Abstract
The peroxisome proliferator-activated receptor-γ (PPARγ) coactivator-1α (PGC-1α) is a major regulator of exercise-induced phenotypic adaptation and substrate utilization. We provide an overview of 1) the role of PGC-1α in exercise-mediated muscle adaptation and 2) the possible insulin-sensitizing role of PGC-1α. To these ends, the following questions are addressed. 1) How is PGC-1α regulated, 2) what adaptations are indeed dependent on PGC-1α action, 3) is PGC-1α altered in insulin resistance, and 4) are PGC-1α-knockout and -transgenic mice suitable models for examining therapeutic potential of this coactivator? In skeletal muscle, an orchestrated signaling network, including Ca2+-dependent pathways, reactive oxygen species (ROS), nitric oxide (NO), AMP-dependent protein kinase (AMPK), and p38 MAPK, is involved in the control of contractile protein expression, angiogenesis, mitochondrial biogenesis, and other adaptations. However, the p38γ MAPK/PGC-1α regulatory axis has been confirmed to be required for exercise-induced angiogenesis and mitochondrial biogenesis but not for fiber type transformation. With respect to a potential insulin-sensitizing role of PGC-1α, human studies on type 2 diabetes suggest that PGC-1α and its target genes are only modestly downregulated (≤34%). However, studies in PGC-1α-knockout or PGC-1α-transgenic mice have provided unexpected anomalies, which appear to suggest that PGC-1α does not have an insulin-sensitizing role. In contrast, a modest (∼25%) upregulation of PGC-1α, within physiological limits, does improve mitochondrial biogenesis, fatty acid oxidation, and insulin sensitivity in healthy and insulin-resistant skeletal muscle. Taken altogether, there is substantial evidence that the p38γ MAPK-PGC-1α regulatory axis is critical for exercise-induced metabolic adaptations in skeletal muscle, and strategies that upregulate PGC-1α, within physiological limits, have revealed its insulin-sensitizing effects.
Keywords: endurance exercise, angiogenesis, mitochondria, fatty acid metabolism, glucose
skeletal muscle is highly adaptable to changes in contractile activity and to changes in the substrate/endocrine milieu. Although the molecular bases for these adaptive responses had remained uncertain for many years, the peroxisome proliferator-activated receptor-γ (PPARγ) coactivator 1α (PGC-1α) has revealed itself to be a major regulator of exercise-induced phenotypic adaptation and substrate utilization. In the present paper, we provide an overview and perspective on the mechanisms by which PGC-1α is regulated by endurance exercise training as well as on the influence of PGC-1α on fiber type transformation, angiogenesis, mitochondrial biogenesis, lipid metabolism, and insulin sensitivity.
The first part of this review examines 1) the pathways involved in PGC-1α regulation in response to endurance exercise or increased contractile activity and 2) the role of PGC-1α in endurance exercise-induced adaptations in skeletal muscle. The second half of this review examines whether PGC-1α acts as an insulin-sensitizing agent, since one of the most beneficial and clinically relevant effects of exercise is the improvement in insulin sensitivity in skeletal muscle. To this end, the impact of type 2 diabetes on PGC-1α expression and function as well as the use of in vivo models to examine the role of this coactivator as a therapeutic target are discussed.
PGC-1α Function in Skeletal Muscle
PGC-1α, a transcriptional coactivator identified through its interaction with PPARγ in brown fat cells, was found to be greatly upregulated in brown fat and skeletal muscle in response to cold exposure (159). PGC-1α is now known to be involved in the regulation of thermogenesis, energy metabolism, and other biological processes that are critical in controlling phenotypic characteristics of various organ systems (112, 158, 159, 213). PGC-1α interacts with and coactivates a growing list of transcription factors and nuclear receptors, including estrogen-related receptor-α (88, 89, 159), thyroid receptor (159), nuclear respiratory factor-1 (NRF-1) (227), NRF-2 (136), and myocyte enhancer factor 2 (MEF2) (72, 132). As a consequence, PGC-1α is involved in the coordinated regulation of nuclear- and mitochondrial-encoded genes required for contractile and metabolic adaptations in skeletal muscle (158, 177, 215). Importantly, PGC-1α expression per se is also regulated by PGC-1α via its interaction with MEF2 on its own promoter in a feed-forward regulatory loop (72). PGC-1α activity is regulated by posttranslational modifications through phosphorylation (93), sumoylation (175), and deacetylation (29). Therefore, posttranslational activation of PGC-1α will lead to enhanced expression of target genes as well as PGC-1α itself.
Skeletal muscle is essential for locomotive and other daily activities, and under insulin-stimulated conditions this tissue removes 70–90% of a glucose load (48, 49, 102). In mammals, skeletal muscles present a mosaic of different fiber types. Based on the expression of the predominant isoform of myosin heavy-chain proteins, myofibers can be classified as type I, IIa, IId/x, and IIb (54, 201). Type I fibers are slow-twitch fibers (slow contractile force development) (219) and have an oxidative profile (high mitochondrial content and capillary density) (156, 187). These myofibers also actively express glucose transporter 4 (GLUT4) (60) and present great sensitivity to insulin (79). Type IIa fibers are fast-twitch fibers (fast contractile force development) (53) but have similar oxidative profiles to the type I fibers, whereas type IId/x fibers are fast-twitch fibers with a glycolytic metabolic profile (low mitochondrial content and capillary density) (156), express low GLUT4 (60), and have low sensitivity to insulin stimulation (79). Rodents also have type IIb fibers with an even more fast-twitch, glycolytic phenotype than type IId/x fibers (166, 167). It is important to note that insulin sensitivity can be affected within a given fiber type by several mechanisms. These will be discussed in more detail in subsequent sections.
It is well known that increased contractile activity, such as endurance exercise training, promotes phenotypic adaptations in skeletal muscle toward a more oxidative phenotype. Specifically, endurance exercise training leads to fiber type transformation, mitochondrial biogenesis, angiogenesis, and other adaptive changes in skeletal muscles along with improved insulin sensitivity and metabolic flexibility in both rodents and humans (38, 43, 65, 82, 105, 179, 184, 203). The orchestrated regulation of these processes is of extreme elegance, and current findings suggest that PGC-1α is a key player for several of these adaptations.
Animal and cellular genetic models with altered expression of the PGC-1α gene have provided much of the evidence for the role of PGC-1α in fiber type specificity (116), mitochondrial biogenesis (70), angiogenesis (5), GLUT4 expression (72, 132), and improved exercise performance (28). In addition, PGC-1α mRNA and protein expressions are very responsive to endurance exercise (11, 67, 90, 153, 172, 199). In the face of the growing body of knowledge underscoring the importance of PGC-1α in skeletal muscle phenotype determination, the two critical questions to be addressed in the context of exercise are 1) how PGC-1α is regulated and 2) what adaptations are indeed dependent on PGC-1α action.
PGC-1α Regulation in Response to Exercise
Multiple signaling pathways act to regulate PGC-1α in skeletal muscle. Table 1 summarizes the main findings of studies investigating pathways potentially involved in PGC-1α regulation in vivo. These and other reports are discussed in the following paragraphs. Current evidence supports that p38γ MAPK signaling is functionally required for endurance exercise-induced PGC-1α regulation. This signaling-transcription regulatory axis may present a node of cross-talk with other signaling pathways reviewed here.
Table 1.
Evidence for basal and exercise-induced PGC-1α regulation in adult skeletal muscle of rodents in vivo*1
| Skeletal Muscle Phenotype*4 |
|||||
|---|---|---|---|---|---|
| Signaling Pathway/Model | Basal PGC-1α Level*2 | Exercise-Induced PGC-1α Upregulation*3 | Basal*5 | In Response to Exercise*6 | References |
| Calcineurin | |||||
| Constitutively active calcineurin | ⇑Protein | Not tested | ⇑Slow-twitch fibers, ⇑troponin I, ⇑myoglobin, ⇑GLUT4, ⇑PDK4, ⇑mitochondrial enzymes, ⇑lipid oxidation rates, ⇓CHO oxidation rates, ⇑exercise performance | Not tested | 97, 123, 142, 174 |
| Pharmacological inhibition (cyclosporine A) | Not tested | Normal induction (mRNA and protein) [5-days of exercise] | ⇓COX I protein, ⇓COX IV protein | ⇑ERRα, ⇑PPARδ, ⇑NRF-2, ⇑TFAM mRNA and several mitochondrial proteins (except COX I and COX IV; compared with sedentary vehicle-treated controls) | 57 |
| CaMKIV | |||||
| Constitutively active CaMKIV | ⇑mRNA | Not tested | ⇑Mitochondrial DNA, ⇑slow-twitch fibers, ⇑myoglobin protein, ⇑CPT I protein | Not tested | 225 |
| CaMKIV-KO | ⇔Protein | Normal induction (mRNA and protein) [nerve stimulation and 4 wk of training] | ⇑Type I fibers, ⇓exercise performance | ⇑myoglobin, ⇑MHCIIa and ⇑COXIV proteins, ⇓exercise performance | 4 |
| Reactive nitrogen species | |||||
| Pharmacological inhibition of NOS (l-NAME)*8 | ⇔Protein | Higher induction (mRNA) [∼53 min of treadmill running] | ⇔COX-III and ⇔COX IV mRNA, ⇔COX activity, ⇔COX IV protein, ⇔citrate synthase and β-HAD activities | ⇑TFAM mRNA in EDL (compared with sedentary l-NAME-treated controls) | 211 |
| eNOS and nNOS-KO*8 | ⇔mRNA eNOS-KO, ⇑mRNA nNOS-KO | Normal induction (mRNA) [1 and 9 days, 60 min of treadmill running] | ⇑NRF-1, ⇑NRF-2, ⇑TFAM mRNA (all in nNOS-KO), no changes in eNOS-KO | ⇑NRF2α mRNA, ⇑cytochrome c protein (both eNOS and nNOS-KO) | 210 |
| Reactive oxygen species | |||||
| Pharmacological inhibition of xanthine oxidase (allopurinol) | Not tested | Reduced induction (protein) [∼88 min of treadmill running] | Not tested | ⇓NRF-1, ⇓TFAM protein (compared with exercise untreated) | 101 |
| AMPK | |||||
| Pharmacological activation (AICAR, metformin) | ⇑mRNA and protein | Not tested | ⇑Cytochrome c, ⇑GLUT4, ⇑activity of citrate synthase, malate dehydrogenase, hexokinase II, and β-HAD, ⇑exercise performance | Not tested | 29*9, 93*10, 141, 195, 218 |
| Mutated AMPKγ3*11 (genetic activation) | ⇑mRNA | Not tested | ⇑NRF-1, ⇑NRF-2, ⇑TFAM, ⇑cytochrome c, ⇑COX IV and ⇑citrate synthase mRNAs, ⇑mitochndrial area and protein expression of respiratory complexes | Not tested | 58 |
| Dominant-negative AMPKα2 | ⇔mRNA*12 | Not tested | ⇔Cytochrome c protein, ⇔ALAS mRNA | Not tested | 230 |
| Global AMPKα2 and global AMPKα1-KO*13 | ⇔mRNA | Normal induction (mRNA) [90-min run test] | ⇔FOXO1, ⇔hexokinase II, ⇔PDK4 mRNA (both α1-KO and α2-KO), ⇔GLUT4, ⇔CPT1, ⇔UCP3 mRNA (α2-KO) | ⇑FOXO1, ⇑hexokinase II, ⇑PDK4 mRNA (both α1-KO and α2-KO) | 98 |
| AMPKα2 muscle- specific KO | ⇓Protein | Normal induction (protein) [6 wk of voluntary wheel running] | ⇓Citrate synthase activity, ⇓%type IIa/IIx fibers, ⇔hexokinase II protein | ⇑Citrate synthase activity, ⇑succinate dehydrogenase activity, ⇑%type IIa/IIx fibers, ⇔hexokinase II protein | 168 |
| Mutated AMPKγ1 (muscle-specific activation) | ⇑Protein | Normal induction (protein) [6 wk of voluntary wheel running] | ⇑Citrate synthase activity, ⇑% type IIa/IIx fibers, ⇑hexokinase II protein | ⇔Citrate synthase activity, ⇔succinate dehydrogenase activity, ⇔%type IIa/IIx fibers, ⇔hexokinase II protein | 168 |
| p38 MAPK | |||||
| MKK6 muscle-specific overexpression (upstream kinase of p38 MAPKs) | ⇑Protein | Not tested | ⇑COX IV | Not tested | 3 |
| p38γ MAPK muscle-specific KO | ⇔mRNA | Reduced induction (mRNA) [nerve stimulation] | ⇔Cytochrome c, ⇔COX IV, ⇔capillary density | ⇑Type IIb to IIa/IIx fiber type shift, ⇔cytochrome c and COX IV (to 4 wk of running), ⇔VEGF (nerve stimulation) | 154 |
PGC-1α, peroxisome proliferator-activated receptor (PPAR)γ coactivator-1α; GLUT4, glucose transporter 4; PDK4, pyruvate dehydrogenase kinase-4; CHO, carbohydrate; COX I, III, and IV, cytochrome oxidase I, III, and IV; ALAS, α-aminolevulinate synthase; ERRα, estrogen-related receptor-α; NRF-1 and -2, nuclear respiratory factor-1 and -2; TFAM, mitochondrial transcription factor A; CPT I, carnitine palmitoyl transferase I; MHCIIa, myosin heavy chain IIa; EDL, extensor digitorum longus; l-NAME, NG-nitro-l-arginine methyl ester; FOXO1, forkhead box-containing protein O1; NOS, nitric oxide synthase; eNOS and nNOS, endothelial and neuronal isoforms of NOS, respectively; KO, knockout; AICAR, 5-aminoimidazole-4-carboxamide-1-β-d-ribofuranoside; β-HAD, β-hydroxyacyl-CoA dehydrogenase; AMPK, AMP-activated protein kinase; MKK6, mitogen-activated protein kinase kinase-6. ⇓Reduction; ⇔no change; ⇑increase;
Refer to text and original references for details.
Results for basal levels of PGC-1α and skeletal muscle phenotype under basal conditions are in comparison with untreated wild-type mice or wild-type littermates.
Results for exercise-induced PGC-1α upregulation are in comparison with exercised wild-type mice (pharmacological treatments) or exercised wild-type littermates (genetic manipulations) submitted to the specified exercise protocol in square brackets.
Only the main findings are listed.
Results for skeletal muscle phenotype in response to exercise are in comparison with the same genotype when sedentary and/or not nerve stimulated (unless when specified in brackets).
Findings suggest that COX I and COX IV mRNA upregulation was normal, but some sort of toxicity imposed by cyclosporine A prevented these proteins from being upregulated.
Only results for the EDL muscle are presented.
Cantó et al. (29) demonstrated that PGC-1α is activated by sirtuin 1-mediated deacetylation following PGC-1α phosphorylation by AMPK (via AICAR stimulation).
Jäger et al. (93) demonstrated that AMPK (via AICAR stimulation) directly phosphorylates and activates PGC-1α.
Trangenic mice expressing the mutant AMPKγ3 R225Q that increases the activity of the AMPK complex, preferentially expressed in glycolytic muscle.
At basal levels, PGC-1α expression was not affected, but PGC-1α upregulation in response to β-guanidinopropionic acid (a creatine analog) was prevented.
Only results for the quadriceps muscle are presented.
Ca2+/calmodulin-dependent signaling.
