Abstract
Background
Newborn cord care practices may directly contribute to infections, which account for a large proportion of the 4 million annual global neonatal deaths. This formative research study assessed current umbilical and skin care knowledge and practices for neonates in Sylhet, Bangladesh in preparation for a cluster-randomised trial of the impact of topical chlorhexidine cord cleansing on neonatal mortality and omphalitis.
Methodology
Unstructured interviews (n=60), structured observations (n=20), rating and ranking exercises (n=40), and household surveys (n=400) were conducted to elicit specific behaviours regarding newborn cord and skin care practices. These included hand-washing, skin and cord care at the time of birth, persons engaged in cord care, cord cutting practices, topical applications to the cord at the time of birth, wrapping/dressing of the cord stump, and use of skin-to-skin care.
Results
Ninety percent of deliveries occurred at home. The umbilical cord was almost always (98%) cut after delivery of the placenta, and cut by mothers in more than half the cases (57%). Substances were commonly (52%) applied to the stump after cord cutting; turmeric was the most common application (83%). Umbilical stump care revolved around bathing, skin massage with mustard oil, and heat massage on the umbilical stump. Forty-two percent of newborns were bathed on the day of birth. Mothers were the principal provider for skin and cord care during the neonatal period and 9% reported umbilical infections in their infants.
Discussion
Unhygienic cord care practices are prevalent in the study area. Efforts to promote hand washing, cord cutting with clean instruments, and avoiding unclean home applications to the cord may reduce exposure and improve neonatal outcomes. Such efforts should broadly target a range of caregivers, including mothers and other female household members.
Keywords: umbilical cord care, formative research, chlorhexidine, skin care, neonatal health, Bangladesh
Introduction
Of the annual four million neonatal deaths, 99% occur in developing countries, and more than one-third can be attributed to infections (1). Some infections in newborns result from exposure of the umbilical cord stump to invasive pathogens, leading to serious illnesses, including tetanus, omphalitis and sepsis (2), and are often related to traditional practices (3). “In community settings with a high proportion of home births, signs of cord infection are commonly seen. For example, in rural Nepal the incidence of redness extending to the skin at the base of the stump exceeded 15 cases in every 100 neonatal period observed, and redness in combination with pus discharge was present in approximately 6% of infants.” (4). Specific changes to cord care practices, including topical cleansing with chlorhexidine (5) may reduce exposure of the cord stump to pathogens and consequent risk of infection and death.
In preparation for a trial of chlorhexidine cleansing regimens in Sylhet, Bangladesh, we conducted formative research to determine perceptions of the umbilicus and its function, skin and umbilical care practices and roles of caretakers in overall and cord-specific newborn care. Such information can guide the design of future interventions to reduce risk of omphalitis within integrated neonatal care programs.
Methods
Semi-structured interviews were conducted with recently delivered women (n=20), mothers-in-law or other senior females (n=20), husbands (n=10) and fathers-in-law or other senior males (n=10). The sample of 20 mothers of infants 3 months of age or less (recently delivered women or RDW) was selected purposively to include high socioeconomic status (SES) families with relatives in a high-income country (4 women), middle SES families without relatives abroad (6 women), low SES families of fishermen and farmers (6 women), and very low SES families who had migrated into the area from central Bangladesh (4 women). Senior females, husbands and senior males were relatives living in the same household as these 20 women.
An exercise to rank five different commercially available topical antiseptic products was included in the unstructured interviews of the 20 RDWs and 20 senior females from the households of these RDWs. These five products were Nebanol powder, Neobacrin ointment, Hexisol, gentian violet, and antiseptic wipes. Respondents ranked these products on ease of application and preservation, and perceived comfort for the child. Project workers directly observed specific behaviours related to umbilical cord care at the time of delivery and during the immediate postnatal period using a semi-structured checklist in 20 households. A household survey on newborn care practices was also administered.
To estimate prevalence of any binary variable with assumed prevalence of 50%, within an absolute precision of 5%, and assuming 5% loss to follow-up, a total of 404 interviews were required, and 410 interviews were completed. Data were collected between September and November 2006.
Consent was obtained from all study participants, and all procedures were approved by the Ethical Review Committee of the International Centre for Diarrhoeal Disease Research, Bangladesh, and the Committee on Human Research at the Johns Hopkins Bloomberg School of Public Health, Baltimore, USA.
