Abstract
Background
It is not known whether social support modifies the association between depression and impairment or disability in older people from developing countries in Asia.
Method
We used a Thai version of the EURO-D scale to measure depression in 1104 Thai rural community-dwelling parents aged ⩾60 years. These were all those providing data on depression who were recruited as part of a study of older adults with at least one living child (biological, stepchild or adopted child). Logistic regression modelling was used to determine: (a) whether impairment, disability and social support deficits were associated with depression; (b) whether social support modified this association.
Results
There were strong graded relationships between impairment, disability, social support deficits and EURO-D caseness. Level of impairment, but not disability, interacted with poor social support in that depression was especially likely in those who had more physical impairments as well as one or more social support deficits (p value for interaction=0.018), even after full adjustment.
Conclusions
Social support is important in reducing the association between physical impairment and depression in Thai older adults, especially for those with a large number of impairments. Enhancing social support as well as improving healthcare and disability facilities should be emphasized in interventions to prevent depression in older adults.
Keywords: Ageing, Asia, depression, developing countries, disability, social support
Introduction
Thailand is one of the fastest ageing countries in South-East Asia (UNFPA, 2006). The rapidly expanding proportion of older adults in the population creates potential challenges, one of the most important of which is chronic physical ill health and associated late-life depression.
Physical impairment and disability are among the most significant risk factors for depression in older adults. Impairment is defined as ‘problems in body function or structure, such as a significant deviation or loss’, while the term ‘disability’ encompasses impairments, activity limitations and restriction in social participation (WHO, 2001). Disability may lead to depression via biological pathways such as direct pathophysiological impacts on the brain (e.g. stroke), indirect physiological effects (e.g. increasing cytokine levels and other inflammatory factors) and side-effects of drugs (Konsman et al. 2002) or via psychosocial effects such as loss of perceived control, low self-esteem, social activity restriction and poverty (Lenze et al. 2001). Conversely, depression itself can cause disability directly though executive-type cognitive impairments, initiation-perseveration deficits, poor appetite or psychomotor retardation or indirectly through changes in health behaviour such as smoking, physical inactivity and poor adherence (Penninx et al. 2000; Lenze et al. 2001).
The meaning of impairment and disability is considered to be significant as they may be viewed as traumatic events. When older adults are facing pain, grief or fear of premature death from impairment and disability, they might reach out to others for support (Coughlin, 2008). Social support can increase self-esteem, coping skill and resilience as well as decrease experienced stigma (Hardy et al. 2004), resulting in a lower risk of depression or a shorter duration of a given episode.
The potential of social support to modify the association between impairment or disability and late-life depression has been demonstrated in studies from Western countries (Beekman et al. 1997; Prince et al. 1998; Schoevers et al. 2000; Hays et al. 2001; Jang et al. 2002). However, social support may vary from one culture to another, which might require modification to measurement strategies (Broadhead et al. 2001) and may limit comparability of findings across cultures. Of the few studies from Asia, social support and disability are both risk factors for depression (Chen et al. 2005) and social support from family appears to be more important than from friends (Chi & Chou, 2001).
In the Thai culture, the focus for this paper, older adults generally live with their family members, usually children. Older adults support their children and also receive financial and emotional support in return. Therefore, social support from children is considered to be imperative for Thai older adults (Knodel & Chayovan, 1997). However, social support from the wider family and from neighbours is also recognized (Knodel & Chayovan, 1997; Ingersoll-Dayton et al. 2001, 2004). Given this evidence and our experience, we thus considered that there were overlaps with the social support model developed for older adults in Western settings with its emphasis on connection with family and, to a lesser extent, with non-family. We therefore modified an existing scale for social support deficits developed in London, taking account of the literature on well-being and ageing in the Thai culture (Knodel and Chayovan, 1997; Prince et al. 1997b; Ingersoll-Dayton et al. 2004).
This is the first community-based study in Asia to look at whether social support modifies the association between depression and impairment or disability in older people. We aimed to assess the independent associations of impairment, disability and social support with late-life depression and to investigate modification by social support of the associations between impairment or disability and late-life depression. We hypothesized that:
High impairment or disability will be independently associated with higher odds of late-life depression.
Increasing number of social support deficits will be independently associated with increasing odds of late-life depression.
Groups with higher social support will show a weaker association between impairment or disability and late-life depression.
Methods
Setting
The study described is part of a longitudinal study designed to study the impact of migration on older adults and nested within the Kanchanaburi Demographic Surveillance System (Institute for Population and Social Research, 2001; Abas et al. 2009a). The Demographic Surveillance System monitors households annually in 100 sampling units, comprising 87 villages and 13 urban census blocks, which were originally selected by stratified random sampling from 900 sampling units in the province. We only used 98 of the 100 units as the other two had very few potentially eligible adults and would have been prohibitively expensive in fieldwork costs. Data were collected from November to December 2006.
