Abstract
Objective. The aim of this study was to determine whether pregnancy increases the recurrence risk of cutaneous malignant melanoma (CMM) in women with a history of stage I CMM. Methods. The electronic medical databases of Medline and Embase were explored. All 1084 obtained articles were screened on title and abstract using predetermined inclusion and exclusion criteria. A critical appraisal of relevance and validity was conducted on the remaining full text available articles. Results. Two studies were selected. Both studies revealed no significant difference in disease-free survival between women with stage I CMM and the control population. Conclusion. Pregnancy does not increase the recurrence risk of CMM in women with a history of stage I CMM.
1. Clinical Scenario
A 33-year-old nulliparous woman was seen by the dermatologist because of a mole on her leg, which had been growing and itching over the past year. After excision of the lesion and pathological examination, the diagnosis made was a cutaneous malignant melanoma, with Clark level IV, a Breslow thickness of 1.25 cm-and tumor-free margins. Because excision had been successful, only a sentinel lymph node dissection was conducted which yielded no metastatic spread. The conclusive diagnosis therefore was a stage I cutaneous malignant melanoma. Every three months now, the patient is seen by the dermatologist in order to keep a close watch on the development of recurrence. Currently, she and her partner would like to embark on a first pregnancy.
2. Introduction
The incidence of Cutaneous Malignant Melanoma (CMM) has shown a rapid increase over the past decades, therefore substantiating a growing problem. About 27% of the noninvasive CMM diagnosed in the Netherlands in 2003 were seen in women between 30 and 44 years of age, of which 13% eventually died because of the disease. The currently known factors determining outcome are mostly the skin location of the melanoma, the Breslow thickness, and the Clark level [1, 2]. Keeping in view the possibility of tumor sensitivity to hormones, although the possible mechanism of this influence is still unknown, the question arises whether pregnancy influences the recurrence of CMM [2]. In the past, some studies have suggested a negative influence [3, 4], whereas other studies showed no effect of pregnancy on the prognosis of cutaneous malignant melanoma [5, 6]. Therefore, the aim of this article is to answer the following clinical question:
does [pregnancy] increase the [recurrence) risk (of cutaneous malignant melanoma] in [women with a history of stage I cutaneous malignant melanoma]?
Pregnancy was defined as occurring within five years of CMM diagnosis in previously nulliparous women. Stage I cutaneous melanoma was defined as a malignant melanoma localized to the site of origin on the skin, with no evidence of regional or distant spread [7]. Recurrence was defined as a subsequent manifestation of CMM within ten years of initial diagnosis and treatment. In addition, the disease-free survival is a period of time in which no CMM recurrence is seen.
3. Methods
3.1. Search and Selection
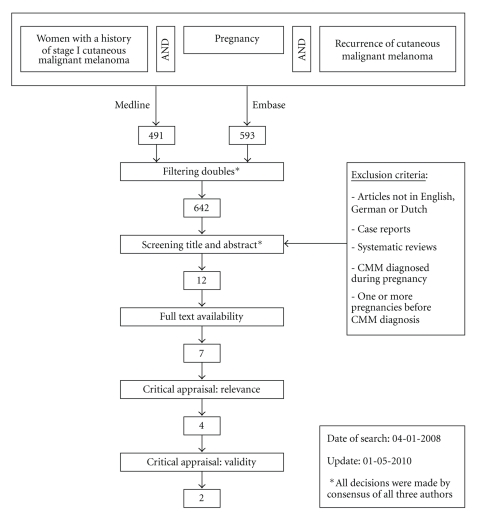
Synonyms for domain, determinant and outcome were identified using Thesaurus, Embase EMTREE-tool, Medline MesH-terms, and Index [Title/Abstract] and were applied in the electronic databases of Embase and Medline. This full cover search resulted in 491 articles in Medline and 593 articles in Embase (Table 1). The title and abstract of a total of 1084 articles were subsequently screened for their relevance concerning the clinical question, based on the following inclusion criteria: pregnancy within five years of CMM diagnosis in previously nulliparous women, the primary diagnosis being stage I cutaneous malignant melanoma, and CMM recurrence within ten years of the primary diagnosis. The exclusion criteria are shown in the flow chart (Figure 1). All decisions were made through a consensus of all three authors. Upon screening, 12 articles remained for further analysis. A total of seven articles appeared to be full text available.
Table 1.
Search strategy.
| Database | Searcha | Hits |
|---|---|---|
| Medline | ((Woman OR Women OR Female OR Females OR Patient OR Patients) AND (Skin OR Cutaneous OR Malignant OR Melanoma OR Melanomas)) AND (Pregnancy OR Pregnancies OR Pregnant OR Gravidity OR Gravidities OR Gestation) AND (Recurrent OR Recurrence OR Recurrences OR Recurring OR Recidive OR Recidives OR Recidivism OR Recidivisms OR Recidivating OR Recidivation OR Relapsing OR Relapse OR Relapses) | 491 |
|
| ||
| Embase | Idem Medline | 593 |
aThe original search was performed on 04-01-2008 according to the strategy above.
