Abstract
Current progress in nanomedicine has exploited the possibility of designing tumor-targeted nanocarriers being able to deliver radionuclide payloads in a site or molecular selective manner to improve the efficacy and safety of cancer imaging and therapy. Radionuclides of auger electron-, α-, β-, and γ-radiation emitters have been surface-bioconjugated or after-loaded in nanoparticles to improve the efficacy and reduce the toxicity of cancer imaging and therapy in preclinical and clinical studies. This article provides a brief overview of current status of applications, advantages, problems, up-to-date research and development, and future prospects of nanotargeted radionuclides in cancer nuclear imaging and radiotherapy. Passive and active nanotargeting delivery of radionuclides with illustrating examples for tumor imaging and therapy are reviewed and summarized. Research on combing different modes of selective delivery of radionuclides through nanocarriers targeted delivery for tumor imaging and therapy offers the new possibility of large increases in cancer diagnostic efficacy and therapeutic index. However, further efforts and challenges in preclinical and clinical efficacy and toxicity studies are required to translate those advanced technologies to the clinical applications for cancer patients.
1. Introduction
Cancer an up-regulated biological process of cell growth with an ability of tumor cells to invade and metastasize. A century ago, Paul Ehrlich hypothesized that a “magic bullet” could be developed to selectively target cancer [1]. Over the past few decades, the progress in molecular biology and the understanding of malignant transformation and tumorigenesis have revealed two major classes of antitumor therapeutics: (i) application of molecularly targeted therapeutics to block major hallmarks of cancer cells, and (ii) employing drug delivery systems through tumor-targeted nanomedicines to improve the pharmacokinetics and bioavailability of vehicle-carried drugs. Targeted cancer therapies can be defined as drugs developed against a specific tumor target according to its important biology function in cancer. From 1980 to 2005, a total of 205 monoclonal antibodies (mAb) were studied in clinical trials [2–5]. The US Food and Drug Administration (FDA) approved the first anti-CD20 mAb (Rituximab) for the treatment of non-Hodgkin's lymphoma in 1997. Today, twelve of these anticancer molecular-targeted mAbs have been approved worldwide, eight of them were approved by US FDA [3–5].
Conventional anticancer drugs exhibit a lack of specificity, poor solubility and distribution, unfavorable pharmacokinetics, and high-tissue damage or toxicity. Nanotechnology can bring fundamental changes to the study and understanding of biological processes in health and disease, as well as enable novel diagnostics and therapeutics for treating cancer. Thus, advances made on the basis of nanotechnology could result in progress of healthcare. Targeted drug delivery systems such as passive and active targeting nanoparticles or nanocarriers, with diameters ranging from 10–100 nm, have been developed to improve the biodistribution, pharmacological, therapeutic and toxicity properties of agents used in cancer diagnostics and therapeutics [6–12]. The status of the development of targeting delivery systems, including targeting strategies, potential applications, and the prospects of tumor-targeted nanocarriers have been reviewed and discussed [6–11]. Nanotechnology is attracting increasing attention in the biomedical community, owing to unique prospects for targeted delivery in imaging, therapy, and drug delivery. Cancer nanotechnology is expected to transform current treatment systems by providing more efficient cancer diagnostics and therapeutics. Today, nanocarriers are used in detecting cancer at an early stage, delivering anticancer drugs specifically to malignant cells, and determining if these drugs are killing malignant cells [9–13]. Two therapeutic nanocarrier-liposomes and albumin nanoparticles have been approved by US FDA for clinical practices [8, 12, 13]. Pegylated liposomal doxorubicin represents a new class of chemotherapy delivery system that may significantly improve the therapeutic index of doxorubicin through improving therapeutic pharmacokinetics [6]. As nanocarriers are evaluated for safety and efficacy, nanotechnology will bring with it significant advances in molecular imaging and specific targeting of tumor therapeutic agents, elevating therapeutic efficacy, and finally achieving the goal of early detection and control of cancer. Customized nanoscale constructs can serve as targeted drug delivery vehicles capable of delivering large doses of radionuclide or chemotherapeutic agents into malignant cells while sparing normal tissues, greatly reducing the side-effects that usually accompany many current cancer therapies [8–13].
Monoclonal antibody-guided radiation therapy, or radioimmunotherapy, demonstrated promise in preclinical and clinical anticancer applications [14–19]. The principles and applications of molecular targeting involving radionuclide methods for tumor nuclear imaging and therapy were reviewed and discussed [19]. Two radiolabeled anti-CD20 monoclonal antibodies 90Y-ibritumomab (Zevalin) and 131I-tositumomab (Bexxar) were approved by US FDA in 2002 and 2003, respectively, for treatment of B-cell non-Hodgkin's lymphoma (NHL), which indicates the potential benefit of antibody-guided systemic radionuclide-targeted therapy [16–18]. However, tumor targeting studies with radiolabeled mAbs also showed some limitations, such as, inefficient targeting and low accumulation in tumor sites (<0.1 % of injection dose per gram (%ID/g) of tumor for human) and irradiation of normal tissues for long circulation of mAbs. Emerging new methods for improving the specific uptake of radionuclides in tumor cells while sparing the normal tissues need to be established. Several advanced strategies for radionuclide-targeted delivery have been studied extensively, including the combination of chemotherapy agents with particle-emitting radionuclides and the development of novel multimodality and multifunctional nanotargeted therapeutics [20, 21]. Optimization of treatment protocols has significantly improved the therapeutic efficacy and reduced toxicity in normal tissues. Nanoparticles delivering radionuclides for improving pharmacokinetics and therapeutic efficacy of cancer have been presented elsewhere [20–22]. The goal of this article is to review and summarize the recent research progress and future prospects of advanced nanoparticles or nanocarriers to deliver radionuclides for cancer in vivo nuclear imaging and therapeutic applications.
2. Nanoparticles and Radionuclides for Tumor Nuclear Imaging and Internal Radiotherapy
2.1. Nanoparticles for Tumor Nuclear Imaging and Radiotherapy
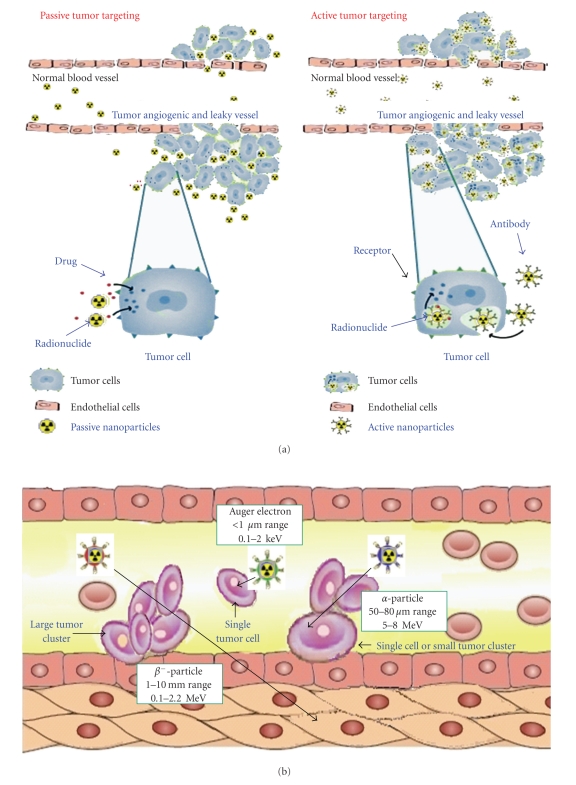
Major challenges of drug delivery carriers in cancer diagnostics and therapeutics are the low drug bioavailability within cancer cells and the high toxicities to normal organs [22, 23]. Targeted radionuclide therapy is often limited by insufficient delivery of radionuclides to tumor sites using the currently available targeting strategies, such as monoclonal antibodies and peptides, due to relatively low and heterogeneous expression of receptors on tumor cells, as well as dose-limiting toxicities to normal tissues. To maximize the therapeutic index and to minimize the toxicity, it is very important to deliver the radionuclides to the right site at the right concentration and at the right time. The rapidly advancing field of cancer nanotechnology has generated several innovative radionuclides and drug delivery systems, such as liposomes [23–31], iron oxide [32–34], polymers [35], dendrimers [36], quantum dots [37–39], and carbon nanotubes [40], to improve and enhance targeted transport of cytotoxic drugs or radionuclides to tumor lesions [20–23, 41, 42]. It is estimated that approximately 240 nano-enabled products entered pharmaceutical research pipelines in 2006 [43]. These nanocarrier systems could provide the delivery platforms needed for improving the delivery of radionuclides to tumor sites. Nanoparticles or nanocarrier delivery systems have also revealed enhanced imaging and therapeutic efficacy by targeted delivery of drugs to the tumor site and by reducing their toxic side-effects [7–13]. Major advantages of nanocarriers are that they can be prepared in sizes <100 nm, and increase selectively the localization of drugs and radionuclides in the tumor through their nanosize or enhanced permeability and retention (EPR) effect of passive targeting to the leaky tumor tissues [20, 21], or nanoparticle surface bio-conjugation, while sparing nontargeted tissue, ensuring minimal drug or radionuclide leakage during circulation, and facilitating intracellular drug or radionuclide delivery and uptake by active targeting [22, 23, 41, 42, 44]. Two major mechanisms for radionuclide- or drug-targeted accumulation delivery system of nanoparticles to tumor tissue sites are (i) site-specific passive tumor targeting and (ii) molecular affinity and site-specific active tumor targeting for tumor diagnostics and therapy as shown in Figure 1(a) [7].
Figure 1.
(a) Schematic illustration showing the possible mechanism for radionuclides or drug accumulation delivery system of nanoparticles by site specific passive tumor targeting using the enhanced permeability and retention (EPR) effect or molecular affinity and site specific active tumor targeting through ligand tumor cell surface receptors interaction, internalization, and intracellular action for tumor diagnostics and therapy (reproduced with modification with permission from [7]). (b) Schematic diagram of tumor tissue penetration range of internal radiotherapy by auger electron (0.1–2 keV, <1 μm )-, α (5–8 MeV, 50–80 μm range)-, and β (0.1–2.2 MeV, 1–10 mm range )- radiation emitters for passively and actively nanotargeted radionuclide therapy (reproduced with modification with permission from [14]).
There are three generations of nanocarriers or nanoparticles developed: (i) the first generation of nanocarriers (passive targeting) which are rapidly trapped in the reticuloendothelial system (RES) organs (e.g., liver and/or spleen) [25–27, 29, 31], (ii) the second generation of sterically stabilized PEGylated nanocarriers (passive targeting), which can evade the RES of the liver and spleen, enjoys a prolonged circulation in the blood and allows for passive targeting through the enhanced permeability and retention (EPR) effect in leaky tumor tissues [25–27, 29, 31], and (iii) the third generation of nanocarriers with a bioconjugated surface modification of the nanoparticles using specific antibodies or peptides to actively target specific tumor or tissues through molecular interaction or affinity (active targeting) [22, 32–42, 44–52]. The pharmacokinetics and bioavailability of drugs and radionuclides delivered by the third-generation nanocarriers have been much improved. There are three major challenges of applying nanoparticles to delivery of drugs or radionuclides: (i) synthesizing nanocarriers with stealth characteristics which are able to decrease uptake of delivered diagnostic and therapeutic agents in the reticuloendothelial system (RES) and prolong blood circulation, (ii) producing multifunctional nanoparticles with improved in vivo targeting capabilities, and interaction with disease biomarkers at the molecular level, (iii) developing reliable approaches to test these new materials in vitro and in vivo for a fast translation from the bench to the bedside [21, 42].
