Abstract
Rocky Mountain spotted fever (RMSF) is the most common tick-borne illness in Tennessee. Little is known about the occurrence of R. rickettsii, the causative agent, in ticks in Tennessee. To better understand the prevalence and distribution of rickettsial agents in ticks, we tested 1,265 Amblyomma, Dermacentor, and Ixodes adult and nymphal ticks. Additionally, we tested 231 Amblyomma americanum larvae. Ticks were collected from 49 counties from humans, wild animals, domestic canines, and flannel drags. Spotted fever group rickettsiae (SFGR) DNA was detected by polymerase chain reaction (PCR) in 32% of adult and nymphal ticks. A total minimum infection rate of 85.63 was found in larval pools tested. Three rickettsial species, Rickettsia montana, Rickettsia amblyommii, and Rickettsia cooleyi were identified by molecular analysis. Rickettsia rickettsii was not detected. This study suggests that some RMSF cases reported in Tennessee may be caused by cross-reactivity with other SFGR antigenically related to R. rickettsii.
Introduction
Rocky Mountain spotted fever (RMSF), a potentially fatal disease caused by Rickettsia rickettsii, is the most common tick-borne disease reported in Tennessee. The vector typically attributed with RMSF transmission and maintenance in the southeastern United States is Dermacentor variabilis (the American dog tick),1 although the widely distributed Rhipicephalus sanguineus (the brown dog tick), is also found in Tennessee2 and has been shown to transmit the pathogen in other parts of the country.3,4 Tennessee historically reports one of the highest incidence rates for RMSF in the United States,5,6 which have rapidly increased in recent years. In 2008, 224 cases were reported to the Tennessee Department of Health (TDH), a 20% increase over 2007 and 120% increase over 2004. Western Tennessee has been recognized for the highest level of RMSF activity, where six deaths were attributed to the disease from 2001 to 2005.7 Despite frequent laboratory testing and reports of RMSF, the true incidence in Tennessee is unclear. The majority of RMSF cases reported to the TDH are classified as probable based on clinically compatible symptoms and a single serologic test with elevated immunoglobulin (Ig)G or IgM antibodies. For most cases, paired convalescent sera were not collected. In addition, it has been proposed that some RMSF cases reported in the United States may be caused by non-R. rickettsii spotted fever group rickettsiae (SFGR) as a result of cross-reactivity among SFGR antibodies.8,9 Rickettsia amblyommii, in particular, has been suggested as a potential cause of high SFGR seroprevalence.10,11
Little is known about the diversity and prevalence of SFGR in ticks in Tennessee because of spatial and technical limitations of previous studies. In 1974 Burgdorfer and others12 identified R. rickettsii in D. variabilis in the Land Between the Lakes area bordering Kentucky by examining hemolymph, which is not as reliable for species identification as modern molecular techniques. In 2001, a study by Kollars and Kengluecha13 in Shelby County, western Tennessee, used polymerase chain reaction (PCR) to identify SFGR in 1% of D. variabilis collected from raccoons and opossums, but SFGR were not identified to the species level. In this study, we used molecular assays to determine the prevalence and identity of rickettsiae in 49 of Tennessee's 95 counties from ticks collected from vegetation and a diverse array of host species.
Materials and Methods
Tick collection and identification.
Adult and nymphal ticks were collected from April 2007 to September 2008 from 49 counties in Tennessee by the United States Department of Agriculture, Animal and Plant Health Inspection Service, Wildlife Services (USDA-APHIS-WS) and the TDH from humans, wild animals, and flannel drags. In addition, ticks were collected at or around the homes of some individuals that had previously been ill with RMSF. The wildlife tick hosts were raccoons, feral hogs, white-tailed deer, skunks, coyote, red foxes, groundhogs, horses, dogs, and opossum, a grey fox, and a feral cat, as previously described.14 To collect additional numbers of dog ticks from high RMSF incidence counties in Western Tennessee, adult and nymphal ticks were collected by veterinarians from domestic canines during peak incidence months of July and August 2009. Larvae were collected by flannel drags and traps at locations of human infection, and from domestic canines. All tick samples were sent to the TDH Vector-Borne Diseases Laboratory and were identified to species and life stage based on morphological criteria.15
DNA isolation.