Sampling
The primary aim of the main study (Abas et al. 2009a) was to study the effect of having children move away. The inclusion criteria were Thai-speaking, aged ⩾60 years and a parent of at least one living child (biological, stepchild or adopted child). As the sample was drawn from a demographic surveillance system that had been in place for 6 years, we had historical data on age. Only 5% of older adults in this rural setting did not have any of the categories of children, which is similar to that found previously in Thailand (Knodel & Chayovan, 1997). For the main study, we had adopted a sampling strategy based on whether or not older adults had children living with them. The sample size was based on a comparison of prevalence of common mental disorder in those with all children migrated versus those with some children migrated and required a total sample size of 954, given the proportions expected of those exposed and not exposed to having all their children migrate from the district. We approached 728 households with at least one adult aged ⩾60 years living with at least one of their children in the same household and 892 households with at least one adult aged ⩾60 years who was not living with at least one of their children in the same household. We randomly selected the participant in situations where there was more than one eligible older adult living in the household.
Measures
Dependent variable
Depression was defined using the Thai version of the EURO-D scale (Prince et al. 1999). The EURO-D scale is a structured scale of depressive symptoms designed for detecting depression in older populations. While the EURO-D can be a self-administered tool, it was read out here. Its items cover 12 symptom domains, including fatigue, appetite, sleep, concentration, interest, irritability, depression, tearfulness, enjoyment, pessimism, guilt and wishing death. In studies from developing countries, the EURO-D has a similar factor structure to that in European countries (Prince et al. 2004). Thai mental health professionals, including two non-English-speaking locally trained providers, considered that it covered symptoms recognized locally as common in psychological disorders in older adults. A team of bilingual mental health professionals, bilingual social scientists and English psychiatrists with relevant experience developed the first translation, paying particular attention to conceptual and semantic equivalence. Eight Thai psychiatrists validated the Thai version of the EURO-D in an out-patient setting against the Thai version of the Mini International Neuropsychiatric Interview, which is a standardized clinical diagnostic interview for DSM-IV Axis-I disorders (Kittirattanapaiboon & Khamwongpin, 2005). The sample size was 150 and the number of gold standard depressed cases was 51. Based on the cut-off point of 5/6, the area under the ROC curve was 0.78 [95% confidence intervals (CI) 0.70–0.85], the kappa was 0.4 and internal consistency for the total scale measured by Cronbach's α was 0.72 (Jirapramukpitak et al. 2009).
Independent variables
Physical impairment
A modified version of the Burvill physical illness scale was used to rate impairment (Pfeiffer, 1978; Lindesay et al. 1989; Burvill et al. 1990). Participants were asked about the presence of 13 common impairments, including breathlessness, faints/blackouts, arthritis, weakness/loss of limb, skin disorders, hearing difficulties, persistent cough, heart trouble, eyesight problems, gastrointestinal problems, high blood pressure, diabetes and pain. The numbers of impairments were summed to produce a score and the score (range 0–13) was then categorized into four groups of 0, 1, 2 and ⩾3 impairments (Prince et al. 1998).
Disability
We used the brief version of the WHO Disability Assessment Schedule (Prince et al. 1998; Epping-Jordan & Ustun, 2000). The domains included in the instrument are understanding and communicating with the world, moving and getting around, self-care, getting along with people, participation in society and life activities. We were unable to translate the item on learning a new task, which was viewed as not applicable for older adults in this setting. Therefore, we used a slightly modified 12-item version of the scale, each item self-rated on a 4-point scale from no problem with carrying out the activity to total/extreme inability. The total disability score (range 0–36) was categorized into quarters.
Social support
Social support was derived from the scale of six social support deficits, which had been found to be highly salient to depression in a previous study of older adults in London, UK (Prince et al. 1997b). These social support deficits were modified in order to be culturally appropriate for the Thai context (Knodel & Chayovan, 1997; Ingersoll-Dayton et al. 2001, 2004). The consensus was achieved by two psychiatrists from Thailand and two British geriatric psychiatrists with experience of working in South-East Asia. In this study, the six social support deficits were defined as follows:
Living alone without a child or other relative.
Seeing a child or other relative less often than once per week.
Lack of reciprocity with neighbours, through asking about amount to which neighbours depend on each other in their village.
Lack of reciprocity between children and extended family members, through asking about amount to which children and relatives care about each other.
Difficulty in relationship with one or more relatives, through asking about severe problems in relationships between the participant and any of their children or relatives in the last year lasting more than a few weeks.
Dissatisfaction with support from children.
Each item was scored 0 (deficit not present) or 1 (deficit present) and item scores were then summed to produce a summary scale. A higher score represents the higher level of social support deficit. Summary scores were then categorized into four groups (0, 1, 2, ⩾3) for general analyses (Kim et al. 2005) but into two groups (having and not having social support deficits) for the stratified analysis of the interaction between impairment, disability and social support deficit on depression because of small numbers in the categories with two and three deficits.
Preparatory work and data collection
The study received prior ethical approval from the King's College Research Ethics Committee (No. 05/05–68) (UK) and the Institute for Population and Social Research Review Board (Thailand). Preparatory qualitative work was carried out to develop the questionnaires, which were pretested by a team of experienced interviewers (Abas et al. 2009a). If the selected older adults and the head of household gave consent, the interviewer first interviewed the head of household with the household questionnaire and then the older adult with the individual questionnaire. The trained data collection team of four supervisors and 12 interviewers stayed in the villages during data collection. Quality control included checking on data completeness and consistency. Interviewers had to return to the participants if the data were inadequate. All the interviews were conducted in Thai.
