Abstract
We used an Approach-Avoidance Task (AAT) to examine response to threatening stimuli in 20 individuals high in contamination-related obsessive-compulsive symptoms (HCs) and 21 individuals low in contamination-related obsessive-compulsive symptoms (LCs). Participants were instructed to respond to contamination-related and neutral pictures by pulling a joystick towards themselves or by pushing it away from themselves. Moving the joystick changed the size of the image to simulate approaching or distancing oneself from the object. Consistent with our hypothesis, the HC group was significantly slower in pulling contamination-related pictures than in pulling neutral pictures, whereas in the LC group there was no difference between speed of pulling contamination-related pictures and neutral pictures. Contrary to our hypothesis, we did not find support for faster pushing away of contamination-related pictures than neutral pictures by the HC group. Moreover, the degree of avoidance of contamination-related stimuli when pulling – but not when pushing – was significantly correlated with self-reported contamination-related obsessive-compulsive symptoms. These results suggest a biased behavioral response for threatening objects in individuals high in contamination fears only when inhibiting the prepotent response to avoid threatening stimuli and not when performing a practiced avoidance response. Thus, our results validate the use of the AAT as a measure of inhibited and uninhibited automatic avoidance reactions to emotional information in individuals with contamination-related obsessive-compulsive symptoms.
Keywords: approach-avoidance task, avoidance, obsessive-compulsive, contamination, information-processing
Obsessive-compulsive disorder (OCD) is a chronic and debilitating disorder that affects approximately 2% of the population (Eisen & Steketee, 1997; Narrow, Rae, Robins, & Regier, 2002; Steketee & Barlow, 2002). Individuals with OCD tend to avoid anxiety-related materials. These avoidance tendencies are usually assessed using introspective reports during an interview (e.g., Yale-Brown Obsessive Compulsive Scale, Y-BOCS; Goodman et al., 1989) or self-report questionnaires (e.g., Maudsley Obsessional-Compulsive Inventory, MOCI, Hodgson & Rachman, 1977; Obsessive–Compulsive Inventory, OCI, Foa, Kozak, Salkovskis, Coles, & Amir, 1998). These measures ask participants to report on their recollections of actions taken or on actions they believe they would be likely to take when confronted with their feared objects or thoughts. A shortcoming of these self-report assessments is that they may be influenced by social desirability or inaccurate reporting (Baumeister, Vohs, & Funder, 2007). Indeed, during the course of exposure and response prevention, the treatment of choice for OCD, patients are often surprised by how easy it is to approach an object or situation they had reported as being high on their fear hierarchy, or conversely, how difficult it is to approach something that they had reported as being low on their fear hierarchy.
To address some of the issues inherent in using self-report measures, researchers have successfully used behavioral assessment tests (BATs) with OCD patients (e.g., Foa, Steketee, and Grayson, 1985; Rachman, Marks, and Hodgson, 1973; Steketee, Chambless, Tran, Worden, & Gillis, 1996) and individuals with subclinical obsessive-compulsive symptoms (e.g., Cougle, Wolitzky-Taylor, Lee, and Telch, 2007; Najmi & Amir, 2010). In these tasks, participants are asked to approach steps in a graduated hierarchy of feared situations and avoidance is measured by the number of steps that remain uncompleted by the participant. Direct measures such as BATs are well suited for the assessment of controlled behavior but do not shed light specifically on the automatic aspects of behavior.
More recently, researchers have used reaction time measures to investigate the more automatic aspects of behavioral approach and avoidance. According to the reflective-impulsive model of behavior (Strack & Deutsch, 2004), stimuli from the environment elicit automatic evaluations that activate affectively congruent behavioral schemas of approach (associated with positive affect) and avoidance (associated with negative affect). One way to assess these behavioral schemas indirectly is in terms of arm flexion (approach) versus extension (avoidance). For example, Solarz (1960) showed that participants were faster to pull pleasant stimuli towards themselves than to pull negative stimuli toward themselves. Conversely, participants were faster in pushing away negative stimuli from themselves than in pushing away positive stimuli away from themselves. Subsequent research has demonstrated that positive stimuli and attitudes are associated with faster arm flexion than arm extension, while negative stimuli and attitudes are associated with faster arm extension than arm flexion (Cacioppo, Priester, & Bernston, 1993; Chen & Bargh, 1999; Kawakami, Phills, Steele, & Dovidio, 2007; Neumann, Hülsenbeck, & Seibt, 2004).