There are five approaches generally used for labeling or encapsulating radionuclides on nanoparticles: (i) labeling nanocarriers by encapsulation during preparation, (ii) nanocarriers surface labeling after preparation, (iii) nanocarrier surface labeling of bioconjugates after preparation, (iv) incorporation into the lipid bilayer after preparation, and (v) after-loading of the aqueous phase of the nanocarriers after preparation. The after-loading method has provided higher labeling efficiencies (>90%) and the greatest in vivo stability for 99mTc, 111In, and 67Ga radionuclides for nuclear imaging [20, 21, 24, 30, 31, 42, 53].
2.2. Radionuclides for Tumor Nuclear Imaging and Radiotherapeutics
The research on tumor-targeted diagnostic and therapeutic radionuclides is one of the potential areas of cancer drug development. Normally, targeted radionuclides consist of two components, a targeting carrier and a trace amount of radionuclide with a specific radiation emitter. The tumor therapeutic efficacy and diagnostic quality are determined by the selectivity or specificity of the targeted delivery systems and the radionuclide radiation characteristics [14, 15, 20, 21]. The selection of potential targeted radionuclides for tumor imaging (Table 1) and targeted radionuclide for internal radiotherapy (Table 2) involves the physical half-life, decay mode, and the emission properties of the radionuclides. Gamma emitters with energy range between 130 and 370 keV can be used for gamma imaging or single photon emission tomography (SPECT) [24–30]. The high-energy positron emitters with annihilation energy at 511 keV energy can be applied for positron-emission tomography (PET) [20, 21, 31]. The major characteristics of nanotargeted nuclear imaging modalities are listed in Table 3. In functional and molecular imaging, the in vivo radionuclide SPECT and PET imaging is the most sensitive with sub-nanomolar amounts of molecular probes and the highest tissue penetration range (Table 3).
Table 1.
| Radionuclide | Production | Emission type | Half-life | Emax(γ), (keV) |
|---|---|---|---|---|
| 131I | 130I(n, γ)131Te (β) 131I | γ (81.2%), β | 8.0 days | 284, 364, 637 |
| 67Ga | 68Zn (n, p)67Ga | γ | 78.3 h | 93, 184, 300, 393 |
| 111In | 111Cd (p, n)111In | Auger, γ | 67.2 h | 171, 245 |
| 123I | 121Sn (α, 2n)123I | Auger, γ | 13.2 h | 159 |
| 99mTc | 99Mo/99mTc-generator | γ | 6.0 h | 140 |
| 18F | 18O (p, n)18F | Positron | 1.83 h | Eβ+ 635 |
| 64Cu | 64Ni(p, n)64Cu | Positron | 12.7 h | Eβ+ 656 |
| 76Br | 76Se(p, n)76Br | Positron | 16.0 h | Eβ+ 3941 |
| 124I | 124Te(p, n)124I | Positron | 100.2 h | Eβ+ 2134, 1533 |
Table 2.
| Radionuclide | Production | Emission type | Half-life | Emax (MeV) | Rmax (mean)1 | Size of tumor cells2 |
|---|---|---|---|---|---|---|
| 186Re | 185Re (n, γ) 186Re | β, γ (9.4%) | 89.2 h | 1.07 | 5 mm (1.8 mm) | Intermediate clusters |
| 188Re | 188W/188Re-generator | β, γ (15.1%) | 17 h | 2.12 | 11 mm (2.4 mm) | L clusters |
| 177Lu | 176Lu (n, γ)177Lu | β | 161 h | 0.49 | 1.6 mm (0.67 mm) | S clusters |
| 131I | 131Te (β)131I | γ (81.2%), β | 8 d | 0.28, 0.36, 0.64 | 2.4 mm (0.8 mm) | S clusters |
| 90Y | 90Sr/90Y-generator | β | 64.1 h | 2.28 | 12 mm (2.8 mm) | L clusters |
| 67Cu | 64Ni(α, p)67Cu | β | 2.6 d | 0.19 | 2.2 mm (0.7 mm) | S clusters |
| 225Ac | 225Ra-generaor | α | 10 d | 5.83, 5.79, 5.79, 5.73 | 40–80 μm | Single cells, S clusters |
| 111In | 111Cd (p, n)111In | Auger,γ | 67 h | 0.42 | 2–500 nm | Single cells |
L: large; S: small.
1Radiation tumor tissue penetration maximum and mean range.
2Small, intermediate and large clusters correspond approximately to the intervals 104–106,106–108, and 108–1010 tumor cells per clusters, respectively [54].
Table 3.
| Modality | Image probe (Amount of probe) | Type of radiation | Sensitivity | Spatial Resolution | Depth | Nanoparticle design |
|---|---|---|---|---|---|---|
| SPECT | 99mTc, 111In etc | γ-ray | 10−10-10−11 (pM) | 0.5–1 mm | No limit | Surface |
| Bio-conjugation | ||||||
| or after loading | ||||||
| loaded or labeled | ||||||
| nanocarriers (ng) | ||||||
| PET | 18F, 64Cu etc | Positron | 10−11-10−12 (pM) | 1-2 mm | No limit | Surface |
| Bio-conjugation | ||||||
| or after loading | ||||||
| loaded or labeled | High energy | |||||
| nanocarriers (ng) | γ-ray |
SPECT: single photon emission computed tomography; PET: positron emission tomography.
For targeted radionuclide internal radiotherapy applications, high- and low-energy between 0.1–2.2 MeV of β-emitters are ideal radioisotopes for the treatment of small to large clusters of tumor cells [14]. The maximum tissue penetration range (1–10 mm) [14, 54] and cross-fire effects of β-particles with energy range between 0.1–2.2 MeV can kill tumor cells in close proximity to neovasculature [14, 21, 54]. Alpha-emitters hold great promise as therapeutics for small cancer lesions and micrometastatic cancers due to the high-linear energy transfer (LET, 80 keV/μm) and short-range energy depositions with tissue penetration range of 50–100 μm. Monoclonal antibody labeled with α-emitters has been demonstrated to have high specific killing effects and minimal normal-tissue damage in a tumor-bearing animal model [14, 54]. Auger electrons have an energy of <30 keV and subcellular pathlength of 2–12 μm. Thus, auger electron emitters can exert their radiotoxic effects on cells when they are internalized into the cytoplasm [55–57].
123I-ITdu-mediated nanoirradiation of DNA induces efficiently death in HL60 leukemia cells and in doxorubicin, β- or γ-radiation-resistant cell lines has been examined. The experimental findings provide evidence that ultra-selective nanoirradiation of DNA through auger electron-carrying metabolic substrates offers an extremely effective strategy for inducing cell death and breaking resistance to more conventional types of irradiation or chemotherapy [58]. The schematic illustration of tumor tissue penetration range of radiation emitters for passively and actively nanotargeted radionuclide therapy is shown in Figure 1(b) [14].
3. Passive Nanotargeting Delivery of Radionuclides for Tumor Nuclear Imaging and Radiotherapy
Typically, nanotargeted radionuclides have a two-component architecture for passive targeting imaging and radiotherapeutics for example, a pegylated nanoliposome loaded with radionuclide payloads for nuclear imaging or radiotherapeutics [20, 21, 31, 59]. The research and applications of selected passively nanotargeted nuclear imaging agents and radiotherapeutics are summarized in Table 4. The history and progress of the preclinical development of liposome-targeted treatments for cancer before 2000 were described in detail [60]. Optimal radiolabeled liposomes for tumor imaging have been established [61]. The clinical development of passively targeted liposomes as vehicles for targeted therapy of cancer have been summarized [62]. In addition, the potential areas for future development of liposome-targeted strategies have also been considered [62].
Table 4.
Selected passively nanotargeted tumor nuclear imaging and radiotherapeutic applications.
| Nanoparticles | Radionuclides | Imaging or Radiotherapeutics | Applications | Reference |
|---|---|---|---|---|
| Liposomes | 99mTc, 111In, 67Ga, 99mTc | Gamma imaging | Multitude diagnostics of tumor, infection, Inflammation, and lymphoscintigraphy | [28, 29, 60–62] |
| Liposomes | 111In | Gamma/SPECT imaging | Clinical biodistribution, PK and imaging studies of breast, head and neck, glioma and lung cancer patients | [53, 62] |
| Liposomes | 18F | PET imaging | Liposomal tracking in vivo with 18F-limposome-PET imaging | [66–68] |
| Liposomes | 111In, 177Lu | Gamma/SPECT imaging | Gamma imaging of tumor targeting for C26 and HT29/luc animal models | [70, 71] |
| Liposomes | 64Cu | PET imaging | Passive targeted delivery and imaging with bioconjugated 64Cu-BAT- PEG-liposome | [69] |
| Liposomes | 131I, 90Y, 188Re, 67Cu | Radiotherapeutics | An analytical dosimetry study for the use of radionuclide-liposome conjugates in internal radiotherapy | [74] |
| Liposomes | 186Re | Radiotherapeutics | Intraoperative 186Re-liposome radionuclide therapy in a head and neck squanous cell carcinoma xenograft positive surgical margin model | [78] |
| Liposomes | 111In, 188Re | Radiotherapeutics | Imaging, biodistribution, pharmacokinetics, and therapeutic efficacy studies of 111In/188Re-liposome on C26 and HT-29 tumor-bearing animal models | [70, 72, 80, 81] |
| Liposomess | 225Ac | Radiotherapeutics | Targeted α-particles emitters of 225Ac-generators encapsulated in liposomes as therapeutic agents for micrometastases cancer | [82–84] |
| Liposomes | 10B | Radiotherapeutics | 10B-liposomes nanotargeted therapeutics for boron neutron capture therapy (BNCT) | [85, 86] |
| Liposomes | 111In, 188Re | Radiochemo-therapeutics | Imaging, biodistribution, pharmacokinetics, therapeutic efficacy, and dosimetry studies of 111In/188Re-VNB/DXR-liposome on C26 and HT-29 tumor/ascites-bearing animal models | [71, 73, 81, 90–93] |
mAb: monoclonal antibody, CNT: carbon nanotube, QD: quantum dots, IO: iron oxide.
Drug and radionuclides encapsulated within the liposome can occur in one of the three potential compartments: water-soluble agents are located in the central aqueous core of the liposome; lipid-soluble agents are carried in the liposome membrane; peptides and small proteins tend to bind to the interface between the lipid bilayer surface and the adjacent aqueous phase [60].
3.1. Passive Nanotargeting Delivery of Radionuclides for Tumor Nuclear Imaging
The major characteristics of nanotargeted nuclear imaging modalities such as gamma imaging, SPECT and PET are listed in Table 3. Liposomes are self-assembling colloidal particles composed of a spherical bilayer of small phospholipid vesicles which is spontaneously formed when water is added to a dried lipid mixture [60]. Significant progress has been made in the use of liposome as a nanoparticle or nanocarrier for the delivery of radionuclides for imaging. Selected research and applications of passively nanotargeted cancer nuclear imaging agents and radiotherapeutics are summarized in Table 4.
