Abstract
Rectus femoris transfer is frequently performed to treat stiff-knee gait in subjects with cerebral palsy. In this surgery, the distal tendon is released from the patella and re-attached to one of several sites, such as the sartorius or the iliotibial band. Surgical outcomes vary, and the mechanisms by which the surgery improves knee motion are unclear. The purpose of this study was to clarify the mechanism by which the transferred muscle improves knee flexion by examining three types of transfers. Muscle-actuated dynamic simulations were created of ten children diagnosed with cerebral palsy and stiff-knee gait. These simulations were altered to represent surgical transfers of the rectus femoris to the sartorius and the iliotibial band. Rectus femoris transfers in which the muscle remained attached to the underlying vasti through scar tissue were also simulated by reducing but not eliminating the muscle’s knee extension moment. Simulated transfer to the sartorius, which converted the rectus femoris’ knee extension moment to a flexion moment, produced 32° ± 8° improvement in peak knee flexion on average. Simulated transfer to the iliotibial band, which completely eliminated the muscle’s knee extension moment, predicted only slightly less improvement in peak knee flexion (28° ± 8°). Scarred transfer simulations, which reduced the muscle’s knee extension moment, predicted significantly less (p < 0.001) improvement in peak knee flexion (14° ± 5°). Simulations revealed that improved knee flexion following rectus femoris transfer is achieved primarily by reduction of the muscle’s knee extension moment. Reduction of scarring of the rectus femoris to underlying muscles has the potential to enhance knee flexion.
Introduction
Stiff-knee gait, characterized by diminished and delayed peak knee flexion in swing (Sutherland and Davids, 1993), is one of the most common gait problems in children with cerebral palsy (Wren et al., 2005). Insufficient knee flexion during swing can lead to tripping and falling, and energy-inefficient compensatory movements. Despite the prevalence of stiff-knee gait, its causes are not well understood. Several factors may contribute to stiff-knee gait (Goldberg et al., 2003; Kerrigan et al., 1999; Kerrigan and Glenn, 1994; Piazza and Delp, 1996; Riley and Kerrigan, 1998), but over-activity of the rectus femoris muscle is considered a primary cause (Perry, 1987; Sutherland et al., 1990; Waters et al., 1979). Treatments including rectus femoris transfer surgery and botulinum toxin injection aim to alter the function of this muscle. A rectus femoris transfer relocates the insertion of the rectus femoris from the patella to a more posterior site to augment knee flexion (Perry, 1987; Gage et al., 1987).
Average improvement in knee flexion after rectus femoris transfer is positive but variable. Most studies report an average increase in peak knee flexion after transfer between 7–10° (Gage et al., 1987; Õunpuu et al., 1993b; Chambers et al., 1998; Moreau et al., 2005; Saw et al., 2003). Some studies report increases in peak knee flexion between 12–26° (Sutherland et al., 1990; Miller et al., 1997; Hemo et al., 2007). Even studies that report no significant improvement (Õunpuu et al., 1993a; Hadley et al., 1992; Rethlefsen et al., 1999) or an average decrease (Carney et al., 2003; Yngve et al., 2002) in peak knee flexion in swing find that patients exhibit an average increase in knee range of motion, typically when rectus femoris transfers are performed in conjunction with hamstrings lengthenings. There is limited understanding of how the transferred rectus femoris affects knee motion and a lack of consensus regarding the effects of transfer site. Several studies have reported no difference among transfer sites on peak knee flexion improvement (Õunpuu et al., 1993a; Muthusamy et al., 2006), whereas others have suggested that outcome is dependent on transfer site (Chung et al., 1997; Hemo et al., 2007).
The mechanism by which rectus femoris transfer may increase knee flexion is unclear. The transfer was originally intended to convert the muscle from a knee extensor to a knee flexor (Perry, 1987), and a study on cadavers showed that the rectus femoris has a knee flexion moment arm after transfer to the sartorius or semitendinosis (Delp et al., 1994). However, examination of postoperative patients revealed that the transferred muscle generates a knee extension moment upon electrical stimulation (Riewald and Delp, 1997). In vivo dynamic imaging confirmed that the muscle is not converted to a knee flexor but that the knee extension capacity of the rectus femoris is diminished after surgery (Asakawa et al., 2002). In these same subjects, magnetic resonance imaging also revealed the formation of scar tissue between the rectus femoris and the vasti postoperatively. This connective tissue may allow force to be transmitted from the rectus femoris to the vasti, resulting in the rectus femoris producing a net knee extension moment despite transfer of its distal tendon to the sartorius or semitendinosus (Asakawa et al., 2004). A proposed mechanism of improvement in knee flexion after rectus femoris transfer is reduction of the muscle’s knee extension moment with preservation of its hip flexion moment (Delp et al., 1994; Riewald and Delp, 1997; Asakawa et al., 2002), which promotes knee flexion through dynamic coupling (Piazza and Delp, 1996; Kerrigan et al., 1998). However, there is little evidence indicating whether this mechanism is likely to increase knee flexion in patients with stiff-knee gait following rectus femoris surgery.
