis. 2010;42:371–376. doi: 10.1016/j.dld.2009.07.019. [DOI] [PubMed] [Google Scholar]
- 38.Winawer SJ, Zauber AG, Ho MN, O’Brien MJ, Gottlieb LS, Sternberg SS, Waye JD, Schapiro M, Bond JH, Panish JF. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med. 1993;329:1977–1981. doi: 10.1056/NEJM199312303292701. [DOI] [PubMed] [Google Scholar]
- 39.Gluecker TM, Johnson CD, Harmsen WS, Offord KP, Harris AM, Wilson LA, Ahlquist DA. Colorectal cancer screening with CT colonography, colonoscopy, and double-contrast barium enema examination: prospective assessment of patient perceptions and preferences. Radiology. 2003;227:378–384. doi: 10.1148/radiol.2272020293. [DOI] [PubMed] [Google Scholar]
- 40.Harewood GC, Wiersema MJ, Melton LJ 3rd. A prospective, controlled assessment of factors influencing acceptance of screening colonoscopy. Am J Gastroenterol. 2002;97:3186–3194. doi: 10.1111/j.1572-0241.2002.07129.x. [DOI] [PubMed] [Google Scholar]
- 41.Iannaccone R, Laghi A, Catalano C, Mangiapane F, Lamazza A, Schillaci A, Sinibaldi G, Murakami T, Sammartino P, Hori M, et al. Computed tomographic colonography without cathartic preparation for the detection of colorectal polyps. Gastroenterology. 2004;127:1300–1311. doi: 10.1053/j.gastro.2004.08.025. [DOI] [PubMed] [Google Scholar]
- 42.Burling D, Taylor SA, Halligan S, Gartner L, Paliwalla M, Peiris C, Singh L, Bassett P, Bartram C. Automated insufflation of carbon dioxide for MDCT colonography: distension and patient experience compared with manual insufflation. AJR Am J Roentgenol. 2006;186:96–103. doi: 10.2214/AJR.04.1506. [DOI] [PubMed] [Google Scholar]
- 43.Edwards JT, Mendelson RM, Fritschi L, Foster NM, Wood C, Murray D, Forbes GM. Colorectal neoplasia screening with CT colonography in average-risk asymptomatic subjects: community-based study. Radiology. 2004;230:459–464. doi: 10.1148/radiol.2302021422. [DOI] [PubMed] [Google Scholar]
- 44.Burling D, Halligan S, Slater A, Noakes MJ, Taylor SA. Potentially serious adverse events at CT colonography in symptomatic patients: national survey of the United Kingdom. Radiology. 2006;239:464–471. doi: 10.1148/radiol.2392051101. [DOI] [PubMed] [Google Scholar]
- 45.Sosna J, Blachar A, Amitai M, Barmeir E, Peled N, Goldberg SN, Bar-Ziv J. Colonic perforation at CT colonography: assessment of risk in a multicenter large cohort. Radiology. 2006;239:457–463. doi: 10.1148/radiol.2392050287. [DOI] [PubMed] [Google Scholar]
- 46.Pickhardt PJ. Incidence of colonic perforation at CT colonography: review of existing data and implications for screening of asymptomatic adults. Radiology. 2006;239:313–316. doi: 10.1148/radiol.2392052002. [DOI] [PubMed] [Google Scholar]
- 47.Gatto NM, Frucht H, Sundararajan V, Jacobson JS, Grann VR, Neugut AI. Risk of perforation after colonoscopy and sigmoidoscopy: a population-based study. J Natl Cancer Inst. 2003;95:230–236. doi: 10.1093/jnci/95.3.230. [DOI] [PubMed] [Google Scholar]
- 48.Neri E, Caramella D, Vannozzi F, Turini F, Cerri F, Bartolozzi C. Vasovagal reactions in CT colonography. Abdom Imaging. 2007;32:552–555. doi: 10.1007/s00261-006-9055-6. [DOI] [PubMed] [Google Scholar]
- 49.Brenner DJ, Georgsson MA. Mass screening with CT colonography: should the radiation exposure be of concern? Gastroenterology. 2005;129:328–337. doi: 10.1053/j.gastro.2005.05.021. [DOI] [PubMed] [Google Scholar]
