Abstract
Purpose
The purpose of this study is to investigate parent reports of the diabetes care support their children receive in school, their concerns about diabetes management in school, and their knowledge of federal laws that protect children with diabetes. In addition, the study explores ethnic and socioeconomic status differences in diabetes management in school.
Methods
An ethnically heterogeneous sample of 309 parents of children with diabetes was recruited from a community-based and a university-based diabetes outpatient clinic. Parents completed a survey assessing supports their child's school provides for diabetes care, worries about diabetes care in school, and awareness of federal laws that pertain to children with diabetes.
Results
Many children did not have a written care plan or a nurse at school, but significantly more white children had these supports than Hispanic or black children. Most children were not allowed to check blood glucose levels or administer insulin in class. Most parents were worried about hyperglycemia and hypoglycemia in school, and most were not at all or only a little confident in the school's ability to care for diabetes. Most parents were not aware of federal laws, but high-income and white parents were more likely to be aware.
Conclusions
According to parents in the current study, children receive inadequate diabetes management support in schools. Minority children are less likely to receive supports than white children. Parents are worried about diabetes management in school, but most do not have the knowledge of federal laws necessary to protect their children.
Diabetes mellitus is one of the most common chronic conditions of childhood.1 Type 1 diabetes is the most common diagnosis, with 1 in every 400 to 600 individuals younger than 20 years affected.2 Recent studies suggest that the incidence of type 1 diabetes may be increasing in the United States and worldwide.3,4 Although type 2 diabetes is less common among school-age children than type 1 diabetes, the incidence of type 2 diabetes has increased in the past several years in concordance with the unprecedented rates of obesity among youth.5 The increasing prevalence of type 2 diabetes among overweight children and adolescents is especially dramatic among minorities.4,6 In total, an estimated 18 700 children younger than 20 years are newly diagnosed with diabetes mellitus each year in the United States.4
Diabetes self-care is complex and requires significant lifestyle adaptations that can be difficult for all people with diabetes; however, these changes are especially complicated for children and adolescents. Frequent monitoring of blood glucose levels is required, and constant access to glucose meters is a necessity. Food intake, particularly carbohydrates, must be carefully monitored. Medication administration includes multiple daily insulin injections or continuous subcutaneous insulin infusion (the insulin pump) in cases of type 1 diabetes and daily oral medication in most cases of type 2 diabetes. Inadequate management in any of these demanding self-care behaviors in children with type 1 diabetes can lead to hyperglycemia (high blood glucose) and hypoglycemia (low blood glucose), each of which can be have serious adverse health consequences in both the short and long term. Youth with poorly managed type 2 diabetes are at risk for hyperglycemia and its associated health risks.
Balancing the array of diabetes self-care behaviors can be frustrating.7 For children and adolescents, who spend approximately half of their waking hours at school, these frustrations can be compounded by difficulties getting the support they need while at school.8,9 To keep up with their self-care regimen, youth with diabetes need a variety of special considerations, including access to and permission to perform blood glucose monitoring, unrestricted access to water and bathrooms, insulin and oral medication administration, and ability to eat anywhere at any time if needed. In addition to these special considerations, support is needed in the form of school personnel who are knowledgeable about diabetes and trained to provide insulin, administer medication, and treat hypoglycemia and hyperglycemia.
