Abstract
Background and objective
One important health outcome of inappropriate medication use in elderly is risk of hospitalization. We examined this relationship over 3 years in a retiree health claims database to determine the strength of this association using alternative definitions of potentially inappropriate medications.
Patients and methods
Prescription and hospitalization claims for U.S. retirees from a single large corporation were examined over the 3-year period, 2003–2005. Purging the database of non-employees (dependents, spouses), employees under age 65 (who were not Medicare-eligible), and retirees not covered for the full 3-year period left a sample of 7,459 retirees. Respondents’ medications were categorized according to two lists of “drugs to avoid”: Beers (updated) and NCQA. Logistic regression models were developed to examine risk of hospitalization in 2005 relative to use of potentially inappropriate medications across different periods of follow-up.
Results
Retirees taking one or more of the potentially inappropriate medications on the Beers or NCQA lists were 1.8 to 1.9 times more likely to have a hospital admission in models that adjusted for age, gender, number of prescriptions overall, and aggregate disease severity. Risk of hospitalization increased in a dose-response relationship according to number of potentially inappropriate medications.
Conclusion
Consistency in the strength of the association between “drugs to avoid” and hospital admission across different definitions of inappropriate medication use suggests the finding is robust. Findings from the retiree cohort provide further evidence for the inappropriateness of these medications among elderly.
Introduction
Inappropriate drug prescribing can be defined as the use of medications whose risks outweigh their benefits.[1] One common approach to examining this issue is development of explicit “drugs-to-avoid” criteria. These were initially developed by the late Dr. Mark H. Beers[2] and updated.[3–4] Other classifications are also available.[5–7] Drugs-to-avoid lists include medications that should be avoided in any circumstance, doses that should not be exceeded, and drugs to avoid in patients with specific disorders.
In the U.S., the National Committee for Quality Assurance (NCQA) assessed the Beers criteria as a quality indicator for ambulatory care.[8] In 2002, NCQA convened a Medication Management Technical Subgroup (consisting of four physicians and three pharmacists, including one of the authors [JTH]) to review geriatric medication issues. The specific activities of the subgroup were to (1) identify, prioritize, and define critical areas for performance measure development in the area of geriatric medication management; (2) work directly with NCQA staff to develop selected measures; and (3) make recommendations to the Geriatric Measurement Advisory Panel that reviews quality indicators. After 4 years of work the NCQA medication measures were included the U.S. Health Plan Employer Data and Information Set (HEDIS) as part of the standard assessment of quality in ambulatory care.
Concern for monitoring appropriate use of medication stems in part from the high prevalence of potentially inappropriate prescribing. A European study showed that 20% of elderly patients living in the community used at least one inappropriate medication.[9] A series of early studies of community-dwelling elderly in the U.S. reported inappropriate medication use in 14%–27%.[10] Not surprisingly, the prevalence of inappropriate medication use is highest in people taking many medications. For example, in an outpatient sample taking five or more medications, 37% were taking a medication on the Beers drugs-to-avoid list.[11]
Overuse (polypharmacy) and underuse are also issues in medication appropriateness and likely account for a larger amount of avoidable morbidity in the elderly than prescription of these proscribed medications.[1] Yet attention to potentially inappropriate prescribed medication is valuable. First, the predictive validity of these criteria with respect to health outcomes is still unclear. A recent review found that of the 17 studies that used some form of Beers criteria, eight studies found an increased risk of death, health service use, adverse drug reactions, or lower health-related quality of life, whereas nine studies found no increased risk in one or more health outcomes.[1] Second, modifying prescribing behavior for these proscribed drugs may be easier than addressing polypharmacy or underuse.
One important health outcome of inappropriate medication use in the elderly is risk of hospitalization. In one review using Beers criteria for inappropriate medication use,[12] three of four studies primarily examining community-dwelling elderly showed earlier onset of hospitalization,[13] greater risk of acute hospitalization,[14] and greater number of inpatient admissions.[15] Inappropriate medication use may increase the risk of hospitalization through adverse drug events, drug interactions, and intolerability among elderly.
Still, prior studies examining inappropriate medication use and risk of hospitalization have been less than ideal because of limitations in design. For example, some studies have relied on self-reported medication use, incomplete information on medical status, and self-reported hospitalization.