- 50.Little MP, Wakeford R, Tawn EJ, Bouffler SD, Berrington de Gonzalez A. Risks associated with low doses and low dose rates of ionizing radiation: why linearity may be (almost) the best we can do. Radiology. 2009;251:6–12. doi: 10.1148/radiol.2511081686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tubiana M, Feinendegen LE, Yang C, Kaminski JM. The linear no-threshold relationship is inconsistent with radiation biologic and experimental data. Radiology. 2009;251:13–22. doi: 10.1148/radiol.2511080671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Health Physics Society (HPS) Ionizing radiation-safety standards for the general public: Position Statement of the Health Physics Society. McLean, VA: 2003. [Google Scholar]
- 53.Tubiana M, Aurengo A. Dose effect relationships and the estimation of the carcinogenic effects of low doses of ionizing radiation. Academy of Medicine (Paris) and Academy of Science (Paris) Joint Report. Int J Low Radiat. 2006;2:135–153. [Google Scholar]
- 54.International Commission on Radiological Protection. Low-dose extrapolation of radiation-related cancer risk. Publication 99. Amsterdam, the Netherlands: Elsevier; 2006. [Google Scholar]
- 55.National Research Council, Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation. Health risks from low levels of ionizing radiation: BEIR VII, Phase 2. Washington, DC: The National Academies Press; 2006. [PubMed] [Google Scholar]
- 56.Liedenbaum MH, Venema HW, Stoker J. Radiation dose in CT colonography--trends in time and differences between daily practice and screening protocols. Eur Radiol. 2008;18:2222–2230. doi: 10.1007/s00330-008-0994-x. [DOI] [PubMed] [Google Scholar]
- 57.Thorne MC. Background radiation: natural and man-made. J Radiol Prot. 2003;23:29–42. doi: 10.1088/0952-4746/23/1/302. [DOI] [PubMed] [Google Scholar]
- 58.Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007;357:2277–2284. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 59.Nelson RS, Thorson AG. Colorectal cancer screening. Curr Oncol Rep. 2009;11:482–489. doi: 10.1007/s11912-009-0065-8. [DOI] [PubMed] [Google Scholar]
- 60.Zeeb H, Blettner M, Langner I, Hammer GP, Ballard TJ, Santaquilani M, Gundestrup M, Storm H, Haldorsen T, Tveten U, et al. Mortality from cancer and other causes among airline cabin attendants in Europe: a collaborative cohort study in eight countries. Am J Epidemiol. 2003;158:35–46. doi: 10.1093/aje/kwg107. [DOI] [PubMed] [Google Scholar]
- 61.Guérin S, Richard G, Biau A, Lebre S, Crescini D, Haddy N, Guldner L, Paoletti C, Hill C, de Vathaire F. Cancer mortality among French nuclear contract workers. Am J Ind Med. 2009;52:916–925. doi: 10.1002/ajim.20768. [DOI] [PubMed] [Google Scholar]
- 62.Jeong M, Jin YW, Yang KH, Ahn YO, Cha CY. Radiation exposure and cancer incidence in a cohort of nuclear power industry workers in the Republic of Korea, 1992-2005. Radiat Environ Biophys. 2010;49:47–55. doi: 10.1007/s00411-009-0247-7. [DOI] [PubMed] [Google Scholar]
- 63.Sonnenberg A, Delcò F, Bauerfeind P. Is virtual colonoscopy a cost-effective option to screen for colorectal cancer? Am J Gastroenterol. 1999;94:2268–2274. doi: 10.1111/j.1572-0241.1999.01304.x. [DOI] [PubMed] [Google Scholar]