Although the above studies have established a relationship between arm flexion/extension and valence of the target, naturalistic approach and avoidance tasks involve both visual and musculoskeletal information. For example, bringing spoiled food towards one's nose to smell it is associated with both flexion of the arm and the increase in size of the visual image of the food as it approaches one's nose. To approximate both components of approach and avoidance, Rinck and Becker (2007) developed a new computer task incorporating arm flexion/extension (i.e., moving a computer joystick) as well as visual cues (i.e., increase/decrease in the size of the image as the arm is flexed/extended). In their study, individuals with spider-related fears completed an Approach-Avoidance Task (AAT) in which they saw neutral pictures and spider-related pictures. In the first block of the experiment, half the participants were instructed to push the joystick if they saw a spider picture and to pull it if they saw a spider-free picture; the other half of the participants were instructed to pull the joystick if they saw a spider picture and to push it if they saw a spider-free picture. Pushing the joystick resulted in zooming out of the picture such that the picture became smaller. Pulling the joystick resulted in zooming in of the picture such that the picture became larger. Hence, this task simulated both visual and motor aspects of approach and avoidance. As predicted, individuals with spider fears responded to spider pictures more quickly by pushing than by pulling, whereas non-anxious individuals did not show a significant difference between pushing and pulling. Variations of this AAT have since been used to examine approach and avoidance tendencies in social anxiety (Heuer, Rinck, & Becker, 2007) and problematic drinking behavior (Wiers, Rinck, Dictus, & van den Wildenberg, 2009).
In the study by Wiers and colleagues (2009), participants were instructed to respond to an irrelevant feature of the picture, namely the format (landscape or portrait), rather than to the content of the image itself. The authors interpreted reliable differences in pushing versus pulling particular categories of pictures as relatively automatic behavioral tendencies because they emerged independently of the goal of the task to respond to the picture format. Thus, these action tendencies are likely driven by the automatic evaluation of the picture content. Research has shown that not all attributes of automaticity (i.e., unconscious, capacity-free, involuntary) necessarily apply to the selective processing of threat in anxiety (McNally, 1995). We believe that the AAT is automatic in the sense that it requires little conscious attention to the content of the pictures. Thus, behavioral tendencies in the AAT are automatic the same way as changing gears in a stick-shift car—which requires similar motion to this task—might be automatic for experienced drivers.
In the AAT studies mentioned above, the authors calculated an approach-avoidance index by subtracting participants’ pull scores from their push scores. To validate this index, they correlated it with a self-report measure of spider fear and a spider-related BAT, and found a strong and significant association. One limitation of using the approach-avoidance index is that it assumes that approach towards an object and avoidance away from the object lie on opposite ends of a continuum. In previous studies, the AAT index was calculated by subtracting each participant's median RT in the pull condition from their median RT in the corresponding push condition (e.g., spider-push minus spider-pull, neutral-push minus neutral-pull). This AAT score may reflect the relative direction of action tendencies, with negative values indicating stronger avoidance than approach, and positive values indicating stronger approach than avoidance. In the present study, we hypothesized that movement towards a feared object and movement away from it represent distinct types of reinforcement that underlie avoidance behavior. For example, an individual with contamination fears may find it particularly difficult to pick up an object that she perceives as being contaminated, or she may be particularly quick to wash off perceived contaminants from her hands, or both instances may be true. Thus, the difficulty approaching the feared object and ease of getting rid of the feared object may represent two independent aspects of avoidance. Washing off the contaminant is a behavior that is negatively reinforced (reduction in anxiety increases the behavior) whereas picking up the contaminant is a behavior that is punished (increase in anxiety decreases the behavior). If independent mechanisms underlie behaviors that are increased by negative reinforcement and those that are decreased by punishment, then combining response latencies for the two types of avoidance behaviors into a single index may not be the most informative measure of avoidance.