Statistical analysis
SPSS version 15.0 for Windows (SPSS Inc., USA) was used for analyses. A categorical measure of depression (case/non-case) from the EURO-D scale was used for all analyses based on the cut-off point of 5/6 derived from the Thai validation. Percentages and odds ratios for EURO-D caseness against each sociodemographic characteristic were analysed using χ2 tests and logistic regression models. Variables were included as potential confounders if they were found to be significantly associated with impairment, disability or social support and EURO-D caseness independently (p<0.05).
Odds ratios and 95% CI were calculated using logistic regression with and without adjustment for the association between impairment in four categories, disability in quarters, social support deficits in four categories and EURO-D caseness. All of the categories were defined to be consistent with previous studies (Prince, 1998; Kim et al. 2005). In order to test for effect modification, odds ratios for the relationship between impairments, disability and depression were stratified by social support deficits (no social support deficit versus at least one social support deficit). The interaction terms generated between impairments, disability and social support were then tested before and after adjustment for potential confounders using logistic regression models.
Results
Participants
Of all 1620 older adults sampled from the 1620 households, 1300 were eligible to take part. Reasons for not being eligible were having no living biological or adopted children or stepchildren (5%), having changed status with regard to having or not having at least one child in the district (4%), having moved out of the village (7%) or having died since 2004 (4%).
Of the 1300 eligible, 196 (15.1%) were non-responders, of whom 8.5% were unavailable for an interview (despite up to 10 visits to the household), 5.0% were too unwell or cognitively impaired and 1.6% refused to take part. This left 1104 (84.9%) participants being included in the analysis.
Sociodemographic characteristics of the participants and associations with EURO-D caseness
A higher proportion of the participants were female (55%), married (56%) and in their sixties (54.7%). In total, 56% of them had completed at least primary education and half of them (50.4%) were still working. The prevalence of depression by the EURO-D scale was 27.2%. Being female, unmarried, older age, having lower education or lower socio-economic status and not currently working were significantly associated with depression in the unadjusted analyses (Table 1).
Table 1.
Sociodemographic characteristics and depression
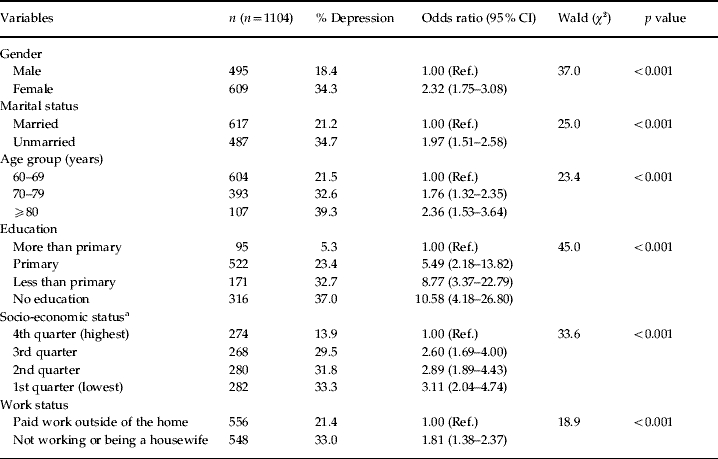
CI, Confidence interval.
Socio-economic status was measured from a household wealth index comprising 14 household assets (such as ownership of a fridge, motorcycle, or mobile phone) and interviewer's global rating of household quality.
Association between impairment, disability and depression
The three most common impairments were arthritis (44%), pain (36%) and eyesight problems (22%). Approximately one-third (32.3%) of the older adults did not have any impairment while another one-third (30.7%) had three or more impairments. All of the 13 impairments were associated with depression (p<0.05). Faints/blackout, persistent cough and breathlessness were the three impairments with the highest odds ratios for depression at 4.0, 3.9 and 3.4 respectively (p<0.001). More impairments and higher disability scores were each significantly associated with higher odds of depression, even after adjustment for age, marital status, education, socio-economic status and working status (Table 2).
Table 2.
The association between impairments, disability and depression
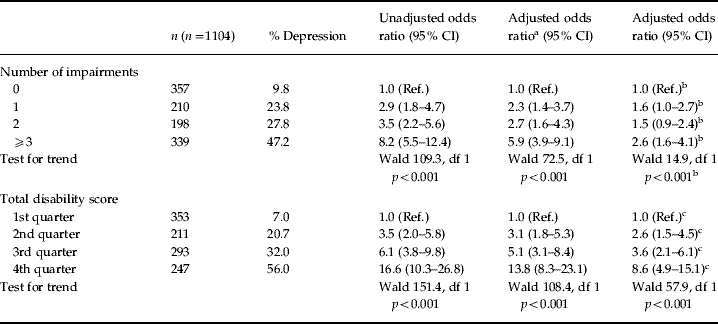
CI, Confidence interval; df, degrees of freedom.