Three federal laws protect the rights of children to obtain the care they need while in school: Section 504 of the Rehabilitation Act of 1973 (Section 504), the Americans With Disabilities Act (ADA), and the Individuals With Disabilities Education Act (IDEA).10 Section 504 and the ADA require schools to provide aids and services to ensure that children will be medically safe while having the same access to educational opportunities as other children. IDEA funds special education services for children whose hypoglycemic or hyperglycemic episodes may significantly impair their ability to concentrate and learn. To best follow these laws, the American Diabetes Association and the American Association of Diabetes Educators have issued position statements that outline guidelines for drafting medical care plans for children with diabetes.11,12
Some research suggests that schools find it difficult to provide support for children with diabetes. In many instances, school personnel are not educated regarding diabetes care needs and therefore do not allow children access to the water, restrooms, glucose meters, and medications they need to care for themselves.9,13 Availability of school nurses is often limited, and many schools have a nurse only 1 or fewer days per week; however, in some schools, only nurses are authorized to provide diabetes care.13 Concerns about liability can prevent school personnel from participating in blood glucose monitoring, insulin injections, and glucagon administration, leaving children without any competent adult assistance in cases of emergency.14
Despite the importance of diabetes care at school, only 2 studies have investigated the experiences of children and families negotiating this process. First, in a qualitative study with 30 adolescents and their parents, researchers asked participants to describe their perceptions of the current system of diabetes care in school.15 Participants expressed concern about school staff's limited knowledge about diabetes, lack of healthy foods available, and inflexible rules that make it difficult to do necessary self-care tasks. In another study, middle school children attending diabetes summer camp reported a need for increased flexibility and individualized care plans to improve diabetes self-management in school.8
In the current study, an ethnically and socioeconomically heterogeneous sample of parents of youth with diabetes reported their experiences managing their child's diabetes at school. Although scarce in the existing literature, the perspectives of parents from diverse ethnic backgrounds are crucial for understanding school-based diabetes care for several reasons. Among type 1 diabetes cases, African American and Latino youth are more likely to be in poorer metabolic control when compared with their Caucasian counterparts.16 The prevalence of type 2 diabetes is on the rise, and minority children represent a disproportionate number of new cases.4 Research indicates that minority adults with diabetes have poorer glycemic control and are at greater risk for long-term health complications than Caucasian adults.17 To improve school-based diabetes care, it is imperative to document the concerns of parents to inform changes in school health policy.
An initial step in supporting parents in their attempt to negotiate diabetes care in their child's school is investigating how much parents know about the federal laws that protect their children with diabetes. The current study assessed concerns of parents about diabetes care in schools as well as parents' knowledge of laws protecting their children's rights to diabetes self-care at school. To date, no known studies have investigated awareness of these laws among parents of children with diabetes.
Therefore, this study addressed 4 main research questions. First, what support do children with diabetes receive in school? Second, to what degree are parents concerned about diabetes care in schools? Third, are parents aware of federal laws protecting children with diabetes at school? Finally, do ethnic or socioeconomic group differences in parental reports about concern and support for diabetes care and knowledge about laws exist?
Methods
Participants and Procedures
Participants were recruited from 2004 to 2006 from 2 sites: a university-based (n = 155) and a community-based outpatient diabetes clinic (n = 154). During a scheduled visit with their child's endocrinologist, parents of children with diabetes were asked to complete a survey regarding awareness of federal laws and concerns about diabetes management while in school. Of 336 parents approached, 309 (92%) consented and completed the survey. Responders were mothers (80%), fathers (15%), or other guardians (5%). Surveys were administered in English (84%) or Spanish (16%). Hollingshead socioeconomic status (SES) scores were calculated based on parent report of both mother and father education level and occupation.18 If both parents worked, scores were averaged between the 2 parents. Families comprised the full range of SES (range = 8-66; mean Hollingshead score = 40.94, SD = 14.07).
Children were 4 to 19 years old (mean age = 11.83, SD = 3.70), and the mean duration of diabetes diagnosis was 4.37 years (SD = 3.62). Of the 302 parents who reported their child's diabetes type, 88% of children were diagnosed with type 1 (n = 267), 9% with type 2 (n = 26), and 3% with atypical (n = 9) diabetes. Medical regimens varied, with 29% of children diagnosed with type 1 diabetes using the insulin pump and 71% administering daily insulin injections. Among children with type 2 diabetes, 38% administered daily insulin injections and 62% took oral medication. All parents reported that their child was required to perform blood glucose level checks every day. When describing their child's racial and ethnic background, most parents reported that their children were minorities (61% Hispanic white, 19% non-Hispanic white, 19% African or Caribbean American, 1% other ethnicity). Most children attended public school (82%), with 18% attending private school.
