Abstract
Background
Although high blood pressure is associated with significant morbidity and mortality, the proportion reaching the goal blood pressures as outlined in the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, Treatment of High Blood Pressure (JNC 7) is low. We conducted a randomized trial in primary care practices of a multifactorial intervention targeted to improve providers' adherence to hypertension guidelines.
Method
A total of 61 primary care practices in North Carolina were randomized to receive either a multifactorial intervention (guideline dissemination via a continuing medical education session, academic detailing sessions, audit and feedback on preintervention rates of adherence, and automated blood pressure machines) or an attention control of similar magnitude but targeted at a different guideline. Outcomes were determined through review of patient charts conducted by an independent masked quality assurance organization.
Results
We found no difference between the 2 groups in any of the adherence measures including no difference in the percentage of patients at goal (intervention 49.2%, control 50.6%), with undiagnosed hypertension (18.1% vs 13.6%), average systolic (126 vs 125.1 mm Hg), or diastolic blood pressure (73.1 vs 73.4 mm Hg). Similarly, there was no difference in provider adherence to treatment recommendations (use of thiazide-type diuretic as first-line therapy: 32% vs 29.5%; use of 2-drug therapy in stage 2 hypertension: 11.3% vs 10.4%).
Conclusion
An intensive, multifactorial intervention did not improve adherence to national hypertension guidelines among community-based primary care. Efforts should be focused on other types of interventions to improve rates of control of hypertension.
Hypertension is associated with significant morbidity and mortality. More than one third of the United States adult population is affected by hypertension1 with approximately 277,000 deaths in 2003 directly or indirectly attributable to hypertension.2 Despite the high prevalence and significant morbidity, only 35% of those with diagnosed hypertension reach their goal blood pressure despite a wide variety of effective treatments.1 The Joint National Commission on the Detection and Treatment of Hypertension, seventh edition (JNC 7) was designed to provide a framework for optimal care of patients with hypertension including diagnosis and treatment.3 Despite the strong evidence base of the JNC 7 guidelines, previous studies have shown low rates of compliance to its recommendations.4 The basis for this low adherence is multifactorial and includes inaccuracy and variability in blood pressure measurement, clinical inertia, poor understanding of the consequences of elevated blood pressure by patients, poor adherence with lifestyle and pharmacologic therapy, and difficulties due to the cost of care.5
Previous studies on improving adherence to the JNC 7 recommendations have focused on overcoming 1 or 2 of these barriers.6,7 Although these have been modestly successful, they have not resulted in substantial improvements in the percent of patients at goal blood pressure or in actual blood pressure values, indicating the need for a broader intervention. The Guideline Adherence for Heart Health (GLAD) Heart Blood Pressure study was designed to determine whether a multifaceted intervention would successfully improve compliance to the JNC 7 guideline and ultimately improve the percent of patients reaching their goal blood pressure.
Methods
The GLAD Heart Blood Pressure Study was a randomized, controlled trial of a multifaceted intervention targeted at primary care practices and designed to improve blood pressure control. The unit of randomization was the primary care practice, whereas the unit for outcome ascertainment was a random selection of medical records of patients seen at each practice. Control practices received an intervention designed to improve compliance to cholesterol management guidelines (NCEP Adult Treatment Panel III-ATPIII)8 with the results reported elsewhere.9 The study was approved by the Institutional Review Board at Wake Forest University School of Medicine.
Participants
Medical practices were eligible for recruitment if they provided primary care to their patients (either internal medicine or family medicine or a combination of the 2), were located within 150 miles of the university coordinating the study, had been in practice for at least 1 year, and had at least 50% of the practice's providers indicate willingness to participate in the intervention. Practices with direct affiliation to a medical school or residency program were excluded from participating. Practices were randomized using block randomization stratified for practice size.
Patient medical records were eligible for abstraction for the outcome measures if they were adults (aged 21–84 years) and seen in the participating primary care practices during the May 1, 2004, to April 30, 2006, follow-up period.
