Abstract
Emotional trauma occurs in many patients with chronic pain, particularly fibromyalgia syndrome (FMS). Current cognitive-behavioral treatments for chronic pain have limited effects, perhaps because the trauma is not addressed, whereas emotional exposure-based treatments improve post-traumatic stress, but have not been tested on chronic pain. We present a novel, brief treatment protocol for people with chronic pain and unresolved trauma (Multi-Stimulus, Multi-Technique Emotional Exposure Therapy), which involves detecting avoidance of a range of emotion-related stimuli, implementing exposure techniques tailored to the patient’s avoidances, and negotiating the process and therapeutic alliance. This treatment was pilot tested on 10 women with intractable FMS and trauma histories. Three months post-treatment, the sample showed moderate to large effects on stress symptoms, FMS impact, and emotional distress; and small to moderate improvements on pain and disability. Two patients showed substantial improvement, four made moderate gains, two showed modest improvement, and two did not benefit. This pilot study suggests that emotional exposure treatment for unresolved trauma may benefit some patients with FMS. Controlled testing of the treatment for FMS and other chronic pain populations is indicated.
Chronic pain is a common source of disability and distress, and fibromyalgia syndrome (FMS) is particularly problematic. This condition, which afflicts about 4% of U.S. adults, primarily women, is marked by widespread muscular pain, multiple tender points, and often by fatigue, sleep problems, disability, and mood disturbance. Controversy surrounds FMS because of the lack of tissue pathology in the face of often incapacitating symptoms, the elevated levels of psychological distress found in many patients, and the limited effectiveness of medical and psychological interventions. Both patients and providers are often quite frustrated.
Many patients with FMS have had serious psychological trauma or conflict. Childhood or adult victimization is common, even before FMS onset and even when compared to other pain conditions. Over half of FMS patients have post-traumatic stress disorder (PTSD) or subclinical PTSD (Cohen et al., 2002), and patients with FMS respond to interpersonal conflict with increased pain (Davis, Zautra, & Reich, 2001). Trauma likely creates difficulties in emotion regulation, such as emotional suppression and avoidance, as well as in relationships, such as balancing trust and autonomy. These emotional and interpersonal problems likely contribute to FMS onset or severity in many patients, and may be key reasons that treatments often fail.
How should one deal with the trauma and its affective and relational consequences found in many patients with FMS? Standard cognitive-behavioral approaches to pain management (e.g., relaxation, distraction, cognitive reappraisal, problem solving), usually bypass the trauma and avoid or minimize negative emotions to reduce the affective arousal that contributes to pain. Yet, theoretical advances and empirical research on emotion regulation, emotional processing, experiential avoidance, and emotional approach coping suggest an alternative view—avoiding negative emotions is often problematic. Exposure and emotional processing treatments for PTSD and other anxiety disorders demonstrate the adaptive nature of accessing, experiencing, and expressing such emotions (Foa & Kozak, 1986), which informs action tendencies, allows the assimilation of cognitions and emotions, and facilitates stress resolution. Interestingly, the pain management literature, which typically advocates emotional avoidance techniques, has developed independently of the exposure-based literature. One exception that demonstrates the value of emotional expression and processing for pain is written emotional disclosure about traumatic experiences, which we view as a low-intensity, self-directed version of exposure therapy. This technique has shown small positive effects for a number of problems, including FMS (Gillis, Lumley, Mosley-Williams, Leisen, & Roehrs, 2006).
We believe that a key limitation of available psychological treatments for FMS and many other chronic pain conditions is the failure to directly address trauma and subsequent emotional and relational difficulties found in a substantial subset of patients. To redress this, we have developed an intervention that integrates a range of theories and techniques. Our approach is strongly influenced by emotional processing theory for anxiety disorders, and it incorporates written emotional disclosure as well as the distinction between primary and secondary emotions. Also important to our model is the unifying framework of “affect phobia” (McCullough et al., 2003), which translates psychodynamic formulations into the parsimonious perspective that emotional experience is fundamentally what is avoided, and encourages creative, “dosed” (hierarchically presented) experiential exercises to engage avoided affects. We further incorporate the view that the therapeutic relationship can be a powerful corrective emotional experience when patients try new relational behaviors that they typically avoid, particularly meta-communication. We pilot tested this intervention in a sample of patients with FMS who also had unresolved stress to determine the intervention’s feasibility and its efficacy with respect to psychological outcomes, pain, and disability.