Delivery of 99mTc, 111In, and 67Ga radionuclides by liposomes for gamma-imaging and monitoring drug treatment have been reviewed and reported for preclinical and clinical studies [28, 29, 60–63]. A systemic study of optimal liposome formulation and encapsulation of radionuclides was also reported [60, 61]. The biodistribution, pharmacokinetics, and nuclear imaging of 111In-DTPA-labeled pegylated liposome were studied in patients with advanced local cancer [53]. Effective targeting of solid tumors of breast (5.3 ± 2.6 %ID/kg for a tumor volume of 234.7 ± 101.4 cm3), head and neck (highest uptake of 33.0 ± 15.8 %ID/kg for a tumor volume of 36.2 ± 18.0 cm3), lung (18.3 ± 5.7 %ID/kg for a tumor volume of 114.5 ± 42.0 cm3), brain, and cervix was also observed with gamma camera and SPECT imaging [53]. Conventional 111In-based liposome (Vescan) preclinical and clinical performance and evaluation of lessons learned from the formulation and process development has been discussed and summarized [64]. In recent years, clinical studies using radiolabeled liposomes for tumor diagnostic imaging of cancer and inflammation from 1979 to 2001 have been reported [65]. A novel amphiphilic probes for 18F-radiolabeling performed liposomes and determination of liposomal trafficking by PET was developed [66]. Liposomes encapsulating positron emitter 18F and 64Cu were applicable for diagnostic imaging and real-time liposomal tracking in vivo [66–69].
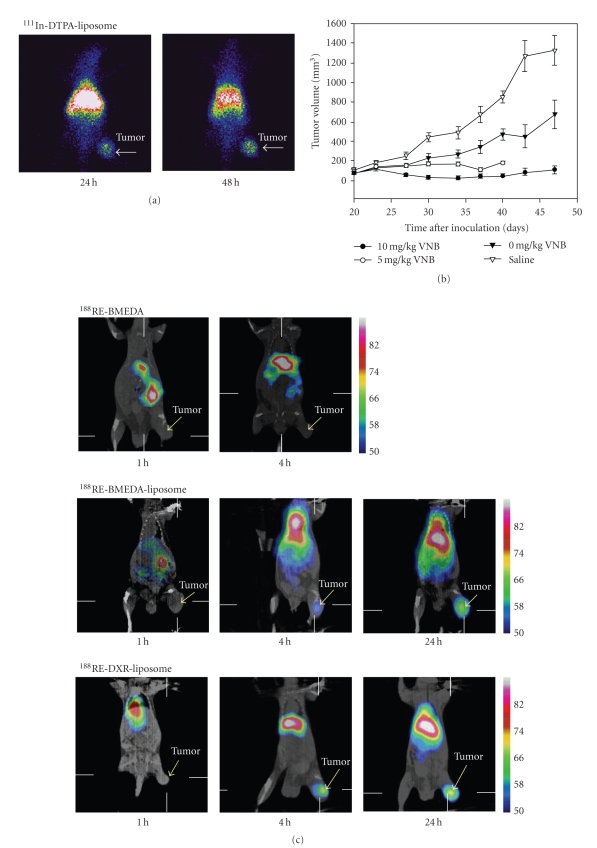
Wang et al. demonstrated an intravenous administration of 111In-liposome by conjugating 111In-oxine to DTPA/PEG-liposome followed by whole-body scintigraphy. Images revealed that the tumor clearly accumulated 111In-liposome up to 48 h postinjection (p.i.) [70]. In addition to the diagnostic imaging of 111In-liposome, Lee et al. demonstrated the bifunctional imaging and bimodality therapeutic efficacy of radiochemo-therapeutics of 111In-VNB-liposomes in HT-29/luc mouse xenografts [71]. Table 4 lists some of the selected passively nanotargeted liposomes delivery of radionuclides for nuclear imaging. The gamma scintigraphy and SPECT/CT image passively nanotargeted radionuclides of 111In-liposome (Figure 2(a)) [70], 188Re-liposome, and 188Re-DXR-liposome (Figure 2(c)) [70, 72] targeting on CT-26 tumor bearing in BALB/c mice animal model through the EPR localization effect were illustrated.
Figure 2.
(a) Gamma scintigraphy of BALB/c mice bearing CT-26 tumor animal model at 24 hr and 48 hr after intravenous injection of passively nanotargeted radionuclides of 111In-DTPA-liposome (reprinted with permission from reference [70]). (b) Tumor growth inhibition with passively nanotargeted radionuclides of 111In-(VNB)-liposome on HT-29/luc tumor bearing in SCID mice animal model (reprinted with permission from reference [71]). (c) MicroSPECT/CT images of passively nanotargeted radionuclides of 188Re-liposome and 188Re-DXR-liposome targeting CT-26 bearing in BALB/c mice animal model at 1 h, 4 h, 24 h, and compare with the control (reprinted with permission from reference [72]). (d) Therapeutic efficacy of tumor volume change and survival ratio for CT-26 tumor-bearing BALB/c mice after intravenous administration of passively nanotargeted radionuclides of 188Re-(DXR)-liposome were illustrated. (reprinted with permission from reference [73]).
3.2. Passive Nanotargeting Delivery of Radionuclides for Tumor Radiotherapy
An analytical dosimetry study for the use of 131I, 90Y, 188Re, and 67Cu radionuclide-labeled liposome for internal radiotherapy has been reported, and the analysis suggested that the optimal liposome system for radiotherapy differs from chemotherapy delivery [74]. In previous clinical targeting tumor imaging studies [53], the results of the effective targeting of solid tumors in patients with advanced local cancers by radiolabeled pegylated liposomes support the possible delivery of β-emitting radionuclide-loaded pegylated liposome for the treatment of solid tumors, particularly those liposomes in head and neck patients.
Bao et al. have developed a method of labeling liposomes with radionuclides using N,N-bis(2-Mercaptoethyl)-N′N′-diethylethylenediamine (BMEDA) to after-load 99mTc or 186Re into liposomes [65, 75, 76]. In addition to therapy via intravenous administration, the intratumoral and intraoperational therapies were also investigated for the potential use of 186Re-liposomes [77–79]. High-resolution SPECT/CT images revealed the intratumoral distribution of therapeutic liposomes; this result indicated the potential use of 186Re-liposomes for intratumoral therapy [78, 79]. Intraoperative passive nanotargeted 186Re-liposome therapy showed an excellent tumor suppression and minimal side-effect profile in the head and neck squamous cell carcinoma xenograft positive surgical margin model [78]. Biodistribution, pharmacokinetics, and nuclear imaging of passively nanotargeted radio-therapeutics of 111In/188Re-liposome on C26 and HT-29 colon carcinoma-bearing animal models have been studied by our group [70, 72, 80]. 111In has a γ-ray with 171 keV energy for nuclear imaging and an auger electron with 0.42 MeV energy in the nm tissue penetration range with specific single tumor cell or small tumor cluster killing effect (Table 2 and Figure 1(b)). 188Re has a γ-ray with 155 keV energy for nuclear imaging and a high-energy beta emitter with 2.12 MeV energy for killing nonspecific large tumor clusters. Both radionuclides can be used in bifunctional nuclear imaging and internal radio-therapeutic applications. The long-circulating pegylated liposomes radiolabeled with 188Re (188Re-liposomes) showed a higher uptake in the tumor as compared with 188Re-BMEDA alone. Passively nanotargeted 188Re-liposomes were found to have a 7.1-fold higher tumor-to-muscle ratio as compared with intravenously administered unencapsulated 188Re-BMEDA in a C26 murine colon carcinoma solid tumor animal model [72]. Improvement of biodistribution and therapeutic index via increase of polyethylene glycol(PEG) from 0.9% to 6% on passively nanotargeted 111In-liposome in an HT-29/luc xenografted mouse model was observed [81]. Targeted α-particle emitters are promising therapeutics for micrometastatic tumors. Enhanced loading of 225Ac and retention of three α-particle-emitting daughters of 225Ac by passively targeted liposomes have been demonstrated [82–84].
Boron neutron capture therapy (BNCT) is a binary approach to cancer therapy involving the nuclear reaction that occurs when 10B is irradiated with thermal neutrons to yield high LET of α-particles and lithium nuclei (2.4 MeV). These particles have a short range (<10 μm) and deposit their energy within single cells. The efficacy and successful treatment of tumors by BNCT depend on the selective delivery of relatively high amounts of 10B to tumors. There are three important parameters for development of boron compounds: (i) achieving tumor concentration in the range of 20–35 μg 10B/g, (ii) reaching a tumor/normal tissue ratio greater than 3–5, and (iii) illustrating sufficiently low toxicity. Application of passive stealth liposome-entrapped 10B delivery systems has been studied for BNCT in animal models [85, 86]. The results of the study on 10B-PEG-liposome through intravenous injection suggested that passively targeted delivery of sodium mercaptoundecahydrododecaborate (10BSH) can increase the retention of 10B by tumor cells, causing the suppression of tumor growth in vivo for BNCT [86]. A high level of 10B concentration (22 ppm) was observed in tumor tissues at 24 h after the administration of boron liposomes, and the tumor was significantly suppressed [85].
3.3. Passive Nanotargeting Codelivery of Radionuclides and Chemotherapeutics for Tumor Radiochemotherapeutics
Concomitant chemotherapy and radiotherapy has been found to improve treatment outcome in a range of solid tumors. Pegylated liposome-encapsulated doxorubicin and cisplatin have shown to be the potential target drugs to tumors, showing increase in therapeutic efficacy and reduction in toxicity [87]. Trimodal cancer therapy combining antiangiogenesis, chemotherapy, and radiotherapy achieves beneficial effects when used as a clinical antitumor strategy [88]. Image-guided and passive nanocarrier-based polymeric nanomedicine for radiotherapy holds significant potential for improving the treatment of advanced solid tumors [89]. Biodistribution, pharmacokinetics, nuclear imaging, and therapeutic efficacies were investigated for nanotargeted bifunctional co-delivery radiochemotherapeutics of 111In/188Re-(vinorelbine/doxorubicin,VNB/DXR)-liposomes on colorectal carcinoma of HT-29 and C26 tumor and ascites-bearing animal models [71, 73, 90–93]. In addition to the diagnostic imaging of 111In/188Re-liposome, the additive therapeutic efficacy was observed for the comparative co-delivery radiochemo-therapeutics of specific-killing auger electron emitters of 111In-(VNB)-liposomes on HT-29/luc mouse xenografts [71, 92]. 188Re-DXR-liposomes could provide a beneficial and promising strategy for the co-delivery of passively nanotargeted bimodality radiochemotherapeutics in the treatment of solid tumor and ascites [73, 91]. The experimental results pointed to the potential benefit of the co-delivery of nanoliposome radiochemotherapeutics for adjuvant cancer treatment in oncology applications [73]. Evaluation of pharmacokinetics of 111In-VNB-liposome on C26/tk-luc after intraperitoneal (i.p.) and intravenous (i.v.) administration in a tumor/ascites mouse model was studied and compared, the results indicated that the i.p. was a better approach than i.v. injection in the treatment of i.p. malignant tumor/ascites model [93]. Previous theoretical dosimetry studies have addressed the potential use of therapeutic nanoliposomes for the treatment of tumors via intravenous injection [74, 94, 95]. The comparative dosimetric evaluation of nanotargeted 188Re-(DXR)-liposome derived from the biodistribution indicated that the delivery radiation doses were safe and feasible for further clinical translation research from bench to bedside [90]. The results for major organs doses for the 188Re-(DXR)-liposome revealed that similar doses were received by spleen and liver, but a lower dose was given to kidney, compared with 111In-DTPA-octreotide therapy. Lower doses were also received by total body and liver, compared with 111In-DTPA-human epidermal growth factor (hEGF) radiotherapeutics (0.19 and 0.76 mGy/MBq, respectively). The absorbed doses for spleen, liver, kidney, and red marrow in these studies are much lower than those from 90Y-1,4,7,10-tetraazacyclododecane-N, N′,N′′,N′′′-tetraacetic acid tyrosine octreotide (DOTATOC) therapy [90]. Table 4 lists the selected passively nanotargeted nuclear imaging and radiotherapeutic applications. The tumor growth inhibition and therapeutic efficacy studies of passively nanotargeted radionuclides of 111In-(VNB)-liposome on HT-29/luc tumor bearing in SCID mice animal model (Figure 2(b)) [71], and 188Re-(DXR)-liposome on CT-26 solid tumor on BALB/c mice animal model were illustrated (Figure 2(d)) [71, 90]. The synergistic therapeutic efficacy was also demonstrated in the co-delivery of nanotargeted radiochemo-therapeutics of 188Re-DXR-liposome [73].
