Abstract
The importance of plasma protein concentration, renal vascular resistance, and arterial pressure as mediators of the natriuretic response to volume expansion was investigated in anesthetized dogs.
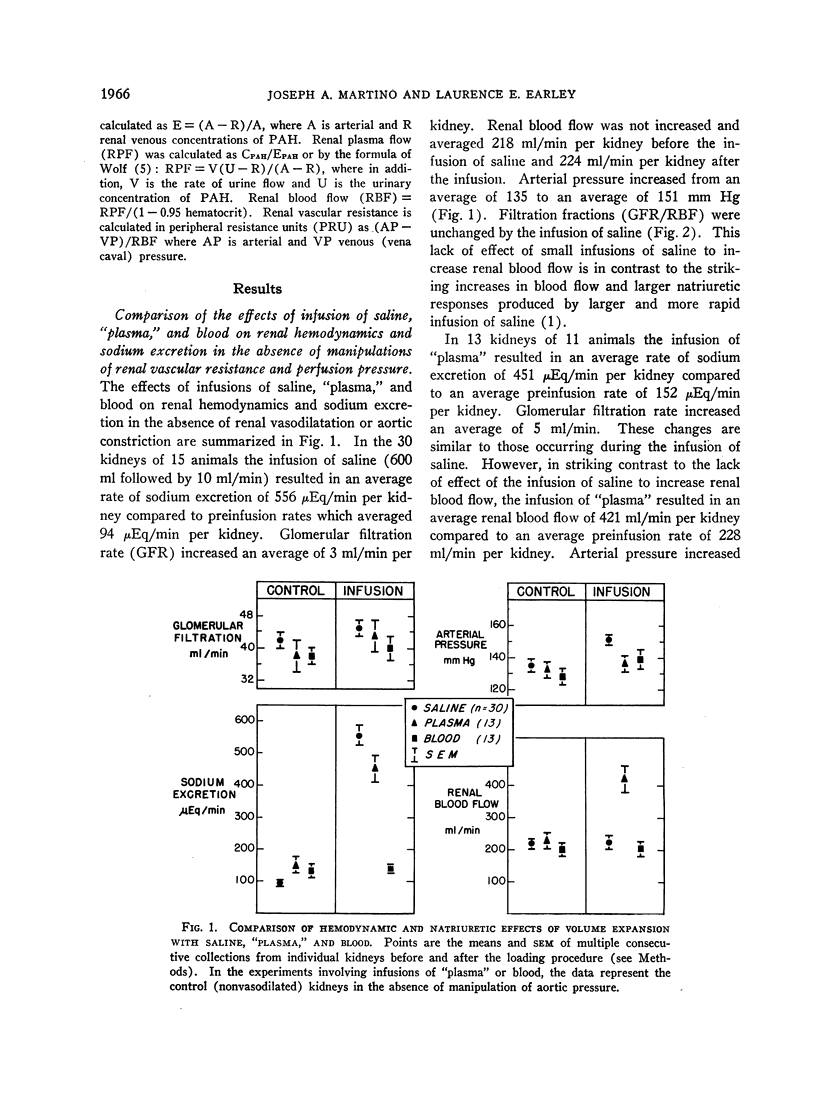
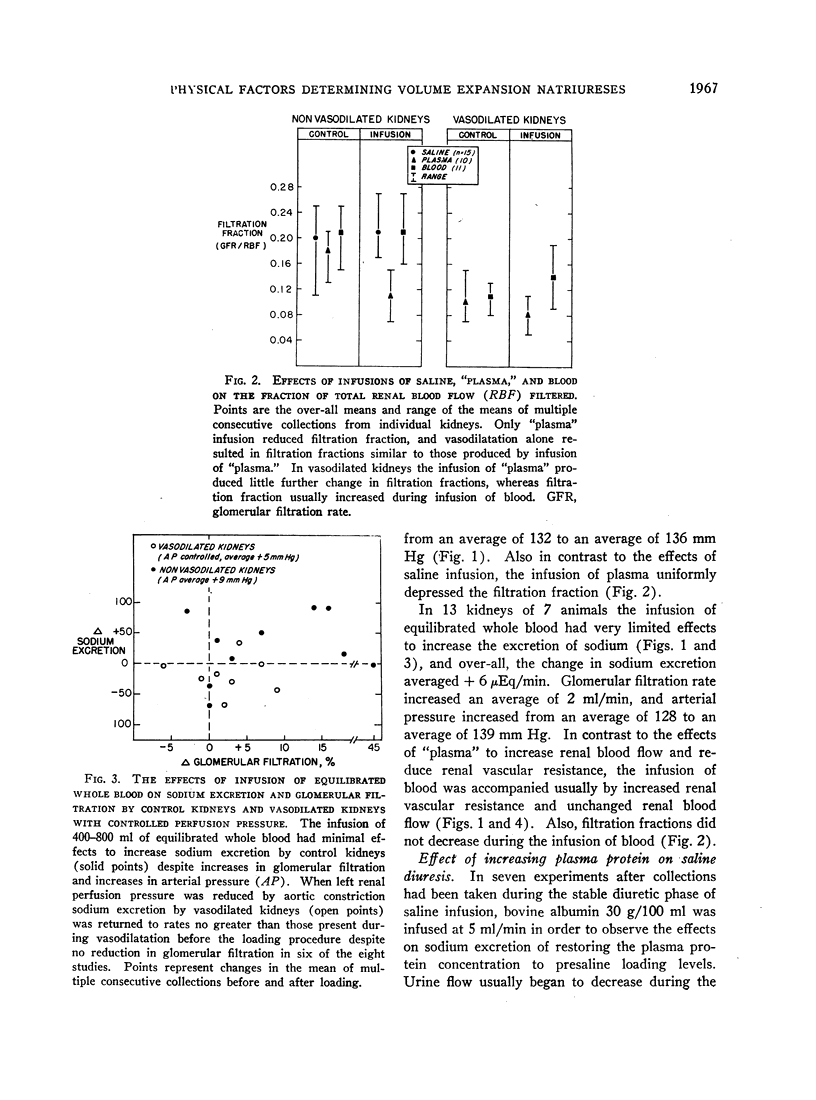