Method
Participants and Procedures
Participants were recruited through advertisements seeking people with a diagnosis of FMS and interested in “treatment of stress.” Respondents were interviewed to verify that they had unresolved trauma or conflict that could be targeted in treatment—defined as experiences that fit Criterion A for the diagnosis of PTSD, or experiences that were stressful because they created substantial fear, humiliation, secrecy, and so on. Patients also had to report re-experiencing, avoidance of stimuli, and hyperarousal. Patients meeting criteria then were told about the treatment’s rationale, techniques, and goals, including that it sought to resolve stress and potentially improve pain by encouraging the patient to confront those experiences that they usually avoid—feelings, relationships, actions, etc. Of 14 people (all women) who contacted us, one did not have a stressor, and three did but declined to participate after learning about the treatment. The 10 women participants were 46 to 77 years old (M = 56), had FMS for a mean of 16.1 years (range, 7 to 26 years), and included eight Caucasians and two African Americans. Six were married (two divorced, two never married), 8 had some college education (although only four had a bachelor’s degree), and all but one had prior psychotherapy experience.
The therapists were clinical psychologists: one experienced senior level male (3 patients), two post-doctoral fellows (female and male; 3 patients and 1 patient, respectively), and one advanced trainee in her fifth year of doctoral studies (3 patients). Training was conducted by the senior psychologist, using didactics, role-playing, and extensive review of videotapes of prior treatments. Treatment was guided by a manual developed by the authors that provided detailed activities for the initial and final session, but general principles for the majority of sessions. Supervision occurred weekly and included a review of each videotaped session. Patients completed stress and health measures at pre-treatment and at follow-up evaluation scheduled 7 months later, which averaged 3 months after the end of treatment.
Description of the Intervention
The time-limited, individual protocol calls for 10 treatment sessions, scheduled once weekly for 60 minutes. Treatment attempts to create a specific focus, and at screening, we provide an explicit rationale and treatment model and clarify goals and tasks so that less time is spent negotiating those issues for patients who accept treatment. The intervention seeks to identify patients’ avoided experiences or stimuli, and then engage the patients in various exposure exercises to these stimuli so that emotional processing occurs, relearning takes place, trauma is resolved, and physical symptoms improve. The traumas usually involve significant others, extend back to childhood, and often recur in various forms over the years (e.g., loss, violence, abuse, rejection, secrecy, manipulation, etc.). We propose that there is continuity across stressors and generalization of avoided emotions; that is, for a given patient, there is some commonality among the affects that are avoided and the cognitions that support these affects. Patients usually avoid many stimuli that evoke similar affective experiences, including certain memories, interpersonal behaviors, words, actions, locations, and objects. Thus, it is not necessary to target only the single, most formative or influential trauma; rather, one can target various stimuli, which will elicit the avoided affect and lead to learning. To do this, treatment incorporates a range of exposure-based techniques that create new experiences. Importantly, this intervention is guided by a set of principles rather than specific session requirements, to allow tailoring to each patient’s unique configuration of avoided experiences as well as patient openness to various exposure techniques.