Adjusted for age, gender, marital status, education, socio-economic status, work status.
Adjusted for age, gender, marital status, education, socio-economic status, work status and disability.
Adjusted for age, gender, marital status, education, socio-economic status, work status and impairment.
Association between social support and depression
Of the older adults, 14% lived alone, 3% saw a relative less often than once per week, 42% reported lack of reciprocity with neighbours, 21% felt that members in the family did not care about each other, 7% had experienced upset in a relationship with a relative and 9% were not satisfied with the support they received from their children. Approximately 40% of the older adults had no social support deficit and only 8% had three or more social support deficits. Four out of six social support deficits were associated with depression, including lack of reciprocity with neighbours, lack of reciprocity between children and extended family members, difficulty in the relationship with one or more relatives and dissatisfaction with support from children. Older adults with more social support deficits were more likely to have depression (Table 3).
Table 3.
The association between social support deficits and depression
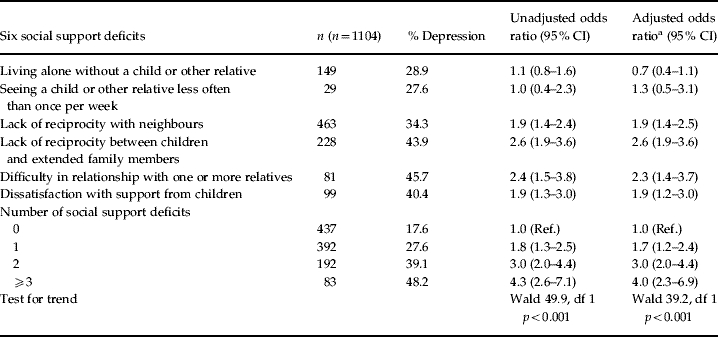
CI, Confidence interval; df, degrees of freedom.
Adjusted for age, gender, marital status, education, socio-economic status and work status.
Interaction between impairment/disability and social support deficit on depression
Table 4 displays the associations of impairments and disability with depression stratified into two groups of present/absent social support deficits. The interaction between impairment and social support deficits was significant at p=0.018 (Wald χ2 for interaction 5.6) after adjustment for potential confounders in the logistic regression model. For older adults with one to two impairments, having or not having social support deficits did not seem to change the effect size much. However, for older adults with three or more impairments, the odds ratios for depression in those with social support deficit were much higher than those without social support deficit. The effect of disability on EURO-D caseness in those with social support deficits tended to be higher than those with no social support deficit, although the interaction between disability and social support deficits was not statistically significant in the logistic regression model.
Table 4.
The association between impairment, disability and depression stratified by social support deficita
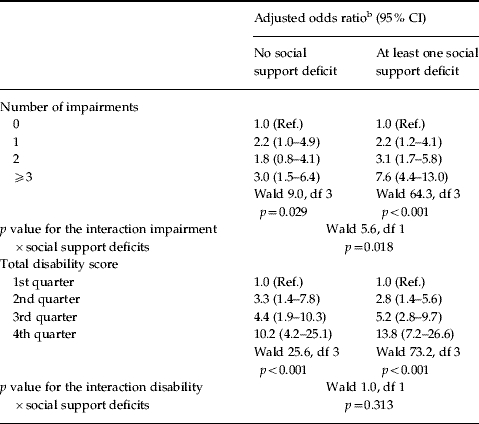
CI, Confidence interval; df, degrees of freedom.
The six social support deficits: living alone without a child or other relative; seeing a child or other relative less often than once per week; lack of reciprocity with neighbours; lack of reciprocity between children and extended family members; difficulty in relationship with one or more relatives; dissatisfaction with support from children.
Adjusted for age, gender, marital status, education, socio-economic status and work status.
Discussion
In this analysis of data from a community population of older people in rural Thailand, we found strikingly similar associations between impairment, disability, social support and depression to those reported from the Gospel Oak study of older people in north London (Prince et al. 1997b). These included both strong individual associations in the directions anticipated as well as an interaction between impairment and social support, supporting a modifying or ‘buffering’ effect of social support on the association between impairment and depression.
Advantages of the study included the large community-based sample, random sampling and a good response rate. We were unable to interview those who were travelling to visit their children at the time of study. It is possible that these were more depressed and seeking support. However, non-responders did not differ on demographic characteristics and selection bias is unlikely to explain our findings. We were able to adjust for a large range of confounders, which were selected carefully at the outset. There could be some residual confounding from unmeasured factors such as family history of depression. However, family history of depression is relatively rare and has been suggested to have a weaker influence on depression occurring in late life (van Ojen et al. 1995). In addition, adjustment for the major potential confounders had little impact on the strengths of associations of interest, which remained highly significant; therefore, residual confounding is unlikely to have been substantial.