Ticks were individually homogenized with metal beads and resuspended in 225 μL phosphate buffered saline (PBS). DNA was extracted from 100 μL of the homogenate using a Qiagen QiaAmp DNA Micro Kit (Qiagen Inc., Valencia, CA) according to manufacturer's instructions.
Identification of rickettsiae.
Extracted DNA was initially screened using a real-time PCR to amplify the 17 kDa gene of all SFGR.16 For species identification, a conventional PCR targeting the ompA gene of SFGR was conducted on positive samples as previously described using primers Rr190.602n and Rr190.70p.17 Field isolates and dH2O were used as positive and negative controls, respectively, for all real-time and conventional PCRs. The OmpA amplicons from PCR-positive samples were further subjected to a restriction fragment length polymorphism assay (RFLP) by digestion with Rsa1 (Promega, Madison, WI) and Pst1 (Fermentas, Glen Burnie, MD) enzymes at 37°C for 2 hours.17 Digested fragments were electrophoresed on 10% polyacrylamide gels. A subset of RFLP samples were verified by sequence analysis with a 3130x1 genetic sequencer (Applied Biosystems, Foster City, CA) using BigDye Terminator (Applied Biosystems).
Ecoregions and statistical analysis.
Level III ecoregion classifications used in the spatial analysis were derived from the United States Environmental Protection Agency and the Tennessee Department of Environment and Conservation collaborative project map.18 From east to west, the represented ecoregions include the Blue Ridge Mountains, the Ridge and Valley of eastern Tennessee, the Southwestern Appalachians, the Interior Plateau of middle Tennessee, the Southeastern Plains of west Tennessee, and the Mississippi Valley Loess Plains bordering Arkansas and Missouri. The vegetation among ecoregions varies greatly. The Blue Ridge Mountains has the most biodiversity with oak forests, northern hardwoods, spruce-fir forests, hemlock, and oak-pine forests. The Ridge and Valley region consists of oak forests with a multitude of springs and caves, and the Southwestern Appalachians have cropland, pasture, mixed oak, and shortleaf pine forests. The Interior Plateau consists of oak-hickory forest, bluestem prairie, and cedar glades. The Southeastern Plains in west Tennessee is made of cropland, pasture, and oak-hickory-pine forests. The Mississippi Valley Loess Plains is made of irregular plains and oak-hickory-pine forests.18 Pearson χ2 tests were used for statistical analyses.
Results
A total of 1,265 adult and nymphal ticks, including 655 Amblyomma americanum, 555 Dermacentor variabilis, 38 Ixodes texanus, 11 Ixodes cookei, 4 Ixodes scapularis, and 2 Amblyomma maculatum, were tested for rickettsial DNA by real-time PCR. Of these, 401 (32%) ticks were positive for SFGR DNA by real-time and conventional PCR. Of the six tick species tested, only D. variabilis, A. americanum, and I. scapularis produced positive amplicons for rickettsial DNA (Table 1). The overall infection rate for A. americanum was significantly higher than that of D. variabilis (P < 0.001). The sample size of I. scapularis was too small to conduct statistical analysis.
Table 1.
Prevalence of Rickettsia spp. of each tick species by life stage
| Tick species* | Males pos/tested (%) | Females pos/tested (%) | Nymphs pos/tested (%) | Total pos/tested (%) |
|---|---|---|---|---|
| A. am | 57/120 (48) | 73/132 (55) | 179/403 (44) | 309/655 (47) |
| D. var | 47/316 (15) | 39/232 (17) | 4/7 (57) | 90/555 (16) |
| I. scap | 0/2 | 2/2 (100) | – | 2/4 (50) |
| I. tex | 0/1 | 0/24 | 0/13 | 0/38 |
| I. cook | – | 0/9 | 0/2 | 0/11 |
| A. mac | – | 0/2 | – | 0/2 |
| Total | 104/439 (24) | 114/401 (28) | 183/425 (43) | 401/1265 (32) |
A. am = Amblyomma americanum; D. var = Dermacentor variabilis; I. scap = Ixodes scapularis; I. tex = Ixodes texanus; I. cook = Ixodes cookei; A. mac = Amblyomma maculatum.