Study intervention
The GLAD Heart Blood Pressure intervention was multifaceted and occurred between September 2004 and June 2006. To increase familiarity with the blood pressure guidelines, all providers, regardless of their randomization status, were invited to an initial educational session that provided an overview of both the intervention guideline, JNC 7, and the guideline that was the focus of the control group, ATPIII. All participants were provided with a paper copy of the JNC 7 guidelines. Academic detailing sessions that targeted the health care providers were held every 6 months at both intervention and control practices. These sessions lasted 1 hour, were case based, and were open to both the providers and the clinic staff. The focus of each session was specific to the randomization status of the practice, with both groups (intervention and control) receiving comparable interaction with the investigators. The focuses for the blood pressure practices were (1) making structural changes to the clinic to improve blood pressure control; (2) helping patients make lifestyle changes as a therapy; (3) rational medication use; and (4) dealing with medication side effects. At each session, written education material for health care providers was distributed as were educational tools for patients (posters for exam rooms, education pamphlets, pill boxes). Provider material included medical record flow sheets, exercise prescription pads, copies of the guidelines, and summaries of supporting medical literature. In addition to the education sessions, intervention practices were provided with automatic blood pressure machines (Omron HEM907 [Omron Healthcare, Kyoto, Japan]—1 for every 3 providers in the practice) for use in their clinic.
The final component of the intervention was feedback of the preintervention hypertension diagnosis and control levels for the practice. The blood pressure intervention was added to the parent study testing the effect of an intervention on cholesterol control; therefore, preintervention medical record abstraction was limited to patients who had received a screening lipid panel in the preintervention period and consisted only of the blood pressure value at the time of the lipid panel. No antihypertensive medication information was obtained at this preintervention review. Chart reviews were conducted by the Carolinas Center for Medical Excellence (Cary, NC), an independent quality monitoring group, which was masked to study arm assignment of the practice. Feedback on the blood pressure results from the baseline chart audit was shared with all clinics regardless of randomization status.
Control intervention
Control practices received an intervention that was similar in intensity and structure to that of the intervention practices but focused on the ATPIII guideline. Health care providers in these practices received a PDA tool with a software program of the ATPIII guideline, 1 initial CME session, 4 academic detailing sessions of similar length and structure, feedback on baseline adherence, and educational material for both health care providers and patients about cholesterol management.
Study objective and outcomes
Outcomes were assessed through a chart review of a random sample of charts at each practice. Evaluation data were abstracted from the medical charts. Demographic information, medical comorbidities, date of blood pressure diagnosis (if it occurred during the abstraction window), systolic and diastolic blood pressure values for visits during the abstraction window, recommendations of therapeutic lifestyle changes, and blood pressure medications were abstracted for each participant for visits occurring during the 2-year period occurring between May 1, 2004, and April 30, 2006.
Our primary measure of guideline compliance was the average percent of patients at or below JNC 7 blood pressure goal in intervention practices as compared to control practices. Secondary outcomes were the percent of patients with undiagnosed hypertension, mean systolic and diastolic blood pressure, intensification of therapy in those not at goal, and appropriate selection of initial therapy in those with newly diagnosed hypertension.
Undiagnosed hypertension was defined as a blood pressure (≥140 systolic or ≥90 diastolic, or ≥130 systolic or ≥80 diastolic if diabetes or chronic renal disease was a comorbidity) with no diagnosis of hypertension documented and no use of blood pressure–lowering medication. A patient was not considered to have undiagnosed hypertension if only 1 blood pressure was available during the abstraction window. At-goal blood pressure was defined as a blood pressure below 140/90 mm Hg or below 130/80 mm Hg if the patient had diabetes or chronic renal disease. The last blood pressure documented during the abstraction window was used to determine whether the patient was at goal and for determination of the mean systolic and diastolic blood pressure for each clinic. Appropriate intensification if not at goal was defined as either the receipt of counseling on lifestyle modification or the addition or increase in dose of blood pressure–lowering medications with no discontinuation or reduction of dose of currently prescribed medications. Appropriateness of initial therapy was measured in 2 ways: (1) in patients with no modifying comorbidities, a thiazide-type diuretic used as (one of) the initial medications; and (2) in patients with stage 2 hypertension (>160/100), the initial medication therapy decision was 2-drug therapy.
Statistical issues
After recruitment, randomization was stratified by practice specialty (internal medicine vs family medicine) and size and blocked (n = 4) to achieve balance within strata. Neither sites nor investigators were masked to study intervention status; however, chart abstractors were masked to intervention status.