Results
Among survey respondents, 369 (90%) mothers delivered at home and 41 in public or private health facility or clinic. Table 2 presents survey results on cutting and tying the umbilical cord for home deliveries. In this study, 57% of RDWs reported they themselves had cut the umbilical cord. The person cutting the cord is considered to remain ritually unclean (napak) for 40 days, during which time he/she is unable to say prayers (namaj). As the mother is already considered to be in an unclean state due to the delivery, assuming the responsibility for cutting the cord does not affect this state, and prevents others from becoming ritually unclean.
Table 2.
Practices related to cutting and tying umbilical cord for deliveries occurring in the home
| Response | Frequency | Percent |
|---|---|---|
| When was the baby’s cord cut? (N=369) | ||
| Before delivery of placenta | 6 | 1.6 |
| After delivery of placenta | 363 | 98.4 |
| Who cut the cord? (N=369) | ||
| Myself (mother of newborn) | 210 | 56.9 |
| Trained birth attendant (dhonni) | 36 | 9.8 |
| Untrained birth attendant (dhonni) | 68 | 18.4 |
| Sister-in-law (Jal) | 14 | 3.8 |
| Young child | 2 | 0.5 |
| Mother-in-law (shashuri) | 4 | 1.1 |
| Paternal aunt (chachi-shashuri) | 14 | 3.8 |
| Other person | 21 | 5.7 |
| What was used to cut the cord? (N=369) | ||
| Blade | 341 | 92.4 |
| Scissors | 3 | 0.8 |
| Sickle | 3 | 0.8 |
| Other utensil | 22 | 6.0 |
| Was the blade/scissor/sickle boiled before it was used? (N=369) | ||
| Yes | 132 | 35.8 |
| No | 237 | 64.2 |
| Was the cord tied or clamped before cutting it? (N=369) | ||
| Yes | 342 | 92.7 |
| No | 26 | 7.0 |
| Don’t know | 1 | 0.3 |
| What was used to tie/clamp the cord? (N=342) | ||
| Thread from CBK | 100 | 29.2 |
| Other thread | 240 | 70.2 |
| Other material | 2 | 0.6 |
| Was the thread boiled before it was used? (N=342) | ||
| Yes | 191 | 55.8 |
| No | 151 | 44.2 |
| Was anything applied to the umbilical cord immediately after cutting it? (N=369) | ||
| Yes | 191 | 51.8 |
| No | 178 | 48.2 |
“Our elders tell us that prayers (namaj) or fasting (roja) of the person who has cut the cord will not be accepted. Since a mother does not need to say prayers (namaj) or fast until 40 days after her delivery, she is the right person to cut the cord.” – A mother.
TBAs cut the cord in some cases (28%), and TBAs normally have limited involvement in skin and cord care during the first week of life. In qualitative interviews, only two mothers reported cutting the cord before delivery of the placenta. One had delivered in a sub-district hospital, while the other received assistance during delivery at home from a trained NGO health worker. The remaining mothers and grandmothers reported delaying cord cutting until after delivery of the placenta. Some respondents mentioned that a mother could be harmed if the cord was cut prior to placental delivery.
“She (TBA) cut the nari (cord) after the chhabra (placenta) came out. If the cord is cut before the placenta comes out, the placenta climbs up to the kolija (~liver), mother gets hurt in her kolija and dies.” – A grandmother.
A clean delivery kit (CDK) was available for 28% of deliveries, mostly from households in the study area where CDKs were concurrently being distributed free of charge. The clean blade (99%), plastic sheet to place under the mother (89%), thread for tying the cord (98%) and soap (97%) were commonly used among those having CDKs. Among 369 home deliveries, the cord was clamped or tied with a thread before being cut in 93% of cases; this proportion was slightly higher (98%) among CDK users. Overall use of a blade was high (92%). Boiling of the cutting instrument (overall 64%) was more common among CDK users (43/103, 42%) compared to those where a non-CDK blade or instrument was used (88/265, 33%). During qualitative interviewers, blade boiling prior to cutting was described by most mothers and grandmothers.