Rhythmic skeletal muscle contractions activate the Ca2+/calmodulin-dependent serine/threonine protein phosphatase calcineurin (CnA) and Ca2+/calmodulin-dependent protein kinases (CaMKs). CnA has been implicated in the expression of slow-twitch muscle genes through dephosphorylation and activation of the nuclear factor of activated T cells (NFAT) (37, 183). Transgenic mice overexpressing constitutively active CnA in skeletal muscle present an increased number of slow-twitch myofibers and elevated expression of slow-twitch troponin I, myoglobin, GLUT4, pyruvate dehydrogenase kinase-4 (PDK4), mitochondrial enzymes, and PGC-1α (142, 174). These mice have low levels of carbohydrate oxidation rates along with high lipid oxidation rates in the glycolytic extensor digitorum longus (EDL) muscle (123, 174) and present enhanced endurance exercise performance (97). The phenotypic changes observed are similar to the ones reported in muscle-specific PGC-1α-transgenic mice (28, 116, 215) and consistent with the notion that CnA activates MEF2 and induces PGC-1α transcription (72, 227). Genetic and pharmacological interventions that inhibit or abolish CnA/NFAT activity have consistently reduced slow-twitch muscle gene expression (129) and blocked mechanical overload-induced transformation of fibers to type IIa and type I (134). However, animals treated with cyclosporine A, a pharmacological inhibitor of CnA, presented normal upregulation of PGC-1α and mitochondrial enzymes in response to endurance exercise training (57). Therefore, there is strong evidence for an essential functional role of the CnA-NFAT regulatory axis in the maintenance of slow-twitch myofibers and in the promotion of IIb/IId/x-to-IIa fiber type transformation in response to increased contractile activity. A direct role of this signaling pathway in the upregulation of PGC-1α and metabolic adaptations in skeletal muscle, especially in the context of exercise, is not currently supported.
CaMKs have been shown to act synergistically with CnA to activate slow and oxidative fiber-specific gene expression in cultured myocytes (226). Skeletal muscle expression of CaMKIV has also been suggested to link energy deprivation to increased expression of PGC-1α and mitochondrial biogenesis in skeletal muscle (230). The forced expression of a constitutively active CaMKIV in skeletal muscle in transgenic mice increases expression of the PGC-1α gene and enhances mitochondrial biogenesis along with reduced fatigability of EDL muscle (225). However, genetic disruption of the CaMKIV gene did not prevent exercise-induced upregulation of PGC-1α and IIb-to-IIa fiber type transformation (4). Actually, current evidence does not support the expression of CaMKIV in skeletal muscle (171). However, it is possible that a different CaMK, such as CaMKII or CaMKK or other protein kinases, may act upon substrates targeted by the constitutively active form of CaMKIV and mediate skeletal muscle plasticity.
CaMKII, the main CaMK isoform in skeletal muscle (36, 170, 171), is activated (phosphorylated) by endurance exercise (160, 170, 171). Caffeine treatment of adult skeletal muscle ex vivo at levels that increase cytosolic calcium but are insufficient to cause contraction activated CaMKII (224) along with p38 MAPK activation, PGC-1α upregulation, and mitochondrial biogenesis (222). These adaptations appeared to be dependent on both CaMKII and p38 MAPK activities because the CaMKII inhibitor KN93 blocked p38 MAPK activation, and the p38 MAPK inhibitor SB-202190 prevented mitochondrial biogenesis (222). These ex vivo studies provide insights into Ca2+-dependent signaling in skeletal muscle by circumventing other cellular events that occur during contraction. However, CaMKII requirement for exercise-induced upregulation of PGC-1α and adaptation remains to be determined. More recently, endurance exercise in humans has been shown to lead to nuclear export of class IIa histone deacetylase (HDAC)4 and HDAC5 along with activation of CaMKII and AMP-activated protein kinase (AMPK) in skeletal muscle (130). HDAC5 normally inhibits MEF2 activity and represses PGC-1α transcription in skeletal muscle (46, 72). These observations suggest a potential pathway for CaMKII regulation of PGC-1α during exercise. Finally, CaMKK has been shown to be a kinase of AMPK (96, 221) responsible for AMPK activation during contractions in skeletal muscle (96). Therefore, CaMKII and CaMKK may function as upstream kinases in exercise-induced regulation of PGC-1α via regulation of p38 MAPK, HDAC5, and AMPK activation. However, these hypotheses would benefit from experiments with loss-of-function approaches in animal models of exercise in vivo.
Reactive nitrogen and oxygen species-dependent signaling.
Nitric oxide (NO) production is increased during contractile activity (13, 149, 185). Both endothelial and neuronal isoforms of NO synthase (eNOS and nNOS, respectively) have been shown to be activated by Ca2+/calmodulin and AMPK (34, 35, 47, 161, 197). Several studies suggest a role of endogenous NO in AMPK- and Ca2+-dependent regulation of PGC-1α, GLUT4, and mitochondrial genes (119, 128). NO is also required for functional overload-induced upregulation of slow myosin heavy chain (MHC; type 1/β) (182) through modulation of Akt and glycogen synthase kinase-3β (GSK-3β) activities and amplification of CnA/NFAT-dependent signaling (51). In support of this, eNOS−/− muscle cells have reduced type 1 MHC expression (52), and low levels of NO donors promote mitochondrial biogenesis, PGC-1α, and GLUT4 expression in cultured muscle cells (119, 145) through a mechanism involving AMPKα1 activation (Lira VA and Criswell DS, unpublished data). However, neither pharmacological inhibition (by NG-nitro-l-arginine methyl ester) in rats nor genetic deletion of eNOS or nNOS genes in mice prevents endurance exercise-induced PGC-1α mRNA expression in skeletal muscle (210, 211). Altogether, these studies support a role for NO in PGC-1α regulation, mitochondrial biogenesis, and fast-to-slow fiber type transformation but not in the exercise-induced increase in PGC-1α.
There is also ample evidence for increased reactive oxygen species (ROS) in the form of superoxide anions (O2−), hydrogen peroxide (H2O2), and hydroxyl radical (OH−) in skeletal muscle during contraction (41, 101, 126, 127, 149, 162, 186). Peroxynitrite (ONOO−), an oxidant formed by a reaction between NO and O2−, is also found in the extracellular fluid of muscle during contraction (149). Most studies point toward H2O2 as an important signaling molecule for metabolic adaptations in skeletal muscle. Silveira et al. (186) showed that H2O2 produced by contracting skeletal muscle cells was required for PGC-1α upregulation. Irrcher et al. (91) observed that treatment of skeletal muscle cells with H2O2 reduced cellular ATP levels, activated AMPK, and increased PGC-1α mRNA, suggesting that H2O2 can promote PGC-1α expression through AMPK. Interestingly, increased H2O2 production has been proposed as an indirect mechanism by which lactate, a by-product of glycolysis, upregulates PGC-1α (75). Most importantly, ROS has been shown to be functionally important for endurance exercise-induced PGC-1α expression and metabolic adaptation in skeletal muscle. High-dose antioxidant supplementation blocks endurance exercise-induced upregulation of transcriptional regulators, including PGC-1α and genes involved in mitochondrial biogenesis (63, 165), and precludes the beneficial effect of endurance exercise on insulin sensitivity in humans (165). More recently, it has been reported that pharmacological inhibition of xanthine oxidase with allopurinol suppresses the exercise-induced upregulation in PGC-1α in parallel to blunted activation (i.e., phosphorylation) of p38 MAPK in rats. These findings suggest that ROS is involved in p38 MAPK activation and subsequent regulation of PGC-1α expression in response to contraction in vivo (101). Future studies should focus on the precise molecular mechanism by which ROS influences exercise-induced PGC-1α regulation and muscle adaptation.
AMPK signaling.
AMPK, a sensor of metabolic stress and energy deprivation, is also activated by contractile activity in skeletal muscle (55, 69, 74, 217, 218, 220). Multiple mechanisms for AMPK-mediated PGC-1α regulation have been postulated. First, exercise-induced AMPK activation is associated with HDAC5 phosphorylation, nuclear export, and derepression of PGC-1α transcription in human skeletal muscle (130, 209). Second, AMPK has been shown to stimulate the cAMP response element-binding protein (202), the upstream stimulatory factor, and possibly GATA4 in transcriptional activation of the PGC-1α gene in cultured cells (72, 92). Third, both phosphorylation and deacetylation of PGC-1α are required for upregulation of the PGC-1α gene and mitochondrial genes (29, 93). Mechanistically, AMPK directly activates PGC-1α by phosphorylating Thr177 and Ser538 (93), which is required for PGC-1α deacetylation by HDAC sirtuin 1 (SIRT1) (29). Interestingly, AMPK activates SIRT1 indirectly by stimulating β-oxidation and subsequently increasing the NAD+/NADH ratio (29) and by promoting the expression of nicotinamide phosphoribosyltransferase in NAD+ biogenesis (45, 56). Endurance exercise in humans can also stimulate SIRT1 through this latter mechanism (45, 56), and a single bout of exercise induces PGC-1α deacetylation especially in the glycolytic EDL and gastrocnemius muscles, correlating with upregulation of PGC-1α target genes such as PDK4, GLUT4, and carnitine palmitoyl transferase Ib (29).
Pharmacological activation of AMPK by 5-aminoimidazole-4-carboxamide-1-β-d-ribofuranoside (AICAR) increases PGC-1α gene expression and mitochondrial biogenesis in skeletal muscle (195, 218). In addition, AICAR enhances the running ability of mice even in the absence of exercise training (141). Mice expressing a gain-of-function mutation in the regulatory γ3-subunit of AMPK, expressed predominantly in glycolytic fibers, present increased expression of PGC-1α and other transcription factors associated with mitochondrial biogenesis (58). More recently, Cantó et al. (30) have demonstrated that exercise-induced PGC-1α deacetylation was blunted in AMPKγ3-knockout (KO) mice. On the other hand, animals expressing a dominant-negative form of AMPK (dnAMPKα2) in skeletal muscle present normal PGC-1α mRNA levels but are unable to upregulate PGC-1α, mitochondrial DNA, and enzyme activity in response to β-guanidinopropionic acid, a creatine analog that causes metabolic stress (230). These findings are consistent with the notion that AMPK serves as a metabolic sensor that regulates PGC-1α expression and promotes mitochondrial biogenesis in skeletal muscle. However, a muscle-specific expression of a dominant-negative form of AMPK blunted IIb-to-IIa/IIx fiber type transformation in response to voluntary running without affecting the induction of PGC-1α expression or mitochondrial enzyme activity (168). Furthermore, genetic deletion of functional AMPK isoforms failed to block exercise-induced PGC-1α gene expression in skeletal muscle (98). Therefore, it remains to be fully determined whether endurance exercise-induced skeletal muscle adaptation depends on functional AMPK.
p38 MAPK signaling.
Various types of exercise lead to activation of the stress-activated protein kinases, including c-Jun-NH2-terminal kinases, p38 MAPKs, and ERKs in skeletal muscle of humans and rodents (9, 10, 66, 216). Of those, early evidence pointed toward p38 MAPK as the one most likely involved in PGC-1α regulation. p38 MAPK phosphorylates and activates PGC-1α (157) as well as MEF2 (228) and activating transcription factor 2 (ATF2) (31), which are transcription factors that bind to the PGC-1α promoter. In this context, Akimoto et al. (3) demonstrated that p38 MAPK acts through ATF2 phosphorylation to induce PGC-1α expression in skeletal muscle and that muscle-specific overexpression of the upstream kinase (mitogen-activated protein kinase kinase-6) of p38 MAPK resulted in upregulation of PGC-1α and mitochondrial proteins in glycolytic muscles. In a subsequent study, Akimoto et al. (2) observed that PGC-1α transcriptional control in response to motor nerve stimulation required functional interaction of ATF2 with the PGC-1α promoter. These studies provided initial genetic evidence for the role of p38 MAPK in exercise-induced skeletal muscle metabolic phenotype.
Wright et al. (223) observed that p38 MAPK and ATF2 phosphorylation occur in parallel with PGC-1α translocation to the nucleus shortly after an exhaustive bout of swimming exercise. These events coincided with increases in citrate synthase and cytochrome c mRNAs and preceded the upregulation in PGC-1α protein. These observations allude to another potential mechanism of p38 MAPK-mediated activation of PGC-1α, which seems to occur prior to increased PGC-1α transcription. The signals responsible for PGC-1α activation and translocation to the nucleus remain to be determined, but it is likely that phosphorylation and/or deacetylation of PGC-1α is required for this process.
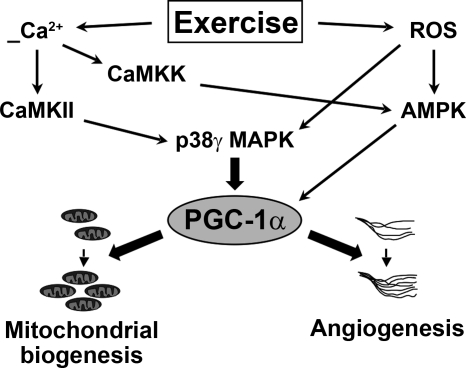
More recently, Pogozelski et al. (154) demonstrated that p38γ MAPK, but not p38α MAPK or p38β MAPK, is required for PGC-1α upregulation in mitochondrial biogenesis and angiogenesis in response to voluntary wheel running and nerve stimulation in mice. None of the p38 MAPK isoforms was required for endurance exercise-induced IIb-to-IIa fiber type transformation in these mice. Of note, a parallel study employing muscle-specific genetic disruption of the PGC-1α gene (61) showed that these mice had the same phenotype as the p38γ MAPK muscle-specific KO mice with impaired metabolic adaptations but normal contractile adaptation to exercise (see below for details). These findings provide functional confirmation for the p38γ MAPK-PGC-1α regulatory axis in exercise-induced skeletal muscle adaptation (Fig. 1) and genetically separate the metabolic adaptation from contractile adaptation in a physiological model of exercise in mice.
Fig. 1.
Signaling pathways involved in exercise-induced peroxisome-proliferator-activated receptor-γ coactivator-1α (PGC-1α) regulation in skeletal muscle. Current evidence suggests roles for calcineurin (CnA), CaMK, AMP-activated protein kinase (AMPK), and p38 MAPK in PGC-1α regulation. Thick arrows depict regulatory events required for exercise-mediated induction of PGC-1α and subsequent adaptations that have been confirmed by gene deletion studies in animal models. Thin arrows depict regulatory events that have been associated with PGC-1α regulation, but their requirement for the exercise-dependent induction of PGC-1α awaits further investigation (refer to text for details). ROS, reactive oxygen species.
PGC-1α and Exercise-Induced Adaptations
Animal and cellular genetic models provide much of the evidence for a functional role of PGC-1α in fiber type specification (72, 116), GLUT4 (132), PDK4 (215), and mitochondrial protein expression (72, 109, 111) as well as angiogenesis (5) in skeletal muscle. However, few studies have examined whether PGC-1α is indeed required for exercise-induced adaptations and what aspects of the adaptive responses, if not all, are affected by the absence of functional PGC-1α in skeletal muscle.
Leick et al. (110) employed a mouse model of global gene disruption of the PGC-1α gene (PGC-1α-KO) and showed that PGC-1α-KO mice had increases in hexokinase II, aminolevulinate synthase 1, and cytochrome oxidase (COX) I protein expression in response to endurance exercise despite the fact that these mice had reduced basal level expression of these metabolic enzymes. They concluded that PGC-1α is not mandatory for exercise- and training-induced adaptive gene responses. Adhihetty et al. (1) extended these findings, confirming that PGC-1α-KO mice have normal voluntary running activity and reduced basal level mitochondrial respiratory function, which can be corrected by endurance exercise training. However, other reports document that PGC-1α-KO mice suffer from hyperactivity due to lesions in the central nervous system, and that these animals have circadian rhythm abnormalities, and present AMPK activation in resting skeletal muscle (70, 117, 121). Therefore, an approach with skeletal muscle-specific gene disruption was then desirable to minimize potential confounding factors of the global PGC-1α-KO models.
Recently, muscle-specific PGC-1α-KO (PGC-1α-MKO) mice were generated (70, 71), and these animals presented reduced locomotive activity, maximal exercise tolerance, and impaired muscle function, consistent with reduced oxidative capacity in skeletal muscles. Despite the fact that PGC-1α-MKO mice exhibited normal voluntary running activity and normal IIb-to-IIa fiber type transformation in skeletal muscles that are recruited during exercise, endurance exercise-induced expression of mitochondrial enzymes (cytochrome c and COX IV) and increases in platelet endothelial cell adhesion molecule-1-positive endothelial cells were significantly attenuated (61). These findings from PGC-1α-MKO underscore the importance of PGC-1α in mitochondrial biogenesis and angiogenesis, but not fiber type transformation, in response to endurance exercise training.