Statistical analysis followed an intention-to-treat model with all patient records analyzed within the original medical practice intervention assignment. Sample size was determined using a 2-sided α of .05 with an intraclass correlation of 0.04 to 0.06. The absolute difference in patients meeting goal blood pressure was assumed to be 10% with the control group having a prevalence of blood pressure control of 60%. With these assumptions, a recruitment goal of 64 practices (32 in each group) was set to provide power of 80% to 90% depending on the intraclass correlation.
Practice characteristics at the time of randomization were compared between those assigned to JNC 7 versus control using χ2 tests. The assessment of patient level treatment differences related to demographic characteristics, medical history, hypertension status, and compliance to guidelines was conducted using the Rao-Scott χ2 test for categorical variables (such as race/ethnicity and guideline compliance) and fitting linear models for continuous variables (such as age and blood pressure levels). The procedures used provided adjustment for the clustered study design. A 2-tailed critical value of α = .05 was used.
To test whether the degree of exposure to the intervention affected provider adherence to the guideline, we devised an “intervention implementation” measure. Although the intervention was multifocal, a large portion consisted of the academic detailing educational visits. We calculated the average health care provider attendance for each practice as a proxy for intervention implementation. Adherence to the guideline was then compared within the JNC arm between low and high intervention implementation groups.
Results
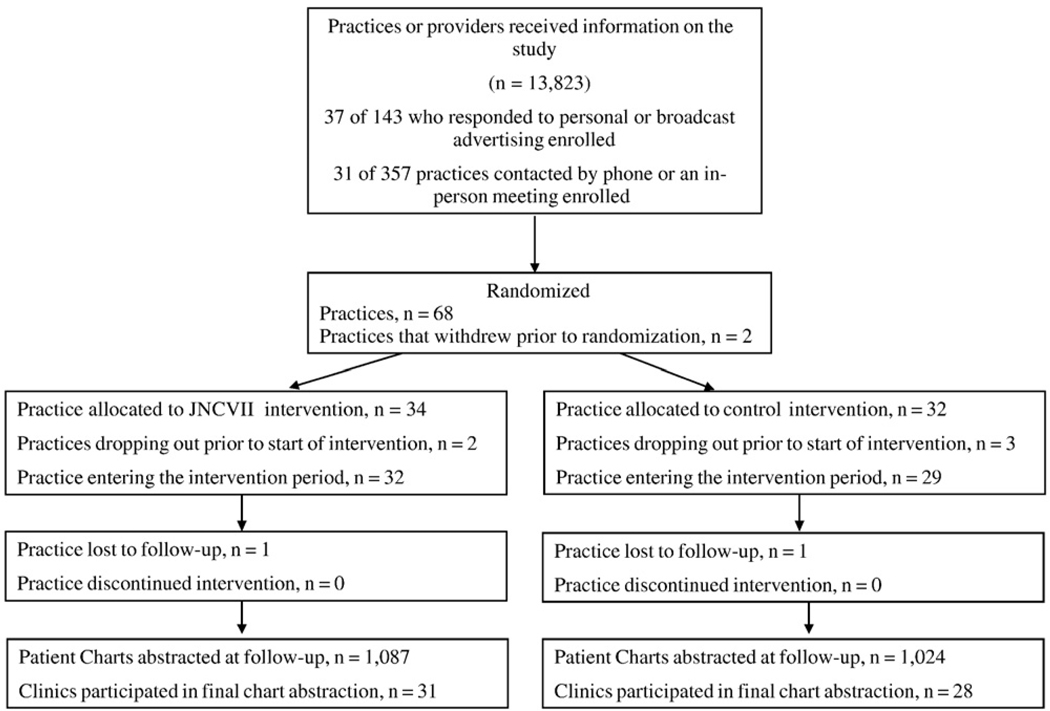
A full description of the practice recruitment process has been described elsewhere.10 Primary care practices and providers were approached using a variety of methods between June 2003 and April 2004. Briefly, 13,823 clinics and providers received information on the study through personal letters, phone calls, and a variety of mass marketing techniques. A total of 143 practices responded to personal and broadcast advertisement with 37 ultimately enrolling in the study. An additional 31 of 357 practices contacted by phone or an in-person meeting also enrolled for a total of 68 practices. Two practices withdrew before randomization and an additional 5 practices withdrew after randomization but before the start of the intervention. This resulted in 61 practices entering the intervention period with 32 in the blood pressure intervention arm and 29 in the control arm. All practices completed the intervention but only 59 practices participated in the final chart evaluation (see Figure 1). One practice that did not meet inclusion criteria (open for <1 year) was enrolled and is included in the results. All practices participated in all aspects of the intervention, although there was variation by health care provider in participation in the academic detailing sessions within practices.