There are four possible combinations of behavioral tendency and perceived valence of the target: approach towards what is perceived as positive, avoidance of positive, approach towards negative, and avoidance of negative. For instance, psychopathology related to addictive behaviors such as substance abuse represents enhanced approach towards positive (i.e., appetitive action tendencies). We propose that contamination-related obsessive-compulsive symptoms represent both impaired approach towards negative (from the example above, difficulty picking up a “contaminated” object) and enhanced avoidance of negative (urgency to wash off “contaminants” from ones hands). Approach towards negative reflects the individual's ability to inhibit automatic behavioral avoidance tendencies. In the present study, we used the AAT to measure automatic avoidance of threatening stimuli (push trials with threatening pictures) as well as the ability to inhibit automatic avoidance of threatening stimuli (pull trials with threatening pictures) in individuals with contamination-related obsessive-compulsive (OC) symptoms. We hypothesized that, relative to individuals low in contamination-related OC symptoms (LC), individuals high in contamination-related OC symptoms (HC) would display more difficulty inhibiting avoidance of contamination-related stimuli compared to neutral stimuli. Similarly, we hypothesized that, compared to the LC group, the HC group will display more ease avoiding contamination-related stimuli compared to neutral stimuli. Thus, the HC group should have larger response latencies when pulling pictures of contaminants than pictures of neutral objects, and will have smaller response latencies when pushing pictures of contaminants than pictures of neutral objects. Furthermore, we hypothesized that these differences will be specific to the HC group. Thus, a measure such as the AAT should tap a relatively automatic behavior and may help elucidate the processes by which compulsive avoidance behavior is maintained in individuals with OC symptoms.
Method
Participants
Participants comprised 41 individuals who were drawn from a pool of undergraduate students at a large university and received course credit for their participation. Participants were included in the low OC group (LC, n = 21) if they scored 3 or lower on the washing subscale of the Obsessive-Compulsive Inventory-Revised (OCI-R; Foa et al., 2002) or in the high OC group (HC, n = 20) if they scored a 4 or higher. The cut-off was based on a median split of the washing subscale of the OCI-R for our sample. For the HC group, the mean total OCI-R score (M = 25.00, SD = 7.99) and the washing subscale score (M = 5.85, SD = 2.16) is comparable to the mean score for clinical samples of patients with contamination-related OCD. For instance, in an investigation of the psychometric properties of the OCI-R, Huppert et al. (2007) report a total OCI-R score of M = 29, SD = 13.4, and the washing subscale score of M = 7.0, SD = 3.7 for patients identified by a clinical interview to have contamination as their primary symptom of OCD.
The LC and HC groups did not differ on age [t(39) = .24, p > .81], education [t(39) = .74, p > .46], or sex [χ2(1) = .73, p > .39]. Furthermore, the LC and HC groups did not differ significantly on trait anxiety [t(39) = 1.68, p = .10]. As expected, groups differed significantly on self-reported contamination-related OC symptoms [t(39) = 8.93, p < .001]. See Table 1 for demographic and self-report symptom data.
Table 1.
Demographics and Questionnaire Data
| Group | ||
|---|---|---|
| HC (n = 20) | LC (n = 21) | |
| % Female | 70.00a | 57.14a |
| Age | 18.50 (0.89)a | 18.57 (1.03)a |
| Education | 13.00 (0.80)a | 13.24 (1.22)a |
| OCI-R | 25.00 (7.99)a | 7.57 (5.00)b |
| OCI-R Washing | 5.85 (2.16)a | 1.05 (1.16)b |
| STAI-Trait | 42.55 (11.92)a | 36.62 (10.62)a |
Note: OCI-R = Obsessive-Compulsive Inventory-Revised; STAI-Trait = State-Trait Anxiety Inventory-Trait version; means with different subscripts differ significantly
Materials and Tasks
Self-Report Measures
The OCI-R is an 18 item measure comprising statements about everyday experiences that are relevant to general obsessive compulsive symptoms (Foa et al., 2002). Using a 5 point scale ranging from not at all to extremely, participants rate how distressed they would feel by the experience described in the statement. The OCI-R comprises 6 subscales: washing, checking/doubting, obsessing, mental neutralizing, ordering, and hoarding. The scale has been shown to have good psychometric properties (Foa et al., 2002). More specifically, the OCI-R has been shown to have good internal consistency with student populations, with Cronbach's alpha coefficients of 0.88 for the total score and 0.76 for the washing subscale (Hajcak, Huppert, Simons, & Foa, 2004). In the present study, Cronbach's alphas for the total sample were 0.86 and 0.78 for the total OCI-R scale and the washing subscale, respectively. Participants also completed the trait version of the Spielberger Trait Anxiety Inventory (STAI-T; Spielberger, Gorsuch, Lushene, Vagg, & Jacobs, 1983). The STAI-T has adequate psychometric properties.
