Abstract
Understanding the impact of the acquired immune deficiency syndrome (AIDS) epidemic is critical for developing appropriate interventions to create supportive environments for orphans and vulnerable children (OVC). Unfortunately, there are very few studies on the psychosocial wellbeing of children orphaned by AIDS in Africa, and even fewer in Tanzania. It has been difficult to make generalizations across studies and to identify and track children suffering from mental health difficulties, given the lack of culturally sensitive, standardized screening scales and diagnostic procedures. As a contribution to filling that gap, the current study demonstrates the applicability of an existing depression screening instrument (CDI) to evaluate both the needs of OVC as well as the effectiveness of interventions designed to support them.
Keywords: AIDS orphans, Child Depression Inventory, cross-cultural validation, depression, OVC, Tanzania
Introduction
Today, 33.2 million people are living with human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS), and sub-Saharan Africa bears the greatest burden of the disease, with 22.5 million infected (UNAIDS, 2007). In 2007 in sub-Saharan Africa, 1.6 million people died of HIV/AIDS and 1.7 million people were newly infected (UNAIDS, 2007). Although Tanzania ranks 10th in HIV/AIDS prevalence rates among countries in sub-Saharan Africa, it ranks fourth in the number of people living with AIDS (Tanzania Commission for HIV/AIDS, 2003). The epidemic has evolved in Tanzania from being a rare and new disease to a common household problem, which has affected most Tanzanian families (Tanzania Commission for HIV/AIDS, 2003). A government analysis of HIV/AIDS in Tanzania has shown a worsening epidemiological situation whereby mother-to-child transmission appears to be on the increase, as more and more women continue to become infected and pregnant. Given international estimates that 50% of those infected are women, it is projected that 30 million children will be orphaned by AIDS by 2020 (UNICEF, 2004a).
Of the 15 million children globally left orphaned by HIV/AIDS, 12.1 million (81%) live in the sub-Saharan region (UNAIDS, 2007) and 980 000 of these live in Tanzania – roughly one child in 19 (UNICEF, 2004a). AIDS orphans have been increasing in number while families, communities and the government cannot cope with the resources needed to cater for their needs. These orphans, already coping with significant poverty, loss and hardship, are at high risk for their own mortality, poor psychosocial function, economic exploitation, violence and discrimination (UNICEF, 2004b). Their ability to survive and thrive as adults is significantly threatened. Understanding the impact of the AIDS epidemic is critical for developing appropriate interventions to strengthen the capacity of families, mobilize community responses, ensure access to essential services, create supportive environments and improve policy and legislation for orphans and vulnerable children (OVC).
Unfortunately, there are very few studies on the psychosocial wellbeing of children orphaned by AIDS in Africa, and even fewer in Tanzania. The limited work that does exist about children orphaned by AIDS in sub-Saharan Africa has occurred mainly in South Africa and suggests that the physical, psychosocial and economic wellbeing of children orphaned by HIV/AIDS is significantly compromised (Foster & Williamson, 2000). Children who lose one or both parents to AIDS are at risk of leaving or falling behind their age group in school because they have to assume their parents’ duties if parents have died or are incapacitated (Preble, 1990). Families often have to pull their children out of school to work when their financial burdens increase as a result of HIV/AIDS (UNICEF, 2004b). If both parents die, orphaned children often have to stay at home to care for their siblings and themselves.
Another major challenge for AIDS orphans is stigmatization, as their parents’ deaths from AIDS are often perceived as being related to promiscuity, prostitution or other ‘improper’ behaviors (UNICEF, 2004a). The children themselves are suspected of being HIV-positive. Stigmatization, together with economic difficulties, may compel orphans to migrate to cities, where they join the growing number of street children and often turn to jobs in the sex industry to provide for their basic needs. This places them more at risk of HIV infection and further transmission of the virus (Preble, 1990; UNICEF, 2004a). One of the few studies with children in Tanzania found that among Tanzanian children aged 10–14 years, those orphaned by AIDS expressed a higher level of suicidal ideation and other mental health problems compared to demographically matched non-orphans (UNICEF, 2004a). Until recently most research on uninfected African children affected by parental HIV has focused upon the economic, material and health care needs considered to be most critical to survival (Foster & Williamson, 2000). Psychosocial factors have been neglected or seen as secondary to other life-threatening issues, yet ignoring these issues may undermine efforts to promote the wellbeing of children affected by HIV disease because psychosocial stressors may hinder children’s ability to obtain economic, material and basic health care resources (Foster & Williamson, 2000).