An update performed on 01-05-2010 following the same search strategy yielded no additional relevant articles.
Figure 1.
Flow chart.
3.2. Critical Appraisal
The selected articles were screened for relevance of domain, determinant, and outcome. As a result, four articles remained for validity screening. These articles were evaluated on the basis of the components shown in Table 2. Because Shaw [5] and Bork et al. [6] failed to report any effect or precision measures and did not compare patients with controls, these studies were excluded from further assessment. In contrast, Reintgen et al. [9] and MacKie et al. [10] did meet the criteria for a valid study with a level of evidence (Offringa et al. [8]) of 2B and were therefore considered valuable for answering the clinical question.
Table 2.
Critical appraisal.
| Study | Study design | Relevance | Blinding | Missing Data | Internal validity | Results | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Domain | Determinant | Outcome | Determinant | Outcome | Follow-up (months) | Drop-out (%) | Loss-to-follow-up (%) | Selectionbias | Informationbias | External Validity | Standardisation | Level of Evidence [8] | Effect measures | Precision measures | ||
| Bork et al. [6] | Retrospective | Women in the childbearing years with stage I malignant melanoma. | Pregnancy after primary therapy. | Recurrence & Disease-free survival. | n.a. | n.a. | n.a. | ? | ? | n.a. | n.a. | − | − | 3 | None | None |
|
| ||||||||||||||||
| Reintgen et al. [9] | Retrospective case/control | Women in the childbearing years treated for stage I primary cutaneous melanoma. | Pregnancy within 5 years of diagnosis. | Disease-free interval (10 years). | n.a. | n.a. | n.a. | None | None | n.a. | n.a. | + | ± | 2B | χ 2 | P |
|
| ||||||||||||||||
| Shaw et al. [5] | Retrospective | Women with malignant melanoma. | Pregnancy after diagnosis. | Local recurrence. | n.a. | n.a. | n.a. | ? | ? | n.a. | n.a. | − | ? | 3 | None | None |
|
| ||||||||||||||||
| MacKie et al. [10] | Retrospective cohort | Women in the reproductive years treated for stage I primary melanoma. | First pregnancy after diagnosis. | Disease-free survival (20 years). | n.a. | n.a. | n.a. | None | None | n.a. | n.a. | + | ± | 2B | RR | p&CI |
+: Good, ±: Moderate, −: Poor, ?: Unknown, n.a.: Not Applicable, RR: Relative risk, CI: Confidence Interval, P: P-value.
4. Results
Reintgen et al. [9] set up a retrospective case control study, whose objective was to assess whether pregnancy within five years of diagnosis would influence the ten-year disease-free interval in women with stage I cutaneous malignant melanoma. Patients were matched with a control population consisting of female stage I CMM patients between the age of 15 and 44 years, who were not pregnant either at diagnosis or within five-years of diagnosis. The study showed that the ten-yeardisease-free interval of the patient group did not significantly differ from that of the control group (Table 3).
Table 3.
Influence of pregnancy on recurrence of cutaneous malignant melanoma in women.
| Study | Population (n) | Effect | Precision | ||
|---|---|---|---|---|---|
| χ 2(*) | RR | P-value | 95% CI | ||
| Reintgen et al. [9] | 43 patients | 0.04 univariate | — | .80 univariate | — |
| 585 controls | 0.0 multivariate | — | 1.00 multivariate | — | |
|
| |||||
| MacKie et al. [10] | 85 patients | — | 1.21 (**) | .66 | 0.52–2.79 |
| 143 controls | — | 0.71 (**) | .54 | 0.23–2.15 | |
(*) With χ 2, the chi-square test is pronounced, which was used to test the significance of differences between the patient and the control groups. A concomitant P-value > .05 means that a correlation between pregnancy and CMM recurrence is not likely, and that if there is a correlation at all, this is not very strong, as suggested by the small χ 2 -values of 0.04 and 0.0 in the univariate and multivariate analyses, respectively.
(**) Compared to women diagnosed with a CMM in between pregnancies.
MacKie et al. [10] also established a retrospective case control study, in which the effect of pregnancy on the twenty year-disease-free survival after diagnosis of stage I cutaneous malignant melanoma was investigated. Patients were matched with a control population of women who had completed all pregnancies before a stage I CMM was diagnosed. The study yielded a relative risk of 1.21, which would suggest a slight effect of pregnancy on CMM recurrence. After regression analysis however, this did not prove to be significant (Table 3).