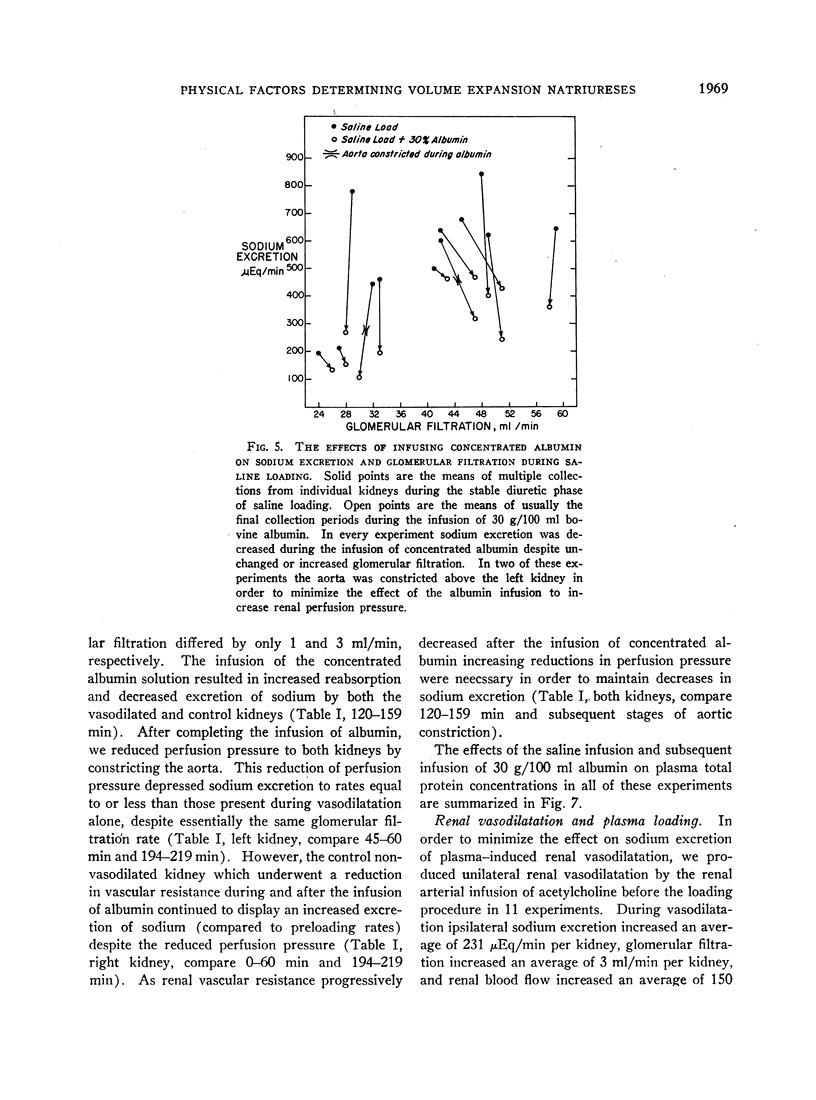
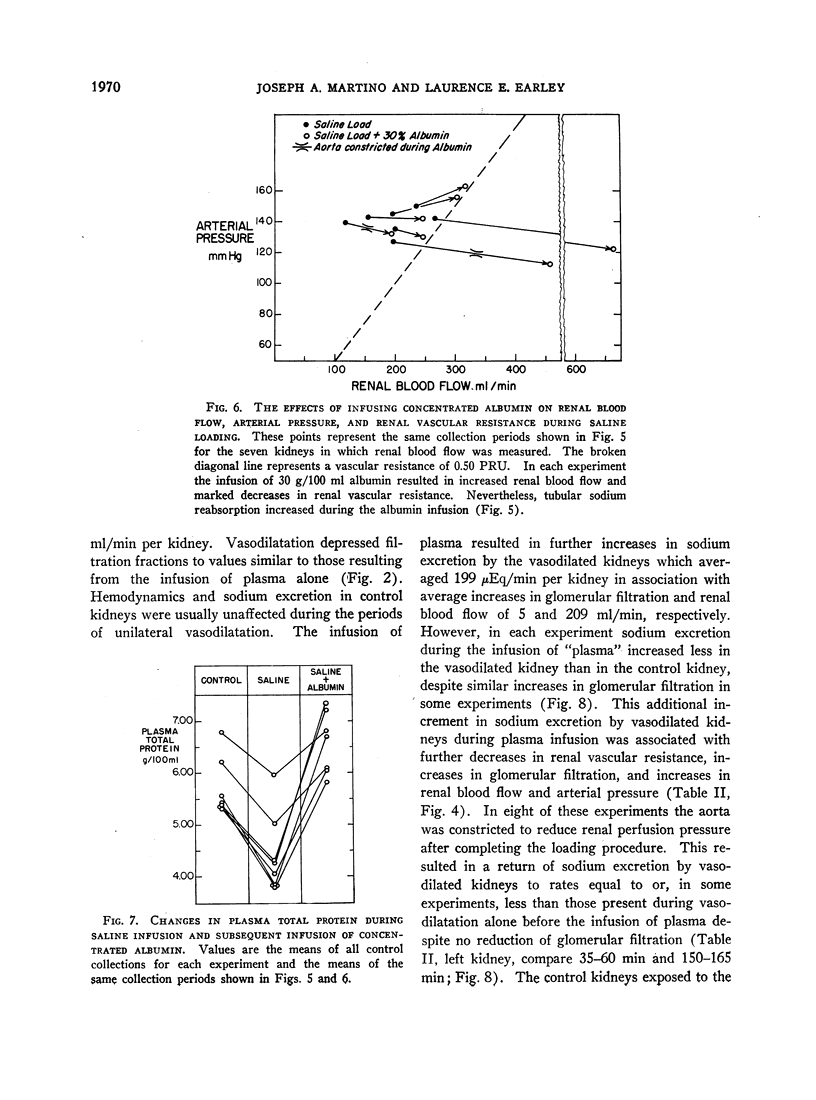
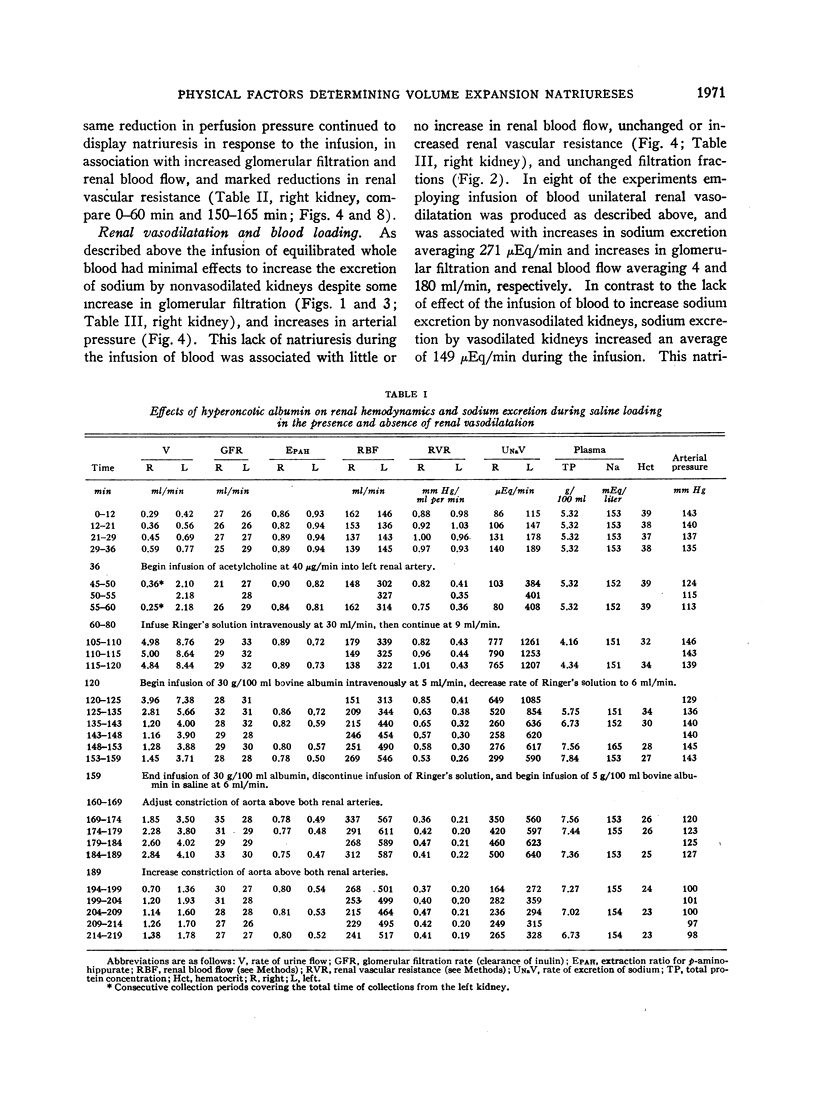
Saline loading depressed plasma protein concentration and increased arterial pressure but did not decrease renal vascular resistance. Restoring plasma protein