The Approach-Avoidance Task
The AAT comprised pictures of contamination-related scenes (e.g., dirty toilet, garbage) and neutral pictures (household objects) taken from the International Affective Picture System (IAPS; Lang, Bradley, & Cuthbert, 2008). Each contamination-related picture was matched to the paired neutral picture on color and shape. We created two sets of six pairs of contamination-related and neutral pictures (sets A and B). Half of the participants were presented pictures from set A and the other half from set B. Following completion of the task, participants rated all pictures used in the AAT for emotionality on a scale ranging from -3 (“How disturbing is the picture for you, not for people in general”) to +3 (How pleasant is the picture for you, not for people in general”). Contamination-related pictures were rated as significantly more disturbing than the neutral pictures by both the HC group [t(14) = 10.10, p < .001] and the LC group [t(17) = 15.43, p < .001]1.
To control for possible effects of landscape versus portrait pictures in previous studies using the AAT, in the present study we used color frames to guide the participants’ direction of movement. All pictures were framed by either a blue or a green border. Participants were seated in front of a computer screen, with a joystick situated on the desk. Participants were told that they would see a series of pictures with different colored borders, and that for each picture they should pull the joystick if the border was green, and push the joystick if the border was blue. Thus, participants were asked to respond only to the color of the border framing each picture, rather than to the content within the image itself. Half the pictures with green borders were contamination-related and half were neutral; similarly, half the pictures with blue borders were contamination-related and half were neutral.
Participants completed 16 practice trials, which comprised a different set of neutral pictures than that used in the assessment. In the assessment task, participants completed 288 trials [6 Pictures × 2 Picture Type (contamination-related, neutral) × 2 Border Color (green, blue) × 12 Repetition]. Trials were presented in a new random order to each participant. To begin each trial, participants were required to press a button on the joystick which resulted in the appearance of a medium sized picture on the screen. In each trial, the pictures became increasingly larger if the participant pulled the joystick, simulating approach, and smaller if the participant pushed the joystick, simulating avoidance. When the joystick reached approximately a 30° position in either direction, the picture disappeared, regardless of whether the participant responded correctly. The next trial began once the joystick was brought fully back to the central position. Reaction time was calculated based on the length of time the image remained on the screen, that is, from the time the picture appeared on the screen to the time it disappeared.
Procedure
After completing the informed consent form, participants were asked to fill out a self-report packet comprising demographic information, the OCI-R, and STAI-T. Next, participants completed the AAT. At the end of the study, the research assistant debriefed participants and dismissed them.
Design
The design of the study was a 2 Group (HC, LC) × 2 Picture Type (Contamination-related, Neutral) × 2 Stimulus Set (set A, set B) mixed ANOVA for each Response Direction (Push, Pull).
Results
Consistent with previous studies using the AAT (Heuer et al., 2007; Rinck & Becker, 2007), error rates were uniformly low and groups did not differ significantly on error rate, t(39) = .13, p > .89 [HC: M = .025, SD = .02; LC: M = .026, SD = .02]. Thus, we excluded incorrect responses from all analyses (see Table 2 for mean RTs for Picture Type and Response Direction by Group).
Table 2.
