Abstract
Evidence suggests variability in adult obesity risk at a small-scale geographic area is associated with differences in neighborhood socioeconomic status (SES). However, the extent to which geographic variability in child obesity is associated with neighborhood SES is unknown. The objective of this paper was to estimate risk of child obesity associated with multiple census tract SES measures and race within a large urban U.S. county. Height, weight, age, sex, medical insurance type and census tract residence were obtained for 6–18 year old children (n = 8,616) who received medical care at a health plan in King County, Washington, in 2006. Spatial analyses examined the individual risk of obesity (BMI ≥95th percentile) with 2000 US census tract measures of median household income, home ownership, adult female education level, single parent households, and race as predictors. Conditional autoregressive regression models that incorporated adjacent census tracts (spatial autocorrelation) were applied to each census tract variable, adjusting for individual variables. We found that in adjusted spatial models, child obesity risk was significantly associated with each census tract variable in the expected direction: lower household income, lower home ownership, and for each 10% increase in less educated women, and single parent households, as well as non-white residents. In a spatial model including all variables, the SES/race variables explained approximately 24% of geographic variability in child obesity. Results indicated that living in census tracts with social disadvantage defined by multiple different measures was associated with child obesity among insured children in a large U.S. urban county. These results contribute new information on relationships between broader social and economic context and child obesity risk using robust spatial analyses.
Keywords: USA, child obesity, neighborhood, socioeconomic status, spatial epidemiology, social inequality, children
Background
Among U.S. children, the prevalence of obesity (defined as BMI ≥ 95th percentile for sex and age) has tripled since 1980 (Ogden, Carroll, Curtin, McDowell, Tabak, & Flegal, 2006), a disquieting harbinger of the global rise in childhood obesity in developed and developing countries (Caballero, 2007; Flynn, McNeil, Maloff, Mutasingwa, Wu, Ford et al., 2006). Currently in the United States, an estimated 1 in 6 children are obese (Ogden et al., 2006), and obesity is calculated to be the second leading cause of death in adults (Mokdad, Marks, Stroup, & Gerberding, 2004, 2005). The recent dramatic increases in obesity prevalence have been attributed to environmental changes that promote excessive food intake and discourage physical activity (French, Story, & Jeffery, 2001; Weinsier, Hunter, Heini, Goran, & Sell, 1998). Research also has found that child and adult risk of obesity is related to individual socioeconomic status (SES) factors, such as household income and educational attainment, as well as race/ethnicity (Baltrus, Everson-Rose, Lynch, Raghunathan, & Kaplan, 2007; McLaren, 2007; Ogden et al., 2006; Truong & Sturm, 2005). There is evidence of a widening social inequality gap in child obesity in the U.S. (Singh, Siahpush, & Kogan, 2010), suggesting a particular vulnerability to environmental factors that confer obesity risk among people who face social disadvantage, including lower SES and certain race/ethnicity groups (Lovasi, Hutson, Guerra, & Neckerman, 2009).
International research in adults examining multiple health outcomes, including mortality, has shown adverse effects of neighborhood poverty beyond individual SES. Some explanations to understand this phenomenon have asserted that low SES of the individuals making up the neighborhood (compositional) do not fully explain an independent effect of neighborhood structure or norms (contextual) (Macintyre, Ellaway, & Cummins, 2002; Wen, Browning, & Cagney, 2003). Differences in mediating pathways for individual and neighborhood measures of SES on health, suggest that neighborhood SES measures indeed represent separate and distinct constructs from individual SES factors, and that both need to be considered in addressing health disparities (van Jaarsveld, Miles, & Wardle, 2007). More recent work has sought to advance the understanding to include ‘relational’ explanations, moving beyond the dichotomy of composition and context, to include the dynamic interactions between individuals and place (Cummins, Curtis, Diez-Roux, & Macintyre, 2007).
The relationship between area-based SES and obesity among children may be of particular interest given the rapid increase in child obesity, and the recognition that prevention earlier in life likely represents the most effective strategy (Ells, Campbell, Lidstone, Kelly, Lang, & Summerbell, 2005). Research on relationships between SES and obesity has been of longstanding interest (Sobal & Stunkard, 1989), but area-based measures for children represent a growing area of investigation. An international systematic review of literature on child obesity and SES (Shrewsbury & Wardle, 2008) included 7 studies examining associations with neighborhood SES. Mixed results were found: two studies found inverse associations (higher obesity in lower SES neighborhoods)(Jansen & Hazebroek-Kampschreur, 1997; Kinra, Nelder, & Lewendon, 2000), two studies found a mixed inverse association (i.e. only within sub-populations or with certain adiposity measures) (Booth, Macaskill, Lazarus, & Baur, 1999; Wardle, Jarvis, Steggles, Sutton, Williamson, Farrimond et al., 2003) and three studies found no association (Burke, Beilin, Dunbar, & Kevan, 2004; Cowell, Warren, & Montgomery, 1999; Wright & Parker, 2004). None of these studies included multi-level analyses controlling for both individual and family level characteristics and all included a composite measure of neighborhood SES but did not examine separate SES measures.
Among the few studies that have used multi-level analyses to examine whether geographic area-based SES are significantly related to children’s obesity risk, all have found inverse associations (Janssen, Boyce, Simpson, & Pickett, 2006; Lumeng, Appugliese, Cabral, Bradley, & Zuckerman, 2006; Nelson, Gordon-Larsen, Song, & Popkin, 2006; Oliver & Hayes, 2005). These studies have had methodological limitations, including using imprecise measures of geographic space and neighborhood SES (Lumeng et al., 2006) and relying on self-report adiposity data (Janssen et al., 2006; Nelson et al., 2006; Oliver & Hayes, 2005). None of these studies used spatial analytic methods, which offers advantages for assessing relationships of geographically-distributed variables. Only one study has used spatial statistical analyses (Drewnowski, Rehm, Kao, & Goldstein, 2009), but was limited by using a non-standard obesity classification, and including only one measure of SES.
