Abstract
The sole FDA-approved treatment for acute stroke is recombinant tissue-type plasminogen activator (rtPA). However, rtPA aggravates the impairment of cerebrovasodilation induced by global hypoxia/ischemia; this impairment is attenuated by the preinjury treatment with the plasminogen activator inhibitor derivative EEIIMD. MAPK (a family of kinases, p38, and JNK) is upregulated after cerebral ischemia. In this study, we determined whether the novel plasminogen activator inhibitor-derived peptide, Ac-RMAPEEIIMDRPFLYVVR-amide, (PAI-1-DP) given 30 min before or 2 h after, focal central nervous system injury induced by photothrombosis would preserve responses to cerebrovasodilators and the role of p38 and JNK MAPK in such effects. Cerebrospinal fluid JNK and p38 levels were elevated by photothrombotic injury, an effect potentiated by rtPA. Cerebrovasodilation was blunted by photothrombosis and reversed to vasoconstriction by rtPA but restored to dilation by PAI-1-DP pre- and posttreatment. PAI-1-DP blocked JNK, but preserved p38 MAPK upregulation after photothrombosis. The JNK MAPK antagonist SP600125 prevented, and the p38 antagonist SB203580 potentiated, impaired cerebrovasodilation after photothrombosis. These data indicate that rtPA impairs cerebrovasodilation after injury by activating JNK, while p38 MAPK is protective, and that the novel peptide PAI-1-DP protects by inhibiting activation of JNK by rtPA. JNK MAPK inhibitors, including PAI-1-DP, may offer a novel approach to increase the benefit-to-risk ratio of thrombolytic therapy and enable its use in central nervous system ischemic disorders.
Keywords: cerebral circulation, newborn, plasminogen activators, signal transduction
endogenous and exogenous plasminogen activators have the potential to be injurious in the setting of occlusive stroke (5, 15, 16, 19, 22). Mechanisms for neuronal toxicity are unclear but may include matrix metalloproteases that disrupt the blood-brain barrier (20) and activation of MAPK, a family of at least three kinases (ERK, p38, and JNK) (12) upregulated by matrix metalloproteases after brain injury (21). Recombinant tissue-type plasminogen activator (rtPA) also activates glutamate receptors (15), which augment dilation of the cerebral vasculature in nonischemic areas, thereby potentially reducing blood flow to the penumbra (13). Impaired cerebral hemodynamics may contribute to neuronal cell integrity in the context of the neurovascular unit (2).
tPA is a serine protease that cleaves the zymogene plasminogen to produce the active serine protease plasmin. In the intravascular compartment, blood clots are formed from the aggregation of platelets and formation of fibrin meshwork from fibrinogen. Fibrinolysis is achieved by plasmin generated chiefly through the action of tPA. Termination of tPA catalytic activity is produced by binding of serine protease (serpin) inhibitors, chiefly the plasminogen activator inhibitor-1 (PAI-1). Inactive tPA/PAI-1 complexes are cleared from the circulation by low-density receptor-related protein. Plasminogen activators may also initiate intracellular signaling by binding to the low-density receptor-related protein (7, 14), through pathways that are independent of its catalytic activity (4, 13). Signaling can be inhibited by a hexapeptide, EEIIMD, derived from PAI-1 (1, 4, 13). The peptide interacts with the PAI-1 docking site in tPA, which lies outside of its catalytic center and therefore does not affect its capacity to activate its physiological substrate plasminogen to inhibit fibrinolysis (5, 13). This peptide provides neuroprotection against endogenous and exogenous rtPA in models of stroke and traumatic brain injury (5, 18). Recent studies show that a novel 18 amino acid PAI-1 derivative based on this peptide, Ac-RMAPEEIIMDRPFLYVVR-amide (PAI-1-derived peptide; PAI-1-DP), may extend the therapeutic time window for improved outcome in mechanical and thromboembolic models of stroke (9).
The plasminogen activator system is involved in impairment of cerebrovasodilation in response to hypercapnia and hypotension after global cerebral hypoxia/ischemia in an low-density receptor-related protein and ERK MAPK dependent process, which can be largely prevented by pretreatment with EEIIMD (2, 3). However, we have not yet investigated the more clinically relevant paradigm involving the posttreatment of a PAI-1 to produce protection of cerebrovasodilation when given after induction of injury. Additionally, our mechanistic studies to date have not considered the possibility that a shift in the MAPK isoform profile (e.g., change in p38, JNK, and/or ERK MAPK) may ultimately link EEIIMD to improved cerebral hemodynamics following CNS injury. Additionally, the role of rtPA in impaired cerebral hemodyanmics and its mechanism may be different in global, compared with focal, cerebral ischemia injury models.