Mean Response Times (ms) by Picture type, Group, and Response Direction
| Picture type | Group | Response Direction |
|
|---|---|---|---|
| Pull | Push | ||
| Contamination | HC | 889 (141) | 785 (104) |
| Contamination | LC | 816 (116) | 712 (108) |
| Neutral | HC | 866 (125) | 774 (96) |
| Neutral | LC | 818 (113) | 711 (94) |
Median RTs for the Push Response Direction were submitted to a 2 (Group: HC, LC) × 2 (Picture Type: Contamination, Neutral) × 2 (Stimulus Set: set A, set B) ANOVA. Stimuli Set did not appear as a significant main effect or interaction (all ps > .16). The main effect of Group was significant [F(1, 37) = 4.55, p = .04, η2 = .11]. However, neither the main effect of Picture Type [F(1, 37) = .26, p > .61, η2 = .01] nor the Group × Picture Type [F(1, 37) = .15, p > .70, η2 = .004] were significant.
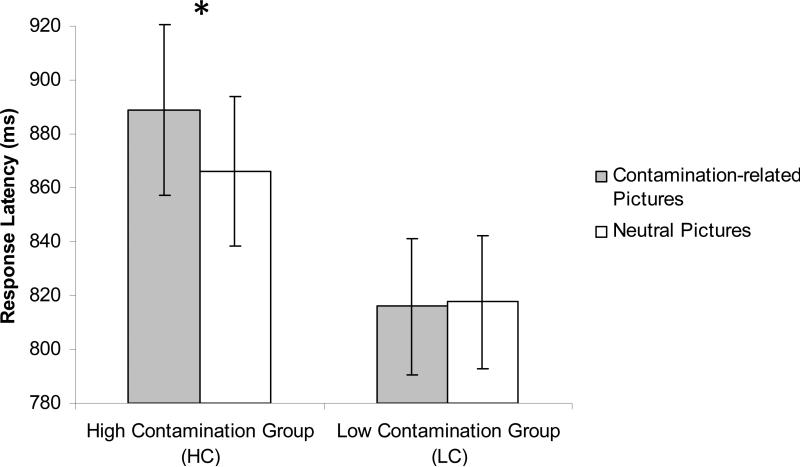
Next, we submitted median RTs for the Pull Response Direction to a 2 (Group: HC, LC) × 2 (Picture Type: Contamination-related, Neutral) × 2 (Stimulus Set: set A, set B) ANOVA. Again, Stimulus Set did not appear as a significant main effect or interaction (all ps > .15). The main effect of Group was not significant [F(1, 37) = 2.23, p = .14, η2 = .06]. The main effect of Picture Type was marginally significant [F(1, 37) = 3.40, p = .07, η2 = .08] and was modified by a significant Group × Picture Type interaction [F(1, 37) = 4.81, p < .04, η2 = .12]. Follow-up simple effects analysis revealed that the HC group was significantly slower at pulling contamination-related pictures than pulling neutral pictures [t(19) = 2.51, p = .02], whereas in the LC group, there was no difference between speed of pulling contamination-related pictures and neutral pictures [t(20) = .21, p > .83]. See Figure 1.
Figure 1.
Response latencies by Group and Picture Type for Response Direction = Pull.
Additionally, for each Response Direction condition, we correlated the difference between response latencies for contamination-related pictures and for neutral pictures with scores of self-reported contamination fears. As predicted, the difference between response latencies for pulling contamination-related pictures and for pulling neutral pictures was significantly correlated with the OCI-R washing subscale score [r(41) = .45, p = .003], whereas the difference between response latencies for pushing contamination-related pictures and for pushing neutral pictures was not [r(41) = .07, p > .64].
Discussion
Individuals high in contamination-related obsessive-compulsive symptoms were slower at pulling pictures of contaminants than pictures of neutral objects, whereas no such difference emerged in individuals low in contamination fears. However, contrary to our hypothesis, individuals high in contamination fears were not faster at pushing pictures of contaminants than pictures of neutral objects. Thus, we found evidence for a biased behavioral response for threatening objects in individuals high in contamination fears only when inhibiting the prepotent response to avoid threatening stimuli (i.e., pulling the feared object closer) and not when performing a practiced avoidance response (i.e., pushing the feared object away). Moreover, the degree of avoidance of contamination-related stimuli relative to avoidance of neutral stimuli was significantly correlated with self-reported contamination-related obsessive-compulsive symptoms, but only when pulling contamination-related stimuli.