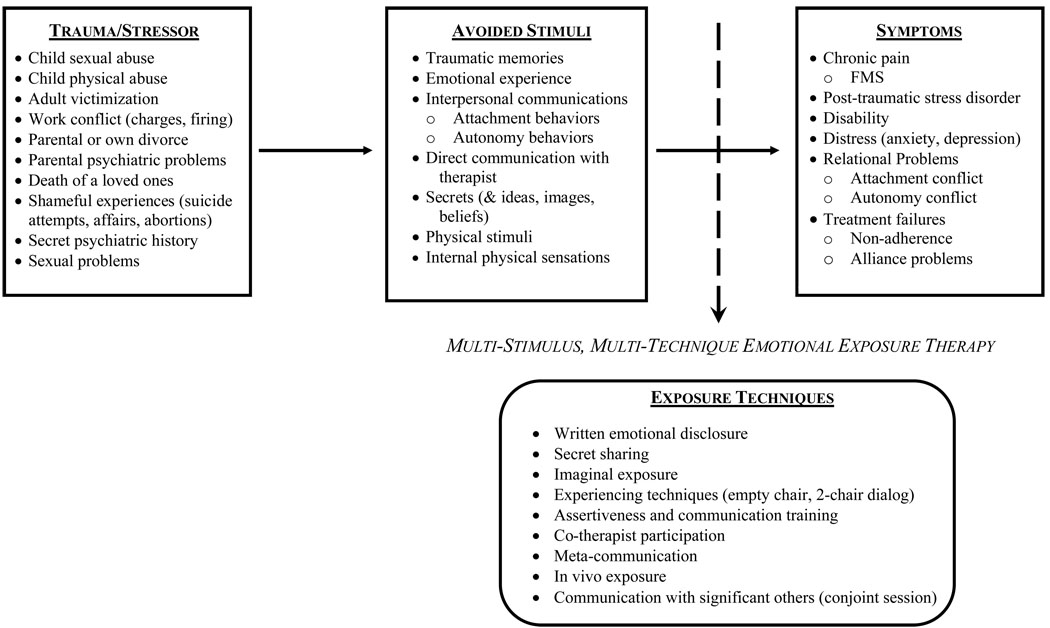
Figure 1 presents the key aspects of the treatment—Multi-stimulus, Multi-technique Emotional Exposure Therapy—including the trauma and various avoided stimuli (the examples were taken from the current sample), the health consequences of this avoidance, and the specific exposure techniques that we employ to reverse the avoidance and create corrective emotional experiences. The treatment has three major components that we conceptualize as detecting avoidance, implementing exposure, and negotiating process.
Figure 1.
Working model of the impact of trauma and avoidance on chronic pain and the corrective action of this therapy
Detecting avoidance
The primary task in the first few sessions is to identify avoided experiences, including traumatic memories, certain emotions and their expression, interpersonal actions, ideas or images, locations, physical stimuli, and physical sensations (including pain). The therapist directly inquires about avoided stimuli and is an “avoidance detective,” actively searching for signs of avoidance, including the patient’s behavior with the therapist. This is done in a spirit of joint exploration and curiosity rather than certainty, and stimuli that evoke anxiety are targeted for exposure.
Implementing exposure
We use different exposure strategies to help patients confront rather than avoid stimuli. Exposure techniques have many forms, but the overarching process is reversing avoidance, which can result in emotional processing and opportunities for cognitive and behavioral change. Listed from generally less to more intense, these are written emotional disclosure, secret sharing, imaginal exposure, experiential techniques (empty chair work and two-chair dialog), assertiveness training (including modeling, role-playing, and co-therapist participation), meta-communication with the therapist, in vivo exposure, and communication with significant others in session. Each week, homework exercises are developed, which typically encourage further exposure and new experiences in daily life.
Negotiating process
There is a substantial focus on the relationship between therapist and patient, both as a method to maintain or repair the alliance as well as a vehicle for experimenting with avoided interpersonal behaviors. The therapist needs to monitor the alliance quality, which often is strained as the therapist encourages the patient to confront threatening experiences. The relationship between therapist and patient needs to be discussed openly. To facilitate this, meta-communication is introduced and practiced in the first session and revisited in every session, typically by negotiating the process—what stimuli are avoided, what exposure techniques to use, how intense to make them, whether change is occurring, and how the patient is feeling about the therapist. Meta-communication also is an interpersonal affect regulation strategy that is often very novel for patients—directly sharing their wishes and frustrations to—and about—an authority (the therapist).
Measures
The Impact of Event Scale-Revised (IES-R; Weiss & Marmar, 1997) assesses three manifestations of unresolved stress: avoidance, intrusions, and hyperarousal. The Fibromyalgia Impact Questionnaire-Revised (FIQ; Bennett, 2005) assesses the impact of FMS symptoms over the previous week. The Arthritis Impact Measurement Scales–2 (AIMS-2; Meenan, Mason, Anderson, Guccione, & Kazis, 1992) assesses limitations in the performance of various behaviors of daily activity during the past month. The McGill Pain Questionnaire (Melzack, 1975) presents sets of pain adjectives, and the values of the highest selected adjective in each set were summed to yield the Pain Rating Index (PRI). The Brief Symptom Inventory (BSI; Derogatis & Melisaratos, 1983) assesses a range of psychological symptoms and provides an overall Global Severity Index (GSI). Finally, the Satisfaction with Life Scale (SWLS; Diener, Emmons, Larsen, & Griffin, 1985) measures one’s perception of general life satisfaction.
