Abstract
The incidence of obesity, insulin resistance and type 2 diabetes (T2D) is increasing at an alarming rate worldwide. Emerging experimental evidence suggests that the hormone melatonin plays an important role in the regulation of glucose metabolisms. In this study we report that removal of melatonin receptor type 1 (MT1) significantly impairs the ability of mice to metabolize glucose and such inability is probably due to an increased insulin resistance in these mice. Our data suggest that MT1 receptors are implicated in the pathogenesis of T2D and open the door for a detailed exploration on the mechanisms by which MT1 receptors signaling may affect glucose metabolism.
Keywords: Melatonin, Melatonin receptors, Diabetes, Insulin Resistance
Introduction
Elevated plasma levels of insulin and glucose due to insulin resistance are believed to be the origin of metabolic syndrome and Type 2 Diabetes (T2D). The incidence of these pathologies is increasing at an alarming rate worldwide. Melatonin plays an important role in many aspects of mammalian physiology by acting via two types of G protein coupled receptors (MT1 and MT2) (1). Previous studies have suggested a role for the pineal gland and melatonin in the regulation of carbohydrate metabolism (2). Additional investigations have also indicated that melatonin receptors are present on pancreatic islets and insulin secretion from isolated islets can be regulated by melatonin (3). Finally a study using melatonin receptor knock-out mice has indicated an active role of these receptors in the regulation of blood glucose (4). A recent paper has also reported that melatonin treatment can improve glucose metabolism in an insulin-resistant mouse model by restoring the action of insulin on the vasculature (5). Additional support for a role of melatonin the regulation of glucose metabolism has been provided by a series of studies that have linked melatonin receptor type 2 (MT2 or MTNR1B) in the pathogenesis of T2D (6,7). The aim of the present study was to investigate glucose metabolism in melatonin receptor knock-out mice.
Materials and Methods
C3H MT1−/−MT2−/− knock-out mice homozygous for the rd1 mutation, generously donated by Drs. Reppert and Weaver (University of Massachusetts Medical School), were back-crossed with C3H/f+/+ mice in which the rd1 mutation has been removed to produce C3H/f+/+MT1−/− and C3Hf+/+MT2−/− (8). Mice were maintained in a 12-h light/12-h dark cycle (light-on at 07:00 am light-off at 7:00 pm). at Morehouse School of Medicine. All the mice used in our experiments were male at the age of 3–4 months.
To determine their glucose tolerance mice were placed in clean cages (without food) 12 h before the experiment and were injected intraperitoneally (i.p., 0.6 ml) with glucose (1.5 mg/g of body weight; 20% glucose in 0.9% NaCl). Blood glucose levels were measured before the injection of glucose and at 20, 40, 100 min after injection. To measure insulin tolerance mice were placed in clean cages (without food) 12 h before testing and injected i.p. (0.6 ml) with 0.5–1.0 unit/kg of body weight of insulin (Humalog, Lilly, Indianapolis, IN) in 0.9% NaCl. Blood glucose was measured by using a One Touch Basic glucometer (Lifescan, Milpitas, CA) before injection of insulin and at 20, 40, 100 mins after insulin injection.
Hemoglobin1Ac levels were measured using a commercially available kit (Bayer Inc, Pittsburgh, PA). Controls were injected i.p. (0.6 ml) with vehicle (0.9% NaCl). All the experiments were performed at Zeitgeber Time (ZT) 6. It is conventional to divide the 24-hour LD cycle into 24-hour ZT units and indicate the time of lights-on as ZT0 and the time of lights-off as ZT12.