Exercise, Insulin Sensitivity, and PGC-1
For more than two decades, a number of studies have demonstrated the benefits of exercise and muscle contraction on improving insulin sensitivity in rodents and in humans (24, 50, 77, 78, 143, 163, 181, 205, 212, 229). More recently, a key prospective study has shown conclusively that a modest program of moderate exercise (“brisk walking”, 150 min/wk) along with a modest weight loss (−7%, or −5.6 kg) over ∼3 yr markedly reduced the incidence of type 2 diabetes (104). With the discovery of PGC-1α (227) and its exercise-mimetic effects on muscle metabolism (cf. Ref. 73) and the subsequent discovery of PGC-1β (114), a PGC-1α homolog, considerable interest arose as to whether these coactivators had a role in skeletal muscle insulin sensitivity (73, 113).
PGC-1α and PGC-1β share a similar tissue distribution and are expressed in tissues characterized with a high mitochondrial content, including skeletal muscle (108, 114, 131). There seems to be considerable redundancy of function between PGC-1α and PGC-1β. For example, PGC-1β, like PGC-1α, activates genes involved with fatty acid oxidation and mitochondrial biogenesis (7, 100, 114, 115, 131, 176, 190), and in muscle cells PGC-1α and -β increased the mRNAs of GLUT4 (132, 139). However, in lean and insulin-resistant (obese) human muscle, PGC-1α and -β protein expression were not correlated, and only PGC-1α protein correlated with rates of palmitate oxidation and citrate synthase activity, an index of mitochondrial content (85). With exercise training only PGC-1α mRNA was increased (105, 131, 140), whereas PGC-1β mRNA was not altered (105, 131) or was reduced (140). With respect to changes in skeletal muscle with aging (118) and type 2 diabetes (148), some have observed reductions in both PGC-1α and -β mRNA (118, 148), whereas others have observed only a reduction in skeletal muscle PGC-1β mRNA in senescence-prone animals (169) and reductions in PGC-1α mRNA, but not PGC-1β mRNA, in type 2 diabetes (204). Collectively, these observations begin to suggest that although PGC-1β and PGC-1α may share similar functions, they also appear to have some different roles. However, only skeletal muscle PGC-1α expression is consistently downregulated in type 2 diabetes. Indeed, work in cell lines has shown that PGC-1α induces exercise-mimetic effects, increasing mitochondrial biogenesis, fatty acid oxidation, GLUT4 expression, and insulin signaling (132), leading to speculations (73, 105, 113) that the molecular basis for the exercise-mediated improvement in glucose transport is attributable, in part, to PGC-1α.
Lipids, Glucose Transport, and PGC-1α
There is a strong association between skeletal muscle insulin resistance and circulating plasma fatty acid concentrations (18–20) and intramuscular triacylglycerol accumulation (94, 95, 107, 147, 192). However, in athletes intramuscular triacylglycerol depots are also increased, yet they are insulin sensitive (208), possibly as a result of an enhanced capacity for fatty acid oxidation (22, 25, 64, 87). This anomaly between increased intramuscular triacylglycerol depots and improved insulin sensitivity was termed the “athlete paradox.” However, recent work indicates that this is much less of a paradox than was once thought. It is the more soluble, bioactive lipid metabolites such as ceramide, diacylglycerol, and long-chain fatty acyl-CoAs, not intramuscular triacylglycerol storage depots (22, 81, 120), that impair postreceptor insulin signaling, thereby interfering with GLUT4 translocation and glucose transport (32, 33, 80, 193, 194). The increase in intramuscular triacylglycerol depots, whether in athletes or in insulin-resistant muscles, appears to be an attempt to limit intramuscular muscle lipotoxicity, since intracellular triacylglycerol provides a cytoprotective role in lipid-overload states (120, 122).
In insulin resistance and type 2 diabetes, intramuscular lipid accumulation does not result from a reduced intrinsic capacity for fatty acid oxidation by mitochondria (83, 84, 86, 135, 207), as had been widely believed (103, 152). Instead, intramuscular lipids accumulation stems, in part, from a FAT/CD36-mediated increase in fatty acid uptake (23, 62, 83, 124). The excess fatty acids taken up cannot be oxidized away (23, 83, 106), because there is an insufficient compensatory increase in mitochondrial mass (68, 83) or an insufficient capacity for fatty acid oxidation (106), or alternatively, the mitochondrial mass may be reduced (86, 138, 152). These observations may be the reason that an improvement in fatty acid oxidation (e.g., with exercise), which allows excess fatty acids to be oxidized away, has so often been associated with improved insulin sensitivity (26, 87, 150). Indeed, exercise training improves fatty acid oxidation not only during exercise (151, 191, 196) but also at rest (65, 188), since under basal conditions there are training-induced increases in mitochondrial carnitine palmitoyl transferase I activity, resulting in an increased rate of fatty acid oxidation by isolated mitochondria under basal conditions (27). A comparable effect could well be provoked by PGC-1α since, similarly to exercise training, PGC-1α induces mitochondrial biogenesis and fatty acid oxidation (cf. Ref. 73 and 113), thereby integrating the upregulation in fatty acid oxidation with improvements in insulin sensitivity.
Whether fatty acids regulate PGC-1α expression in muscle has been controversial. Palmitate (0.75 mM), but not oleate, reduced PGC-1α mRNA by 66% in C2C12 muscle cells and appeared to involve MAPK-ERK 1/2 and nuclear factor-κβ activation (44). Similarly, in humans, prolonged (48 h) lipid infusion increased circulating fatty acids 3.6-fold (0.48–1.73 mM) and reduced muscle PGC-1α mRNA by 30% (164). In contrast, prolonged fasting for 24 or 48 h, which increased circulating fatty acids 1.6- and 2.1-fold, respectively, did not alter muscle PGC-1α mRNA or protein (206). Contradictory results have also been observed when circulating fatty acids were reduced by acipimox (12) or nicotinic acid (214), since these treatments reduced (12) or increased PGC-1α mRNA (214), respectively. Taken altogether, it is difficult to conclude that fatty acids influence the expression of PGC-1α.
Type 2 Diabetes and PGC-1α
Given 1) the linkage between the dysregulation in fatty acid metabolism and impairment in insulin sensitivity and 2) that PGC-1α induces mitochondrial biogenesis (cf. Ref. 73) and the expression of key enzymes involved in skeletal muscle fatty acid utilization (for review, see Refs. 16, 73, and 113), it was of considerable interest to examine whether PGC-1α expression was altered in type 2 diabetes.
Oxidative phosphorylation genes and PGC-1α are reduced in type 2 diabetes.
Based on multiple statistical comparisons of high-density oligonucleotide arrays and quantitative real-time PCR, it has been concluded that differences in muscle gene expression between type 2 diabetes patients and healthy humans are quite modest (i.e., ≤34% reduction in type 2 diabetes), involving only a small number of selected genes in fatty acid transport and metabolism and oxidative phosphorylation (OXPHOS) (137, 148). Concurrently, PGC-1α mRNA expression was also reduced modestly (20–36%) in muscles of type 2 diabetes patients (137, 148) as well as in asymptomatic individuals with a family history of type 2 diabetes (−34%) (148). Reductions in PGC-1α have also been observed when fasting insulin concentrations are increased and with an increased body mass index in diabetes-prone humans (8, 155). Thus, there appears to be a potential role for PGC-1α in the etiology of insulin resistance in human skeletal muscle. This linkage is strengthened by the fact that 1) PGC-1α is also downregulated in selected animal models of insulin resistance and type 2 diabetes (99, 189), 2) PGC-1α is known to regulate genes involved in lipid metabolism and OXPHOS (cf. Ref. 16, 73, and 113), and 3) PGC-1α transfection in a mouse skeletal muscle cell line upregulated almost precisely a subset of OXPHOS genes that were downregulated in muscles of type 2 diabetes patients (137). Importantly, in type 2 diabetes, the reductions in the expression of skeletal muscle PGC-1α and its associated OXPHOS genes were quite modest (≤34%) (137, 148). This suggests that a modest increase in PGC-1α may be sufficient to improve insulin sensitivity.
Does the reduction in PGC-1α in type 2 diabetes reflect reduced muscle activity?
To date, little recognition has been given to the fact that reductions in PGC-1α and its associated OXPHOS genes could be spuriously associated with type 2 diabetes. Individuals with type 2 diabetes have low levels of physical activity (76, 180), and PGC-1α and OXPHOS genes are downregulated, when physical activity is reduced (59, 172, 204). Indeed, there is a highly significant positive relationship between maximal aerobic capacity (V̇o2max; an index of low physical activity) and the expression of OXPHOS genes among individuals with type 2 diabetes and those with normal and impaired glucose tolerance (137). Close inspection of these data revealed that individuals with type 2 diabetes had a 25% lower V̇o2max and were clustered in the lowest third of the correlational analysis (OXPHOS vs. V̇o2max). Others have shown that PGC-1α mRNA and its associated genes are positively correlated with V̇o2max (59) and that “diabetes-like” reductions in PGC-1α mRNA are induced by muscle inactivity (204). Thus, it is unclear to what extent the observed reductions in skeletal muscle PGC-1α mRNA and its associated OXPHOS genes in type 2 diabetes (137, 148) are 1) the result of type 2 diabetes per se or 2) due to reduced physical activity patterns in individuals with type 2 diabetes.
Effects of PGC-1α on Glucose Utilization and Lipid Metabolism
Experimental studies to examine the role of PGC-1α in insulin sensitivity have been conducted in cell lines and in PGC-1α-KO and -overexpressing mice. In general, these studies, except for a report in muscle cells (132), have yielded unexpected results (Table 2).
Table 2.
Comparison of glucose and lipid metabolism responses in different models of PGC-1α ablation and overexpression
| PGC-1α-Null |
Large (600–2,000%) PGC-1α Overexpression |
Modest (25%) Muscle-Specific PGC-1α Overexpression |
||||
|---|---|---|---|---|---|---|
| Metabolic Parameter | Whole body, Refs. 111, 117* | Muscle specific, Ref. 71** | Whole body (1,000–2,000%), Refs. 109, 133 | Muscle specific (600%), Ref. 39 | Healthy muscle (25%), Ref. 15 | Zucker obese muscle (25%), Ref. 14 |
| Glucose metabolism | ||||||
| Insulin sensitivity | †Improveda | No difference | †Reduced | †Reduceda | ||
| Glucose tolerance | †Improveda | †Intoleranta | †Intolerant | |||
| Peripheral glucose flux | Improved | †Reduceda | ||||
| Muscle glucose transport | †Reduceda | √Increased | √Increased | |||
| Protein expression | ||||||
| Muscle GLUT4 | √Reduced | †Reduced | √Increased | √Increased | ||
| Muscle IRS-1 | No difference | |||||
| Muscle PI 3-kinase | No difference | |||||
| Muscle Akt2 protein | No difference | No difference | ||||
| Muscle AS160 protein | No difference | No difference | ||||
| Insulin signaling | ||||||
| Muscle p-IRS-1 | No difference | Reduced | ||||
| Muscle p-Akt or activity | Increased | Increased | Increased | Increased | ||
| Muscle p-AS160 | Increased | Increased | ||||
| Lipid metabolism | ||||||
| Fatty acid oxidation | Increased | √Increasedc | √Increasedc | |||
| Intramuscular lipids | †No difference | †Increased | √Decreased | √Decreased | ||
| Lipid metabolism gene | ||||||
| AMPKα2 protein | Increased | |||||
| p-AMPKα2 or activity | No difference | |||||
| CD36 mRNA/protein | √Large increasec | √Increased | √Increased | |||
| CPT I mRNA, protein or activity | √Increasedc | √Increasedd,e, | √Increasede | |||
| ACC2 protein | √Increased | |||||
| mtGPAT mRNA | Increased | |||||
| DGAT1 mRNA | Increased | |||||
| Diet-induced obesity | †No (Ref. 117) | †No | †Severely (Ref.109) | No difference | ||
| √Yes (Ref. 111)*** | ||||||
| Fat mass | †Reduced | No difference | ||||
IRS-1, insulin receptor substrate-1; PI, phosphatidylinositol; ACC2, acetyl-CoA carboxylase-2; mtGPAT, mitochondrial glycerol-3-phosphate acyltransferase-1; DGAT1, diacylglycerol acyltransferase 1. Comparisons are relative to wild-type mice or muscles not transfected with PGC-1α.
Response observed is the expected response in the PGC-1α model.
Response observed is contrary to the expected response in the PGC-1α model.
PGC-1α-null mice in Ref. 117 are hyperactive and exhibit neurological disorders characteristic of Huntington's disease.
PGC-1α muscle-specific null mice in Ref. 71 are hypoactive.
Results are observed primarily in female mice.
Observations after a period of high-fat feeding;
fatty acid oxidation was improved in subsarcolemma mitochondria only, not in intramyofibrillar mitochondria;
mRNA;
protein;
activity.
Cell lines.
In L6 and C2C12 myotubes, but not in the COS-1 kidney epithelial cell line, PGC-1α overexpression increased insulin-stimulated glucose transport largely via an increase in GLUT4 expression through a PGC-1α and MEF2C interaction at the promoter of GLUT4 (132). This study forged the notion that PGC-1α can have insulin-sensitizing effects.
PGC-1α-null mice.
Two models of PGC-1α-null mice have been created (111, 117). In one model the expression of selected mitochondrial genes was reduced by 20–50% (117), but surprisingly, the animals were hyperactive, possibly accounting for their unexpected lean phenotype (6, 117). Other PGC-1α-null mice were not hyperactive (111) and exhibited most of the expected metabolic changes, including 1) abnormally increased body fat (only in female mice), 2) diminished mitochondrial number and respiratory capacity of soleus muscle, 3) reduced muscle performance and exercise capacity, and 4) short-term, starvation-induced hepatic steatosis (111). Yet, contrary to the expectation that the PGC-1α-null mice were susceptible to insulin resistance, both models were resistant to diet-induced obesity (111, 117).
Muscle-specific PGC-1α-null mice.
Muscle-specific PGC-1α-KO mice exhibited the expected reductions in selected mitochondrial genes (73). Moreover, the animals were hypoactive and exercise intolerant (70, 73). PGC-1α ablation provoked a reduction in GLUT4 mRNA, yet surprisingly, peripheral (i.e., muscle) insulin sensitivity and Akt activity were increased (71).
PGC-1α-overexpressing mice.
In PGC-1α-transgenic mice there was the expected increase in selected mitochondrial genes, a robust increase in mitochondrial proliferation in muscle (116) and heart (109, 173), and a resistance to muscle fatigue (116). However, anomalies were also reported, including the loss of cardiac sarcomeric structure due to excess mitochondria (109, 173). Moreover, whereas a lean phenotype was expected, these animals were severely obese (109). In addition, neither the expected increase in GLUT4 expression nor the expected increase in insulin-stimulated glucose transport was observed. Instead, a >10-fold increase in PGC-1α mRNA unexpectedly reduced GLUT4 mRNA and whole body insulin sensitivity (133).
Muscle-specific PGC-1α overexpression.
Limiting PGC-1α overexpression to skeletal muscle also induced deleterious effects. These muscle-specific PGC-1α-overexpressing mice were not protected from diet-induced insulin resistance as had been expected. Instead, these mice developed insulin resistance when provided with a high-fat diet (39). This was attributed to reduced peripheral (muscle) insulin sensitivity (−25%) and impaired muscle insulin-stimulated glucose transport, insulin receptor substrate-1 (IRS-1) phosphorylation, and Akt2 activity (39). Concurrently, there were increases in selected genes regulating lipid metabolism as well as in functional measurements of muscle fatty acid metabolism, including fatty acid oxidation (+30%), and 200–300% increases in intramuscular lipids (triacylglycerol, diacylglycerol, lysophosphatidic acid, long-chain fatty acyl-CoA) (39), which have been implicated in interfering with insulin signaling.
Are PGC-1α-Null and -Transgenic Animals Suitable for Revealing PGC-1α Insulin-Sensitizing Effects In Vivo?