In this study, we therefore determined whether the novel PAI-1-DP, given 30 min before or 2 h after induction of focal injury through photothrombosis, would preserve responses to cerebrovasodilators and the role of p38, JNK, and ERK MAPK in such effects.
MATERIALS AND METHODS
Closed cranial window technique and cerebral photothrombosis.
Newborn pigs (1–5 days, 1.0–1.6 kg) of either sex were studied. All protocols were approved by the University of Pennsylvania Institutional Animal Care and Use Committee. Animals were sedated with isoflurane (1–2 mean alveolar concentration). Anesthesia was maintained with a-chloralose (30–50 mg/kg supplemented with 5 mg·kg−1·h−1 iv). Catheters were inserted into femoral arteries and veins, while the trachea was cannulated for ventilation with room air. The closed cranial window technique was used to measure pial artery diameter and collect cerebrospinal fluid (CSF) for ELISA analysis (2). For sample collection, 300 μl of the total cranial window volume of 500 μl was collected by slowly infusing artificial CSF into one side of the window and allowing the CSF to drip freely into a collection tube on the opposite side.
Induction of photothrombosis was based on that described for the newborn pig (11), but in our studies we used the area of the closed cranial window to expose two to three main and one to three smaller arteries supplying the middle cerebral artery territory. Arterial occlusion was achieved by photothrombosis in which a stable thrombus, consisting of aggregating platelets, fibrin, and other blood components, is formed in response to endothelial peroxidative damage. The photochemical reaction occurs due to interaction of intravenous photosensitizing dye erythrosine B (20 mg/kg iv) and the focused beam of a solid-state laser operated at 532 nm, power of 200 mW, average intensity of 60–75 W/cm2, and durations of up to 3–5 min using a Snake Creek minilaser (Hallstead, PA).
Hypotension was induced by the rapid withdrawal of either 5–8 or 10–15 ml blood/kg to induce moderate or severe hypotension (decreases in mean arterial blood pressure of 25 and 45%, respectively). Such drops in blood pressure were maintained constant for 10 min by titration of additional blood withdrawal or blood reinfusion. Two levels of hypercapnia (low and high) were induced via inhalation of graded levels of a 10% CO2-21% O2-balance N2 gas mixture for 10 min to produce levels of Pco2 of 50–60 mmHg for the low exposure and 70–80 mmHg for the high exposure.
Protocol.
Two types of pial vessels, small arteries (resting diameter, 120–160 μm) and arterioles (resting diameter, 50–70 μm) were examined to determine whether segmental differences in the effects of photothrombosis could be identified. Fifteen experimental protocols were studied in 15 separate groups of animals (each group: n = 5): 1) sham control, vehicle treated; 2) photothrombosis, vehicle pretreated; 3) photothrombosis pretreated with rtPA (2 mg/kg iv); 4) photothrombosis pretreated with PAI-1-DP (1 mg/kg iv); 5) photothrombosis pretreated with ERK-antagonist U0126 (1 mg/kg iv); 6) photothrombosis pretreated with p38-antagonist SB203580 (1 mg/kg iv); 7) photothrombosis pretreated with JNK-antagonist SP600125 (1 mg/kg iv); 8) photothrombosis pretreated with D-JNKI1(1 mg/kg iv); 9) photothrombosis vehicle posttreated; 10) photothrombosis posttreated with rPA (2 mg/kg iv); 11) photothrombosis posttreated with PAI-1-DP (1 mg/kg iv); 12) photothrombosis posttreated with U0126 (1 mg/kg iv); 13) photothrombosis posttreated with SB203580 (1 mg/kg iv); 14) photothrombosis posttreated with SP600125 (1 mg/kg iv); and 15) photothrombosis posttreated with D-JNKI1 (1 mg/kg iv). Pretreatment time was 30 min prior to insult, while posttreatment time was 2 h postinsult. The vehicle for all agents was 0.9% saline, except for the PAI-1-DP (50% ethanol