Our results validate the use of the AAT as a measure of inhibited and uninhibited automatic avoidance reactions to threatening information in individuals with contamination-related obsessive-compulsive symptoms. The behavioral tendencies assessed by the AAT are automatic in the sense that they require little conscious attention to the content of the threat-related stimuli presented in the task. Moreover, these results highlight the fact that moving a feared object closer versus moving it away are not necessarily inversely correlated behavioral tendencies. Instead, they represent independent aspects of behavior. A functional analysis reveals distinct types of reinforcement that underlie the two aspects of avoidance behavior. Pushing away a feared object is a behavior that is negatively reinforced (reduction in anxiety increases the behavior) whereas approaching a feared object is a behavior that is punished (increase in anxiety decreases the behavior). Indeed, our results lend support to the idea that independent mechanisms underlie behaviors that are increased by negative reinforcement those that are decreased by punishment. More specifically, our results suggest that individuals high in contamination-related obsessive-compulsive symptoms do not necessarily have stronger automatic avoidance tendencies; instead, they exhibit impaired inhibition of these tendencies.
Recently, the AAT has been modified to change automatic behavioral tendencies in individuals with substance abuse problems (Wiers, Rinck, Kordts, Houben, & Strack, 2010). This research is based on dual-process models of addictive behaviors (Deutsch & Strack, 2006) that suggest that these addictive behaviors are maintained by two independent systems: an impulsive system in which the valence of stimuli are evaluated automatically, and a reflective system which entails more deliberate, conscious evaluations. According to these models, behavioral tendencies associated with the impulsive system are automatic, whereas those associated with the reflective system are slower and determined by more strategic, controlled processes. Wiers et al. (2010) adapted the AAT to modify automatic action tendencies of the impulsive system to train participants to avoid alcohol. In the avoid-alcohol condition, participants pushed pictures of alcoholic beverages and pulled pictures of non-alcoholic beverages. They were instructed to respond to the format of the pictures (landscape versus portrait) and not explicitly to the content of the pictures. Results of the study revealed that action tendencies for alcoholic drinks had indeed changed in accordance with training condition. These effects were found not only on automatic behavioral bias measured by the AAT but also on actual drinking behavior during a taste-test that was administered to participants at the end of the training. Participants in the avoid-alcohol training condition consumed less alcohol than participants in the approach-alcohol condition. Because substance abuse involves enhanced approach towards perceived positive (in this case, alcohol), it follows that treatment comprises training avoidance of positive. Results of the present study suggest that contamination-related obsessive-compulsive symptoms involve impaired inhibition of automatic avoidance tendencies. Following from the rationale of the AAT training study by Wiers et al. (2010), a next step from the present research would be to modify the AAT to train the inhibition of automatic avoidance tendencies that interfere with controlled approach behavior in individuals with contamination-related obsessive-compulsive symptoms.
Our study has limitations. First, our findings are in a non-clinical sample and therefore may not generalize to individuals with a clinical diagnosis of OCD. Follow-up studies conducted with individuals with OCD would greatly improve the conclusions that can be drawn regarding the use of the AAT in OCD. Moreover, although the absence of a significant difference between the groups on trait anxiety could be viewed as a strength of our study in that it suggests that the findings are specific to contamination fear and not anxiety in general, it also raises questions about the validity of our analogue group, as patients with OCD are usually characterized by elevated trait anxiety (e.g., Tolin, Abramowitz, Brigidi, Amir, Street, & Foa, 2001). A limitation of our assessment measures is that the washing subscale of the OCI-R may not capture the range of contaminated-related behavior. In future studies, multi-item contamination-related BATs (e.g., Cougle et al., 2007; Najmi & Amir, 2010) should be used to assess their association with behavioral biases on the AAT. Another limitation of our assessment measures is that we did not include measures of disgust in our study. Future studies using the contamination AAT should include a measure of disgust propensity/sensitivity to test whether disgust functions as a mediating variable. Finally, we restricted our research question to the contamination subtype of OCD so that we could standardize the stimuli used in the AAT. It may be the case that our results generalize more readily to other forms of specific fear than to other symptoms of OCD. Additional research with the various OCD subtypes is needed to determine the generalizability of our findings for this heterogeneous disorder.