Based on the foregoing studies with PGC-1α ablation or overexpression, it appears that 1) PGC-1α does not contribute to regulating insulin sensitivity. However, this contrasts with 2) experiments in muscle cells in which GLUT4 and insulin signaling were increased by PGC-1α (132) and 3) gene array data in human type 2 diabetes (137, 148) in which reductions in muscle PGC-1α expression have been interpreted as evidence that PGC-1α has a role in regulating insulin sensitivity. Taken altogether these observations may suggest that 1) the associative evidence between reductions in PGC-1α and type 2 diabetes in humans cannot be interpreted causally or, 2) alternatively, the use of genetic approaches, rather than physiological/metabolic considerations, for examining the insulin-sensitizing role of PGC-1α in vivo may have inadvertently obscured the positive metabolic effects of this coactivator.
In recent years, genetically altered animal models have proved to be extremely useful to examine the function of specific genes, particularly those with a specific restrictive function dedicated to a single process. However, genes involved in broader metabolic functions and actions in multiple tissues have, not unexpectedly, led to unanticipated results (e.g., various murine PPARγ models) (for review, see Ref. 42). Hence, the appropriateness of PGC-1α-null or -overexpressing animal models to examine insulin sensitivity (39, 71, 109, 111, 117, 133) may be questioned, given the multiple metabolic effects induced by this coactivator among and within tissues.
Viewed from a physiological perspective, it is not entirely surprising that completely ablating or massively overexpressing PGC-1α has consistently provided unexpected results with respect to establishing a role for PGC-1α in improving insulin sensitivity in vivo (Table 2). PGC-1α overexpression by 600–2,000% (39, 133) is physiologically unrealistic, exceeding by five- to 10-fold the changes that can be expected to be induced in muscle by physiological stimuli such as cold exposure (146), acute exercise (200, 223), or exercise training (3, 189, 198). Just as studies with PPARγ animal models have shown that too much of a good thing causes harm (42), this may also apply to PGC-1α. Indeed, there is now ample evidence that a massive PGC-1α overexpression (600–2,000%) (39, 109, 116, 133, 173) can have unexpected pathophysiological consequences.
An Alternative Approach: PGC-1α Overexpression Within Physiological Limits
Since traditional genetic approaches, including insulin sensitivity, may not be suitable for examining the role of PGC-1α in muscle metabolism, another strategy has evolved. This approach aimed to 1) upregulate PGC-1α modestly and 2) mimic physiologically realistic changes in PGC-1α protein expression (i.e., 20–150%) (3, 125, 146, 172, 189, 198, 200, 223).
Overexpressing PGC-1α Within a Physiological Range Improves Lipid Metabolism and Glucose Transport in Healthy and Insulin-Resistant Muscle
When PGC-1α was modestly overexpressed (∼25%) in rat muscle (15), using an electrotransfection approach (17, 40, 144), PGC-1α mRNA (28%) and protein (24%) were modestly upregulated (15). Typically, only 30–40% of the muscle fibers are electrotransfected (15, 17, 26, 40, 144, 178). Hence, PGC-1α upregulation in the transfected muscle fibers was 60–75%, which is within a physiological range. This level of PGC-1α overexpression is accompanied by a visible increase in the capacity for oxidative metabolism, namely, the redder coloration of PGC-1α-transfected muscle [see Fig. 5 in Benton et al. (15)].
The modest or physiological overexpression of PGC-1α induced a number of positive metabolic changes in healthy animals, including improvements in insulin-stimulated glucose transport, mitochrondrial fatty acid oxidation (subsarcolemmal mitchondria only, not intermyofibrillar mitochondria), and mitochondrial density (15). These changes were accompanied by PGC-1α-induced upregulation of some proteins (FAT/CD36, GLUT4, AMPKα2), but not others (plasma membrane-associated fatty acid binding protein, IRS-1, phosphatidylinositol 3-kinase, Akt2, hormone-sensitive lipase), improvements in insulin-stimulated phosphorylation of Akt2, and increased expression of COX IV and FAT/CD36 in isolated mitochondria (15). Similarly, PGC-1α upregulation (20–27%) in insulin-resistant muscles (obese Zucker rats) (14) improved insulin-stimulated glucose transport, reduced intramuscular lipids (triacylglycerol, diacylglycerol, ceramide), increased mitochondrial fatty acid oxidation (subsarcolemmal mitochondria only, not intermyofibrillar mitochondria), and increased expression of FAT/CD36 and GLUT4, but not Akt2 or AS160, although their insulin-stimulated phosphorylation was increased (14). Modest PGC-1α overexpression also protected animals from diet-induced insulin resistance (Bonen A, unpublished data).
For all parameters examined, whether in healthy or insulin-resistant animals, the PGC-1α-induced alterations in selected parameters ranged from 15 to 85%, with most being in the range of 20 to 50%. Although these responses are not large when compared against those that can be induced in transgenic animals, these increases are metabolically meaningful, because in skeletal muscle of type 2 diabetic patients there are only 1) small reductions in PGC-1α (≤36%) (137, 148) and 2) a small number of selected genes involved in fatty acid transport and metabolism and in OXPHOS (≤34%) (137, 148). Moreover, unlike with massive PGC-1α overexpression (Table 2), the changes with modest PGC-1α overexpression in all of the parameters collectively provide a metabolically coordinated response in lipid and carbohydrate metabolism such that insulin sensitivity was improved (Table 2) (14, 15). Thus, experiments based on physiological and metabolic rationales for controlling the overexpression of PGC-1α have demonstrated the insulin-sensitizing effects of this coactivator.
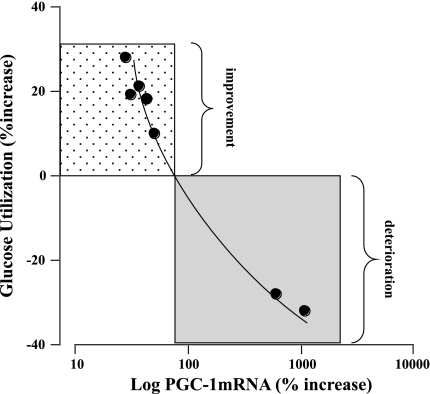
Comparing PGC-1α Overexpression With Improvements in Glucose Utilization
The effects of PGC-1α overexpression on insulin sensitivity in vivo can be strikingly different. When PGC-1α overexpression is within a physiological range (<100%), improvements in insulin sensitivity are observed (Table 2 and Fig. 2). However, when muscle-specific PGC-1α overexpression is far beyond normal physiological limits, insulin-stimulated glucose disposal is impaired (Fig. 2). Although this relationship between PGC-1α overexpression and insulin-stimulated glucose utilization (Fig. 2) does not reflect the complexity of PGC-1α's effects or its mechanisms of action, this relationship (Fig. 2) does provide insight as to when PGC-1α upregulation is likely to be most effective.
Fig. 2.
Comparison between relative changes in PGC-1α overexpression (%) and changes in insulin-stimulated glucose utilization (%) in healthy animals. These data suggest that when PGC-1α expression is more than doubled (i.e., >100% increase), insulin-stimulated glucose utilization deteriorates sufficiently to result in insulin resistance (gray box). In contrast, increasing PGC-1α expression more modestly (<100%) increases insulin sensitivity (dotted box). These contrasting responses may reflect, in part, the differential effects of PGC-1α, depending on its level of overexpression, on intramuscular bioactive lipid accumulation that can interfere with insulin signaling. Data are from Refs. 14, 15, 39, 112, and 133, in which PGC-1α was overexpressed to varying levels in transgenic animals or in electrotransfected muscles. PGC-1α mRNA increase (%) was calculated relative to controls in these studies. Insulin-stimulated glucose utilization was based on various methods, and the increase (%) was calculated relative to controls.
Speculation Concerning Disparate Effects of PGC-1α-Mediated Glucose Utilization
Disparate changes in PGC-1α-mediated glucose utilization may be linked, in part, to the differential PGC-1α-induced upregulation of proteins involved with lipid metabolism. Key among these is the fatty acid transporter FAT/CD36. This PGC-1α-inducible gene (15, 39) has been linked to insulin resistance (21, 23, 62, 83), since it promotes excess uptake of fatty acids beyond the capacity to oxidize them (21, 23, 62, 83). Hence, intramuscular lipids accumulate. Because of this work, we (15, 16) had already suggested several years ago that it may be critically important to limit the PGC-1α-induced overexpression of FAT/CD36, even in the face of PGC-1α-induced improvements in fatty acid oxidation. Indeed, an excessively large PGC-1α overexpression (+600%) induced a large upregulation of FAT/CD36 (+300%) (39), which not unexpectedly increased intramuscular lipids by 200–300% and therefore likely reduced insulin-stimulated glucose transport and activation of insulin-signaling proteins (39). In contrast, modest PGC-1α overexpression only moderately increased FAT/CD36 (20–35%) in muscle (Table 2) (14, 15), an increase that may be expected to improve fatty acid oxidation while not increasing intramuscular lipids (144). Thus, it seems that if PGC-1α is to be a therapeutic target, its upregulation in muscle must be modest, since this limits PGC-1α-induced FAT/CD36 upregulation, thereby preventing excess fatty acid uptake and intramuscular lipid accumulation.
Summary
Multiple signaling transduction pathways, including Ca2+-dependent signaling, ROS, NO, AMPK, and p38 MAPK, have been linked to the regulation of PGC-1α expression and function in skeletal muscle plasticity. Gene deletion studies have demonstrated that the CnA/NFAT signaling controls fiber type transformation, whereas p38γ MAPK/PGC-1α signaling controls mitochondrial biogenesis and angiogenesis in response to endurance exercise in skeletal muscle. The insulin-sensitizing effects of exercise may be mediated, in part, via the exercise-induced upregulation of PGC-1α, since its modest overexpression within an exercise-like range is sufficient to improve both lipid metabolism and insulin sensitivity.
GRANTS
These studies were supported in part by grants from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (RO1-AR-050429 to Z. Yan) and the Natural Sciences and Engineering Research Council of Canada (A. Bonen), the Canadian Institutes of Health Research (A. Bonen), and the Canada Research Chair program (A. Bonen) A. Bonen is the Canada Research Chair in Metabolism and Health.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
REFERENCES
- 1.Adhihetty PJ, Uguccioni G, Leick L, Hidalgo J, Pilegaard H, Hood DA. The role of PGC-1α on mitochondrial function and apoptotic susceptibility in muscle. Am J Physiol Cell Physiol 297: C217–C225, 2009 [DOI] [PubMed] [Google Scholar]
- 2.Akimoto T, Li P, Yan Z. Functional interaction of regulatory factors with the Pgc-1α promoter in response to exercise by in vivo imaging. Am J Physiol Cell Physiol 295: C288–C292, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Akimoto T, Pohnert SC, Li P, Zhang M, Gumbs C, Rosenberg PB, Williams RS, Yan Z. Exercise stimulates Pgc-1alpha transcription in skeletal muscle through activation of the p38 MAPK pathway. J Biol Chem 280: 19587–19593, 2005 [DOI] [PubMed] [Google Scholar]
- 4.Akimoto T, Ribar TJ, Williams RS, Yan Z. Skeletal muscle adaptation in response to voluntary running in Ca2+/calmodulin-dependent protein kinase IV-deficient mice. Am J Physiol Cell Physiol 287: C1311–C1319, 2004 [DOI] [PubMed] [Google Scholar]
- 5.Arany Z, Foo SY, Ma Y, Ruas JL, Bommi-Reddy A, Girnun G, Cooper M, Laznik D, Chinsomboon J, Rangwala SM, Baek KH, Rosenzweig A, Spiegelman BM. HIF-independent regulation of VEGF and angiogenesis by the transcriptional coactivator PGC-1alpha. Nature 451: 1008–1012, 2008 [DOI] [PubMed] [Google Scholar]
- 6.Arany Z, He H, Lin J, Hoyer K, Handschin C, Toka O, Ahmad F, Matsui T, Chin S, Wu PH, Rybkin II, Shelton JM, Manieri M, Cinti S, Schoen FJ, Bassel-Duby R, Rosenzweig A, Ingwall JS, Spiegelman BM. Transcriptional coactivator PGC-1 alpha controls the energy state and contractile function of cardiac muscle. Cell Metab 1: 259–271, 2005 [DOI] [PubMed] [Google Scholar]
- 7.Arany Z, Lebrasseur N, Morris C, Smith E, Yang W, Ma Y, Chin S, Spiegelman BM. The transcriptional coactivator PGC-1beta drives the formation of oxidative type IIX fibers in skeletal muscle. Cell Metab 5: 35–46, 2007 [DOI] [PubMed] [Google Scholar]
- 8.Araya R, Blangero J, Almasy L, O'Connell P, Stern M, Duggirala R. A major locus for body mass index (BMI) on chromosome 4p in Mexican Americans (Abstract). Obes Res 9: 70S, 2001 [Google Scholar]
- 9.Aronson D, Boppart MD, Dufresne SD, Fielding RA, Goodyear LJ. Exercise stimulates c-Jun NH2 kinase activity and c-Jun transcriptional activity in human skeletal muscle. Biochem Biophys Res Commun 251: 106–110, 1998 [DOI] [PubMed] [Google Scholar]
- 10.Aronson D, Violan MA, Dufresne SD, Zangen D, Fielding RA, Goodyear LJ. Exercise stimulates the mitogen-activated protein kinase pathway in human skeletal muscle. J Clin Invest 99: 1251–1257, 1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baar K, Wende AR, Jones TE, Marison M, Nolte LA, Chen M, Kelly DP, Holloszy JO. Adaptations of skeletal muscle to exercise: rapid increase in the transcriptional coactivator PGC-1. FASEB J 16: 1879–1886, 2002 [DOI] [PubMed] [Google Scholar]
- 12.Bajaj M, Medina-Navarro R, Suraamornkul S, Meyer C, DeFronzo RA, Mandarino LJ. Paradoxical changes in muscle gene expression in insulin-resistant subjects after sustained reduction in plasma free fatty acid concentration. Diabetes 56: 743–752, 2007 [DOI] [PubMed] [Google Scholar]
- 13.Balon TW, Nadler JL. Nitric oxide release is present from incubated skeletal muscle preparations. J Appl Physiol 77: 2519–2521, 1994. [DOI] [PubMed] [Google Scholar]
- 14.Benton CR, Holloway GP, Han XX, Yoshida Y, Snook LA, Lally J, Glatz JFC, Luiken JJ, Chabowski A, Bonen A. PGC-1α overexpression improves lipid utilization, insulin signalling, and glucose transport in skeletal muscle of lean and insulin resistant obese Zucker rats. Diabetologia. In press [DOI] [PubMed] [Google Scholar]