A health care claims database that captures claims for prescriptions and hospitalization offers certain advantages over prior studies. Claims data overcome issues of recall bias and provide nearly complete information on prescription use, medical status, and health care utilization. Employee-based retiree databases offer such data. While limited to people who have worked in prior years, these databases may nonetheless be very useful for examining health, medication, and health service use in old age.
In this research, we examined inappropriate medication use and risk of hospitalization over 3 years to determine the strength of this association. In particular, through careful assessment of start of medication use and year of hospitalization, we are able to assess temporal priority. We sought to examine these relationships using alternative categorizations of inappropriate medication use.
Methods and Measures
Sample
Participants in this analysis were U.S. retirees receiving medical insurance from PPG Industries, Inc. (the “Employer”), all age 65 or older. Thomson Reuters, the data warehouse for the Employer medical and pharmacy claims, prepared a series of datasets for prescription claims, hospitalizations, medical status, and demographics over the 3-year period, 2003–2005. The datasets were merged and then purged of non-employees (dependents, spouses), employees under age 65 (who were not Medicare-eligible), and retirees not covered for the full 3-year period. We obtained the data set as part of a data use agreement between the Employer and the University of Pittsburgh. These administrative data are used for billing and payment to vendors, along with Employer monitoring of health plan performance. This report represents the first use of the Employer retiree pharmacy claims for research purposes. Analyses were approved by the University of Pittsburgh Institutional Review Board as part of an exempt study of worksite health promotion.
Measures
Inappropriate medication use
Prescriptions in the Thomson Reuters database are coded in great detail and include three levels of therapeutic class as well as product name. For example, fluoxetine appears as “Fluoxetine HCL” (product name), “fluoxetine” (therapeutic class-detailed), “antidepressant” (therapeutic class-intermediate), and “central nervous system agent” (therapeutic class-general). This level of detail, along with dosage and medical condition, allowed coding for the two lists of inappropriate medications, including updated Beers,[4] and NCQA[8] criteria.
We used both Beers and NCQA criteria because, while similar, NCQA criteria exclude a number of controversial drugs (e.g., oxybutynin). We recognize as well that NCQA criteria are not limited to drugs to avoid but also include attention to drug-disease interactions and laboratory monitoring requirements for certain drugs (which we were unable to assess in this secondary analysis).
Also, we made one change in the Beers criteria. The Beers criteria involve three types of potential prescribing problems: drugs to avoid, drug-disease interactions, and dosage for a few drugs (e.g., digoxin, ferrous sulfate, and short half-life benzodiazepines). We decided to include lorazepam because it is the most commonly prescribed short half-life benzodiazepine and because emerging data suggest that exposure to benzodiazepines, regardless of half-life, increases the risk of falls, fractures, and cognitive impairment.[16,17]
Retirees were considered to be taking a potentially inappropriate medication if they had a claim for any one of Beers or NCQA medications in a particular year; we also computed the number of claims for potentially inappropriate medications in subsidiary analyses. Given our focus on the presence of any potentially inappropriate medication in a year, use of these medications should be considered a prevalent exposure. We were unable to code 5.3% of prescription claims and these were excluded from analyses. We considered as well the total number of prescription claims for each respondent.
Medical comorbidity
The Thomson Reuters database contains a disease stage indicator. The disease staging algorithm categorizes people according to “increasing complexity and system involvement.”[18] Details of the classification and weighing used in the algorithm are not available in the Data Users Guide provided by Thomson Reuters. The measure ranges from 0 to 4, with 4 representing greatest acuity, and is based on Medicare Diagnosis Related Groups (DRG) associated with physician and hospital visits. We used the mean score for each respondent, with the distribution of scores divided into quartiles for regression analyses to allow for appropriate risk stratification. 3.1% of respondents were missing comorbidity information. While we have not been able to identify studies that have validated this disease staging algorithm, results presented below suggest that the comorbidity score is highly correlated with risk of hospitalization.
Sociodemographics
Information was available for age, gender, and dates of coverage, as well as indicators that allowed us to exclude dependents and people under age 65.
Hospitalization
Dates for hospital admissions were available for the retiree cohort. We examined timing of hospitalization relative to start of use of potentially inappropriate medications.