4. Active Nanotargeting Delivery of Radionuclides for Tumor Nuclear Imaging and Radiotherapy
Typically, nanotargeted radionuclides have a three-component architecture for active targeting therapeutics, such as pegylated nanoliposome surface bioconjugated with bioactive antibody or peptide, and encapsulated or bioconjugated with therapeutic radionuclide payloads for tumor-targeted nuclear imaging or radiotherapeutics [20, 21]. In addition, tumor-specific receptor targeting of nanocarriers could provide for high-antitumor therapeutic activity and imaging efficacy with low adverse side effects on healthy organs for practically any type of anticancer/imaging drug delivery systems [22, 23, 41, 42]. The selected research and applications of actively nanotargeted tumor nuclear imaging and radiotherapeutics are summarized in Table 5.
Table 5.
Selected actively nanotargeted tumor nuclear imaging and radiotherapeutic applications.
| Nanoparticles | Radionuclides | Imaging or Radiotherapeutics | Applications | Reference |
|---|---|---|---|---|
| Immunoliposome | 111In | Gamma imaging and therapeutics | 111In-liposome-2C5(mAb) nucleosome-specific monoclonal 2C5 targeting delivery vehicles for tumor visualization of murine lewis lung carcinoma and human HT-29 tumors | [45–47] |
| Perfluorocarbon nanoparticles | 111In | Gamma imaging | Imaging of targeted tumor angiogenesis of αvβ3-integrin in Vx-2 rabbit tumors | [48] |
| Carbon nanotubes | 111In | Gamma or SPECT imaging | Multifunctional targeted delivery and imaging with. functionalized and bioconjugated 111In-DOTA-CNT-Rituximab nanoconstructs | [40] |
| Quantum dots | 64Cu | Bifunctional PET/NIRF imaging | Dual-functional targeted delivery with amine functionalized 64Cu-DOTA-QD-RGD for tumor angiogenesis PET/NIRF imaging | [37] |
| Quantum dots | 64Cu | Bifunctional PET/NIRF imaging | Dual-functional targeted delivery with amine functionalized 64Cu-DOTA-QD-VEGF for tumor angiogenesis PET/NIRF imaging | [38] |
| Quantum dots | 18F | Bifunctional PET/optical imaging | 18F labeled phospholipids quantum dot micelles for in vivo multimodal imaging | [39] |
| Iron oxide | 64Cu | Bifunctional PET/MRI imaging | PET/MRI dual-modality tumor angiogenesis imaging with 64Cu-DOTA-IO-RGD nanoconstructs | [32, 33] |
| Iron oxide | 18F | Trimodel MRI/PET-CT/optical imaging | 18F labeled iron oxide for in vivo PET-CT imaging | [34] |
| Polymer | 99mTc | Scintigraphic images of tumor targeting | Targeting tumor angiogenesis: comparison of 99mTc -peptide and 99mTc -polymer-peptide conjugates | [35] |
| Dendrimers | 76Br | RGD directed-demdrimers PET imaging | 76Br labeled RGD-directed-dendritic nanoprobes for PET imaging of angiogenesis | [36] |
| Streptavidin | 111In | Radiotherapeutics | 111In labeled 3-component streptavidin (111In-MORF/tat/trastuzmab) nanoparticles for auger electron induced antisense-mediated cytoxicity of tumor cells | [50] |
| Immunoliposomes | 90Y | Radiotherapeutics | Targeted antiangiogenesis of αvβ3-integrin or VEGFR2 anti-FLK-1 therapy with nanotargeted therapeutics of 90Y-DTPA-liposome-IA(integrin antagonist) or 90Y-DTPA-liposome-mAb | [49] |
| Immunoliposomes | 225Ac | Radiotherapeutics | Targeted α-particles emitters of 225Ac-generators encapsulated in liposomes as therapeutic agents for micrometastases cancer | [82–84] |
| Immunoiposomes and Folate-dendrimers | 10B | Radiotherapeutics | 10B-immunoliposomes-anti-EGFR and 10B-PAMAM dendrimers-anti-folate nanotargeted therapeutics for boron neutron capture therapy (BNCT) | [51, 52] |
4.1. Active Nanotargeting Delivery of Radionuclides for Tumor Nuclear Imaging
The ability to modify the surface of nanocarriers permits the improvement in the pharmacokinetics, bioavailability, toxicity, and customization of nanocarrier formulations for particular actively nanotargeted tumor imaging [96]. Enhanced tumor accumulation and visualization by γ-scintigraphy with 111In-labeled nucleosome-specific monoclonal antibody 2C5 bioconjugated immunoliposome has been studied, and the results indicated better and faster imaging in various tumor-bearing mice [45–47]. Pharmaceutical lipid-based nanocarriers modified with mAb 2C5 could represent a new system for tumor-specific delivery of soluble, insoluble, and radionuclide pharmaceuticals [45]. αvβ3-Integrin-targeted 111In perfluorocarbon nanoparticles have been developed and studied for the detection of rabbit Vx-2 tumor angiogenesis. The circulatory half-life was estimated to be 5 h. The mean tumor uptake was 4-fold higher than the nontargeted control. The specificity activity (mCi/ml) (111In/NP) of 111In to nanoparticle (NP) may affect the tumor-to-muscle ratio in patients. The tumor-to-muscle uptake ratios for the nanotargeted 111In/NP = 10 to 111In/NP = 1 were 6.3 ± 0.2 to 5.1 ± 0.1, respectively. The data suggest that αvβ3-targeted 111In perfluorocarbon nanoparticles may provide a clinically useful tool for detecting angiogenesis in nascent tumors [48]. 111In radiolabeled soluble functionalized multifunctional drug delivery platforms of active targeting with rituximab monoclonal antibody bioconjugated on single-wall carbon nanotubes have been developed, and the selectivity of targeting disseminated human lymphoma was evaluated in vitro and in vivo [40]. The results of the ability to target tumor specifically with prototype-radiolabeled or fluorescent-labeled, antibody-appended carbon nanotube constructs are encouraging and suggest further investigation of carbon nanotubes as a novel radionuclide delivery platform [40].
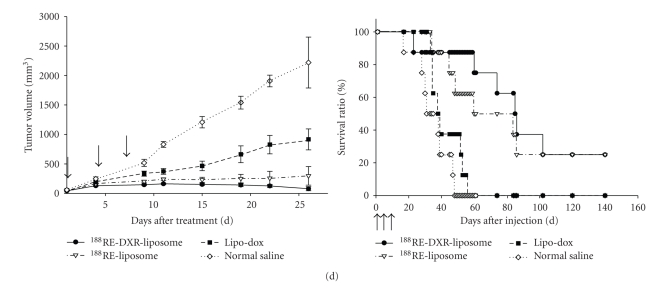
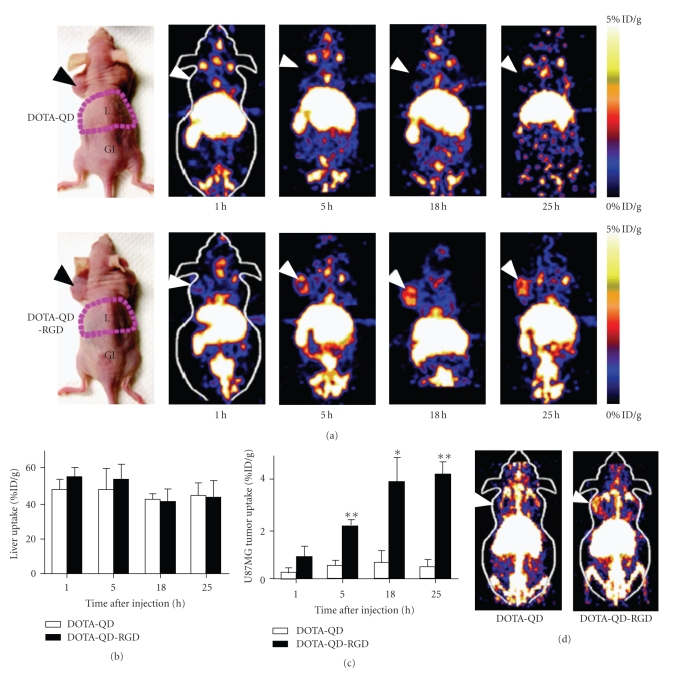
The development of a dual-function PET/near-infrared fluorescence (NIRF) molecular probe for the accurate assessment of pharmacokinetics and tumor-targeting efficacy of U87MG human glioblastoma tumor-bearing mice has been reported [37]. The amine-functionalized surface of quantum dot (QD) bioconjugated with arginine-glycine-aspartic acid (RGD) peptides and 1,4,7,10-tetraazacyclododecane-1,4,7,10-tetraacetic acid (DOTA) for 64Cu radiolabeled 64Cu-DOTA-QD-RGD nanoconstructs with 90 RGD per QD to target angiogenesis for application in integrin-αvβ3 PET/NIRF imaging was also illustrated [37]. This dual-function nuclear/optical in vivo molecular probe revealed a quantitative targeting ability in deep tumor lesions [37]. Dual modality optical and PET imaging of vascular endothelial growth factor receptor (VEGFR) on tumor vasculature using QDs of 64Cu radiolabeled 64Cu-DOTA-QD-VEGF was also investigated [38]. The U87MG tumor uptake of active nanotargeted 64Cu-DOTA-QD-VEGF (1.52 ± 0.6 % injected dose/gram (%ID/g), 2.81 ± 0.3 %ID/g, 3.84 ± 0.4 %ID/g, and 4.16 ± 0.5 %ID/g at 1, 4, 16, and 24 h, respectively, postinjection) was one percentage injected dose per gram (%ID/g) higher than that of passively targeted 64Cu-DOTA-QD [38]. 18F-labeled phospholipids quantum dot micelles for in vivo PET and optical fluorescence imaging from cells to whole body have been designed and studied [39]. Development of a bifunctional nanotargeted iron oxide (IO) molecular probe for PET and magnetic resonance imaging (MRI) of tumor integrin-αvβ3 expression was reported; this bifunctional 64Cu-DOTA-IO-RGD nanotargeted molecular imaging approach may allow for earlier tumor detection and may provide insight into the molecular mechanisms of cancer [32, 33]. The synthesis and in vivo characterization of an 18F-labeled trimodal (MRI/PET-CT/optical) iron oxide(IO) for tumor imaging, the facile conjugation chemistry, provides a simple platform for rapid and efficient IO labeling [34]. Tumor targeting angiogenesis and comparison of 99mTc-labeled peptide and 99mTc-labeled polymer-peptide nanocarrier conjugates were investigated [35]. Specific targeting of the αvβ3 integrin and nonspecific vascular permeability are both significant, but active specific targeting is more important than EPR of the carrier molecule. Nonspecific vascular permeability appears to be a major factor in reducing tumor-to-normal tissue localization ratio for the peptide molecules [35]. Biodegradable 76Br-labeled dendritic bioconjugated RGD bifunctional nanoprobes for the noninvasive PET imaging of angiogenesis was reported [36]. Figure 3 demonstrated the in vivo actively nanotargeted radionuclides of 64Cu-DOTA-QD-RGD for dual-function PET and near-infrared fluorescence (NIR) imaging of a U87MG tumor vasculature mice animal model [37].