Measures
Parents were given a survey created for the purpose of this study to assess parental awareness of federal care laws and concerns about their child's diabetes management while in school. In addition to demographic information about the parent, child, and family, the questionnaire assessed 8 major content areas: knowledge of federal laws, child's care plan for diabetes in school, concern for child's diabetes in school, responsibility for medical needs at school, school staff ability/resources, special accommodations for child at school, disruption of parents' work activities, and child's medical regimen. Questions included both quantitative prompts (eg, “How confident are you in school staff's ability to properly care for your child's diabetes: not at all, a little, pretty much, or very much confident?”) and qualitative prompts (eg, “List in importance to you the major concerns you have about caring for your child's diabetes in school?”).
Results
Parental Report of Diabetes Care Support in School
Parents described the support their children receive in school regarding diabetes care; responses to these questions for each ethnic group and among all participants are depicted in Table 1. Overall, 45% of children did not have a written care plan, and 45% did not have a nurse at their school; 24% of parents reported that schools had been unable to meet their child's diabetes care needs. Only 49% of parents reported that schools had a glucagon kit available. Most children were not allowed to check blood glucose level (52%) or administer insulin (79%) in class. Only 46% of parents reported insulin injections were allowed in special places at school (other than the classroom), with just 50% reporting blood glucose checks were allowed in special places. A series of χ2 analyses were completed to detect differences in diabetes support in schools by SES, ethnicity, and type of school (public vs private). For these and all other χ2 analyses, SES was categorized into low (Hollingshead code = 1 or 2), middle (Hollingshead code = 3), or high (Hollingshead code = 4 or 5) SES. No significant SES differences were detected; however, ethnic differences emerged in several areas. White parents were more likely to report the existence of a written care plan, χ2(5, n = 284) = 15.26, P < .05, and the existence of a nurse at their child's school, χ2(5, n = 265) = 14.23, P < .05, than Hispanic or black parents. Black parents were more likely to report that their child's school denied access to extra snacks when needed, χ2(5, n = 282) = 16.14, P < .01, and access to water fountains or restrooms, χ2(6, n = 282) = 17.04, P < .01, than Hispanic or white parents. Public and private schools did not vary significantly on any measure of diabetes care support in school.
Table 1.
Parent Report of Diabetes Support in School by Ethnicity
| Form of Diabetes Support in School | Percentage of “Yes” Responses Within Group | |||
|---|---|---|---|---|
| Hispanic | White | Black | Overall | |
| Does child have written care plan?a | 52 | 74 | 46 | 55 |
| Does school have a nurse?a | 48 | 78 | 54 | 55 |
| Does child have glucagon kit at school?a | 45 | 70 | 43 | 49 |
| Blood glucose checks in class allowed? | 50 | 57 | 31 | 48 |
| Blood glucose checks in special places allowed? | 53 | 47 | 26 | 50 |
| Insulin in class allowed? | 23 | 20 | 10 | 21 |
| Insulin in special places allowed? | 57 | 55 | 46 | 54 |
| Extra snacks allowed when needed?a | 86 | 90 | 70 | 84 |
| Access to bathroom when needed?a | 80 | 93 | 69 | 81 |
Responses vary significantly by ethnic group, P < .05.
Parental Concerns About Diabetes Care in School
Overall, parents expressed significant concerns regarding their children's diabetes care in school (see Figure 1). Most parents reported having at least a little worry about their child having high (92%) or low (93%) blood glucose levels at school. Similarly, as shown in Figure 2, most parents reported that they were not at all or only a little confident that their child's school can care for diabetes (57%) or assess hypoglycemia (60%). Analysis of variance (ANOVA) tests revealed significant differences between ethnic groups in parental worry about low blood glucose levels, F(2, 282) = 2.73, P < .05, and about high blood glucose levels while at school, F(2, 284) = 5.40, P < .001. Post hoc t tests comparing ethnic groups were conducted to detect group differences in parental worry. Hispanic parents were significantly more worried about high (t = 3.32, P < .001) and low (t = 4.00, P < .001) blood glucose than white parents. No other ethnic group differences emerged. ANOVAs were conducted to test for SES differences in worry and confidence. No significant differences emerged. A series of t tests revealed significant differences between public and private school parents in both worry and confidence. Parents of children in public schools had higher levels of worry about low blood glucose (t = 2.42, P < .05) and high blood glucose (t =3.18, P < .01) than parents of children in private schools. Similarly, parents of children in public schools had lower levels of confidence in the school's ability to care for their child's diabetes needs (t = −3.32, P < .001) and to assess hypoglycemia (t = −2.58, P < .01).