- 64.Ladabaum U, Song K, Fendrick AM. Colorectal neoplasia screening with virtual colonoscopy: when, at what cost, and with what national impact? Clin Gastroenterol Hepatol. 2004;2:554–563. doi: 10.1016/s1542-3565(04)00247-2. [DOI] [PubMed] [Google Scholar]
- 65.Vijan S, Hwang I, Inadomi J, Wong RK, Choi JR, Napierkowski J, Koff JM, Pickhardt PJ. The cost-effectiveness of CT colonography in screening for colorectal neoplasia. Am J Gastroenterol. 2007;102:380–390. doi: 10.1111/j.1572-0241.2006.00970.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Pickhardt PJ, Hassan C, Laghi A, Zullo A, Kim DH, Morini S. Cost-effectiveness of colorectal cancer screening with computed tomography colonography: the impact of not reporting diminutive lesions. Cancer. 2007;109:2213–2221. doi: 10.1002/cncr.22668. [DOI] [PubMed] [Google Scholar]
- 67.Lin OS, Kozarek RA, Schembre DB, Ayub K, Gluck M, Cantone N, Soon MS, Dominitz JA. Risk stratification for colon neoplasia: screening strategies using colonoscopy and computerized tomographic colonography. Gastroenterology. 2006;131:1011–1019. doi: 10.1053/j.gastro.2006.08.015. [DOI] [PubMed] [Google Scholar]
- 68.Heitman SJ, Manns BJ, Hilsden RJ, Fong A, Dean S, Romagnuolo J. Cost-effectiveness of computerized tomographic colonography versus colonoscopy for colorectal cancer screening. CMAJ. 2005;173:877–881. doi: 10.1503/cmaj.050553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hassan C, Zullo A, Laghi A, Reitano I, Taggi F, Cerro P, Iafrate F, Giustini M, Winn S, Morini S. Colon cancer prevention in Italy: cost-effectiveness analysis with CT colonography and endoscopy. Dig Liver Dis. 2007;39:242–250. doi: 10.1016/j.dld.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 70.Mavranezouli I, East JE, Taylor SA. CT colonography and cost-effectiveness. Eur Radiol. 2008;18:2485–2497. doi: 10.1007/s00330-008-1058-y. [DOI] [PubMed] [Google Scholar]
- 71.Siddiki H, Fletcher JG, McFarland B, Dajani N, Orme N, Koenig B, Strobel M, Wolf SM. Incidental findings in CT colonography: literature review and survey of current research practice. J Law Med Ethics. 2008;36:320–331, 213. doi: 10.1111/j.1748-720X.2008.00276.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Edwards JT, Wood CJ, Mendelson RM, Forbes GM. Extracolonic findings at virtual colonoscopy: implications for screening programs. Am J Gastroenterol. 2001;96:3009–3012. doi: 10.1111/j.1572-0241.2001.04679.x. [DOI] [PubMed] [Google Scholar]
- 73.Gluecker TM, Johnson CD, Wilson LA, Maccarty RL, Welch TJ, Vanness DJ, Ahlquist DA. Extracolonic findings at CT colonography: evaluation of prevalence and cost in a screening population. Gastroenterology. 2003;124:911–916. doi: 10.1053/gast.2003.50158. [DOI] [PubMed] [Google Scholar]
- 74.Pickhardt PJ, Hanson ME, Vanness DJ, Lo JY, Kim DH, Taylor AJ, Winter TC, Hinshaw JL. Unsuspected extracolonic findings at screening CT colonography: clinical and economic impact. Radiology. 2008;249:151–159. doi: 10.1148/radiol.2491072148. [DOI] [PubMed] [Google Scholar]
- 75.Hassan C, Pickhardt PJ, Laghi A, Kim DH, Zullo A, Iafrate F, Di Giulio L, Morini S. Computed tomographic colonography to screen for colorectal cancer, extracolonic cancer, and aortic aneurysm: model simulation with cost-effectiveness analysis. Arch Intern Med. 2008;168:696–705. doi: 10.1001/archinte.168.7.696. [DOI] [PubMed] [Google Scholar]