and 50% 0.9% saline), and U0126, SB203580, and SP600125, which used dimethyl sulfoxide (100 μl) diluted with 9.9 ml 0.9% saline. In sham control and photothrombotic animals, responses to hypercapnia, hypotension, and isoproterenol (10−8, 10−6 M) were obtained initially and then again 1 and 4 h later in the presence of vehicle. In drug-treated photothrombotic animals, drugs were administered either 30 min before or 2 h after injury, and the insult protocol followed. Pial artery reactivity was determined in pial small arteries and arterioles close to the area of injury (peri-ischemic area). Pial artery reactivity data were quantified by determining the diameter in the absence and presence of the agonist and dividing that numeric difference by baseline diameter to allow display of data as a percent of baseline diameter. Doses of antagonists used in this study were chosen based on efficacy and selectivity data from our prior published studies (2). Confirmation of clot formation with photothrombosis and recanalization with rtPA within damaged pial arteries was made visually through the closed cranial window. These data were quantified through use of radiolabeled microspheres, which showed a reduction in cerebral blood flow with photothrombosis (68 ± 8 to 30 ± 5 ml·min−1·100 g−1, n = 5) and a corresponding hyperemia with tPA administration in the peri-ischemia area (32 ± 3 to 77 ± 6 ml·min−1·100 g−1, n = 5).
ELISA.
Commercially available ELISA kits were used to quantity CSF ERK, p38, and JNK MAPK (Assay Designs, EMD Chemicals) concentration. Phosphorylated MAPK isoform enzyme values were normalized to the sum total of the isoforms and then expressed as a percent of the total.
Statistical analysis.
Pial artery diameter, CSF ERK, p38, and JNK MAPK values were analyzed using ANOVA for repeated measures. If the value was significant, the data were then analyzed by Fishers protected least significant difference test. An α-level of P < 0.05 was considered significant in all statistical tests. Values are represented as means ± SE of the absolute value or as percentage changes from control value.
RESULTS
Influence of the PAI-1-DP, MAPK inhibitors, and photothrombosis on pial artery diameter.
The PAI-1-DP, U0126, SB203580, SP600125, and D-JNKI1 all had no significant effect on pial artery diameter. The PAI-1-DP (1 mg/kg iv) blocked pial artery dilation in response to rtPA (2 mg/kg iv). Photothrombosis reduced baseline pial artery diameter by 18 ± 3%.
Blood chemistry.
Blood chemistry values were collected before and after all experiments. There were no statistically significant differences among groups. Low levels of hypercapnia raised Pco2 to 59 ± 8 and high levels of hypercapnia raised Pco2 to 79 ± 9 mmHg. Oxygen levels were kept constant during periods of hypercapnia.
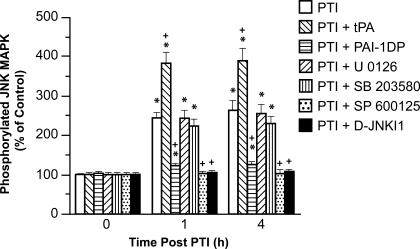
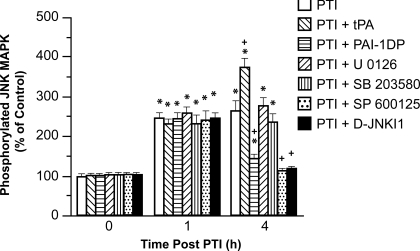
PAI-1-DP blocks, whereas tPA augments, photothrombosis-induced phosphorylation of JNK MAPK.
The activation (phosphorylation) state of the JNK MAPK isoform was determined by expressing the data as a percent of control (total). Photothrombosis induced a marked phosphorylation of JNK MAPK within 1 h postinjury (Figs. 1 and 2). Exogenous tPA administered 30 min prior to or 2 h after photothrombosis potentiated phosphorylation of JNK MAPK (Figs. 1 and 2). In contrast, administration of the PAI-1-DP pre- or postinjury blocked insult-induced phosphorylation of CSF JNK MAPK. Notably, the PAI-1-DP not only blocked the potentiation of CSF JNK MAPK release observed with tPA, but almost completely restored the values to those measured under sham control conditions (Figs. 1 and 2). SP600125 and D-JNKI1 (1 mg/kg iv), purported JNK MAPK antagonists, blocked JNK MAPK phosophorylation, (Figs. 1 and 2), while having no effect on p38 MAPK (Figs. 3 and 4) or ERK MAPK (data not shown).