Figure 1.
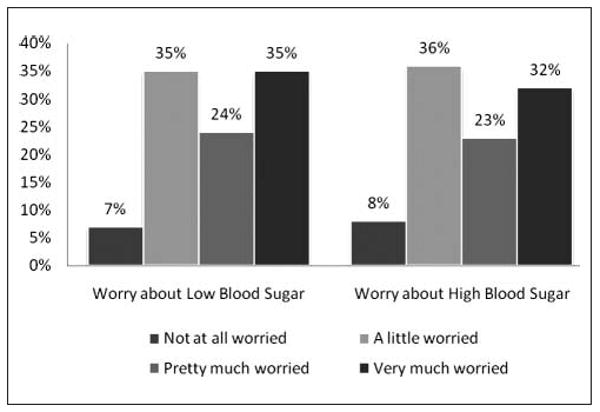
Parent ratings of concern about child's blood glucose level in school.
Figure 2.
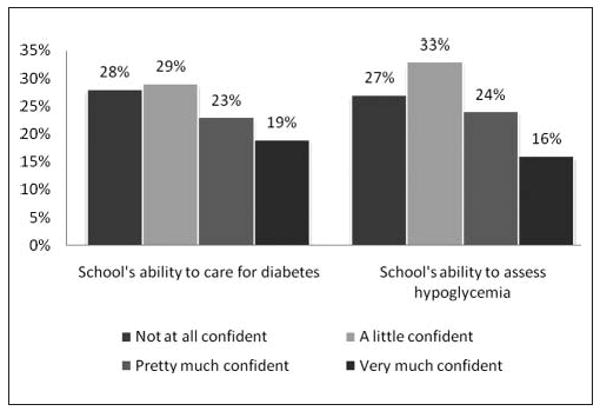
Parent ratings of confidence in the school's ability to care for diabetes and assess hypoglycemia.
Parental Awareness of Federal Laws
Most parents were not aware of any of the federal laws that may apply to children with diabetes while they are attending school (see Figure 3): one-third of parents were aware of Section 504, 36% were aware of ADA, and just 13% were aware of IDEA. Chi-square analyses revealed group differences in parental awareness of laws. Parents of children with type 1 diabetes were more likely to be aware of Section 504, χ2(2, n = 297) = 11.59, P = .02, and of the ADA, χ2(2, n = 294) = 9.77, P = .05, than were parents of children with type 2 or atypical diabetes. SES differences in knowledge of Section 504, χ2(2, n = 242) = 12.92, P < .01, and the ADA, χ2(2, n = 240) = 6.93, P < .05, existed as well. A higher percentage of high SES parents were aware of Section 504 (43%) than low SES (23%) or middle SES (19%) parents. Similarly, high SES parents were more likely to be aware of the ADA (47%) than middle SES (30%) or low SES (29%) parents. Chi-square analyses also revealed ethnic differences in knowledge of federal laws. A higher percentage of white parents (58%) were aware of Section 504 than Hispanic (31%) or black (13%) parents, χ2(3, n = 286) = 26.88, P < .001. Similarly, a larger proportion of white parents (64%) were aware of ADA than Hispanic (30%) or black (30%) parents, χ2(3, n = 283) = 20.20, P < .001. Most parents were unaware of IDEA (87%), and no significant group differences emerged. Parents of children in public and private schools were not significantly different in their knowledge of federal laws.
Figure 3.