Analyses
We first examined sociodemographic features of the cohort and calculated the proportion of retirees with any potentially inappropriate medication by each classification. We also examined the proportion with any hospitalization in each of the three years. As part of this descriptive effort, we identified the most prevalent potentially inappropriate medications in each classification. These included any medication accounting for more than 5% of the total potentially inappropriate medication claims within each classification.
To examine the association between potentially inappropriate medications and hospitalization in the cohort, we compared risk of hospitalization in people with and without claims for the medications stratified by the four-level disease stage indicator. In this way, we were able to examine the association between use of potentially inappropriate medications and hospitalization among people at comparable levels of health. Significance was assessed with the Mantel-Haenszel test across the four stages of disease severity.
In addition, we developed logistic regression models to examine the odds of hospitalization associated with use of potentially inappropriate medication adjusting for age, gender, disease stage, and total number of prescription claims. The outcome was hospitalization in 2005, the last year of follow-up, to assess the likelihood that use of inappropriate medications may increase risk of later, subsequent hospitalization. We developed models for the two inappropriate medication classifications.
To examine temporal associations more closely, we developed a series of alternative logistic regression models. First, we categorized respondents according to start and duration of use of potentially inappropriate medications. We wished to assess whether respondents with continuing use of inappropriate medications or first use in 2005 were at greater risk of hospitalization in 2005 than respondents with more limited use of the medications. Second, we categorized respondents according to the number of potentially inappropriate medication claims and determined if a greater number of inappropriate medications increased risk of hospitalization in a dose-response relationship.
Results
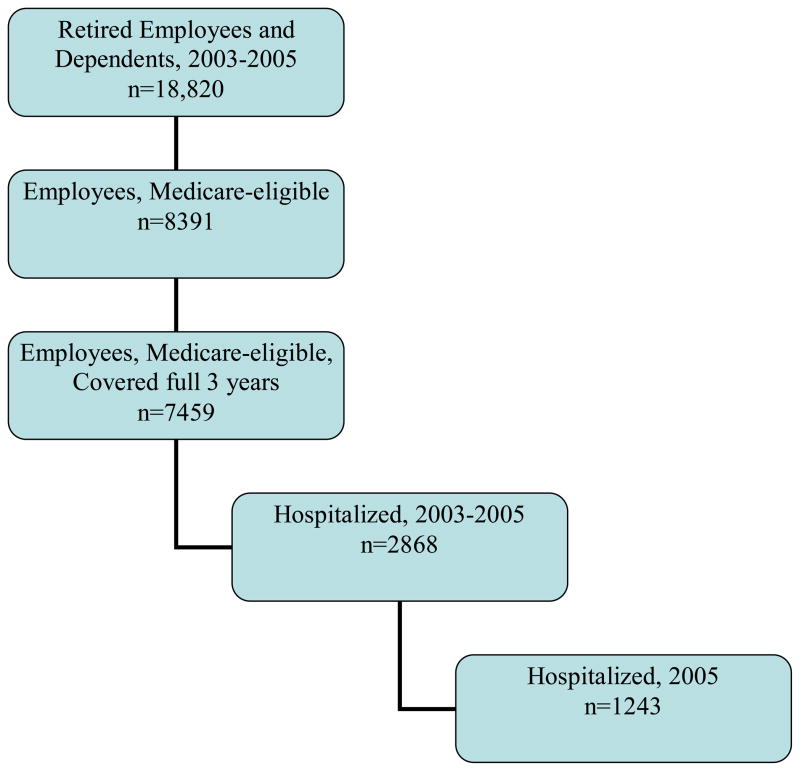
Among the employee retirees, 7,459 were covered for the entire period 2003–2005. Figure 1 shows derivation of the analytic sample from the original medication claims files. 38.5% (n=2,868) were hospitalized over the 3-year period, with 16.7% (n=1,243) first hospitalized in 2005. Consistent with the aging of the cohort, the proportion hospitalized increased with each successive year. The 7,459 retirees had a total of 509,566 medication claims and refills for the 3-year period, or 22.8 claims per person per year.
Figure 1.