The underlying framework for the current analysis draws on a conceptual model by Schulz et al. (Schulz, Kannan, Dvonch, Israel, Allen, James et al., 2005) that articulates how neighborhood-level SES inequalities increase the risk of chronic disease. The hypothesized mechanism is such that SES inequalities within neighborhoods result in intermediate differences in social and physical environments (e.g. neighborhood condition, land use, services, parks, etc.), which in turn impact proximate behaviors and exposures (e.g. stressors, health behaviors, psychosocial factors), thereby increasing the risk of chronic disease, such as obesity. The current analysis sought evidence to better understand relationships of these broad social determinants to the outcome of obesity specifically among children. While our analysis focuses specifically on the proximal SES and race factors representing potential social determinants of child obesity, there are a number of plausible neighborhood contextual factors likely related to SES (Gordon-Larsen, Nelson, Page, & Popkin, 2006; Nelson et al., 2006; Sallis & Glanz, 2006) that may explain how the environmental variables influence diet and physical activity behaviors and, in effect, create “obesogenic environments” (Nelson & Woods, 2009; Townshend & Lake, 2009). These variables include low walkability (Berke, Koepsell, Moudon, Hoskins, & Larson, 2007; Timperio, Salmon, Telford, & Crawford, 2005), lack of recreation sites for physical activity (Norman, Nutter, Ryan, Sallis, Calfras, & Patrick, 2006), lack of grocery stores offering affordable fresh fruits and vegetables (Morland, Diez Roux, & Wing, 2006; Smoyer-Tomic, Spence, Raine, Amrhein, Cameron, Yasenovskiy et al., 2008), and higher density of fast food outlets (Li, Harmer, Cardinal, Bosworth, & Johnson-Shelton, 2009; Powell, Chaloupka, & Bao, 2007; Simon, Kwan, Angelescu, Shih, & Fielding, 2008).
Advances in data availability through geographic information systems and spatial analytic tools allow for new opportunities to explore disease risk at a small-area scale in relation to the distribution of socioeconomic factors (Elliott & Wartenberg, 2004). The correlation between geographic area of residence and obesity is of particular interest in identifying the social determinants of obesity (Drewnowski, Rehm, & Solet, 2007; Drewnowski & Specter, 2004), especially factors that may be modifiable in communities most severely affected by obesity. The current study seeks to describe the relationship between child BMI and census-based measures of social advantage, using geographic information systems mapping and spatial analytic methods. Specifically, our study characterizes the associations between objectively-measured obesity and five different measures of social status among children enrolled in a single, large health plan in King Co. Washington, USA. This large urban county is comparable to overall average demographics in U.S. Furthermore, among developed countries, the U.S. has generally represented the early development of the obesity epidemic, including for children; therefore, studying potential etiologic factors for obesity within the U.S. is likely relevant to other countries where obesity is emerging as a major public health problem (Wang, Beydoun, Liang, Caballero, & Kumanyika, 2008), particularly in urban environments (Caballero, 2007) .
Methods
Study Population
The study was conducted at a prepaid health plan and delivery system which includes an integrated group practice serving approximately 300,000 members in western Washington State, USA. The Institutional Review Board reviewed and approved all study procedures.
Children ages 6 to 18 years of age who had been continuously enrolled in the health plan for at least six months as of July 31, 2006 and were residents of King County, WA were eligible for inclusion. Nursing staff and/or medical assistants obtained weight measurements during routine clinical care and entered these into the electronic medical record (EMR). Care standards indicate that weights should be obtained at each outpatient visit without extra clothing or shoes. For each child in this study, we extracted the most recent measurements of height and weight from the EMR that occurred on the same outpatient clinic visit during the preceding two-year period. Among the 14,401 children in our cohort, 5,408 (37.6%) were excluded because they did not have a weight and height measurement on the same day in the EMR. Lack of weight/height could have been due to no visit during the two years or not having both measures taken at the same visit (more common during acute care visits in which height is often not recorded). Another 377 (2.6%) were excluded due to no valid address to identify census tract location. Therefore, 8,616 (59.8%) were retained for all subsequent analyses.
The population retained for analysis resided in 369 of the 372 census tracts in King County. These census tracts include 99.8% of King County’s population less than 18 years old. All census tracts with children enrolled were retained given the capability of the spatial analytic techniques and statistical tests used to adjust for small numbers.
Child-Level Variables
The child-level variables included age, sex, and medical insurance plan. Medical plan was included as it reflects a child’s household income status in one of three categories: 1) commercial (for higher-income families receiving insurance through employment), 2) a state-sponsored reduced cost plan (for qualifying families with household income less than 200% of the U.S. federal poverty level but too high to qualify for Medicaid), and 3) Medicaid (a joint federal and state-sponsored medical plan for the poorest families). Each child’s residence was determined from administrative files and used to identify the census tract of residence, which was the smallest geographic designation available.
Census Tract Variables
Socioeconomic and race information for census tracts (a well-defined area-level measure with comprehensive data available from each U.S. census) was obtained from the 2000 U.S. Census (U.S. Census Bureau, 2000). The variables included were selected to represent multiple, broad but theoretically distinct constructs of social status, consistent with prior research postulating health disparities related to multiple measures of SES, including income, property, education, and head of household status (Braveman, Cubbin, Egerter, Chideya, Marchi, Metzler et al., 2005; Drewnowski et al., 2007). We also included a variable for race/ethnicity, as it represents an important measure of social advantage in the U.S., has been strongly correlated with SES and obesity in the U.S. (Braveman, 2009; Schulz et al., 2005), and thus represents a broad measure of social advantage in the U.S. Among possible variables, we selected five census tract variables that we hypothesized would be most likely to impact a child’s level of social advantage: 1) median household income, 2) percent of population residing in a home they own, 3) percent of females age 25 and older with high school education or less, 4) percent single parent households (among households with children), and 5) percent white race. We used separate SES measures rather than create a composite index because distinct measures are arguably more precise (Braveman et al., 2005) and facilitate comparison across different countries which may define SES differently. Furthermore, we sought to explain as much of the obesity variability across the region as possible, therefore including all variables separately in the model is likely more conservative in potentially explaining variability than a single composite measure.
All census tracts in King Co. were classified as urban and none were rural in the 2000 Census. To account for neighborhood differences that may be due to urban versus suburban population density, we conducted a sub-analysis including a variable for residential density from the 2000 Census defined as number of households per acre within the census tract. We categorized residential density into tertiles defined as low (0–2 households per acre), middle (3–4 households per acre), and high (5 or more households per acre).
Statistical Analysis
For all analyses the outcome was childhood obesity defined as BMI ≥ 95th percentile (American Medical Association, 2007), where the BMI percentile is determined by age, sex, weight, and height standards of the U.S. population before the obesity epidemic (Kuczmarski, Ogden, Guo, Grummer-Strawn, Flegal, Mei et al., 2002). Frequency distributions and odds ratios, using logistic regression, were determined for the census tract socioeconomic predictors and were described for King Co. compared to the U.S. census tracts overall.