It has been difficult to make generalizations across studies and to identify and track children suffering from mental health difficulties, given the lack of culturally sensitive, standardized screening scales and diagnostic procedures (Rivera, Bernal, & Rossello, 2005). Research has shown the danger of assuming metric equivalency of translated measures or that a given metric has the same meaning in different cultures (Okasaki & Sue, 1995). Scant data exist on how symptoms of depression are manifested in community samples of adolescents from diverse ethnic groups (Rivera et al., 2005). The absence of information on the validity and reliability of instruments is particularly acute in Tanzania. The validation of instruments across different cultural groups is crucial to provide evidence of the scales sensibility to cultural diversity (Abdel-Khalec & Soliman, 1999). The information provided by the screening scales is critical for the decision-making process, as it enables practitioners to differentiate people with mental disorders from those without, and to identify those disorders that may need immediate intervention. Only then will we be able to truly identify the incidence and prevalence of mental health difficulties and mental health needs and develop interventions that are appropriately sensitive.
Established as one of the most utilized self-report measures of depression, the Children’s Depression Inventory (CDI) has the potential to be a useful instrument for screening depression among children in Tanzania. The original 27-item English version of the CDI is a self-report measure of childhood and adolescent symptomology, normalized originally on a large sample of US school children (Kovacs, 2001; Kovacs, Goldstein, & Gastonis, 1993). However, the CDI has yet to be translated into the Tanzanian national language of Swahili and tested for reliability. As part of an evaluation of a children’s center for AIDS orphans, we adapted the CDI for Tanzania. The goal of this article is to describe and evaluate the adaptation process and to document the incidence of depression among a pediatric community sample of children affected by HIV.
In August 2005, a team of US and Tanzanian-based social scientists collaborated on the design and implementation of an evaluation of the Godfrey Children’s Center, a community-based residential facility built to provide a home for more than 50 orphans in Idweli, Tanzania (Lundy Foundation, 2007). Idweli is a small village situated in the wooded highlands of southwestern Tanzania. It is located about 28 km from the city of Mbeya along a highway that carries heavy truck traffic as it connects Malawi with the rest of Tanzania, and especially its port at Dar es Salaam. The rate of HIV infection in the Mbeya region, where Idweli is located, is more than twice that for Tanzania (13.5% vs. 7%) (Tanzania Commission for HIV/AIDS, 2003). This rate may be higher because of the highway to Malawi and the subsequent sex trade generated by truckers.
Aims
The first aim of the study was to compare the psychosocial and physical wellbeing of Center residents, family-placed orphans and parented children in Idweli, and evaluate the socioeconomic sustainability of the Center. The second aim was to learn how best to design and conduct an evaluation of children’s wellbeing in rural Tanzania. The study detailed in this article represents a portion of the findings from the second aim.
Methods
Sample
We recruited a convenience sample of children from the village of Idweli – a small rural village in Tanzania, where the Godfrey Children’s Center is located. This village has about 1250 inhabitants, 400 of whom are children. Nearly 300 children are orphans [for the purposes of this study, orphans were defined as children who have lost both parents or whose parent(s) have effectively abandoned them; that is, they are double orphans. The purpose of concentrating on double orphans was to consider the wellbeing of children most likely to be in the greatest need]. A total of 209 children in four sample groups participated in this study: (1) Center orphans; (2) village orphans; (3) village non-orphans; and (4) those receiving microfinance loans (Table 1).
Center orphans: of the 58 Center orphans, 51 are double-orphans five years of age or older and were included in the sample group.
Village orphans: this group of 40 includes all double-orphaned children living with caregivers in the village.
Village non-orphans: this group includes a random sample of 99 double-parented children living with both parents in the village.
Orphaned children in households receiving microfinance loans: children in households receiving either an Africa Bridge microfinance loan or a savings and credit association (SACCOS) loan were interviewed. These loans were designed to provide financial support to families who had taken in children whose parents had died or could no longer care for them. This group includes 19 children.
Table 1.
Frequency of sample group.
| Group | Frequency | % |
|---|---|---|
| Center orphans | 51 | 24.4 |
| Village orphans | 40 | 19.1 |
| Village non-orphans | 99 | 47.3 |
| Microfinance loans | 19 | 9.2 |
| Total | 209 | 100 |
Village leaders assisted fieldworkers by mapping the community, identifying every family in the village, creating a list of all children in each household and determining their orphan status. To preserve confidentiality, unique identifiers were assigned to all project participants, linking child number to parent or caregiver number. After data were collected, some children in the sample were excluded or recategorized, in order to have non-overlapping and distinct groups.
Measures
The CDI (Kovacs, 2001; Kovacs et al., 1993, pp. 8–20) was selected as the measure most appropriate to translate and validate for use in assessing depression among Tanzanian children. This measure was chosen by a US–Tanzanian collaborative process in which Tanzanian investigators and community members identified childhood depression as a critical construct. The CDI is one of the most widely used self-report measure of depression in children with normative data available from psychiatric, pediatric and school-based populations, and is a 27-item self-rating scale designed to assess cognitive, affective and behavioral symptoms of depression in children and adolescents. Each item is scored on a three-point scale (0 absent; 1 moderate; 2 severe) according to symptom severity. The total possible scores on the CDI range from 0 to 54. A cutoff point of 12 has been established as the ideal threshold discriminating children at risk of depression from non-depressed children within homogeneous samples (Kovacs, 2001; Kovacs et al., 1993). Studies have shown that internal consistency for the CDI ranges from 0.80 to 0.88 among domestic and international samples (Rivera et al., 2005). In addition to a total score, the CDI also produces subscale scores to identify negative mood, interpersonal problems, ineffectiveness, anhedonia and negative self-esteem. Studies have shown that the internal consistency for the subscales ranges from 0.59 to 0.68 (Kovacs et al., 1993).