Employer Retiree Sample
Table 1 shows demographic features of the retiree cohort. The cohort was primarily male (82.8%), as expected (given that the Employer is primarily involved in manufacturing). More than half the cohort was in their seventies and over a quarter were age 80 or greater.
Table 1.
Employer Medicare-Eligible Retirees, Covered Full 3 Years (2003–2005)
| % (n) | |
|---|---|
| Gender | |
| Male | 82.8 (6179) |
| Female | 17.2 (1280) |
| Age, 20031 | |
| <65 | 3.6 (270) |
| 65–69 | 20.0 (1493) |
| 70–74 | 25.1 (1869) |
| 75–79 | 25.4 (1893) |
| 80–84 | 16.7 (1247) |
| 85+ | 9.2 (687) |
| Any Use of Potentially Inappropriate Medication1 | |
| Beers | 53.5 (3780) |
| NCQA | 38.8 (2393) |
| First Hospital Admission, by Year | |
| 2003 | 10.0 (746) |
| 2004 | 11.8 (879) |
| 2005 | 16.7 (1243) |
5.3% with missing data on drug claims
Use of at least one potentially inappropriate medication was common in the cohort. Over the 3-year period, slightly more than half (53.5%) had a prescription for a medication on the Beers list. Medications on the NCQA list were prescribed to 38.8% of the cohort. The common use of at least one potentially inappropriate medication over the three years should be viewed in light of the small proportion of claims represented by these drugs. Of the 509,566 medication claims tracked over the 3 years, Beers criteria drugs included 5% of claims and NCQA drugs 2.6%. Thus, while the likelihood of using a proscribed drug at least once was high, these drugs comprised a very small part of the medications people used over the period.
Most Prevalent Potentially Inappropriate Medications
Table 2 shows the most prevalent potentially inappropriate medications prescribed for the cohort. Included in the table are medications that accounted for greater than 5% of prescriptions within each medication classification. These included diazepam, amitriptyline, acetaminophen-propoxyphene, cyclobenzaprine, hydroxyzine, nifedipine, doxazosin, promethazine, dipyridamole, and nitrofurantoin.
Table 2.
Most Prevalent Potentially Inappropriate Drugs in Beers and NCQA Classifications in Employer Retiree Sample
| Beers | NCQA |
|---|---|
| Diazepam | Diazepam |
| Amitriptyline | |
| Acetaminophen/propoxyphene | Acetaminophen/propoxyphene |
| Cyclobenzaprine | |
| Hydroxyzine | |
| Nifedipine (immediate release) | |
| Doxazosin | |
| Promethazine | |
| Dipyridamole (as single agent) | |
| Nitrofurantoin |
Note: 509,566 pharmacy claims for n=7459 retirees covered for 3-year period, 2003–2005. Medications listed here include those with >5% of claims within potentially inappropriate drug categorization. Beers criteria drugs included 5% of total claims and NCQA drugs 2.6%.
Risk of Hospitalization Associated with Potentially Inappropriate Medications, by Disease Stage
The medications claims data, as mentioned earlier, include a measure of disease severity or stage, a continuous measure that ranges from 0 to 4. We recoded the risk adjustment measure to represent quartiles of the sample distribution. Table 3 shows the risk of hospitalization at any point over the 3-year period by use of any potentially inappropriate medication, within disease stage, for the two “drugs to avoid” classifications.
Table 3.