Fig. 1.
Pretreatment phosphorylation of JNK MAPK in cerebrospinal fluid (CSF) prior to photothrombotic injury (PTI) (0 min) and as a function of time (hour) after PTI in vehicle or pretreated with recombinant tissue-type plasminogen activator (rtPA; 2 mg/kg iv), Ac-RMAPEEIIMDRPFLYVVR-amide [PAI-1-derived peptide (PAI-1-DP)], U0126, SB203580, SP600125, or D-JNKI1 (ERK, p38, and JNK MAPK inhibitors, all 1 mg/kg iv), n = 5 per group. Data are expressed as %control by ELISA determination of phospho-MAPK and total MAPK isoforms and subsequent normalization to total form. Pretreatment was 30 min before PTI. *P < 0.05 vs. corresponding time 0; +P < 0.05 vs. corresponding PTI-nontreated value.
Fig. 2.
Posttreatment phosphorylation of JNK MAPK in CSF prior to PTI (0 min) and as a function of time (hour) after PTI in vehicle, or posttreated with rtPA (2 mg/kg iv), PAI-1-DP, U0126, SB203580, SP600125, or D-JNKI1 (ERK, p38, and JNK MAPK inhibitors, all 1 mg/kg iv), n = 5 per group. Data expressed as %control by ELISA determination of phospho-MAPK and total MAPK isoforms and subsequent normalization to total form. Posttreatment time was 2 h after PTI. *P < 0.05 vs. corresponding time 0 value; +P < 0.05 vs. corresponding PTI nontreated value.
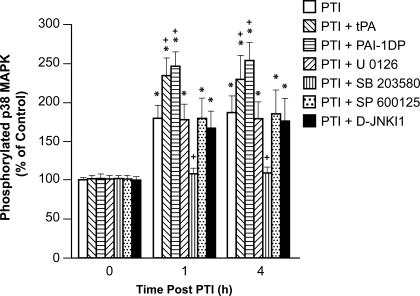
Fig. 3.
Pretreatment phosphorylation of p38 MAPK in CSF prior to PTI (0 min) and as a function of time (hour) after PTI in vehicle, or pretreated with rtPA (2 mg/kg iv), PAI-1-DP, U0126, SB203580, SP600125, or D-JNKI1 (ERK, p38, and JNK MAPK inhibitors, all 1 mg/kg iv), n = 5 per group. Data expressed as %control by ELISA determination of phospho-MAPK and total MAPK isoforms and subsequent normalization to total form. Pretreatment was 30 min before PTI. *P < 0.05 vs. corresponding time 0 value; +P < 0.05 vs. corresponding PTI nontreated value.
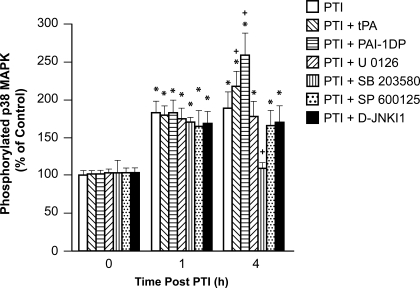
Fig. 4.
Posttreatment phosphorylation of p38 MAPK in CSF prior to PTI (0 min) and as a function of time (hour) after PTI in vehicle, or posttreated with rtPA (2 mg/kg iv), PAI-1-DP, U0126, SB203580, SP600125, or D-JNKI1 (ERK, p38, and JNK MAPK inhibitors, all 1 mg/kg iv), n = 5 per group. Data expressed as %control by ELISA determination of phospho-MAPK and total MAPK isoforms and subsequent normalization to total form. Posttreatment time was 2 h after PTI. *P < 0.05 vs. corresponding time 0 value; +P < 0.05 vs. corresponding PTI nontreated value.
Photothrombosis increases p38 MAPK, which is potentiated by tPA and preserved by the PAI-1-DP.
Photothrombosis elevated CSF p38 MAPK, which was potentiated by tPA, and the increase was maintained in the presence of the PAI-1-DP (Figs. 3 and 4). SB203580 (1 mg/kg iv), a p38 MAPK antagonist, blocked injury-induced elevation of CSF p38 MAPK (Figs. 3 and 4), while having no effect on JNK MAPK (Figs. 1 and 2) or ERK MAPK (data not shown).