Figure 3.
In vivo actively nanotargeted radionuclides of 64Cu-DOTA-QD-RGD for dual-function PET and near-infrared fluorescence (NIR) imaging of U87MG tumor vasculature mice animal model. (a) PET images of 64Cu-labeled nanoparticles of DOTA-QD or DOTA-QD-RGD. Arrow heads indicate tumors. (b) Liver uptake of 64Cu-labeled nanoparticles of DOTA-QD or DOTA-QD-RGD. (c) U87MG tumor uptake of 64Cu-labeled nanoparticles of DOTA-QD or DOTA-QD-RGD. (d) Two-dimensional image of the 2 mice shown in (a) at 5 hr after injection (reprinted with permission from reference [37]). DOTA: 1,4,7,10-tetraazacyclodocecane- N, N′,N′′,N′′′- tetraacetic acid chelators for radionuclides labeling. QD: Quantum dots conjugated with NIR probe. RGD: Arginine-glycine-aspartic acid peptide for targeting tumor angiogenesis integrin αvβ3.
4.2. Active Nanotargeting Delivery of Radionuclides for Tumor Radiotherapeutics
Significant radiation-induced antisense-mediated cytotoxicity of tumor cells in vitro was achieved using an auger electron-emitting antisense antiR1α messenger RNA antisense morpholino (MORF) oligomer administered as a member of a three-component streptavidin-delivery nanoparticle (111In-MORF/tat/trastuzumab) [50]. Targeted angiogenesis αvβ3 and VEGFR2 with three-component actively nanotargeted radionuclides of 90Y-liposome-IA (integrin antagonist) and 90Y-liposome-anti-Flk-1 (mAb) have been reported in murine melanoma K1735-M2 and colon CT26 animal models [49]. The results demonstrated that 90Y-liposome-anti-Flk-1 (mAb) was significantly more efficacious than conventional radioimmunotherapy in the mouse melanoma model [49].
Enhanced targeting, loading and retention of 225Ac, and three α-particle-emitting daughters of 225Ac by actively nanotargeted immunoliposomes have also been illustrated [82–84]. The efficacy and successful treatment of tumors by BNCT depend on the selective delivery of relatively high amounts of 10B to tumors. Application of active folate-receptor targeted PAMAM-dendrimers and active cetuximab immunoliposome-entrapped 10B delivery systems has been studied for BNCT applications in animal models [51, 52]. Major challenges that have to be addressed by drug-delivery nanocarriers in cancer therapy are the low drug bioavailability of therapeutics within cancer cells and the high toxicities at normal organs due to the low tumor targeting or localization. The combination of molecular targeting of bioconjugated nanoparticles or immunoliposomes can provide targeted cell internalization and intracellular drug release to improve anticancer therapeutic efficacy and to reduce toxicity [97]. Active receptor nanotargeted polymers, dendrimers, and liposomes employed for targeting to tumor-specific receptors can prevent serious adverse side effects on healthy organs. In addition, the internalization and intracellular distribution of nanocarriers in cancer cells indicated that tumor-specific receptor active targeting of nanocarriers could provide high antitumor therapeutic activity and imaging efficacy with low adverse side effects on normal tissues [41].
4.3. Nanoparticles for Concurrent Multimodality Nuclear Imaging and Radiotherapeutics
Nanoparticles have advantages for cancer nuclear imaging and radiotherapy. The ultimate goal in the design and preparation of multifunctional and multimodality nanoparticles in drug delivery is the creation of combined diagnostics and therapeutics (or theragnostics) and combined radiochemo-therapeutics for the targeted diagnosis and treatment of cancer [44, 97]. Recent advances in the field of nanotechnology and nanomedicine indeed offer the promise of better diagnostic and therapeutic options. Newer generation of nanoparticles has been designed and synthesized to target specific types of cell and molecule via affinity ligands from phage or small molecules, or involving antibodies or peptides for nanotargeted radionuclide or drug concurrent delivery.
Synergistically integrated nanoparticles with multifunctional and multimodality novel core platform for cancer nuclear imaging and radiotherapeutics have been developed [98]. Important multifunctions include imaging (single or multimodality), therapy (single drug or combination of two or more drugs), and targeting (one or more ligands) with multivalent. For example, binary nanoparticles with two functions could be developed for simultaneous molecular imaging and targeted therapy, ternary nanoparticles with three functions could be designed for simultaneous imaging, therapy and targeting, targeted dual-modality imaging, or targeted dual-modality therapy. Some typical and potential nanoparticles for nuclear imaging and therapeutics are illustrated as follows: (i) radionuclide (e.g., 111In/188Re/64Cu)-labeled passively nanotargeted multimodel nanoliposomes [90–92] or actively nanotargeted multifunctional and multimodal immunoliposomes [45–47, 99–101], (ii) radionuclide (e.g., 18F/64Cu)-labeled iron oxide magnetic nanoparticles for multimodal and multivalent MRI-PET-optical imaging agents and therapeutics [32–34] (iii) radionuclide (e.g., 18F/64Cu)-labeled QDs for multifunctional and multimodal imaging and therapeutics [37–39, 59, 102] and (iv) silica nanoparticles as a platform for multimodality imaging agents and therapeutics [103, 104]. The simultaneous attainment of preferential localization and avoidance of the sequential biological barriers, such as RES system uptake, has been studied with a multifunctional multistage delivery system of mesoporous silicon particles for imaging and therapeutic applications [105]. Development of multidrug resistance (MDR) is one of the most challenging aspects of cancer chemotherapy. Bimodality codelivery chemotherapeutics in nanoemulsion formulations has shown to be very effective in enhancing the cytotoxicity in wild-type and resistant tumor cells [106].
5. Nano-/Radiotoxicology
Although nanocarriers have provided some new breakthroughs for cancer diagnosis and therapy, the potential adverse human health effects resulting from exposure to nanoparticles should also be a concern [22, 107, 108]. Research shows that nanoparticles can stimulate and/or suppress the immune response, and that their compatibility with the immune system is largely determined by their surface chemistry. Modifying these factors can significantly reduce the immunotoxicity of nanoparticles and make them useful platforms for drug delivery [43]. The biodistribution and movements of nanoparticles through tissues and the phagocytosis and endocytosis of nanoparticles would all likely affect the potential toxicity of nanoparticles. The practical strategies for identifying and controlling interferences in common evaluation methods and the implications for regulation of nanoparticle immunotoxicity have been discussed and suggested [109]; the standardization of nanoparticle-tuned methods through international “round robin” inter-laboratory testing was proposed [109]. Toxicity of nanocarrier systems involves physiological, physicochemical, and molecular considerations. Nanocarrier systems may induce cytotoxicity and/or genotoxicity [110]. To minimize the risks posed by nanomaterials, there are two basic avenues. One is to develop new highly biocompatible nanomaterials with low toxicity. The other is surface modification of nanoparticles with biocompatible chemicals. Many great efforts are being made to develop nanoparticles satisfactory for clinical applications, but nanoregulation is still undergoing major changes to encompass environmental, health, and safety issues [43, 107, 108, 110]. QDs larger than the renal filtration threshold quickly accumulate in the RES system following intravenous administration. Great concern has been raised over the use of quantum dots in living cells and animals due to their chemical composition of toxic heavy-metal atoms (e.g., Cd, Hg, Pb, As) [59].
Radiolabeled pegylated liposomes have demonstrated effective targeting of solid tumors in patients by nuclear imaging [53]. There were no important adverse reactions attributable to the liposome infusion, and repeated hematological and biochemical profiles performed at day 10 showed no significant changes [53]. Absorbed dose calculations provide a scientific basis for evaluating the biological effects associated with administrated radiopharmaceuticals. In cancer therapy, radiation dosimetry supports treatment planning, dose-response analyses, predications of therapy effectiveness and safety [111]. An analytical dosimetry study for the use of radionuclide (67Cu, 131I, 188Re, and 90Y)-liposome in internal radiotherapy has been reported [74]. Unlike the case with radioimmunotherapy, the dose-limiting organ is likely to be the liver, and strategies intended to reduce RES accumulation are needed to further improve such a tumor-targeting approach [74]. We have studied the radiation dosimetric analysis of passively nanotargeted radiotherapeutics of 188Re-liposome and radiochemo-therapeutics of 188Re-DXR-liposome with OLINDA/EXM software for system-targeted radionuclide therapy. The results showed that the red marrow was to be the critical organ in determining the maximally tolerated absorbed doses, and it was promising and beneficial to carry out further preclinical and clinical investigations [90]. Comparisons with the radiation-absorbed dose estimates for 111In- and 90Y-ibritumomab tiuxetan, and the radiation absorbed per unit administered activity (mGy/MBq) for nanotargeted 188Re-(DXR)-liposome were much lower in the major organs [90, 111].
6. Conclusions and Future Prospective
Recent advances in the field of nanotechnology applications in biomedicine offer the promise of better diagnostic and therapeutic options. Medicine and synthetic scientists are making strides in developing nanoconstructs that can be used as core platforms for attaching different functionalities by surface conjugating or after-loading of various nanoparticles for the purposes of cancer molecular imaging and targeted drug delivery. As compared with conventional targeted radionuclide therapy or radioimmunotherapy, the use of nanocarriers can allow for specific multivalent attachment of targeted molecules of antibodies, peptides, or ligands to the surface of nanocarriers. Nanotargeted radionuclide therapy can deliver a high payload of radionuclides, chemotherapeutics, and/or imaging agents to achieve multifunctional and multimodality targeting to tumor cells. The new nanocarrier drug delivery system platform can enhance the efficacy and safety of targeted therapy. Future clinical trial studies are required to translate those advanced technologies to the health care of cancer patients. The optimization of the nanoparticle compositions and structure, the simultaneous attainment of preferential targeting location, reducing immunotoxic effect, and the avoidance of sequential biological barriers of the nanoparticles are the major challenges in the future research and development of passively and actively nanotargeted drug delivery systems.