The above limitations notwithstanding, our study is the first to demonstrate the use of a measure of automatic avoidance tendencies in individuals with obsessive-compulsive symptoms. If replicated in a clinical sample of OCD patients, these findings may have promising implications for the assessment of treatment gains in individuals with OCD. The behavioral treatment of exposure with response prevention is considered the psychological treatment of choice for OCD. If replicated in a clinical sample, these findings suggest the potential for using the AAT to modify automatic behavioral tendencies and to facilitate the behavioral approach required for exposure therapy.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Five participants from the HC group and 3 participants from the LC group did not complete the picture ratings.
References
- Baumeister R, Vohs K, Funder D. Psychology as the science of self-reports and finger movements: Whatever happened to actual behavior? Perspectives on Psychological Science. 2007;2(4):396–403. doi: 10.1111/j.1745-6916.2007.00051.x. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Priester JR, Bernston GG. Rudimentary determinants of attitudes. II. Arm flexion and extension have differential effects on attitudes. Journal of Personality and Social Psychology. 1993;65(1):5–17. doi: 10.1037//0022-3514.65.1.5. [DOI] [PubMed] [Google Scholar]
- Chen M, Bargh JA. Consequences of automatic evaluation: Immediate behavioral predispositions to approach or avoid the stimulus. Personality and Social Psychology Bulletin. 1999;25:215–224. [Google Scholar]
- Cougle J, Wolitzky-Taylor K, Lee H, Telch M. Mechanisms of change in ERP treatment of compulsive hand washing: Does primary threat make a difference? Behaviour Research and Therapy. 2007;45(7):1449–1459. doi: 10.1016/j.brat.2006.12.001. [DOI] [PubMed] [Google Scholar]
- Deutsch R, Strack F. Reflective and impulsive determinants of addictive behavior. In: Wiers RW, Stacy AW, editors. Handbook of implicit cognition and addiction. SAGE Publishers; Thousand Oaks, CA: 2006. pp. 45–57. [Google Scholar]
- Eisen JL, Steketee G. Course of illness in obsessive-compulsive disorder. In: Dickstein LJ, Riba MB, Oldham JM, editors. Review of psychiatry. Vol. 16. American Psychiatric Press; Washington, DC: 1997. [Google Scholar]
- Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G, et al. The Obsessive-Compulsive Inventory: Development and validation of a short version. Psychological Assessment. 2002;14:485–496. [PubMed] [Google Scholar]
- Foa EB, Kozak MJ, Salkovskis P, Coles ME, Amir N. The validation of a new obsessive-compulsive disorder scale: The Obsessive-Compulsive Inventory. Psychological Assessment. 1998;10:206–214. [Google Scholar]
- Foa EB, Steketee G, Grayson JB. Imaginal and in vivo exposure: A comparison with obsessive-compulsive checkers. Behavior Therapy. 1985;16:292–302. [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, et al. The Yale-Brown Obsessive Compulsive Scale: I. Development, use, and reliability. Archives of General Psychiatry. 1989;46:1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- Hajcak G, Huppert JD, Simons RF, Foa EB. Psychometric properties of the OCI-R in a college sample. Behaviour Research and Therapy. 2004;42(1):115–123. doi: 10.1016/j.brat.2003.08.002. [DOI] [PubMed] [Google Scholar]
- Heuer K, Rinck M, Becker ES. Avoidance of emotional facial expressions in social anxiety: The Approach-Avoidance Task. Behaviour Research and Therapy. 2007;45:2990–3001. doi: 10.1016/j.brat.2007.08.010. [DOI] [PubMed] [Google Scholar]
- Hodgson RJ, Rachman S. Obsessional-compulsive complaints. Behaviour Research and Therapy. 1977;15:389–395. doi: 10.1016/0005-7967(77)90042-0. [DOI] [PubMed] [Google Scholar]