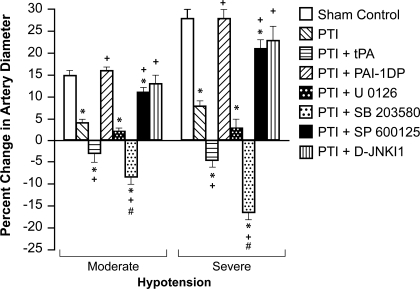
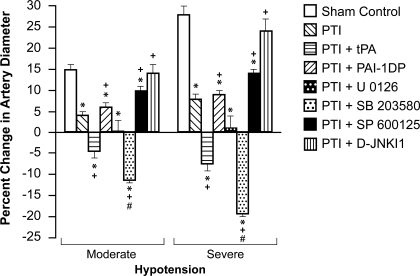
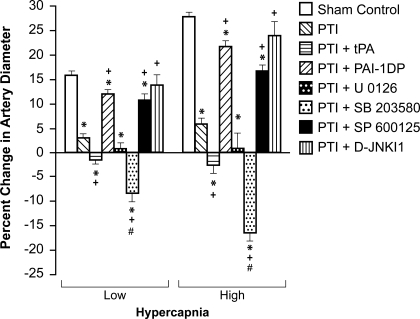
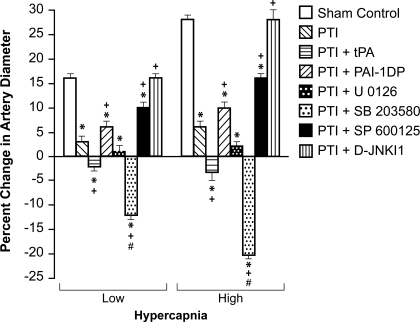
PAI-1-DP prevents, whereas tPA aggravates, photothrombosis-induced impairment of hypercapnic and hypotensive cerebrovasodilation.
Hypotension, hypercapnia, and isoproterenol elicited reproducible dilation of pial small arteries and arterioles. Dilation of small pial arteries in response to hypotension and hypercapnia was blunted after photothrombosis, and further reversed to vasoconstriction in pigs treated before (30 min) or after (2 h) insult with rtPA (2 mg/kg iv) (Figs. 5, 6, 7, and 8). In contrast, dilation was fully protected in animals given the PAI-1-DP (1 mg/kg iv) preinsult (Figs. 5–8). Postinsult administration of the PAI-1-DP partially restored pial artery dilation to hypercapnia and hypotension (Figs. 5–8). Vasodilation was also fully maintained by either pre- or posttreatment with the more cell-permeable JNK antagonist D-JNKI1 (1 mg/kg iv), and nearly fully protected by SP600125 (1 mg/kg iv) (Figs. 5–8). However, the p38 MAPK inhibitor SB203580 (1 mg/kg iv) potentiated impaired cerebrovasodilation in response to hypercapnia and hypotension after photothrombosis (Figs. 5–8). Impaired vasodilation in response to hypercapnia and hypotension observed after photothrombosis was unchanged by U0126 (1 mg/kg iv). Vasodilation of small pial arteries in response to isoproterenol was unaffected by photothrombosis, rtPA, the PAI-1-DP, and MAPK inhibitors. For example, isoproterenol (10−8, 10−6 M) produced 15 ± 1 and 26 ± 1%, 16 ± 1 and 27 ± 2%, and 16 ± 2 and 25 ± 2% dilation under sham control, photothrombosis, and photothrombosis+rtPA conditions, respectively. Similar observations were made in pial arterioles.
Fig. 5.
Pretreatment influence of hypotension (moderate, severe) on pial artery diameter in newborn pigs before (control), after PTI, or pretreated with rtPA (2 mg/kg iv), PAI-1-DP, U0126, SB203580, SP600125, or D-JNKI1 (ERK, p38, and JNK MAPK inhibitors, all 1 mg/kg iv), n = 5 per group. Pretreatment time was 30 before PTI. *P < 0.05 vs. corresponding control value; +P < 0.05 vs. corresponding nontreated PTI value; #P < 0.05 vs. corresponding PTI+rtPA value.
Fig. 6.