Several passively nanotargeted radiolabeled nanocarriers have been successfully employed to image and treat tumor models both preclinically and clinically. Future studies should be designed to optimize these novel approaches and to combine targeted delivery, potent radionuclides, imaging agents, chemotherapeutics and/or radiosensitizing agents. We have demonstrated that a co-delivery of radiochemo-therapeutics and simultaneous multifunctional imaging is an advantageous characteristic of nanotargeted radionuclides for cancer imaging and therapy. A good multidisciplines and multi-institutes collaboration between the academia, research institutes, and industry combing with an integrated “bench-to-clinic” translational approach would accelerate the progress in research of nanotargeted radionuclides toward clinical applications for the healthcare of cancer patients.
References
- 1.Strebhardt K, Ullrich A. Paul Ehrlich’s magic bullet concept: 100 years of progress. Nature Reviews Cancer. 2008;8(6):473–480. doi: 10.1038/nrc2394. [DOI] [PubMed] [Google Scholar]
- 2.Adams GP, Weiner LM. Monoclonal antibody therapy of cancer. Nature Biotechnology. 2005;23(9):1147–1157. doi: 10.1038/nbt1137. [DOI] [PubMed] [Google Scholar]
- 3.Reichert JM, Valge-Archer VE. Development trends for monoclonal antibody cancer therapeutics. Nature Reviews Drug Discovery. 2007;6(5):349–356. doi: 10.1038/nrd2241. [DOI] [PubMed] [Google Scholar]
- 4.Carter PJ. Potent antibody therapeutics by design. Nature Reviews Immunology. 2006;6(5):343–357. doi: 10.1038/nri1837. [DOI] [PubMed] [Google Scholar]
- 5.Newsome BW, Ernstoff MS. The clinical pharmacology of therapeutic monoclonal antibodies in the treatment of malignancy; have the magic bullets arrived? British Journal of Clinical Pharmacology. 2008;66(1):6–19. doi: 10.1111/j.1365-2125.2008.03187.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gabizon A, Shmeeda H, Barenholz Y. Pharmacokinetics of pegylated liposomal doxorubicin: review of animal and human studies. Clinical Pharmacokinetics. 2003;42(5):419–436. doi: 10.2165/00003088-200342050-00002. [DOI] [PubMed] [Google Scholar]
- 7.Allen TM, Cullis PR. Drug delivery systems: entering the mainstream. Science. 2004;303(5665):1818–1822. doi: 10.1126/science.1095833. [DOI] [PubMed] [Google Scholar]
- 8.Davis ME, Chen Z, Shin DM. Nanoparticle therapeutics: an emerging treatment modality for cancer. Nature Reviews Drug Discovery. 2008;7(9):771–782. doi: 10.1038/nrd2614. [DOI] [PubMed] [Google Scholar]
- 9.Ferrari M. Cancer nanotechnology: opportunities and challenges. Nature Reviews Cancer. 2005;5(3):161–171. doi: 10.1038/nrc1566. [DOI] [PubMed] [Google Scholar]
- 10.Lammers T, Hennink WE, Storm G. Tumour-targeted nanomedicines: principles and practice. British Journal of Cancer. 2008;99(3):392–397. doi: 10.1038/sj.bjc.6604483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kairemo K, Erba P, Bergström K, Pauwels EKJ. Nanoparticles in cancer. Current Radiopharmaceuticals. 2008;1(1):30–36. [Google Scholar]
- 12.Bawarski WE, Chidlowsky E, Bharali DJ, Mousa SA. Emerging nanopharmaceuticals. Nanomedicine. 2008;4(4):273–282. doi: 10.1016/j.nano.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 13.Sanhai WR, Sakamoto JH, Canady R, Ferrari M. Seven challenges for nanomedicine. Nature Nanotechnology. 2008;3(5):242–244. doi: 10.1038/nnano.2008.114. [DOI] [PubMed] [Google Scholar]
- 14.Milenic DE, Brady ED, Brechbiel MW. Antibody-targeted radiation cancer therapy. Nature Reviews Drug Discovery. 2004;3(6):488–499. doi: 10.1038/nrd1413. [DOI] [PubMed] [Google Scholar]
- 15.Wong JYC. Systemic targeted radionuclide therapy: potential new areas. International Journal of Radiation Oncology Biology Physics. 2006;66(2, supplement):S74–S82. doi: 10.1016/j.ijrobp.2005.05.029. [DOI] [PubMed] [Google Scholar]
- 16.Macklis RM, Pohlman B. Radioimmunotherapy for non-Hodgkin’s lymphoma: a review for radiation oncologists. International Journal of Radiation Oncology Biology Physics. 2006;66(3):833–841. doi: 10.1016/j.ijrobp.2006.05.030. [DOI] [PubMed] [Google Scholar]
- 17.Davies AJ. Radioimmunotherapy for B-cell lymphoma: Y90 ibritumomab tiuxetan and I131 tositumomab. Oncogene. 2007;26(25):3614–3628. doi: 10.1038/sj.onc.1210378. [DOI] [PubMed] [Google Scholar]
- 18.Jacene HA, Filice R, Kasecamp W, Wahl RL. Comparison of 90Y-ibritumomab tiuxetan and 131I- tositumomab in clinical practice. Journal of Nuclear Medicine. 2007;48(11):1767–1776. doi: 10.2967/jnumed.107.043489. [DOI] [PubMed] [Google Scholar]
- 19.Britz-Cunningham SH, Adelstein SJ. Molecular targeting with radionuclides: state of the science. Journal of Nuclear Medicine. 2003;44(12):1945–1961. [PubMed] [Google Scholar]
- 20.Hamoudeh M, Kamleh MA, Diab R, Fessi H. Radionuclides delivery systems for nuclear imaging and radiotherapy of cancer. Advanced Drug Delivery Reviews. 2008;60(12):1329–1346. doi: 10.1016/j.addr.2008.04.013. [DOI] [PubMed] [Google Scholar]
- 21.Mitra A, Nan A, Line BR, Ghandehari H. Nanocarriers for nuclear imaging and radiotherapy of cancer. Current Pharmaceutical Design. 2006;12(36):4729–4749. doi: 10.2174/138161206779026317. [DOI] [PubMed] [Google Scholar]
- 22.Liu Y, Miyoshi H, Nakamura M. Nanomedicine for drug delivery and imaging: a promising avenue for cancer therapy and diagnosis using targeted functional nanoparticles. International Journal of Cancer. 2007;120(12):2527–2537. doi: 10.1002/ijc.22709. [DOI] [PubMed] [Google Scholar]
- 23.Sofou S. Surface-active liposomes for targeted cancer therapy. Nanomedicine. 2007;2(5):711–724. doi: 10.2217/17435889.2.5.711. [DOI] [PubMed] [Google Scholar]
- 24.Ogihara I, Kojima S, Jay M. Differential uptake of gallium-67-labeled liposomes between tumors and inflammatory lesions in rats. Journal of Nuclear Medicine. 1986;27(8):1300–1307. [PubMed] [Google Scholar]
- 25.Klibanov AL, Maruyama K, Torchilin VP, Huang L. Amphipathic polyethyleneglycols effectively prolong the circulation time of liposomes. FEBS Letters. 1990;268(1):235–237. doi: 10.1016/0014-5793(90)81016-h. [DOI] [PubMed] [Google Scholar]
- 26.Papahadjopoulos D, Allen TM, Gabizon A, et al. Sterically stabilized liposomes: improvements in pharmacokinetics and antitumor therapeutic efficacy. Proceedings of the National Academy of Sciences of the United States of America. 1991;88(24):11460–11464. doi: 10.1073/pnas.88.24.11460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lasic D. Doxorubicin in sterically stabilized. Nature. 1996;380(6574):561–562. doi: 10.1038/380561a0. [DOI] [PubMed] [Google Scholar]
- 28.Phillips WT. Delivery of gamma-imaging agents by liposomes. Advanced Drug Delivery Reviews. 1999;37(1–3):13–32. doi: 10.1016/s0169-409x(98)00108-2. [DOI] [PubMed] [Google Scholar]
- 29.Boerman OC, Laverman P, Oyen WJG, Corstens FHM, Storm G. Radiolabeled liposomes for scintigraphic imaging. Progress in Lipid Research. 2000;39(5):461–475. doi: 10.1016/s0163-7827(00)00013-8. [DOI] [PubMed] [Google Scholar]
- 30.Bao A, Goins B, Klipper R, Negrete G, Mahindaratne M, Phillips WT. A novel liposome radiolabeling method using 99mTc-“SNS/S” complexes: in vitro and in vivo evaluation. Journal of Pharmaceutical Sciences. 2003;92(9):1893–1904. doi: 10.1002/jps.10441. [DOI] [PubMed] [Google Scholar]
- 31.Phillips WT, Goins BA, Bao A. Radioactive liposomes. Wiley Interdisciplinary Reviews. Nanomedicine and Nanobiotechnology. 2009;1(1):69–83. doi: 10.1002/wnan.3. [DOI] [PubMed] [Google Scholar]
- 32.Jarrett BR, Gustafsson B, Kukis DL, Louie AY. Synthesis of 64Cu-labeled magnetic nanoparticles for multimodal imaging. Bioconjugate Chemistry. 2008;19(7):1496–1504. doi: 10.1021/bc800108v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee H-Y, Li Z, Chen K, et al. PET/MRI dual-modality tumor imaging using arginine-glycine-aspartic (RGD)-conjugated radiolabeled iron oxide nanoparticles. Journal of Nuclear Medicine. 2008;49(8):1371–1379. doi: 10.2967/jnumed.108.051243. [DOI] [PubMed] [Google Scholar]
- 34.Devaraj NK, Keliher EJ, Thurber GM, Nahrendorf M, Weissleder R. 18F labeled nanoparticles for in Vivo PET-CT imaging. Bioconjugate Chemistry. 2009;20(2):397–401. doi: 10.1021/bc8004649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Line BR, Mitra A, Nan A, Ghandehari H. Targeting tumor angiogenesis: comparison of peptide and polymer-peptide conjugates. Journal of Nuclear Medicine. 2005;46(9):1552–1560. [PubMed] [Google Scholar]
- 36.Almutairi A, Rossin R, Shokeen M, et al. Biodegradable dendritic positron-emitting nanoprobes for the noninvasive imaging of angiogenesis. Proceedings of the National Academy of Sciences of the United States of America. 2009;106(3):685–690. doi: 10.1073/pnas.0811757106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cai W, Chen K, Li Z-B, Gambhir SS, Chen X. Dual-function probe for PET and near-infrared fluorescence imaging of tumor vasculature. Journal of Nuclear Medicine. 2007;48(11):1862–1870. doi: 10.2967/jnumed.107.043216. [DOI] [PubMed] [Google Scholar]
- 38.Chen K, Li Z-B, Wang H, Cai W, Chen X. Dual-modality optical and positron emission tomography imaging of vascular endothelial growth factor receptor on tumor vasculature using quantum dots. European Journal of Nuclear Medicine and Molecular Imaging. 2008;35(12):2235–2244. doi: 10.1007/s00259-008-0860-8. [DOI] [PubMed] [Google Scholar]
- 39.Ducongé F, Pons T, Pestourie C, et al. Fluorine-18-labeled phospholipid quantum dot micelles for in vivo multimodal imaging from whole body to cellular scales. Bioconjugate Chemistry. 2008;19(9):1921–1926. doi: 10.1021/bc800179j. [DOI] [PubMed] [Google Scholar]