The purpose of this study was to investigate the mechanisms of improved knee flexion after rectus femoris transfer by comparing the changes in knee flexion predicted by simulating transfers to sartorius, transfers to iliotibial band, scarred rectus femoris transfers, and botulinum toxin injection of the rectus femoris. This study evaluated the relative importance of the transferred muscle’s hip and knee moments by analyzing subject-specific simulations of children with stiff-knee gait.
Methods
Muscle-actuated simulations were created to investigate the mechanism by which rectus femoris transfer alters muscle function. We created simulations that reproduced the gait dynamics of ten subjects with stiff-knee gait prior to treatment. The rectus femoris was then altered to simulate the effects of different treatments. Resulting changes in peak knee flexion were compared.
Subjects
All ten subjects in this study were diagnosed with cerebral palsy and classified as exhibiting stiff-knee gait (Fig. 1). To be classified as “stiff” the subject’s knee motion was outside a normal range by more than two standard deviations for at least three of four gait parameters: (1) peak knee flexion angle, (2) range of knee flexion in early swing (from toe-off to peak knee flexion), (3) total range of knee motion, and (4) timing of peak knee flexion in swing (Goldberg et al., 2006). Control data was collected from 15 typical children of approximately the same average age, height, and weight as the subjects with stiff-knee gait. Each stiff-knee subject underwent a physical exam and gait analysis at Connecticut Children’s Medical Center in Hartford, CT. All subjects met the following selection criteria: (i) underwent rectus femoris transfer surgery to treat stiff-knee gait, (ii) were 6 - 17 years of age at surgery, (iii) had not undergone a selective dorsal rhizotomy, and (iv) walked without orthoses or other assistance. The group of subjects had an average age of 10.6 years. Rectus femoris was transferred distally to sartorius in all subjects. Retrospective analysis of these data was performed with approval of participating institutions.
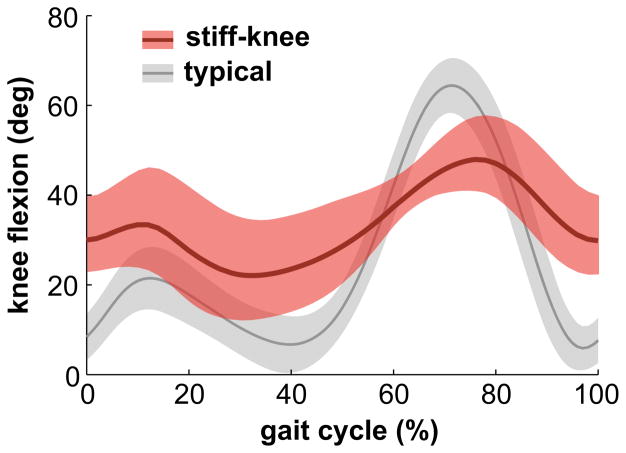
Figure 1.
Average experimental knee flexion (in more stiff limb) of ten subjects with stiff-knee gait (thick line) ± one standard deviation (dark shaded region), compared to average knee flexion of typical subjects (thin line) ± one standard deviation (light shaded region).
Creating subject-specific simulations
The musculoskeletal system was represented by a three-dimensional model with 21 degrees of freedom and 92 muscle-tendon actuators. The position and orientation of the pelvis segment with respect to ground was defined with six degrees of freedom. A single rigid segment articulating with the pelvis by a ball and socket joint represented the head, arms, and torso. Each hip was modeled as a ball and socket joint, each knee as a planar joint with tibiofemoral and patellofemoral kinematics defined by knee flexion angle (Delp et al., 1990), and each ankle and subtalar joint as revolute joints (Inman, 1976). The musculoskeletal model and corresponding dynamic simulation code were produced using SIMM (Delp and Loan, 2000) and SD/FAST (Parametric Technology Corporation, Waltham, MA).