A multi-level modeling framework was applied to assess the relationship between area-level SES/race variables and obesity. Obesity and individual predictors were measured at the child-level with area-level variables measured at the census tract. We applied a standard multi-level model with a logistic framework to account for census tract correlation and an extension using a Conditional Autoregressive Regression (CAR) model structure that further incorporates adjacent census tract correlation (spatial autocorrelation) (Gelman, Carlin, Stern, & Rubin, 1995). The advantage of this autocorrelation model is that it accounts for the somewhat arbitrary definition of contextual influence in the boundary lines of census tracts, which are not determined based on predictors of health outcomes. Therefore, two census tracts adjacent to each other may be very similar socioeconomically. Allowing for this correlation produces better estimates of the overall effect of area-level SES/race variables on health outcomes and reduces the bias due to residual confounding. The best model fit, based on the statistical measure Deviance Information Criteria (DIC)(Spiegelhalter, Best, Carlin, & Van der Linde, 2002), was the model which included the adjacent census tract correlation and was used in all analyses unless otherwise specified.
We evaluated the odds ratios for obesity associated with each of the census level SES/race predictors separately and then combined. For each variable, we present results based on the hypothesized direction that would result in an increased obesity risk. For median income, we present the odds ratio of obesity associated with each decrease of $10,000. For percent home ownership, we present the odds of a 10 percentage point decrease. For percent female education less than high school, percent single parent households, and percent non-white residents, we present the odds of a 10 percentage point increase.
A multivariable analysis was conducted including all of the SES/race variables. Several census tract socioeconomic variables were highly correlated (≥ .80 Spearman correlation coefficient) including median household income with percent home ownership and single parent households; as well as percent home ownership with percent single parent households. While these SES variables are highly correlated, they are not defined based on the same criteria. Therefore, we evaluated the relationships between the variables and obesity risk both separately (thus allowing an examination without possible collinearity) and together (to understand the relative importance of the SES/race variables compared to each other). Our approach to the selection and analysis of SES/race variables is consistent with the research of Braveman and colleagues (2005) to include all relevant measures of social advantage that assess different, but potentially overlapping, constructs, while considering how unmeasured factors may affect conclusions. Two sensitivity analyses were conducted adjusting for residential density as either a continuous or a categorical variable to evaluate if the relationships between SES/race variables and obesity held after accounting for residential density.
We compared all SES/race variables to determine which ones explained the greatest amount of spatial variability of child obesity between the census tracts. Spatial variability explained by a given variable is defined as spatial variance without the variable minus spatial variance with the variable divided by spatial variance without the variable. Spatial variance is calculated as the sum of the estimated spatial variances from the census tract random variable and adjacent census tract random variable from the CAR multi-level model. Spatial variability explained by a given SES/race variable is approximating how much outcome variability between census tracts is explained by the SES/race variable since spatial variance tends to zero as residual variability across census tracts is explained. All analyses were adjusted for the three child-level covariates (age, sex, and insurance type).
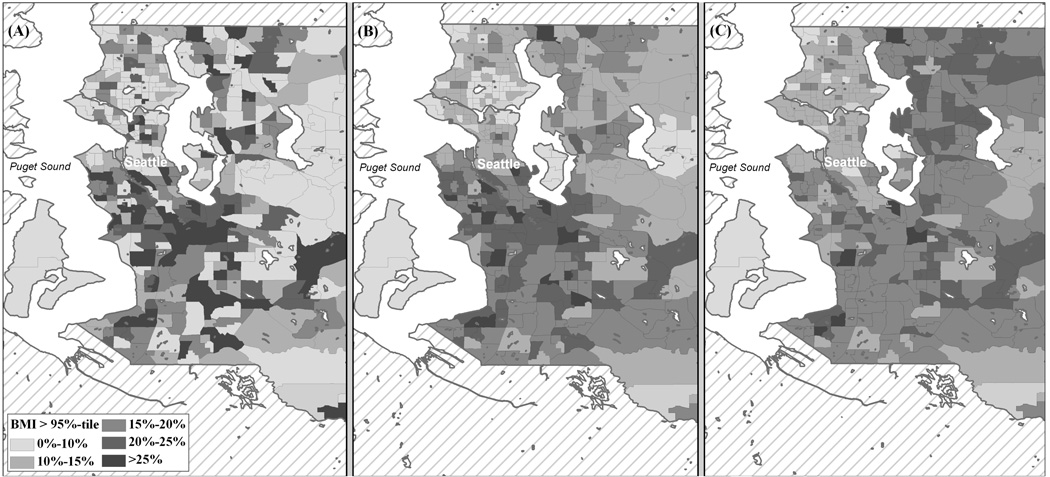
Maps were created from the multi-level models to visually display the observed and predicted probability of child obesity across King Co. census tracts. Predicted probabilities are calculated from the multi-level models for an average census tract by assuming mean covariate values. The maps depict the degree of reduced variation in obesity rates across census tracts after taking into account the spatial correlation and all of the variation of the area-level socioeconomic predictors. The maps were created using ArcGIS 9.1 and shapefiles provided from the 2000 US census.
All data analyses were conducted using the functions glm or bugs from R software, Version 2.5.1, of the R GUI system for Windows (R Development Core Team, 2007) and R package R2WinBugs, Version 2.1.6 (Lunn, Thomas, Best, & Spiegelhalter, 2000; Sturtz, Ligges, & Gelman, 2005). A Bayesian modeling framework was applied with a burn in of 1000, 5000 iterations, and two chains for each model. Two-sided statistical tests with p-values < 0.05 were considered statistically significant.
Results
The population included in the analyses had a mean age of 12.3 years, 51.9% were male, 3.0% were enrolled in the state-sponsored subsidized insurance and 5.4% in Medicaid, which was comparable to the excluded population mean age of 11.6 years, 50.3% male, 3.4% with state-sponsored subsidized insurance and 4.7% with Medicaid. Demographic and BMI characteristics of the children included as study subjects are presented in Table 1. Thirteen percent of girls and 17% of boys had BMI ≥ 95th percentile (obese). Boys had higher odds of being obese compared to girls. No differences in obesity were found by age. Children who had Medicaid health insurance had higher odds of being obese, compared to children with commercial insurance.
Table 1.
Prevalence and odds ratios of obesity (≥95th percentile) by demographic characteristics among children receiving carea (n=8,616)
| N (%) | Proportion Obese |
ORb |
(95% CI) | ||
|---|---|---|---|---|---|
| Sex | |||||
| Female | 4143 (48) | 0.13 | 1 | ||
| Male | 4473 (52) | 0.17 | 1.27 | (1.13, 1.43) | |
| Age (years) | |||||
| 6–11 | 3306 (38) | 0.15 | 1 | ||
| 12–18 | 5310 (62) | 0.15 | 0.99 | (0.87, 1.12) | |
| Insurancec | |||||
| Commercial | 7860 (91) | 0.15 | 1 | ||
| State-sponsored | |||||
| subsidized | 260 (3) | 0.15 | 1.00 | (0.71, 1.42) | |
| Medicaid | 496 (6) | 0.23 | 1.75 | (1.40, 2.17) | |
6 to 18 year old children receiving medical care at the health plan in King County, WA
Odds ratios of obesity by demographic characteristic (referent group OR = 1)
Insurance generally corresponds to tiers of household income: commercial insurance = higher income families receiving insurance through employment; state-sponsored subsidized = low-middle income families that do not qualify as poor; Medicaid = lowest income families in poverty qualifying for government insurance
Census tract SES/race characteristics of King County, WA compared to the average across the United States are presented in Table 2. The population of King Co. in 2000 was 76.4% white, similar to the national mean of 75.1%. Compared to national means, King County had higher median household incomes and a lower percent of adult females with a high school education or less, but the percentage of single parent households was similar. The excluded group census tract demographic variables means were similar to the analysis population ($59,118 median household income, 72.9% white, 67.5% home owners, 32.4% with females with a high school education or less, and 26.0% single parent households).