Posttreatment influence of hypotension (moderate, severe) on pial artery diameter in newborn pigs before (control), after PTI, or posttreated with rtPA (2 mg/kg iv), PAI-1-DP, U0126, SB203580, SP600125, or D-JNKI1 (ERK, p38, and JNK MAPK inhibitors, all 1 mg/kg iv), n = 5 per group. Posttreatment time was 2 h after PTI. *P < 0.05 vs. corresponding control value; +P < 0.05 vs. corresponding nontreated PTI value; #P < 0.05 vs. corresponding PTI+rtPA value.
Fig. 7.
Pretrement influence of hypercapnia (Low, High) on pial artery diameter in newborn pigs before (control), after PTI, or pretreated with rtPA (2 mg/kg iv), PAI-1-DP (PAI-1-DP), U0126, SB203580, SP600125 or D-JNKI1 (ERK, p38, and JNK MAPK inhibitors, all 1 mg/kg iv), n = 5 per group. Pretreatment time was 30 before PTI. *P < 0.05 vs. corresponding control value; +P < 0.05 vs. corresponding nontreated PTI value; #P < 0.05 vs. corresponding PTI +rtPA value.
Fig. 8.
Posttreatment influence of hypercapnia (Low, High) on pial artery diameter in newborn pigs before (control), after PTI, or posttreated with rtPA (2 mg/kg iv), PAI-1-DP, U0126, SB203580, SP600125, or D-JNKI1 (ERK, p38, and JNK MAPK inhibitors, all 1 mg/kg iv), n = 5 per group. Posttreatment time was 2 h after PTI. *P < 0.05 vs. corresponding control value; +P < 0.05 vs. corresponding nontreated PTI value; #P < 0.05 vs. corresponding PTI +rtPA value.
DISCUSSION
There are two principal new findings from this study. First, these data show that cerebrovasodilation in response to hypercapnia and hypotension, which was blunted by photothrombosis and reversed to vasoconstriction by rtPA, was fully restored to dilation by the intravenous preinjury treatment with the novel PAI-1-DP, PAI-1-DP. Second, blockade of JNK MAPK and preservation of p38 MAPK upregulation maintained vasodilation in animals given the PAI-1-DP. Prior studies involved local application of a hexapeptide derived from PAI-1, EEIIMD, to the brain surface prior to global cerebral hypoxia/ischemia and achieved only partial cerebrovasodilator protection (3).
New data in the present study show that postinjury administration of the PAI-1-DP similarly achieves partial protection of dilation in response to hypercapnia and hypotension, thereby making the present results translationally relevant. The observation that the PAI-1-DP preserves cerebrovasodilation, whether given pre- or postphotothrombosis, suggests its potential utility both as a treatment for cerebral ischemia and a means to prevent delayed injury in settings where the risk of recurrent ischemic occlusion is high (prophylaxis). While global cerebral hypoxia/ischemia can certainly occur as a consequence of stroke, the injury methodology we employed in the present study extends the implications of these findings to disorders characterized by focal CNS ischemia. The protection afforded by the PAI-1-DP appears selective, since vasodilation in response to isoproterenol was unchanged by both this peptide and photothrombosis.
The second major finding of this study is that blockade of JNK MAPK and preservation of p38 MAPK upregulation maintained vasodilation to hypercapnia and hypotension in animals given the PAI-1-DP. These data suggest that upregulation of JNK MAPK is deleterious, while induction of p38 MAPK is protective in the setting of focal thrombotic ischemia. A shift in the MAPK isoform profile by the PAI-1-DP, therefore, appears to contribute to improved cerebrovasodilator responsiveness postinsult. It is important to note that CSF ERK MAPK was unchanged and U0126 was not protective after photothrombosis, in contrast to their effect in the setting of global cerebral hypoxia/ischemia (2). These data suggest that global and focal ischemia may utilize different signaling pathways to impair cerebral hemodynamics. Because JNK MAPK antagonists blocked JNK upregulation postinjury, while having no effect on p38 or ERK, these data, conducted as part of a cross-selectivity paradigm, support the efficacy and specificity of these agents as probes for the role of JNK MAPK in hemodynamic effects of photothrombosis.