The musculoskeletal model was scaled to match the size and weight of each subject. Next, we solved for the joint angles that minimized the distances between virtual markers on the model and experimentally measured marker positions. Then, a residual elimination algorithm (Thelen and Anderson, 2006) was applied to make model kinematics consistent with measured ground reaction forces by adjusting pelvis translations and back angles. Finally, computed muscle control (Thelen et al., 2003) was utilized to determine a set of muscle excitations that produced a forward simulation of the subject’s preoperative kinematics. The muscle excitations were constrained to be consistent with measured EMG patterns. Sagittal knee, hip, and ankle angles were within 3° of measured preoperative angles. Simulations represented a portion of the gait cycle from preswing to peak knee flexion, centered around toe-off.
Comparing effects of simulated treatments on knee flexion
Three types of rectus femoris transfers and a botulinum toxin injection into the rectus femoris were simulated for each subject. The three different types of rectus femoris transfer investigated included transfer to the sartorius, transfer to the iliotibial band, and a transfer in which rectus femoris was scarred to the underlying vasti. The preoperative musculoskeletal model for each subject (Fig. 2a) was altered to represent each transfer scenario. The tendon slack length of the transferred muscle was adjusted to keep muscle fibers operating near preoperative length ranges. The set of muscle excitations from each subject’s preoperative simulation was applied to each transfer model to simulate the effects of the surgery.
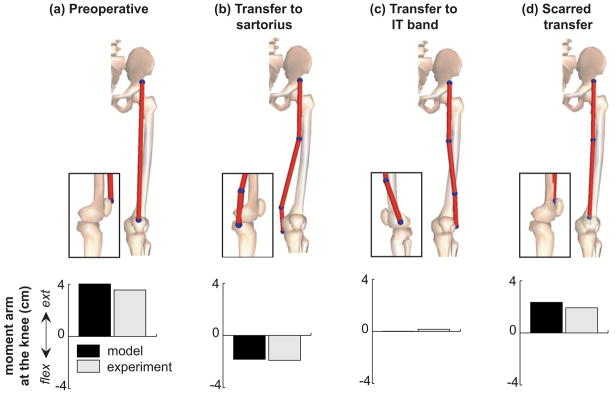
Figure 2.
Illustrations of the rectus femoris muscle (top panels) and its moment arm at the knee averaged over 20–60 degrees of knee flexion (bottom panels). The moment arms of the models (black bars) are compared with moment arms measured experimentally (grey bars) by Delp et al. (1994) in cadaver specimens in the (a) preoperative condition, after (b) transfer to the sartorius, and after (c) transfer to the iliotibial band. The muscle insertions shown in models (b) and (c) are effective insertions used to calculate moment arms (see Methods). The muscle’s knee extension moment arm in the (d) scarred transfer model is compared to its moment arm calculated from in vivo measurements of the muscle’s displacement in the patient from Asakawa et al. (2002) with the minimum reduction in knee extension moment arm after rectus femoris transfer.
To simulate a transfer of the rectus femoris to the sartorius the rectus femoris insertion was relocated to the effective insertion of the sartorius in the model (Fig. 2b). Even though the effective insertion of the sartorius is more proximal and posterior than the anatomical insertion, the simulated rectus femoris transfer closely approximates moment arms of transferred muscles measured experimentally by Delp et al. (1994; compare model to experiment in Fig. 2b). To simulate the negligible knee extension moment arm (0–5 mm) measured by Delp et al. (1994) after transfer to the iliotibial band, the muscle’s insertion was fixed on the femur, transforming it into a uniarticular hip flexor. To simulate the effects of a transfer surgery in which the rectus femoris becomes scarred to the underlying vasti we reduced the knee extension moment arm of rectus femoris by half (Fig. 2d). Although the model for the scarred transfer does not resemble a typical transfer surgery, it represents the net effect of a scarred rectus femoris transfer on the muscle’s knee extension capacity based on the subject who showed the least reduction in rectus femoris knee extension capacity in the study of Asakawa et al. (2002). To simulate the effects of injection of botulinum toxin into the rectus femoris, which decreases active muscle force by inhibiting the release of acetylcholine from the neuromuscular junction (Burgen et al., 1949), we applied the set of muscle excitations in the preoperative simulation to the preoperative model but eliminated rectus femoris excitation.
After creating simulations of each treatment for each subject, the improvements in peak knee flexion, measured at the point of preoperative peak knee flexion, were quantified (Fig. 3). The average amounts of peak knee flexion improvement for all subjects were compared among treatments, using a two-tailed, paired t-test (p < 0.05) with Bonferroni correction for multiple comparisons.