A total of 327 A. americanum larval ticks were separated into 30 pools and tested for rickettsial DNA by real-time PCR. Twenty-eight pools tested positive for SFGR (Table 2). The total minimum infection rate (MIR) of lone star ticks in the counties surveyed was 85.63. Higher MIRs were seen in counties with high human RMSF infection rates (120.25–153.85). Lower MIRs were seen in counties with lower RMSF incidence rates (35.09–43.96).
Table 2.
Minimum infection rates (MIR/1000) of larval pools in selected counties in Tennessee*
| County | No. of larval pools | Total no. of larvae | No. positive pools | MIR/1,000 |
|---|---|---|---|---|
| Henry | 3 | 57 | 2 | 35.09 |
| Henderson | 19 | 158 | 19 | 120.25 |
| Decatur | 2 | 8 | 1 | 125.00 |
| Caroll | 2 | 13 | 2 | 153.85 |
| Davidson | 4 | 91 | 4 | 43.96 |
| Total | 30 | 327 | 28 | 85.63 |
MIR = minimum infection rate.
Three rickettsial species were identified by RFLP and sequence analyses. Rickettsia montana was identified in 53 (10%) D. variabilis from 16 counties and 5 ecoregions (Table 3). Rickettsia montana was identified in 2 (0.3%) A. americanum from the Southwestern Appalachians and Southeastern Plains ecoregions (Table 4). Rickettsia amblyommii was identified in 14 (3%) D. variabilis from 7 counties and 4 ecoregions (Table 3), and 259 (40%) A. americanum from 23 counties and 5 ecoregions (Table 4). All 28 of the SFGR positive larval pools were positive for R. amblyommii. Rickettsia cooleyi was identified in 2 (50%) I. scapularis from the Mississippi Valley Loess Plains ecoregion (Table 1). There was no observed difference in the prevalence of rickettsiae between male and female ticks of each species, although the prevalence of rickettsial DNA in A. americanum nymphs was significantly lower than in A. americanum adults (P < 0.001).
Table 3.
Prevalence of Rickettsia amblyommii and Rickettsia montana in Dermacentor variabilis—ecoregions listed from west Tennessee to east Tennessee
| Ecoregion* | No. D. var | No. R. amb (%) | No. R. mon (%) |
|---|---|---|---|
| MVLP | 52 | 0 | 2 (4) |
| SP | 95 | 5 (6) | 5 (7) |
| IP | 64 | 3 (5) | 3 (5) |
| SA | 24 | 1 (4) | 1 (4) |
| RV | 301 | 4 (1) | 40 (13) |
| BRM | 19 | 1 (5) | 2 (11) |
| Totals | 555 | 14 (3) | 53 (10) |
MVLP = Mississippi Valley Loess Plains; SP = Southeastern Plains; IP = Interior Plateau; SA = Southwestern Appalachians; RV = Ridge and Valley; BRM = Blue Ridge Mountains.
D. var = Dermacentor variabilis; R. amb = Rickettsia amblyommii; R. mon = Rickettsia montana.
Table 4.
Prevalence of Rickettsia amblyommii and Rickettsia montana in Amblyomma americanum—ecoregions listed from west Tennessee to east Tennessee
| Ecoregion* | No. A. am | No. R. amb (%) | No. R. mon (%) |
|---|---|---|---|
| MVLP | 15 | 7 (47) | 0 |
| SP | 291 | 110 (38) | 1 (0.5) |
| IP | 196 | 82 (42) | 0 |
| SA | 100 | 46 (46) | 1 (1) |
| RV | 53 | 14 (26) | 0 |
| BRM | – | – | – |
| Totals | 655 | 259 (40) | 2 (0.3) |
MVLP = Mississippi Valley Loess Plains; SP = Southeastern Plains; IP = Interior Plateau; SA = Southwestern Appalachians; RV = Ridge and Valley; BRM = Blue Ridge Mountains.