Previous findings indicate that upregulation of JNK MAPK contributes to neuronal cell death in a rodent model of focal middle cerebral artery occlusion (6). Our data are the first to investigate the role of this MAPK isoform in impaired cerebral hemodynamics. A limitation of the closed cranial window technique to quantify CSF MAPK concentration is that the cellular site of origin cannot be determined. Potential sources include neurons, glia, vascular smooth muscle, and endothelial sources. We were nonetheless somewhat surprised to detect MAPK in CSF because it more traditionally is thought of as being localized exclusively intracellularly. However, our recent studies indicate that quantification of ERK MAPK in CSF appears to parallel changes in brain parenchyma under hypoxic/ischemic conditions (2), thereby suggesting that presence of such signaling molecules in CSF reflects intracellular-mediated events.
Many studies of cerebral ischemia have been performed in rodent models. Piglets offer a unique advantage in elucidating pathways involved in CNS ischemic injury by virtue of having a gyrencepahalic brain that contains substantial white matter similar to humans, which is more sensitive to ischemic damage than grey matter (17). On the basis of interspecies extrapolation of brain growth curves (8), the age of the newborn pig used in these studies roughly approximated the newborn-infant time period in the human. Although the incidence of cerebral ischemic events in the pediatric population is relatively low compared with the adult (10), the magnitude of the condition is amplified by the potential long-term loss of quality of life years for children with CNS ischemic disorders. Many individual children, however, are receiving rtPA based on the assumption that studies in adults are generalizable to children. The data from this study provide additional evidence that both safety and efficacy of rtPA must be evaluated systematically in children before being widely adopted in clinical care.
Perspectives and Significance
In summary, these data indicate that tPA impairs cerebrovasodilation after photothrombosis through JNK, while activation of p38 MAPK is protective. These data suggest that a novel PAI-1-DP protects against impairment of cerebrovasodilation after photothrombosis through inhibition of JNK and preservation of p38 MAPK. JNK MAPK inhibitors and the PAI-1-DP may provide a novel approach to increase the benefit-to-risk ratio of thrombolytic therapy used in treating disorders involving CNS ischemia.
GRANTS
This research was supported by National Institutes of Health Grants NS-53410 and HD-57355 (to W. M. Armstead), HL-76406, CA-83121, HL-76206, HL-07971, and HL-81864 (to D. B. Cines), and HL-77760 and HL-82545 (to A. A. R. Higazi); and by grants from the University of Pennsylvania Research Foundation (to W. M. Armstead), the University of Pennsylvania Institute for Translational Medicine and Therapeutics (to D. B. Cines), and the Israeli Science Foundation (to A. A. R. Higazi).
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
REFERENCES
- 1.Akkawi S, Nassar T, Tarshis M, Cines DB, Higazi AAR. LRP and avB3 mediate tPA- activation of smooth muscle cells. Am J Physiol Heart Circ Physiol 291: H1351–H1359, 2006 [DOI] [PubMed] [Google Scholar]
- 2.Armstead WM, Cines DB, Bdeir K, Kulikovskaya I, Stein SC, Higazi AAR. uPA impairs cerebrovasodilation after hypoxia/ischemia through LRP and ERK MAPK. Brain Res 1231: 121–131, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Armstead WM, Cines DB, Higazi AA. Plasminogen activators contribute to impairment of hypercapnic and hypotensive cerebrovasodilation after cerebral hypoxia/ischemia in the newborn pig. Stroke 36: 2265–2269, 2005 [DOI] [PubMed] [Google Scholar]
- 4.Armstead WM, Cines DB, Higazi AAR. Plasminogen activators contribute to age dependent impairment of NMDA cerebrovasodilation after brain injury. Dev Brain Res 156: 139–146, 2005 [DOI] [PubMed] [Google Scholar]