Table 2.
King Co., WA census tract characteristics compared with U.S. census tract averages (n = 8,616)
| King County | U.S. | ||
|---|---|---|---|
| Census tract variable | Mean | (SD) | Meana |
| Median household income (U.S. dollars) | 57,236 | (19,533) | 41,994 |
| Home ownership, % | 62.8 | (22.38) | 66.2 |
| Females with ≤ high school education, % | 30.4 | (14.44) | 48.9 |
| Single parent household, % | 27.1 | (12.36) | 28.2 |
| White, % | 76.4 | (16.21) | 75.1 |
Values from US Census not aggregated by census tract
The DIC and spatial variance for each of the multi-level models are presented in Table 3. Each census tract SES/race variable in the model resulted in lower DIC (better model fit), and explained more variability. Among the five census tract variables examined, median income had the lowest DIC and corresponding reduction in spatial variability. The model including all five variables resulted in the lowest DIC and explained 23.8% of variability (reduction in spatial variance estimate from .411 to .313).
Table 3.
| Model | Model Choice Criterion DIC |
Spatial Variance | |
|---|---|---|---|
| σ2 | (95% CI) | ||
| Spatial Multi-level Models | |||
| No Spatial Structure | 7309.0 | ||
| Census Tract Only | 7199.5 | ||
| Conditional Autoregressive Regression (CAR) | 7160.6 | 0.414 | (0.281, 0.588) |
| Covariate Adjustment with CAR Multi-level Model | |||
| Individual Predictors | 7143.9 | 0.411 | (0.276, 0.596) |
| Individual + Each Census Tract Variable | |||
| Median income ($US) | 7126.2 | 0.318 | (0.219, 0.444) |
| Home ownership, % | 7140.5 | 0.385 | (0.264, 0.565) |
| Female with ≤ high school education, % | 7128.3 | 0.328 | (0.225, 0.476) |
| Single parent family households, % | 7130.2 | 0.344 | (0.236, 0.486) |
| White, % | 7137.0 | 0.370 | (0.253, 0.543) |
| Individual + All Census Variables | 7123.1 | 0.313 | (0.215, 0.458) |
Low Deviance Information Criteria (DIC) indicates best model fit
σ2 is the total spatial variance equal to σ2 due to census track variability + σ2 due to neighboring census track variability
Table 4 presents logistic regression models assessing the relationship between risk of obesity and each census level SES/race variable separately, adjusting for child-level demographic factors and for spatial correlation. All SES/race variables were significantly (p<.05) associated with the risk of obesity in an expected direction. There were increased odds of child obesity for each $10,000 decrease in median household income and 10% decrease in percent of home owners and for each 10% increase in percentage of females with high school education or less, single parent households, and non-white race.
Table 4.
Odds ratios for child obesity associated with single census tract SES/race variables in adjusted spatial models (n = 8,616)
| Census tract variable | OR | (95% CI) |
|---|---|---|
| Median household income ($10,000 decrease) | 1.17 | (1.11,1.24) |
| Home ownership (10% decrease) | 1.07 | (1.02,1.11) |
| Females with ≤ high school education (10% increase) | 1.24 | (1.15,1.35) |
| Single parent households (10% increase) | 1.22 | (1.13,1.33) |
| Non-white race (10% increase) | 1.12 | (1.05,1.20) |
Each variable analyzed separately, adjusted for child’s age, sex, and health plan and accounting for spatial correlation
All ORs statistically significant, p-value < .05
A multivariable model including spatial correlation and all five census tract-level SES/race variables is presented in Table 5. In this model, child-level characteristics significantly associated with obesity were male sex and Medicaid insurance. A lower census tract median household income was associated with an increased risk of child obesity as in the model examining SES/race variables separately; however, a decrease in percent home ownership was associated with lower risk of child obesity when accounting for the other SES/race variables. These relationships were not changed after adjusting for residential density (data not shown). Residential density was not predictive of obesity alone or in the multivariable analysis.
Table 5.
Odds of obesity in multivariable spatial model including all child and census tract variables (n = 8,616)
| Model | OR | (95% CI)a |
|---|---|---|
| Individual | ||
| Gender | ||
| Female | 1 | -- |
| Male | 1.29 | (1.14, 1.45) |
| Age | ||
| 6–11 | 1 | -- |
| 12–18 | 0.99 | (0.87, 1.12) |
| Insurance | ||
| Commercial (employer-provided) | 1 | -- |
| State-sponsored subsidized (low-middle income) | 0.84 | (0.58, 1.19) |
| Medicaid (government insurance for lowest income) | 1.34 | (1.05, 1.71) |
| Census Tract Variables | ||
| Median income ($10,000 decrease) | 1.15 | (1.03, 1.29) |
| Home ownership (10% decrease) | 0.92 | (0.85, 1.00) |
| Females with ≤ high school education (10% increase) | 1.07 | (0.96, 1.21) |
| Single parent households (10% increase) | 1.12 | (0.97, 1.28) |
| Non-white race (10% increase) | 1.01 | (0.94, 1.09) |
Bold indicates significant (α-level <0.05)
The Figure panels depict maps of the degree of geographic variability in King Co. for rates of child obesity after implementing successive spatial models to explain variability. Panel A shows the observed rates of obesity by census tract without adjustment for spatial correlation or child-level variables. Panel B shows that some variability is explained by adjusting for child-level variables and spatial structure. Panel C, which additionally adjusts for census tract SES/race variables, shows that more variability (but not all), is explained. If census tract socioeconomic variables explained all of the variability between census tracts, then the map in Panel C would be a single color, with no additional spatial variability of obesity remaining.
Discussion
We found significant associations between multiple measures of lower neighborhood social advantage and increased risk of child obesity using objective measures of child weight and height and accounting for child-level factors. We used robust spatial analyses that accounted for auto-correlation, or the effects of adjacent areas, to create more precise estimates of child obesity risk associated with neighborhood-level factors. Our measures of SES and race of the neighborhood explained 24% of the spatial variability between rates of child obesity across census tracts in King Co., Washington. Our findings confirm and add to previous studies that lower neighborhood SES increases risk for overweight beginning in childhood (Janssen et al., 2006; Nelson et al., 2006; Oliver & Hayes, 2005; Shrewsbury & Wardle, 2008).