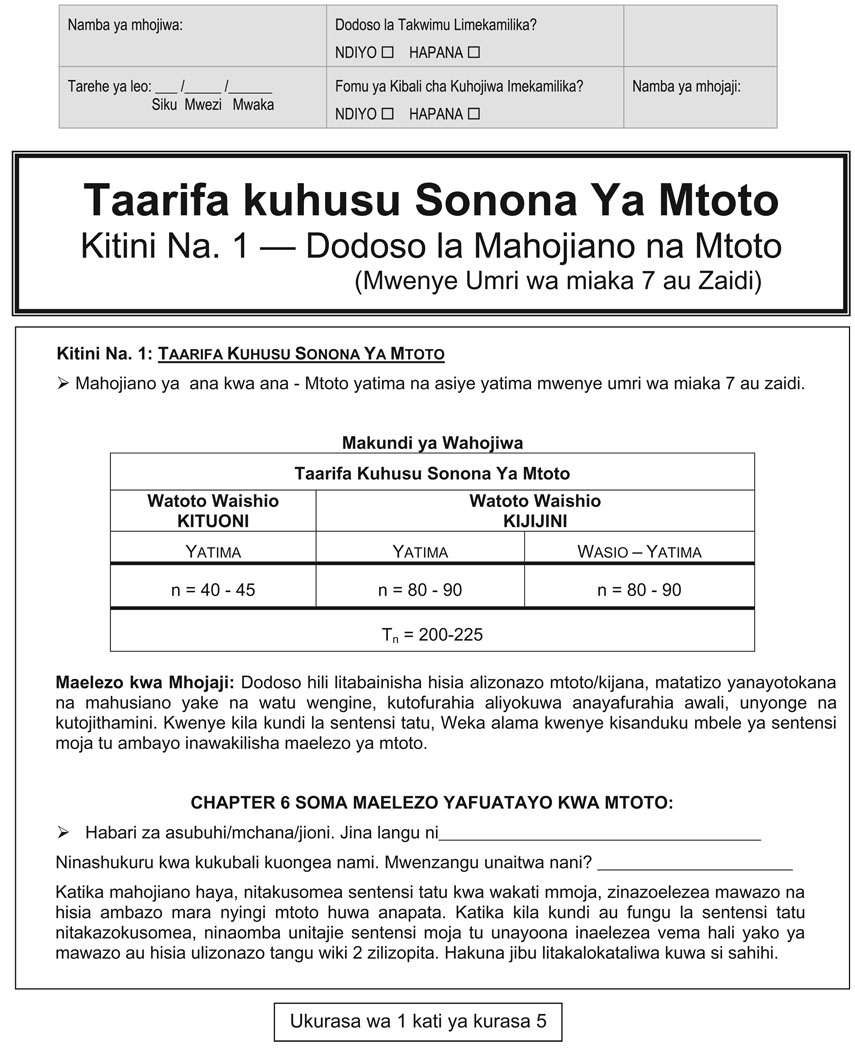
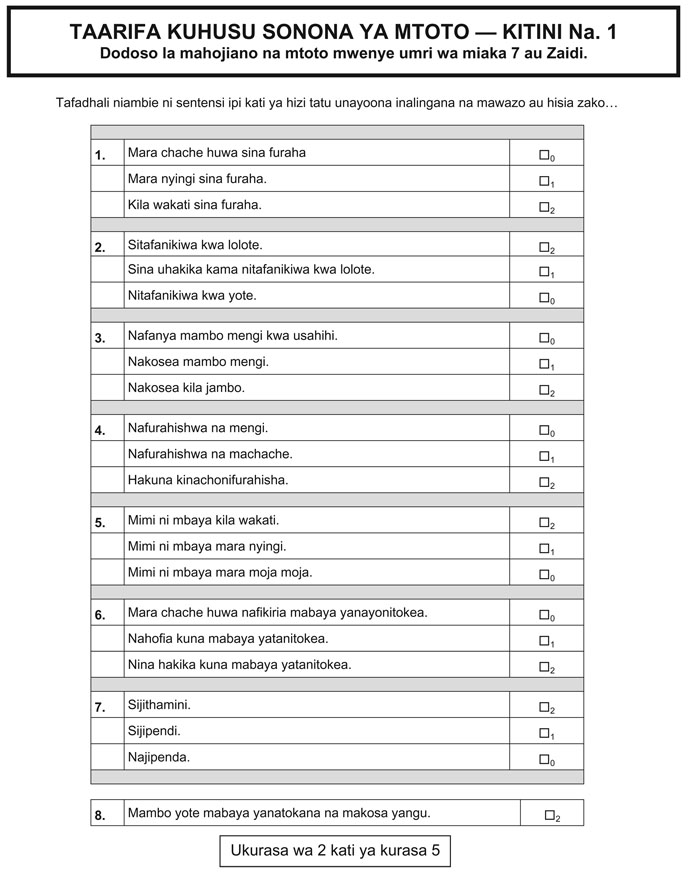
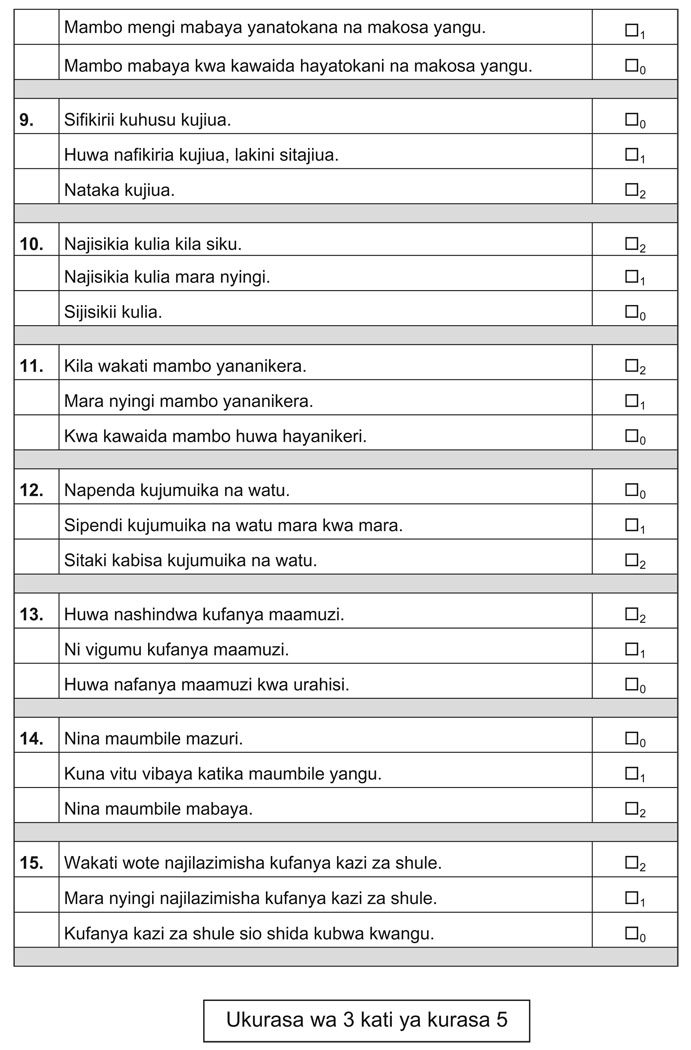
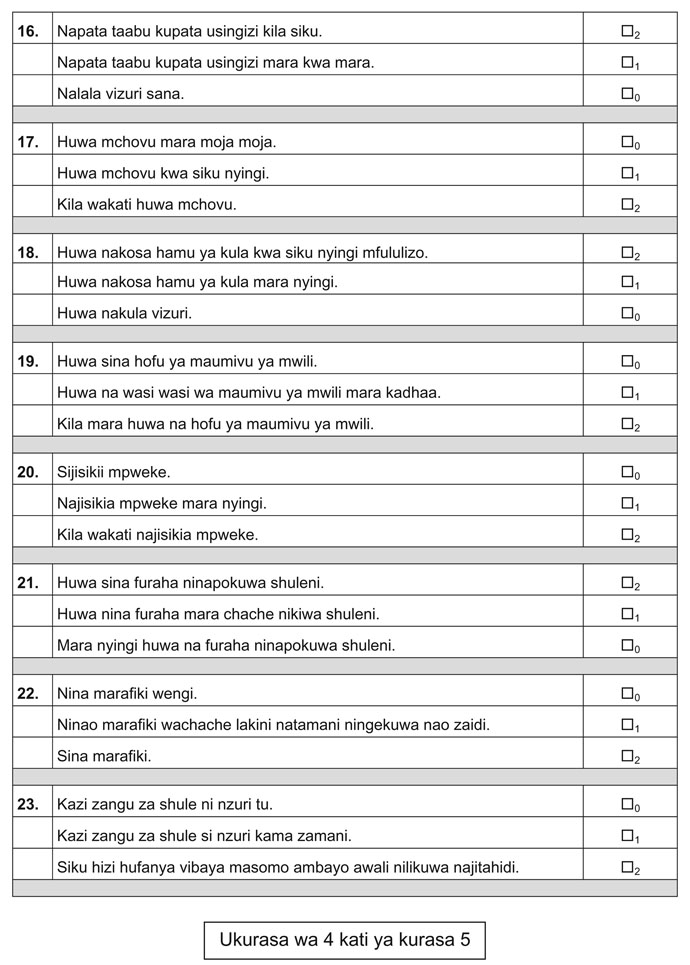
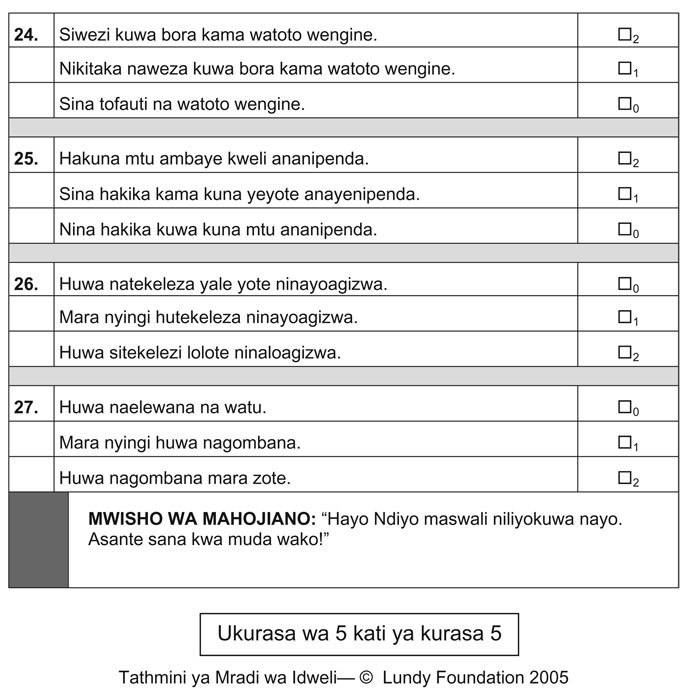
The CDI was translated into Swahili by a local Tanzanian work-group. The instrument was back-translated and field-tested to ensure proper readability. Cultural validity was a key concern in translating and evaluating this instrument. To understand and interpret accurately the nuances of the translation required an understanding of the cultures of Tanzania and, more specifically, of Idweli. To achieve accuracy of cultural understanding and translational accuracy, the project was designed to include a close collaboration between US and Tanzanian researchers, as well as Idweli community members, in the entire adaptation process and analysis of survey findings. See Figure 1 for a copy of the CDI in Swahili.
Figure 1.
Swahili translation of CDI.
There was relative ease in translating conceptual meanings of the English version of the CDI to Swahili, and the translation of most items was straightforward. Tanzanian fieldworkers asked for further discussion on three items. For ‘sadness’, the Swahili version used ‘feeling unhappy’ as the most relevant conceptual meaning to gain understanding from the perspective of children. Furthermore, for the eighth item on the CDI, inquiring into children ‘perceiving bad things as being their fault’, the phrasing in the Swahili version that had most resonance for children was ‘perceiving bad things as being due to the child’s own mistakes’. Finally, for item 13, ‘difficulties making up ones’ mind about things’ were framed as ‘difficulties in making decisions about things’.