- 5.Armstead WM, Nassar T, Akkawi S, Smith DH, Chen XH, Cines DB, Higazi AAR. Neutralizing the neurotoxic effects of exogenous and endogenous tPA. Nat Neurosci 9: 1150–1157, 2006 [DOI] [PubMed] [Google Scholar]
- 6.Borsello T, Clarke PGH, Hirt L, Vercelli A, Repici M, Schorderet DF, Bogousslavsky J, Bonny C. A peptide inhibitor of c-Jun N-terminal kinase protects against excitotoxicity and cerebral ischemia. Nat Med 9: 1180–1186, 2003 [DOI] [PubMed] [Google Scholar]
- 7.Bu G, Wjilliams S, Strickland DR, Schwartz AL. Low density lipoprotein receptor-related protein/α2-macroglobulin receptor is an hepatic receptor for tissue-type plasminogen activator. Proc Natl Acad Sci USA 89: 7427–7431, 1992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dobbing J. The later growth of the brain and its vulnerability. Pediatrics 53: 2–6, 1974 [PubMed] [Google Scholar]
- 9.Fanne RA, Nassar T, Yarovoi S, Rayan A, Lamensdorf I, Cines DB, Higazi AAR. Bloodbrain barrier permeability and tPA-mediated neurotoxicity. Neuropharm 58: 972–980, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Janjua N, Nasar A, Lynch JK, Qureshi AI. Thrombolysis for ischemic stroke in children. Data from the nationwide inpatient sample. Stroke 38: 1850–1854, 2007 [DOI] [PubMed] [Google Scholar]
- 11.Kuluz JW, Prado R, He D, Zhao W, Dietrich WD, Watson B. New pediatric model of ischemic stroke in infant piglets by photothrombosis. Stroke 38: 1932–1937, 2007 [DOI] [PubMed] [Google Scholar]
- 12.Laher I, Zhang JH. Protein kinase C and cerebral vasospasm. J Cereb Blood Flow Metab 21: 887–906, 2001 [DOI] [PubMed] [Google Scholar]
- 13.Nassar T, Akkawi S, Shin A, Haj-Yehia A, Bdeir K, Tarshis M, Heyman SN, Higazi AA. In vitro and in vivo effects of tPA and PAI-1 on blood vessel tone. Blood 103: 897–202, 2004 [DOI] [PubMed] [Google Scholar]
- 14.Nassar T, Haj-Yehia A, Akkawi S, Kuo A, Bdeir K, Mazar A, Cines DB, Higazi AA. Binding of urokinase to low density lipoprotein-related receptor (LRP) regulates vascular smooth muscle cell contraction. J Biol Chem 277: 40499–404504, 2002 [DOI] [PubMed] [Google Scholar]
- 15.Nicole O, Docagne F, Ali C, Margaill I, Carmeliet P, MacKenzie ET, Vivien D, Buisson A. The proteolytic activity of tissue-plasminogen activator enhances NMDA receptor-mediated signaling. Nat Med 7: 59–64, 2001 [DOI] [PubMed] [Google Scholar]
- 16.Rogove AD, Siao C, Keyt B, Strickland S, Tsirka SE. Activation of microglia reveals a non-proteolytic cytokine function for tissue plasminogen activator in the central nervous system. J Cell Sci 112: 4007–4016, 1999 [DOI] [PubMed] [Google Scholar]
- 17.Shaver EG, Duhaime AC, Curtis M, Gennarelli LM, Barrett R. Experimental acute subdural hematoma in infant piglets. Pediatr Neurol 125: 123–129, 1996 [DOI] [PubMed] [Google Scholar]
- 18.Tan Z, Li X, Kelly k, Rosen C, Huber J. Plasminogen activator inhibitor type I derived peptide, EEIIMD, diminishes cortical infarct but fails to improve neurological function in aged rats following middle cerebral artery occlusion. Brain Res 1281: 84–90, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tsirka SE, Gualandris A, Amaral DG, Strickland S. Excitotoxin-induced neuronal degeneration and seizure are mediated by tissue plasminogen activator. Nature 377: 340–344, 1995 [DOI] [PubMed] [Google Scholar]
- 20.Yepes M, Sandkvist M, Moore EG, Bugge TH, Strickland DS, Lawrence DA. Tissue-type plasminogen activator induces opening of the blood brain barrier via the LDL receptor-related protein. J Clin Invest 112: 1533–1540, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang X, Mori T, Jung JC, Fini ME, Lo EH. Secretion of matrix metalloproteinase-29 after mechanical trauma injury in rat cortical cultures and involvement of MAP kinase. J Neurotrauma 19: 615–625, 2002 [DOI] [PubMed] [Google Scholar]
- 22.Wang YF, Tsirka SE, Strickland S, Stiege PE, Lipton SA. Tissue plasminogen activator (tPA) increases neuronal damage after focal cerebral ischemia in wild type and tPA-deficient mice. Nat Med 4: 228–231, 1998 [DOI] [PubMed] [Google Scholar]