Results
All 10 patients remained in treatment until termination; six patients completed 10 sessions, one finished in eight, two had 13 sessions, and one had 15 sessions. Table 1 presents sample data for each measure at pretreatment and follow-up, as well as change scores (follow-up minus pre-treatment), the t-value (and p-value) from a paired-sample t-test, and effect size (ES) of the change (mean change score divided by sample pretreatment SD). Improvement is indicated by decreases for all measures except life satisfaction. Our primary goal was to estimate the effect size of this treatment on this sample, but we also tested the statistical significance of the change. With respect to the unresolved stress symptoms, the sample experienced a moderate to large effect reduction (ES = 0.70), which was also significant. The measure of global FMS status showed a similar, large effect (ES = 0.74), which was marginally significant. With respect to specific domains of health and functioning, measures of emotional distress and life satisfaction also had moderate to large effect sizes (ES = 0.79 and 0.77 that were marginally or fully significant), whereas disability and pain had small to moderate effects (ES = 0.42 and 0.36); disability was marginally significant.
Table 1.
Pretreatment and Follow-up Data (M, SD) and Analyses of Change for 10 Patients with FMS
| Outcome measure |
Pretreatment | Follow-up (3-month) |
Change score |
t | p | Effect size (d) |
|---|---|---|---|---|---|---|
| IES-R | 2.44 | 1.93 | −0.51 | −2.81 | .02 | 0.70 |
| (0.72) | (0.45) | |||||
| FIQ | 57.10 | 45.70 | −1.14 | −1.86 | .10 | 0.74 |
| (15.30) | (21.00) | |||||
| AIMS-2 | 2.03 | 1.74 | −0.29 | −1.95 | .08 | 0.42 |
| Physical | (0.69) | (0.75) | ||||
| McGill-PRI | 25.50 | 21.90 | −3.60 | −1.60 | .15 | 0.36 |
| (9.98) | (11.28) | |||||
| BSI-GSI | 1.16 | 0.72 | −0.44 | −2.76 | .02 | 0.79 |
| (0.56) | (0.38) | |||||
| SWLS | 14.59 | 17.80 | 3.21 | 1.93 | .09 | 0.77 |
| (4.15) | (6.89) |
Note. IES-R = Impact of Events Scale-Revised; FIQ = Fibromyalgia Impact Questionnaire; AIMS-2 Physical = Arthritis Impact Measurement Scales-2, Physical functioning subscale; McGill-PRI = McGill Pain Questionnaire Pain Rating Index; BSI-GSI = Brief Symptom Inventory Global Severity Index; SWLS = Satisfaction with Life Scale.
t- and p-values from paired t-tests comparing pretreatment and follow-up scores.
Effect size calculated as change score divided by sample pretreatment SD.
We also examined individual patient outcomes using the reliable change index (RCI), which indicates how much change occurred while accounting for measurement error across time. It is a ratio of the individual patient’s change score (follow-up minus pretreatment) to the sample’s standard error of the difference between the scores. For the RCI, we used two cut-offs: the conventional 1.96 (p < .05), which represents a large effect but is very conservative, and an RCI of at least 0.50, which represents a moderate effect. On the IES-R, three patients showed large effects (RCI > 1.96), and seven showed at least moderate effects (RCI > 0.50); one additional patient had an RCI of 0.49. On the FIQ, four had large effects, and eight patients showed at least moderate effects. There was substantial improvement on the emotional distress measure; two had large effects and eight had at least moderate effects. Improvement rates for pain and disability were somewhat lower. Three patients experienced large improvements in disability, and a total of six had at least moderate gains. For pain, however, only one had a large gain, and four had at least moderate gains. Finally, in terms of life satisfaction, half of the sample showed a large effect, but the other half showed no effect. Overall, the self-report measures, therapist impressions, and exit interviews suggest the following conclusions: two patients made substantial improvement, four made moderate and meaningful gains, two showed modest benefits, and two did not benefit at all.
Discussion
This initial study of emotional exposure-based treatment for people with FMS who also have unresolved trauma demonstrated generally positive results. Across measures, the average improvement three months after treatment was between 0.36 and 0.79 SDs from pretreatment scores—effects that are moderate to large. These benefits are particularly noteworthy because they were obtained in relatively few sessions (typically 10, and no more than 15) among patients with substantial pain, disability, and emotional distress for many years, which would not be expected to resolve on its own over a few months. Furthermore, these patients had extensive medical treatments and histories of psychotherapy, which apparently had been of little success. With respect to treatment acceptability, of the 13 patients offered treatment, 10 accepted, and all of them completed the protocol. Thus, this study suggests that a time-limited, individually tailored, emotional exposure-based treatment protocol for women with FMS and unresolved stress may be both acceptable and effective.