Procedure
In December 2005, three senior team members conducted a six day training workshop for 10 local Tanzanians who were being considered for positions as fieldworkers. Possible fieldwork applicants were chosen from the village population and were considered for the position of which they were not part of the study, were able to attend fieldworker training and could demonstrate an employment history or skill set that would allow them to interview children and their families. The curriculum included mini-lectures, discussion and role-play in quantitative/qualitative data collection techniques (e.g. interviewing skills, focus group facilitation, working with both adults and children), plus a review and discussion of all survey tools and administrative procedures. Data collection occurred during the first half of 2006 by the project coordinator and fieldworkers. Once all survey instruments were ready for use (January 2006), a Tanzanian project coordinator was hired to supervise data collection in Idweli. Six fieldworkers of the 10 trained were also hired. Input from fieldworkers was used to further refine the instruments. Once in the field there was an additional day-and-a-half of training conducted by a psychiatrist from the hospital in Mbeya, who also participated in the evaluation design regarding which fieldworkers should use if they observed trauma in a child during an interview. In case a child became traumatized by recalling facts of orphanhood, a safety net protocol was developed to identify signs of trauma, then contacting a parent or caregiver for assistance and then, if they could not deal with the situation, sending the child to the hospital in Mbeya.
From January to May 2006, the project coordinator and fieldworkers conducted all data collection. Every adult participant in the project completed an informed consent process where the purpose of the study was explained as well as any possible risks and benefits. Informed consent forms were signed by a parent or caregiver for each child. Interviews were conducted in Swahili in meeting rooms within the Godfrey Children’s Center in the village. Interviewers met with children privately while their parent or caregiver waited at the premises of the Center. Fieldworkers opened each interview with a statement describing the purpose of the study. Additionally, each participant was told that information shared by individuals would remain confidential and, if the participant felt uncomfortable at any time, that the session could be ended. Local Tanzanians were hired to transcribe, edit and translate (from Swahili to English) interviews. In order to ensure that minimal errors were made in quantitative data entry, a research assistant double-checked a random sample of 60% of all interviews. Data entry was nearly perfect, with only three errors in more than 700 items.