concentration by infusing hyperoncotic albumin increased sodium reabsorption and decreased sodium excretion during saline loading despite simultaneous decreases in renal vascular resistance and increases in arterial pressure.
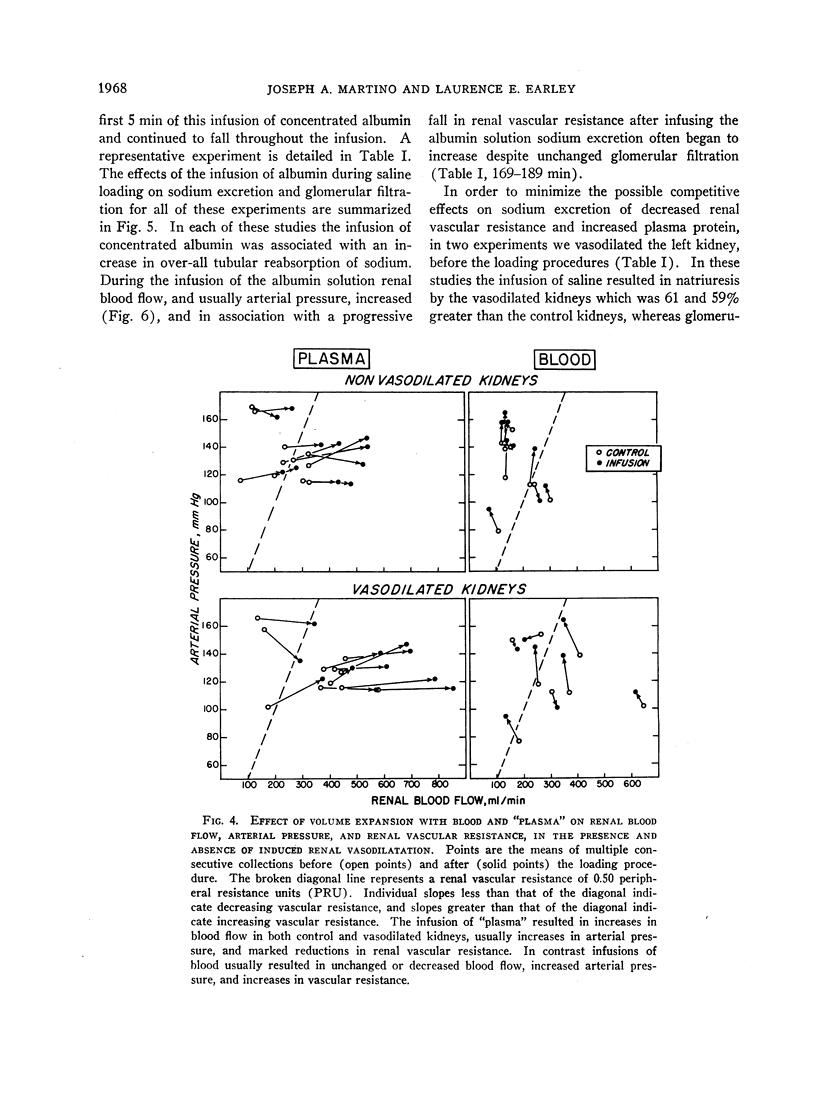