Figure 1.
Flow diagram of clinics enrolled in GLAD Heart.
The intervention and control groups were well matched on practice type (internal medicine vs family medicine), number of providers, location (rural vs urban), and ethnicity and gender of providers (see Table I). The average number of health care providers in the intervention arm was 4.0 per practice (SD 3.3, range 1–14) and 3.0 per practice (SD 2.3, range 1–11) in the control arm.
Table I.
Practice characteristics
| Characteristic | JNC 7 (n = 32) |
Control (n = 29) |
P value* |
|---|---|---|---|
| Practice type | .94 | ||
| Family medicine | 75 (24) | 76 (22) | |
| Internal medicine | 25 (8) | 24 (7) | |
| Practice size | |||
| Single provider | 16 (5) | 28 (8) | .33 |
| 2–4 providers | 53 (17) | 55 (16) | |
| >5 providers | 31 (10) | 17 (5) | |
| Rural practice location | 19 (6) | 24 (7) | .61 |
| Female provider predominant | 25 (8) | 28 (8) | .82 |
| Minority provider predominant | 22 (7) | 10 (3) | .31 |
Values are shown as % (n).
Based on χ2 test except last entry (minority provider) based on Fisher exact test owing to small expected cell sizes.
We examined 2,111 unique patient medical records during the evaluation period. The patients were well matched between the intervention and control groups (see Table II). The majority were female with an average age of 49 years and predominantly non-Hispanic white, although ethnicity was frequently missing. The most common comorbidity was tobacco use with diabetes the second most common. The mean body mass index was 29 kg/m2.
Table II.
Characteristics of patients in the evaluation chart review (N = 2111)
| Characteristic | JNC 7 (n = 1087) |
Control (n = 1024) |
P value |
|---|---|---|---|
| Mean age (y, SD) | 49.9 (1.4) | 49.0 (0.9) | .53 |
| Mean BMI (SD) | 29.5 (0.5) | 29.3 (0.3) | .71 |
| Female, % (n) | 59.6 (648) | 58.8 (602) | .79 |
| Race/ethnicity, % (n) | .05 | ||
| Non-Hispanic white | 55.0 (598) | 67.1 (687) | |
| African American | 13.8 (150) | 5.9 (60) | |
| Hispanic | 0.9 (10) | 1.6 (16) | |
| Other | 1.0 (11) | 1.6 (16) | |
| Unknown | 29.3 (318) | 23.9 (245) | |
| Medical history, % (n) | |||
| CAD | 7.4 (80) | 8.9 (91) | .28 |
| CHF | 2.6 (28) | 2.4 (2.5) | .87 |
| Stroke/TIA | 3.0 (33) | 2.4 (25) | .44 |
| PAD | 2.3 (25) | 2.6 (27) | .68 |
| Diabetes | 14.1 (153) | 12.3 (126) | .31 |
| Renal disease (diagnosis or serum creatine >2.0) | 3.4 (37) | 3.9 (40) | .60 |
| Current tobacco use, % (n) | 25.5 (244) | 28.1 (251) | .35 |
BMI, Body mass index; CAD, coronary artery disease; CHF, congestive heart failure; TIA, transient ischemic attack; PAD, periperal artery disease.
Nearly one half of the unique patient records examined did not show any evidence of diagnosed or undiagnosed hypertension (see Table III). Approximately 35% had evidence of a diagnosis of hypertension (either listed as a problem in a clinical note or in the problem list or use of a blood pressure–lowering medication), whereas a further 10% were given a diagnosis of hypertension in the chart abstraction window. The remaining 9% had elevated blood pressures in the chart, but no evidence that this condition was recognized via a diagnosis. A slightly higher percentage of unrecognized hypertension was observed in practices randomized to the JNC 7 arm.