- 15.Benton CR, Nickerson JG, Lally J, Han XX, Holloway GP, Glatz JF, Luiken JJ, Graham TE, Heikkila JJ, Bonen A. Modest PGC-1alpha overexpression in muscle in vivo is sufficient to increase insulin sensitivity and palmitate oxidation in subsarcolemmal, not intermyofibrillar, mitochondria. J Biol Chem 283: 4228–4240, 2008 [DOI] [PubMed] [Google Scholar]
- 16.Benton CR, Wright DC, Bonen A. PGC-1alpha-mediated regulation of gene expression and metabolism: implications for nutrition and exercise prescriptions. Appl Physiol Nutr Metab 33: 843–862, 2008 [DOI] [PubMed] [Google Scholar]
- 17.Benton CR, Yoshida Y, Lally J, Han XX, Hatta H, Bonen A. PGC-1α increases skeletal muscle lactate uptake by increasing the expression of MCT1 but not MCT2 or MCT4. Physiol Genomics 35: 45–54, 2008 [DOI] [PubMed] [Google Scholar]
- 18.Boden G. Free fatty acids, insulin resistance, and type 2 diabetes mellitus. Proc Assoc Am Physicians 111: 241–248, 1999 [DOI] [PubMed] [Google Scholar]
- 19.Boden G, Chen X, Iqbal N. Acute lowering of plasma fatty acids lowers basal insulin secretion in diabetic and nondiabetic subjects. Diabetes 47: 1609–1612, 1998 [DOI] [PubMed] [Google Scholar]
- 20.Boden G, Jadali F, White J, Liang Y, Mozzoli M, Chen X, Coleman E, CS Effects of fat on insulin-stimulated carbohydrate metabolism in normal men. J Clin Invest 88: 960–966, 1991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bonen A, Chabowski A, Luiken JJ, Glatz JF. Is membrane transport of FFA mediated by lipid, protein, or both? Mechanisms and regulation of protein-mediated cellular fatty acid uptake: molecular, biochemical, and physiological evidence. Physiology (Bethesda) 22: 15–29, 2007 [DOI] [PubMed] [Google Scholar]
- 22.Bonen A, Dohm GL, van Loon LJ. Lipid metabolism, exercise and insulin action. Essays Biochem 42: 47–59, 2006 [DOI] [PubMed] [Google Scholar]
- 23.Bonen A, Parolin ML, Steinberg GR, Calles-Escandon J, Tandon NN, Glatz JF, Luiken JJ, Heigenhauser GJ, Dyck DJ. Triacylglycerol accumulation in human obesity and type 2 diabetes is associated with increased rates of skeletal muscle fatty acid transport and increased sarcolemmal FAT/CD36. FASEB J 18: 1144–1146, 2004 [DOI] [PubMed] [Google Scholar]
- 24.Bonen A, Tan MH, Watson-Wright WM. Effects of exercise on insulin binding and glucose metabolism in muscle. Can J Physiol Pharmacol 62: 1500–1504, 1984 [DOI] [PubMed] [Google Scholar]
- 25.Bruce CR, Anderson MJ, Carey AL, Newman DG, Bonen A, Kriketos AD, Cooney GJ, Hawley JA. Muscle oxidative capacity is a better predictor of insulin sensitivity than lipid status. J Clin Endocrinol Metab 88: 5444–5451, 2003 [DOI] [PubMed] [Google Scholar]
- 26.Bruce CR, Hoy AJ, Turner N, Watt MJ, Allen TL, Carpenter K, Cooney GJ, Febbraio MA, Kraegen EW. Overexpression of carnitine palmitoyltransferase-1 in skeletal muscle is sufficient to enhance fatty acid oxidation and improve high-fat diet-induced insulin resistance. Diabetes 58: 550–558, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bruce CR, Thrush AB, Mertz VA, Bezaire V, Chabowski A, Heigenhauser GJ, Dyck DJ. Endurance training in obese humans improves glucose tolerance and mitochondrial fatty acid oxidation and alters muscle lipid content. Am J Physiol Endocrinol Metab 291: E99–E107, 2006 [DOI] [PubMed] [Google Scholar]
- 28.Calvo JA, Daniels TG, Wang X, Paul A, Lin J, Spiegelman BM, Stevenson SC, Rangwala SM. Muscle-specific expression of PPARγ coactivator-1α improves exercise performance and increases peak oxygen uptake. J Appl Physiol 104: 1304–1312, 2008 [DOI] [PubMed] [Google Scholar]
- 29.Cantó C, Gerhart-Hines Z, Feige JN, Lagouge M, Noriega L, Milne JC, Elliott PJ, Puigserver P, Auwerx J. AMPK regulates energy expenditure by modulating NAD+ metabolism and SIRT1 activity. Nature 458: 1056–1060, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cantó C, Jiang LQ, Deshmukh AS, Mataki C, Coste A, Lagouge M, Zierath JR, Auwerx J. Interdependence of AMPK and SIRT1 for metabolic adaptation to fasting and exercise in skeletal muscle. Cell Metab 11: 213–219, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cao W, Daniel KW, Robidoux J, Puigserver P, Medvedev AV, Bai X, Floering LM, Spiegelman BM, Collins S. p38 mitogen-activated protein kinase is the central regulator of cyclic AMP-dependent transcription of the brown fat uncoupling protein 1 gene. Mol Cell Biol 24: 3057–3067, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chavez JA, Holland WL, Bar J, Sandhoff K, Summers SA. Acid ceramidase overexpression prevents the inhibitory effects of saturated fatty acids on insulin signaling. J Biol Chem 280: 20148–20153, 2005 [DOI] [PubMed] [Google Scholar]
- 33.Chavez JA, Knotts TA, Wang LP, Li G, Dobrowsky RT, Florant GL, Summers SA. A role for ceramide, but not diacylglycerol, in the antagonism of insulin signal transduction by saturated fatty acids. J Biol Chem 278: 10297–10303, 2003 [DOI] [PubMed] [Google Scholar]
- 34.Chen ZP, McConell GK, Michell BJ, Snow RJ, Canny BJ, Kemp BE. AMPK signaling in contracting human skeletal muscle: acetyl-CoA carboxylase and NO synthase phosphorylation. Am J Physiol Endocrinol Metab 279: E1202–E1206, 2000 [DOI] [PubMed] [Google Scholar]
- 35.Chen ZP, Mitchelhill KI, Michell BJ, Stapleton D, Rodriguez-Crespo I, Witters LA, Power DA, Ortiz de Montellano PR, Kemp BE. AMP-activated protein kinase phosphorylation of endothelial NO synthase. FEBS Lett 443: 285–289, 1999 [DOI] [PubMed] [Google Scholar]
- 36.Chin ER. The role of calcium and calcium/calmodulin-dependent kinases in skeletal muscle plasticity and mitochondrial biogenesis. Proc Nutr Soc 63: 279–286, 2004 [DOI] [PubMed] [Google Scholar]
- 37.Chin ER, Olson EN, Richardson JA, Yang Q, Humphries C, Shelton JM, Wu H, Zhu W, Bassel-Duby R, Williams RS. A calcineurin-dependent transcriptional pathway controls skeletal muscle fiber type. Genes Dev 12: 2499–2509, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chinsomboon J, Ruas J, Gupta RK, Thom R, Shoag J, Rowe GC, Sawada N, Raghuram S, Arany Z. The transcriptional coactivator PGC-1alpha mediates exercise-induced angiogenesis in skeletal muscle. Proc Natl Acad Sci USA 106: 21401–21406, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Choi CS, Befroy DE, Codella R, Kim S, Reznick RM, Hwang YJ, Liu ZX, Lee HY, Distefano A, Samuel VT, Zhang D, Cline GW, Handschin C, Lin J, Petersen KF, Spiegelman BM, Shulman GI. Paradoxical effects of increased expression of PGC-1alpha on muscle mitochondrial function and insulin-stimulated muscle glucose metabolism. Proc Natl Acad Sci USA 105: 19926–19931, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Clarke DC, Miskovic D, Han XX, Calles-Escandon J, Glatz JF, Luiken JJ, Heikkila JJ, Bonen A. Overexpression of membrane-associated fatty acid binding protein (FABPpm) in vivo increases fatty acid sarcolemmal transport and metabolism. Physiol Genomics 17: 31–37, 2004 [DOI] [PubMed] [Google Scholar]
- 41.Close GL, Ashton T, McArdle A, Jackson MJ. Microdialysis studies of extracellular reactive oxygen species in skeletal muscle: factors influencing the reduction of cytochrome c and hydroxylation of salicylate. Free Radic Biol Med 39: 1460–1467, 2005 [DOI] [PubMed] [Google Scholar]
- 42.Cock TA, Houten SM, Auwerx J. Peroxisome proliferator-activated receptor-gamma: too much of a good thing causes harm. EMBO Rep 5: 142–147, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Coggan AR, Spina RJ, King DS, Rogers MA, Brown M, Nemeth PM, Holloszy JO. Skeletal muscle adaptations to endurance training in 60- to 70-yr-old men and women. J Appl Physiol 72: 1780–1786, 1992 [DOI] [PubMed] [Google Scholar]
- 44.Coll T, Jové M, Rodríguez-Calvo R, Eyre E, Palomer X, Sánchez RM, Merlos M, Laguna JC, Vázquez-Carrera M. Palmitate-mediated downregulation of peroxisome proliferator-activated receptor-gamma coactivator 1alpha in skeletal muscle cells involves MEK1/2 and nuclear factor-kappaB activation. Diabetes 55: 2779–2787, 2006 [DOI] [PubMed] [Google Scholar]
- 45.Costford SR, Bajpeyi S, Pasarica M, Albarado DC, Thomas SC, Xie H, Church TS, Jubrias SA, Conley KE, Smith SR. Skeletal muscle NAMPT is induced by exercise in humans. Am J Physiol Endocrinol Metab 298: E117–E126, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Czubryt MP, McAnally J, Fishman GI, Olson EN. Regulation of peroxisome proliferator-activated receptor gamma coactivator 1 alpha (PGC-1 alpha) and mitochondrial function by MEF2 and HDAC5. Proc Natl Acad Sci USA 100: 1711–1716, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Davis BJ, Xie Z, Viollet B, Zou MH. Activation of the AMP-activated kinase by antidiabetes drug metformin stimulates nitric oxide synthesis in vivo by promoting the association of heat shock protein 90 and endothelial nitric oxide synthase. Diabetes 55: 496–505, 2006 [DOI] [PubMed] [Google Scholar]
- 48.DeFronzo RA, Ferrannini E, Sato Y, Felig P, Wahren J. Synergistic interaction between exercise and insulin on peripheral glucose uptake. J Clin Invest 68: 1468–1474, 1981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.DeFronzo RA, Jacot E, Jequier E, Maeder E, Wahren J, Felber JP. The effect of insulin on the disposal of intravenous glucose. Results from indirect calorimetry and hepatic and femoral venous catheterization. Diabetes 30: 1000–1007, 1981 [DOI] [PubMed] [Google Scholar]
- 50.Devlin JT, Hirshman MS, Horton ED, Horton ES. Enhanced peripheral and splanchic insulin sensitivity in NIDDM men after a single bout of exercise. Diabetes 36: 434–439, 1987 [DOI] [PubMed] [Google Scholar]
- 51.Drenning JA, Lira VA, Simmons CG, Soltow QA, Sellman JE, Criswell DS. Nitric oxide facilitates NFAT-dependent transcription in mouse myotubes. Am J Physiol Cell Physiol 294: C1088–C1095, 2008 [DOI] [PubMed] [Google Scholar]
- 52.Drenning JA, Lira VA, Soltow QA, Canon CN, Valera LM, Brown DL, Criswell DS. Endothelial nitric oxide synthase is involved in calcium-induced Akt signaling in mouse skeletal muscle. Nitric Oxide 21: 192–200, 2009 [DOI] [PubMed] [Google Scholar]
- 53.Eddinger TJ, Moss RL. Mechanical properties of skinned single fibers of identified types from rat diaphragm. Am J Physiol Cell Physiol 253: C210–C218, 1987 [DOI] [PubMed] [Google Scholar]
- 54.Ennion S, Sant'ana Pereira J, Sargeant AJ, Young A, Goldspink G. Characterization of human skeletal muscle fibres according to the myosin heavy chains they express. J Muscle Res Cell Motil 16: 35–43, 1995 [DOI] [PubMed] [Google Scholar]
- 55.Fujii N, Hayashi T, Hirshman MF, Smith JT, Habinowski SA, Kaijser L, Mu J, Ljungqvist O, Birnbaum MJ, Witters LA, Thorell A, Goodyear LJ. Exercise induces isoform-specific increase in 5′AMP-activated protein kinase activity in human skeletal muscle. Biochem Biophys Res Commun 273: 1150–1155, 2000 [DOI] [PubMed] [Google Scholar]
- 56.Fulco M, Sartorelli V. Comparing and contrasting the roles of AMPK and SIRT1 in metabolic tissues. Cell Cycle 7: 3669–3679, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Garcia-Roves PM, Huss J, Holloszy JO. Role of calcineurin in exercise-induced mitochondrial biogenesis. Am J Physiol Endocrinol Metab 290: E1172–E1179, 2006 [DOI] [PubMed] [Google Scholar]
- 58.Garcia-Roves PM, Osler ME, Holmstrom MH, Zierath JR. Gain-of-function R225Q mutation in AMP-activated protein kinase gamma3 subunit increases mitochondrial biogenesis in glycolytic skeletal muscle. J Biol Chem 283: 35724–35734, 2008 [DOI] [PubMed] [Google Scholar]
- 59.Garnier A, Fortin D, Zoll J, N'Guessan B, Mettauer B, Lampert E, Veksler V, Ventura-Clapier R. Coordinated changes in mitochondrial function and biogenesis in healthy and diseased human skeletal muscle. FASEB J 19: 43–52, 2005 [DOI] [PubMed] [Google Scholar]
- 60.Gaster M, Staehr P, Beck-Nielsen H, Schroder HD, Handberg A. GLUT4 is reduced in slow muscle fibers of type 2 diabetic patients: is insulin resistance in type 2 diabetes a slow, type 1 fiber disease? Diabetes 50: 1324–1329, 2001 [DOI] [PubMed] [Google Scholar]
- 61.Geng T, Li P, Okutsu M, Yin X, Kwek J, Zhang M, Yan Z. PGC-1α plays a functional role in exercise-induced mitochondrial biogenesis and angiogenesis but not fiber-type transformation in mouse skeletal muscle. Am J Physiol Cell Physiol 298: C572–C579, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Glatz JF, Luiken JJ, Bonen A. Membrane fatty acid transporters as regulators of lipid metabolism: implications for metabolic disease. Physiol Rev 90: 367–417, 2010 [DOI] [PubMed] [Google Scholar]
- 63.Gomez-Cabrera MC, Domenech E, Romagnoli M, Arduini A, Borras C, Pallardo FV, Sastre J, Viña J. Oral administration of vitamin C decreases muscle mitochondrial biogenesis and hampers training-induced adaptations in endurance performance. Am J Clin Nutr 87: 142–149, 2008 [DOI] [PubMed] [Google Scholar]
- 64.Goodpaster BH, Brown NF. Skeletal muscle lipid and its association with insulin resistance: what is the role for exercise? Exerc Sport Sci Rev 33: 150–154, 2005 [DOI] [PubMed] [Google Scholar]
- 65.Goodpaster BH, Katsiaras A, Kelley DE. Enhanced fat oxidation through physical activity is associated with improvements in insulin sensitivity in obesity. Diabetes 52: 2191–2197, 2003 [DOI] [PubMed] [Google Scholar]
- 66.Goodyear LJ, Chang PY, Sherwood DJ, Dufresne SD, Moller DE. Effects of exercise and insulin on mitogen-activated protein kinase signaling pathways in rat skeletal muscle. Am J Physiol Endocrinol Metab 271: E403–E408, 1996 [DOI] [PubMed] [Google Scholar]
- 67.Goto M, Terada S, Kato M, Katoh M, Yokozeki T, Tabata I, Shimokawa T. cDNA cloning and mRNA analysis of PGC-1 in epitrochlearis muscle in swimming exercised rats. Biochem Biophys Res Commun 274: 350–354, 2000 [DOI] [PubMed] [Google Scholar]