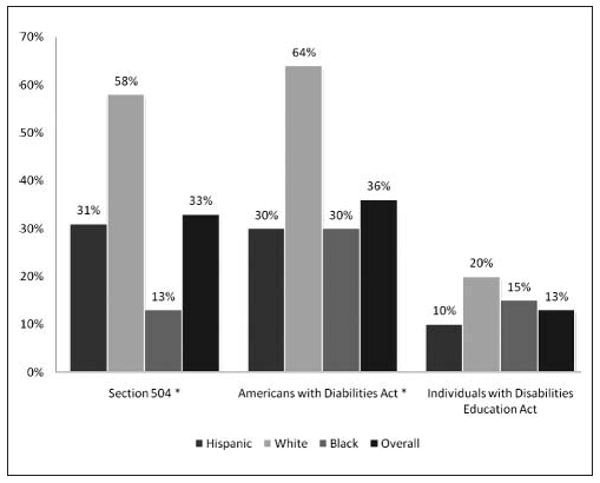
Percentage of parents within group reporting awareness of federal disability laws. *Indicates significant group differences by ethnicity, P < .05.
Discussion
Parents completed a survey regarding several important aspects of diabetes care in their child's school, and 4 major findings emerged. First, support for diabetes care from schools was lacking in many areas, including written care plans, school nurses, and flexibility to attend to diabetes care needs such as blood glucose monitoring and insulin injections. Second, most parents reported concern about their child's health while at school and expressed some doubt about the school's ability to support diabetes care needs. Third, most parents were not aware of the federal laws that may protect children with diabetes. Fourth, parental concerns, school support for diabetes care, and parental awareness of federal laws differed depending on ethnic background and SES.
A surprising number of parents (45%) reported that their child did not have a written care plan in school. Written care plans are critical for children with diabetes. Not only is daily management of glucose levels essential, a clear and precise plan in case of emergency is of utmost importance. If students are not treated properly during episodes of hypoglycemia, unconsciousness and convulsions can result. Findings from this study revealed that only 49% of schools reportedly had a glucagon kit available. Improperly treated hyperglycemia can lead to diabetic ketoacidosis, which can also be life threatening. Federal law protects the rights of children to be medically safe while at school; the absence of a glucagon kit is clearly inconsistent with these laws. Federal law also requires children with diabetes to have an individualized assessment, and the American Diabetes Association guidelines recommend every child have an individualized diabetes medical management plan.11 Results from the current study clearly indicate a need for increased advocacy for children with diabetes in schools and enforcement of federal disability laws that require children with diabetes to have written care plans.
In addition to written care plans, parents in the study reported on school rules that may prohibit their children from attending to diabetes care needs. Contrary to the American Diabetes Association's recommendation that children be allowed to check blood glucose levels in the classroom, only 48% of parents reported that their children were afforded this privilege. Only 21% of children were allowed to administer insulin in the classroom, and only 54% were allowed to administer insulin in special places. A total of 25% of students were not allowed to administer insulin anywhere at school. In a study of middle school children with diabetes and their parents, Wagner and colleagues19 found that children who were allowed to attend to diabetes care needs in their classroom had lower HbA1C levels than those who had to leave class to check blood glucose and inject insulin.19 Taken together, these results suggest that the restrictions that many schools put on children with diabetes may have serious health implications.
Perhaps as a result of the lack of support available in schools, most parents in the current study were worried about their children experiencing episodes of both hypoglycemia and hyperglycemia while at school. In general, parents expressed reservations about the school's ability to provide diabetes support; in fact, 28% of parents reported that they were “not at all confident” in the school's ability to care for diabetes. These results are consistent with a prior study of the perceptions of school support among children with diabetes in which youth described a need for improved knowledge of diabetes among school staff and increased support from other people to help manage diabetes in school.8 Similarly, in a qualitative study with adolescents and their parents, lack of knowledge and training of school staff was a major theme.15 Whereas the previous literature provided valuable qualitative information about the areas of concern among children, teens, and parents of teens with diabetes, the current study provides quantitative information about the prevalence of worry and concern. Past research has relied on more homogeneous white samples, but the current study relies on the perspectives of primarily minority participants.