Quantitative analysis
Statistical analysis proceeded in several stages. First, univariate analysis was conducted in order to describe the sample characteristics and assess any issues related to skewed distribution or kurtosis. Next, Cronbach’s alpha coefficients, Spearman–Brown correlation coefficients, and Guttman split-half coefficients were estimated as an indicator of internal consistency reliability and split-half reliability. The cut-point (≥12) recommended by Kovacs was used to define ‘suprathreshold’ depressive symptomatology. Cronbach’s alpha coefficients were estimated as an indicator of internal consistency reliability. Split-half reliability was calculated by estimating the Spearman–Brown split-half coefficient and Guttman split-half coefficient between the sums of the odd and even items of each of the scale versions. Finally, correlation analyses between subscales within the CDI were calculated to ensure that items were related appropriately across domains.
Results
Univariate analysis
As stated previously, the study sample consisted of 209 children, including 51 center orphans, 40 village orphans, 99 village non-orphans and 19 microfinance loan recipients. See Table 2 for a list of demographic features. These features include the following: of the center orphans, 41.2% were male, 56.9% were female and they ranged in age from 5 to 15 years, with an average age of 10 years. Among village orphans, 47.5% were male, 52.5% were female and they ranged in age from 3 to 17 years, with an average age of 12 years. Forty-seven per cent of village non-orphans were male, 52.6% were female and they ranged in age from 4 to 19 years, with an average age of 9 years. Finally, 52.6% of microfinance loan recipients were male, 36.8% were female and they ranged in age from 6 to 17 years, with an average age of 11 years. Two children did not complete data about their gender. Among all four groups, distribution of age and gender were relatively similar, with the average participant being a pre-teen and each group having an approximately equal proportion of males to females. The groups were distinct in terms of overall numbers within each group. Because this was a convenience sample, the sample size within each group is similar to the prevalence within the total population. Therefore, there were disproportionately more village orphans than center orphans, village non-orphans or orphaned children in households receiving microfinance loans.
Table 2.
Demographics by sample group.
| Variable | Center orphan (n=51) (%) |
Village orphan (n=40) (%) |
Village non-orphan (n=99) (%) |
Microfinance loan (n=19)* (%) |
|---|---|---|---|---|
| Male | 41.2 | 47.5 | 47.4 | 52.6 |
| Female | 56.9 | 52.5 | 52.6 | 36.8 |
| Attend school | 90.2 | 75.0 | 83.5 | 84.2 |
| Female caregiver | 11.5 | 90.0 | 41.4 | 36.8 |
| Male caregiver | 88.5 | 10.0 | 8.6 | 5.3 |
| Mean (SD); range | Mean (SD); range | Mean (SD); range | Mean (SD); range | |
| Age | 10.40 (3.37); 5–15 | 11.97 (3.18); 3–17 | 9.25 (3.67); 4–19 | 11.44 (3.12); 6–17 |
Note: SD: standard deviation.
Missing data n=2; 10.6%.
Estimates of reliability
The alpha estimate for the CDI was 0.669. While this is lower than the average estimate of reliability found by the instrument’s author (0.80–0.89), it still falls within the range of acceptability when employing a community-based sample (Chatterji, 2003). Internal consistency reliability estimates for the five subscales of the CDI range from 0.109 to 0.575, compared to those for the original English CDI (ranging from 0.59 to 0.68) (Kovacs, 2001; Kovacs et al., 1993). The subscales tended to be less reliable indicators, with the feelings of ineffectiveness being the least reliable. As expected, the subscales with fewer items (interpersonal problems and ineffectiveness) tended to be less reliable. These findings are consistent with findings from translation studies employing community-based samples (see Davanzo et al., 2004 for further information). A summary of the Cronbach alpha coefficients for the total CDI and subscales is provided in Table 3.
Table 3.
Cronbach’s alpha coefficients.
| Scale | Cronbach’s alpha |
|---|---|
| CDI total | 0.669 |
| Subscale 1: negative mood (6 items) | 0.314 |
| Subscale 2: interpersonal problems (4 items) | 0.236 |
| Subscale 3: ineffectiveness (4 items) | 0.109 |
| Subscale 4: anhedonia (8 items) | 0.575 |
| Subscale 5: negative self-esteem (5 items) | 0.340 |
Note: CDI: Children’s Depression Inventory.
The Spearman–Brown split-half reliability coefficient was used as a form of split-halves reliability measure. As an additional check, Guttman split-half reliability coefficients were calculated. Table 4 indicates that both the Spearman–Brown and Guttman split-half testing produced comparable results: 0.661 and 0.643, respectively. These findings of reliability for a randomly selected portion of half of the measure are consistent with the findings for the Cronbach’s alpha analysis, indicating acceptable reliability within the items of the Swahili translation of the CDI.
Table 4.