A. am = Amblyomma americanum; R. amb = Rickettsia amblyommii; R. mon = Rickettsia montana.
Dermacentor variabilis were predominately collected from raccoons with a prevalence of 92%. Amblyomma americanum were predominately collected from white-tailed deer with a prevalence of 94%.14 Ticks collected from raccoon and skunk wildlife hosts had the highest rate of infection (10% each) with R. montana. Ticks collected from white-tailed deer had an infection rate of 60% with Rickettsia amblyommii. In addition, ticks collected from cotton drags had an infection rate of 42% with R. amblyommii (Figure 1).
Figure 1.
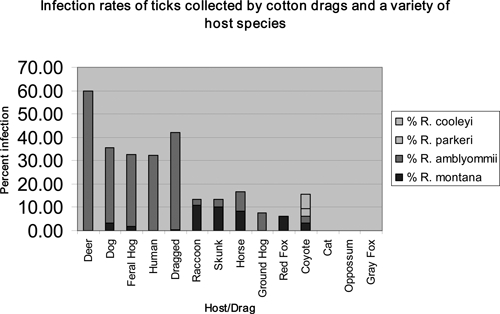
Tick infection rates of Rickettsia spp. by drag, human, or wildlife host collection.
Prevalence of R. amblyommii in A. americanum ranged from 26% to 47% by ecoregion and was significantly lower in Ridge and Valley compared with other regions (P = 0.02). Amblyomma americanum was not collected from the Blue Ridge Mountains, but R. amblyommii was detected in a single D. variabilis from that ecoregion (Table 3). The prevalence of R. montana in D. variabilis was significantly higher in the two easternmost ecoregions (8%) compared with the four western ecoregions (2%) (P = 0.01).
Discussion
Despite frequent reports of human RMSF infection in Tennessee, R. rickettsii, the etiologic agent of RMSF, was not identified from the 1,265 adult and nymphal ticks and 327 larval ticks collected from 49 counties throughout the state (Figure 2). Previous studies have isolated R. rickettsii from D. variabilis ticks both in the east coast and the Midwest.19,20 In 1981 Gordon and others found R. rickettsii infection rates in D. variabilis ticks to be only 1.3% in Ohio.19 In Connecticut R. rickettsii infection rates in D. variabilis ticks were found to be 5.4% in a 1986 study.20 However, more recent studies are showing R. rickettsii isolated from several other tick species. In southern California, Wikswo and others found8 R. rickettsii in Dermacentor occidentalis ticks at a low rate of 0.3%. Rickettsia rickettsii has also been found in Rhipicephalus sanguineus ticks associated with an RMSF outbreak in Arizona.4
Figure 2.
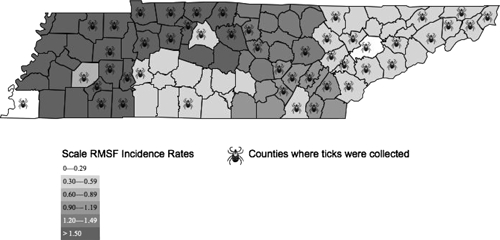
Human Rocky Mountain spotted fever (RMSF) incidence rates by county and tick collection by county.
Additionally, R. montana is a non-pathogenic rickettsiae21 that has previously been found in naturally infected D. variabilis.20,22 Rickettsia montana infection in D. variabilis has been shown to be as high as 4.2%. It has been shown to interfere with vertical transmission of pathogenic rickettsiae in D. variabilis and R. rickettsii models,23 which may partially explain the infrequent detection of R. rickettsii in nature. For this reason, the observation of increased infection rates of R. montana in D. variabilis in the two easternmost ecoregions of Tennessee is notable. The average human RMSF incidence rate for those two regions is 0.83 per 100,000, which is significantly lower than the Southeastern Plains of western Tennessee at 4.2 (P < 0.001). Ticks are capable of maintaining naturally occurring mixed rickettsial infections as was shown in Ohio in 2006.24 Although a causal relationship cannot be determined between high incidence of R. montana and low incidence of RMSF from this study, ecological factors such as interference may potentially impact the rickettsial transmission cycle.