It is noteworthy that stress symptoms (intrusions, avoidance, and hyperarousal), as well as emotional distress and life satisfaction improved the most (large effects), whereas pain and disability improved the least (small to moderate effects). In theory, stress symptoms should change the most because they are targeted directly by this treatment, whereas pain and disability are not. The latter are influenced by multiple factors (e.g., environmental contingencies, physical conditioning, tissue damage, neuronal functioning), and larger effects on these outcomes may require additional interventions, such as behavioral techniques (exercise, activity rest-cycling), altered contingencies, or medication. A provocative possibility is that patients whose post-traumatic stress improves (i.e., better emotional regulation and interpersonal relationships) may be more amenable to and successful with a subsequent course of cognitive-behavior pain management training or rehabilitation.
Our review of individual data, exit interviews, and therapist observations suggested that 20% of our patients (two of ten) had substantial or even remarkable improvements, including greatly reduced stress symptoms, markedly more adaptive behavior and relationships, and one had nearly full remission of pain. Another 40% were judged as having made moderate and meaningful gains in their mental and physical health. Patients with these positive outcomes typically addressed long-avoided affects and worked on these issues between sessions. Although initially fearful, they found the courage—usually with substantial therapist prodding—to face experiences and behaviors that were affectively charged. Interestingly, the experiences that were avoided and the specific techniques that were used differed markedly across cases, supporting our contention that flexibly identifying avoided stimuli and tailoring the exposure techniques are important features of this treatment. Some patients emotionally processed childhood trauma, others addressed avoided interpersonal patterns using assertiveness training and role plays, others had corrective experiences with the therapist to alter rigid interpersonal styles, and some brought in family members to experiment with new ways of communicating.
This study has implications for theory and clinical practice. We hope that further development and testing of this treatment will make available a useful intervention for those patients who currently are not benefiting from cognitive behavioral treatments such as pain coping skills training, or from multidisciplinary rehabilitation including exercise. Although these other treatments are of value for some people with FMS, patients with affect or interpersonal regulation problems—often stemming from a history of trauma—may need an alternative approach like the one described here. Although pain sometimes worsens when patients have affectively charged experiences, such an observation is valuable evidence to the patient and practitioner that emotions directly influence the pain. Also, exacerbations of pain and distress often are temporary effects of treatment and may be key indicators of change processes, much as increased arousal is an indicator of successful emotional processing of an anxiety disorder. Further processing rather than escape may be needed to allow change to occur.
Our treatment highlights the value of assessment and the active role of the therapist in both assessment and change processes. Empirically-supported cognitive-behavioral pain management programs usually offer all patients a defined and structured treatment program, and the therapist’s role is primarily an educator or coach. Such approaches are more efficient and easier to teach, monitor, and implement than this intervention, and may be the preferred option for chronic pain patients who have reasonably good emotional and relational functioning. But we think that there may be added benefits of assessing the patient’s experiences and needs, and of the therapist becoming part of the change process. First, assessment can identify those patients who have unresolved trauma and who can then be targeted for this type of intervention. Second, therapists need to be alert for subtle signs of avoidance, which can be found not only in patients’ reports of daily events, but also in the behaviors they manifest with the therapist. Therapists can then use the relationship to have the patient try new behaviors, the most important of which is meta-communication about the process of therapy, in which patients are encouraged to communicate directly to the therapist, who validates the patient’s fear and need for control, yet also encourages the patient to confront avoided experiences. Importantly, therapists doing this type of treatment need the conviction that it is therapeutic to move patients toward avoided experiences, as well as the courage to do so. This process can be emotionally challenging, and the tendency is for both patient and therapist to collude to avoid such experiences. We hope that research support for this treatment, early therapist training in these techniques, providing the patient a clear rationale for this approach, and the use of meta-communication will better prepare therapists and patients to engage in this type of therapy.