On average, the cord was cut approximately 4–7 finger widths from the abdomen. Half of the families (52%) applied a substance to the cord immediately after cutting. The most commonly reported substances used on the cord were turmeric (83%) and boric powder (53%). Other substances applied were mustard oil, ash, Dettol, coconut oil, Nebanol ointment, ginger, and chewed rice.
Bathing, skin massage and heat treatment of the umbilical stump, employed individually or separately (Figure 1), are principal components of skin and umbilical cord practices during the first week of life.
Figure 1.
Elements of local newborn skin and umbilical stump care practices in the home in Sylhet District
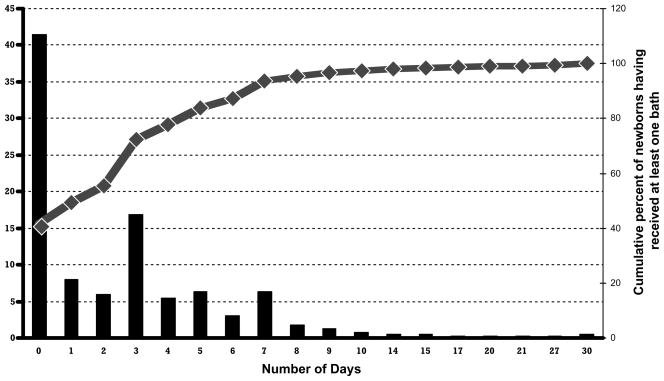
Bathing newborns soon after birth is a cultural norm in Sylhet District. Although a large proportion of newborns are bathed within 24 hours (42%), a substantial proportion of newborns received their first bath more than 72 hours after birth (Figure 2), potentially due to promotion of delayed bathing in the previous Projahnmo-1 study. Water was usually warmed prior to the bath (96% of 388 newborns receiving a bath), usually over a stove (99%).
Figure 2. Timing of first bath for newborn in Sylhet District.
N = 388 newborns given a bath (94.6% of 410 newborns in sample)
Babies are bathed soon after birth to clean and purify the newborn, remove the vernix (shada shada moyla), remove blood from delivery process, and to prepare newborn for hearing call to prayer or azan (reported mostly by male respondents). The necessity of purification of newborn predominated among these reasons:
“I bathed the baby (chhawal) right after birth to purify it. If the baby is not bathed and a senior holds it on the lap (kole neye), he/she will not be allowed to say prayers (namaj). Therefore, I bathed the baby (right after the delivery).” – A grandmother.
Concern regarding pneumonia restrained many caretakers from bathing right after birth.
“I bathed my baby after six days. You people (pointing to health workers) keep saying that bathing immediately after birth causes cold and pneumonia.” – A mother.
In-depth interviews and observations revealed that newborns were normally bathed 2–3 times during first week of life. The suggested optimal time for newborn bathing was between 10:00am and 12:00pm, as sun is strong and therefore reduces risk of cold-related diseases such as pneumonia. Mustard oil massage is another way families try to protect the child from getting cold during bathing.
Bathing practices are shown in Table 3. Most women reported using pond water to bathe the newborn. Substances are sometimes (21%) added to the water - most commonly Dettol or Savlon (a common household antiseptic containing chlorhexidine).
Table 3.
Newborn bathing practices
| Response | Frequency | Percent |
|---|---|---|
| Was the baby bathed after birth? (N=410) | ||
| Yes | 388 | 94.6 |
| No | 22 | 5.4 |
| Was the water warmed before the bath? (N=388) | ||
| Yes | 371 | 95.6 |
| No | 17 | 4.4 |
| How was the bath water warmed? (N=371) | ||
| Set out in sun | 3 | 0.8 |
| On stove | 368 | 99.2 |
| Was anything added to the bath water? (N=388) | ||
| Yes | 82 | 21.1 |
| No | 306 | 78.9 |
| What was added to the bath water? (N=82) | ||
| Hand/body soap | 4 | 4.9 |
| Dettol | 59 | 72.0 |
| Savlon | 16 | 19.5 |
| Other substance | 3 | 3.7 |
| How was the baby bathed? (N=388) | ||
| Immersion in water | 194 | 50.0 |
| Pour water over baby | 127 | 32.7 |
| Wipe baby with cloth | 66 | 17.0 |
| Don’t know | 1 | 0.3 |
| How frequently was the baby bathed during the first week of life? (N=388) | ||
| Daily | 55 | 14.2 |
| 2–3 times | 212 | 54.6 |
| Once | 117 | 30.2 |
| Don’t know | 4 | 1.0 |
Many participants appreciated the importance of thermal care in prevention of perceived illnesses caused by cold. Respondents reported four methods of keeping newborns warm in their first week (multiple responses possible): wrapping the newborn infant in a “blanket” (96%), oil massage (31%), placing the newborn infant near a heat source such as a fire (5%), and skin-to-skin contact (2%). When wrapping the baby, most common materials used were either a tolpani (also called katha, a thin, home-made mat made with several layers of used cloths), or layers of used cloths from a woman’s sari or man’s lungi.