Rickettsia cooleyi was first characterized as a novel rickettsiae from I. scapularis in 1998.24 The pathogenicity of this species remains unclear and it is possible that it causes clinical symptoms distinct from typical RMSF. It may also cause a mild to asymptomatic immune response leading to seroconversion without disease.25 However, Noda and others26 suggest that it is an endosymbiont restricted to the ovaries of the tick, thus inhibiting its transmission to host species.
Rickettsia amblyommii has been found to frequently infect A. americanum throughout the southeastern states, lower Midwest, and coastal New England of the United States.10,27,28 Since a 1993 study identified R. amblyommii as a possible agent of illness among members of a military unit,29 researchers have begun examining the organism as a possible cause of human illness potentially misdiagnosed as RMSF. In 2007 it was temporally associated with a macular rash when it was detected in an A. americanum removed from a patient.30 More recently, a group in North Carolina obtained serum samples from patients considered probable cases of RMSF and found that some of the patients had higher end-point titers against R. amblyommii antigen than R. rickettsii.11
In our study, the most common rickettsial species in all sexes and stages of ticks was R. amblyommii. The finding of R. amblyommii in the A. americanum larval pools indicates that transovarial transmission of R. amblyommii may be occurring. This may be occurring more often in counties of the state where higher incidence of human RMSF has been reported, as indicated by MIR values in high incidence counties (Henderson, Decatur, and Caroll) versus counties of lower relative incidence (Henry and Davidson). In addition, several questing nymphal A. americanum and D. variabilis ticks were collected that were infected with SFGR, implying that transstadial transmission of Rickettsia spp. is also occurring. Thus, some R. amblyommii may be maintained in the tick populations of Tennessee by feeding on infected hosts and transovarial and transstadial transmission. A high percentage (38–47%) of A. americanum ticks were infected with R. amblyommii in our study in all ecoregions with the exception of the Ridge and Valley ecoregion where 26% of A. americanum were infected with this rickettsial species. Interestingly, the lowest incidence of human RMSF is also in the Ridge and Valley ecoregion in eastern Tennessee (Figure 2).
We expected to find R. rickettsii in western Tennessee because of the high prevalence of RMSF infection in the region and were surprised not to find any throughout the entire state. Other pathogenic rickettsiae exist in nature and may cause human illness. For example, R. parkeri was identified as a human pathogen in 200431–33 and was detected in an A. americanum from Knox County, Tennessee in 2007.34 It is possible that the current human surveillance system over-reports RMSF cases based on antibodies, which cross-react against other SFGR, including R. parkeri and R. amblyommii. Because R. amblyommii was found in nearly half of all A. americanum, which frequently feeds on humans,35 and is antigenically related to R. rickettsii, a large proportion of patients may test seropositive as a result of exposure to this organism.
Studies have not been able to produce pathology consistent with RMSF infection in animals following artificial infection with R. amblyommii.1,12 If R. amblyommii truly is non-pathogenic or only mildly pathogenic, the severe disease observed in western Tennessee remains unexplained by rickettsial species other than R. rickettsii. Additionally, active surveillance is currently underway in western Tennessee to determine the etiologic agent of severe disease attributed to RMSF.
Acknowledgments
We thank Christina Moore and Sheri Roberts for their assistance with sequencing reactions.
Footnotes
Financial support: This research was supported by an appointment to the Emerging Infectious Diseases (EID) Fellowship Program administered by the Association of Public Health Laboratories (APHL) and funded by the Centers for Disease Control and Prevention (CDC).
Authors' addresses: Abelardo C. Moncayo, Sara B. Cohen, Charissa M. Fritzen, Eileen Huang, Junjun Huang, Timothy F. Jones, and John R. Dunn, Vector-Borne Diseases Section, Communicable and Environmental Disease Services, Tennessee Department of Health, Nashville, TN, E-mails: Abelardo.Moncayo@tn.gov, sarabeth.cohen@gmail.com, Charissa.Fritzen@tn.gov, eileen.huang11@gmail.com, Junjun.Huang@tn.gov, John.Dunn@tn.gov, and Tim.F.Jones@tn.gov. Michael J. Yabsley, Southeastern Cooperative Wildlife Disease Study, Warnell School of Forestry and Natural Resources, Department of Population Health, College of Veterinary Medicine, University of Georgia, Athens, GA, E-mail: myabsley@uga.edu. Daniel G. Mead, Southeastern Cooperative Wildlife Disease Study, Warnell School of Forestry and Natural Resources, Department of Population Health, College of Veterinary Medicine, University of Georgia, Athens, GA, E-mail: dmead@uga.edu. James D. Freye and Brett G. Dunlap, United States Department of Agriculture, Animal and Plant Health Inspection Service, Wildlife Services, Madison, TN, E-mails: Brett.G.Dunlap@aphis.usda.gov and James.D.Freye@aphis.usda.gov.