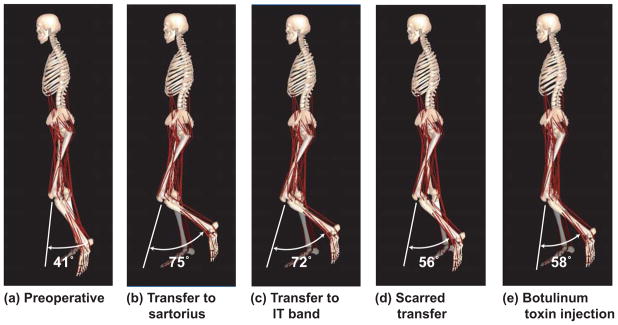
Figure 3.
Peak knee flexion resulting from simulation of (a) preoperative gait, (b) RF transfer to sartorius, (c) RF transfer to iliotibial band, (d) scarred RF transfer, and (e) botulinum toxin injection for a single subject.
Comparing influence of hip and knee moments of rectus femoris on knee flexion
To investigate the relative importance of the hip and knee moments of transferred rectus femoris on peak knee flexion in swing, we analyzed four additional simulations for each subject to represent conditions under which the hip and knee moments of the muscle were separately eliminated or preserved. The simulations of each subject’s preoperative gait served as the first condition that preserved both hip and knee moments of the muscle. A second model was created for each subject in which the muscle’s knee extension moment was eliminated, while its hip flexion capacity after transfer was preserved. We preserved the transferred muscle’s hip flexion capacity by maintaining its hip flexion moment arm and adjusting tendon slack length to approximate the range of fiber operating lengths in the preoperative simulation. A third model was created for each subject in which the muscle’s hip flexion moment was eliminated while its knee extension moment was preserved. A fourth model was created for each subject in which rectus femoris was removed from the model, eliminating both hip and knee moments.
The set of muscle excitations found for each subject’s preoperative simulation was applied to each model to simulate the effects of each condition on knee flexion. We compared the changes in peak knee flexion from the preoperative condition using a two-tailed, paired t-test (p < 0.05) with Bonferroni correction.
Results
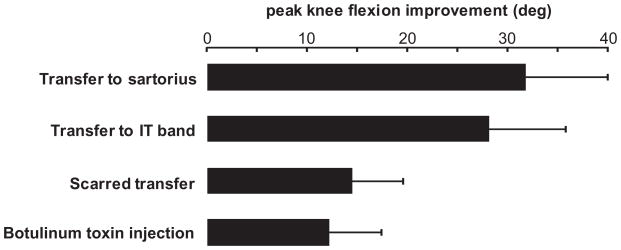
The largest improvement in peak knee flexion (32° ± 8°) occurred after simulated transfer of the rectus femoris to sartorius (Fig. 4). Transfer of the muscle to the iliotibial band predicted a smaller (p < 0.001) improvement in peak knee flexion (28° ± 8°). Simulated scarred rectus femoris transfer resulted in an average improvement in peak knee flexion of 14° ± 5°, which was significantly less (p < 0.001) than the average improvement from unscarred transfer to either the sartorius or the iliotibial band. Simulated botulinum toxin injection to the rectus femoris, which eliminated the muscle’s active hip flexion and knee extension moments, resulted in an average improvement of 12° ± 5° in knee flexion.
Figure 4.
Average increases (and one standard deviation) in peak knee flexion of the subject group for each of the simulated treatments.
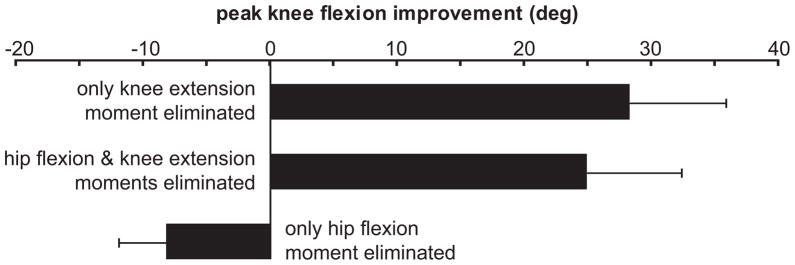
The knee extension moment of rectus femoris was more influential than its hip flexion moment on peak knee flexion (Fig. 5). All subjects showed larger (p < 0.001) increase in peak knee flexion (28° on average) when knee extension moment was eliminated compared to decrease in peak knee flexion (−8° on average) when hip flexion moment was eliminated. In the absence of the muscle’s knee extension moment, average improvement in peak knee flexion was 3° greater (p < 0.001) with hip flexion moment than without hip flexion moment.
Figure 5.
Average increases (and one standard deviation) in peak knee flexion of the subject group for simulations in which knee extension or hip flexion moments of rectus femoris were independently eliminated.