“I had the baby wear a jama (clothing for upper part of the body) and then covered (wrapped) it with a katha or kombol (blanket). If temperature is low, I had the baby wear socks and warm jama. What else could we do (to keep it warm)?” – A grandmother
Newborn massage (malish kora) was practiced by 367 (90%) respondents (Table 4) and mustard oil (mitha tel) was the most common type of oil chosen (86%). The oil is normally applied to entire body from the first day of life. A “generous” amount is used for each session, enough to massage the belly, back, legs (including toes), hands (including fingers) and head. The observations revealed this “generous” amount was sufficient to complete a full-body massage. Normally the face, genital organs and umbilical stump were excluded from the massage, but some participants reported that mustard oil was applied to the cord stump directly prior to the time when it falls off.
Table 4.
Newborn oil massage practices
| Response | Frequency | Percent |
|---|---|---|
| Is the baby given an oil massage? (N=410) | ||
| Yes | 367 | 89.5 |
| No | 43 | 10.5 |
| What type of oil was used for the massage? (N=367) | ||
| Mustard Oil | 315 | 85.8 |
| Coconut Oil | 39 | 10.6 |
| Other Oil | 12 | 3.3 |
| Don’t Know | 1 | 0.3 |
| Was the oil heated? (N=367) | ||
| Yes | 120 | 32.7 |
| No | 247 | 67.3 |
| Who gave the massage? (N=367) | ||
| Mother of newborn | 331 | 90.2 |
| Maternal Grandmother | 54 | 14.7 |
| Paternal Grandmother | 51 | 13.9 |
| Maternal Aunt | 4 | 1.1 |
| Paternal Aunt | 8 | 2.2 |
| Other person | 11 | 3.0 |
| Was anything added to the oil? (N=367) | ||
| No | 247 | 67.3 |
| Various herbs/spices | 118 | 32.3 |
| Other oil | 2 | 0.5 |
| How frequently was oil massage given during baby’s first week of life? (N=367) | ||
| Daily | 100 | 27.2 |
| 2–3 times | 197 | 53.7 |
| Once | 67 | 18.3 |
| Don’t know | 3 | 0.8 |
| How frequently was oil massage given during baby’s first month of life? (N=367) | ||
| Daily | 82 | 22.3 |
| 2–3 times a week | 243 | 66.2 |
| Once a week | 39 | 10.6 |
| Don’t know | 3 | 0.8 |
Mustard oil is perceived as an intrinsically hot substance that protects the baby from cold and associated health problems (6). Some respondents mixed various herbs and spices (33%), especially garlic, into the mustard oil, which they heated and applied to the baby’s body after cooling the mixture. Other additives include ginger, turmeric and bonjamra leaves. Massage generally continues for 4–5 minutes and is performed two to three times daily, especially after bathing.
“I used mustard oil to remove white moila (referring to vernix). If you massage your baby with mustard oil, cold will not catch it, and its muscles will become strong. This is why we massaged our baby with mustard oil.” – A mother.
The person responsible for massaging the baby is almost universally a female household member, normally the mother or grandmother.
Similarly, heat treatment (shek dewa) and cleaning are usually performed by the mother and grandmother, with occasional help from the mother’s or father’s sisters. Though keeping newborn close to chest while wrapped in warm clothes (blankets) is common, skin-to-skin care was rarely (2%) reported; when provided, it is primarily given by mother (8 out of 9 respondents) or grandmother (5 out of 9 respondents), but never by a male.