References
- 1.Burgdorfer W. A review of Rocky Mountain spotted fever (tick-borne typhus), its agent, and its tick vectors in the United States. J Med Entomol. 1975;12:269–278. doi: 10.1093/jmedent/12.3.269. [DOI] [PubMed] [Google Scholar]
- 2.Durden LA, Kollars TM., Jr An annotated list of the ticks (Acari: Ixodoidea) of Tennessee, with records of four exotic species for the United States. Bulletin of the Society for Vector Ecologists. 1992;17:125–131. [Google Scholar]
- 3.Wikswo ME, Hu R, Metzger ME, Eremeeva ME. Detection of Rickettsia rickettsii and Bartonella henselae in Rhipicephalus sanguineus ticks from California. J Med Entomol. 2007;44:158–162. doi: 10.1603/0022-2585(2007)44[158:dorrab]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 4.Demma LJ, Traeger MS, Nicholson WL, Paddock CD, Blau DM, Eremeeva ME, Dasch GA, Levin ML, Singleton J, Jr, Zaki SR, Cheek JE, Swerdlow DL, McQuiston JH. Rocky Mountain spotted fever from an unexpected tick vector in Arizona. N Engl J Med. 2005;353:587–594. doi: 10.1056/NEJMoa050043. [DOI] [PubMed] [Google Scholar]
- 5.Dalton MJ, Clarke MJ, Holman RC, Krebs JW, Fishbein DB, Olson JG, Childs JE. National surveillance for Rocky Mountain spotted fever, 1981–1992: epidemiologic summary and evaluation of risk factors for fatal outcome. Am J Trop Med Hyg. 1995;52:405–413. doi: 10.4269/ajtmh.1995.52.405. [DOI] [PubMed] [Google Scholar]
- 6.Treadwell TA, Holman RC, Clarke MJ, Krebs JW, Paddock CD, Childs JE. Rocky Mountain spotted fever in the United States, 1993–1996. Am J Trop Med Hyg. 2000;63:21–26. doi: 10.4269/ajtmh.2000.63.21. [DOI] [PubMed] [Google Scholar]
- 7.Adjemian JZ, Krebs J, Mandel E, McQuiston J. Spatial clustering by disease severity among reported Rocky Mountain spotted fever cases in the United States, 2001–2005. Am J Trop Med Hyg. 2009;80:72–77. [PubMed] [Google Scholar]
- 8.Wikswo ME, Hu R, Dasch GA, Krueger L, Arugay A, Jones K, Hess B, Bennett S, Kramer V, Eremeeva ME. Detection and identification of spotted fever group rickettsiae in Dermacentor species from southern California. J Med Entomol. 2008;45:509–516. doi: 10.1603/0022-2585(2008)45[509:daiosf]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 9.Parola P, Paddock CD, Raoult D. Tick-borne rickettsioses around the world: emerging diseases challenging old concepts. Clin Microbiol Rev. 2005;18:719–756. doi: 10.1128/CMR.18.4.719-756.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stromdahl EY, Vince MA, Billingsley PM, Dobbs NA, Williamson PC. Rickettsia amblyommii infecting Amblyomma americanum larvae. Vector Borne Zoonotic Dis. 2008;8:15–24. doi: 10.1089/vbz.2007.0138. [DOI] [PubMed] [Google Scholar]
- 11.Apperson CS, Engber B, Nicholson WL, Mead DG, Engel J, Yabsley MJ, Dail K, Johnson J, Watson DW. Tick-borne diseases in North Carolina: is “Rickettsia amblyommii” a possible cause of rickettsiosis reported as Rocky Mountain spotted fever? Vector Borne Zoonotic Dis. 2008;8:597–606. doi: 10.1089/vbz.2007.0271. [DOI] [PubMed] [Google Scholar]