Potentially Inappropriate Medication Use and Risk of Hospitalization, 2003–2005, by Disease Stage in Employer Retiree Sample
| a. Beers Criteria | ||
|---|---|---|
| Disease Stage | Medication Category: Beers (n) | Hospitalization, % |
| 1 | No potentially inappropriate drug (956) 1+ potentially inappropriate (686) |
10.7 19.0 |
| 2 | No potentially inappropriate drug (802) 1+ potentially inappropriate (986) |
23.6 41.3 |
| 3 | No potentially inappropriate drug (735) 1+ potentially inappropriate (1066) |
37.6 56.2 |
| 4 | No potentially inappropriate drug (734) 1+ potentially inappropriate (1003) |
48.6 73.3 |
| b. NCQA Criteria | ||
|---|---|---|
| Disease Stage | Medication Category: NCQA (n) | Hospitalization, % |
| 1 | No potentially inappropriate drug (1158) 1+ potentially inappropriate (484) |
11.4 20.7 |
| 2 | No potentially inappropriate drug (1013) 1+ potentially inappropriate (775) |
25.5 43.6 |
| 3 | No potentially inappropriate drug (955) 1+ potentially inappropriate (846) |
38.2 60.3 |
| 4 | No potentially inappropriate drug (975) 1+ potentially inappropriate (762) |
52.7 75.9 |
Mantel-Haenszel OR (95% CI) = 2.3 (2.1–2.6), p < .001
Mantel-Haenszel OR (95% CI) = 2.4 (2.2–2.7), p < .001
As expected, the prevalence of hospitalization increased with greater severity of disease. Notably, within each disease stage the likelihood of hospitalization was considerably higher (in some cases double) if respondents were taking a potentially inappropriate medication. The risk of hospitalization associated with use of potentially inappropriate drugs was apparent in patients with mild disease as well as patients with more severe disease. For example, among people in disease stage 1, 10.7% of people not prescribed a Beers-listed medication were hospitalized. Among those prescribed a Beers-listed drug, 19.0% were hospitalized (Table 3a). Among people with the most severe disease, 48.6% were hospitalized if not prescribed a Beers drug and 73.3% if prescribed such a drug.
This pattern held true for the NQCA classification as well. The association between potentially inappropriate medication use and risk of hospitalization was significant when adjusted for disease severity. Mantel-Haenszel statistics were significant for both classifications. Odds ratios for hospitalization for potentially inappropriate medication were 2.3 (95% confidence interval [CI], 2.1–2.6) for Beers criteria and 2.4 (95% CI, 2.2–2.7) for NCQA criteria.
Use of Potentially Inappropriate Drugs as an Independent Risk Factor for Hospitalization
To capture temporal associations between use of potentially inappropriate medications and hospitalization, we examined first hospitalizations in 2005, the last year of follow-up. In this way we are able to examine use of potentially inappropriate medications as a risk factor for later hospitalization. In these analyses, we consider people with earlier hospitalizations as not having met the hospitalization outcome. Thus, analyses are conservative.
Table 4 presents logistic regression models for first hospitalization in 2005. Models adjust for gender, age, disease stage, and total number of prescription claims over the 3 years. The models show expected increases in risk of hospitalization with greater age and greater disease severity. In each classification, risk of hospitalization was associated with use of potentially inappropriate medications. Odds ratios (95% CI) for use of potentially inappropriate medications within classifications were 1.78 (1.5–2.1) for Beers criteria and 1.94 (1.7–2.2) for NCQA criteria. Models accounted for 16–17% of variance in hospitalization.
Table 4.
Potentially Inappropriate Medication Class and Risk of Hospitalization in 2005: Logistic Regression Models
| Beers | NCQA | |
|---|---|---|
| OR (95% CI) | OR (95% CI) | |
| Gender | ||
| Male (reference) | 1.00 | 1.00 |
| Female | 1.10 (.9–1.3) | 1.05 (.9–1.3) |
| Age (yr) | 1.02 (1.0–1.03) | 1.02 (1.0–1.03) |
| Disease Stage | ||
| 1 (reference) | 1.00 | 1.00 |
| 2 | 2.40 (1.9–3.2) | 2.39 (1.8–3.1) |
| 3 | 4.60 (2.7–4.6) | 3.50 (2.7–4.6) |
| 4 | 6.40 (5.0–8.3) | 6.45 (5.0–8.4) |
| Number Prescriptions | 1.01 (1.0–1.02) | 1.01 (1.0–1.02) |
| Potentially Inappropriate Drug Status | ||
| None (reference) | 1.00 | 1.0 |
| Any | 1.78 (1.5–2.1) | 1.94 (1.7–2.2) |
| Model X2 | 707.6 (p < .001) | 733.9 (p < .001) |
| R2 | 0.16 | 0.17 |
To examine the timing of use of potentially inappropriate medications relative to the 2005 hospitalization outcome, we developed additional models that include an indicator for when cohort members were first prescribed such medications. In one approach, we defined three groups of respondents: early but short use of potentially inappropriate medications (use only in 2003 or only in 2004, n=1170), longer but limited use (use in both 2003 and 2004 but not in 2005, n=350), and first use or continuing use in 2005 (n=2662). In an alternative approach, we divided the sample into people who took potentially inappropriate medications only in 2003 (n=637), in 2004 for the first time or continuing from 2003 (n=883), or first or continuing use in 2005 (as above, n=2662). In both approaches, users of potentially inappropriate medications were compared to people who never took one of the Beers- or NCQA-listed medications.