Measurement error might have occurred through the adaptation of the EURO-D scale in a new culture, although the validity coefficients for EURO-D against a psychiatric diagnosis were acceptable. Any measurement error is likely to be random and thus to have biased any true associations towards the null; therefore, not accounting for our positive findings. It should be borne in mind that EURO-D caseness encompasses a broader spectrum of depressive disorder than major depressive disorder, as rigorously defined by DSM-IV criteria. Major depression is relatively rare among older adults, while minor depressive syndromes not fulfilling rigorous diagnostic criteria are common and important in this age group (Beekman et al. 1995).
Measurement error may also have occurred in the way we measured social support. Given the importance of support from children in the Thai culture, the scale may appear to have limitations in that only one of six items of the social supports deficits scale measures only support from children. However, four of the remaining six include support from children as well as from other relatives; thus, the scale is heavily weighted towards support from the family as appropriate in this culture (Knodel & Chayovan, 1997). One out of the six items deals with support from neighbours, which has been found to be associated with greater psychological well-being in Thai older people (Abas et al. 2009b). While the inclusion of more items on support only from children might have shown a stronger correlation with depression, their absence cannot explain the positive association that we found between social support and depression. However, this may explain why we did not find an interaction with disability. If we had used continuous measures of impairment, disability and social support, we might have had more power to demonstrate interaction, but we chose the categorical measures to allow comparability with a previous study in a Western cultural setting.
We believe that our analysis is the first investigation to test the modifying effect of social support on the association between impairment and depression in Asia. The result confirms the protective effect of social support from previous studies in Western countries (Beekman et al. 1997; Prince et al. 1997b, 2007). It also supports the universal applicability of the social support model cross-culturally (Broadhead et al. 2001). A protective effect of social support has been reported in specific physical diseases. A longitudinal study in people with chronic cardiac disease found that a higher level of social support at baseline was significantly associated with being less depressed at follow-up (Holahan et al. 1995). Likewise, a study in patients with rheumatoid arthritis found that social support predicted a decrease in psychological distress after 1 year (Evers et al. 1998). Nonetheless, a study in stroke patients did not find any significant difference between depressed stroke patients who received social support and those who did not (Shimoda & Robinson, 1998). This might be because the pathology of stroke involves cerebrovascular dysfunction, and post-stroke depression is more likely to be due to biological causes or other pathways that are not modified by the social environment.
Social support may reduce stress and consequently buffer the neuroendocrine effects of developing depression by decreasing cortisol level (Holt-Lunstad et al. 2008). Moreover, greater social support might also help older adults with impairment to perform daily tasks, encourage them to be more physically active, increase drug compliance, decrease social restriction and enhance self-esteem as well as coping skill of the older adults (Greenglass et al. 2005). Although the graded relationship between social support deficits and depression found in this study is similar to that found in the Gospel Oak study from London, the prevalence of social support deficits in Thailand was much lower (Prince et al. 1997b). Only 14% of Thai older adults lived alone and 3% of them saw a relative less often than once per week. These percentages in London were 49 and 29 respectively (Prince et al. 1997b). Furthermore, only 8% of Thai older adults had three or more social support deficits compared with 26% of the British older adults (Prince et al. 1997b). Most older adults in Thailand live close to their families and tend to co-reside or live very close to at least one child (Knodel & Ofstedal, 2002). Comparable results have been found in other Asian countries (Chi & Chou, 2001; Knodel & Ofstedal, 2002; Chen et al. 2005).
Association between impairment/disability and late-life depression
The three impairments showing the strongest associations with depression in this study were faints/blackout, persistent cough and breathlessness, while those reported by the Gospel Oak study were hypertension, severe pain and breathlessness (Prince et al. 1998). Although hypertension was reported in the previous study to have the highest strength of association with depression, it was found to be one of the five impairments with the weakest association in our study. One explanation might be the use of antihypertensives in the UK, which can have a depressogenic effect. Few older adults in rural Thailand have access to such medication. Another explanation is that hypertension might be under-recognized in Thailand and hypertensive patients might present with faints or blackouts instead.
Our findings of the associations between impairments, disability and late-life depression are again consistent with the findings from previous studies in very different samples and settings (Penninx et al. 2000; Cole & Dendukuri, 2003; Kim et al. 2005; Djernes, 2006; McDougall et al. 2007; Rasul et al. 2007). Moreover, the present study replicated the finding from the EURODEP study that the association of depression with disability was stronger than that with impairment (Braam et al. 2005). The odds ratios for depression in older adults with impairment/disability from this study are higher than those from other studies in Western countries (Prince et al. 1997a, 1998; McDougall et al. 2007). This might due to the limitations in healthcare services and disability facilities in Thailand and/or the difference in study design or measurements as disability in this study, applying a broader construct than has been used in some earlier research. However, the odds ratios found in this study are in the range of those reported in the review by Djernes (2006).