Table III.
Hypertension status of patients in the evaluation period (N = 2111)
| JNC 7 (N = 1087) |
Control (N = 1024) |
P value | |
|---|---|---|---|
| None | 42.7 (464) | 49.8 (510) | .07 |
| Established | 35.5 (386) | 34.0 (348) | |
| Newly diagnosed | 11.4 (124) | 9.4 (96) | |
| Unrecognized | 10.4 (113) | 6.8 (70) |
Values are shown as % (n).
We found no difference in compliance to JNC 7 guidelines between the intervention practices and the control practices. Specifically, there was no statistical difference in the percentage of patients with undiagnosed hypertension, percent of patients at goal blood pressure, or average systolic or diastolic blood pressure. To account for the contribution of patient adherence to medication and behavioral counseling to overall adherence to guidelines, we also examined aspects that were entirely the purview of health care providers. Again, no difference was seen between intervention practices and control practices when we compared the percent of patients receiving therapeutic lifestyle counseling, medication intensification when not at goal blood pressure, or selection of appropriate first line therapy for patients with newly diagnosed hypertension (see Table IV).
Table IV.
Compliance with recommendations among patient with hypertension
| Characteristic | JNC 7 | Control | P value |
|---|---|---|---|
| At-goal blood pressure | 49.2% (251) | 50.6% (224) | .75 |
| Undiagnosed hypertension | 18.1% (113) | 13.6% (70) | .12 |
| Average systolic blood pressure | 126.4 | 125.1 | .68 |
| Average diastolic blood pressure | 73.1 | 73.4 | .87 |
| Therapeutic lifestyle counseling among those not at goal | 40.3% (131) | 36.7% (101) | .58 |
| Medication addition or increase among those not at goal | 59.9% (130) | 53.8% (98) | .30 |
| Initial treatment with thiazide-type diuretic among newly diagnosed hypertension | 32.0% (24) | 29.5% (18) | .82 |
| Initial treatment with 2-drug therapy among newly diagnosed stage 2 hypertension | 11.3% (14) | 10.4% (10) | .83 |
Values are shown as % (n).
We found no statistical difference between intervention and control practices for our measure of intervention implementation (intervention practices average attendance 80%, control practices 86%, P = .15). When we compared adherence to the guideline by our intervention implementation measure within the intervention practices, we found no difference in provision of therapeutic lifestyle counseling among those not at goal (low implementers 42.3% vs high implementers 38.6%, P = .7); medication addition or increase among those not at goal (low 61.8% vs high 58.3%, P = .63); use of thiazide diuretic as a first-line treatment (low 32.4% vs high 31.7%, P = .97); use of 2 drugs for initial treatment in stage 2 hypertension (low 10.7% vs high 11.8%, P = .86).
Discussion
In this randomized controlled trial of a multifactorial intervention to improve adherence to hypertension guidelines, we found no difference in the percentage of patients with undiagnosed hypertension, percent of patients with hypertension at goal blood pressure, or mean goal blood pressure at the conclusion of the intervention. In each of study arms, approximately 50% were at goal blood pressure at the end of the study, slightly better than the rate of control nationally in 2003.1 Although this lack of difference in patient outcomes between treatment groups may be due to the focus of the intervention on health care provider behaviors, we did not see any difference either in the provision of lifestyle counseling, selection of first-line therapy for patients with newly diagnosed hypertension, or intensification of therapy in patients with uncontrolled hypertension. These outcomes point to an overall lack of effectiveness of the intervention to change provider behavior.