Examined separately, all of the census tract-level SES/race variables were significantly related to risk of obesity in the expected direction. That is, odds of obesity increased by 7–24% (ORs ranging from 1.07–1.24) for each $10,000 decrease in household income and for each 10% change in the SES variables examined (lower homes owned, lower female education, more single parent households), and more non-white race.
In our fully adjusted spatial model that included all census tract socioeconomic and race variables, higher household incomes in the census tract remained associated with lower obesity as expected; however, higher percent home ownership was paradoxically associated with an increased risk of obesity. Percent home ownership is strongly related to median income (correlation .83) therefore it is not surprising that increased home ownership in the separate (bivariable) model is associated with lower obesity prevalence similar to increased median income. After adjusting for median household income in our full model, the home ownership variable may take on new meaning for the census tract, perhaps representing newer development areas with affordable housing but potentially more obesogenic factors. Lack of significance for the other SES/race variables in the full regression models may reflect collinearity. Given this limitation, we recognize that individual point estimates generated by the full multivariable model should be interpreted with caution.
Our use of multiple SES/race indicators is consistent with recommendations to broaden the measures of social advantage (Braveman, 2006). It is noteworthy that in the Conditional Autoregressive Regression (CAR) spatial analyses, the best fitting model (lowest DIC) which explained the most spatial variability in child obesity included all SES/race variables; that model explained an additional 24% of the variability between census tracts beyond that explained by spatial factors and individual characteristics. It is possible that different aspects of social advantage contribute differently to a child’s energy balance and likelihood of obesity at the individual and neighborhood level.
Our results are consistent with the growing body of evidence for an inverse association between SES and child obesity in developed countries. As summarized by the international review by Shrewsbury and Wardle (Shrewsbury & Wardle, 2008), most prior studies have examined neighborhood SES as a gradient of composite variables (e.g. including neighborhood incomes, education, occupation, and/or others, many defined a priori by government entities). Previously obtained estimated ORs range from 1.26 to 1.95 for low SES compared to high SES (referent) neighborhoods for varying measures of child obesity (Shrewsbury & Wardle, 2008), however these did not have the advantage of using spatial models. Our study expands on this prior work by isolating each SES measure in spatial models, where we found a similar odds ratio magnitude for each variable in association with child overweight and obesity. Our findings are perhaps most readily comparable to Nelson et al. (2006), who examined data from the 1994–1995 U.S. National Longitudinal Study of Adolescent Health among 20,745 7–12th graders and estimated associations between neighborhood income, education, and race/ethnicity for adolescent BMI (using self-report of weight and height) within census block groups. They found a reduced risk of adolescent overweight between high and moderate tertiles of neighborhood median household income (adjusted risk ratio (ARR) of .83 [CI: .71-.98]); and for percent of population with a college education (ARR .74, [CI: .65-.85]) between high and moderate tertiles). They found no differences between low and middle SES tertiles. Unlike our findings for neighborhood race, they found no differences for adolescent weight by neighborhood ethnic minority distribution.
In addition to census tract-level SES and race variables, two child-level variables, male sex and insurance status, were related to child obesity risk in our analysis. Higher obesity rates among male than female children in King County is consistent with sex differences at a national level in the U.S. (Ogden, Carroll, & Flegal, 2008). While children with Medicaid insurance (government-provided insurance for the poorest families) had higher obesity risk compared with commercially insured children in our sample, there was no difference between the insurance groups corresponding to low-middle income and highest income. Several prior studies have found complex relationships between child obesity and SES-related variables (Jansen & Hazebroek-Kampschreur, 1997; Kinra et al., 2000; Nelson et al., 2006; Wardle et al., 2003), such that children in middle SES areas have higher risk than children in the upper SES areas, but no difference in risk between the middle and lowest SES areas. More specific information about the household SES of children (not available for the present study) at each insurance level in our cohort would have helped inform the potential mechanisms for our findings.
Our results provide greater evidence of broad geographically-situated social determinants of obesity among children, as in adults (Drewnowski et al., 2007). While these cross-sectional analyses cannot expose the causal pathway, results are indeed consistent with prior hypothesized relationships as described in the theoretical model provided by Schulz et al. (Schulz et al., 2005). Research identifying differences in mediating pathways for individual and neighborhood measures of SES on health adds evidence to the assertion that neighborhood SES measures in fact represent separate and distinct constructs from individual SES factors, and that both likely need to be addressed in seeking to ameliorate health disparities (van Jaarsveld et al., 2007).
The plausible neighborhood contextual factors that may mediate the SES determinants through environmental variables are now increasingly emerging; a review (Lovasi et al., 2009) of built environment factors related to obesity among disadvantaged populations, defined by poverty and race/ethnicity, found that evidence to-date suggests important factors are access to healthy foods in supermarkets, places to exercise, and neighborhood safety. Future research could expand on emerging studies that test multiple environmental variables (Stafford, Cummins, Ellaway, Sacker, Wiggins, & Macintyre, 2007) to examine how area-level SES influences obesity risk, which is beyond the scope of this study.
Whatever the mechanism by which the area-based SES measures impact child obesity, this association has concerning implications for future health given changing SES factors in the U.S. The census tract variable most highly correlated in our analyses with obesity was average household income level, which has been recognized as one of the most powerful predictors of health and is declining in the U.S. as wealth continues to become concentrated among fewer and fewer people (Woolf, 2007). The cumulative or synergistic effects of income in addition to other neighborhood SES factors likely impact not just obesity but multiple child health outcomes (O'Campo, Burke, Culhane, Elo, Eyster, Holzman et al., 2008; Spilsbury, Storfer-Isser, Kirchner, Nelson, Rosen, Drotar et al., 2006), which may continue into adulthood.
Limitations of this study include the few child/household-level sociodemographic variables available. Adjustment was made for parent insurance type, which provides a proxy for household income, but more precise measures of each child’s household income were not available. Thus, we were unable to fully control for each child’s household income or for other intra-household variables. In addition, we were not able to adjust for parental weight status or child race/ethnicity (Ogden et al., 2006). We are aware that parental weight status may also be influenced by the same neighborhood context. Race/ethnicity has complex interactions with SES with regard to child and adolescent obesity, with some evidence of a decreased gradient in risk of obesity based on SES over time (Wang & Zhang, 2006), but persistent racial disparities particularly for African-American compared to white populations (Gordon-Larsen, Adair, & Popkin, 2003; Robert & Reither, 2004; Wang & Zhang, 2006). We note that while race/ethnicity often defines study of health disparities in the U.S. and thus was included here, it is most relevant to the U.S. as an important measure of social advantage (Braveman, 2006). Race/ethnicity is hypothesized to exert influence on social status primarily through other measures of socioeconomic disparity, namely education and income (Braveman, 2009), which generalize to other countries.