Using a similar logistic regression model to adjust for age, gender, disease severity, and number of prescriptions, risk of hospitalization in 2005 was highest in the group using potentially inappropriate medications in 2005. This was true for both classifications of prior and continuing use. Relative to people not taking a potentially inappropriate medication, risk of hospitalization in 2005 was twice as high in this group (OR, 2.07 [95% CI: 1.8–2.4]). Retirees with earlier but limited use of potentially inappropriate medications also faced an elevated risk of hospitalization in 2005 relative to non-users. For people prescribed potentially inappropriate medications in 2004, the OR was 1.65 (1.2–2.2) in the first classification and 1.45 (1.18–1.79) in the second. For people prescribed potentially inappropriate medications in 2003, the OR for hospitalization in 2005 was lower and marginally significant, 1.22 (1.0–1.5) in the first classification and 1.21 (0.95–1.54) in the second.
Finally, we examined risk of late hospitalization according to the number of potentially inappropriate medications. We identified respondents with no claims for such medications, those with a small number of claims for such medications (1–3 in the Beers and NCQA classifications), and those with a greater number of claims. In both classifications, risk of hospitalization increased in a dose-response relationship according to number of potentially inappropriate prescriptions.
Discussion
This research confirms the high prevalence of potentially inappropriate medications among the elderly. The 3-year prevalence evident in this retiree database is comparable to the 15–20% per year reported for other elderly populations, such as Medicare beneficiaries overall,[19] nationally-representative cross-sections of elders in the community,[20] longitudinal cohorts,[21] elders at the end-of-life,[22] elders receiving home health care,[9] and national veteran samples.[23] While the prevalence of a prescription for any of the medications was high, in this retiree sample these “drugs to avoid” accounted for only 5% of total medication claims.
It is thus quite striking to see the strong association between any use of the medications and risk of hospitalization. Retirees taking one or more of the potentially inappropriate medications on the Beers or NCQA lists were 1.8 to 1.9 times more likely to have a hospital admission in models that adjusted for age, gender, number of prescriptions overall, and aggregate disease severity. We sought to establish the temporal priority of inappropriate medication use by limiting the hospitalization outcome to first admissions in 2005 and examining when participants first began use of a potentially inappropriate medication. We also noted that the risk of hospitalization increased in a dose-response relationship in both categorizations as the number of potentially inappropriate medications increased. Thus, our findings support prior studies that have shown an increased risk for hospital admissions.[13–15] Results from this research confirm the conclusion of a prior review: “data on community-dwelling elderly suggest that inappropriate drug use was associated with hospitalization measures in most studies.”[12]
The retiree claims database offers the strength of detailed prescription and hospitalization information, which is likely to be complete given that vendors must submit such information for payment. Because both domains also include information on dates of use, we were able to examine temporal relationships. In addition, the dataset allowed adjustment for disease severity, a critical adjustment, because disease severity is associated both with medication use and hospital admission. We further adjusted for differences in disease severity among respondents by including a count of total prescriptions in regression models. Consistency in the strength of the association between “drugs to avoid” and hospital admission across different definitions of inappropriate medication use suggests the finding is robust.
The similar strength of association between each “drugs-to-avoid” list and risk of later hospitalization suggests that the shorter NCQA list may identify inappropriate medications as effectively as the longer Beers list. Further analyses would be appropriate to examine particular medications on each list and their association with risk of hospitalization.