Results
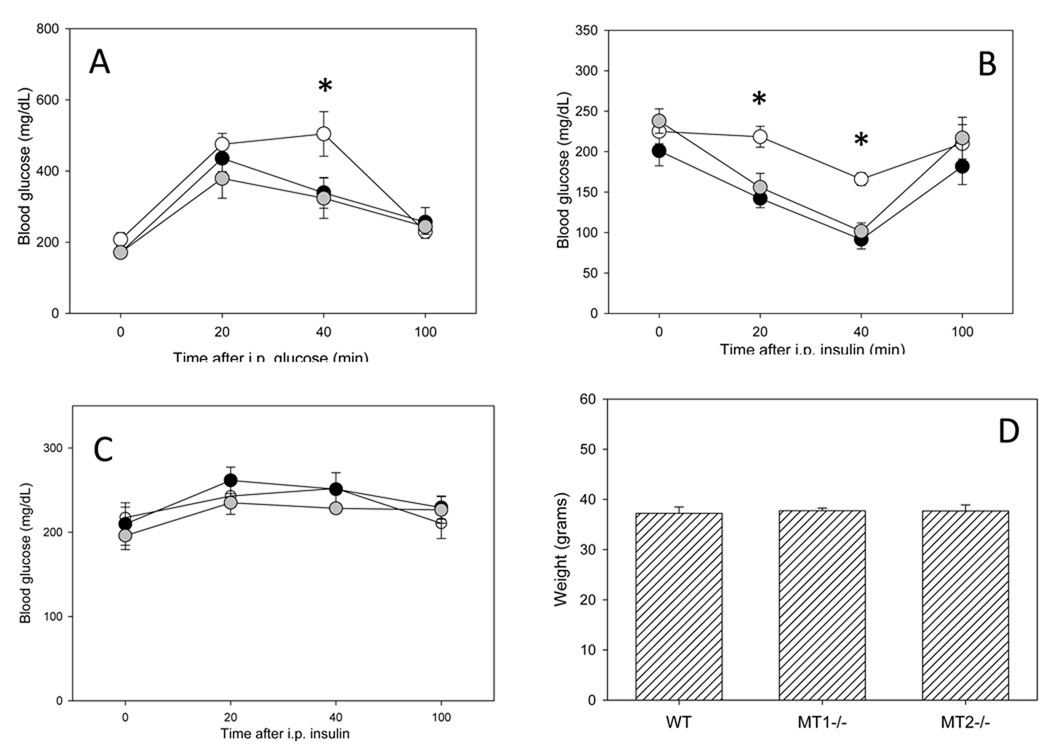
In Figure 1 are shown the levels of normal resting glucose levels and body weights in WT and melatonin receptor knock-out mice. Although MT1−/− mice did have normal resting glucose levels (t-test, P > 0.1) they showed intolerance to a bolus of glucose, and they responded with abnormally high blood glucose concentrations that were restored to normal values at a significant slower pace than in wild-type (WT, Two-Way ANOVA, P < 0.05, Figure 1A). As previously mentioned melatonin may modulate insulin secretion (4) and therefore, we decide to test whether the observed change in the glucose levels were due to a delayed insulin secretion or to an increased tolerance towards insulin by performing an insulin tolerance test. Indeed, MT1−/− mice exhibited an increase tolerance towards insulin (Two-Way ANOVA, P < 0.001, Figure 1B). Surprisingly, mice lacking MT2 receptors (MT2−/−) - the melatonin receptor recently implicated in the pathogenesis of T2D (3, 6–7) - did not show any significant changes in glucose metabolism or insulin tolerance with respect to WT (Two-Way ANOVA, P > 0.1 in both cases, Figure 1A, B). Injection of vehicle did not affect resting glucose levels in WT, MT1−/− and MT2−/− (One-Way ANOVA, P > 0.1 in all cases, Figure 1C). No significant differences in the body weights among the three groups at the time of injection were observed (One-way ANOVA, P > 0.1; Figure 1 D). A previous study has shown that loss of melatonin signaling via removal of MT1 receptor in the mouse resulted in a modest, but significant, increase in blood glucose levels (4); therefore we decided to investigate the levels of hemoglobin A1C - a reliable indicator of overall glucose level - in these mice. Our data show that although MT1−/− mice showed impaired glucose metabolism and increased insulin resistance they did not show any significant difference in the level hemoglobin A1C (WT = 4.65+/− 0.252; MT1−/− = 4.70 +/− 0.361 ; MT2−/− = 4.8 +/− 0.216;, One-way ANOVA P > 0.1).
Figure 1.
Glucose intolerance (A) and insulin tolerance in wild-type (WT) (black circles) and in MT1−/− (white circles) and MT2−/− (grey circles). (A) MT1−/− mice showed a significant alteration in the metabolism of glucose with respect to WT and MT2−/− mice (Two-Way ANOVA, P < 0.05). (B) MT1−/− mice showed a significant increase in insulin tolerance with respect to WT and MT2−/− mice (Two-Way ANOVA, P < 0.001). (C) MT1−/− mice have higher glucose levels 20 minutes after glucose injection and 20 and 40 minutes after insulin injection (* P < 0.05). (C) Injection of vehicle did not affect resting glucose levels in WT, MT1−/− and MT2−/− (One-Way ANOVA, P > 0.1). Each point represents the mean +/− SEM. (N= 4–8 mice for each genotype and time point). No differences were observed in body weight (mean+/− SEM, N=12–14 mice for each group) among the three genotypes (One-Way ANOVA, P > 0.1).
Discussion
The main finding of this study is that removal of melatonin receptor type 1 significantly impairs the ability of the mice to metabolize glucose and such inability is probably due to an increase insulin resistance (Figure 1). Although MT1−/− mice have an insulin resistance they did not show any significant difference in their weight or in the levels of hemoglobin A1C at least at this age (3–4 months) and under our experimental conditions (ad libitum feeding with normal diet). As we have previously mentioned several recent studies have reported that melatonin and melatonin receptors are involved in the modulation of glucose homeostasis but the mechanisms underlying this action are not well characterized (2–3).