5. Conclusion
According to both Reintgen et al. [9] and MacKie et al. [10], pregnancy does not increase the recurrence risk of cutaneous malignant melanoma in women with a history of stage I cutaneous malignant melanoma.
6. Discussion
This evidence-based case report suggests that there is no negative influence of pregnancy on the recurrence of cutaneous malignant melanoma in women. There are however a number of drawbacks with respect to the critically appraised studies. Firstly, both Reintgen et al. [9] and MacKie et al. [10] used only a small number of patients compared to the relatively large control groups that were included. Secondly, in the study of MacKie et al. [10] the results of the patient group were not compared with the results of the control group, but both groups were compared with women diagnosed with a CMM in between pregnancies. Reintgen et al. [9] on the other hand used a more realistic control group composed of nulliparous women with a CMM diagnosis. Worth mentioning is the use of a regression analysis in both the study of Reintgen et al. [9] and that of MacKie et al. [10], which is a reliable statistical analysis method to determine the effect of possible confounders.
7. Recommendation
The best available evidence does not show any effect of pregnancy on the recurrence risk of cutaneous malignant melanoma in women. Nevertheless, a careful recommendation should be given, with Breslow thickness, Clark level, and skin localization taken into account. Because recurrence, independent of pregnancy, is most likely to develop within two to three years after CMM diagnosis and treatment [11, 12], and since both diagnostic and therapeutical interventions are possibly harmful to the unborn child, appropriate timing is necessary. Women should therefore consider delaying pregnancy for at least two to three years, taking into account the concomitant risk of maternal age related problems such as infertility and fetal developmental abnormalities.
Acknowledgment
MA and VIW contributed equally to this paper.
References
- 1.Netherlands Cancer Registry. Incidence of Cancer in the Netherlands
- 2.Driscoll MS, Grant-Kels JM. Hormones, nevi, and melanoma: an approach to the patient. Journal of the American Academy of Dermatology. 2007;57(6):919–931. doi: 10.1016/j.jaad.2007.08.045. [DOI] [PubMed] [Google Scholar]
- 3.Pack GT, Scharnagel IM. The Prognosis for Malignant Melanoma in the Pregnant Woman. Cancer. 1951;4:324–334. doi: 10.1002/1097-0142(195103)4:2<324::aid-cncr2820040218>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 4.Byrd BF, Jr., McGanity WJ. The effect of pregnancy on the clinical course of malignant melanoma. Southern medical journal. 1954;47(3):196–200. doi: 10.1097/00007611-195403000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Shaw JHF. Malignant melanoma in Auckland, New Zealand. Surgery Gynecology and Obstetrics. 1988;166(5):425–430. [PubMed] [Google Scholar]
- 6.Bork K, Brauninger W, Czarnetzki BM. Schwangerschaft nach Malignem Melanom: Verlaufsbeobachtung bei 23 Patientinnen. Deutsche Medizinische Wochenschrift. 1985;110(35):1323–1327. doi: 10.1055/s-2008-1069003. [DOI] [PubMed] [Google Scholar]
- 7.Retsas S, Mastrangelo MJ. Reflecting on the 2001 American Joint Committee on Cancer Staging System for melanoma. Seminars in Oncology. 2007;34(6):491–497. doi: 10.1053/j.seminoncol.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 8.Offringa M, Assendelft WJJ, Scholten RJPM. Inleiding in evidence-based medicine: klinisch handelen gebaseerd op bewijsmateriaal. 2nd edition. Houten, The Netherlands: Bohn Stafleu van Loghum; 2003. [Google Scholar]
- 9.Reintgen DS, McCarthy KS, Jr., Vollmer R. Malignant melanoma and pregnancy. Cancer. 1985;55(6):1340–1344. doi: 10.1002/1097-0142(19850315)55:6<1340::aid-cncr2820550630>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 10.MacKie RM, Bufalino R, Morabito A, Sutherland C, Cascinelli N. Lack of effect of pregnancy on outcome of melanoma. Lancet. 1991;337(8742):653–655. doi: 10.1016/0140-6736(91)92462-b. [DOI] [PubMed] [Google Scholar]
- 11.Poo-Hwu W-J, Ariyan S, Lamb L, et al. Follow-up recommendations for patients with American Joint Committee on cancer stages I-III malignant melanoma. Cancer. 1999;86(11):2252–2258. [PubMed] [Google Scholar]
- 12.Fincher TR, McCarty TM, Fisher TL, et al. Patterns of recurrence after sentinel lymph node biopsy for cutaneous melanoma. American Journal of Surgery. 2003;186(6):675–681. doi: 10.1016/j.amjsurg.2003.08.010. [DOI] [PubMed] [Google Scholar]