- 68.Hancock CR, Han DH, Chen M, Terada S, Yasuda T, Wright DC, Holloszy JO. High-fat diets cause insulin resistance despite an increase in muscle mitochondria. Proc Natl Acad Sci USA 105: 7815–7820, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hancock CR, Janssen E, Terjung RL. Contraction-mediated phosphorylation of AMPK is lower in skeletal muscle of adenylate kinase-deficient mice. J Appl Physiol 100: 406–413, 2006 [DOI] [PubMed] [Google Scholar]
- 70.Handschin C, Chin S, Li P, Liu F, Maratos-Flier E, Lebrasseur NK, Yan Z, Spiegelman BM. Skeletal muscle fiber-type switching, exercise intolerance, and myopathy in PGC-1alpha muscle-specific knock-out animals. J Biol Chem 282: 30014–30021, 2007 [DOI] [PubMed] [Google Scholar]
- 71.Handschin C, Choi CS, Chin S, Kim S, Kawamori D, Kurpad AJ, Neubauer N, Hu J, Mootha VK, Kim YB, Kulkarni RN, Shulman GI, Spiegelman BM. Abnormal glucose homeostasis in skeletal muscle-specific PGC-1alpha knockout mice reveals skeletal muscle-pancreatic beta cell crosstalk. J Clin Invest 117: 3463–3474, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Handschin C, Rhee J, Lin J, Tarr PT, Spiegelman BM. An autoregulatory loop controls peroxisome proliferator-activated receptor gamma coactivator 1alpha expression in muscle. Proc Natl Acad Sci USA 100: 7111–7116, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Handschin C, Spiegelman BM. Peroxisome proliferator-activated receptor gamma coactivator 1 coactivators, energy homeostasis, and metabolism. Endocr Rev 27: 728–735, 2006 [DOI] [PubMed] [Google Scholar]
- 74.Hardie DG. Minireview: the AMP-activated protein kinase cascade: the key sensor of cellular energy status. Endocrinology 144: 5179–5183, 2003 [DOI] [PubMed] [Google Scholar]
- 75.Hashimoto T, Hussien R, Oommen S, Gohil K, Brooks GA. Lactate sensitive transcription factor network in L6 cells: activation of MCT1 and mitochondrial biogenesis. FASEB J 21: 2602–2612, 2007 [DOI] [PubMed] [Google Scholar]
- 76.Hays LM, Clark DO. Correlates of physical activity in a sample of older adults with type 2 diabetes. Diabetes Care 22: 706–712, 1999 [DOI] [PubMed] [Google Scholar]
- 77.Heath GW, Gavin JR, Hinderliter JM, Hagberg JM, Bloomfield SA, Holloszy JO. Effects of exercise and lack of exercise on glucose tolerance and insulin sensitivity. J Appl Physiol 55: 512–517, 1983 [DOI] [PubMed] [Google Scholar]
- 78.Henriksen EJ. Invited review: Effects of acute exercise and exercise training on insulin resistance. J Appl Physiol 93: 788–796, 2002 [DOI] [PubMed] [Google Scholar]
- 79.Henriksen EJ, Bourey RE, Rodnick KJ, Koranyi L, Permutt MA, Holloszy JO. Glucose transporter protein content and glucose transport capacity in rat skeletal muscles. Am J Physiol Endocrinol Metab 259: E593–E598, 1990 [DOI] [PubMed] [Google Scholar]
- 80.Holland WL, Brozinick JT, Wang LP, Hawkins ED, Sargent KM, Liu Y, Narra K, Hoehn KL, Knotts TA, Siesky A, Nelson DH, Karathanasis SK, Fontenot GK, Birnbaum MJ, Summers SA. Inhibition of ceramide synthesis ameliorates glucocorticoid-, saturated-fat-, and obesity-induced insulin resistance. Cell Metab 5: 167–179, 2007 [DOI] [PubMed] [Google Scholar]
- 81.Holland WL, Knotts TA, Chavez JA, Wang LP, Hoehn KL, Summers SA. Lipid mediators of insulin resistance. Nutr Rev 65: S39–S46, 2007 [DOI] [PubMed] [Google Scholar]
- 82.Holloszy JO. Biochemical adaptations in muscle. Effects of exercise on mitochondrial oxygen uptake and respiratory enzyme activity in skeletal muscle. J Biol Chem 242: 2278–2282, 1967 [PubMed] [Google Scholar]
- 83.Holloway GP, Benton CR, Mullen KL, Yoshida Y, Snook LA, Han XX, Glatz JF, Luiken JJ, Lally J, Dyck DJ, Bonen A. In obese rat muscle transport of palmitate is increased and is channeled to triacylglycerol storage despite an increase in mitochondrial palmitate oxidation. Am J Physiol Endocrinol Metab 296: E738–E747, 2009 [DOI] [PubMed] [Google Scholar]
- 84.Holloway GP, Bonen A, Spriet LL. Regulation of skeletal muscle mitochondrial fatty acid metabolism in lean and obese individuals. Am J Clin Nutr 89: 455S–462S, 2009 [DOI] [PubMed] [Google Scholar]
- 85.Holloway GP, Perry CG, Thrush AB, Heigenhauser GJ, Dyck DJ, Bonen A, Spriet LL. PGC-1α's relationship with skeletal muscle palmitate oxidation is not present with obesity despite maintained PGC-1α and PGC-1β protein. Am J Physiol Endocrinol Metab 294: E1060–E1069, 2008 [DOI] [PubMed] [Google Scholar]
- 86.Holloway GP, Thrush AB, Heigenhauser GJ, Tandon NN, Dyck DJ, Bonen A, Spriet LL. Skeletal muscle mitochondrial FAT/CD36 content and palmitate oxidation are not decreased in obese women. Am J Physiol Endocrinol Metab 292: E1782–E1789, 2007 [DOI] [PubMed] [Google Scholar]
- 87.Houmard JA. Intramuscular lipid oxidation and obesity. Am J Physiol Regul Integr Comp Physiol 294: R1111–R1116, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Huss JM, Kopp RP, Kelly DP. Peroxisome proliferator-activated receptor coactivator-1alpha (PGC-1alpha) coactivates the cardiac-enriched nuclear receptors estrogen-related receptor-alpha and -gamma. Identification of novel leucine-rich interaction motif within PGC-1alpha. J Biol Chem 277: 40265–40274, 2002 [DOI] [PubMed] [Google Scholar]
- 89.Huss JM, Torra IP, Staels B, Giguere V, Kelly DP. Estrogen-related receptor alpha directs peroxisome proliferator-activated receptor alpha signaling in the transcriptional control of energy metabolism in cardiac and skeletal muscle. Mol Cell Biol 24: 9079–9091, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Irrcher I, Adhihetty PJ, Sheehan T, Joseph AM, Hood DA. PPARγ coactivator-1α expression during thyroid hormone- and contractile activity-induced mitochondrial adaptations. Am J Physiol Cell Physiol 284: C1669–C1677, 2003 [DOI] [PubMed] [Google Scholar]
- 91.Irrcher I, Ljubicic V, Hood DA. Interactions between ROS and AMP kinase activity in the regulation of PGC-1α transcription in skeletal muscle cells. Am J Physiol Cell Physiol 296: C116–C123, 2009 [DOI] [PubMed] [Google Scholar]
- 92.Irrcher I, Ljubicic V, Kirwan AF, Hood DA. AMP-activated protein kinase-regulated activation of the PGC-1alpha promoter in skeletal muscle cells. PLoS One 3: e3614, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Jäger S, Handschin C, St-Pierre J, Spiegelman BM. AMP-activated protein kinase (AMPK) action in skeletal muscle via direct phosphorylation of PGC-1alpha. Proc Natl Acad Sci USA 104: 12017–12022, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Jenkins AB, Storlein LH, Chisholm DJ, Kraegen EW. Effects of nonesterified fatty acid availability on tissue-specific glucose utilization in rats in vivo. J Clin Invest 82: 293–299, 1988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Jenkins AB, Storlien LH, Cooney GJ, Denyer GS, Caterson ID, Kraegen EW. Effects of blockade of fatty acid oxidation on whole body and tissue-specific glucose metabolism in rats. Am J Physiol Endocrinol Metab 265: E592–E600, 1993 [DOI] [PubMed] [Google Scholar]
- 96.Jensen TE, Rose AJ, Jørgensen SB, Brandt N, Schjerling P, Wojtaszewski JF, Richter EA. Possible CaMKK-dependent regulation of AMPK phosphorylation and glucose uptake at the onset of mild tetanic skeletal muscle contraction. Am J Physiol Endocrinol Metab 292: E1308–E1317, 2007 [DOI] [PubMed] [Google Scholar]
- 97.Jiang LQ, Garcia-Roves PM, de Castro Barbosa T, Zierath JR. Constitutively active calcineurin in skeletal muscle increases endurance performance and mitochondrial respiratory capacity. Am J Physiol Endocrinol Metab 298: E8–E16, 2010 [DOI] [PubMed] [Google Scholar]
- 98.Jørgensen SB, Wojtaszewski JF, Viollet B, Andreelli F, Birk JB, Hellsten Y, Schjerling P, Vaulont S, Neufer PD, Richter EA, Pilegaard H. Effects of alpha-AMPK knockout on exercise-induced gene activation in mouse skeletal muscle. FASEB J 19: 1146–1148, 2005 [DOI] [PubMed] [Google Scholar]
- 99.Jové M, Salla J, Planavila A, Cabrero A, Michalik L, Wahli W, Laguna JC, Vázquez-Carrera M. Impaired expression of NADH dehydrogenase subunit 1 and PPARgamma coactivator-1 in skeletal muscle of ZDF rats: restoration by troglitazone. J Lipid Res 45: 113–123, 2004 [DOI] [PubMed] [Google Scholar]
- 100.Kamei Y, Ohizumi H, Fujitani Y, Nemoto T, Tanaka T, Takahashi N, Kawada T, Miyoshi M, Ezaki O, Kakizuka A. PPARgamma coactivator 1beta/ERR ligand 1 is an ERR protein ligand, whose expression induces a high-energy expenditure and antagonizes obesity. Proc Natl Acad Sci USA 100: 12378–12383, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kang C, O'Moore KM, Dickman JR, Ji LL. Exercise activation of muscle peroxisome proliferator-activated receptor-gamma coactivator-1alpha signaling is redox sensitive. Free Radic Biol Med 47: 1394–1400, 2009 [DOI] [PubMed] [Google Scholar]
- 102.Katz LD, Glickman MG, Rapoport S, Ferrannini E, DeFronzo RA. Splanchnic and peripheral disposal of oral glucose in man. Diabetes 32: 675–679, 1983 [DOI] [PubMed] [Google Scholar]
- 103.Kelley DE, He J, Menshikova EV, Ritov VB. Dysfunction of mitochondria in human skeletal muscle in type 2 diabetes. Diabetes 51: 2944–2950, 2002 [DOI] [PubMed] [Google Scholar]
- 104.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 346: 393–403, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Koves TR, Li P, An J, Akimoto T, Slentz D, Ilkayeva O, Dohm GL, Yan Z, Newgard CB, Muoio DM. Peroxisome proliferator-activated receptor-gamma co-activator 1alpha-mediated metabolic remodeling of skeletal myocytes mimics exercise training and reverses lipid-induced mitochondrial inefficiency. J Biol Chem 280: 33588–33598, 2005 [DOI] [PubMed] [Google Scholar]
- 106.Koves TR, Ussher JR, Noland RC, Slentz D, Mosedale M, Ilkayeva O, Bain J, Stevens R, Dyck JR, Newgard CB, Lopaschuk GD, Muoio DM. Mitochondrial overload and incomplete fatty acid oxidation contribute to skeletal muscle insulin resistance. Cell Metab 7: 45–56, 2008 [DOI] [PubMed] [Google Scholar]
- 107.Koyama K, Chen G, Lee Y, Unger RH. Tissue tryglycerides, insulin resistance, and insulin production: implications for hyperinsulinemia of obesity. Am J Physiol Endocrinol Metab 273: E708–E713, 1997 [DOI] [PubMed] [Google Scholar]
- 108.Kressler D, Schreiber SN, Knutti D, Kralli A. The PGC-1-related protein PERC is a selective coactivator of estrogen receptor alpha. J Biol Chem 277: 13918–13925, 2002 [DOI] [PubMed] [Google Scholar]
- 109.Lehman JJ, Barger PM, Kovacs A, Saffitz JE, Medeiros DM, Kelly DP. Peroxisome proliferator-activated receptor γ coactivator-1 promotes cardiac mitochondrial biogenesis. J Clin Invest 106: 847–856, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Leick L, Wojtaszewski JF, Johansen ST, Kiilerich K, Comes G, Hellsten Y, Hidalgo J, Pilegaard H. PGC-1α is not mandatory for exercise- and training-induced adaptive gene responses in mouse skeletal muscle. Am J Physiol Endocrinol Metab 294: E463–E474, 2008 [DOI] [PubMed] [Google Scholar]
- 111.Leone TC, Lehman JJ, Finck BN, Schaeffer PJ, Wende AR, Boudina S, Courtois M, Wozniak DF, Sambandam N, Bernal-Mizrachi C, Chen Z, Holloszy JO, Medeiros DM, Schmidt RE, Saffitz JE, Abel ED, Semenkovich CF, Kelly DP. PGC-1alpha deficiency causes multi-system energy metabolic derangements: muscle dysfunction, abnormal weight control and hepatic steatosis. PLoS Biol 3: e101, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Liang H, Balas B, Tantiwong P, Dube J, Goodpaster BH, O'Doherty RM, Defronzo RA, Richardson A, Musi N, Ward WF. Whole body overexpression of PGC-1α has opposite effects on hepatic and muscle insulin sensitivity. Am J Physiol Endocrinol Metab 296: E945–E954, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Lin J, Handschin C, Spiegelman BM. Metabolic control through the PGC-1 family of transcription coactivators. Cell Metab 1: 361–370, 2005 [DOI] [PubMed] [Google Scholar]
- 114.Lin J, Puigserver P, Donovan J, Tarr P, Spiegelman BM. Peroxisome proliferator-activated receptor gamma coactivator 1beta (PGC-1beta), a novel PGC-1-related transcription coactivator associated with host cell factor. J Biol Chem 277: 1645–1648, 2002 [DOI] [PubMed] [Google Scholar]
- 115.Lin J, Tarr PT, Yang R, Rhee J, Puigserver P, Newgard CB, Spiegelman BM. PGC-1beta in the regulation of hepatic glucose and energy metabolism. J Biol Chem 278: 30843–30848, 2003 [DOI] [PubMed] [Google Scholar]
- 116.Lin J, Wu H, Tarr PT, Zhang CY, Wu Z, Boss O, Michael LF, Puigserver P, Isotani E, Olson EN, Lowell BB, Bassel-Duby R, Spiegelman BM. Transcriptional co-activator PGC-1 alpha drives the formation of slow-twitch muscle fibres. Nature 418: 797–801, 2002 [DOI] [PubMed] [Google Scholar]
- 117.Lin J, Wu PH, Tarr PT, Lindenberg KS, St-Pierre J, Zhang CY, Mootha VK, Jager S, Vianna CR, Reznick RM, Cui L, Manieri M, Donovan MX, Wu Z, Cooper MP, Fan MC, Rohas LM, Zavacki AM, Cinti S, Shulman GI, Lowell BB, Krainc D, Spiegelman BM. Defects in adaptive energy metabolism with CNS-linked hyperactivity in PGC-1alpha null mice. Cell 119: 121–135, 2004 [DOI] [PubMed] [Google Scholar]
- 118.Ling C, Poulsen P, Carlsson E, Ridderstrale M, Almgren P, Wojtaszewski J, Beck-Nielsen H, Groop L, Vaag A. Multiple environmental and genetic factors influence skeletal muscle PGC-1alpha and PGC-1beta gene expression in twins. J Clin Invest 114: 1518–1526, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Lira VA, Soltow QA, Long JH, Betters JL, Sellman JE, Criswell DS. Nitric oxide increases GLUT4 expression and regulates AMPK signaling in skeletal muscle. Am J Physiol Endocrinol Metab 293: E1062–E1068, 2007 [DOI] [PubMed] [Google Scholar]
- 120.Listenberger LL, Han X, Lewis SE, Cases S, Farese RV, Jr, Ory DS, Schaffer JE. Triglyceride accumulation protects against fatty acid-induced lipotoxicity. Proc Natl Acad Sci USA 100: 3077–3082, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Liu C, Li S, Liu T, Borjigin J, Lin JD. Transcriptional coactivator PGC-1alpha integrates the mammalian clock and energy metabolism. Nature 447: 477–481, 2007 [DOI] [PubMed] [Google Scholar]