Clearly, a sample of 10 women in a study that lacks a control group and relies on self-report outcome measures is not sufficient to conclude treatment efficacy. The uncontrolled nature of this study leaves open alternative explanations for the observed benefits, including demand effects and maturation. We need replication on a larger sample, inclusion of attention control and comparison treatments, and objective outcomes, such as measures of actual pain behavior, health care use, and collateral reports. Follow-up assessment beyond three months is needed to determine the duration of the effects and whether pain and disability show delayed improvement. Also, the generalizability of this intervention when offered directly to men or to patients in medical settings (rather than self-referred patients) may be limited. Although we suspect that this treatment will be effective for people with unresolved trauma and other chronic pain conditions (e.g., low back pain, migraine headaches, irritable bowel syndrome, pelvic pain), this needs to be tested.
A substantial contribution of this study, however, is that it highlights the potential value of an emotional exposure and processing approach to dealing with the unresolved psychological trauma found in many patients with FMS, and perhaps other pain conditions. The field needs to target treatments to particular people, rather than continue to behave as if “one approach fits all.” We hope that this initial research will spur the field to study ways to address the effects of the elevated levels of trauma and stress found in some people with chronic pain. But we also hope that researchers and clinicians will be mindful that many people with these pain problems likely do not need—and should not be given—this treatment, and research is needed to identify which approach is best for which patients.
Acknowledgments
Preparation of this article was supported, in part, by National Institutes of Health grants AR049059 and AG009203.
Contributor Information
Mark A. Lumley, Department of Psychology, Wayne State University, Detroit, MI.
Jay L. Cohen, Department of Psychology, Wayne State University, Detroit, MI. Psychology Section, Mental Health Service, John D. Dingell VAMC, Detroit, MI.
Rebecca L. Stout, Department of Psychology, Wayne State University, Detroit, MI.
Lynn C. Neely, Department of Psychology, Wayne State University, Detroit, MI. Department of Psychology, Oakland University.
Lindsay M. Sander, Department of Psychology, Wayne State University, Detroit, MI.
Amanda J. Burger, Department of Psychology, Wayne State University, Detroit, MI.
References
- Bennett R. The Fibromyalgia Impact Questionnaire (FIQ): A review of its development, current version, operating characteristics and uses. Clinical and Experimental Rheumatology. 2005;23:154–162. [PubMed] [Google Scholar]
- Cohen H, Neumann L, Haiman Y, Matar MA, Press J, Buskila D. Prevalence of post-traumatic stress disorder in fibromyalgia patients: overlapping syndromes or post-traumatic fibromyalgia syndrome? Seminars in Arthritis & Rheumatism. 2002;32:38–50. doi: 10.1053/sarh.2002.33719. [DOI] [PubMed] [Google Scholar]
- Davis MC, Zautra AJ, Reich JW. Vulnerability to stress differs in older women with fibromyalgia versus osteoarthritis. Annals of Behavioral Medicine. 2001;23:215–226. doi: 10.1207/S15324796ABM2303_9. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Melisaratos The Brief Symptom Inventory: An introductory report. Psychological Medicine. 1983;13:595–605. [PubMed] [Google Scholar]
- Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction with Life Scale. Journal of Personality Assessment. 1985;49:71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear: Exposure to corrective information. Psychological Bulletin. 1986;99:20–35. [PubMed] [Google Scholar]
- Gillis ME, Lumley MA, Mosley-Williams A, Leisen JC, Roehrs T. The health effects of at-home written emotional disclosure in fibromyalgia: A randomized trial. Annals of Behavioral Medicine. 2006;32:135–146. doi: 10.1207/s15324796abm3202_11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCullough L, Kuhn N, Andrews S, Kaplan A, Wolf J, Hurley CL. Treating affect phobia: A manual for short-term dynamic psychotherapy. New York: Guilford; 2003. [Google Scholar]
- Meenan RF, Mason JH, Anderson JJ, Guccione AA, Kazis LE. AIMS2. The content and properties of a revised and expanded Arthritis Impact Measurement Scales Health Status Questionnaire. Arthritis and Rheumatism. 1992;35:1–10. doi: 10.1002/art.1780350102. [DOI] [PubMed] [Google Scholar]
- Melzack R. The McGill Pain Questionnaire: Major properties and scoring methods. Pain. 1975;1:277–299. doi: 10.1016/0304-3959(75)90044-5. [DOI] [PubMed] [Google Scholar]
- Weiss D, Marmar C. The Impact of Event Scale -Revised. In: Wilson J, Keane T, editors. Assessing psychological trauma and PTSD. New York: Guildford; 1997. [Google Scholar]