- 40.McDevitt MR, Chattopadhyay D, Kappel BJ, et al. Tumor targeting with antibody-functionalized, radiolabeled carbon nanotubes. Journal of Nuclear Medicine. 2007;48(7):1180–1189. doi: 10.2967/jnumed.106.039131. [DOI] [PubMed] [Google Scholar]
- 41.Saad M, Garbuzenko OB, Ber E, et al. Receptor targeted polymers, dendrimers, liposomes: which nanocarrier is the most efficient for tumor-specific treatment and imaging? Journal of Controlled Release. 2008;130(2):107–114. doi: 10.1016/j.jconrel.2008.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shokeen M, Fettig NM, Rossin R. Synthesis, in vitro and in vivo evaluation of radiolabeled nanoparticles. Quarterly Journal of Nuclear Medicine and Molecular Imaging. 2008;52(3):267–277. [PubMed] [Google Scholar]
- 43.Dobrovolskaia MA, McNeil SE. Immunological properties of engineered nanomaterials. Nature Nanotechnology. 2007;2(8):469–478. doi: 10.1038/nnano.2007.223. [DOI] [PubMed] [Google Scholar]
- 44.Lucignani G. Nanoparticles for concurrent multimodality imaging and therapy: the dawn of new theragnostic synergies. European Journal of Nuclear Medicine and Molecular Imaging. 2009;36(5):869–874. doi: 10.1007/s00259-009-1104-2. [DOI] [PubMed] [Google Scholar]
- 45.Elbayoumi TA, Pabba S, Roby A, Torchilin VP. Antinucleosome antibody-modified liposomes and lipid-core micelles for tumor-targeted delivery of therapeutic and diagnostic agents. Journal of Liposome Research. 2007;17(1):1–14. doi: 10.1080/08982100601186474. [DOI] [PubMed] [Google Scholar]
- 46.Elbayoumi TA, Torchilin VP. Enhanced accumulation of long-circulating liposomes modified with the nucleosome-specific monoclonal antibody 2C5 in various tumours in mice: gamma-imaging studies. European Journal of Nuclear Medicine and Molecular Imaging. 2006;33(10):1196–1205. doi: 10.1007/s00259-006-0139-x. [DOI] [PubMed] [Google Scholar]
- 47.Erdogan S, Roby A, Torchilin VP. Enhanced tumor visualization by γ-scintigraphy with 111In-labeled polychelating-polymer-containing immunoliposomes. Molecular Pharmaceutics. 2006;3(5):525–530. doi: 10.1021/mp060055t. [DOI] [PubMed] [Google Scholar]
- 48.Hu G, Lijowski M, Zhang H, et al. Imaging of Vx-2 rabbit tumors with ανβ3- integrin-targeted 111In nanoparticles. International Journal of Cancer. 2007;120(9):1951–1957. doi: 10.1002/ijc.22581. [DOI] [PubMed] [Google Scholar]
- 49.Li L, Wartchow CA, Danthi SN, et al. A novel antiangiogenesis therapy using an integrin antagonist or anti-Flk-1 antibody coated 90Y-labeled nanoparticles. International Journal of Radiation Oncology Biology Physics. 2004;58(4):1215–1227. doi: 10.1016/j.ijrobp.2003.10.057. [DOI] [PubMed] [Google Scholar]
- 50.Liu X, Wang Y, Nakamura K, et al. Auger radiation-induced, antisense-mediated cytotoxicity of tumor cells using a 3-component streptavidin-delivery nanoparticle with 111In. Journal of Nuclear Medicine. 2009;50(4):582–590. doi: 10.2967/jnumed.108.056366. [DOI] [PubMed] [Google Scholar]
- 51.Pan X, Wu G, Yang W, Barth RF, Tjarks W, Lee RJ. Synthesis of cetuximab-immunoliposomes via a cholesterol-based membrane anchor for targeting of EGFR. Bioconjugate Chemistry. 2007;18(1):101–108. doi: 10.1021/bc060174r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shukla S, Wu G, Chatterjee M, et al. Synthesis and biological evaluation of folate receptor-targeted boronated PAMAM dendrimers as potential agents for neutron capture therapy. Bioconjugate Chemistry. 2003;14(1):158–167. doi: 10.1021/bc025586o. [DOI] [PubMed] [Google Scholar]
- 53.Harrington KJ, Mohammadtaghi S, Uster PS, et al. Effective targeting of solid tumors in patients with locally advanced cancers by radiolabeled pegylated liposomes. Clinical Cancer Research. 2001;7(2):243–254. [PubMed] [Google Scholar]
- 54.Carlsson J, Aronsson EF, Hietala S-O, Stigbrand T, Tennvall J. Tumour therapy with radionuclides: assessment of progress and problems. Radiotherapy and Oncology. 2003;66(2):107–117. doi: 10.1016/s0167-8140(02)00374-2. [DOI] [PubMed] [Google Scholar]
- 55.Chen P, Cameron R, Wang J, Vallis KA, Reilly RM. Antitumor effects and normal tissue toxicity of 111In-labeled epidermal growth factor administered to athymic mice bearing epidermal growth factor receptor-positive human breast cancer xenografts. Journal of Nuclear Medicine. 2003;44(9):1469–1478. [PubMed] [Google Scholar]
- 56.Reilly RM, Chen P, Wang J, Scollard D, Cameron R, Vallis KA. Preclinical pharmacokinetic, biodistribution, toxicology, and dosimetry studies of 111In-DTPA-human epidermal growth factor: an auger electron-emitting radiotherapeutic agent for epidermal growth factor receptor-positive breast cancer. Journal of Nuclear Medicine. 2006;47(6):1023–1031. [PubMed] [Google Scholar]
- 57.Reilly RM, Kiarash R, Cameron RG, et al. 111In-labeled EGF is selectively radiotoxic to human breast cancer cells overexpressing EGFR. Journal of Nuclear Medicine. 2000;41(3):429–438. [PubMed] [Google Scholar]
- 58.Reske SN, Deisenhofer S, Glutting G, et al. 111I-ITdU-mediated nanoirradiation of DNA efficiently induces cell kill in HL60 leukemia cells and in doxorubicin-, β-, or γ-radiation-resistant cell lines. Journal of Nuclear Medicine. 2007;48(6):1000–1007. doi: 10.2967/jnumed.107.040337. [DOI] [PubMed] [Google Scholar]
- 59.Smith AM, Duan H, Mohs AM, Nie S. Bioconjugated quantum dots for in vivo molecular and cellular imaging. Advanced Drug Delivery Reviews. 2008;60(11):1226–1240. doi: 10.1016/j.addr.2008.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Harrington KJ, Lewanski CR, Stewart JSW. Liposomes as vehicles for targeted therapy of cancer. Part 1: preclinical development. Clinical Oncology. 2000;12(1):2–15. doi: 10.1053/clon.2000.9104. [DOI] [PubMed] [Google Scholar]
- 61.Ogihara-Umeda I, Sasaki T, Kojima S, Nishigori H. Optimal radiolabeled liposomes for tumor imaging. Journal of Nuclear Medicine. 1996;37(2):326–332. [PubMed] [Google Scholar]
- 62.Harrington KJ, Lewanski CR, Stewart JSW. Liposomes as vehicles for targeted therapy of cancer. Part 2: clinical development. Clinical Oncology. 2000;12(1):16–24. doi: 10.1053/clon.2000.9105. [DOI] [PubMed] [Google Scholar]
- 63.Kleiter MM, Yu D, Mohammadian LA, et al. A tracer dose of technetium-99m- labeled liposomes can estimate the effect of hyperthermia on intratumoral doxil extravasation. Clinical Cancer Research. 2006;12(22):6800–6807. doi: 10.1158/1078-0432.CCR-06-0839. [DOI] [PubMed] [Google Scholar]
- 64.Jensen GM, Bunch TH. Conventional liposome performance and evaluation: lessons from the development of Vescan. Journal of Liposome Research. 2007;17(3-4):121–137. doi: 10.1080/08982100701527981. [DOI] [PubMed] [Google Scholar]
- 65.Goins BA. Radiolabeled lipid nanoparticles for diagnostic imaging. Expert Opinion on Medical Diagnostics. 2008;2(7):853–873. doi: 10.1517/17530059.2.7.853. [DOI] [PubMed] [Google Scholar]
- 66.Urakami T, Akai S, Katayama Y, Harada N, Tsukada H, Oku N. Novel amphiphilic probes for [18F]-radiolabeling preformed liposomes and determination of liposomal trafficking by positron emission tomography. Journal of Medicinal Chemistry. 2007;50(26):6454–6457. doi: 10.1021/jm7010518. [DOI] [PubMed] [Google Scholar]
- 67.Oku N. Delivery of contrast agents for positron emission tomography imaging by liposomes. Advanced Drug Delivery Reviews. 1999;37(1–3):53–61. doi: 10.1016/s0169-409x(98)00110-0. [DOI] [PubMed] [Google Scholar]
- 68.Marik J, Tartis MS, Zhang H, et al. Long-circulating liposomes radiolabeled with [18F]fluorodipalmitin ([18F]FDP) Nuclear Medicine and Biology. 2007;34(2):165–171. doi: 10.1016/j.nucmedbio.2006.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Seo JW, Zhang H, Kukis DL, Meares CF, Ferrara KW. A novel method to label preformed liposomes with 64Cu for positron emission tomography (PET) imaging. Bioconjugate Chemistry. 2008;19(12):2577–2584. doi: 10.1021/bc8002937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wang H-E, Yu H-M, Lu Y-C, et al. Internal radiotherapy and dosimetric study for 111In/177Lu-pegylated liposomes conjugates in tumor-bearing mice. Nuclear Instruments and Methods in Physics Research A. 2006;569(2):533–537. [Google Scholar]
- 71.Lee W-C, Hwang J-J, Tseng Y-L, et al. Therapeutic efficacy evaluation of 111In-VNB-liposome on human colorectal adenocarcinoma HT-29/luc mouse xenografts. Nuclear Instruments and Methods in Physics Research A. 2006;569(2):497–504. [Google Scholar]
- 72.Chang Y-J, Chang C-H, Chang T-J, et al. Biodistribution, pharmacokinetics and microSPECT/CT imaging of 188Re-BMEDA-liposome in a C26 murine colon carcinoma solid tumor animal model. Anticancer Research. 2007;27(4B):2217–2225. [PubMed] [Google Scholar]
- 73.Chang Y-J, Chang C-H, Yu C-Y, et al. Therapeutic efficacy and microSPECT/CT imaging of 188Re-DXR-liposome in a C26 murine colon carcinoma solid tumor model. Nuclear Medicine and Biology. 2010;37(1):95–104. doi: 10.1016/j.nucmedbio.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 74.Emfietzoglou D, Kostarelos K, Sgouros G. An analytic dosimetry study for the use of radionuclide-liposome conjugates in internal radiotherapy. Journal of Nuclear Medicine. 2001;42(3):499–504. [PubMed] [Google Scholar]
- 75.Bao A, Goins B, Klipper R, Negrete G, Phillips WT. 186Re-liposome labeling using 186Re-SNS/S complexes: in vitro stability, imaging, and biodistribution in rats. Journal of Nuclear Medicine. 2003;44(12):1992–1999. [PubMed] [Google Scholar]
