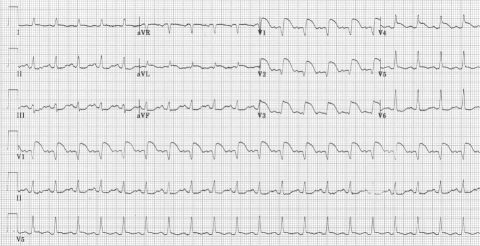
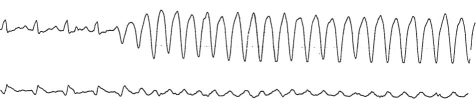
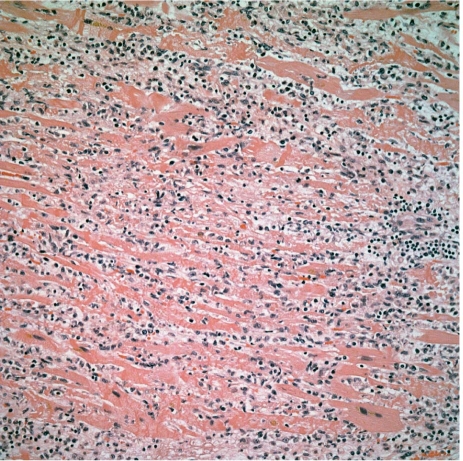
A 50-year-old woman with a history of hypertension and smoking presented at a hospital with a 4-day history of nonproductive coughing and persistent fever, and recent dyspnea, nausea, and vomiting. She reported no chest discomfort, orthopnea, or paroxysmal nocturnal dyspnea. Her heart rate was 138 beats/min; blood pressure, 103/66 mmHg; body temperature, 99.8 °F; respiratory rate, 17 breaths/min; and oxygen saturation, 98% on room air. Auscultation revealed diffuse bilateral rhonchi. Notable laboratory results were sodium, 123 mEq/L; potassium, 3.5 mEq/L; blood urea nitrogen, 27 mg/dL; and creatinine, 0.7 mg/dL. A chest radiograph showed bilateral atelectasis. The patient was admitted with diagnoses of bronchitis and hyponatremia. After 4 hours, her dyspnea worsened. Nebulizer treatment and intravenous methylprednisolone were given. Electrocardiography showed an acute injury pattern (Fig. 1). Cardiac enzyme levels included creatine kinase of 919 U/L (MB fraction, 79.7 ng/mL) and troponin T of 4.3 ng/mL. Emergent coronary angiography revealed normal coronary arteries, and echocardiography showed a left ventricular ejection fraction of 0.15. An intra-aortic balloon pump (IABP) was placed, and an overnight dopamine drip was administered. The IABP support was ended after 24 hours because the patient's condition improved. However, 12 hours later, she developed sustained ventricular tachycardia that degenerated into fatal ventricular fibrillation (Fig. 2). Histopathologic studies at autopsy showed extensive acute myocarditis (Fig. 3). An immunologic assay was positive for Coxsackie B virus antibodies type 1 at 1:320 dilution.
Fig. 1 Electrocardiogram shows ST-segment elevation in leads I, aVL, and V1 through V5, with ST-segment depression in leads II, III, and aVF.
Fig. 2 Rhythm strip shows the fatal event of monomorphic ventricular tachycardia.
Fig. 3 Histopathologic analysis shows diffuse mononuclear cell infiltrate and associated myocyte necrosis (H & E, orig. ×10).
Comment
Myocarditis is defined as inflammation of the myocardium. Fulminant myocarditis is characterized by the abrupt onset of heart failure after a recent viral illness. The precise characterization and natural history of myocarditis are still not well understood, because it progresses through distinctly different mechanisms and has varying clinical manifestations—from nonspecific constitutional symptoms to cardiogenic shock.1 Therefore, even for seasoned clinicians, diagnosis is a challenge. Potential causes include infections, autoimmune diseases, toxins, physical stress, and medications. Viral infection, especially from picornaviruses, is the most common cause in human beings.2 Myocarditis from the Coxsackie virus is only occasionally fatal in adults, and ventricular arrhythmias are uncommon at clinical presentation.2
Supportive care is the cornerstone of treatment. Hemodynamically unstable patients often require vasopressors, IABP support, or both. If these measures are ineffective, left ventricular assist device support should be considered. Immunosuppressive therapy is indicated in patients with autoimmune and giant-cell myocarditis1; however, the routine use of such therapy in patients with viral myocarditis is not recommended.
Footnotes
Address for reprints: Dennis Doan, MD, MBA, Department of Cardiology, St. John Hospital & Medical Center, 2nd flr. VEP, 22101 Moross Rd., Detroit, MI 48236
E-mail: Dennis.Doan@stjohn.org