Some limitations should be taken into account when interpreting findings from this study. First, this observational cross-sectional analysis cannot provide direct evidence of causality. Indeed, potentially complex bi-directional inter-relationships may underlie the observations. Impairment, disability and social support deficits might lead to depression, which may worsen impairment or disability and lead to a deterioration in social support. Second, as a number of associations were analysed in this study, a problem of multiple testing might have occurred. However, it is unlikely that this would explain our findings as most of the associations found in this study were highly significant at p<0.001. Third, the findings from this study might lack generalizability to all older adults in this population as this was only a study of parents with at least one living child. However, we excluded only 5% of older adults from the random sample as 95% had a biological or adopted child or stepchild. Fourth, all impairment and disability variables were measured relying on subjective perception, which may lead to misclassification of health status. Furthermore, the scales measured the number of types of impairments, disabilities and social support deficits rather than the severity/intensity of individual items, which should be borne in mind when interpreting associations. For instance, one specific social support deficit might be very severe to an individual, but using our method would have been rated only as present or absent. However, this limitation would not explain our positive findings but might explain why we did not find an interaction between social support deficit and disability. Finally, there might be potential bias introduced by the influence of depressed mood on subjective perception and reporting of social support deficits and other parameters. Nevertheless, a previous study demonstrated a high level of agreement between self-report and objective health status measures (Burvill et al. 1990) and the measurements used in this study followed accepted international approaches for these constructs (Prince et al. 1997b, 1999).
Social support significantly weakened the association between impairment and late-life depression. This suggests a possible avenue of intervention, particularly in the rural Thai context where impairments may persist due to limited health care services. Social support, on the other hand, is more amenable to change. Furthermore, the present study provides evidence that impairment, disability and social support deficit are strongly associated with late-life depression. This is helpful not only in planning appropriate preventive strategies but also in developing knowledge about treatment for late-life depression in older adults living in the community. Care is currently provided by family members, especially daughters and granddaughters. Valuable services in rural areas may include home-care programmes for older people and their carers and extending the existing network of ‘elderly clubs’. Given that the relationship between impairment and late-life depression appears to be at least partially mediated through disability and that the effect of disability on late-life depression was much stronger than the effect of impairment itself, health services should emphasize early recognition and treatment to limit the possibility of impairment turning into disability. Once disability has occurred, limitation of disability through promoting transportation, home aids and adaptations, controlling of pain and enhancing rehabilitation might prevent depression, while for those already depressed these facilities might promote recovery.
Acknowledgements
We thank the interviewers and participants and all the staff from the Institute for Population and Social Research connected with the Kanchanaburi Demographic Surveillance System, which is part of the INDEPTH network of demographic surveillance sites in developing countries. We also thank the Wellcome Trust for funding the study (WT 078567).
Declaration of Interest
None.
References
- Abas MA Punpuing S Jirapramukpitak T Guest P Tangchonlatip K Leese M Prince M 2009aRural-urban migration and depression in ageing family members left behind British Journal of Psychiatry 19554–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abas MA Punpuing S Jirapramupitak T Tangchonlatip K Leese M 2009bPsychological wellbeing, physical impairments and rural aging in a developing country setting Health and Quality of Life Outcomes 766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beekman AT, Deeg DJ, van Tilburg T, Smit JH, Hooijer C, van Tilburg W. Major and minor depression in later life: a study of prevalence and risk factors. Journal of Affective Disorders. 1995;36:65–75. doi: 10.1016/0165-0327(95)00061-5. [DOI] [PubMed] [Google Scholar]
- Beekman AT, Penninx BW, Deeg DJ, Ormel J, Braam AW, van Tilburg W. Depression and physical health in later life: results from the Longitudinal Aging Study Amsterdam (LASA) Journal of Affective Disorders. 1997;46:219–231. doi: 10.1016/s0165-0327(97)00145-6. [DOI] [PubMed] [Google Scholar]