- Huppert J, Walther M, Hajcak G, Yadin E, Foa E, Simpson H, et al. The OCI-R: Validation of the subscales in a clinical sample. Journal of Anxiety Disorders. 2007;21(3):394–406. doi: 10.1016/j.janxdis.2006.05.006. [DOI] [PubMed] [Google Scholar]
- Kawakami K, Phills CE, Steele JR, Dovidio JF. (Close) distance makes the heart grow fonder: Improving implicit racial attitudes and interracial interactions through approach behaviors. Journal of Personality and Social Psychology. 2007;92(6):957–971. doi: 10.1037/0022-3514.92.6.957. [DOI] [PubMed] [Google Scholar]
- Lang PJ, Bradley MM, Cuthbert BN. International affective picture system (IAPS): Affective ratings of pictures and instruction manual. Technical Report A-8. University of Florida; Gainesville, FL: 2008. [Google Scholar]
- McNally R. Automaticity and the anxiety disorders. Behaviour Research and Therapy. 1995;33(7):747–754. doi: 10.1016/0005-7967(95)00015-p. [DOI] [PubMed] [Google Scholar]
- Najmi S, Amir N. The effect of attention training on a behavioral test of contamination fears in individuals with subclinical obsessive-compulsive symptoms. Journal of Abnormal Psychology. 2010;119(1):136–142. doi: 10.1037/a0017549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narrow WE, Rae DS, Robins LN, Regier DA. Revised prevalence estimates of mental disorders in the United States. Archives of General Psychiatry. 2002;59:115–123. doi: 10.1001/archpsyc.59.2.115. [DOI] [PubMed] [Google Scholar]
- Neumann R, Hülsenbeck K, Seibt B. Attitudes towards people with AIDS and avoidance behavior: Automatic and reflective bases of behavior. Journal of Experimental Social Psychology. 2004;40:543–550. [Google Scholar]
- Rachman S, Marks I, Hodgson R. The treatment of obsessive-compulsive neurotics by modelling and flooding in vivo. Behaviour Research and Therapy. 1973;11(4):463–471. doi: 10.1016/0005-7967(73)90105-8. [DOI] [PubMed] [Google Scholar]
- Rinck M, Becker ES. Approach and avoidance in fear of spiders. Journal of Behavior Therapy and Experimental Psychiatry. 2007;38:105–120. doi: 10.1016/j.jbtep.2006.10.001. [DOI] [PubMed] [Google Scholar]
- Solarz A. Latency of instrumental responses as a function of compatibility with the meaning of eliciting verbal signs. Journal of Experimental Psychology. 1960;59:239–245. doi: 10.1037/h0047274. [DOI] [PubMed] [Google Scholar]
- Spielberger C, Gorsuch R, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory: STAI (Form Y) Consulting Psychologist Press; Palo Alto, CA: 1983. [Google Scholar]
- Steketee G, Barlow DH. Obsessive-compulsive disorder. In: Barlow DH, editor. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2nd ed. Guilford Press; New York: 2002. [Google Scholar]
- Steketee G, Chambless DL, Tran GQ, Worden H, Gillis MM. Behavioral avoidance test for obsessive compulsive disorder. Behaviour Research and Therapy. 1996;34(1):73–83. doi: 10.1016/0005-7967(95)00040-5. [DOI] [PubMed] [Google Scholar]
- Strack F, Deutsch R. Reflective and impulsive determinants of social behavior. Personality and Social Psychology Review. 2004;8:220–247. doi: 10.1207/s15327957pspr0803_1. [DOI] [PubMed] [Google Scholar]
- Tolin DF, Abramowitz JS, Brigidi BD, Amir N, Street GP, Foa EB. Memory and memory confidence in obsessive-compulsive disorder. Behaviour Research and Therapy. 2001;39:913–927. doi: 10.1016/s0005-7967(00)00064-4. [DOI] [PubMed] [Google Scholar]
- Wiers RW, Rinck M, Dictus M, van den Wildenberg E. Relatively strong automatic action-tendencies in male carriers of the OPRM1 G-allele. Genes, Brain, and Behavior. 2009;8:101–106. doi: 10.1111/j.1601-183X.2008.00454.x. [DOI] [PubMed] [Google Scholar]
- Wiers RW, Rinck M, Kordts R, Houben K, Strack F. Retraining automatic action-tendencies to approach alcohol in hazardous drinkers. Addiction. 2010;105(2):279–287. doi: 10.1111/j.1360-0443.2009.02775.x. [DOI] [PubMed] [Google Scholar]