Split-half reliability statistics.
| Test | Value |
|---|---|
| Spearman–Brown coefficient | 0.661 |
| Guttman split-half coefficient | 0.643 |
Finally, Table 5 illustrates the correlation coefficients between the subscales of the CDI and the total CDI. All correlations were statistically significant (p>0.00) and fell within and moderate level of correlation with the total scale. Anhedonia had the highest correlation with the total scale with a correlation coefficient of 0.799, followed by negative mood at 0.762, ineffectiveness at 0.582, negative self-esteem at 0.573 and finally interpersonal problems at 0.383. While the correlation coefficient for interpersonal problems is low this is to be expected, given its poor performance during reliability testing.
Table 5.
Correlation between subscale and CDI total.
| Subscale | R=CDI total | p |
|---|---|---|
| Subscale 1: negative mood | 0.762 | 0000 |
| Subscale 2: interpersonal problems | 0.383 | 0.000 |
| Subscale 3: ineffectiveness | 0.582 | 0.000 |
| Subscale 4: anhedonia | 0799 | 0.000 |
| Subscale 5: negative self-esteem | 0.573 | 0.000 |
Note: CDI: Children’s Depression Inventory.
Group comparisons
Based on the reliability criteria detailed above, the investigators completed further analysis to determine the frequency of children meeting the CDI clinical cutoff for significant depression symptoms (Rivera et al., 2005). The percentage of children with a score greater than 12 was calculated for the following groups: gender, center orphans, village orphans, village non-orphans and microfinance loan. Children in the village orphan group had the highest percentage of children meeting the criteria for depression (47.1%), followed by village non-orphans (30%), microfinance loan (26.7%) and center orphans (14.3%). Thirty per cent of males and females met the clinical cutoff, with no gender group differences. This finding is contrary to domestic findings, where young women generally have higher rates of depression (Burwell & Shirk, 2007; Cicchetti & Toth, 1998; Nolen-Hoesksema, 1991; Strunk, Lopez, & DeRubeis, 2006) (Table 6).
Table 6.
Number and percentage of children scoring ≥ 12 on CDI scale by gender and group.
| Variable | n | % |
|---|---|---|
| Gender: male | 21 | 30.0 |
| Gender: female | 24 | 30.0 |
| Group: center orphans | 5 | 14.3 |
| Group: village orphans | 16 | 47.1 |
| Group: village non-orphans | 20 | 30.00 |
| Group: microfinance loan | 4 | 26.7 |
Note: CDI: Children’s Depression Inventory.
Discussion
In sub-Saharan Africa it has been difficult to identify and track children suffering from mental health difficulties, given the lack of culturally sensitive, standardized screening scales and diagnostic procedures (Rivera et al., 2005). Such measures are already being used effectively in other countries and can also be applied to a vulnerable population in sub-Saharan Africa. The general psychometric properties of the Swahili translation of the 27-item version of the CDI appear to be adequate, according to a Cronbach’s alpha coefficient estimate of internal reliability and Spearman–Brown and Guttman split-half reliability coefficients. Considerable uniformity was found in the correlation between subscales and the total score on the CDI. This reliability is concordant with that reported for the English version of the CDI when administered to community-based samples (Kovacs et al., 1993). However, the Cronbach’s alpha coefficient estimate of internal reliability for the subscales was less than that established on American samples, and should be used with caution.
Having determined that the psychometric properties of the Swahili version of the CDI were reliable, we compared the depression scores for the children in each sample group. The level of depression for the Center orphans was about half that of the village orphans. Interpretation of this finding is limited by the fact that these are cross-sectional data. In order to determine whether residence in the Center is responsible for lower depression levels among those children, it would be necessary to have data from before the children entered the Center. These data could not be gathered because the evaluation began after children had been living at the Center for six months. Similarly, in claiming a causal connection it would be necessary to follow these children over time. Nevertheless, the results are in the direction hypothesized by the investigators, namely that Center children are less depressed. Additionally, interviews with the members of the Center’s governing board and its manager contained clear claims that the children selected to live in the Center were the most ‘needy’ children of the village – those who were living in the worst circumstances and potentially most prone to depression. Rather than intensifying the psychologically debilitating effects of losing one’s parents to AIDS, living in the Center appears to be associated with a lower rate of depression compared to orphans living in the village. In addition, researchers did not have the opportunity to incorporate medical data that might indicate biological and physiological determinants of mental health difficulties. Finally, the fourth sample group, microfinance loan recipients, was comprised of children from various economic backgrounds with vastly different family compositions, making it difficult to draw reliable conclusions about the sample.
There is a need to understand the circumstances in which children affected by HIV/AIDS are vulnerable to HIV infection so that targeted interventions can be established. Although considerable literature exists on the vulnerability of children to HIV/AIDS and other sexually transmitted infections, there is a striking lack of research on the prevalence and circumstances surrounding vulnerability of orphans, particularly studies that allow cross-cultural comparisons (Foster & Williamson, 2000). The psychological impacts of HIV/AIDS on orphans increase their vulnerability to HIV infection. A cause for concern is that, in spite of the considerable amount of activity being carried out to support children affected by HIV/AIDS, there is a lack of data and limited study of many key issues related to identification of and interventions related to mental health difficulties. As a contribution towards filling that gap, the current study demonstrates the applicability of an existing depression screening instrument (CDI) to evaluate both the needs of OVC as well as the effectiveness of interventions designed to support them. There is an ongoing need to validate psychosocial measures for future use in Tanzania and elsewhere in sub-Saharan Africa.