Another limitation was restriction of the population to a single county. Small area-based spatial analyses do offer some advantages in terms of identifying etiologic factors that may be exerting influence on a neighborhood scale (Elliott & Wartenberg, 2004). We note potential for generalizable findings given King County’s overall similar social and economic profile to the U.S. nationally, as well as child obesity rates similar to national levels (Ogden et al., 2006). The U.S. is most comparable to other developed countries, but there may be generalizability to developing countries as well, where lower income families are being affected by obesity particularly in urban settings (Caballero, 2007).
Finally, we were limited to children who had insurance for medical care. We would predict the bias in this case, however, might favor finding a null relationship between area-based social disadvantage and obesity given a potentially more homogeneous healthy child population obtaining routine medical care with medical insurance coverage. Thus, our findings of associations between area-level social disadvantage and obesity in this more socioeconomically advantaged population of children is notable.
Conclusion
Using geocoded data and objective measures of child weight status, this study demonstrated that child obesity was significantly associated with census tract of residence and with multiple specific measures of social disadvantage at the census tract level. These results suggest that social disadvantage in a child’s broader environment, not just a child’s household, may confer risk of obesity. These data also demonstrated more powerful estimates of risk when including data about adjacent census tracts through a spatial analysis smoothing technique, which better characterizes the geographic location of individuals. Census tract social status measures explained 24% of spatial variability between census tracts in child obesity rates. Additional SES characteristics of individuals and neighborhoods not measured here as well as built environment factors may account for census tract variability in risk of child obesity not explained in this study. Further research is needed to characterize results with more comprehensive area-based socio-ecological variables and to understand how neighborhood social disadvantage influences child obesity risk. Potential policy implications of these findings are important: programs targeting individual or family households may have little impact without more comprehensive environmental changes that address social and economic disparities.
Figure.
Unadjusted and adjusted child obesity (≥95th percentile) prevalence by census tract in King Co., WA. A) Unadjusted and no spatial structure; B) Adjusted for individual level covariates and spatial structure; C) Adjusted for both individual and census tract level socioeconomic and race predictors and spatial structure.
Acknowledgments
HMG received salary support from HRSA grant # T32 HP10002 National Research Service Award (NRSA). AJC received salary support from a subcontract of the University of Washington Exploratory Center for Obesity Research, Grant # 5P20RR020774 (Drewnowski), National Institutes of Health Roadmap Initiative.
The authors would like to acknowledge Anne Vernez-Moudon PhD for her assistance in obtaining data.
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
H Mollie Greves Grow, Email: greves@u.washington.edu, University of Washington and Seattle Children's Research Institute, Seattle, WA, USA.
Andrea J Cook, Group Health Research Institute.
David E Arterburn, Group Health Research Institute.
Brian E Saelens, University of Washington and Seattle Children's Research Institute, Seattle, WA, USA.
Adam Drewnowski, University of Washington.
Paula Lozano, University of Washington and Seattle Children's Research Institute, Seattle, WA, USA.
References
- American Medical Association. Expert Committee Recommendations on the Assessment, Prevention, and Treatment of Child and Adolescent Overweight and Obesity. 2007 [Google Scholar]
- Baltrus PT, Everson-Rose SA, Lynch JW, Raghunathan TE, Kaplan GA. Socioeconomic Position in Childhood and Adulthood and Weight Gain over 34 Years: The Alameda County Study. Annals of Epidemiology. 2007;17(8):608–614. doi: 10.1016/j.annepidem.2007.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berke EM, Koepsell TD, Moudon AV, Hoskins RE, Larson EB. Association of the Built Environment With Physical Activity and Obesity in Older Persons. American Journal of Public Health. 2007;97(3):486–492. doi: 10.2105/AJPH.2006.085837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth ML, Macaskill P, Lazarus R, Baur LA. Sociodemographic distribution of measures of body fatness among children and adolescents in New South Wales, Australia. International Journal of Obesity. 1999;23(5):456. doi: 10.1038/sj.ijo.0800841. [DOI] [PubMed] [Google Scholar]
- Braveman P. Health disparities and health equity: concepts and measurement. Annual Review of Public Health. 2006;27:167–194. doi: 10.1146/annurev.publhealth.27.021405.102103. [DOI] [PubMed] [Google Scholar]
- Braveman P. A health disparities perspective on obesity research. Preventing Chronic Disease. 2009;6(3):A91. [PMC free article] [PubMed] [Google Scholar]
- Braveman PA, Cubbin C, Egerter S, Chideya S, Marchi KS, Metzler M, et al. Socioeconomic status in health research: one size does not fit all. Journal of American Medical Association. 2005;294(22):2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- Burke V, Beilin LJ, Dunbar D, Kevan M. Associations between blood pressure and overweight defined by new standards for body mass index in childhood. Preventive Medicine. 2004;38(5):558–564. doi: 10.1016/j.ypmed.2003.09.023. [DOI] [PubMed] [Google Scholar]
- Caballero B. The Global Epidemic of Obesity: An Overview. Epidemiologic Reviews. 2007;29(1):1–5. doi: 10.1093/epirev/mxm012. [DOI] [PubMed] [Google Scholar]
- Cowell JM, Warren JS, Montgomery AC. Cardiovascular risk prevalence among diverse school-age children: implications for schools. Journal of School Nursing. 1999;15(2):8–12. doi: 10.1177/096703359901500201. [DOI] [PubMed] [Google Scholar]
- Cummins S, Curtis S, Diez-Roux AV, Macintyre S. Understanding and representing 'place' in health research: a relational approach. Social Science and Medicine. 2007;65(9):1825–1838. doi: 10.1016/j.socscimed.2007.05.036. [DOI] [PubMed] [Google Scholar]