- 12.Burgdorfer W, Cooney JC, Thomas LA. Zoonotic potential (Rocky Mountain spotted fever and tularemia) in the Tennessee Valley region. II. Prevalence of Rickettsia rickettsi and Francisella tularensis in mammals and ticks from Land Between the Lakes. Am J Trop Med Hyg. 1974;23:109–117. doi: 10.4269/ajtmh.1974.23.109. [DOI] [PubMed] [Google Scholar]
- 13.Kollars TM, Jr, Kengluecha A. Spotted fever group Rickettsia in Dermacentor variabilis (Acari: Ixodidae) infesting raccoons (Carnivora: Procyonidae) and opossums (Marsupialia: Didelphimorphidae) in Tennessee. J Med Entomol. 2001;38:601–602. doi: 10.1603/0022-2585-38.4.601. [DOI] [PubMed] [Google Scholar]
- 14.Cohen SB, Freye JD, Dunlap BG, Dunn JR, Jones TF, Moncayo AC. Host associations of Dermacentor, Amblyommai, and Ixodes (Acari: Ixodidae) ticks in Tennessee. J Med Entomol. 2010 doi: 10.1603/me09065. in press. [DOI] [PubMed] [Google Scholar]
- 15.Keirans JE, Litwak TR. Pictorial key to the adults of hard ticks, family Ixodidae (Ixodida:Ixodoidea), east of the Mississippi River. J Med Entomol. 1989;26:435–448. doi: 10.1093/jmedent/26.5.435. [DOI] [PubMed] [Google Scholar]
- 16.Loftis AD, Reeves WK, Szumlas DE, Abbassy MM, Helmy IM, Moriarity JR, Dasch GA. Surveillance of Egyptian fleas for agents of public health significance: Anaplasma, Bartonella, Coxiella, Ehrlichia, Rickettsia, and Yersinia pestis. Am J Trop Med Hyg. 2006;75:41–48. [PubMed] [Google Scholar]
- 17.Eremeeva M, Yu X, Raoult D. Differentiation among spotted fever group rickettsiae species by analysis of restriction fragment length polymorphism of PCR-amplified DNA. J Clin Microbiol. 1994;32:803–810. doi: 10.1128/jcm.32.3.803-810.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Griffith GE, Omernik JM, Azevedo SH. Ecoregions of Tennessee. Corvallis, OR: U.S. Environmental Protection Agency, National Health and Environmental Effects Research Laboratory; 1997. EPA/600/R-97/022. [Google Scholar]
- 19.Gordon JC, Gordon SW, Peterson E, Philip RN. Epidemiology of Rocky Mountain spotted fever in Ohio, 1981: serologic evaluation of canines and rickettsial isolation from ticks associated with human case exposure sites. Am J Trop Med Hyg. 1984;33:1026–1031. doi: 10.4269/ajtmh.1984.33.1026. [DOI] [PubMed] [Google Scholar]
- 20.Anderson JF, Magnarelli LA, Philip RN, Burgdorfer W. Rickettsia rickettsii and Rickettsia montana from Ixodid ticks in Connecticut. Am J Trop Med Hyg. 1986;35:187–191. doi: 10.4269/ajtmh.1986.35.187. [DOI] [PubMed] [Google Scholar]
- 21.Breitschwerdt EB, Walker DH, Levy MG, Burgdorfer W, Corbett WT, Hurlbert SA, Stebbins ME, Curtis BC, Allen DA. Clinical, hematologic, and humoral immune response in female dogs inoculated with Rickettsia rickettsii and Rickettsia montana. Am J Vet Res. 1988;49:70–76. [PubMed] [Google Scholar]
- 22.Stromdahl EY, Evans SR, O'Brien JJ, Gutierrez AG. Prevalence of infection in ticks submitted to the human tick test kit program of the U.S. Army Center for Health Promotion and Preventive Medicine. J Med Entomol. 2001;38:67–74. doi: 10.1603/0022-2585-38.1.67. [DOI] [PubMed] [Google Scholar]
- 23.Macaluso KR, Sonenshine DE, Ceraul SM, Azad AF. Rickettsial infection in Dermacentor variabilis (Acari: Ixodidae) inhibits transovarial transmission of a second Rickettsia. J Med Entomol. 2002;39:809–813. doi: 10.1603/0022-2585-39.6.809. [DOI] [PubMed] [Google Scholar]