Discussion
Our results suggest that the primary mechanism by which rectus femoris transfer improves knee flexion is the reduction of the rectus femoris’ knee extension moment. Previous observations that the surgery diminishes knee extension moment but generally does not convert the rectus femoris to a knee flexor (Asakawa et al., 2002; Riewald and Delp, 1997) support this finding.
A secondary mechanism of improvement is preservation of some of the muscle’s hip flexion moment, which induces knee flexion (Piazza and Delp, 1996; Riley and Kerrigan, 1998). However, it is likely the hip flexion moment generated by the rectus femoris is diminished after transfer. The hip flexion moment generated by the rectus femoris could not be preserved in simulations in which the muscle’s insertion was relocated. In the preoperative simulation, the rectus femoris lengthened due to the patella translating distally on the femur with knee flexion. In the transfer simulations in which the rectus femoris was relocated from the patella the muscle shortened. Concentric muscle contraction in the transfer simulations produced less force than the eccentric muscle contraction in the preoperative simulations; this reduced the hip flexion moment generated by the rectus femoris in transfer simulations. This suggests that when the rectus femoris is transferred from its insertion on the patella the muscle’s hip flexion moment may not be preserved, reducing the contribution of the muscle’s hip flexion moment to knee flexion and increasing the importance of reducing, or eliminating, the muscle’s knee extension moment.
Our results show that rectus femoris transfers to either the sartorius or the iliotibial band predicted greater improvements in peak knee flexion than a scarred transfer, suggesting that methods to reduce postoperative scarring of the muscle to underlying vasti may be beneficial. Transfer to the sartorius predicted only slightly greater peak knee flexion in swing (approximately 4°) than transfer to the iliotibial band, even though the simulated transfer to the sartorius converted the muscle to a knee flexor. Although the rectus femoris had a knee flexion moment arm in the model of transfer to the sartorius, the amount of force the rectus femoris produced was diminished after transfer since the change in muscle path caused the muscle to shorten rather than lengthen while contracting. Transfer to semitendinosus or gracilis, which have larger knee flexion moment arms than sartorius, may result in larger changes in knee flexion. Transfer to sartorius was investigated in this study because of its prevalence as a surgical option (Gage et al., 1987; Õunpuu et al., 1993a; Saw et al., 2003; Moreau et al., 2005; Hemo et al., 2007).
Simulated botulinum toxin injection to the rectus femoris predicted less peak knee flexion improvement than transfer of the muscle. This is likely due to the preservation of detrimental passive knee extension moments (i.e., the knee extension moment generated by stretch of the rectus femoris even when it is inactive) and elimination of helpful active hip flexion moments. The simulated result may overestimate anticipated clinical improvement since injection of botulinum toxin is unlikely to achieve complete elimination of active muscle force. Stoquart et al. (2008) reported a 5° average increase in peak knee flexion after botulinum toxin injection into rectus femoris in adults with stiff-knee gait due to stroke. Other studies have reported no significant change (Chantraine et al., 2005) and 9° average improvement (Sung and Bang, 2000) in peak knee flexion after motor branch block of the rectus femoris in patients with stiff-knee gait.
Simulations of rectus femoris transfers to the sartorius and the iliotibial band resulted in larger peak knee flexion improvements than those reported clinically or observed in the postoperative kinematics of our subjects (2° ± 13°) measured approximately one year postoperatively. This is likely to occur because the rectus femoris may not produce the intended knee flexion moment due to scarring of the transferred muscle to underlying soft tissues (Asakawa et al., 2004). Also, the subjects in this study were treated with other surgeries that may affect knee flexion. All ten subjects received hamstrings lengthenings and many received additional bony or soft-tissue surgeries. We have not attempted to model the effects of concomitant surgeries in our subject group because our goal was to isolate the effects of rectus femoris transfer surgery. Our simulations of scarred rectus femoris transfers predict improvements in knee flexion of 14° on average, which is similar to a clinical report of 12° of increase after isolated rectus femoris transfer (Hemo et al., 2007).
Several assumptions were made in implementing the gait simulations. First, the muscle excitations used to drive the treatment simulations were assumed to remain unchanged from preoperative simulations. While some muscle excitations are likely to change, Patikas et al. (2007) found no significant changes in rectus femoris activity after multilevel surgery, including rectus femoris transfer. Secondly, muscle parameters prescribed in these models were based on data for typical adults, which are unlikely to be accurate representations of muscles in children with cerebral palsy. Additionally, our subject-specific models were scaled to the sizes of each subject and accurately represented the kinematics and kinetics measured preoperatively for each subject, but did not replicate skeletal deformities or contractures which may have been present. Also, we cannot be certain that the muscle forces produced in our simulations accurately represented the forces generated by individual subjects in vivo, although the net joint moments and muscle excitations in the preoperative simulations were consistent with those measured in the gait lab. Finally, we modeled the net effect of a scarred transfer by reducing the average moment arm of rectus femoris at the knee by half. This is an approximation of the function of a scarred transfer, and may not represent secondary effects of scarring or variations in the actual moment arm of the transferred muscle throughout a range of knee flexion. Although different modeling assumptions may have resulted in different peak knee flexion improvements, the relationships of improvement in peak knee flexion among treatments would not be likely to change since the same assumptions were used in each treatment simulation.