- 122.Liu L, Shi X, Bharadwaj KG, Ikeda S, Yamashita H, Yagyu H, Schaffer JE, Yu YH, Goldberg IJ. DGAT1 expression increases heart triglyceride content but ameliorates lipotoxicity. J Biol Chem 284: 36312–36323, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Long YC, Glund S, Garcia-Roves PM, Zierath JR. Calcineurin regulates skeletal muscle metabolism via coordinated changes in gene expression. J Biol Chem 282: 1607–1614, 2007 [DOI] [PubMed] [Google Scholar]
- 124.Luiken JJ, Arumugam Y, Dyck DJ, Bell RC, Pelsers MM, Turcotte LP, Tandon NN, Glatz JF, Bonen A. Increased rates of fatty acid uptake and plasmalemmal fatty acid transporters in obese Zucker rats. J Biol Chem 276: 40567–40573, 2001 [DOI] [PubMed] [Google Scholar]
- 125.Mathai AS, Bonen A, Benton CR, Robinson DL, Graham TE. Rapid exercise-induced changes in PGC-1α mRNA and protein in human skeletal muscle. J Appl Physiol 105: 1098–1105, 2008 [DOI] [PubMed] [Google Scholar]
- 126.McArdle A, Pattwell D, Vasilaki A, Griffiths RD, Jackson MJ. Contractile activity-induced oxidative stress: cellular origin and adaptive responses. Am J Physiol Cell Physiol 280: C621–C627, 2001 [DOI] [PubMed] [Google Scholar]
- 127.McArdle F, Pattwell DM, Vasilaki A, McArdle A, Jackson MJ. Intracellular generation of reactive oxygen species by contracting skeletal muscle cells. Free Radic Biol Med 39: 651–657, 2005 [DOI] [PubMed] [Google Scholar]
- 128.McConell GK, Ng GP, Phillips M, Ruan Z, Macaulay SL, Wadley GD. Central role of nitric oxide synthase in AICAR and caffeine-induced mitochondrial biogenesis in L6 myocytes. J Appl Physiol 108: 589–595, 2010 [DOI] [PubMed] [Google Scholar]
- 129.McCullagh KJ, Calabria E, Pallafacchina G, Ciciliot S, Serrano AL, Argentini C, Kalhovde JM, Lomo T, Schiaffino S. NFAT is a nerve activity sensor in skeletal muscle and controls activity-dependent myosin switching. Proc Natl Acad Sci USA 101: 10590–10595, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.McGee SL, Fairlie E, Garnham AP, Hargreaves M. Exercise-induced histone modifications in human skeletal muscle. J Physiol 587: 5951–5958, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Meirhaeghe A, Crowley V, Lenaghan C, Lelliott C, Green K, Stewart A, Hart K, Schinner S, Sethi JK, Yeo G, Brand MD, Cortright RN, O'Rahilly S, Montague C, Vidal-Puig AJ. Characterization of the human, mouse and rat PGC1 beta (peroxisome-proliferator-activated receptor-gamma co-activator 1 beta) gene in vitro and in vivo. Biochem J 373: 155–165, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Michael LF, Wu Z, Cheatham RB, Puigserver P, Adelmant G, Lehman JJ, Kelly DP, Spiegelman BM. Restoration of insulin-sensitive glucose transporter (GLUT4) gene expression in muscle cells by the transcriptional coactivator PGC-1. Proc Natl Acad Sci USA 98: 3820–3825, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Miura S, Kai Y, Ono M, Ezaki O. Overexpression of peroxisome proliferator-activated receptor gamma coactivator-1alpha down-regulates GLUT4 mRNA in skeletal muscles. J Biol Chem 278: 31385–31390, 2003 [DOI] [PubMed] [Google Scholar]
- 134.Miyazaki M, Hitomi Y, Kizaki T, Ohno H, Haga S, Takemasa T. Contribution of the calcineurin signaling pathway to overload-induced skeletal muscle fiber-type transition. J Physiol Pharmacol 55: 751–764, 2004 [PubMed] [Google Scholar]
- 135.Mogensen M, Sahlin K, Fernström M, Glintborg D, Vind BF, Beck-Nielsen H, Højlund K. Mitochondrial respiration is decreased in skeletal muscle of patients with type 2 diabetes. Diabetes 56: 1592–1599, 2007 [DOI] [PubMed] [Google Scholar]
- 136.Mootha VK, Handschin C, Arlow D, Xie X, St Pierre J, Sihag S, Yang W, Altshuler D, Puigserver P, Patterson N, Willy PJ, Schulman IG, Heyman RA, Lander ES, Spiegelman BM. Erralpha and Gabpa/b specify PGC-1alpha-dependent oxidative phosphorylation gene expression that is altered in diabetic muscle. Proc Natl Acad Sci USA 101: 6570–6575, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Mootha VK, Lindgren CM, Eriksson KF, Subramanian A, Sihag S, Lehar J, Puigserver P, Carlsson E, Ridderstrale M, Laurila E, Houstis N, Daly MJ, Patterson N, Mesirov JP, Golub TR, Tamayo P, Spiegelman B, Lander ES, Hirschhorn JN, Altshuler D, Groop LC. PGC-1alpha-responsive genes involved in oxidative phosphorylation are coordinately downregulated in human diabetes. Nat Genet 34: 267–273, 2003 [DOI] [PubMed] [Google Scholar]
- 138.Morino K, Petersen KF, Shulman GI. Molecular mechanisms of insulin resistance in humans and their potential links with mitochondrial dysfunction. Diabetes 55, Suppl 2: S9–S15, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Mortensen OH, Frandsen L, Schjerling P, Nishimura E, Grunnet N. PGC-1α and PGC-1β have both similar and distinct effects on myofiber switching toward an oxidative phenotype. Am J Physiol Endocrinol Metab 291: E807–E816, 2006 [DOI] [PubMed] [Google Scholar]
- 140.Mortensen OH, Plomgaard P, Fischer CP, Hansen AK, Pilegaard H, Pedersen BK. PGC-1β is downregulated by training in human skeletal muscle: no effect of training twice every second day vs. once daily on expression of the PGC-1 family. J Appl Physiol 103: 1536–1542, 2007 [DOI] [PubMed] [Google Scholar]
- 141.Narkar VA, Downes M, Yu RT, Embler E, Wang YX, Banayo E, Mihaylova MM, Nelson MC, Zou Y, Juguilon H, Kang H, Shaw RJ, Evans RM. AMPK and PPARdelta agonists are exercise mimetics. Cell 134: 405–415, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Naya FJ, Mercer B, Shelton J, Richardson JA, Williams RS, Olson EN. Stimulation of slow skeletal muscle fiber gene expression by calcineurin in vivo. J Biol Chem 275: 4545–4548, 2000 [DOI] [PubMed] [Google Scholar]
- 143.Nesher R, Karl IE, Kipnis DM. Dissociation of effects of insulin and contraction on glucose transport in rat epitrochlearis muscle. Am J Physiol Cell Physiol 249: C226–C232, 1985 [DOI] [PubMed] [Google Scholar]
- 144.Nickerson JG, Alkhateeb H, Benton CR, Lally J, Nickerson J, Han XX, Wilson MH, Jain SS, Snook LA, Glatz JF, Chabowski A, Luiken JJ, Bonen A. Greater transport efficiencies of the membrane fatty acid transporters FAT/CD36 and FATP4 compared with FABPpm and FATP1 and differential effects on fatty acid esterification and oxidation in rat skeletal muscle. J Biol Chem 284: 16522–16530, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Nisoli E, Falcone S, Tonello C, Cozzi V, Palomba L, Fiorani M, Pisconti A, Brunelli S, Cardile A, Francolini M, Cantoni O, Carruba MO, Moncada S, Clementi E. Mitochondrial biogenesis by NO yields functionally active mitochondria in mammals. Proc Natl Acad Sci USA 101: 16507–16512, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Oliveira RL, Ueno M, de Souza CT, Pereira-da-Silva M, Gasparetti AL, Bezzera RM, Alberici LC, Vercesi AE, Saad MJ, Velloso LA. Cold-induced PGC-1α expression modulates muscle glucose uptake through an insulin receptor/Akt-independent, AMPK-dependent pathway. Am J Physiol Endocrinol Metab 287: E686–E695, 2004 [DOI] [PubMed] [Google Scholar]
- 147.Pan DA, Lillioja S, Kriketos AD, Milner MR, Baur LA, Jenkins AB, Storlien LH. Skeletal muscle triglyceride levels are inversely related to insulin action. Diabetes 46: 983–988, 1997 [DOI] [PubMed] [Google Scholar]
- 148.Patti ME, Butte AJ, Crunkhorn S, Cusi K, Berria R, Kashyap S, Miyazaki Y, Kohane I, Costello M, Saccone R, Landaker EJ, Goldfine AB, Mun E, DeFronzo R, Finlayson J, Kahn CR, Mandarino LJ. Coordinated reduction of genes of oxidative metabolism in humans with insulin resistance and diabetes: Potential role of PGC1 and NRF1. Proc Natl Acad Sci USA 100: 8466–8471, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Pattwell DM, McArdle A, Morgan JE, Patridge TA, Jackson MJ. Release of reactive oxygen and nitrogen species from contracting skeletal muscle cells. Free Radic Biol Med 37: 1064–1072, 2004 [DOI] [PubMed] [Google Scholar]
- 150.Perdomo G, Commerford SR, Richard AM, Adams SH, Corkey BE, O'Doherty RM, Brown NF. Increased beta-oxidation in muscle cells enhances insulin-stimulated glucose metabolism and protects against fatty acid-induced insulin resistance despite intramyocellular lipid accumulation. J Biol Chem 279: 27177–27186, 2004 [DOI] [PubMed] [Google Scholar]
- 151.Perry CG, Heigenhauser GJ, Bonen A, Spriet LL. High-intensity aerobic interval training increases fat and carbohydrate metabolic capacities in human skeletal muscle. Appl Physiol Nutr Metab 33: 1112–1123, 2008 [DOI] [PubMed] [Google Scholar]
- 152.Petersen KF, Dufour S, Befroy D, Garcia R, Shulman GI. Impaired mitochondrial activity in the insulin-resistant offspring of patients with type 2 diabetes. N Engl J Med 350: 664–671, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Pilegaard H, Saltin B, Neufer P. Exercise induces transient transcriptional activation of the PGC-1alpha gene in human skeletal muscle. J Physiol 546: 851–858, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Pogozelski AR, Geng T, Li P, Yin X, Lira VA, Zhang M, Chi JT, Yan Z. p38gamma mitogen-activated protein kinase is a key regulator in skeletal muscle metabolic adaptation in mice. PLoS One 4: e7934, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Pratley RE, Thomson DB, Prochazka M, Baier L, Mott D, Ravussin E, Sahkul H, Ehm MG, Burns DK, Foroud T, Garvey W, Hanson RL, Knowler WC, Bennett PH, Bogardus C. An autosomal gneomic scan for loci linked to pre-diabetic phenotypes in Pima Indians. J Clin Invest 101: 1757–1764, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Prince FP, Hikida RS, Hagerman FC, Staron RS, Allen WH. A morphometric analysis of human muscle fibers with relation to fiber types and adaptations to exercise. J Neurol Sci 49: 165–179, 1981 [DOI] [PubMed] [Google Scholar]
- 157.Puigserver P, Rhee J, Lin J, Wu Z, Yoon JC, Zhang CY, Krauss S, Mootha VK, Lowell BB, Spiegelman BM. Cytokine stimulation of energy expenditure through p38 MAP kinase activation of PPARgamma coactivator-1. Mol Cell 8: 971–982, 2001 [DOI] [PubMed] [Google Scholar]
- 158.Puigserver P, Spiegelman BM. Peroxisome proliferator-activated receptor-gamma coactivator 1 alpha (PGC-1 alpha): transcriptional coactivator and metabolic regulator. Endocr Rev 24: 78–90, 2003 [DOI] [PubMed] [Google Scholar]
- 159.Puigserver P, Wu Z, Park CW, Gracves R, Wright M, Spiegelman BM. A cold-inducible coactivator of nuclear receptors linked to adaptive thermogenesis. Cell 92: 829–839, 1998 [DOI] [PubMed] [Google Scholar]
- 160.Raney MA, Turcotte LP. Evidence for the involvement of CaMKII and AMPK in Ca2+-dependent signaling pathways regulating FA uptake and oxidation in contracting rodent muscle. J Appl Physiol 104: 1366–1373, 2008 [DOI] [PubMed] [Google Scholar]
- 161.Reid MB. Role of nitric oxide in skeletal muscle: synthesis, distribution and functional importance. Acta Physiol Scand 162: 401–409, 1998 [DOI] [PubMed] [Google Scholar]
- 162.Reid MB, Shoji T, Moody MR, Entman ML. Reactive oxygen in skeletal muscle. II. Extracellular release of free radicals. J Appl Physiol 73: 1805–1809, 1992 [DOI] [PubMed] [Google Scholar]
- 163.Reitman JS, Vasquez B, Klimes I, Nagulesparan M. Improvement of glucose homeostasis after exercise training in non-insulin-dependent diabetes. Diabetes Care 7: 434–441, 1984 [DOI] [PubMed] [Google Scholar]
- 164.Richardson DK, Kashyap S, Bajaj M, Cusi K, Mandarino SJ, Finlayson J, Defronzo RA, Jenkinson CP, Mandarino LJ. Lipid infusion decreases the expression of nuclear encoded mitochondrial genes and increases the expression of extracellular matrix genes in human skeletal muscle. J Biol Chem 280: 10290–10297, 2005 [DOI] [PubMed] [Google Scholar]
- 165.Ristow M, Zarse K, Oberbach A, Kloting N, Birringer M, Kiehntopf M, Stumvoll M, Kahn CR, Bluher M. Antioxidants prevent health-promoting effects of physical exercise in humans. Proc Natl Acad Sci USA 106: 8665–8670, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Rivero JL, Talmadge RJ, Edgerton VR. Fibre size and metabolic properties of myosin heavy chain-based fibre types in rat skeletal muscle. J Muscle Res Cell Motil 19: 733–742, 1998 [DOI] [PubMed] [Google Scholar]
- 167.Rivero JL, Talmadge RJ, Edgerton VR. Interrelationships of myofibrillar ATPase activity and metabolic properties of myosin heavy chain-based fibre types in rat skeletal muscle. Histochem Cell Biol 111: 277–287, 1999 [DOI] [PubMed] [Google Scholar]
- 168.Rockl KS, Hirshman MF, Brandauer J, Fujii N, Witters LA, Goodyear LJ. Skeletal muscle adaptation to exercise training: AMP-activated protein kinase mediates muscle fiber type shift. Diabetes 56: 2062–2069, 2007 [DOI] [PubMed] [Google Scholar]
- 169.Rodríguez-Calvo R, Jové M, Coll T, Camins A, Sánchez RM, Alegret M, Merlos M, Pallàs M, Laguna JC, Vázquez-Carrera M. PGC-1beta down-regulation is associated with reduced ERRalpha activity and MCAD expression in skeletal muscle of senescence-accelerated mice. J Gerontol A Biol Sci Med Sci 61: 773–780, 2006 [DOI] [PubMed] [Google Scholar]
- 170.Rose AJ, Hargreaves M. Exercise increases Ca2+-calmodulin-dependent protein kinase II activity in human skeletal muscle. J Physiol 553: 303–309, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Rose AJ, Kiens B, Richter EA. Ca2+-calmodulin-dependent protein kinase expression and signalling in skeletal muscle during exercise. J Physiol 574: 889–903, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Russell AP, Feilchenfeldt J, Schreiber S, Praz M, Crettenand A, Gobelet C, Meier CA, Bell DR, Kralli A, Giacobino JP, Deriaz O. Endurance training in humans leads to fiber type-specific increases in levels of peroxisome proliferator-activated receptor-gamma coactivator-1 and peroxisome proliferator-activated receptor-alpha in skeletal muscle. Diabetes 52: 2874–2881, 2003 [DOI] [PubMed] [Google Scholar]
- 173.Russell AP, Hesselink MK, Lo SK, Schrauwen P. Regulation of metabolic transcriptional co-activators and transcription factors with acute exercise. FASEB J 19: 986–988, 2005 [DOI] [PubMed] [Google Scholar]
- 174.Ryder JW, Bassel-Duby R, Olson EN, Zierath JR. Skeletal muscle reprogramming by activation of calcineurin improves insulin action on metabolic pathways. J Biol Chem 278: 44298–44304, 2003 [DOI] [PubMed] [Google Scholar]