- Drewnowski A, Rehm C, Kao C, Goldstein H. Poverty and childhood overweight in California Assembly districts. Health & Place. 2009;15(2):631–635. doi: 10.1016/j.healthplace.2008.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A, Rehm CD, Solet D. Disparities in obesity rates: analysis by ZIP code area. Social Science and Medicine. 2007;65(12):2458–2463. doi: 10.1016/j.socscimed.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. American Journal of Clinical Nutrition. 2004;79(1):6–16. doi: 10.1093/ajcn/79.1.6. [DOI] [PubMed] [Google Scholar]
- Elliott P, Wartenberg D. Spatial epidemiology: current approaches and future challenges. Environmental Health Perspectives. 2004;112(9):998–1006. doi: 10.1289/ehp.6735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ells LJ, Campbell K, Lidstone J, Kelly S, Lang R, Summerbell C. Prevention of childhood obesity. Best Practice & Research Clinical Endocrinology & Metabolism. 2005;19(3):441–454. doi: 10.1016/j.beem.2005.04.008. [DOI] [PubMed] [Google Scholar]
- Flynn MAT, McNeil DA, Maloff B, Mutasingwa D, Wu M, Ford C, et al. Reducing obesity and related chronic disease risk in children and youth: a synthesis of evidence with best practice recommendations. Obesity Reviews. 2006;7:7–66. doi: 10.1111/j.1467-789X.2006.00242.x. [DOI] [PubMed] [Google Scholar]
- French SA, Story M, Jeffery RW. Environmental Influences on Eating and Physical Activity. Annual Review of Public Health. 2001;22(1):309–335. doi: 10.1146/annurev.publhealth.22.1.309. [DOI] [PubMed] [Google Scholar]
- Gelman A, Carlin JB, Stern HS, Rubin DB. Bayesian Data Analysis. London: Chapman and Hall; 1995. Chapter 14. [Google Scholar]
- Gordon-Larsen P, Adair LS, Popkin BM. The Relationship of Ethnicity, Socioeconomic Factors, and Overweight in U.S. Adolescents. Obesity Research. 2003;11(1):121–129. doi: 10.1038/oby.2003.20. [DOI] [PubMed] [Google Scholar]
- Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117(2):417–424. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- Jansen W, Hazebroek-Kampschreur A. Differences in height and weight between children living in neighbourhoods of different socioeconomic status. Acta Paediatrica. 1997;86(2):224–225. doi: 10.1111/j.1651-2227.1997.tb08875.x. [DOI] [PubMed] [Google Scholar]
- Janssen I, Boyce WF, Simpson K, Pickett W. Influence of individual- and area-level measures of socioeconomic status on obesity, unhealthy eating, and physical inactivity in Canadian adolescents. American Journal of Clinical Nutrition. 2006;83(1):139–145. doi: 10.1093/ajcn/83.1.139. [DOI] [PubMed] [Google Scholar]
- Kinra S, Nelder RP, Lewendon GJ. Deprivation and childhood obesity: a cross sectional study of 20 973 children in Plymouth, United Kingdom. Journal of Epidemiology and Community Health. 2000;54(6):456–460. doi: 10.1136/jech.54.6.456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital and Health Statistics. Series 11: Data from the National Health Survey. 2002;246:1–190. [PubMed] [Google Scholar]
- Li F, Harmer P, Cardinal BJ, Bosworth M, Johnson-Shelton D. Obesity and the built environment: does the density of neighborhood fast-food outlets matter? American Journal of Health Promotion. 2009;23(3):203–209. doi: 10.4278/ajhp.071214133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovasi GS, Hutson MA, Guerra M, Neckerman KM. Built Environments and Obesity in Disadvantaged Populations. Epidemiologic Reviews. 2009;31(1):7–20. doi: 10.1093/epirev/mxp005. [DOI] [PubMed] [Google Scholar]
- Lumeng JC, Appugliese D, Cabral HJ, Bradley RH, Zuckerman B. Neighborhood Safety and Overweight Status in Children. Archives of Pediatrics and Adolescent Medicine. 2006;160(1):25–31. doi: 10.1001/archpedi.160.1.25. [DOI] [PubMed] [Google Scholar]
- Lunn DJ, Thomas A, Best N, Spiegelhalter D. WinBUGS -- a Bayesian modelling framework: concepts, structure, and extensibility. Statistics and Computing. 2000;10:325–337. [Google Scholar]
- Macintyre S, Ellaway A, Cummins S. Place effects on health: how can we conceptualise, operationalise and measure them? Social Science and Medicine. 2002;55(1):125–139. doi: 10.1016/s0277-9536(01)00214-3. [DOI] [PubMed] [Google Scholar]
- McLaren L. Socioeconomic status and obesity. Epidemiologic Reviews. 2007;29:29–48. doi: 10.1093/epirev/mxm001. [DOI] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual Causes of Death in the United States, 2000. Journal of the American Medical Association. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Correction: Actual Causes of Death in the United States, 2000. Journal of the American Medical Association. 2005;293(3):293–294. doi: 10.1001/jama.293.3.293. [DOI] [PubMed] [Google Scholar]
- Morland K, Diez Roux AV, Wing S. Supermarkets, Other Food Stores, and Obesity: The Atherosclerosis Risk in Communities Study. American Journal of Preventive Medicine. 2006;30(4):333–339. doi: 10.1016/j.amepre.2005.11.003. [DOI] [PubMed] [Google Scholar]
- Nelson MC, Gordon-Larsen P, Song Y, Popkin BM. Built and social environments associations with adolescent overweight and activity. American Journal of Preventive Medicine. 2006;31(2):109–117. doi: 10.1016/j.amepre.2006.03.026. [DOI] [PubMed] [Google Scholar]
- Nelson NM, Woods CB. Obesogenic environments: Are neighbourhood environments that limit physical activity obesogenic? Health & Place. 2009;15(4):917–924. doi: 10.1016/j.healthplace.2009.02.001. [DOI] [PubMed] [Google Scholar]
- Norman GJ, Nutter SK, Ryan S, Sallis JF, Calfras KJ, Patrick K. Community Design and Access to Recreational Facilities as Correlates of Adolescent Physical Activity and Body-Mass Index. Journal of Physical Activity and Health. 2006;3 (Supplement 1):S118–S128. doi: 10.1123/jpah.3.s1.s118. [DOI] [PubMed] [Google Scholar]
- O'Campo P, Burke JG, Culhane J, Elo IT, Eyster J, Holzman C, et al. Neighborhood Deprivation and Preterm Birth among Non-Hispanic Black and White Women in Eight Geographic Areas in the United States. American Journal of Epidemiology. 2008;167(2):155–163. doi: 10.1093/aje/kwm277. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of Overweight and Obesity in the United States, 1999–2004. JAMA. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Flegal KM. High Body Mass Index for Age Among US Children and Adolescents, 2003–2006. JAMA. 2008;299(20):2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- Oliver LN, Hayes MV. Neighbourhood socio-economic status and the prevalence of overweight Canadian children and youth. Canadian Journal of Public Health. 2005;96(6):415–420. doi: 10.1007/BF03405180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell LM, Chaloupka FJ, Bao Y. The availability of fast-food and full-service restaurants in the United States: associations with neighborhood characteristics. American Journal of Preventive Medicine. 2007;33(4 Suppl):S240–S245. doi: 10.1016/j.amepre.2007.07.005. [DOI] [PubMed] [Google Scholar]