Muhlbauer et al., (4) reported that insulin secretion from islets is increased in melatonin receptor knock-outs when they are stimulated by 1 µM (but not by 1 nM) of melatonin and they also showed that plasma glucose levels are elevated in MT1−/− with respect to WT. In addition, they also reported that plasma insulin levels, albeit slightly reduced, are not statistically different between MT1−/− and WT. Our data indicate that MT1−/− mice have are insulin resistant (Figure 1) and therefore they may partially explain the results obtained by Muhlbauer et al., (4). However, it is important to note that in Muhlbauer et al., (4) the mice- during the testing - had access to food and water ad libitum whereas in our study the mice did not have access to food during the previous 12 hrs. In conclusion, we believe that additional studies are required to fully understand the role played by these receptors in the regulation of blood glucose levels.
Previous investigations have shown that insulin-resistant is mostly due to the inability of insulin to induce glucose uptake in skeletal muscle (9) and additional investigations have reported that impaired insulin stimulation of skeletal muscle blood flow and associated signaling pathways can also induce insulin-resistant states (10–11). Interestingly a recent study has indicated that melatonin can improve insulin sensitivity since melatonin treatment can significantly improve insulin-induced vasodilation of the skeletal muscle and insulin-dependent phosphorylation of Akt, a key molecule in the insulin dependent signaling cascade (5). Our new data indicate that the action of melatonin is mediated via MT1 receptors and open the door for a detailed exploration on the mechanisms by which MT1 receptors signaling may affect glucose metabolism.
Finally, it is worth noting that a few recent studies have reported that MT2 receptors are implicated in the pathogenesis of T2D (6–7). Our data indicate that under our experimental conditions MT2 receptors removal did not produce any significant effect on glucose metabolism (Figure 1). At first glance this result may seem surprising, however it must be noted that the study by Lyssenko et al., (6) reported that an increased levels of MT2 receptors is risk factor for T2D, not the removal of the receptors. Therefore, we believe that our data expand and support the conclusions of this previous report by showing that removal of MT2 has no effect on glucose metabolism. In conclusion our findings suggest that the MT1 receptors may be implicated in the development of insulin resistance at least in the mouse.
Acknowledgments
Supported by a grant from the NIH to G.T. (NS43459)
References
- 1.Dubocovich ML, Markowska M. Functional MT1 and MT2 melatonin receptors in mammals. Endocrine. 2005;27:101–110. doi: 10.1385/ENDO:27:2:101. [DOI] [PubMed] [Google Scholar]
- 2.Peschke E. Melatonin, endocrine pancreas and diabetes. J. Pineal Res. 2007;44:26–40. doi: 10.1111/j.1600-079X.2007.00519.x. [DOI] [PubMed] [Google Scholar]
- 3.Mulder, et al. Melatonin receptors in pancreatic islets: good morning to a novel type 2 diabetes gene. Diabetologia. 2009;52:1240–1249. doi: 10.1007/s00125-009-1359-y. [DOI] [PubMed] [Google Scholar]
- 4.Muhlbauer, et al. Loss of melatonin signalling and its impact on circadian rhythms in mouse organs regulating blood glucose. Eur. J. Pharmacology. 2009;606:61–71. doi: 10.1016/j.ejphar.2009.01.029. [DOI] [PubMed] [Google Scholar]
- 5.Sartori, et al. Melatonin improves glucose homeostasis and endothelial vascular function in high-fat diet-fed insulin resistant mice. Endocrinology. 2009 doi: 10.1210/en.2009-0425. doi10.1210/en.2006-0425. [DOI] [PubMed] [Google Scholar]
- 6.Lyssenko, et al. Common variant in MTNR1B associated with increased risk of type 2 diabetes and impaired early insulin secretion. Nat Genet. 2009;41:82–88. doi: 10.1038/ng.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bouatia-Naji N, et al. A variant near MTNR1B is associated with increased fasting plasma glucose levels and type 2 diabetes risk. Nat Genet. 2009;41:89–94. doi: 10.1038/ng.277. [DOI] [PubMed] [Google Scholar]
- 8.Baba K, et al. Melatonin modulates visual function and cell viability in the mouse retina via the MT1 melatonin receptor. Proc Natl Acad Sci U S A. 2009;106:15043–15048. doi: 10.1073/pnas.0904400106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Duplain, et al. Insulin resistance, hyperlipidemia, and hypertension in mice lacking endothelial nitric oxide synthase. Circulation. 2001;104:342–345. doi: 10.1161/01.cir.104.3.342. [DOI] [PubMed] [Google Scholar]
- 10.Cook, et al. Partial gene deletion of endothelial nitric oxide synthase predisposes to exaggerated high-fat diet-induced insulin resistance and arterial hypertension. Diabetes. 2004;53:2067–2072. doi: 10.2337/diabetes.53.8.2067. [DOI] [PubMed] [Google Scholar]
- 11.Cabou, et al. Central insulin regulates heart rate and arterial blood flow: an endothelial nitric oxide synthase-depended mechanism altered during diabetes. Diabetes. 2007;56:2872–2877. doi: 10.2337/db07-0115. [DOI] [PubMed] [Google Scholar]