Footnotes
Publisher's Disclaimer: Full terms and conditions of use: http://www.informaworld.com/terms-and-conditions-of-access.pdf
This article may be used for research, teaching and private study purposes. Any substantial or systematic reproduction, re-distribution, re-selling, loan or sub-licensing, systematic supply or distribution in any form to anyone is expressly forbidden.
The publisher does not give any warranty express or implied or make any representation that the contents will be complete or accurate or up to date. The accuracy of any instructions, formulae and drug doses should be independently verified with primary sources.
References
- Abdel-Khalec AM, Soliman HH. A cross cultural evaluation of depression in children in Egypt, Kuwait, and the United States. Psychological Reports. 1999;85:973–980. doi: 10.2466/pr0.1999.85.3.973. [DOI] [PubMed] [Google Scholar]
- Burwell RA, Shirk SR. Subtypes of rumination in adolescence: Associations between brooding, reflection, depressive symptoms, and coping. Journal of Clinical Child and Adolescent Psychology. 2007;36:56–65. doi: 10.1080/15374410709336568. [DOI] [PubMed] [Google Scholar]
- Chatterji M. Designing and using tools for educational assessment. New York: Allyn and Bacon; 2003. [Google Scholar]
- Cicchetti D, Toth SL. The development of depression in children and adolescents. American Psychologist. 1998;52:221–241. doi: 10.1037//0003-066x.53.2.221. [DOI] [PubMed] [Google Scholar]
- Davanzo P, Kerwin L, Nikore V, Esparaza C, Forness S, Murrelle L. Spanish translation and reliability testing of the child depression inventory. Child Psychiatry and Human Development. 2004;35:75–92. doi: 10.1023/b:chud.0000039321.56041.cd. [DOI] [PubMed] [Google Scholar]
- Foster G, Williamson J. A review of current literature of the impact of HIV/AIDS on children in sub-Saharan Africa. AIDS. 2000;14 Suppl. 3:S275–S284. [PubMed] [Google Scholar]
- Joint United Nations Joint Programme on HIV/AIDS (UNAIDS) Geneva, Switzerland: UNAIDS and World Health Organization (WHO); 2007 AIDS epidemic update. 2007
- Kovacs MD. Children’s depression inventory (CDI): Technical manual. North Tonawanda, NY: Multi Health Systems Inc.; 2001. [Google Scholar]
- Kovacs M, Goldstein D, Gastonis C. Suicidal behaviors and childhood-onset depressive disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32:8–20. doi: 10.1097/00004583-199301000-00003. [DOI] [PubMed] [Google Scholar]
- Lundy Foundation. Evaluation of a community-based response to the needs of orphans and vulnerable children. Denver, CO: Lundy Foundation; 2007. [Google Scholar]
- Nolen-Hoesksema S. Responses to depression and their duration of depressive episodes. Journal of Abnormal Psychology. 1991;100:569–582. doi: 10.1037//0021-843x.100.4.569. [DOI] [PubMed] [Google Scholar]
- Okasaki S, Sue S. Methodological issues in assessment research with ethnic minorities. Psychological Assessment. 1995;7:367–375. [Google Scholar]
- Preble EA. Impact of HIV/AIDS on African children. Social Science & Medicine. 1990;31:671–680. doi: 10.1016/0277-9536(90)90249-r. [DOI] [PubMed] [Google Scholar]
- Rivera CL, Bernal G, Rossello J. The Children Depression Inventory (CDI) and the Beck Depression Inventory (BDI): Their validity as screening measures for major depression in a group of Puerto Rican adolescents. International Journal of Clinical and Health Psychology. 2005;5:485–498. [Google Scholar]
- Strunk DR, Lopez H, DeRubeis RJ. Depressive symptoms are associated with unrealistic negative predictions of future life events. Behaviour Research and Therapy. 2006;44:861–882. doi: 10.1016/j.brat.2005.07.001. [DOI] [PubMed] [Google Scholar]
- Tanzania Commission for HIV/AIDS. Dar Es Salaam: Prime Minister’s Office; National Multi-Sectorial Strategic Framework on HIV/AIDS 2003–2007. 2003
- United Nations Children’s Fund (UNICEF) New York: USAID Population Health and Nutrition Program; Children on the brink 2004: A joint report of new orphan estimates and a framework for action. 2004a
- United Nations Children’s Fund (UNICEF) New York: USAID Population Health and Nutrition Program; Psychosocial needs of children affected by AIDS in low resource countries. RFA-MH-05-008. 2004b