Cord separation between 3 and 7 days after birth was considered normal; some respondents were concerned in those infrequent cases when separation occurred after first week. The most frequently practiced method of helping the umbilical cord fall in time is shek dewa (also called heda dewa, heat treatment with a ball of cloth and/or warmed fingers). According to the observations and in-depth interviews, heda dewa/shek dewa normally includes holding a cloth on or close to a hot object or the fire, checking it to make sure it is not too hot, placing in on the nari (cord) or nabi (umbilical stump) until it loses its heat, and repeating the process. Another method includes putting one’s thumbs close to the fire and then placing them on the newborn’s umbilical stump, with the focus of the heat massage on the bottom of the stump. We did not detect concern for cleanliness of hands or cloth used for shek dewa during the observations.
The shek dewa treatment continues for 3–4 days after cord separation. If problems occur after the stump separates, people again administer shek dewa, and on advice of the community health worker, might apply gentian violet, or other topical regimens including shidur (vermilion), boric acid powder and cold cream.
To speed cord healing and separation, the stump and surrounding area are cleansed with warm water, soap, Dettol or Savlon, or dried with cloth or a piece of cotton. The majority of informants for the qualitative interviews cleaned the stump two times a day (morning and afternoon), and in a few cases up to four times daily. Application of substances to the stump in the first seven days was reported by 100 (24%) respondents. Most commonly mentioned substances were mustard oil (N=16), ash (N=10), coconut oil (N=7), shidur (N=7) and Dettol (N=6).
Among the 20 families participating in in-depth interviews, all completed the rating/ranking exercise and consistently preferred Nebanol powder, followed by Neobacrin ointment. The least preferred product was gentian violet.
Discussion
Several unhygienic cord care practices are prevalent in Sylhet district, Bangladesh. Such practices have been associated with umbilical cord infections, and therefore efforts to reduce harmful practices and promote interventions that reduce potential exposure of the cord may result in improved neonatal outcomes. Mothers and other female relatives are primary neonatal care-givers, while TBAs play a lesser role. Thus, improved cord care promotion efforts should be targeted to the full range of caregivers.
The fact that mothers themselves, rather than female caregivers or TBAs, cut the cord, strengthens our recommendation that interventions be directed at mothers and other female caregivers. The practice of cord cutting by mothers differs from other parts of Bangladesh and South Asia, where TBAs are reported to play active role in the postpartum period (7, 8). Respondents indicated that cord was cut at a distance from the abdomen (4–7 fingers) generally slightly longer than advised (WHO 1998). While length of the umbilical stump may be associated with cord infection, there are no existing data available and further investigation is warranted. A particularly alarming result is that umbilical cord was not tied prior to cutting for 7% of newborns. A previous study in Bangladesh on risk factors for neonatal tetanus found that mortality from tetanus was significantly higher among those not tying/clamping the cord before cutting (111 per 1000) than among newborns whose cord was tied (24 per 1,000 live births) (9).
Removal of vernix is commonly practiced at time of bath and should be discouraged. Although awareness of the importance of thermal care was high, the majority primarily reported keeping the newborn warm by wrapping it in a blanket or katha and only 2% of respondents reported using skin-to-skin care. Given the known benefits of skin-to-skin care (10) and association with reduced risk of cord infection (11), future interventions should further promote it.
The high proportion of infants receiving mustard oil massage is consistent with numerous previous reports from Bangladesh and the region (6, 12, 13). The neonatal skin plays an important role in protecting the newborn infant from invasive pathogens. Some neonatal care practices in the community, including mustard oil massage, may compromise the skin barrier function, increase trans-epidermal water loss, decrease structural integrity, and increase risk of percutaneous penetration by invasive pathogens, especially for those that are pre-term of low birth weight (12). Given centrality of mustard oil in newborn care, further evaluation is needed of its beneficial and harmful effects.
Caregivers are concerned about timing of separation of the umbilical cord and become worried if it does not fall off after seven days. Most clean the area around the stump and use a method called shek dewa to facilitate the cord separation. If, in future programs, topical chlorhexidine applications to the cord during the first week of life are promoted, improved overall coverage may be achieved by focusing on household members who perform shek dewa. It is known that application of topical antiseptics will generally increase the average time to cord separation (14–17), but in settings where colonization rates and risk of infection are high, the impact of this intervention on separation time is likely to be substantially less. For example, in Nepal the application of chlorhexidine increased the time to cord separation by approximately 24 hours, or 25% (18). Even this short increase in cord separation time may, however, be noticed by caregivers and lead to dissatisfaction with the intervention. There is no evidence that delaying cord separation time increases risk of infection and, if the impact of chlorhexidine cleansing of the cord on omphalitis and mortality risk is confirmed, these benefits would far outweigh any concerns of increased separation time. To achieve acceptability and maintain high coverage, programs promoting cord cleansing with antiseptics should provide appropriate educational messages about the balance between these benefits and the likelihood that separation of umbilical cord may be slightly delayed.