Why should use of inappropriate medications independently increase the risk of hospital admission in the elderly? Evidence from community settings suggests that many of these medications, especially the psychotropic agents, may be associated with falls[24] and other adverse events. It is important to note that the adverse effect of potentially inappropriate medications was highest among people with the greatest number of medical morbidities. Among participants with low disease burden, for example, the risk of hospitalization associated with potentially inappropriate drugs was relatively low: 10.7% over 3 years if participants were not taking a medication on the Beers list and 19.0% if they were, a risk difference of 8.3% (see Table 3a, disease stage 1). Among respondents with more severe disease burden, the risk difference increased dramatically, approaching 25% in the most severe stage of disease (disease stage 4). This difference suggests that potentially inappropriate medications have the greatest impact among people with a greater number of medical conditions, who take many medications. The retiree database will allow further exploration of the source of the increased risk of hospital admission as we examine specific drug-disease and drug-drug interactions. Still, the stratified analyses presented here suggest that the increased risk of hospitalization associated with potentially inappropriate medications is not an artifact of the association between medication use and medical conditions.
Findings from this study should be viewed in light of the study sample, which consists of adults, primarily men, who retired from a single workplace. Thus, generalizability of findings is limited to similar retiree populations. Still, the consistency and strength of the association of these medications with hospital admission provides further evidence for their inappropriateness among elders. This research is also limited by our focus on prescription medication claims rather than dosages of particular medications. We did not examine drug-drug or drug-disease interactions and thus cannot specify mechanisms by which potentially inappropriate medications increase the risk of hospitalizations. The robust association between potentially inappropriate medications and hospitalization established in this research points to the need to investigate such mechanisms. Also, as mentioned earlier, we were unable to code 5.3% of the prescription claims. This may have introduced bias into analyses. Finally, as is the case with secondary analyses of claims data, this research is limited by absence of information on medication adherence.
Despite these limitations, consistency in the strength of the association between “drugs to avoid” and hospital admission across different definitions of inappropriate medication use suggests the finding is robust. Findings from the retiree cohort provide further evidence for the inappropriateness of these medications among elderly.
Acknowledgments
Chongji Wei assisted with data pre-processing. PPG Industries, Inc. provided retiree data through Healthcare Business of Thomson Reuters.
This study was supported in part by National Institute of Aging grants R01 AG027017 and P30 AG024827, and VA Health Services Research grant IIR-06-062.
Footnotes
The authors report no conflicts of interest relating to this research.
References
- 1.Spinewine A, Schmader KE, Barber N, Hughes C, Lapane K, Swine C, Hanlon JT. Appropriate prescribing in elderly people: How can it be measured and optimized? Lancet. 2007;370:173–184. doi: 10.1016/S0140-6736(07)61091-5. [DOI] [PubMed] [Google Scholar]
- 2.Beers MH, Ouslander JG, Rollingher I, et al. Explicit criteria for determining potentially inappropriate medication use in the elderly. Arch Intern Med. 1991;151:1825–32. [PubMed] [Google Scholar]
- 3.Beers MH. Explicit criteria for determining potentially inappropriate medication use in the elderly: An update. Arch Intern Med. 1997;157:1531–36. [PubMed] [Google Scholar]
- 4.Fick DM, Cooper JW, Wade WE, et al. Updating the Beers criteria for potentially inappropriate medication use in the elderly: Results of a US consensus panel of experts. Arch Intern Med. 2003;163:2716–24. doi: 10.1001/archinte.163.22.2716. [DOI] [PubMed] [Google Scholar]
- 5.McLeod PJ, Huang AR, Tamblyn RM, et al. Defining inappropriate practices in prescribing for elderly people: A national consensus panel. CMAJ. 1997;156:385–91. [PMC free article] [PubMed] [Google Scholar]
- 6.Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D. STOPP (Screening Tool for Older Person’s Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Internat J Clin Pharmacol and Therapeut. 2008;46:72–83. doi: 10.5414/cpp46072. [DOI] [PubMed] [Google Scholar]
- 7.Laroche ML, Charmes JP, Bouthier F, Merle L. Inappropriate medications in the elderly. Clin Pharmacol Therapeut. 2009;85:94–97. doi: 10.1038/clpt.2008.214. [DOI] [PubMed] [Google Scholar]
- 8.NCQA. [Accessed 6/5/09];2007 http://www.ncqa.org/Portals/0/Newsroom/2007/Drugs_Avoided_Elderly.pdf.