Most of the parents in the current study were not aware of any of the federal laws that protect children with diabetes. Only 36% were aware of the ADA and only 33% were aware of Section 504 as they may apply to children with diabetes while attending school. The ADA and Section 504 require schools to provide the necessary supports to ensure that children are medically safe at school and have the same access to all educational opportunities as other children. Most parents in the current study reported that their children are not being afforded these supports (ie, nurses, permission to complete diabetes care tasks in the classroom, etc). Without knowledge of the ADA and Section 504 laws that protect their children, parents may not be prepared to negotiate with schools to ensure their child gets what he or she needs for optimal diabetes management.
Several interesting group differences were detected in parents' responses to the survey. In terms of diabetes support provided by schools, white parents were more likely to report the existence of a written care plan and a school nurse than Hispanic or black parents. Black parents were more likely to report that their children were denied access to extra snacks and bathrooms than white or Hispanic parents. These results shed light on previous research showing that minority children have poorer metabolic control than white children.16 Without the ability to properly attend to diabetes care needs in the setting where children spend at least half of their waking hours, metabolic control will likely suffer. Group differences in awareness of federal laws applicable to children with diabetes also existed. High SES parents were more likely to know about Section 504 and the ADA than middle or low SES parents. White parents were more likely to know about these laws than Hispanic or black parents. Taken together, these results suggest that the children who most need advocacy for diabetes support in schools have parents who are least likely to be aware of the federal laws that protect their children. Acknowledging these ethnic and SES disparities in diabetes care support in schools is crucial for future research.
Although the current study is the first to survey a large ethnically diverse sample of parents of children with diabetes regarding issues surrounding diabetes management in schools, several limitations of the current study suggest future avenues of research. Because of the geographic region in which data were collected, most of the sample was Hispanic, and black parents were underrepresented. Although significant ethnic group differences were found, future research is needed to replicate these findings with larger black samples. Because of widely varied policies among states and regional school systems, the degree to which the results of the study are generalizable to students in other areas of the country is uncertain. The study relied on parents' reports about diabetes supports in their child's school rather than observational measures. Future research might work directly with schools to investigate modifications being made to support diabetes management. In addition, the current study did not include a measure of children's glycemic control or their actual diabetes management behaviors while in school. Collection of such data would allow future researchers to investigate the relation between diabetes support in school and how well children are managing their diabetes.
Implications
The current study has several implications for diabetes educators. First, educators should be aware of the often inadequate diabetes management support provided by schools. At the most basic level, many children do not even have a written care plan while at school. Many children do not have adequate access to blood glucose monitoring, insulin administration, bathrooms, and snacks when needed. Second, diabetes management in schools is important to families. Parents are concerned about their children experiencing hyperglycemic and hypoglycemic episodes while at school, and many are not confident in the school's ability to care for diabetes needs. Third, most parents must be educated about the federal laws that protect children with diabetes by requiring schools to provide the supports they need for diabetes management. Finally, black children and youth from low SES backgrounds may have less diabetes care support in schools and their parents may have less knowledge about federal care laws, so these children would be most likely to benefit from enhanced support and advocacy.
Acknowledgments
This research was supported in part by a grant from the Dyson Foundation and by a research training grant from the National Institutes of Health (T32HD07510).
References
- 1.Libman I, Songer T, LaPorte R. How many people in the US have IDDM? Diabetes Care. 1993;16:841–842. doi: 10.2337/diacare.16.5.841. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. National Diabetes Fact Sheet, United States. 2005 http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2005.pdf.