- 175.Rytinki MM, Palvimo JJ. SUMOylation modulates the transcription repressor function of RIP140. J Biol Chem 283: 11586–11595, 2008 [DOI] [PubMed] [Google Scholar]
- 176.Sadana P, Zhang Y, Song S, Cook GA, Elam MB, Park EA. Regulation of carnitine palmitoyltransferase I (CPT-Ialpha) gene expression by the peroxisome proliferator activated receptor gamma coactivator (PGC-1) isoforms. Mol Cell Endocrinol 267: 6–16, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Scarpulla RC. Transcriptional paradigms in mammalian mitochondrial biogenesis and function. Physiol Rev 88: 611–638, 2008 [DOI] [PubMed] [Google Scholar]
- 178.Schertzer JD, Plant DR, Lynch GS. Optimizing plasmid-based gene transfer for investigating skeletal muscle structure and function. Mol Ther 13: 795–803, 2006 [DOI] [PubMed] [Google Scholar]
- 179.Schiaffino S, Sandri M, Murgia M. Activity-dependent signaling pathways controlling muscle diversity and plasticity. Physiology (Bethesda) 22: 269–278, 2007 [DOI] [PubMed] [Google Scholar]
- 180.Searle MS, Ready AE. Survey of exercise and dietary knowledge and behaviour in persons with type II diabetes. Can J Public Health 82: 344–348, 1991 [PubMed] [Google Scholar]
- 181.Segal KR, Edano A, Abalos A, Albu J, Blando L, Tomas MB, Pi-Sunyer X. Effect of exercise training on insulin sensitivity and glucose metabolism on lean, obese, and diabetic men. J Appl Physiol 71: 2402–2411, 1991 [DOI] [PubMed] [Google Scholar]
- 182.Sellman JE, DeRuisseau KC, Betters JL, Lira VA, Soltow QA, Selsby JT, Criswell DS. In vivo inhibition of nitric oxide synthase impairs upregulation of contractile protein mRNA in overloaded plantaris muscle. J Appl Physiol 100: 258–265, 2006 [DOI] [PubMed] [Google Scholar]
- 183.Serrano AL, Murgia M, Pallafacchina G, Calabria E, Coniglio P, Lomo T, Schiaffino S. Calcineurin controls nerve activity-dependent specification of slow skeletal muscle fibers but not muscle growth. Proc Natl Acad Sci USA 98: 13108–13113, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Short KR, Vittone JL, Bigelow ML, Proctor DN, Rizza RA, Coenen-Schimke JM, Nair KS. Impact of aerobic exercise training on age-related changes in insulin sensitivity and muscle oxidative capacity. Diabetes 52: 1888–1896, 2003 [DOI] [PubMed] [Google Scholar]
- 185.Silveira LR, Pereira-Da-Silva L, Juel C, Hellsten Y. Formation of hydrogen peroxide and nitric oxide in rat skeletal muscle cells during contractions. Free Radic Biol Med 35: 455–464, 2003 [DOI] [PubMed] [Google Scholar]
- 186.Silveira LR, Pilegaard H, Kusuhara K, Curi R, Hellsten Y. The contraction induced increase in gene expression of peroxisome proliferator-activated receptor (PPAR)-gamma coactivator 1alpha (PGC-1alpha), mitochondrial uncoupling protein 3 (UCP3) and hexokinase II (HKII) in primary rat skeletal muscle cells is dependent on reactive oxygen species. Biochim Biophys Acta 1763: 969–976, 2006 [DOI] [PubMed] [Google Scholar]
- 187.Sjogaard G. Capillary supply and cross-sectional area of slow and fast twitch muscle fibres in man. Histochemistry 76: 547–555, 1982 [DOI] [PubMed] [Google Scholar]
- 188.Solomon TP, Sistrun SN, Krishnan RK, Del Aguila LF, Marchetti CM, O'Carroll SM, O'Leary VB, Kirwan JP. Exercise and diet enhance fat oxidation and reduce insulin resistance in older obese adults. J Appl Physiol 104: 1313–1319, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Sriwijitkamol A, Ivy JL, Christ-Roberts C, Defronzo RA, Mandarino LJ, Musi N. LKB1-AMPK signaling in muscle from obese insulin-resistant Zucker rats and effects of training. Am J Physiol Endocrinol Metab 290: E925–E932, 2006 [DOI] [PubMed] [Google Scholar]
- 190.St-Pierre J, Lin J, Krauss S, Tarr PT, Yang R, Newgard CB, Spiegelman BM. Bioenergetic analysis of peroxisome proliferator-activated receptor gamma coactivators 1alpha and 1beta (PGC-1alpha and PGC-1beta) in muscle cells. J Biol Chem 278: 26597–26603, 2003 [DOI] [PubMed] [Google Scholar]
- 191.Starritt EC, Howlett RA, Heigenhauser GJ, Spriet LL. Sensitivity of CPT I to malonyl-CoA in trained and untrained human skeletal muscle. Am J Physiol Endocrinol Metab 278: E462–E468, 2000 [DOI] [PubMed] [Google Scholar]
- 192.Storlien LH, Jenkins AB, Chisholm DJ, Pascoe WS, Khouri S, Kraegen EW. Influence of dietary fat composition on development of insulin resistance in rats. Diabetes 40: 280–289, 1991 [DOI] [PubMed] [Google Scholar]
- 193.Stratford S, Hoehn KL, Liu F, Summers SA. Regulation of insulin action by ceramide: dual mechanisms linking ceramide accumulation to the inhibition of Akt/protein kinase B. J Biol Chem 279: 36608–36615, 2004 [DOI] [PubMed] [Google Scholar]
- 194.Summers SA, Garza LA, Zhou H, Birnbaum MJ. Regulation of insulin-stimulated glucose transporter GLUT4 translocation and Akt kinase activity by ceramide. Mol Cell Biol 18: 5457–5464, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Suwa M, Egashira T, Nakano H, Sasaki H, Kumagai S. Metformin increases the PGC-1α protein and oxidative enzyme activities possibly via AMPK phosphorylation in skeletal muscle in vivo. J Appl Physiol 101: 1685–1692, 2006 [DOI] [PubMed] [Google Scholar]
- 196.Talanian JL, Galloway SD, Heigenhauser GJ, Bonen A, Spriet LL. Two weeks of high-intensity aerobic interval training increases the capacity for fat oxidation during exercise in women. J Appl Physiol 102: 1439–1447, 2007 [DOI] [PubMed] [Google Scholar]
- 197.Tatsumi R, Wuollet AL, Tabata K, Nishimura S, Tabata S, Mizunoya W, Ikeuchi Y, Allen RE. A role for calcium-calmodulin in regulating nitric oxide production during skeletal muscle satellite cell activation. Am J Physiol Cell Physiol 296: C922–C929, 2009 [DOI] [PubMed] [Google Scholar]
- 198.Taylor EB, Lamb JD, Hurst RW, Chesser DG, Ellingson WJ, Greenwood LJ, Porter BB, Herway ST, Winder WW. Endurance training increases skeletal muscle LKB1 and PGC-1α protein abundance: effects of time and intensity. Am J Physiol Endocrinol Metab 289: E960–E968, 2005 [DOI] [PubMed] [Google Scholar]
- 199.Terada S, Goto M, Kawanaka K, Shimokawa T, Tabata I. Effects of low-intensity prolonged exercise on PGC-1 mRNA expression in rat epitrochlearis muscle. Biochem Biophys Res Commun 296: 350–354, 2002 [DOI] [PubMed] [Google Scholar]
- 200.Terada S, Tabata I. Effects of acute bouts of running and swimming exercise on PGC-1α protein expression in rat epitrochlearis and soleus muscle. Am J Physiol Endocrinol Metab 286: E208–E216, 2004 [DOI] [PubMed] [Google Scholar]
- 201.Termin A, Staron RS, Pette D. Myosin heavy chain isoforms in histochemically defined fiber types of rat muscle. Histochemistry 92: 453–457, 1989 [DOI] [PubMed] [Google Scholar]
- 202.Thomson DM, Herway ST, Fillmore N, Kim H, Brown JD, Barrow JR, Winder WW. AMP-activated protein kinase phosphorylates transcription factors of the CREB family. J Appl Physiol 104: 429–438, 2008 [DOI] [PubMed] [Google Scholar]
- 203.Thyfault JP, Cree MG, Zheng D, Zwetsloot JJ, Tapscott EB, Koves TR, Ilkayeva O, Wolfe RR, Muoio DM, Dohm GL. Contraction of insulin-resistant muscle normalizes insulin action in association with increased mitochondrial activity and fatty acid catabolism. Am J Physiol Cell Physiol 292: C729–C739, 2007 [DOI] [PubMed] [Google Scholar]
- 204.Timmons JA, Norrbom J, Scheele C, Thonberg H, Wahlestedt C, Tesch P. Expression profiling following local muscle inactivity in humans provides new perspective on diabetes-related genes. Genomics 87: 165–172, 2006 [DOI] [PubMed] [Google Scholar]
- 205.Tomas E, Zorzano A, Ruderman NB. Exercise and insulin signaling: a historical perspective. J Appl Physiol 93: 765–772, 2002 [DOI] [PubMed] [Google Scholar]
- 206.Tsintzas K, Jewell K, Kamran M, Laithwaite D, Boonsong T, Littlewood J, Macdonald I, Bennett A. Differential regulation of metabolic genes in skeletal muscle during starvation and refeeding in humans. J Physiol 575: 291–303, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Turner N, Bruce CR, Beale SM, Hoehn KL, So T, Rolph MS, Cooney GJ. Excess lipid availability increases mitochondrial fatty acid oxidative capacity in muscle: evidence against a role for reduced fatty acid oxidation in lipid-induced insulin resistance in rodents. Diabetes 56: 2085–2092, 2007 [DOI] [PubMed] [Google Scholar]
- 208.van Loon LJ, Koopman R, Manders R, van der Weegen W, van Kranenburg GP, Keizer HA. Intramyocellular lipid content in type 2 diabetes patients compared with overweight sedentary men and highly trained endurance athletes. Am J Physiol Endocrinol Metab 287: E558–E565, 2004 [DOI] [PubMed] [Google Scholar]
- 209.Vissing K, McGee SL, Roepstorff C, Schjerling P, Hargreaves M, Kiens B. Effect of sex differences on human MEF2 regulation during endurance exercise. Am J Physiol Endocrinol Metab 294: E408–E415, 2008 [DOI] [PubMed] [Google Scholar]
- 210.Wadley GD, Choate J, McConell GK. NOS isoform-specific regulation of basal but not exercise-induced mitochondrial biogenesis in mouse skeletal muscle. J Physiol 585: 253–262, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Wadley GD, McConell GK. Effect of nitric oxide synthase inhibition on mitochondrial biogenesis in rat skeletal muscle. J Appl Physiol 102: 314–320, 2007 [DOI] [PubMed] [Google Scholar]
- 212.Wallberg-Henriksson H. Glucose transport into skeletal muscle. Influence of contractile activity, insulin, catecholamines and diabetes mellitus. Acta Physiol Scand Suppl 564: 1–80, 1987 [PubMed] [Google Scholar]
- 213.Wareski P, Vaarmann A, Choubey V, Safiulina D, Liiv J, Kuum M, Kaasik A. PGC-1{alpha} and PGC-1{beta} regulate mitochondrial density in neurons. J Biol Chem 284: 21379–21385, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Watt MJ, Southgate RJ, Holmes AG, Febbraio MA. Suppression of plasma free fatty acids upregulates peroxisome proliferator-activated receptor (PPAR) alpha and delta and PPAR coactivator 1alpha in human skeletal muscle, but not lipid regulatory genes. J Mol Endocrinol 33: 533–544, 2004 [DOI] [PubMed] [Google Scholar]
- 215.Wende AR, Schaeffer PJ, Parker GJ, Zexhner C, Han DH, Chen M, Hancock CR, Lehman JJ, Huss JM, McClain DA, Holloszy JO, Kelly DP. A role for the transcriptional co-activator PGC-1α in muscle refuelling. J Biol Chem 282: 36642–36651, 2007 [DOI] [PubMed] [Google Scholar]
- 216.Widegren U, Jiang XJ, Krook A, Chibalin AV, Björnholm M, Tally M, Roth RA, Henriksson J, Wallberg-henriksson H, Zierath JR. Divergent effects of exercise on metabolic and mitogenic signaling pathways in human skeletal muscle. FASEB J 12: 1379–1389, 1998 [DOI] [PubMed] [Google Scholar]
- 217.Winder WW, Hardie DG. Inactivation of acetyl-CoA carboxylase and activation of AMP-activated protein kinase in muscle during exercise. Am J Physiol Endocrinol Metab 270: E299–E304, 1996 [DOI] [PubMed] [Google Scholar]
- 218.Winder WW, Holmes BF, Rubink DS, Jensen EB, Chen M, Holloszy JO. Activation of AMP-activated protein kinase increases mitochondrial enzymes in skeletal muscle. J Appl Physiol 88: 2219–2226, 2000 [DOI] [PubMed] [Google Scholar]
- 219.Witzmann FA, Kim DH, Fitts RH. Hindlimb immobilization: length-tension and contractile properties of skeletal muscle. J Appl Physiol 53: 335–345, 1982 [DOI] [PubMed] [Google Scholar]
- 220.Wojtaszewski JF, Nielsen P, Hansen BF, Richter EA, Kiens B. Isoform-specific and exercise intensity-dependent activation of 5′-AMP-activated protein kinase in human skeletal muscle. J Physiol 528: 221–226, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Woods A, Dickerson K, Heath R, Hong SP, Momcilovic M, Johnstone SR, Carlson M, Carling D. Ca2+/calmodulin-dependent protein kinase kinase-beta acts upstream of AMP-activated protein kinase in mammalian cells. Cell Metab 2: 21–33, 2005 [DOI] [PubMed] [Google Scholar]
- 222.Wright DC, Geiger PC, Han DH, Jones TE, Holloszy JO. Calcium induces increases in peroxisome proliferator-activated receptor gamma coactivator-1alpha and mitochondrial biogenesis by a pathway leading to p38 mitogen-activated protein kinase activation. J Biol Chem 282: 18793–18799, 2007 [DOI] [PubMed] [Google Scholar]
- 223.Wright DC, Han DH, Garcia-Roves PM, Geiger PC, Jones TE, Holloszy JO. Exercise-induced mitochondrial biogenesis begins before the increase in muscle PGC-1alpha expression. J Biol Chem 282: 194–199, 2007 [DOI] [PubMed] [Google Scholar]
- 224.Wright DC, Hucker KA, Holloszy JO, Han DH. Ca2+ and AMPK both mediate stimulation of glucose transport by muscle contractions. Diabetes 53: 330–335, 2004 [DOI] [PubMed] [Google Scholar]
- 225.Wu H, Kanatous SB, Thurmond FA, Gallardo T, Isotani E, Bassel-Duby R, Williams RS. Regulation of mitochondrial biogenesis in skeletal muscle by CaMK. Science 296: 349–352, 2002 [DOI] [PubMed] [Google Scholar]
- 226.Wu H, Naya FJ, McKinsey TA, Mercer B, Shelton JM, Chin ER, Simard AR, Michel RN, Bassel-Duby R, Olson EN, Williams RS. MEF2 responds to multiple calcium-regulated signals in the control of skeletal muscle fiber type. EMBO J 19: 1963–1973, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Wu Z, Puigserver P, Andersson U, Zhang C, Adelmant G, Mootha V, Troy A, Cinti S, Lowell B, Scarpulla RC, Spiegelman BM. Mechanisms controlling mitochondrial biogenesis and respiration through the thermogenic coactivator PGC-1. Cell 98: 115–124, 1999 [DOI] [PubMed] [Google Scholar]
- 228.Zhao M, New L, Kravchenko VV, Kato Y, Gram H, di Padova F, Olson EN, Ulevitch RJ, Han J. Regulation of the MEF2 family of transcription factors by p38. Mol Cell Biol 19: 21–30, 1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Zierath JR. Invited review: Exercise training-induced changes in insulin signaling in skeletal muscle. J Appl Physiol 93: 773–781, 2002 [DOI] [PubMed] [Google Scholar]
- 230.Zong H, Ren JM, Young LH, Pypaert M, Mu J, Birnbaum MJ, Shulman GI. AMP kinase is required for mitochondrial biogenesis in skeletal muscle in response to chronic energy deprivation. Proc Natl Acad Sci USA 99: 15983–15987, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]