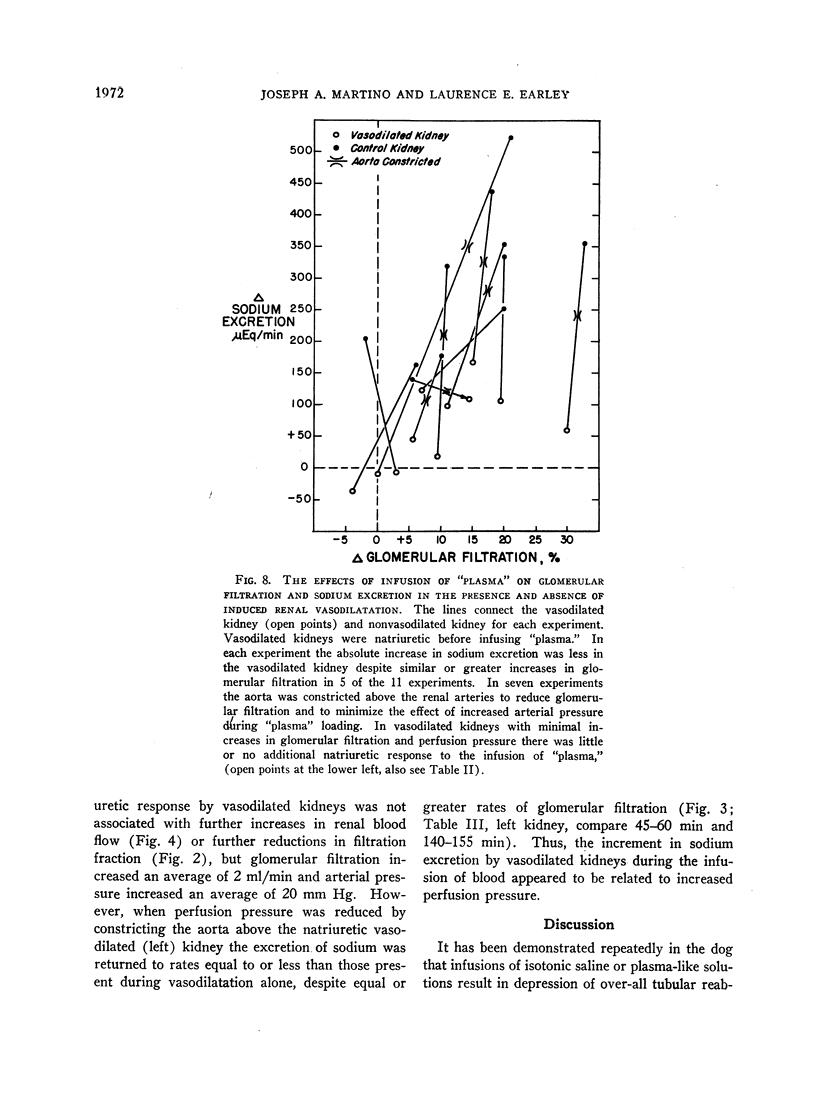
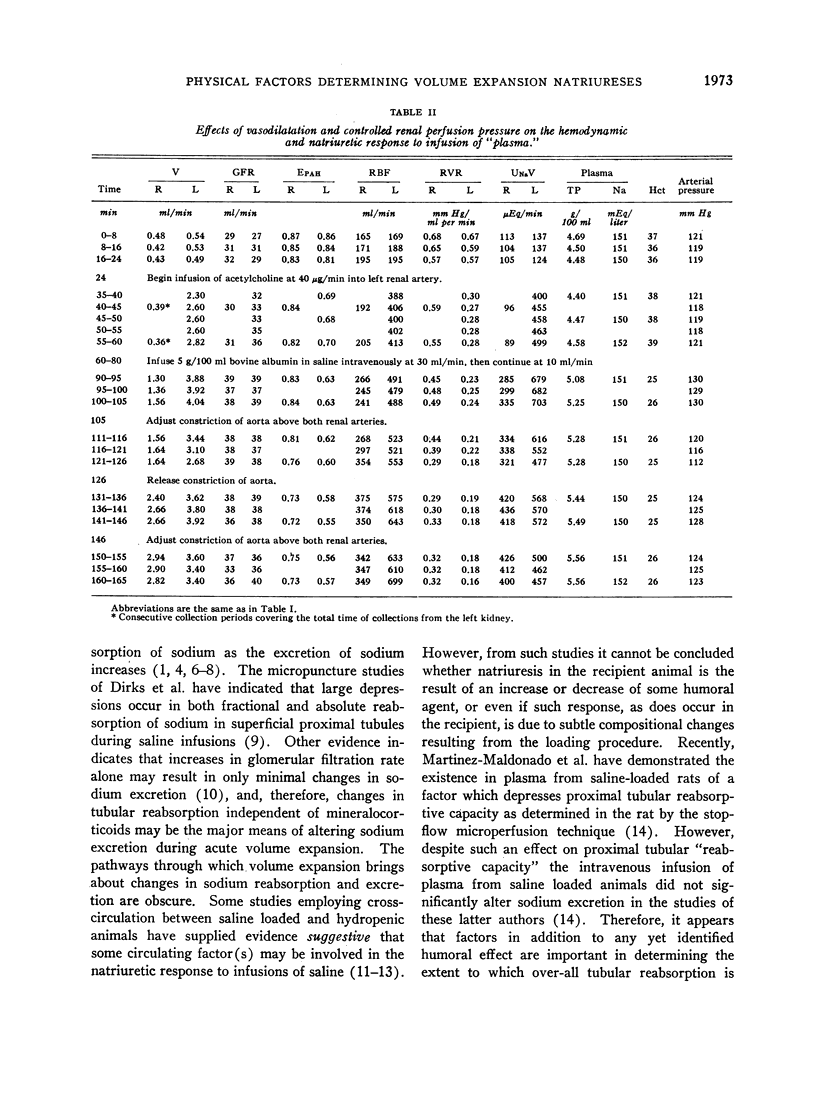
Infusion of “plasma” did not depress plasma protein concentration and produced natriuresis associated with increased arterial pressure and marked decreases in renal vascular resistance. Unilateral hemodynamic natriuresis was produced before “plasma” loading by the renal arterial infusion of acetylcholine, and the subsequent infusion of “plasma” resulted in much smaller increases in sodium excretion by the vasodilated kidney than by the control kidney. If perfusion pressure to both kidneys was then reduced by aortic constriction sodium excretion by the vasodilated kidney could be reduced to preloading (vasodilated) levels without reduced glomerular filtration, despite continued natriuresis in control kidneys which underwent vasodilatation in response to the infusion of plasma.