- 3.Onkamo P, Vaananen S, Karvonen M, Tuomilehto J. Worldwide increase in incidence of type 1 diabetes: the analysis of the data on published incidence trends. Diabetologia. 1999;42:1395–1403. doi: 10.1007/s001250051309. [DOI] [PubMed] [Google Scholar]
- 4.The Writing Group for the SEARCH for Diabetes in Youth Study Group. Incidence of diabetes in youth in the United States. JAMA. 2007;297:2716–2724. doi: 10.1001/jama.297.24.2716. [DOI] [PubMed] [Google Scholar]
- 5.Rocchini AP. Childhood obesity and a diabetes epidemic. N Engl J Med. 2002;346:354–355. doi: 10.1056/NEJM200203143461112. [DOI] [PubMed] [Google Scholar]
- 6.Dabelea D, Pettitt DJ, Jones KL, Arslanian SA. Type 2 diabetes mellitus in minority children and adolescents: an emerging problem. Endocrinol Metab Clin North Am. 1999;28:709–729. doi: 10.1016/s0889-8529(05)70098-0. [DOI] [PubMed] [Google Scholar]
- 7.Polonsky W. Emotional and quality-of-life aspects of diabetes management. Curr Diab Rep. 2002;2:153–159. doi: 10.1007/s11892-002-0075-5. [DOI] [PubMed] [Google Scholar]
- 8.Nabors L, Lehmkuhl H, Chrostos N, Andreone TL. Children with diabetes: perceptions of supports for self-management at school. J School Health. 2003;73(6):216–221. doi: 10.1111/j.1746-1561.2003.tb06563.x. [DOI] [PubMed] [Google Scholar]
- 9.Nabors L, Troillett A, Nash T, Masiulis B. School nurse perceptions of barriers and supports for children with diabetes. J School Health. 2005;75(4):119–124. [PubMed] [Google Scholar]
- 10.Kaufman FR. Diabetes at school: what a child's health care team needs to know about federal disability law. Clin Diabetes. 2002;29(2):91–92. [Google Scholar]
- 11.American Diabetes Association. Diabetes care in the school and day care setting. Diabetes Care. 2008;31:S79–S86. doi: 10.2337/dc08-S079. [DOI] [PubMed] [Google Scholar]
- 12.American Association of Diabetes Educators. Management of children with diabetes in the school setting. Diabetes Educ. 2000;26(1):32–35. doi: 10.1177/014572170002600105. [DOI] [PubMed] [Google Scholar]
- 13.Brener ND, Burstein GR, DuShaw ML, Vernon ME, Wheeler L, Robinson J. Health services: results from the school health policies and programs study 2000. J School Health. 2001;71(7):294–303. doi: 10.1111/j.1746-1561.2001.tb03506.x. [DOI] [PubMed] [Google Scholar]
- 14.Gray DL, Golden MP, Reiswerg J. Diabetes care in schools: benefits and pitfalls of public law. Diabetes Educ. 1991;17:33–36. doi: 10.1177/014572179101700107. [DOI] [PubMed] [Google Scholar]
- 15.Hayes-Bohn R, Neumark-Sztainer D, Mellin A, Patterson J. Adolescent and parent assessments of diabetes mellitus management at school. J School Health. 2004;74(5):166–169. doi: 10.1111/j.1746-1561.2004.tb08215.x. [DOI] [PubMed] [Google Scholar]
- 16.Delamater AM, Shaw KH, Pratt IA, et al. Risk for metabolic control problems in minority youths with diabetes mellitus. Diabetes Care. 1999;22:700–705. doi: 10.2337/diacare.22.5.700. [DOI] [PubMed] [Google Scholar]
- 17.Harris MI, Eastman RC, Cowie CC, Flegal KM, Eberhardt MS. Racial and ethnic differences in glycemic control with type 2 diabetes. Diabetes Care. 1999;22:403–408. doi: 10.2337/diacare.22.3.403. [DOI] [PubMed] [Google Scholar]
- 18.Hollingshead AB. Two Factor Index of Social Position. New Haven, CT: Yale University; 1965. [Google Scholar]
- 19.Wagner J, Heapy A, James A, Abbott G. Glycemic control, quality of life, and school experiences among students with diabetes. J Pediatr Psychol. 2006;31(8):764–769. doi: 10.1093/jpepsy/jsj082. [DOI] [PubMed] [Google Scholar]