- Braam AW, Prince MJ, Beekman AT, Delespaul P, Dewey ME, Geerlings SW, Kivela SL, Lawlor BA, Magnusson H, Meller I, Peres K, Reischies FM, Roelands M, Schoevers RA, Saz P, Skoog I, Turrina C, Versporten A, Copelan JR. Physical health and depressive symptoms in older Europeans. Results from EURODEP. British Journal of Psychiatry. 2005;187:35–42. doi: 10.1192/bjp.187.1.35. [DOI] [PubMed] [Google Scholar]
- Broadhead J, Abas M, Sakutukwa GK, Chigwanda M, Garura E. Social support and life events as risk factors for depression amongst women in an urban setting in Zimbabwe. Social Psychiatry and Psychiatric Epidemiology. 2001;36:115–122. doi: 10.1007/s001270050299. [DOI] [PubMed] [Google Scholar]
- Burvill PW, Mowry B, Hall WD. Quantification of physical illness in psychiatric research in the elderly. International Journal of Geriatric Psychiatry. 1990;5:161–170. [Google Scholar]
- Chen R, Wei L, Hu Z, Qin X, Copeland JR, Hemingway H. Depression in older people in rural China. Archives of Internal Medicine. 2005;165:2019–2025. doi: 10.1001/archinte.165.17.2019. [DOI] [PubMed] [Google Scholar]
- Chi I, Chou KL. Social support and depression among elderly Chinese people in Hong Kong. International Journal of Aging and Human Development. 2001;52:231–252. doi: 10.2190/V5K8-CNMG-G2UP-37QV. [DOI] [PubMed] [Google Scholar]
- Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. American Journal of Psychiatry. 2003;160:1147–1156. doi: 10.1176/appi.ajp.160.6.1147. [DOI] [PubMed] [Google Scholar]
- Coughlin SS. Surviving cancer or other serious illness: a review of individual and community resources. CA: A Cancer Journal for Clinicians. 2008;58:60–64. doi: 10.3322/CA.2007.0001. [DOI] [PubMed] [Google Scholar]
- Djernes JK. Prevalence and predictors of depression in populations of elderly: a review. Acta Psychiatrica Scandinavica. 2006;113:372–387. doi: 10.1111/j.1600-0447.2006.00770.x. [DOI] [PubMed] [Google Scholar]
- Epping-Jordan J, Ustun T. The WHODAS-II: leveling the playing field for all disorders. WHO Mental Health Bulletin. 2000;6:5. [Google Scholar]
- Evers AW, Kraaimaat FW, Geenen R, Bijlsma JW. Psychosocial predictors of functional change in recently diagnosed rheumatoid arthritis patients. Behaviour Research and Therapy. 1998;36:179–193. doi: 10.1016/s0005-7967(98)00019-9. [DOI] [PubMed] [Google Scholar]
- Greenglass ER, Marques S, deRidder M, Behl S. Positive coping and mastery in a rehabilitation setting. International Journal of Rehabilitation Research. 2005;28:331–339. doi: 10.1097/00004356-200512000-00005. [DOI] [PubMed] [Google Scholar]
- Hardy SE, Concato J, Gill TM. Resilience of community-dwelling older persons. Journal of the American Geriatrics Society. 2004;52:257–262. doi: 10.1111/j.1532-5415.2004.52065.x. [DOI] [PubMed] [Google Scholar]
- Hays JC, Steffens DC, Flint EP, Bosworth HB, George LK. Does social support buffer functional decline in elderly patients with unipolar depression? American Journal of Psychiatry. 2001;158:1850–1855. doi: 10.1176/appi.ajp.158.11.1850. [DOI] [PubMed] [Google Scholar]
- Holahan CJ, Moos RH, Holahan CK, Brennan PL. Social support, coping, and depressive symptoms in a late-middle-aged sample of patients reporting cardiac illness. Health Psychology. 1995;14:152–163. doi: 10.1037//0278-6133.14.2.152. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Birmingham WA, Light KC. Influence of a ‘warm touch’ support enhancement intervention among married couples on ambulatory blood pressure, oxytocin, alpha amylase, and cortisol. Psychosomatic Medicine. 2008;70:976–985. doi: 10.1097/PSY.0b013e318187aef7. [DOI] [PubMed] [Google Scholar]
- Ingersoll-Dayton B, Saengtienchai C, Kespichayawattana J, Aungsuroch Y. Psychological well-being Asian style: the perspective of Thai elders. Journal of Cross-Cultural Gerontology. 2001;16:283–302. doi: 10.1023/a:1011984017317. [DOI] [PubMed] [Google Scholar]
- Ingersoll-Dayton B, Saengtienchai C, Kespichayawattana J, Aungsuroch Y. Measuring psychological well-being: insights from Thai elders. The Gerontologist. 2004;44:596–604. doi: 10.1093/geront/44.5.596. [DOI] [PubMed] [Google Scholar]
- Institute for Population and Social Research. Report of Baseline Survey (2000. Institute for Population and Social Research, Mahidol University; Nakhonpathom: 2001. [Google Scholar]
- Jang Y, Haley WE, Small BJ, Mortimer JA. The role of mastery and social resources in the associations between disability and depression in later life. The Gerontologist. 2002;42:807–813. doi: 10.1093/geront/42.6.807. [DOI] [PubMed] [Google Scholar]
- Jirapramukpitak T, Darawuttimaprakorn N, Punpuing S, Abas M. Validation and factor structure of the Thai version of the EURO-D scale for depression among older psychiatric patients. Aging and Mental Health. 2009;13:899–904. doi: 10.1080/13607860903046479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JM, Stewart R, Glozier N, Prince M, Kim SW, Yang SJ, Shin IS, Yoon JS. Physical health, depression and cognitive function as correlates of disability in an older Korean population. International Journal of Geriatric Psychiatry. 2005;20:160–167. doi: 10.1002/gps.1266. [DOI] [PubMed] [Google Scholar]