The GLAD Heart intervention was multifactorial and designed to overcome a variety of barriers. A major component of the intervention was academic detailing, a technique that has been tested in other studies. Simon et al11 conducted a randomized study in primary care practice of academic detailing to change prescribing habits of physicians. Although they found an increase in the use of diuretics and β blockers in the intervention practices, they found no change in blood pressure control. Fretheim et al6 also found an increase in the use of guideline-recommended medication in their trial of a tailored intervention that included academic detailing, audit and feedback, and provider and patient educational material, but found no change in achieving blood pressure goals. Hennessy et al12 conducted a randomized controlled trial of a multifaceted intervention that included academic detailing, audit and feedback, and patient and provider education. They found no difference either in blood pressure control in the intervention practices. These studies differed from ours in that they had a less intense intervention (a single academic detailing visit vs 4 academic detailing visits in GLAD Heart), shorter period of intervention and follow-up (6 months to 1 year compared to 2 years for GLAD Heart), and did not include an automatic blood pressure machine to increase accuracy of measurement.
Academic detailing (also called educational outreach visits) is based on the marketing outreach conducted by pharmaceutical companies. There has been enthusiasm for incorporation of this type of intervention in other settings. The federal government is currently considering funding of a nationwide program of academic detailing targeted at increasing the use of lower cost prescription medication,13 and examples of similar programs sponsored by states and large insurance companies exist.14 A Cochrane collaboration review of academic detailing found it is most effective when targeted at provider behaviors that are a single step (eg, prescription of a medication).15 Adherence to guidelines and improved blood pressure control involves a large number of steps by the provider and active participation on the part of the patient. The complexity of our outcome may have limited the success of our intervention.
Although our study intervention was multifaceted, it focused primarily on the health care provider. We did not actively intervene on patients, although patient education material and pill boxes were provided to practices for distribution to patients. We do not know how many patients received the educational material or if patients who did receive the material had improved blood pressure values. A previous study that tested the addition of patient education to provider education found a larger reduction in systolic blood pressure and a greater percentage of patients reaching goal blood pressure.16 It is possible that a more focused effort on patients could have resulted in different outcomes.
It is possible that our intervention was not intense enough to result in changes. Although we conducted more academic detailing visits than previous studies (4 vs 1), this may still be insufficient to affect change. It is also possible that the interval between visits (6 months) was too long. To accomplish the intervention in this study, study investigators and staff conducted 240 visits in 22 months at considerable cost and time. If this intervention were to be instituted nationwide, the cost would be substantial. Interestingly, the number of pharmaceutical representatives who conduct similar types of visits to increase drug sales doubled between 1996 and 2000 (from 41,800 to 83,000) at a cost of $48 billion in 2000 alone.17 Although not all of the pharmaceutical representatives' effort and advertising dollars were spent on promoting increased use of hypertension therapy, it is likely that a substantial portion was. In comparison, the 2003–2004 NHANES (National Health and Nutrition Examination Survey) study found that only 37% of individuals with hypertension met the guideline goals, an increase of only 8% from the 1999–2000 NHANES.1 Extrapolating between these 2 studies, a relatively small gain in hypertension control was realized despite a large effort and expenditure by the pharmaceutical industry to increase hypertension therapy sales, providing further indication of the intensity and cost needed.
Although our study had many strengths including the large number of practices, the randomized controlled study design, long intervention period, and large number of patient records examined in the outcome, there are limitations that should be mentioned. We were unable to compare the change in blood pressure control before and after the intervention among a random sample of patients in each practice. Our control group received an intervention that was identical in intensity and also focused on a cardiovascular guideline (ATPIII). Although only the initial continuing medical education session discussed both guidelines, it is possible that the similarity of focus (improvement of cardiovascular disease risk factors) of the intervention and control groups resulted in change in blood pressure control in both groups. However, we examined change in blood pressure in the smaller number of patient records that were abstracted at both baseline and follow-up for the control practices (n = 836) and found no difference between study arms (P = .81 for systolic and P = .51 for diastolic blood pressures).
Our study results, in combination with the universal lack of improvement seen in previous studies that focused on the use of academic detailing,6,7,12,18 illustrate the challenge of improving blood pressure control. Although arguments could be made that interventions tested in earlier studies of academic detailing did not have the intensity or frequency of visits needed to improve rates of blood pressure control, the results of GLAD Heart should shift the focus of future research away from expensive, labor-intensive methods to improve guideline adherence. New, innovative methods to increase blood pressure control should be rigorously tested including methods of patient activation, point of care computerized decision support, pay for performance, and simplified medication regimens through the use of “polypills” that combine standard doses of multi antihypertensive medications into a single pill. As the complexity of guidelines developed to enhance the quality of care increases, innovative techniques to enhance adherence must be developed.