- R Development Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2007. ( http://www.R-project.org) [Google Scholar]
- Robert SA, Reither EN. A multilevel analysis of race, community disadvantage, and body mass index among adults in the US. Social Science and Medicine. 2004;59(12):2421–2434. doi: 10.1016/j.socscimed.2004.03.034. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Glanz K. The role of built environments in physical activity, eating, and obesity in childhood. Future of Children. 2006;16(1):89–108. doi: 10.1353/foc.2006.0009. [DOI] [PubMed] [Google Scholar]
- Schulz AJ, Kannan S, Dvonch JT, Israel BA, Allen A, 3rd, James SA, et al. Social and physical environments and disparities in risk for cardiovascular disease: the healthy environments partnership conceptual model. Environmental Health Perspectives. 2005;113(12):1817–1825. doi: 10.1289/ehp.7913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrewsbury V, Wardle J. Socioeconomic Status and Adiposity in Childhood: A Systematic Review of Cross-sectional Studies 1990–2005. Obesity. 2008;16(2):275–284. doi: 10.1038/oby.2007.35. [DOI] [PubMed] [Google Scholar]
- Simon PA, Kwan D, Angelescu A, Shih M, Fielding JE. Proximity of fast food restaurants to schools: do neighborhood income and type of school matter? Preventive Medicine. 2008;47(3):284–288. doi: 10.1016/j.ypmed.2008.02.021. [DOI] [PubMed] [Google Scholar]
- Singh GK, Siahpush M, Kogan MD. Rising Social Inequalities in US Childhood Obesity, 2003–2007. Annals of Epidemiology. 2010;20(1):40–52. doi: 10.1016/j.annepidem.2009.09.008. [DOI] [PubMed] [Google Scholar]
- Smoyer-Tomic KE, Spence JC, Raine KD, Amrhein C, Cameron N, Yasenovskiy V, et al. The association between neighborhood socioeconomic status and exposure to supermarkets and fast food outlets. Health and Place. 2008;14(4):740–754. doi: 10.1016/j.healthplace.2007.12.001. [DOI] [PubMed] [Google Scholar]
- Sobal J, Stunkard AJ. Socioeconomic status and obesity: a review of the literature. Psychological Bulletin. 1989;105(2):260–275. doi: 10.1037/0033-2909.105.2.260. [DOI] [PubMed] [Google Scholar]
- Spiegelhalter DJ, Best NG, Carlin BP, Van der Linde A. Bayesian Measures of Model Complexity and Fit (with Discussion) J Royal Statistical Society, Series B. 2002;64(4):583–616. [Google Scholar]
- Spilsbury JC, Storfer-Isser A, Kirchner HL, Nelson L, Rosen CL, Drotar D, et al. Neighborhood disadvantage as a risk factor for pediatric obstructive sleep apnea. Journal of Pediatrics. 2006;149(3):342–347. doi: 10.1016/j.jpeds.2006.04.061. [DOI] [PubMed] [Google Scholar]
- Stafford M, Cummins S, Ellaway A, Sacker A, Wiggins RD, Macintyre S. Pathways to obesity: identifying local, modifiable determinants of physical activity and diet. Social Science and Medicine. 2007;65(9):1882–1897. doi: 10.1016/j.socscimed.2007.05.042. [DOI] [PubMed] [Google Scholar]
- Sturtz S, Ligges U, Gelman A. R2WinBUGS: A Package for Running WinBUGS from R. J Statistical Software. 2005;12(3):1–16. [Google Scholar]
- Timperio A, Salmon J, Telford A, Crawford D. Perceptions of local neighbourhood environments and their relationship to childhood overweight and obesity. International Journal of Obesity. 2005;29(2):170–175. doi: 10.1038/sj.ijo.0802865. [DOI] [PubMed] [Google Scholar]
- Townshend T, Lake AA. Obesogenic urban form: Theory, policy and practice. Health & Place. 2009;15(4):909–916. doi: 10.1016/j.healthplace.2008.12.002. [DOI] [PubMed] [Google Scholar]
- Truong KD, Sturm R. Weight Gain Trends Across Sociodemographic Groups in the United States. American Journal of Public Health. 2005;95(9):1602–1606. doi: 10.2105/AJPH.2004.043935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. U.S. Census 2000. 2000 http://www.census.gov/main/www/cen2000.html.
- van Jaarsveld CHM, Miles A, Wardle J. Pathways from deprivation to health differed between individual and neighborhood-based indices. Journal of Clinical Epidemiology. 2007;60(7):712–719. doi: 10.1016/j.jclinepi.2006.10.005. [DOI] [PubMed] [Google Scholar]
- Wang Y, Beydoun MA, Liang L, Caballero B, Kumanyika SK. Will All Americans Become Overweight or Obese? Estimating the Progression and Cost of the US Obesity Epidemic. Obesity. 2008;16(10):2323–2330. doi: 10.1038/oby.2008.351. [DOI] [PubMed] [Google Scholar]
- Wang Y, Zhang Q. Are American children and adolescents of low socioeconomic status at increased risk of obesity? Changes in the association between overweight and family income between 1971 and 2002. American Journal of Clinical Nutrition. 2006;84(4):707–716. doi: 10.1093/ajcn/84.4.707. [DOI] [PubMed] [Google Scholar]
- Wardle J, Jarvis MJ, Steggles N, Sutton S, Williamson S, Farrimond H, et al. Socioeconomic disparities in cancer-risk behaviors in adolescence: baseline results from the Health and Behaviour in Teenagers Study (HABITS) Preventive Medicine. 2003;36(6):721–730. doi: 10.1016/s0091-7435(03)00047-1. [DOI] [PubMed] [Google Scholar]
- Weinsier RL, Hunter GR, Heini AF, Goran MI, Sell SM. The etiology of obesity: relative contribution of metabolic factors, diet, and physical activity. The American Journal of Medicine. 1998;105(2):145–150. doi: 10.1016/s0002-9343(98)00190-9. [DOI] [PubMed] [Google Scholar]
- Wen M, Browning CR, Cagney KA. Poverty, affluence, and income inequality: neighborhood economic structure and its implications for health. Social Science and Medicine. 2003;57(5):843–860. doi: 10.1016/s0277-9536(02)00457-4. [DOI] [PubMed] [Google Scholar]
- Woolf SH. Future Health Consequences of the Current Decline in US Household Income. Journal of American Medical Association. 2007;298(16):1931–1933. doi: 10.1001/jama.298.16.1931. [DOI] [PubMed] [Google Scholar]
- Wright CM, Parker L. Forty years on: the effect of deprivation on growth in two Newcastle birth cohorts. International Journal of Epidemiology. 2004;33(1):147–152. doi: 10.1093/ije/dyg187. [DOI] [PubMed] [Google Scholar]