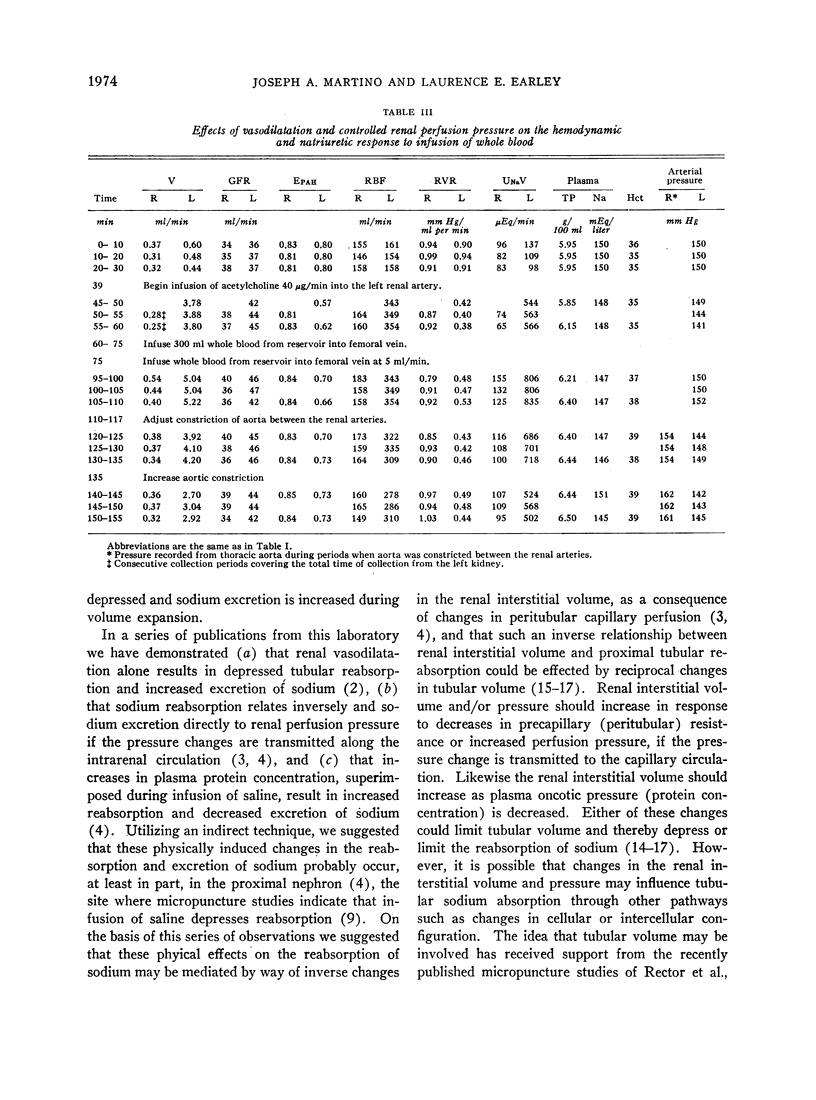
Infusion of equilibrated whole blood did not alter plasma protein concentration or the hematocrit, and renal vascular resistance did not decrease. Sodium excretion was increased minimally or not at all by the infusion of blood despite increased arterial pressure and glomerular filtration. However, in kidneys vasodilated before infusing blood sodium excretion increased in response to the infusion in association with increased arterial pressure. This increased excretion of sodium by vasodilated kidneys during infusion of blood could be abolished by reducing perfusion pressure to the preloading level.
These observations indicate that changes in plasma oncotic pressure, renal vascular resistance, and arterial pressure either alone or in combination are important variables determining the natriuretic response to volume expansion, and that the relative importance of each of these factors depends on the manner in which volume is expanded (viz., the infusion of saline, plasma, or blood).