- Kittirattanapaiboon P, Khamwongpin M. The validity of the Mini International Neuropsychiatric Interview (M.I.N.I.)-Thai version. Journal of Mental Health of Thailand. 2005;13:126–136. [Google Scholar]
- Knodel J, Chayovan N. Family support and living arrangements of Thai elderly. Asia-Pacific Population Journal. 1997;12:51–68. [PubMed] [Google Scholar]
- Knodel J, Ofstedal MB. Hermalin A. I. The Well-being of the Elderly in Asia: A Four-country Comparative Study. The University of Michigan Press; Ann Arbor, Michigan: 2002. Patterns and determinants of living arrangements; pp. 143–184. ), pp. [Google Scholar]
- Konsman JP, Parnet P, Dantzer R. Cytokine-induced sickness behaviour: mechanisms and implications. Trends in Neurosciences. 2002;25:154–159. doi: 10.1016/s0166-2236(00)02088-9. [DOI] [PubMed] [Google Scholar]
- Lenze EJ, Rogers JC, Martire LM, Mulsant BH, Rollman BL, Dew MA, Schulz R, Reynolds CF 3rd. The association of late-life depression and anxiety with physical disability: a review of the literature and prospectus for future research. American Journal of Geriatric Psychiatry. 2001;9:113–135. [PubMed] [Google Scholar]
- Lindesay J, Briggs K, Murphy E. The Guy's/Age Concern survey. Prevalence rates of cognitive impairment, depression and anxiety in an urban elderly community. British Journal of Psychiatry. 1989;155:317–329. [PubMed] [Google Scholar]
- McDougall FA, Kvaal K, Matthews FE, Paykel E, Jones PB, Dewey ME, Brayne C. Prevalence of depression in older people in England and Wales: the MRC CFA Study. Psychological Medicine. 2007;37:1787–1795. doi: 10.1017/S0033291707000372. [DOI] [PubMed] [Google Scholar]
- Penninx BW, Deeg DJ, van Eijk JT, Beekman AT, Guralnik JM. Changes in depression and physical decline in older adults: a longitudinal perspective. Journal Affective Disorders. 2000;61:1–12. doi: 10.1016/s0165-0327(00)00152-x. [DOI] [PubMed] [Google Scholar]
- Pfeiffer E. Multidimensional Functional Assessment: The OARS Methodology. Duke University; Durham, NC: 1978. [Google Scholar]
- Prince M. The classification and measurement of disablement, with emphasis on depression, and its applications for clinical gerontology. Reviews in Clinical Gerontology. 1998;8:227–240. [Google Scholar]
- Prince M, Acosta D, Chiu H, Copeland J, Dewey M, Scazufca M, Varghese M. Effects of education and culture on the validity of the Geriatric Mental State and its AGECAT algorithm. British Journal of Psychiatry. 2004;186:429. doi: 10.1192/bjp.185.5.429. [DOI] [PubMed] [Google Scholar]
- Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, Rahman A. No health without mental health. Lancet. 2007;370:859–877. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- Prince MJ Harwood RH Blizard RA Thomas A Mann AH 1997aImpairment, disability and handicap as risk factors for depression in old age. The Gospel Oak Project V Psychological Medicine 27311–321. [DOI] [PubMed] [Google Scholar]
- Prince MJ Harwood RH Blizard RA Thomas A Mann AH 1997bSocial support deficits, loneliness and life events as risk factors for depression in old age. The Gospel Oak Project VI Psychological Medicine 27323–332. [DOI] [PubMed] [Google Scholar]
- Prince MJ, Harwood RH, Thomas A, Mann AH. A prospective population-based cohort study of the effects of disablement and social milieu on the onset and maintenance of late-life depression. The Gospel Oak Project VII. Psychological Medicine. 1998;28:337–350. doi: 10.1017/s0033291797006478. [DOI] [PubMed] [Google Scholar]
- Prince MJ, Reischies F, Beekman AT, Fuhrer R, Jonker C, Kivela SL, Lawlor BA, Lobo A, Magnusson H, Fichter M, van Oyen H, Roelands M, Skoog I, Turrina C, Copeland JR. Development of the EURO-D scale-a European Union initiative to compare symptoms of depression in 14 European centres. British Journal of Psychiatry. 1999;174:330–338. doi: 10.1192/bjp.174.4.330. [DOI] [PubMed] [Google Scholar]
- Rasul F, Stansfeld SA, Smith GD, Shlomo YB, Gallacher J. Psychological distress, physical illness and risk of myocardial infarction in the Caerphilly study. Psychological Medicine. 2007;37:1305–1313. doi: 10.1017/S0033291707000402. [DOI] [PubMed] [Google Scholar]
- Schoevers RA, Beekman AT, Deeg DJ, Geerlings MI, Jonker C, Van Tilburg W. Risk factors for depression in later life; results of a prospective community based study (AMSTEL) Journal of Affective Disorders. 2000;59:127–137. doi: 10.1016/s0165-0327(99)00124-x. [DOI] [PubMed] [Google Scholar]
- Shimoda K, Robinson RG. The relationship between social impairment and recovery from stroke. Psychiatry. 1998;61:101–111. doi: 10.1080/00332747.1998.11024821. [DOI] [PubMed] [Google Scholar]
- UNFPA. Population Aging in Thailand: Prognosis and Policy Response. United Nations Population Fund Thailand; Bangkok: 2006. [Google Scholar]
- van Ojen R, Hooijer C, Bezemer D, Jonker C, Lindeboom J, van Tilburg W. Late-life depressive disorder in the community. II. The relationship between psychiatric history, MMSE and family history. British Journal of Psychiatry. 1995;166:316–319. doi: 10.1192/bjp.166.3.316. [DOI] [PubMed] [Google Scholar]
- WHO. International Classification of Functioning, Disability and Health. World Health Organization; Geneva: 2001. [Google Scholar]