In a quarter of newborns (24%), a substance was applied to the stump. Application of mustard oil, associated with cord infections in Nepal (11), and other substances such as ash, mud, mother’s saliva, ginger and/or chewed rice to cord stump should be discouraged. WHO suggests that cord simply be kept clean and dry, or topical antiseptic such as chlorhexidine used to substitute for traditional harmful practices (19).
Few wash hands before attending to newborn, massaging newborn or applying heat treatment to umbilical cord stump. Even if the TBA, mother or other person caring for newborn washes her hands, she often wipes them on unclean clothing or surfaces. Although evidence is limited on its specific effects, washing hands before handling the newborn may be beneficial. Encouragement to use materials (such as clean cotton) other than fingers for the application of medicine/antiseptic should also be included. Along with promotion of hand washing, messages should stress avoiding recontamination of washed hands before attending to newborn, and hand-washing prior to assisting with delivery.
Conclusion
In the Projahnmo-III intervention trial, information will be given concerning hand-washing prior to assisting with delivery and cord cutting; tying cord prior to cutting; and avoidance of applying specific substances to the cord. The educational component will be targeted to mothers, TBAs, and other family members. Given that cord separation time might be increased, chlorhexidine cleansing will be provided in conjunction with discussion regarding its potential benefits, and delay in cord separation will be minimal and not affect the newborn’s health. Scale-up of chlorhexidine antisepsis of the cord awaits results from the Projahnmo-III trial of chlorhexidine cleansing regimens (1 day, 7 days) as compared to dry cord care. While there is already some use of products with chlorhexidine as an active ingredient such as Savlon, the concentration is far below the minimum concentration recommended by the World Health Organization for this purpose: 4.0% (19). Promotion of the 4% solution is likely to provide greater benefit, and build upon current practices.
Table 1.
Examples of cord care practices at delivery and through progression of cord stump healing and separation
| Type of practice | Specific Examples and citations |
|---|---|
| General hygiene related to delivery | |
| Timing and method for tying (clamping of the cord) | |
| Cutting the cord: instrument and length | |
| Use and disposal of the cord, significance of separation | |
| Topical applications to the cord | |
| Bathing of the infant and other skin care | |
| Wrapping/dressing/bin ding of the cord stump |
Acknowledgments
Source of Support
This study was supported by the Dhaka, Bangladesh Mission of the United States Agency for International Development (USAID) through the GRA Cooperative Agreement # GHS-A-00-03-00019-00. The contents are the responsibility of the authors and do not necessarily reflect the views of USAID or the United States Government.