Our dynamic simulations of individual subjects with stiff-knee gait revealed that substantial improvement in peak knee flexion in swing after rectus femoris transfer may be obtained by reducing the muscle’s knee extension moment. Preserving the muscle’s hip flexion moment may provide some additional improvement, but was less influential than decreasing the muscle’s knee extension moment. Surgeries that intend to convert the rectus femoris to a knee flexor may instead only reduce its knee extension moment, possibly due to scarring (Asakawa et al., 2002). Reducing postoperative scarring of the rectus femoris to underlying tissues may improve postoperative peak knee flexion in swing.
Acknowledgments
We are grateful to Allison Arnold, May Liu, Darryl Thelen, and the staff of the Center for Motion Analysis at the Connecticut Children’s Medical Center. Funding for this work was provided by a National Science Foundation Graduate Fellowship, NIH R01 HD046814, and NIH Roadmap for Medical Research U54 GM072970.
Footnotes
Conflict of interest
None of the authors has a conflict of interest regarding this manuscript.
References
- Anderson FC, Pandy MG. A dynamic optimization solution for vertical jumping in three dimensions. Computer Methods in Biomechanics and Biomedical Engineering. 1999;2:201–231. doi: 10.1080/10255849908907988. [DOI] [PubMed] [Google Scholar]
- Asakawa DS, Blemker SS, Gold GE, Delp SL. In vivo motion of the rectus femoris muscle after tendon transfer surgery. Journal of Biomechanics. 2002;35:1029–1037. doi: 10.1016/s0021-9290(02)00048-9. [DOI] [PubMed] [Google Scholar]
- Asakawa DS, Blemker SS, Rab GT, Bagley A, Delp SL. Three-dimensional muscle-tendon geometry after rectus femoris tendon transfer. Journal of Bone and Joint Surgery. 2004;86:348–354. doi: 10.2106/00004623-200402000-00019. [DOI] [PubMed] [Google Scholar]
- Burgen ASV, Dickens J, Zatman LJ. The action of botulinum toxin on the neuro-muscular junction. Journal of Physiology. 1949;109:10–24. doi: 10.1113/jphysiol.1949.sp004364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carney BT, Oeffinger D. Sagittal knee kinematics following combined hamstring lengthening and rectus femoris transfer. Journal of the Southern Orthopaedic Association. 2003;12:149–153. [PubMed] [Google Scholar]
- Chambers H, Lauer A, Kaufman K, Cardelia JM, Sutherland D. Prediction of outcome after rectus femoris surgery in cerebral palsy: the role of cocontraction of the rectus femoris and vastus lateralis. Journal of Pediatric Orthopaedics. 1998;18:703–711. [PubMed] [Google Scholar]
- Chung CY, Stout J, Gage JR. Rectus femoris transfer – gracilis versus sartorius. Gait and Posture. 1997;6:137–146. [Google Scholar]
- Delp SL, Loan JP. A computational framework for simulation and analysis of human and animal movement. IEEE Computing in Science and Engineering. 2000;2:46–55. [Google Scholar]
- Delp SL, Loan JP, Hoy MG, Zajac FE, Topp EL, Rosen JM. An interactive graphics-based model of the lower extremity to study orthopaedic surgical procedures. IEEE Transactions on Biomedical Engineering. 1990;37:757–767. doi: 10.1109/10.102791. [DOI] [PubMed] [Google Scholar]
- Delp SL, Ringwelski DA, Carroll NC. Transfer of the rectus femoris: effects of transfer site on moment arms about the knee and hip. Journal of Biomechanics. 1994;27:1201–1211. doi: 10.1016/0021-9290(94)90274-7. [DOI] [PubMed] [Google Scholar]
- Gage JR, Perry J, Hicks RR, Koop S, Werntz JR. Rectus femoris transfer to improve knee function of children with cerebral palsy. Developmental Medicine and Child Neurology. 1987;29:159–166. doi: 10.1111/j.1469-8749.1987.tb02131.x. [DOI] [PubMed] [Google Scholar]