- 9.Fialova D, Topinkova E, Gambassi G, et al. Potentially inappropriate medication use among elderly home care patients in Europe. J Am Med Assoc. 2005;293:1348–58. doi: 10.1001/jama.293.11.1348. [DOI] [PubMed] [Google Scholar]
- 10.Hanlon JT, Schmader KE, Ruby CM, et al. Suboptimal prescribing in older inpatients and outpatients. J Am Geriatrics Soc. 2001;49:200–209. doi: 10.1046/j.1532-5415.2001.49042.x. [DOI] [PubMed] [Google Scholar]
- 11.Steinman MA, Landefeld CS, Rosenthal GE, et al. Poloypharmacy and prescribing quality in older adults. J Am Geriatrics Soc. 2006;54:1516–23. doi: 10.1111/j.1532-5415.2006.00889.x. [DOI] [PubMed] [Google Scholar]
- 12.Jano E, Aparasu RR. Healthcare outcomes associated with Beers’ criteria: A systematic review. Annal Pharmacother. 2007;41:438–48. doi: 10.1345/aph.1H473. [DOI] [PubMed] [Google Scholar]
- 13.Fillenbaum GG, Hanlon JT, Landerman LR, et al. Impact of inappropriate drug use on health services utilization among representative older community-dwelling residents. Am J Geriatr Pharmacother. 2004;2:92–101. doi: 10.1016/s1543-5946(04)90014-1. [DOI] [PubMed] [Google Scholar]
- 14.Klarin A, Wimo A, Fastbom J. The association of inappropriate drug use with hospitalization and mortality: A population-based study of the very old. Drugs Aging. 2005;22:69–82. doi: 10.2165/00002512-200522010-00005. [DOI] [PubMed] [Google Scholar]
- 15.Fick DM, Waller JL, Maclean JR, et al. Potentially inappropriate medication use in a Medicare managed care population: Association with higher costs and utilization. J Managed Care Pharm. 2001;7:407–13. [Google Scholar]
- 16.Hanlon JT, Horner RD, Schmader KE, Fillenbaum GG, Lewis IK, Wall WE, Landerman LR, Pieper CF, Blazer DG, Cohen HJ. Benzodiazepine use and cognitive function among community dwelling elderly. Clin Pharmacol Ther. 1998;64:684–92. doi: 10.1016/S0009-9236(98)90059-5. [DOI] [PubMed] [Google Scholar]
- 17.Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: I. Psychotropic drugs. J Am Geriatr Soc. 1999;47:30–39. doi: 10.1111/j.1532-5415.1999.tb01898.x. [DOI] [PubMed] [Google Scholar]
- 18.Thomson Reuters (Medstat) Field Definition Guide. 2006. [Google Scholar]
- 19.GAO. Prescription drugs and the elderly: Many still receive potentially harmful drugs despite recent improvements. Washington, D.C: Government Accounting Office; 1996. [Google Scholar]
- 20.Willcox SM, Himmelstein DU, Woolhandler S. Inappropriate drig prescribing for the community-dwelling elderly. J Am Med Assoc. 1994;272:292–96. [PubMed] [Google Scholar]
- 21.Hanlon JT, Schmader KE, Boult C, et al. Use of inappropriate prescription drugs by older people. J Am Geriatr Soc. 2002;50:26–34. doi: 10.1046/j.1532-5415.2002.50004.x. [DOI] [PubMed] [Google Scholar]
- 22.Fahlman C, Lynn J, Finch M, et al. Potentially inappropriate medication use by Medicaid+Choice Benficiaries in the last year of life. J Palliative Med. 2007;10:686–695. doi: 10.1089/jpm.2006.0215. [DOI] [PubMed] [Google Scholar]
- 23.Pugh MJ, Hanlon JT, Zeber JE, et al. Assessing potentially inappropriate prescribing in the elderly Veterans Affairs population using the HEDIS 2006 quality measure. J Managed Care Pharmacy. 2006;12:537–545. doi: 10.18553/jmcp.2006.12.7.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aparasu RR, Mort JR. Prevalence, correlates, and associated outcomes of potentially inappropriate psychotropic use in community-dwelling elderly. Am J Geriatr Pharmacother. 2004;2:102–11. doi: 10.1016/s1543-5946(04)90015-3. [DOI] [PubMed] [Google Scholar]