- 24.Carmichael JR, Fuerst PA. A rickettsial mixed infection in a Dermacentor variabilis tick from Ohio. Ann NY Acad Sci. 2006;1078:334–337. doi: 10.1196/annals.1374.064. [DOI] [PubMed] [Google Scholar]
- 25.Billings AN, Teltow GJ, Weaver SC, Walker DH. Molecular characterization of a novel Rickettsia species from Ixodes scapularis in Texas. Emerg Infect Dis. 1998;4:305–309. doi: 10.3201/eid0402.980221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Noda H, Munderloh UG, Kurtti TJ. Endosymbionts of ticks and their relationship to Wolbachia spp. and tick-borne pathogens of humans and animals. Appl Environ Microbiol. 1997;63:3926–3932. doi: 10.1128/aem.63.10.3926-3932.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mixson TR, Campbell SR, Gill JS, Ginsberg HS, Reichard MV, Schulze TL, Dasch GA. Prevalence of Ehrlichia, Borrelia, and Rickettsial agents in Amblyomma americanum (Acari: Ixodidae) collected from nine states. J Med Entomol. 2006;43:1261–1268. doi: 10.1603/0022-2585(2006)43[1261:poebar]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 28.Childs JE, Paddock CD. The ascendancy of Amblyomma americanum as a vector of pathogens affecting humans in the United States. Annu Rev Entomol. 2003;48:307–337. doi: 10.1146/annurev.ento.48.091801.112728. [DOI] [PubMed] [Google Scholar]
- 29.Dasch GA, Kelly DJ, Richards AL, Sanchez JL, Rives CC. Western blotting analysis of sera from military personnel exhibiting serological reactivity to spotted fever group Rickettsiae. Am Soc Trop Med Hyg. 1993;49((Suppl. 3)):220. [Google Scholar]
- 30.Billeter SA, Blanton HL, Little SE, Levy MG, Breitschwerdt EB. Detection of Rickettsia amblyommii in association with a tick bite rash. Vector Borne Zoonotic Dis. 2007;7:607–610. doi: 10.1089/vbz.2007.0121. [DOI] [PubMed] [Google Scholar]
- 31.Paddock CD, Sumner JW, Comer JA, Zaki SR, Goldsmith CS, Goddard J, McLellan SL, Tamminga CL, Ohl CA. Rickettsia parkeri: a newly recognized cause of spotted fever rickettsiosis in the United States. Clin Infect Dis. 2004;38:805–811. doi: 10.1086/381894. [DOI] [PubMed] [Google Scholar]
- 32.Raoult D, Paddock CD. Rickettsia parkeri infection and other spotted fevers in the United States. N Engl J Med. 2005;353:626–627. doi: 10.1056/NEJM200508113530617. [DOI] [PubMed] [Google Scholar]
- 33.Whitman TJ, Richards AL, Paddock CD, Tamminga CL, Sniezek PJ, Jiang J, Byers DK, Sanders JW. Rickettsia parkeri infection after tick bite, Virginia. Emerg Infect Dis. 2007;13:334–336. doi: 10.3201/eid1302.061295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cohen SB, Yabsley MJ, Garrison LE, Freye JD, Dunlap BG, Dunn JR, Mead DG, Jones TF, Moncayo AC. Rickettsia parkeri in Amblyomma americanum ticks, Tennessee and Georgia, USA. Emerg Infect Dis. 2009;15:1471–1473. doi: 10.3201/eid1509.090330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Merten HA, Durden LA. A state-by-state survey of ticks recorded from humans in the United States. J Vector Ecol. 2000;25:102–113. [PubMed] [Google Scholar]