- Goldberg SR, Õunpuu S, Arnold AS, Gage JR, Delp SL. Kinematic and kinetic factors that correlate with improved knee flexion following treatment for stiff-knee gait. Journal of Biomechanics. 2006;39:689–698. doi: 10.1016/j.jbiomech.2005.01.015. [DOI] [PubMed] [Google Scholar]
- Goldberg SR, Õunpuu S, Delp SL. The importance of swing-phase initial conditions in stiff-knee gait. Journal of Biomechanics. 2003;36:1111–1116. doi: 10.1016/s0021-9290(03)00106-4. [DOI] [PubMed] [Google Scholar]
- Hadley N, Chambers C, Scarborough N, Cain T, Rossi D. Knee motion following multiple soft-tissue releases in ambulatory patients with cerebral palsy. Journal of Pediatric Orthopaedics. 1992;12:324–328. doi: 10.1097/01241398-199205000-00008. [DOI] [PubMed] [Google Scholar]
- Hemo Y, Aiona MD, Pierce RA, Dorociak R, Sussman MD. Comparison of rectus femoris transposition with traditional transfer for treatment of stiff knee gait in patients with cerebral palsy. Journal of Children’s Orthopaedics. 2007;1:37–41. doi: 10.1007/s11832-006-0002-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inman VT. The Joints of the Ankle. Williams and Wilkins Co; Baltimore, MD: 1976. [Google Scholar]
- Kerrigan DC, Bang MS, Burke DT. An algorithm to assess stiff-legged gait in traumatic brain injury. The Journal of Head Trauma Rehabilitation. 1999;14:136–145. doi: 10.1097/00001199-199904000-00004. [DOI] [PubMed] [Google Scholar]
- Kerrigan DC, Roth RS, Riley PO. The modeling of adult spastic paretic stiff-legged gait swing period based on actual kinematic data. Gait and Posture. 1998;7:117–124. doi: 10.1016/s0966-6362(97)00040-4. [DOI] [PubMed] [Google Scholar]
- Kerrigan DC, Glenn MB. An illustration of clinical gait laboratory use to improve rehabilitation management. American Journal of Physical Medicine and Rehabilitation. 1994;73:421–427. doi: 10.1097/00002060-199411000-00007. [DOI] [PubMed] [Google Scholar]
- Miller F, Cardoso Dias R, Lipton GE, Albarracin JP, Dabney KW, Castagno P. The effect of rectus EMG patterns on the outcome of rectus femoris transfers. Journal of Pediatric Orthopaedics. 1997;17:603–607. doi: 10.1097/00004694-199709000-00006. [DOI] [PubMed] [Google Scholar]
- Moreau N, Tinsley S, Li L. Progression of knee joint kinematics in children with cerebral palsy with and without rectus femoris transfers: a long-term follow up. Gait and Posture. 2005;22:132–137. doi: 10.1016/j.gaitpost.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Muthusamy K, Seidl AJ, Fries RM. Rectus femoris transfer in children with cerebral palsy: evaluation of transfer site and preoperative indicators. Gait and Posture. 2006;24:S137–S138. doi: 10.1097/BPO.0b013e3181804c04. [DOI] [PubMed] [Google Scholar]
- Õunpuu S, Muik E, Davis RB, Gage JR, DeLuca PA. Rectus femoris surgery in children with cerebral palsy. Part I: The effect of rectus femoris transfer location on knee motion. Journal of Pediatric Orthopaedics. 1993a;13:325–330. doi: 10.1097/01241398-199305000-00010. [DOI] [PubMed] [Google Scholar]
- Õunpuu S, Muik E, Davis RB, 3rd, Gage JR, DeLuca PA. Rectus femoris surgery in children with cerebral palsy. Part II: A comparison between the effect of transfer and release of the distal rectus femoris on knee motion. Journal of Pediatric Orthopaedics. 1993b;13:331–335. doi: 10.1097/01241398-199305000-00011. [DOI] [PubMed] [Google Scholar]
- Patikas D, Wolf SI, Schuster W, Armbrust P, Dreher T, Döderlein L. Electromyographic patterns in children with cerebral palsy: do they change after surgery? Gait Posture. 2007;26:362–71. doi: 10.1016/j.gaitpost.2006.10.012. [DOI] [PubMed] [Google Scholar]
- Perry J. Distal rectus femoris transfer. Developmental Medicine and Child Neurology. 1987;29:153–158. doi: 10.1111/j.1469-8749.1987.tb02130.x. [DOI] [PubMed] [Google Scholar]
- Piazza SJ, Delp SL. The influence of muscles on knee flexion during the swing phase of gait. Journal of Biomechanics. 1996;29:723–733. doi: 10.1016/0021-9290(95)00144-1. [DOI] [PubMed] [Google Scholar]