- 76.Bao A, Goins B, Klipper R, Negrete G, Phillips WT. Direct 99mTc labeling of pegylated liposomal doxorubicin (Doxil) for pharmacokinetic and non-invasive imaging studies. Journal of Pharmacology and Experimental Therapeutics. 2004;308(2):419–425. doi: 10.1124/jpet.103.059535. [DOI] [PubMed] [Google Scholar]
- 77.Phillips WT, Klipper R, Goins B. Novel method of greatly enhanced delivery of liposomes to lymph nodes. Journal of Pharmacology and Experimental Therapeutics. 2000;295(1):309–313. [PubMed] [Google Scholar]
- 78.Wang SX, Bao A, Herrera SJ, et al. Intraoperative 186Re-liposome radionuclidetherapy in a head and neck squamous cell carcinoma xenograft positive surgical margin model. Clinical Cancer Research. 2008;14(12):3975–3983. doi: 10.1158/1078-0432.CCR-07-4149. [DOI] [PubMed] [Google Scholar]
- 79.Zavaleta C, Goins B, Bao A, Mcmanus L, Mcmahan CA, Phillips W. Imaging of 186Re-liposome therapy in ovarian cancer xenograft model of peritoneal carcinomatosis. Journal of Drug Targeting. 2008;16(7-8):626–637. doi: 10.1080/10611860802230372. [DOI] [PubMed] [Google Scholar]
- 80.Chen L-C, Chang C-H, Yu C-Y, et al. Biodistribution, pharmacokinetics and imaging of 188Re-BMEDA-labeled pegylated liposomes after intraperitoneal injection in a C26 colon carcinoma ascites mouse model. Nuclear Medicine and Biology. 2007;34(4):415–423. doi: 10.1016/j.nucmedbio.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 81.Chow T-H, Lin Y-Y, Hwang J-J, et al. Improvement of biodistribution and therapeutic index via increase of polyethylene glycol on drug-carrying liposomes in an HT-29/luc xenografted mouse model. Anticancer Research. 2009;29(6):2111–2120. [PubMed] [Google Scholar]
- 82.Change M-Y, Seideman J, Sofou S. Enhanced loading efficiency and retention of 225Ac in rigid liposomes for potential targeted therapy of micrometastases. Bioconjugate Chemistry. 2008;19(6):1274–1282. doi: 10.1021/bc700440a. [DOI] [PubMed] [Google Scholar]
- 83.Sofou S, Kappel BJ, Jaggi JS, McDevitt MR, Scheinberg DA, Sgouros G. Enhanced retention of the α-particle-emitting daughters of actinium-225 by liposome carriers. Bioconjugate Chemistry. 2007;18(6):2061–2067. doi: 10.1021/bc070075t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sofou S, Thomas JL, Lin H-Y, McDevitt MR, Scheinberg DA, Sgouros G. Engineered liposomes for potential α-particle therapy of metastatic cancer. Journal of Nuclear Medicine. 2004;45(2):253–260. [PubMed] [Google Scholar]
- 85.Nakamura H, Ueno M, Ban HS, et al. Development of boron nanocapsules for neutron capture therapy. Applied Radiation and Isotopes. 2009;67(7-8):S84–S87. doi: 10.1016/j.apradiso.2009.03.091. [DOI] [PubMed] [Google Scholar]
- 86.Yanagie H, Maruyama K, Takizawa T, et al. Application of boron-entrapped stealth liposomes to inhibition of growth of tumour cells in the in vivo boron neutron-capture therapy model. Biomedicine and Pharmacotherapy. 2006;60(1):43–50. doi: 10.1016/j.biopha.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 87.Harrington KJ, Rowlinson-Busza G, Syrigos KN, et al. Pegylated liposome-encapsulated doxorubicin and cisplatin enhance the effect of radiotherapy in a tumor xenograft model. Clinical Cancer Research. 2000;6(12):4939–4949. [PubMed] [Google Scholar]
- 88.Huber PE, Bischof M, Jenne J, et al. Trimodal cancer treatment: beneficial effects of combined antiangiogenesis, radiation, and chemotherapy. Cancer Research. 2005;65(9):3643–3655. doi: 10.1158/0008-5472.CAN-04-1668. [DOI] [PubMed] [Google Scholar]
- 89.Lammers T, Subr V, Peschke P, et al. Image-guided and passively tumour-targeted polymeric nanomedicines for radiochemotherapy. British Journal of Cancer. 2008;99(6):900–910. doi: 10.1038/sj.bjc.6604561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chang C-H, Stabin MG, Chang Y-J, et al. Comparative dosimetric evaluation of nanotargeted 188Re-(DXR)- liposome for internal radiotherapy. Cancer Biotherapy and Radiopharmaceuticals. 2008;23(6):749–758. doi: 10.1089/cbr.2008.0489. [DOI] [PubMed] [Google Scholar]
- 91.Chen L-C, Chang C-H, Yu C-Y, et al. Pharmacokinetics, micro-SPECT/CT imaging and therapeutic efficacy of 188Re-DXR-liposome in C26 colon carcinoma ascites mice model. Nuclear Medicine and Biology. 2008;35(8):883–893. doi: 10.1016/j.nucmedbio.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 92.Chow T-H, Lin Y-Y, Hwang J-J, et al. Diagnostic and therapeutic evaluation of 111In-vinorelbine-liposomes in a human colorectal carcinoma HT-29/luc-bearing animal model. Nuclear Medicine and Biology. 2008;35(5):623–634. doi: 10.1016/j.nucmedbio.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 93.Lin Y-Y, Li J-J, Chang C-H, et al. Evaluation of pharmacokinetics of 111In-labeled VNB-PEGylated liposomes after intraperitoneal and intravenous administration in a tumor/ascites mouse model. Cancer Biotherapy and Radiopharmaceuticals. 2009;24(4):453–460. doi: 10.1089/cbr.2008.0572. [DOI] [PubMed] [Google Scholar]
- 94.Kostarelos K, Emfietzoglou D. Tissue dosimetry of liposome-radionuclide complexes for internal radiotherapy: toward liposome-targeted therapeutic radiopharmaceuticals. Anticancer Research. 2000;20(5A):3339–3345. [PubMed] [Google Scholar]
- 95.Syme AM, McQuarrie SA, Middleton JW, Fallone BG. Dosimetric model for intraperitoneal targeted liposomal radioimmunotherapy of ovarian cancer micrometastases. Physics in Medicine and Biology. 2003;48(10):1305–1320. doi: 10.1088/0031-9155/48/10/305. [DOI] [PubMed] [Google Scholar]
- 96.Huwyler J, Drewe J, Krähenbühl S. Tumor targeting using liposomal antineoplastic drugs. International Journal of Nanomedicine. 2008;3(1):21–29. [PMC free article] [PubMed] [Google Scholar]
- 97.Park JW, Benz CC, Martin FJ. Future directions of liposome- and immunoliposome-based cancer therapeutics. Seminars in Oncology. 2004;31(13):196–205. doi: 10.1053/j.seminoncol.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 98.Cheon J, Lee J-H. Synergistically integrated nanoparticles as multimodal probes for nanobiotechnology. Accounts of Chemical Research. 2008;41(12):1630–1640. doi: 10.1021/ar800045c. [DOI] [PubMed] [Google Scholar]
- 99.Elbayoumi TA, Torchilin VP. Enhanced cytotoxicity of monoclonal anticancer antibody 2C5-modified doxorubicin-loaded PEGylated liposomes against various tumor cell lines. European Journal of Pharmaceutical Sciences. 2007;32(3):159–168. doi: 10.1016/j.ejps.2007.05.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kamaly N, Kalber T, Thanou M, Bell JD, Miller AD. Folate receptor targeted bimodal liposomes for tumor magnetic resonance imaging. Bioconjugate Chemistry. 2009;20(4):648–655. doi: 10.1021/bc8002259. [DOI] [PubMed] [Google Scholar]
- 101.Lukyanov AN, Elbayoumi TA, Chakilam AR, Torchilin VP. Tumor-targeted liposomes: doxorubicin-loaded long-circulating liposomes modified with anti-cancer antibody. Journal of Controlled Release. 2004;100(1):135–144. doi: 10.1016/j.jconrel.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 102.Diagaradjane P, Orenstein-Cardona JM, Colón-Casasnovas NE, et al. Imaging epidermal growth factor receptor expression in vivo: pharmacokinetic and biodistribution characterization of a bioconjugated quantum dot nanoprobe. Clinical Cancer Research. 2008;14(3):731–741. doi: 10.1158/1078-0432.CCR-07-1958. [DOI] [PubMed] [Google Scholar]
- 103.Koole R, van Schooneveld MM, Hilhorst J, et al. Paramagnetic lipid-coated silica nanoparticles with a fluorescent quantum dot core: a new contrast agent platform for multimodality imaging. Bioconjugate Chemistry. 2008;19(12):2471–2479. doi: 10.1021/bc800368x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.van Schooneveld MM, Vucic E, Koole R, et al. Improved biocompatibility and pharmacokinetics of silica nanoparticles by means of a lipid coating: a multimodality investigation. Nano Letters. 2008;8(8):2517–2525. doi: 10.1021/nl801596a. [DOI] [PubMed] [Google Scholar]
- 105.Tasciotti E, Liu X, Bhavane R, et al. Mesoporous silicon particles as a multistage delivery system for imaging and therapeutic applications. Nature Nanotechnology. 2008;3(3):151–157. doi: 10.1038/nnano.2008.34. [DOI] [PubMed] [Google Scholar]
- 106.Ganta S, Amiji M. Coadministration of paclitaxel and curcumin in nanoemulsion formulations to overcome multidrug resistance in tumor cells. Molecular Pharmaceutics. 2009;6(3):928–939. doi: 10.1021/mp800240j. [DOI] [PubMed] [Google Scholar]
- 107.Garnett MC, Kallinteri P. Nanomedicines and nanotoxicology: some physiological principles. Occupational Medicine. 2006;56(5):307–311. doi: 10.1093/occmed/kql052. [DOI] [PubMed] [Google Scholar]
- 108.Nel A, Xia T, Mädler L, Li N. Toxic potential of materials at the nanolevel. Science. 2006;311(5761):622–627. doi: 10.1126/science.1114397. [DOI] [PubMed] [Google Scholar]
- 109.Dobrovolskaia MA, Germolec DR, Weaver JL. Evaluation of nanoparticle immunotoxicity. Nature Nanotechnology. 2009;4(7):411–414. doi: 10.1038/nnano.2009.175. [DOI] [PubMed] [Google Scholar]
- 110.Vega-Villa KR, Takemoto JK, Yáñez JA, Remsberg CM, Forrest ML, Davies NM. Clinical toxicities of nanocarrier systems. Advanced Drug Delivery Reviews. 2008;60(8):929–938. doi: 10.1016/j.addr.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 111.Fisher DR, Shen S, Meredith RF. MIRD dose estimate report No. 20: radiation absorbed-dose estimates for 111In- and 90Y-ibritumomab tiuxetan. Journal of Nuclear Medicine. 2009;50(4):644–652. doi: 10.2967/jnumed.108.057331. [DOI] [PubMed] [Google Scholar]