References
- 1.Lawn JE, Cousens S, Zupan J. 4 million neonatal deaths: when? Where? Why? Lancet. 2005;365(9462):891–900. doi: 10.1016/S0140-6736(05)71048-5. [DOI] [PubMed] [Google Scholar]
- 2.Mullany LC, Darmstadt GL, Tielsch JM. Role of antimicrobial applications to the umbilical cord in neonates to prevent bacterial colonization and infection: a review of the evidence. Pediatr Infect Dis J. 2003;22(11):996–1002. doi: 10.1097/01.inf.0000095429.97172.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perry DS. The umbilical cord: transcultural care and customs. J Nurse Midwifery. 1982;27(4):25–30. doi: 10.1016/0091-2182(82)90166-5. [DOI] [PubMed] [Google Scholar]
- 4.Mullany LC, Darmstadt GL, Khatry SK, Katz J, LeClerq SC, Shrestha S, et al. Topical applications of chlorhexidine to the umbilical cord for prevention of omphalitis and neonatal mortality in southern Nepal: a community-based, cluster-randomised trial. Lancet. 2006;367(9514):910–8. doi: 10.1016/S0140-6736(06)68381-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mullany LCDG, Khatry SK, Katz J, LeClerq SC, Shrestha SR, Adhikari K, Tielsch JM. Topical applications of chlorhexidine to the umbilical for prevention of omphalitis and neonatal mortality in southern Nepal: a community-based, cluster-randomized trial. Lancet. 2006;367:910–918. doi: 10.1016/S0140-6736(06)68381-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Winch PJ, Alam MA, Akther A, Afroz D, Ali NA, Ellis AA, et al. Local understandings of vulnerability and protection during the neonatal period in Sylhet District, Bangladesh: a qualitative study. Lancet. 2005;366(9484):478–85. doi: 10.1016/S0140-6736(05)66836-5. [DOI] [PubMed] [Google Scholar]
- 7.Bhatia S. Traditional childbirth practices: implications for a rural MCH program. Stud Fam Plann. 1981;12(2):66–75. [PubMed] [Google Scholar]
- 8.Goodburn EA, Gazi R, Chowdhury M. Beliefs and practices regarding delivery and postpartum maternal morbidity in rural Bangladesh. Stud Fam Plann. 1995;26(1):22–32. [PubMed] [Google Scholar]
- 9.Islam MS, Rahaman MM, Aziz KM, Munshi MH, Rahman M, Patwari Y. Birth care practice and neonatal tetanus in a rural area of Bangladesh. J Trop Pediatr. 1982;28(6):299–302. doi: 10.1093/tropej/28.6.299. [DOI] [PubMed] [Google Scholar]
- 10.DiMenna L. Considerations for implementation of a neonatal kangaroo care protocol. Neonatal Netw. 2006;25(6):405–12. doi: 10.1891/0730-0832.25.6.405. [DOI] [PubMed] [Google Scholar]
- 11.Mullany LC, Darmstadt GL, Katz J, Khatry SK, LeClerq SC, Adhikari RK, et al. Risk factors for umbilical cord infection among newborns of southern Nepal. Am J Epidemiol. 2007;165(2):203–11. doi: 10.1093/aje/kwj356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Darmstadt GL, Mao-Qiang M, Chi E, Saha SK, Ziboh VA, Black RE, et al. Impact of topical oils on the skin barrier: possible implications for neonatal health in developing countries. Acta Paediatr. 2002;91(5):546–54. doi: 10.1080/080352502753711678. [DOI] [PubMed] [Google Scholar]
- 13.Mullany LC, Darmstadt GL, Khatry SK, Tielsch JM. Traditional massage of newborns in Nepal: implications for trials of improved practice. J Trop Pediatr. 2005;51(2):82–6. doi: 10.1093/tropej/fmh083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Medves JM, O’Brien BA. Cleaning solutions and bacterial colonization in promoting healing and early separation of the umbilical cord in healthy newborns. Can J Public Health. 1997;88(6):380–2. doi: 10.1007/BF03403910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rais-Bahrami K, Schulte EB, Naqvi M. Postnatal timing of spontaneous umbilical cord separation. Am J Perinatol. 1993;10(6):453–4. doi: 10.1055/s-2007-994630. [DOI] [PubMed] [Google Scholar]
- 16.Ronchera-Oms C, Hernandez C, Jimemez NV. Antiseptic cord care reduces bacterial colonization but delays cord detachment. Arch Dis Child Fetal Neonatal Ed. 1994;71(1):F70. doi: 10.1136/fn.71.1.f70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smales O. A comparison of umbilical cord treatment in the control of superficial infection. N Z Med J. 1988;101(849):453–5. [PubMed] [Google Scholar]