- Rethlefsen S, Tolo VT, Reynolds RA, Kay R. Outcome of hamstring lengthening and distal rectus femoris transfer surgery. Journal of Pediatric Orthopaedics. 1999;8:75–79. [PubMed] [Google Scholar]
- Riewald SA, Delp SL. The action of the rectus femoris muscle following distal tendon transfer: does it generate a knee flexion moment? Developmental Medicine and Child Neurology. 1997;39:99–105. doi: 10.1111/j.1469-8749.1997.tb07391.x. [DOI] [PubMed] [Google Scholar]
- Riley PO, Kerrigan DC. Torque action of two-joint muscles in the swing period of stiff-legged gait: a forward dynamic model analysis. Journal of Biomechanics. 1998;31:835–840. doi: 10.1016/s0021-9290(98)00107-9. [DOI] [PubMed] [Google Scholar]
- Saw A, Smith PA, Sirirungruangsarn Y, Chen S, Hassani S, Harris G, Kuo KN. Rectus femoris transfer for children with cerebral palsy: long-term outcome. Journal of Pediatric Orthopaedics. 23:672–678. doi: 10.1097/00004694-200309000-00020. [DOI] [PubMed] [Google Scholar]
- Stoquart GG, Detrembleur C, Palumbo S, Deltombe T, Lejeune TM. Effect of botulinum toxin injection in the rectus femoris on stiff-knee gait in people with stroke: a prospective observational study. Archives of Physical Medicine and Rehabilitation. 2008;89:56–61. doi: 10.1016/j.apmr.2007.08.131. [DOI] [PubMed] [Google Scholar]
- Sung DH, Bang HJ. Motor branch block of the rectus femoris: its effectiveness in stiff-legged gait in spastic paresis. Archives of Physical Medicine and Rehabilitation. 2000;81:910–915. doi: 10.1053/apmr.2000.5615. [DOI] [PubMed] [Google Scholar]
- Sutherland DH, Davids JR. Common gait abnormalities of the knee in cerebral palsy. Clinical Orthopaedics and Related Research. 1993;288:139–147. [PubMed] [Google Scholar]
- Sutherland DH, Santi M, Abel MF. Treatment of stiff-knee gait in cerebral palsy: a comparison by gait analysis of distal rectus femoris transfer versus proximal rectus release. Journal of Pediatric Orthopaedics. 1990;10:433–441. [PubMed] [Google Scholar]
- Thelen DG, Anderson FC, Delp SL. Generating dynamic simulations of movement using computed muscle control. Journal of Biomechanics. 2003;36:321–328. doi: 10.1016/s0021-9290(02)00432-3. [DOI] [PubMed] [Google Scholar]
- Thelen DG, Anderson FC. Using computed muscle control to generate forward dynamic simulations of human walking from experimental data. Journal of Biomechanics. 2006;39:1107–1115. doi: 10.1016/j.jbiomech.2005.02.010. [DOI] [PubMed] [Google Scholar]
- Waters RL, Garland DE, Perry J. Stiff-legged gait in hemiplegia: surgical correction. Journal of Bone and Joint Surgery. 1979;61-A:927–933. [PubMed] [Google Scholar]
- Wren TA, Rethlefsen S, Kay RM. Prevalence of specific gait abnormalities in children with cerebral palsy: influence of cerebral palsy subtype, age, and previous surgery. Journal of Pediatric Orthopaedics. 2005;25:79–83. doi: 10.1097/00004694-200501000-00018. [DOI] [PubMed] [Google Scholar]
- Yamaguchi GT, Zajac FE. A planar model of the knee joint to characterize the knee extensor mechanism. Journal of Biomechanics. 1989;22:1–10. doi: 10.1016/0021-9290(89)90179-6. [DOI] [PubMed] [Google Scholar]
- Yngve DA, Scarborough N, Goode B, Haynes R. Rectus and hamstring surgery in cerebral palsy: a gait analysis study of results by functional ambulation level. Journal of Pediatric Orthopaedics. 2002;22:672–676. [PubMed] [Google Scholar]
- Zajac FE. Muscle and tendon: properties, models, scaling, and application to biomechanics and motor control. Critical Reviews in Biomedical Engineering. 1989;17:359–411. [PubMed] [Google Scholar]
- Zajac FE, Gordon ME. Determining muscle’s force and action in multi-articular movement. Exercise and Sport Sciences Reviews. 1989;17:187–230. [PubMed] [Google Scholar]