Footnotes
Registered Clinical Trial No.: NCT00224848.
References
- 1.Ong KL, Cheung BM, Man YB, et al. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49:69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- 2.Thom T, Haase N, Rosamond W, et al. Heart disease and stroke statistics—2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006;113:e85–e151. doi: 10.1161/CIRCULATIONAHA.105.171600. [DOI] [PubMed] [Google Scholar]
- 3.Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 4.Thier SL, Yu-Isenberg KS, Leas BF, et al. In chronic disease, nationwide data show poor adherence by patients to medication and by physicians to guidelines. Manag Care. 2008;17:48–52. 55–57. [PubMed] [Google Scholar]
- 5.Cabana MD, Rand CS, Powe NR, et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282:1458–1465. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 6.Fretheim A, Oxman AD, Havelsrud K, et al. Rational prescribing in primary care (RaPP): a cluster randomized trial of a tailored intervention. PLoS Med. 2006;3:e134. doi: 10.1371/journal.pmed.0030134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goldstein MK, Lavori P, Coleman R, et al. Improving adherence to guidelines for hypertension drug prescribing: cluster-randomized controlled trial of general versus patient-specific recommendations. Am J Manag Care. 2005;11:677–685. [PubMed] [Google Scholar]
- 8.Grundy SM, Becker D, Clark LT, et al. The Third Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. National Heart Lung and Blood Institute. 2002 [Google Scholar]
- 9.Bertoni AG, Bonds DE, Chen H, et al. Impact of decision support intervention on cholesterol management in primary care practices: results from the Guideline Adherence for Heart Trial. Circulation. 2008;117:e414. [Google Scholar]
- 10.Ellis SD, Bertoni AG, Bonds DE, et al. Value of recruitment strategies used in a primary care practice-based trial. Contemp Clin Trials. 2007;28:258–267. doi: 10.1016/j.cct.2006.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Simon SR, Majumdar SR, Prosser LA, et al. Group versus individual academic detailing to improve the use of antihypertensive medications in primary care: a cluster-randomized controlled trial. Am J Med. 2005;118:521–528. doi: 10.1016/j.amjmed.2004.12.023. [DOI] [PubMed] [Google Scholar]
- 12.Hennessy S, Leonard CE, Yang W, et al. Effectiveness of a two-part educational intervention to improve hypertension control: a cluster-randomized trial. Pharmacotherapy. 2006;26:1342–1347. doi: 10.1592/phco.26.9.1342. [DOI] [PubMed] [Google Scholar]
- 13.Goldstein J. Feds mull funding drug pitches to counter big pharma. [Last accessed April 2, 2008];Wall St J: Dow Jones Company, Inc. 2008 Available at: http://blogs.wsj.com/health/2008/03/12/feds-mull-funding-drug-pitches-to-counter-big-pharma/?mod=WSJBlog/trackback/.
- 14.Thompson A. Beating the drug industry at its own game. [Last accessed April 23, 2008];Stateside Dispatch. New York: Progressive Network. 2007 Available at: http://www.progressivestates.org/content/573/fast-track-montana-senate-says-no-to-bad-trade-deals#3.
- 15.O'Brien MA, Rogers S, Jamtvedt G, et al. Educational outreach visits: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2007 doi: 10.1002/14651858.CD000409.pub2. CD000409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roumie CL, Elasy TA, Greevy R, et al. Improving blood pressure control through provider education, provider alerts, and patient education: a cluster randomized trial. Ann Intern Med. 2006;145:165–175. doi: 10.7326/0003-4819-145-3-200608010-00004. [DOI] [PubMed] [Google Scholar]
- 17.Clark E. ‘Tis Always the Season for Giving’; A white paper on the practice and problems of pharmaceutical detailing. Sacramento (Calif): CALPIRG. 2004 [Google Scholar]
- 18.Goldberg HI, Wagner EH, Fihn SD, et al. A randomized controlled trial of CQI teams and academic detailing: can they alter compliance with guidelines? Jt Comm J Qual Improv. 1998;24:130–142. doi: 10.1016/s1070-3241(16)30367-4. [DOI] [PubMed] [Google Scholar]