- 18.Mullany LC, Darmstadt GL, Khatry SK, LeClerq SC, Katz J, Tielsch JM. Impact of umbilical cord cleansing with 4.0% chlorhexidine on time to cord separation among newborns in southern Nepal: a cluster-randomized, community-based trial. Pediatrics. 2006;118(5):1864–71. doi: 10.1542/peds.2006-1091. [DOI] [PubMed] [Google Scholar]
- 19.World Health Organization. WHO/FHE/MSM-cord care. Geneva: WHO; 1998. Care of the umbilical cord. [Google Scholar]
- 20.Faridi MM, Rattan A, Ahmad SH. Omphalitis neonatorum. J Indian Med Assoc. 1993;91(11):283–5. [PubMed] [Google Scholar]
- 21.Sharma N, Bali P. Care of the newborn by traditional birth attendants. Indian Pediatr. 1989;26(7):649–53. [PubMed] [Google Scholar]
- 22.Bennett J, Azhar N, Rahim F, Kamil S, Traverso H, Killgore G, et al. Further observations on ghee as a risk factor for neonatal tetanus. Int J Epidemiol. 1995;24(3):643–7. doi: 10.1093/ije/24.3.643. [DOI] [PubMed] [Google Scholar]
- 23.Quddus A, Luby S, Rahbar M, Pervaiz Y. Neonatal tetanus: mortality rate and risk factors in Loralai District, Pakistan. Int J Epidemiol. 2002;31(3):648–53. doi: 10.1093/ije/31.3.648. [DOI] [PubMed] [Google Scholar]
- 24.Otoo SN. The traditional management of puberty and childbirth among the Ga people, Ghana. Trop Geogr Med. 1973;25(1):88–94. [PubMed] [Google Scholar]
- 25.Tsu V. Clean home delivery kit: Evaluation of the health impact. Program for Appropriate Technology in Health. 2000 May; [Google Scholar]
- 26.Chongsuvivatwong V, Bucharkorn L, Treetrong R. Traditional birth attendants in an endemic area of tetanus neonatorum in Thailand: pitfalls in the control program. J Community Health. 1991;16(6):325–31. doi: 10.1007/BF01324517. [DOI] [PubMed] [Google Scholar]
- 27.Semali IA. Some aspects of traditional birth attendants’ practice in a rural area in Tanzania. Trans R Soc Trop Med Hyg. 1992;86(3):330–1. doi: 10.1016/0035-9203(92)90336-b. [DOI] [PubMed] [Google Scholar]
- 28.Bennett J, Macia J, Traverso H, Banoagha S, Malooly C, Boring J. Protective effects of topical antimicrobials against neonatal tetanus. Int J Epidemiol. 1997;26(4):897–903. doi: 10.1093/ije/26.4.897. [DOI] [PubMed] [Google Scholar]
- 29.Garner P, Lai D, Baea M, Edwards K, Heywood P. Avoiding neonatal death: an intervention study of umbilical cord care. J Trop Pediatr. 1994;40(1):24–8. doi: 10.1093/tropej/40.1.24. [DOI] [PubMed] [Google Scholar]
- 30.Zupan J, Garner P, Omari AA. Topical umbilical cord care at birth. Cochrane Database Syst Rev. 2004;(3):CD001057. doi: 10.1002/14651858.CD001057.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Idema CD, Harris BN, Ogunbanjo GA, Durrheim DN. Neonatal tetanus elimination in Mpumalanga Province, South Africa. Trop Med Int Health. 2002;7(7):622–4. doi: 10.1046/j.1365-3156.2002.00903.x. [DOI] [PubMed] [Google Scholar]
- 32.Mull DS, Anderson JW, Mull JD. Cow dung, rock salt, and medical innovation in the Hindu Kush of Pakistan: the cultural transformation of neonatal tetanus and iodine deficiency. Soc Sci Med. 1990;30(6):675–91. doi: 10.1016/0277-9536(88)90253-5. [DOI] [PubMed] [Google Scholar]
- 33.Vural G, Kisa S. Umbilical cord care: a pilot study comparing topical human milk, povidone-iodine, and dry care. J Obstet Gynecol Neonatal Nurs. 2006;35(1):123–8. doi: 10.1111/j.1552-6909.2006.00012.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tielsch JM, Darmstadt GL, Mullany LC, Khatry SK, Katz J, LeClerq SC, et al. Impact of newborn skin-cleansing with chlorhexidine on neonatal mortality in southern Nepal: a community-based, cluster-randomized trial. Pediatrics. 2007;119(2):e330–40. doi: 10.1542/peds.2006-1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Darmstadt GL, Saha SK. Traditional practice of oil massage of neonates in Bangladesh. J Health Popul Nutr. 2002;20(2):184–8. [PubMed] [Google Scholar]
- 36.Bennett J, Schooley M, Traverso H, Agha SB, Boring J. Bundling, a newly identified risk factor for neonatal tetanus: implications for global control. Int J Epidemiol. 1996;25(4):879–84. doi: 10.1093/ije/25.4.879. [DOI] [PubMed] [Google Scholar]