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brunner F. P., Rector F. C., Jr, Seldin D. W. Mechanism of glomerulotubular balance. II. Regulation of proximal tubular reabsorption by tubular volume, as studied by stopped-flow microperfusion. J Clin Invest. 1966 Apr;45(4):603–611. doi: 10.1172/JCI105374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DE WARDENER H. E., MILLS I. H., CLAPHAM W. F., HAYTER C. J. Studies on the efferent mechanism of the sodium diuresis which follows the administration of intravenous saline in the dog. Clin Sci. 1961 Oct;21:249–258. [PubMed] [Google Scholar]
- DIRKS J. H., CIRKSENA W. J., BERLINER R. W. THE EFFECTS OF SALINE INFUSION ON SODIUM REABSORPTION BY THE PROXIMAL TUBULE OF THE DOG. J Clin Invest. 1965 Jul;44:1160–1170. doi: 10.1172/JCI105223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EARLEY L. E., FRIEDLER R. M. CHANGES IN RENAL BLOOD FLOW AND POSSIBLY THE INTRARENAL DISTRIBUTION OF BLOOD DURING THE NATRIURESIS ACCOMPANYING SALINE LOADING IN THE DOG. J Clin Invest. 1965 Jun;44:929–941. doi: 10.1172/JCI105210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earley L. E., Friedler R. M. Studies on the mechanism of natriuresis accompanying increased renal blood flow and its role in the renal response to extracellular volume expansion. J Clin Invest. 1965 Nov;44(11):1857–1865. doi: 10.1172/JCI105293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earley L. E., Friedler R. M. The effects of combined renal vasodilatation and pressor agents on renal hemodynamics and the tubular reabsorption of sodium. J Clin Invest. 1966 Apr;45(4):542–551. doi: 10.1172/JCI105368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earley L. E., Martino J. A., Friedler R. M. Factors affecting sodium reabsorption by the proximal tubule as determined during blockade of distal sodium reabsorption. J Clin Invest. 1966 Nov;45(11):1668–1684. doi: 10.1172/JCI105474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston C. I., Davis J. O. Evidence from cross circulation studies for a humoral mechanism in the natriuresis of saline loading. Proc Soc Exp Biol Med. 1966 Apr;121(4):1058–1063. doi: 10.3181/00379727-121-30965. [DOI] [PubMed] [Google Scholar]
- Johnston C. I., Davis J. O., Howards S. S., Wright F. S. Cross-circulation experiments on the mechanism of the natriuresis during saline loading in the dog. Circ Res. 1967 Jan;20(1):1–10. doi: 10.1161/01.res.20.1.1. [DOI] [PubMed] [Google Scholar]
- LEVINSKY N. G., LALONE R. C. THE MECHANISM OF SODIUM DURESIS AFTER SALINE INFUSION IN THE DOG. J Clin Invest. 1963 Aug;42:1261–1276. doi: 10.1172/JCI104811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinsky N. G. Nonaldosterone influences on renal sodium transport. Ann N Y Acad Sci. 1966 Nov 22;139(2):295–303. doi: 10.1111/j.1749-6632.1966.tb41204.x. [DOI] [PubMed] [Google Scholar]
- Lichardus B., Pearce J. W. Evidence for a humoral natriuretic factor released by blood volume expansion. Nature. 1966 Jan 22;209(5021):407–409. doi: 10.1038/209407a0. [DOI] [PubMed] [Google Scholar]
- MILLS I. H., DE WARDENER H. E., HAYTER C. J., CLAPHAM W. F. Studies on the afferent mechanism of the sodium chloride diuresis which follows intravenous saline in the dog. Clin Sci. 1961 Oct;21:259–264. [PubMed] [Google Scholar]
- Rector F. C., Jr, Brunner F. P., Seldin D. W. Mechanism of glomerulotubular balance. I. Effect of aortic constriction and elevated ureteropelvic pressure on glomerular filtration rate, fractional reabsorption, transit time, and tubular size in the proximal tubule of the rat. J Clin Invest. 1966 Apr;45(4):590–602. doi: 10.1172/JCI105373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rector F. C., Jr, Sellman J. C., Martinez-Maldonado M., Seldin D. W. The mechanism of suppression of proximal tubular reabsorption by saline infusions. J Clin Invest. 1967 Jan;46(1):47–56. doi: 10.1172/JCI105510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuster A., Alexander E. A., Lalone R. C., Levinsky N. G. Renal blood flow, sodium excretion, and concentrating ability during saline infusion. Am J Physiol. 1966 Nov;211(5):1181–1186. doi: 10.1152/ajplegacy.1966.211.5.1181. [DOI] [PubMed] [Google Scholar]



